Abstract
Purpose: This study evaluates the effect of power wheelchair telemonitoring and battery charging training on user charging behavior and repair measures and assesses the relationship between wheelchair usage and repair measures to support technician-led servicing.Methods: This is a retrospective analysis of two matched cohorts with a total of n=237 users from the NHS service dataset. In the training cohort, a wheelchair usage telemonitoring device monitored the battery usage of n=119 power wheelchair users for 12 months. Users whose battery charging behavior was not optimal were instructed on appropriate charging practices. Wheelchair usage parameters of wheelchair drive and power time every month were used to predict repairs and associated costs.Results: Fifty-four out of 119 users in the training cohort did not charge batteries regularly and were instructed on appropriate charging. Twenty-six of them changed their behavior and charged their batteries every night. This cohort experienced reduced battery repairs by 18%, wheelchair repairs by 11%, and repair costs by £3,092 compared to a matched standard care cohort (n=118). User age and drive time were associated with repair measures. Drive time predicted time-to-failure for wheelchair parts and classified failure risk with the area under the receiver operating characteristic curve as 0.71 (95% CI 0.61 to 0.82; p<.001). Conclusions: By leveraging the significant relationships between wheelchair usage and repairs, wheelchair users at risk of part failures can be identified, and technician-led servicing tools for proactive interventions can be developed. Wheelchair battery health telemonitoring and instructing users on appropriate battery charging reduced repairs and associated costs.
IMPLICATIONS FOR REHABILITATION
Proactive wheelchair servicing by repair technicians in collaboration with wheelchair users safeguards users against critical part failures and minimises repair-related operating costs for service providers.
Providers should leverage wheelchair telemonitoring technologies and related research outputs to improve repair services and support their clients’ continued mobility and community participation.
It is important that healthcare plans and policies recognise the benefits of proactive wheelchair servicing and use data as a tool to allocate device usage and performance-based reimbursements.
Introduction
Globally, 80 million people with locomotor disabilities need wheelchairs [Citation1]. Wheelchair devices provide a means of community mobility, participation, and access to meaningful daily activities. Engaging in daily activities through a wheeled device enhances independence and quality of life. Unfortunately, these devices often break and require repair, reducing access to work, community, and other aspects of daily life [Citation2–4].
Over the last 15 years, cross-sectional study findings approximate that 45%-88% of wheelchair users experience part failures and repairs every 6 months [Citation2–5]. Components often fail, including casters, rear wheels, batteries, armrests, joysticks, and motors [Citation6]. Like part failures, immediate consequences have climbed from 9% to 44% [Citation3,Citation5,Citation7–9]. Users experience immediate consequences such as injury, missing work or school, or inability to participate in critical daily activities. Reports reveal that once the chair is dysfunctional, many users are subject to extended wait periods before repairing their wheelchairs [Citation10,Citation11]. Experiencing immediate consequences has been linked to long-term consequences of bed sores, pain, and depression [Citation12]. Not only are health and function outcomes affected, but a survey of n = 173 wheelchair users reported that device quality, repairability, and reliability affect community participation [Citation13]. User frustration from adverse consequences and longer repair wait times has led to enacting the Right to Repair law in Colorado [Citation14], where users, caregivers, and local technicians can purchase parts directly from manufacturers and conduct repairs sooner instead of calling their provider for such services. Taken together, frequent wheelchair part failures negatively impact users and should be prevented.
Wheelchairs, like other commercial mobility and transportation equipment like passenger vehicles, undergo standardised quality testing. Product regulatory agencies, mostly in developed countries, use the International Organisation for Standardisation (ISO) 7176 standards to evaluate wheelchair quality before approval for marketing and sale [Citation15]. While standards set the minimum screening requirement for quality, wheelchair devices suffer from a lack of upkeep in the community. Like passenger vehicles, servicing wheelchairs is necessary. Servicing includes maintenance, repair and replacement of wheelchairs according to Medicare policy [Citation16]. Maintenance includes upkeep of the parts to stay functional and last longer before they fail and need repair. Repair is needed after a part partially fails to function as intended; repair activities include inspection followed by adjusting, cleaning, or greasing parts. Replacement is necessary when the part can no longer serve its intended function or cannot be repaired. When wheelchair repair technicians perform these servicing activities, it can prevent or reduce part failures and mediate the consequences of wheelchair failures [Citation17,Citation18]. A randomised controlled trial (n = 243) by Hansen et al. 2004 found that an active check-up intervention significantly reduced repairs and accidents compared with standard care [Citation17]. Servicing by technicians was also proven effective in a secondary data analysis of n = 6470 caster repairs reported in a U.S. wheelchair repair registry [Citation18]. Servicing was performed for the front casters following condition inspection during repair visits for other broken wheelchair parts, which significantly reduced repairs that could cause user injury or damage to other wheelchair parts. Despite the evidence favouring technician-led wheelchair servicing, it is rarely conducted.
The current policies adopted by Medicare and private healthcare payers do not support active servicing. Wheelchairs are considered durable medical equipment for indoor and institutional use, and they are repaired by providers following part failure or wheelchair breakdown only if the wheelchair continues to serve the user’s medical needs [Citation16]. Wheelchair service providers are reimbursed only for repair and replacement of parts and related labour but not for technician travel to the user’s home and repair diagnostics, making servicing or the repair unit of the wheelchair service business a burden for providers [Citation19]. The lack of reimbursement has resulted in a lack of innovation; no automated tools or technologies exist to inform technicians of users at risk of part failures and coordinate the replacement of critical parts before they break. Maintenance is the responsibility of users per policy. Manufacturers include maintenance guidelines in their user manuals. Research groups have developed maintenance training programs [Citation20,Citation21]. Training programs improve user knowledge, satisfaction, and compliance [Citation21–23]; however, the training research has yet to demonstrate the efficacy of failure prevention. A recent qualitative study showed that maintenance burdens some users for various reasons, including a lack of user training, knowledge, physical ability, and access to tools and personnel support. In sum, appropriate tools to inform technicians for active servicing interventions are required so that wheelchair users are not left vulnerable to the continuous risk of wheelchair failures leading to repairs, adverse consequences, and hardships.
This retrospective study addresses research gaps to support new servicing tool development and suitable wheelchair servicing interventions. It analyzes data on power wheelchair repairs, battery maintenance, and telemonitored usage from two matched cohorts – a telemonitoring (TM) device intervention cohort and a standard care cohort. The study explores 1) whether servicing enabled by the TM device affects repairs and associated costs and 2) the feasibility of using telemonitored usage as a servicing tool to screen power wheelchair users at risk of frequent repairs. The following are the study’s research questions and aims:
Research Question 1: Is wheelchair battery maintenance training effective in reducing repairs and associated costs?
Aim 1: To compare the number of repairs and associated costs between the TM device and standard care cohorts.
Research Question 2: Which power wheelchair usage and user demographic factors can predict high-risk users in the TM device cohort?
Aim 2: To evaluate the relationship between wheelchair usage factors, user demographic characteristics, wheelchair location of use, and repair measures.
Aim 3: To test the feasibility of diagnosing users at high risk of failure.
Materials and methods
Study design
This is a retrospective analysis study where the National Health Services of West of Scotland Mobility and Rehabilitation Centre (NHS) observed two matched cohorts for 12 months and collected data on usage parameters and repair measures. The evaluation data comes from power wheelchair users in and around the Greater Glasgow area, whom the NHS clinic serves.
Materials
A power wheelchair controller manufacturer developed Dealer Data—a power wheelchair TM device (see ). This device connects with power wheelchair controllers and enables repair technicians to monitor usage parameters, battery health, and error codes and perform servicing as needed. This study evaluates this TM device with an application for battery servicing for a Group 2 power wheelchair model (no seating functions) of a leading manufacturer. The model did not include sub-models, but additional wheelchair accessories may be installed.
Figure 1. Dealer Data device data collection process.

Recruitment
Between February 2015 and April 2015, the NHS database was used to identify users and randomly assign them to two cohorts. Selective matching criteria were user age, the number of repairs in the previous year, and the age of the wheelchair at the beginning of the evaluation. Inclusion criteria for the evaluation were 18 years or older and a user of the selected power wheelchair model. Exclusion criteria were wheelchair issued less than 12 months ago or longer than 50 months. There was an increased likelihood of wheelchairs issued for over 50 months being replaced before the end of the one-year evaluation from May 2015 to April 2016. Wheelchairs issued 12 months before were needed because included participants were supposed to have a history of repairs. Also, 12 months are typically required for users to get used to a routine wheelchair-driving pattern. Post hoc analysis with an effect size of 0.22, as reported in the results section with a sample size of 120 and assuming no behaviour change in the standard care cohort, gives a study power of 0.79 with α = .05.
Importance of wheelchair battery charging
Like electric vehicles, power wheelchair batteries require regular charging by users or caregivers. Power wheelchair user manuals and maintenance checklists [24] recommend wheelchair charging as a regular servicing routine so that batteries remain reliable. The standard care cohort received standard instructions on regularly charging batteries, usually overnight. The standard care service by NHS requires instructing or training wheelchair users during wheelchair fitting and repair-related clinic visits. This cohort was passively monitored and not contacted otherwise during the study. The TM device cohort received the device, allowing NHS technicians to monitor battery health and charging behaviour and, as part of the care delivery, screen users in the cohort to receive further charging instructions over the phone for practicing appropriate charging behaviour. As shown in Supplementary Material S1, a modified repair process was followed for the TM device cohort, while the other cohort underwent a standard repair process.
Battery charging training
TM device cohort participants were contacted sequentially by phone to discuss participation in the evaluation and procedures until the required sample size was reached. Interested users were visited at home. The TM device was demoed, followed by a discussion of additional service of battery charging training. If the user agreed to participate in the evaluation, the device was fitted to the wheelchair using adhesive-backed Velcro, and the user was registered on the data collection portal. During the 12-month evaluation, data on wheelchair use, tilt-recline actuator use, battery charging, and fault codes was collected on a data collection portal (see ). If a participant did not regularly charge the battery for at least 8–10 h daily or preferably every night, as instructed during initial wheelchair provision, the NHS team contacted them for training. The user was instructed on the importance of charging the battery every day for at least 8 h. This can happen when the wheelchair is not used, typically when participants go to bed. To emphasise the importance of longer battery life and preventing adverse consequences of battery failure, NHS sent monthly summaries informing users how their wheelchair was used. The monthly report (Supplementary Material S2) includes tips on improving the performance of the wheelchair and on improving battery-charging behaviour. Error codes from the TM device assisted in planning servicing activities in this cohort.
Data collection
De-identified data from NHS service dataset was made available to the OSU study team, including postcode, wheelchair issued date, duration of power wheelchair use in years, disability type (congenital/acquired/progressive), date of birth or age, gender, and wheelchair repair history. TM device provided usage measures: wheelchair drive time (hours), activity bouts and duration, power-up time (hours), fault code, and battery indicators of charging time, charging level (%), and voltage dip duration (hours) and level (volts). While TM devices can collect continuous data, only the means of usage measures were available in the shared dataset. Repairs in both cohorts over the course of the evaluation, including information on dates of repairs, repair and replacement parts used, and costs of parts, labour, technician travel, and administration, were tracked by the NHS team.
Data analysis
Data was cleaned prior to analysis. Descriptive statistics were computed for demographic and wheelchair-related information and TM device parameters. Differences in continuous variables were compared using paired t-tests and categorical ones (gender and diagnosis) using the Chi-square tests. Battery voltage dips below the typical 25 V full battery voltage level were categorised into moderate dips (voltage dropped below 24 V) and serious dips (voltage dropped below 21 V).
Efficacy testing of battery maintenance training (aim 1)
The percentage of users in the TM device cohort whose behaviour changed after the training was recorded. The efficacy of the battery charging maintenance training was assessed between the cohorts by the percentage difference in repair frequency across batteries and other parts and repair costs.
Usage-repair relationship (aim 2)
The Pearson correlation was used to evaluate associations between wheelchair usage measures, participant demographic characteristics, and repair measures. Once significant correlations were identified, regression modelling was performed to test the association with repair measures. In the TM device cohort, the usage measures of users with no repairs were compared to those witnessing repairs using t-tests.
Effect of location of wheelchair use on repair measures (aim 2)
Differences in wheelchair usage and repair between rural and urban locations were compared. The user’s postcode was used to generate the urban and rural classification using the 2016, 6-fold NHS Urban Rural Classification [Citation25]. In this classification, classes 1–2 are urban, and 3–6 are rural areas. ANOVA tested differences in usage and repair measures between urban and rural areas.
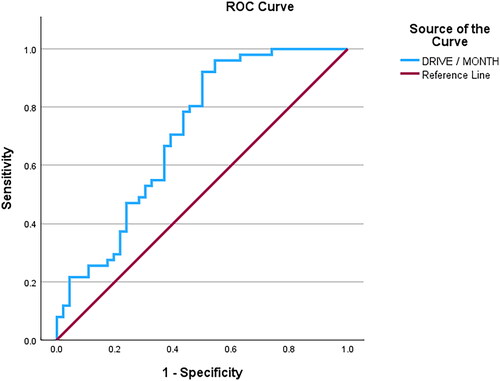
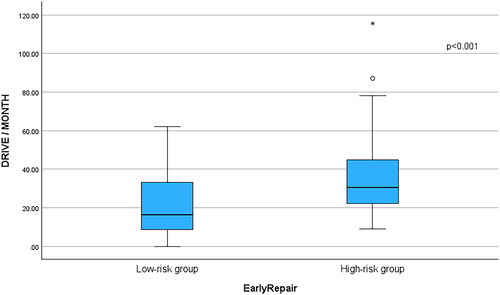
Diagnosing high-risk users (aim 3)
Correlated independent variables were tested to diagnose failure risk. Participants who received the TM device were grouped into two categories: one with multiple repairs within 6 months (high-risk) and the other with one or no repairs (low-risk) during the study. A 6-month interval was chosen since research on power wheelchair repairs shows a high part repair frequency within 6 months of use. A receiver-operating-characteristic (ROC) curve was generated to assess how well the correlated variable(s) classify the high- and low-risk participants [Citation26]. The area under the ROC curve (AUC) shows the accuracy of classification or diagnosis. The ROC curve with the largest AUC is considered to have a better diagnostic performance. Those who participated for less than 6 months were omitted from this analysis.
The level of significance was set a priori at α = .05. All statistical analyses were performed using SPSS 28.0.
Results
Characteristics of participants and repairs are listed in . Fewer than 9 participants declined to participate because they believed their location was tracked or the wheelchair could be taken back during or after the study. Electronic repairs included repairs witnessed with cables, power modules, batteries and battery chargers, remote controllers, and actuators. In the TM device cohort, the study participation averaged 9.42 ± 4.03 months, with 31 participants withdrawing during the evaluation period. Eight-five out of 119 participants in the TM device cohort witnessed a total of 257 repairs. Comparatively, 88 out of the 118 in the standard care cohort experienced 287 repairs. Wheelchair usage parameters recorded by the TM devices are shown in .
Table 1. Demographic characteristics and wheelchair repairs per user for the two study cohorts.
Table 2. Wheelchair usage recorded for the TM device cohort.
Efficacy testing of battery maintenance training
After reviewing battery charging behaviour, 54 out of 119 users were contacted to provide charging training, and 26 out of the 54 changed their charging practices. Before the training, users missed at least 3 days per week of charging and charged the battery for at most 4 h. Following training and behaviour change, charging occurred for at least 8 h every night. shows the difference in the charging behaviour of a participant before and after.
Figure 2. Battery charging behaviour (A) before training and (B) after training.

Usage-repair relationship in the TM device cohort
User characteristics and TM device information on wheelchair usage were related to repair measures. Participant’s age and drive time per month were moderately associated with total repairs (F(2118) = 26.12, p < .01, R2 = .31), electronic repairs (F(2118) = 8.35, p < .01, R2 = .12), and caster repairs (F(2118) = 13.6, p < .01, R2 = .19) and total repair costs (F(2118) = 26.97, p < .01, R2 = .32). Battery voltage dip duration and frequency of serious voltage dips were associated with battery failures (F(1118) = 19.01, p < .01, R2 = .25). Drive time per month was associated with the time-to-failure for wheelchair parts (F(1118) = 17.1, p < .01, R2 = .13). In the standard care cohort, age was weakly associated with total repair costs (F(2117) = 5.99, p < .05, R2 = .05).
Effect of location of wheelchair use on repair measures
Ninety-six participants in the TM device cohort were from urban areas, while 23 were from rural areas. Between the areas, usage and repair measures varied, as shown in .
Table 3. Wheelchair usage and repair measures for TM device cohort users in urban and rural areas.
Diagnosing high-risk users
Fifty-one participants experienced between 2 to 13 repairs within 6 months and were allocated to a high-risk group. The low-risk group included 46 participants who experienced one or no repair during the evaluation. Twenty-one users had withdrawn before 6 months of data collection and were excluded from the ROC model. shows the distributions of drive time per month of both groups. The high-risk group drive time (36.42 ± 21.29h) was significantly higher than the low-risk group drive time (22.18 ± 17.82h). When driving time per month was used to classify participants into two groups, the area under the ROC curve was 0.71 (95% CI 0.61 to 0.82; p < .001) (). At the cut-off of 15.42h, drive time per month predicted repairs with 92% sensitivity and 50% specificity.
Figure 3. Comparing high-risk to low-risk failure groups.
Discussion
Telemonitoring wheelchair usage by technicians and intervening to modify users’ battery charging behaviour reduced repairs and associated costs. Twenty-six out of the 54 users contacted for training charged batteries regularly, contributing to a difference in battery repairs by 18% between the two study cohorts. This repair reduction translated into reduced battery repair costs by £882 and annual NHS operations spending by £3092 on all wheelchair part repairs for the TM device cohort. While the telemonitoring-based servicing intervention led to fewer repairs and financial benefits, there was no statistically significant difference in repair measures between the TM device and standard care cohorts. The battery charging maintenance did not yield a significant effect. To make servicing effective and contribute to additional cost savings, the authors emphasise employing technician-led, proactive wheelchair servicing interventions. Hansen [Citation17] and Mhatre [Citation18] demonstrated that technician inspection and servicing reduce repairs. However, routine manual inspections, as performed in these studies, are not reimbursed. This calls for novel tools to screen users at risk for failures and inform technicians. Usage-failure relationships observed in this study can assist with such developments.
Wheelchair usage and user demographic characteristics are linked to failures. Normalised drive time and user’s age are moderately associated with repair counts and costs. Identifying these usage risk factors led to the development of classification and regression models. Drive time monitored by the TM device effectively classifies users at high- and low-risk of frequent failures. Once such a diagnosis has occurred, drive time, similar to mileage in passenger vehicles, can be used to predict servicing type and intervals as part of the prognosis. Such failure diagnostic and prognostic models can become part of fleet management services that providers and technicians can leverage to telemonitor wheelchair usage and coordinate servicing events, especially replacing parts before they break and reducing wheelchair waste.
Although a statistical significance was observed in usage-failure correlations, the R-squared values are low to moderate. For an exploratory study performed by clinicians and repair technicians in the field along with new technology implementation, these moderate correlations are practically useful to drive future research. The authors aim to evaluate the usage-failure relationship further with comprehensive and granular data collection and improve the accuracy of the models. The identified risk factors can be monitored prospectively for the development of longitudinal failure progression models. Wheelchair road shocks and environmental factors have been identified as risk factors in previous works [Citation27] and should be included in modelling. In addition to central measures of tendency, time-frequency domain features of the correlated variables can be employed. The development of advanced analytical models and machine learning models is highly encouraged in future work.
The drive time per month cut-off value of 15.42h from the ROC analysis is a statistical value that technicians and clinicians can use for diagnosing a high-risk client. Wheelchair users who drive more than this cut-off value should schedule routine inspections. For this value to be of clinical relevance, it must be informed by the impact of adverse consequences on the user, which should be documented in future works.
Most of the TM device cohort participants came from urban NHS. The number of wheelchair repairs was twice as many in urban areas compared to rural areas, potentially owing to greater wheelchair usage indicated by drive time. The observed difference in usage could be attributed to the lack of accessibility and rehabilitation services in rural areas necessary to keep users mobile in the community. NHS should ensure inaccessibility does not translate into healthcare inequity or poor health outcomes for rural wheelchair users.
The study findings demonstrate alignment with published evidence. Cross-sectional survey studies have reported a 45-88% failure rate in 6 months [Citation2–5]. Grouping both cohorts, this study witnessed an 86% failure rate over 12 months. This result is comparable to the participants in the previous studies, who were in their 40s, while this study’s participants were 20 years older. Also, the younger the participants, the greater the usage, so a lesser failure rate in this study seems reasonable. This failure-user age relationship may have influenced the rate of failures in the standard care cohort, which was, on average, 5 years younger than the TM device cohort.
Comparing proportions across previous wheelchair repair reporting studies in the US [Citation4,Citation6], critical parts like batteries and casters had lower repairs in this study. On the other hand, the usage parameters of drive time and activity bout counts recorded by the TM device were slightly higher than that reported for power wheelchair devices in US [Citation28]. More repairs with less usage suggest that outdoor use conditions, device quality and user training differ between the UK and US. While this may be attributed to the service provision models in both countries and stakeholder interests, the telemonitoring of wheelchair condition and the proactive servicing approach are imperative for the US wheelchair sector. Repair savings from this approach should persuade US providers who have suffered financial losses historically [Citation19]. Additionally, providers seem to club servicing activities for users when they visit for inspection or repair visits because of travel-related reimbursement restrictions [Citation18]. Telemonitoring wheelchairs using servicing technology like TM devices can assist with coordinating and clubbing servicing visits in distant areas that require significant travel. Additionally, collaborating with users for servicing interventions, as done in this study, may prove beneficial. For instance, beyond performing maintenance activities, users could be alerted about visiting the rehabilitation repair service shop for inspection, a facility that is available in the latest passenger car models. Such future work calls for collaborative science where repair service providers and healthcare plan providers work with researchers towards assessing the effectiveness of technician-led, model-based servicing enabled by wheelchair usage telemonitoring technology.
Study limitations
About 50% of wheelchair user participants in the TM device cohort contacted by NHS technicians did not change their behaviour, signalling the need for alternate behaviour change approaches. The reasons for their non-compliance were not recorded. In the TM device cohort, participants should have been instructed on the device’s functionality to address privacy concerns and support recruitment. Discontinuity was observed in usage data collection with 31 participants due to several reasons, including the TM device being damaged from contact with a wheelchair part, users moving home, spending time in the hospital, being fitted with a replacement chair, being frustrated or annoyed due to flashing lights from the hub or going on vacation. Another limitation is the lack of usage information and charging behaviour in the standard care cohort, which was explicitly used to compare repair measures in this study. Cost calculations did not include costs associated with TM devices and running the telemonitoring and training service.
Conclusions
While the wheelchair repair rate continues to rise in the community, wheelchair usage telemonitoring and servicing offer a solution to reduce failures, repairs, and associated costs. The battery charging intervention led by technicians and carried out with users in this study reduced failures and costs. Effective interventions can be developed for servicing by repair technicians using the relationships between usage parameters and repair measures to reduce repairs, costs, and adverse consequences to wheelchair users.
Ethical approval
The longitudinal evaluation data was transferred by NHS to The Ohio State University (OSU) for data analysis in December 2022, following NHS Caldicott Guardian approval. The OSU Office of Responsible Research Practices determined that study #2023E0291 did not meet the federal definition of human subject research requiring review because OSU received a de-identified dataset from a third party via a data use agreement and would make no attempts to re-identify participants.
Supplemental Material
Download Zip (876.1 KB)Acknowledgements
The authors are grateful to NHS for supporting study conduct and scientific advice.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- World Health Organization. Wheelchair provision guidelines. Geneva: World Health Organization, 2023. Accessed: Dec. 12, 2023. Online]. Available: https://www.who.int/publications/i/item/9789240074521
- Mhatre A, Martin D, McCambridge M, et al. Developing product quality standards for wheelchairs used in less-resourced environments. Afr J Disabil. 2017;6(0):288. doi: 10.4102/ajod.v6i0.288.
- Toro M, Worobey L, Boninger ML, et al. Type and frequency of reported wheelchair repairs and related adverse consequences among people with spinal cord injury. Arch Phys Med Rehabil. 2016;97(10):1753–1760. doi: 10.1016/J.APMR.2016.03.032.
- Worobey LA, Heinemann AW, Anderson KD, et al. Factors influencing incidence of wheelchair repairs and consequences among individuals with spinal cord injury. Arch Phys Med Rehabil. 2022;103(4):779–789. doi: 10.1016/j.apmr.2021.01.094.
- Henderson GV, Boninger ML, Dicianno BE, et al. Type and frequency of wheelchair repairs and resulting adverse consequences among veteran wheelchair users. Disabil Rehabil Assist Technol. 2020;17(3):331–337.
- James AM, Pramana G, Schein RM, et al. A descriptive analysis of wheelchair repair registry data. Assistive Technol. 2022;35(4):312–320. doi: 10.1080/10400435.2022.2044407.
- McClure LA, Boninger ML, Oyster ML, et al. Wheelchair repairs, breakdown, and adverse consequences for people with traumatic spinal cord injury. Arch Phys Med Rehabil. 2009;90(12):2034–2038. doi: 10.1016/j.apmr.2009.07.020.
- Worobey L, Oyster M, Pearlman J, et al. Differences between manufacturers in reported power wheelchair repairs and adverse consequences among people with spinal cord injury. Arch Phys Med Rehabil. 2014;95(4):597–603. doi: 10.1016/j.apmr.2013.11.022.
- Worobey L, Oyster M, Nemunaitis G, et al. Increases in wheelchair breakdowns, repairs, and adverse consequences for people with traumatic spinal cord injury. Am J Phys Med Rehabil. 2012;91(6):463–469. doi: 10.1097/PHM.0b013e31825ab5ec.
- Boccardi A, Wu F, Pearlman J, et al. Older wheelchair users recommend age-Friendly design improvements to a wheelchair maintenance app: mixed methods development study. JMIR Aging. 2022;5(4):e39301. doi: 10.2196/39301.
- Veterans Health Administration. Veterans health administration audit of the timeliness of VISN 7 power wheelchair and scooter repairs. 2018.
- Hogaboom NS, Worobey LA, Houlihan BV, et al. Wheelchair breakdowns are associated with pain, pressure injuries, rehospitalization, and self-perceived health in full-time wheelchair users with spinal cord injury. Arch Phys Med Rehabil. 2018;99(10):1949–1956. doi: 10.1016/j.apmr.2018.04.002.
- Magasi S, Wong A, Miskovic A, et al. Mobility device quality affects participation outcomes for people with disabilities: a structural equation modeling analysis. Arch Phys Med Rehabil. 2018;99(1):1–8. doi: 10.1016/j.apmr.2017.06.030.
- Colorado General Assembly. Consumer Right To Repair Powered Wheelchairs. 2022. Accessed: Jun. 01, 2023. [Online]. Available: https://leg.colorado.gov/bills/hb22-1031.
- Cooper RA. Wheelchair standards: it’s all about quality assurance and evidence-based practice. J Spinal Cord Med. 2006;29(2):93–94. doi: 10.1080/10790268.2006.11753862.
- U.S. Centers for Medicare & Medicaid Services. “Standard Documentation Requirements for All Claims Submitted to DME MACs (A55426),” 2022. Accessed: Jun. 01, 2023. [Online]. Available: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid = 55426.
- Hansen R, Tresse S, Gunnarsson RK. Fewer accidents and better maintenance with active wheelchair check-ups: a randomized controlled clinical trial. Clin Rehabil. 2004;18(6):631–639. doi: 10.1191/0269215504cr777oa.
- Mhatre A, Pearlman J, Schmeler M, et al. Community-based wheelchair caster failures call for improvements in quality and increased frequency of preventative maintenance. Spinal Cord. 2021;60(1):58–62. doi: 10.1038/s41393-021-00689-3.
- Ruffing J, Schein RM, Schmeler MR, et al. A cross sectional descriptive analysis of complex rehabilitation technology (CRT) provider opinions on the current state of wheelchair repair services. Disabil Rehabil Assist Technol; 2022;19(3):739–744. doi: 10.1080/17483107.2022.2121007.
- Múnera S, Pearlman J, Toro M, et al. Development and efficacy of an online wheelchair maintenance training program for wheelchair personnel. Assistive Technol. 2019;33(1):49–55. doi: 10.1080/10400435.2019.1619632.
- Toro ML, Bird E, Oyster M, et al. Development of a wheelchair maintenance training programme and questionnaire for clinicians and wheelchair users. Disabil Rehabil Assist Technol. 2017;12(8):843–851. doi: 10.1080/17483107.2016.1277792.
- Worobey LA, McKernan G, Toro M, et al. Effectiveness of group wheelchair maintenance training for people with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2022;103(4):790–797. doi: 10.1016/J.APMR.2021.02.031.
- Toro Hernandez ML. “Development, Implementation, and Dissemination of a Wheelchair Maintenance Training Program,” 2016. Accessed: Apr. 03, 2024. [Online]. Available: https://d-scholarship-dev.library.pitt.edu/26290/.
- Model Systems Knowledge Translation Center (MSKTC). “Maintenance Guide for Users of Manual and Power Wheelchairs | Model Systems Knowledge Translation Center (MSKTC).” Accessed: Jun. 04, 2020. [Online]. Available: https://msktc.org/sci/factsheets/maintenance-guide-users-manual-and-power-wheelchairs.
- Scottish Government. “Urban Rural Classification 2016.” Accessed: Dec. 16, 2023. Online]. Available: https://www.gov.scot/publications/scottish-government-urban-rural-classification-2016/pages/2/.
- Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5(9):1315–1316. doi: 10.1097/JTO.0b013e3181ec173d.
- Mhatre A, Reese N, Pearlman J. Design and evaluation of a laboratory-based wheelchair castor testing protocol using community data. PLOS One. 2020;15(1):e0226621. doi: 10.1371/journal.pone.0226621.
- Sonenblum SE, Sprigle S, Harris FH, et al. Characterization of power wheelchair use in the home and community. Arch Phys Med Rehabil. 2008;89(3):486–491. doi: 10.1016/j.apmr.2007.09.029.