Abstract
Purpose: The study examined the benefits of transparent versus non-transparent surgical masks on the speech intelligibility in quiet of adult cochlear implant (CI) users, in conjunction with patient preferences and the acoustic effects of the different masks on the speech signal.
Methods: Speech tracking test (STT) scores and acoustical characteristics were measured in quiet for live speech in three different conditions, without mask, with a non-transparent surgical mask and with a transparent surgical mask. Patients were asked about their experience with the face masks. The study sample consists of 30 patients using a cochlear implant.
Results: We found a significant difference in speech perception among all conditions, with the speech tracking scores revealing a significant advantage when switching from the non-transparent surgical mask to the transparent one. The transparent surgical mask, although it does not transmit high frequencies effectively, seems to have minimal effect on speech comprehension in practice when lip movements are visible. This substantial benefit is further emphasized in the questionnaire, where 82% of the patients express a preference for the transparent surgical mask.
Conclusion: The study highlights significant benefits for patients in speech intelligibility in quiet with the use of medically safe transparent facemasks. Transitioning from standard surgical masks to transparent masks demonstrates highly significant effectiveness and patient satisfaction for patients with hearing loss. This research strongly advocates for the implementation of transparent masks in broader hospital and perioperative settings.
IMPLICATIONS FOR REHABILITATI-ON
In scenarios mandating mask usage, it’s advisable for caregivers to opt for transparent surgical masks. Specifically within perioperative settings, where patients might not be able to utilise their hearing aids or cochlear implants, it becomes imperative for all caregivers to consistently wear transparent surgical masks to prevent communication impediments.
When utilising a transparent surgical mask, caregivers must recognise that sound may be altered and maintaining a clear view of the face and lips is crucial for effective communication.
Introduction
The increasing prevalence of hearing loss underscores the critical importance of considering this factor in hospital communication, particularly as the global response to the COVID-19 pandemic has led to the widespread adoption of mask-wearing policies in healthcare settings. While the pandemic is waning, the continued use of masks in hospitals necessitates an examination of their impact on communication with individuals experiencing hearing difficulties. This is essential for ensuring effective communication and warrants the exploration of alternatives for the non-transparent surgical masks.
The ageing demographic trend anticipates a substantial influx of elderly patients with varying degrees of hearing loss in healthcare settings in the years ahead. According to an estimate by Homans et al. [Citation1], approximately one-third of individuals aged 65 and older in the Netherlands have a hearing loss of 35 dB HL or more[Citation1]. This highlights the persistent need for clear and effective communication strategies in hospitals and other healthcare facilities, especially for the elderly and those with hearing loss.
Non-transparent surgical masks muffle speech and obstruct lip movements and facial expressions, impacting understanding. People with, and even without, hearing difficulties are often dependent on visual cues, such as lip-reading or facial expressions, to understand speech, especially in noisy environments [Citation2]. In hospitals and nursing homes, clear communication is critical for providing safe and effective care. The use of transparent surgical masks can be a possible solution to ensure that hearing-impaired individuals are included in the communication. Furthermore, research has indicated that transparent surgical masks may lead to lower pain scores. This could be attributed to patients feeling more at ease reporting their pain when they can see the healthcare professional’s face [Citation3]. Improved communication can be a potential factor contributing to these lower pain scores. In recent years, both certified and non-certified face masks have become widely available in the market. However, there is limited research on transparent surgical masks with properties similar to surgical, CE-approved, non-transparent surgical masks, especially in the context of enhancing speech comprehension through lip reading for individuals with hearing loss. CE approved indicates that a product complies with European Union legislation. Atcherson showed an improved speech perception performance in noise for listeners with hearing impairment when visual input was provided using a transparent surgical mask[Citation4]. Yi et al. showed when using face masks, either a transparent surgical mask or a non-transparent surgical mask negatively affects speech understanding in noise for individuals with hearing loss, but transparent surgical masks remediated the detrimental effects of face masks on speech intelligibility in noise [Citation5]. Thibodeau stated that the use of transparent surgical masks can significantly facilitate speech recognition in noise even for persons with normal hearing. These earlier findings might offer a significant contribution to healthcare, particularly in perioperative settings where masks are mandatory. In some cases, the use of cochlear implants (CI) or hearing aids may even be restricted, heightening the urgency for solutions in these circumstances. The transparent panel on these masks not only facilitates lip reading but also allows for better visibility of facial expressions. This, in turn, can help reduce misunderstandings and enhance the overall experience for patients who rely on lip reading to comprehend spoken language. Studies have also found that transparent surgical masks and face shields can introduce sound distortion [Citation4,Citation6–10]. The work of Corey et al. (2020) and Homans & Vroegop showed attenuation of sounds above 1 kHz for all type of masks. However, transparent surgical masks and face shields showed to have the worst acoustic performance, as they caused an increase in sound level below 1 kHz and a large attenuation of sound above 1 kHz [Citation6,Citation11,Citation12]. Some studies showed that even those with normal hearing were better able to understand speech in noise when the speaker wore a clear mask instead of a solid one. However, sound distortion is a known problem and improved transparent surgical mask are developed by lowering the mass of the plastic to reduce speech distortion [Citation7,Citation13].
At the Erasmus Medical Centre in Rotterdam, Netherlands, healthcare professionals typically wear non-transparent surgical IIR masks when a surgical mask is required. IIR is a classification referring to the level of protection and performance of the mask according to European standards. Type IIR masks are fluid-resistant and offer high filtration efficiency, making them suitable for use in surgical settings. Despite the reduction of COVID-19 threat, masks continue to be used in many care settings (e.g., perioperative), presenting a challenge for individuals with hearing difficulties in comprehending speech while wearing masks. As mentioned above, several studies have concentrated on comprehending speech amid noisy environments, exploring speech perception in individuals with normal hearing and/or hearing loss. However, in our perspective, a significant aspect has been overlooked in these research efforts: the communication obstacles encountered by individuals with hearing impairments in quiet settings, especially when utilising standard surgical masks. It remains unexplored what advantages could be attained by substituting the standard surgical masks with transparent surgical masks. Additionally, there persists a gap in investigating patients’ preferences, despite the growing emphasis on enhancing effective communication and ensuring patient satisfaction within the healthcare domain.
In this study, we aimed to investigate how the use of transparent surgical masks could enhance communication in clinical settings. Our objective was to assess the impact of both conventional non-transparent surgical masks and transparent surgical masks on acoustics and speech tracking scores for adults wearing a cochlear implant. Additionally, we incorporated the opinions of the participating cochlear implant users regarding the different types of masks to provide a comprehensive understanding of the benefits of transparent masks.
Methods
Subjects
A total of 30 patients with hearing loss participated in this study.
The patients in our study were CI users, but it is important to note that these participants underwent the test in the best aided condition. The participants used either one CI, or had a CI on one side and a hearing aid on the other ear, known as bimodal (n = 10 vs 19). One participant had a cochlear implant on both sides (bilateral). The participants ranged in age from 44 to 90 years (mean age = 69 years, SD = 12.2 years) and were predominantly female (63%). All participants were undergoing treatment for their hearing loss at the Erasmus University Medical Centre and were required to be fluent in Dutch. The Medical Ethics Committee of the Erasmus MC has reviewed the research protocol and has judged that the rules laid down in the Medical Research Involving Human Subjects Act do not apply to this research proposal (MEC-2020-0870). The study was conducted according to the principles of the Declaration of Helsinki (64th WMA, 2013) and the general Data Protection Regulation.
Study design and procedures
A prospective observational design was used for the study. Participants were asked to participate during their regular visit at our outpatient clinic. After informed consent was given, participants completed the tests. The speech tracking test was conducted under three different (randomly ordered) conditions: 1 without mask, 2 with a surgical IIR mask and 3 while wearing a transparent surgical IIR mask known as Smile Shield™ (which is CE | MDR | EN14683 + AC:2019 and EN166:2019 certified) [Citation14]. Speech perception in quiet was performed as part of the normal clinical routine on the same day as the speech tracking test. All participants received a short questionnaire which they were asked to return by mail.
Test materials
Speech perception in quiet
Speech perception in quiet was tested during the normal clinical appointment of the participants. This was tested with the Dutch speech test of the Dutch Society of Audiology (Bosman and Smoorenburg 1995), which consists of phonetically balanced monosyllabic words (consonant-vowel-consonant; CVC) [Citation15]. A clinical audiometer (Decos audiology workstation, version 210.2.6) was used. Participants were placed in front of the loudspeaker at a distance of one metre. The word lists were presented at 65 dB SPL in best-aided condition; participants wore their CI and if a participant used a hearing aid on the other side, it was also worn during the study. The participant was required to repeat the words. This test is purely auditory, without association between the words and without visual input. Testing was performed in a sound-attenuated booth.
Speech tracking test (STT)
During the Speech Tracking Test, a story was orally presented to the participant at a comfortable volume at the best (same) aided condition as described by De Filippo and Scott [Citation16]. The test was conducted by two skilled speech therapists in a quiet room at the hospital. Participants were positioned 1.5 metres away facing the speech therapist, which is in line with our previous research study [Citation6]. The participant was then instructed to repeat each sentence. The sentence was read aloud by the speech therapist up to three times while the time continued to elapse. Any words that were incorrectly repeated or not heard were excluded from the final word count. The number of correctly repeated words leads to the score (number of words correctly repeated per minute). Feedback for incorrect responses was not provided during the STT. Typically, individuals with normal hearing score between 70 to 80 words per minute (W/m) on this particular test. The participants took the STT under three different conditions: without a mask, with a non-transparent surgical mask, and with a transparent surgical mask. If the speech therapist did not wear a surgical mask or used a transparent face mask, the patient could see their mouth movements, allowing for lip reading. The order of the conditions and stories was randomised for all participants. The difference between a CVC test and the STT is that in the CVC test, there is no coherence between the words, while the sentences used in the STT provide more context and insight into daily functioning.
Questionnaire
All participants got a questionnaire which they were asked to fill in at home and return via mail. By incorporating these questions, we sought to gain a more comprehensive understanding of the challenges faced by CI users during the tests. This qualitative data complements the quantitative measurements obtained during the study, allowing for a more nuanced interpretation of the impact of face masks on daily communication for CI users and people with hearing loss. The asked questions were: 1. Did you feel that you could understand better during the test when you could see the lip movements because of the transparent surgical mask? The possible answers were: 1) No, I cannot lip-read; 2) No, I didn’t need lip movements; 3) It might have helped a little; 4) Yes, it made it (much) easier. 2. Imagine you are in a situation where people are wearing face masks, for example, before your surgery. Do you have a preference for a specific type of face mask? Answers: 1) No preference; 2) Preferably a surgical face mask (and why?); 3) Preferably a transparent surgical mask (and why?). 3. When you think back to the period when face masks were mandatory due to Covid-19, would it have helped if people in your surroundings had worn transparent surgical masks? Answers: 1) No, it wouldn’t have made any difference; 2) It would have somewhat improved communication; 3) It could have significantly improved communication. Additionally, there was an option for free text. Twenty-two patients (73%) filled in the questionnaire.
Measurement of acoustic effects
Voice recordings were conducted in a quiet consultation room in the hospital, the same room as the STT. Speech spectra of two speech therapists reading three different stories were measured using a 4189 sound level metre (Brüel & Kjær) to assess the acoustic impact of the masks. The microphone was positioned 1.5 metres in front of the talker and captured frequency responses from 250 Hz to 16 kHz, using a 1/3 octave LZeq measurement. The therapists were asked to use their habitual voice to read three stories wearing a transparent surgical mask. The measurements for the non-transparent surgical face mask and without mask were already conducted for a previous study under the exact circumstances, by the same therapists and were not repeated. [6] The speech therapists ensured a secure and proper fit when wearing the different types of masks.
Data analysis
The data was examined with SPSS (v28) and demonstrated a non-normal distribution for the speech understanding with non-transparent surgical mask. This necessitated the use of non-parametric statistical methods. After using the Friedman test, the Wilcoxon Signed Ranks Test was used to compare listening conditions and Spearman correlation coefficient was used to calculate correlations. Differences in speech tracking scores were determined as the difference between scores with and without a mask or a transparent surgical mask. p-values < 0.05 were considered significant.
Results
Speech perception and impact of masks on speech tracking scores
displays the results of the speech tracking test for three conditions: without a face mask, with a transparent surgical mask, and with a non-transparent surgical mask. Significantly different scores were found across the different conditions (Friedman test: x2(3) = 30,1, p < 0.001). Post hoc comparisons made using the Wilcoxon Signed Ranks Test shows a significant difference between all conditions. Exhibiting a distinction of 20 words per minute in the STT between the non-transparent surgical mask and the transparent surgical mask (median = 46 vs median = 66), the contrast is evident (Z = −4.078, p < .001). The difference between the score with the speech tracking with a transparent surgical mask and without any mask is much smaller (median = 66 vs median =68) but still significant (Z = −2459, p< .014). The difference in STT scores, as expected, is also significant between the test with and without the surgical mask (Z = −2,316, p< .001). The study showed a moderate positive correlation between the routine clinical speech test (CVC-test) and speech tracking scores in the different test conditions (Between CVC-test and surgical mask; Spearman r(28) = [.495], p = [.005]between CVC-test and without mask; Spearman r(28) = [.395], p = [.031], between CVC-test and transparent surgical mask; Spearman r(28) = [.541], p = [.002]. Better CVC scores are associated with better speech-tracking scores for all conditions. We also analysed whether the obtained CVC scores were related to the improvement in speech tracking scores per testing condition, showing a moderate yet non-significant negative correlation upon exchanging the surgical mask for the transparent facemask; Spearman r(28) = [-0.358], p < 0.052. When examining the improvement between the STT with a surgical face mask and the measurement without a face mask, we observe approximately the same correlation it is significant; Spearman r(28) = [-0.398], p < 0.029. In other words, individuals who perform poorly in the CVC test might benefit more from lip reading, though there is considerable variability.
Questionnaire
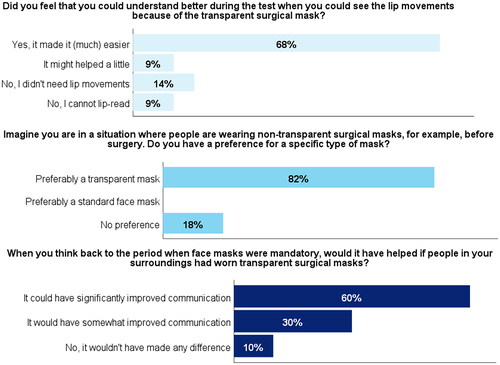
shows the answers from the patients on the questionnaire. Sixty-eight percent of the patients reported that the transparent surgical mask made the test much easier. Eighty-two percent preferred the transparent surgical mask over a non-transparent surgical facemask, the rest of the patients did not have a preference for one or the other mask. Thinking back about the period when facemasks were mandatory, 60% of the patients think using transparent surgical masks would have made a significant difference. An additional 30% indicated that it would have resulted in at least a minor enhancement. In the free-text responses, several patients expressed the view that transparent surgical masks should always be considered as an option or even become the standard in healthcare. Other places mentioned where transparent surgical masks should (or could) be used include hair salons, beauty salons, and dental offices.
Acoustic measurements
When visually comparing the non-transparent surgical mask to the transparent surgical mask, we observed differences in acoustic performance across various frequency ranges. illustrates the average difference in decibels between the transparent surgical mask and non-transparent surgical mask in comparison to the reference situation without a mask (X-axis). It provides a visual representation of the frequencies attenuated by both types of masks, revealing a remarkable reduction in higher frequencies. This observation underscores the substantial impact of both mask types on frequencies that are crucial for speech intelligibility.
Figure 1. Box-whisker plot of the speech tracking score per listening condition. Boxes represent the median (thick horizontal line), lower and upper quartiles (end of boxes), minimum and maximum values (ends of whiskers), outliers (values between 1.5 and 3 times the interquartile range under the third quartile, circles).
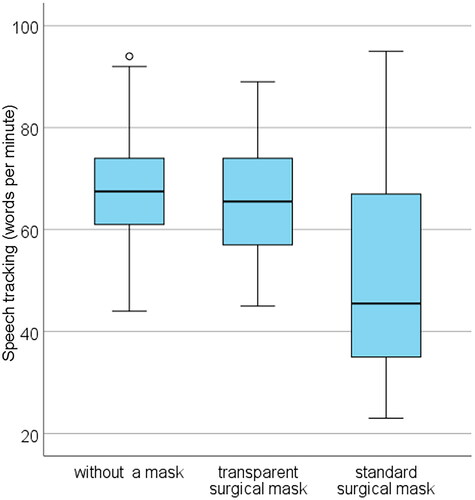
Figure 3. Differences per frequency between 1. without mask and with a transparent surgical mask and 2. without mask and with a standard, non-transparent, surgical mask.
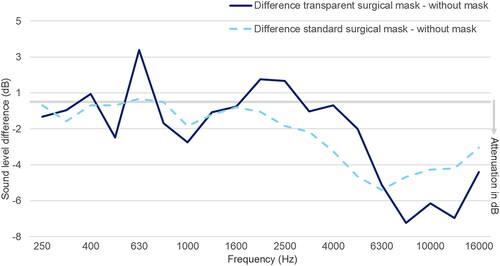
Figure 2. Answers from the patients (n = 22) on the questionnaire for the three different questions.
Discussion
This study investigated the effect of IIR non-transparent surgical masks and transparent surgical masks on speech perception in adult patients using a cochlear implant. The masks have an acoustic impact on the vocal sound. However, this effect seems to be compensated during live speech, as the mouth remains visible. The inability to see facial expressions and read lips significantly impacts speech comprehension.
Acoustic measurements
It is evident that both the transparent surgical mask and non-transparent surgical mask attenuate high frequencies. The reduction in high frequencies is up to 7 dB around 8 kHz for the transparent mask. The findings from our study cannot be completely compared to other investigations into the acoustic impact of transparent surgical masks, as other transparent surgical masks were used [Citation8,Citation11,Citation12,Citation17,Citation18]. The type of mask utilised gives specific amplification or attenuations. For instance, Corey et al. and Maryn et al. used handmade masks [Citation11,Citation12]. Meanwhile, Vos et al. utilised a FDA-cleared and CE-marked mask, but from a different brand [Citation8]. The measurements obtained from this latter brand seem to be more comparable with the results in our study.
Effect of protective equipment on speech tracking scores
We found significantly worse speech tracking scores for the listening situations with non-transparent surgical masks compared to the listening situations with transparent surgical mask and the listening situation without any mask. Small, but significant differences were also found between the transparent surgical mask and the listening situation without a mask. This is in contrast to the study by Vos et al. [Citation8] with CI-users, who found no significant differences between the non-transparent N95 mask and the listening condition without a mask, but found a worse score for speech perception by adding a transparent surgical mask to the condition with a mask. However, no visual speech cues were available in their study. Probably, due to the availability of visual cues in our study, the transparent surgical mask did not affect speech perception in our study. Our results are in line with the study by Atcherson et al. [Citation4] and Thibodeau et al. [Citation7] who found improved speech perception in noise in patients with (suspected) hearing loss when visual input was provided through the use of a transparent surgical mask compared to a conventional mask [Citation4,Citation7]. Thus, transparent surgical masks are likely to distort sound to a greater degree in the high frequencies, but with the availability of visual input, this effect can be well compensated. However, even the transparent surgical mask has already a significant impact on the speech tracking scores, so likely patients with poor auditory functioning need both auditory and visual cues for optimal functioning, even in more quiet environments. In our analysis of the improvement in STT, we found the enhancement to be significant when examining the improvement after removing the surgical mask, enabling lip-reading and preserving natural sound quality. However, this significance fell just short when investigating the improvement after replacing the surgical mask with a transparent one. Our assumption is that with a larger sample size, a significant difference may have been detected. Nonetheless, it is also plausible that the sound quality could still affect intelligibility. Further research is required to delve deeper into this matter.
Questionnaire
From the questionnaire, it is shown that 82% of the participants have a preference for a transparent face mask. The other 18% have no preference, meaning they would also be satisfied when a transparent mask would be used in the clinical setting. This clear preference emphasises the importance of implementing transparent face masks in healthcare settings where communication is essential. Even in quiet situations, there is still a significant preference for the transparent surgical mask. This preference is further supported by the tests we have conducted, showing a big improvement in speech tracking scores when a transparent surgical mask is used. Considering the measurements were taken under optimal conditions, it is expected that the preference for the transparent surgical mask would likely rise if the CI were removed, due to, for instance, a treatment. This anticipation stems from the probable decrease in speech comprehension without the aid of lip-reading cues.
Strengths and limitations
An advantage of our study is that we assessed the influence of masks on live speech interactions in a relatively quiet, consultation room, closely simulating a clinical consultation setting. The used masks are CE certified and can be used in all (sterile) environments. The speech was delivered by speech therapists, offering a less controlled environment than pre-recorded sentences but more closely mirroring real-life situations. As previous studies in the literature primarily rely on pre-recorded speakers, the communication lacks a ‘live’ quality, resulting in the exclusion of numerous cues conveyed through face expression and lip reading. This absence of visual cues has a notable impact expressionson individuals with hearing loss, especially those who heavily depend on visual information. In the near future, more research should be conducted to explore how the introduction of transparent surgical masks in healthcare and perioperative settings can facilitate and enhance communication. As tests had to be carried out during regular clinical consultations, we were unable to include additional test conditions, such as test-retest with the transparent surgical mask, due to time limitations. However, we previously conducted a test-retest of the acoustic analysis in our earlier study and discovered no substantial variations in the sound spectrum [Citation6]. Another reason why the results from this study cannot be directly compared to those from previous studies is the absence of statistical analysis. The aim was to provide a comprehensive overview of the advantages and disadvantages of a transparent face mask, rather than to conduct extensive acoustic analysis, as this has been done frequently before, as noted in the introduction. Additionally, we used live speech, which can inherently vary in sound, making a firm analysis less reliable. Different weather and lighting conditions can affect the visibility of the mouth when wearing a transparent surgical mask. For example, if the lighting is bright or there is glare from the sun, it may be more difficult to see the mouth through the mask. This was once reported by a patient during the test. Additionally, if it is humid, the mask may become wet on the outside, obscuring the mouth. In our study, we did not encounter any fogging on the inside of the transparent window, indicating it does not negatively affect clear view of the mouth. Future research could offer more insights or recommendations on the optimal transparent mask for use in clinical settings.
Conclusion
In this study, through the integration of acoustic measurements, CVC scores, speech tracking scores, and patient preferences, we draw the conclusion that the absence of lip-reading significantly influences speech perception in quiet for patients more than the reduction of high frequencies. Replacing the surgical mask with a transparent face mask in healthcare settings enhances speech intelligibility and better accommodates patients’ needs while ensuring safety with medically approved face masks.
Acknowledgments
We would like to thank all participating CI users and speech therapists Barbara van Oel and Debbie Smit for performing all tests and Geert Geleijnse for supporting the measurements of the acoustic effects of the different surgical masks.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Homans NC, Metselaar RM, Dingemanse JG, et al. Prevalence of age-related hearing loss, including sex differences, in older adults in a large cohort study. Laryngoscope. 2017;127(3):725–730. doi: 10.1002/lary.26150.
- Sönnichsen R, Llorach Tó G, Hochmuth S, et al. How face masks interfere with speech understanding of normal-hearing individuals: vision makes the difference. Otol Neurotol. 2022;43(3):282–288. doi: 10.1097/MAO.0000000000003458.
- Natan MB, Steinfeld Y, Badash S, et al. Association between type of face mask and visual analog scale scores during pain assessment. Pain Manag Nurs. 2022;23(3):370–373. doi: 10.1016/j.pmn.2021.09.005.
- Atcherson SR, Mendel LL, Baltimore WJ, et al. The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. J Am Acad Audiol. 2017;28(1):58–67. doi: 10.3766/jaaa.15151.
- Yi H, Choudhury M, Hicks C. A transparent mask and clear speech benefit speech intelligibility in individuals with hearing loss. J Speech Lang Hear Res. 2023;66(11):4558–4574. doi: 10.1044/2023_JSLHR-22-00636.
- Homans NC, Vroegop JL. The impact of face masks on the communication of adults with hearing loss during COVID-19 in a clinical setting. Int J Audiol. 2022;61(5):365–370. doi: 10.1080/14992027.2021.1952490.
- Thibodeau LM, Thibodeau-Nielsen RB, Tran CMQ, et al. Communicating during COVID-19: the effect of transparent masks for speech recognition in noise. Ear Hear. 2021;42(4):772–781. doi: 10.1097/AUD.0000000000001065.
- Vos TG, Dillon MT, Buss E, et al. Influence of protective face coverings on the speech recognition of cochlear implant patients. Laryngoscope. 2021;131(6):E2038–E2043. doi: 10.1002/lary.29447.
- Flaherty MM, Arzuaga B, Bottalico P. The effects of face masks on speech-in-speech recognition for children and adults. Int J Audiol. 2023;62(11):1014–1021.
- Hong N, Yu W, Xia J, et al. Evaluation of ocular symptoms and tropism of SARS-CoV-2 in patients confirmed with COVID-19. Acta Ophthalmol. 2020;98(5):e649–e655. doi: 10.1111/aos.14445.
- Corey RM, Jones U, Singer AC. Acoustic effects of medical, cloth, and transparent face masks on speech signals. J Acoust Soc Am. 2020;148(4):2371–2375. doi: 10.1121/10.0002279.
- Maryn Y, Wuyts FL, Zarowski A. Are acoustic markers of voice and speech signals affected by nose-and-mouth-covering respiratory protective masks? J Voice. 2021;37(3):468.e1–468.e12. doi: 10.1016/j.jvoice.2021.01.013.
- Cox TJ, Dodgson G, Harris L, et al. Improving the measurement and acoustic performance of transparent face masks and shields. J Acoust Soc Am. 2022;151(5):2931–2944. doi: 10.1121/10.0010384.
- Medimast. Medimast [cited 2022 Jun 21 ]; Available from: https://medimast.nl/data/mediablocks/Smile%20Shield%E2%84%A2%20Productinformatie%202022.2.pdf.
- Bosman AJ, Smoorenburg GF. Intelligibility of Dutch CVC syllables and sentences for listeners with normal hearing and with three types of hearing impairment. Audiology. 1995;34(5):260–284. doi: 10.3109/00206099509071918.
- De Filippo CL, Scott BL. A method for training and evaluating the reception of ongoing speech. J Acoust Soc Am. 1978;63(4):1186–1192. doi: 10.1121/1.381827.
- Atcherson SR, McDowell BR, Howard MP. Acoustic effects of non-transparent and transparent face coverings. J Acoust Soc Am. 2021;149(4):2249–2254. doi: 10.1121/10.0003962.
- Gan D, Hu W, Zhao B. A comparative study of pathological voice based on traditional acoustic characteristics and nonlinear features. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. 2014;31:1149–1154.
