ABSTRACT
Objective: Evaluate the feasibility of implementing cycling-based exergames for children with cerebral palsy (CP) following lower extremity orthopedic surgery and explore its impact on pain and well-being.
Methods: Ten children with CP were recruited; the first five received physiotherapy (comparison) and next five received fifteen exergame sessions over 3 weeks and physiotherapy (case) (NCT0376907). Feasibility indicators evaluated recruitment, questionnaire and exergame completion. Faces Pain Scale-Revised (FPS-R), PROMIS Pediatric Pain Interference Scale (PPIS), and KIDSCREEN-27 were administered. Wilcoxon signed-rank and effect size (r) tests evaluated within-group differences and between-group differences were assessed using Mann–Whitney U tests.
Results: All feasibility indicators were met. Large effects for improved case group pain were identified (FPS-R r = 0.60, PPIS r = 0.58), as well as significant improvement in KIDSCREEN-27 total (U = 0.50, p = .05) and psychological well-being (U = 3.00, p = .01) scores, favoring the case group.
Conclusions: Incorporating pediatric exergames is feasible and demonstrates potential for improving pain and well-being.
Introduction
Cerebral palsy (CP), a group of non-progressive movement and posture disorders that occur due to disturbances of infant or fetal brain development, is the most common physical disability in children with birth prevalence rates of 2 per 1000 live births.Citation1,Citation2 When children with CP grow, they often require lower extremity orthopedic surgery due to joint contractures, bony deformities, or joint instability that negatively impacts their physical function.Citation3 While postoperative rehabilitation, consisting of intense and frequent physiotherapy, is widely regarded as critical for regaining motor function, postoperative pain and muscle spasms are common.Citation4–6
Our team of clinicians and computer scientists developed the Liberi Exergames, designed specifically for children with CP who are ambulatory and functioning at Gross Motor Functional Classification Scale (GMFCS) I–III.Citation7,Citation8 This interactive multiplayer exergame consists of seven different minigames and is powered by pedaling on a stationary bicycle and using game-controllers, allowing children to engage in exercise while playing together. Stationary cycling has demonstrated improvements in psychosocial health, emotional well-being, and gross motor function for nonoperative ambulatory children with CP as well as improvements in physical function, pain, and activities of daily living for adults following total hip replacement.Citation9,Citation10 Previous research has shown that cycling on exergames at a moderately elevated heart rate (HR) for at least 60 minutes per week is doable and led to improvements in cardiovascular fitness for youth with CP.Citation7 A target heart rate (tHR) for children with CP can be estimated at 116 beats per minute (bpm) or higher representing 60% of an HRmax of 194 bpm.Citation11 Sixty minutes per week at tHR may promote health-related fitness for children and adults with CP, in accordance with the American College of Sports Medicine recommendations.Citation12 Post-operatively, individuals spend considerable time in bed or sitting (sedentary behavior) and can become de-conditioned. Opportunities for fun-based cardiovascular fitness may help promote recovery and well-being.
It is currently unknown whether it is feasible to implement Liberi Exergames into the postoperative rehabilitation setting for children with CP, and what the impact will be on postoperative pain, well-being, and cardiovascular fitness. Evaluating the feasibility of utilizing the Liberi Exergames as a rehabilitation modality may lead to the development of new, fun, and innovative ways to relieve pain, improve well-being, and achieve tHR. Thus, this study’s objectives were 1) to assess the feasibility of implementing exergames for children with CP of GMFCS I–III receiving inpatient rehabilitation for lower extremity orthopedic surgery, and 2) explore the impact of the exergames on pain, well-being, and achieving tHR.
Materials and Methods
Participants
Participants were recruited from a pediatric rehabilitation hospital’s inpatient unit. Inclusion criteria included: children with CP admitted for inpatient rehabilitation following lower extremity orthopedic surgery, 7–18 years of age, functioning preoperatively at GMFCS I–III, ability to operate a game-controller and pedal on the Liberi Exergames, ability to self-report on the Faces Pain Scale-Revised (FPS-R), and weight bearing as tolerated.Citation7,Citation13,Citation14 Exclusion criteria included health conditions (e.g. exercise-induced asthma, uncontrolled seizures) that prevented cycling. This study is registered in the ClinicalTrials.gov database (NCT03769077) and ethics approval was granted by local ethics boards. Informed consent from participants was obtained.
Study Design
A case-comparison design was utilized with consecutive recruitment of ten participants into two groups: the first five received standard physiotherapy (“comparison group”) and the next five received five exergame sessions per week, 30 minutes per session, for 3 weeks in addition to standard physiotherapy (“case group”).
Physiotherapy
All participants received standard physiotherapy consisting of weekday sessions working on range of motion, posture and balance exercises, transfers, and re-introduction of weight-bearing activities. Cycling on a MOTOmed® movement therapy device, adaptive tricycle, or stationary bicycle was done for 5 to 10 min per physiotherapy session, one to five times per week.
Exergame Sessions
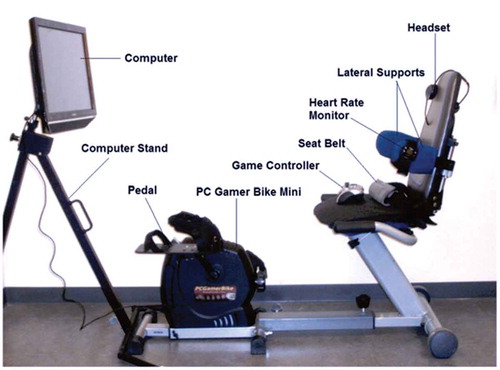
The Liberi Exergames () are played using a standard game controller, a 24-inch all-in-one computer and specialized seat equipped with a seatbelt and lateral supports connected to a stationary bicycle. Heart rate monitors were worn by participants and cadence sensors on the bicycle recorded pedaling speed. During the first session of every week, bicycle leg length and seat were adjusted according to each participant’s height, leg length, and ability to comfortably flex and extend the knees for a full cycle rotation. During the first session of every week, gameplay difficulty level was set relative to each participant’s cycling ability by calibrating the participant’s average cadence during a racing minigame while playing against bots (AI-controlled opponents). The playing level for the bots was set at 70–80% of the participant’s average racing cadence, giving participants difficult but achievable challenges. Case group participants played with other participants, recreational therapy staff or ‘bots.’ Exergame sessions were monitored by recreation therapy, nursing, and research staff.
Outcome Measures
The primary outcome evaluated feasibility based on process, resource, and management indicators.Citation15 The process indicator evaluated recruitment rate and was defined a priori as being met if more than 40% of eligible potential participants enrolled. The resource indicator evaluated data collection and was defined as being met if 80% of participants completed the FPS-R at baseline and at the end of the study period.Citation14 The management indicator evaluated adherence to exergame sessions and was defined as being met if each case group participant completed at least 12/15 exergame sessions.
The two pain questionnaires used were the FPS-R, evaluating self-reported intensity of pain, and the Patient-Reported Outcome Measurement Information System Pediatric Pain Interference (PROMIS-PI), evaluating the extent to which pain interfered with activities of daily living.Citation14,Citation16 The FPS-R consists of six faces portraying expressions from “no pain” (scored 0) to “very much pain” (scored 10).Citation14 Participants were asked to point to the face that indicated the intensity of pain he/she felt over the last seven days. Scores ranged from 0 to 10 and higher scores indicated greater pain. The FPS-R was administered to both groups at baseline and at the end of each week for the 3-week study period.Citation14 The PROMIS-PI consists of a self-reported 8-item questionnaire and evaluated pain interference.Citation16 Items were scored 1–5, summed to obtain total raw scores, then converted to T-scores. Higher scores indicated higher pain interference. The PROMIS-PI was administered to both groups at baseline and at the end of each week for the 3-week study period.Citation16
The KIDSCREEN-27, a standardized health-related quality of life questionnaire, examined five dimensions of well-being including Physical Well-Being, Psychological Well-Being, Autonomy and Parents, Peers and Social Support, and School and Environment, with items scored 1–5 and a total raw score calculated as the sum of all domain scores.Citation17 Physical well-being and psychological well-being domain T-scores (only available for these domains) were also reported on a scale with a mean of 50 and a standard deviation of 10. Higher values indicated higher well-being for raw and T-scores. The KIDSCREEN-27 was administered to both groups at baseline and at the end of the 3-week study period.Citation17
Gameplay data including HR and time spent at tHR were recorded. Sixty minutes per week at an HR of at least 116 beats per minute (bpm) was set as the tHR.Citation11,Citation12
Case group participants completed semi-structured feedback interviews following the last exergame session. Interviews explored case group experiences through open-ended questions and additional prompts if needed. Example questions included asking participants what their experience was playing the exergames, how the exergames made their legs feel, and if the exergames influenced physiotherapy. Interviews were audio-recorded and transcribed.
Statistical Analyses
Descriptive statistics characterized outcomes and demographic parameters. Feasibility indicators were evaluated based on a priori criteria and were considered “successful” or “unsuccessful.” For consistency in the KIDSCREEN-27 and PROMIS-PI, if answers were reported not applicable, the lowest score, “1” for was inputted to allow for computation of total scores.Citation16,Citation17 For FPS-R, PROMIS-PI, and KIDSCREEN-27 total, psychological, and physical well-being scores, Wilcoxon signed-rank and effect size r tests were employed to evaluate changes from baseline to the end of week three within the case and comparison groups.Citation18 Mann–Whitney U and effect size r tests were employed to compare the baseline to end of week three changes between the case and comparison groups.Citation18 Statistical significance was indicated with p ≤ 0.05 and r values of 0.5, 0.3, and 0.1 indicated large, medium, and small effect sizes, respectively.Citation19 Interview responses were assessed descriptively and summarized.
Results
Participant Demographics
Ten children were recruited. Participant characteristics are outlined in . Orthopedic surgeries included 1) femur and tibia derotational osteotomies; 2) hamstring (semitendinosus, semimembranosus, gracilis), and gastrocnemius muscle lengthening procedures; and 3) patella tendon shortenings and tibialis anterior tendon transfer procedures.
Table 1. Demographic information
Feasibility Indicators
Process Indicator
Ten potential participants were identified through the participants’ circle of care and the hospital’s centralized research database.Citation15 Of the ten approached, ten (100%) agreed to participate. Two additional families were approached and had agreed to participate but were excluded due to early discharge and inability to participate in the full study period. As the success criterion for recruitment was set at enrolling more than 40% of potential participants, the process indicator was deemed “successful.”
Resource Indicator
All participants (100%) completed the FPS-R at baseline and at the end of the study.Citation14 The resource indicator, assessing questionnaire completion, was deemed “successful”.Citation14
Management Indicator
All case group participants completed at least 12 of their respective 15 total exergame sessions.Citation15 Two participants missed two sessions each, one participant missed one session, and two participants did not miss any sessions. The average number of completed sessions was 14.2 ± 0.8 sessions. Reasons for missed sessions included a family event, personal commitments, and inability to cycle due to knee stiffness. As all participants completed at least 12/15 exergame sessions, the management indicator, assessing adherence to exergame sessions, was deemed “successful.”
Adverse Events
One case group participant was unable to play the first two exergame sessions due to left knee discomfort and inability to complete a full cycle rotation on the bicycle. The participant spent the sessions progressively pedaling with increasing degrees of rotation. No other adverse events occurred.
Pain and Well-being
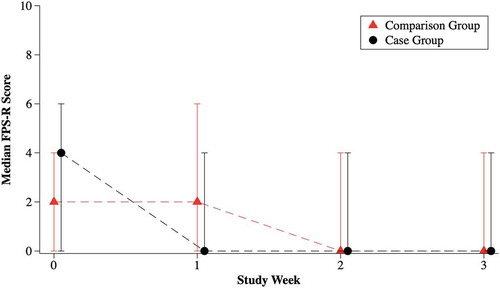
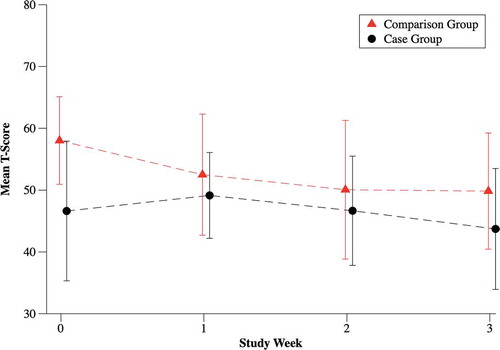
For the FPS-R, one comparison and two case group participants experienced no pain, one case group participant experienced no change in pain, and two comparison and two case group participants experienced decreasing pain.Citation14 Two comparison group and no case group participants experienced increasing pain. Median FPS-R and mean total PROMIS-PI scores are presented in .Citation14,Citation16 KIDSCREEN-27 scores are presented in .Citation17 Results of the Wilcoxon signed rank, Mann–Whitney U and r effect sizes (as absolute values) are presented in .Citation17
Table 2. KIDSCREEN-27 scores
Table 3. Pain and well-being results
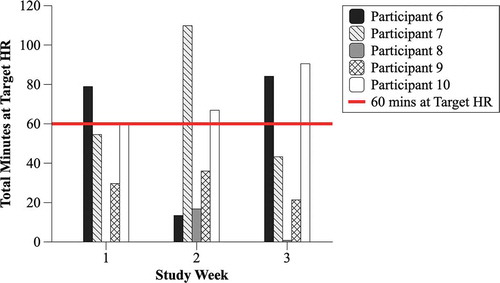
Time at Target HR
Total time spent at tHR for the case group participants per week is presented in . Average time spent at tHR for all case group participants was 44.7 ± 30.5 minutes for week one, 48.6 ± 40.3 minutes for week two, and 48.0 ± 39.0 minutes for week three.
Semi-Structured Interviews
Case group participants were unanimous that playing the exergames was enjoyable and fun. Of the five case group participants, three expressed that the exergames reduced pain, while two commented that there was no difference because no pain was experienced. Four case group participants expressed that the exergames helped with their activity and physiotherapy by helping them bend and move their knees more, made stretching less painful and easier, increased stamina, helped with mobility, and allowed them to stretch their legs out faster. One commented that no difference in activity or physiotherapy was observed. On average, when asked to rate how fun the exergames were on a scale of zero (least fun they’ve ever had) to ten (most fun they’ve ever had), the mean score was 8 ± 1.5. All case group participants said that if they could go back in time, they would play the exergames again.
Discussion
To our knowledge, this is the first study to evaluate the feasibility of incorporating cycling-based exergames for children with CP following lower extremity orthopedic surgery and to explore its impact on pain, well-being, and target HR. All criteria in the feasibility framework were successfully met. The process indicator, evaluating recruitment, was met with a 100% recruitment rate, demonstrating high motivation and enthusiasm by participants to participate in this research study.Citation15 This supports the potential for developing larger studies, as failure to reach a sufficient sample size is a key barrier in conducting randomized controlled trials (RCTs). Resource and management indicators, evaluating questionnaire and exergame completion, were also met.Citation15 Both exergame sessions and questionnaires were completed after school and before dinnertime, a time that participants had no other commitments. The completion of at least 12 exergame sessions for each case group participant indicates that children with CP are able to cycle on an exergame station for 30 minutes following lower extremity orthopedic surgery. This promising finding demonstrates that implementing exergames for pediatric orthopedic rehabilitation is both feasible and does not increase leg or joint pain.
Children in both the exergame and the comparison groups had a decrease in pain as measured by the FPS-R score over the 3-week study period that met the minimally clinically important difference of two points.Citation20 When reviewing individual participant responses on the FPS-R, two comparison group participants experienced increasing pain over the study period. In contrast, no individual participants in the exergame group experienced increasing pain. It is reassuring that the cycling in the exergame group did not trigger pain in children with CP in the rehabilitation period following orthopedic surgery. Indeed, when within-group changes in the exergame group were assessed, a large effect size (r = 0.60) for reduction in pain as measured by the FPS-R was found, in contrast to a small effect size reported in the comparison group (r = 0.17). Children in both the exergame and comparison groups also had a decrease in pain interference, as measured by the PROMIS-PI, over the 3-week study period that exceeded the minimal clinically important difference of three points. Both groups had large effects in reduction in pain interference from baseline to week three, as measured by the PROMIS-PI. A larger sample size will be required in future studies to assess differences in rates of pain reduction and/or interference between the exergame and physiotherapy group versus physiotherapy alone.
Children in the exergame group had significant improvement in overall and psychological well-being compared to children in the comparison group, and also reported a large effect size for physical well-being improvement over the 3 weeks. Opportunities for cardiovascular physical activity may contribute to improved well-being, as previous research has established a positive relationship between physical fitness and well-being in children with CP following exercise programs.Citation21–23 In addition, the exergames were perceived as enjoyable which may contribute to the improved well-being seen in the exergame group as compared to the comparison group.
The exergame case group’s average time spent at tHR approached but did not reach 60 minutes per week, ranging from 44 to 48 minutes. Three out of the five case group participants were able to reach target HR at least once out of the 3 weeks. To enhance the time spent in target HR, consideration could be given for adding a sixth exergame session per week.
There are limitations to this study that should be highlighted. First, there is an imbalance in opposite directions between the comparison and case groups baseline scores for the FPS-R and PROMIS-PI. A potential reason for this may be that the two questionnaires explore different aspects of pain. The FPS-R examines self-reported pain intensity while the PROMIS-PI examines pain interference on activities of daily living. Additionally, a small sample size and lack of randomization may also impact the comparability of the groups at baseline, and limits power for statistical testing and generalizability. Another limitation is that all participants received varying amounts of postoperative cycling through physiotherapy.
Conclusion
This study supports the feasibility of implementing cycling-based exergames for children with CP following lower extremity orthopedic surgery. Cycling on the exergames demonstrates the potential to improve pain and pain interference over the 3 weeks. Large positive changes in overall and psychological well-being were also identified in favor of cycling on the exergames compared to children receiving standard physiotherapy alone. While tHR was not achieved for all case group participants, moderate elevations in HR were achievable. The inclusion of additional exergame sessions in future studies may allow for further HR elevation.
Future studies should consider an appropriately powered RCT to optimize recruitment of participants while also balancing the varying characteristics of age, GMFCS, baseline pain scores, and time of enrollment into the study following surgery. Given the improvement in overall and psychological well-being for children who were exergaming, future studies could consider positioning subjective well-being as the primary outcome of the RCT. This study provides the foundation for the development of larger clinical trials implementing cycling-based exergames for children with CP following lower extremity orthopedic surgery.
Declaration of Interest
The authors report no conflict of interest.
Acknowledgments
The authors thank the participants and families who participated in this study. This research was supported by Holland Bloorview Kids Rehabilitation Hospital’s Centre for Leadership program, the Ontario Brain Institute and A.C. received Canadian Institutes of Health Research’s Canadian Graduate Scholarship (CIHR-CGS M) award. The funders have no involvement in study design, data collection, data analysis, and article preparation or publication decisions. D.F., N.G., and L.S. have intellectual property interest surrounding the Liberi Exergames.
Additional information
Funding
References
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacbonsson B. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol. 2007;109:8–14. [accessed 2018 Nov 19]. http://www.ncbi.nlm.nih.gov/pubmed/17370477.
- Australian Cerebral Palsy Register. Australian cerebral palsy register report. 2018. https://cpregister.com/wp-content/uploads/2019/02/Report-of-the-Australian-Cerebral-Palsy-Register-Birth-Years-1995-2012.pdf.
- Narayanan UG. Management of children with ambulatory cerebral palsy: an evidence-based review. J Pediatr Orthop. 2012;32:172–81. doi:10.1097/BPO.0b013e31825eb2a6.
- Jefferson RJ. The treatment of gait problems in cerebral palsy. Arch Dis Child. 2005. doi:10.1136/adc.2004.060491.
- Shrader MW, Jones J, Falk MN, White GR, Burk DR, Lee SS. Hip reconstruction is more painful than spine fusion in children with cerebral palsy. J Child Orthop. 2015;9:221–25. doi:10.1007/s11832-015-0656-x.
- Mcginley JL, Dobson F, Ganeshalingam R, Shore BJ, Rutz E, Kerr Graham H. Single-event multilevel surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2011;54:117–28. doi:10.1111/j.1469-8749.2011.04143.x.
- Knights S, Graham N, Switzer L, Hernandez H, Ye Z, Findlay B, Xie WY, Wright V, Fehlings D. An innovative cycling exergame to promote cardiovascular fitness in youth with cerebral palsy. Dev Neurorehabil. 2014;19(2):135–40. doi:10.3109/17518423.2014.923056.
- MacIntosh A, Switzer L, Hwang S, Schneider ALJ, Clarke D, Graham TCCN, Fehlings DL. Ability-based balancing using the gross motor function measure in exergaming for youth with cerebral palsy. Games Health J. 2017;6(6):379–85. doi:10.1089/g4h.2017.0053.
- Demuth SK, Loretta KM, Fowler EG. The PEDALS stationary cycling intervention and health-related quality of life in children with cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2012;54(7):654–61. doi:10.1111/j.1469-8749.2012.04321.
- Liebs TR, Herzberg W, Ruther W, Haasters J, Russlies M, Hassenpflug J. Ergometer cycling after hip or knee replacement surgery: a randomized controlled trial. The Journal of Bone and Joint Surgery-American Volume. 2010;92(4):814–22. doi:10.2106/JBJS.H.01359.
- Verschuren O, Maltais DB, Takken T. The 220-age equation does not predict maximum heart rate in children and adolescents. Dev Med Child Neurol. 2011;53(9):861–64. doi:10.1111/j.1469-8749.2011.03989.x.
- American College of Sports Medicine. Health-related fitness for children and adults with cerebral palsy. Indianapolis (IN). 2007. http://www.acsm.org/docs/current-com-ments/health-relatedfitnessforcawithcp.pdf.
- MacIntosh A, Switzer L, Hernandez H, Hwang S, Schneider ALJ, Moran D, Graham TCN, Fehlings DL. Balancing for gross motor ability in exergaming between youth with cerebral palsy at gross motor function classification system levels ii and III. Games for Health Journal. 2017;6(2):104–10. doi:10.1089/g4h.2016.0073.
- Hicks CL, Von Baeyer CL, Spafford PA, Van Korlaar I, Goodenough B. The faces pain scale – revised: toward a common metric in pediatric pain measurement. Pain. 2001;93(2):173–83. www.elsevier.nl/locate/pain.
- Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, Robson R, Thabane M, Giangregorio L, Goldsmith CH, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1–10. http://www.nsf.gov/pubs/2005/nsf0531/nsf0531_6.pdf.
- Varni JW, Stucky BD, Thissen D, DeWitt EM, Irwin DE, Lai J-S, Yeatts K, DeWalt DA. PROMIS Pediatric Pain Interference Scale: an item response theory analysis of the pediatric pain item bank. The Journal of Pain. 2010;11(11):1109–19. doi:10.1016/j.jpain.2010.02.005.
- Ravens-Sieberer U, Herdman M, Devine J, Otto C, Bullinger M, Rose M, Klasen F. The European KIDSCREEN approach to measure quality of life and well-being in children: development, current application, and future advances. Qual Life Res. 2014;23(3):791–803. doi:10.1007/s11136-013-0428-3.
- Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2–18. doi:10.1037/a0024338.
- Coolican H. Research methods and statistics in psychology. 2017. Taylor and Francis. doi:10.4324/9780203769836.
- Tsze DS, Hirschfeld G, von Baeyer CL, Suarez LE, Dayan PS. Changes in pain score associated with clinically meaningful outcomes in children with acute pain. Acad Emerg Med. 2019;26(9):1002–13. doi:10.1111/acem.13683.
- Dodd KJ, Taylor NF, Graham HK. Strength training can have unexpected effects on the self-concept of children with cerebral palsy. Pediatr Phys Ther. 2004. doi:10.1097/01.PEP.0000127566.90996.50.
- Darrah J, Wessel J, Nearingburg P, O’Connor M. Evaluation of a community fitness program for adolescents with cerebral palsy. Pediatr Phys Ther. 1999. doi:10.1097/00001577-199901110-00004.
- Verschuren O, Ketelaar M, Gorter JW, Helders PJM, Uiterwaal CSPM, Takken T. Exercise training program in children and adolescents with cerebral palsy: A randomized controlled trial. Arch Pediatr Adolesc Med. 2007. doi:10.1001/archpedi.161.11.1075.