ABSTRACT
This paper describes the software design/development process leading to an improved computerized clinical/management solution—RSIPA (2016 version)—integrating care pathways (CPs) specifically designed to meet the needs of frail and disabled older adults in home care. The development methodology used Soft Systems Methodology (SSM) for the initial system design and participatory design (PD) to involve stakeholders and end users, along with AGILE SCRUM methodology to provide rapid iterations in adapting to new requests. Given scarce project resources, we opted to combine methodologies to efficiently deliver a fully functional system for three of the five CP clinical phases. The development methodology aggregated assessment-based data to identify risk factors and assist in needs prioritization leading to care plans and addressed in the current system. The new Quebec RSIPA solution incorporating CCPs is a promising example of technologies that support person-centered care, clinical and management processes, and proactive care in home-care settings.
Introduction
Integrated service networks (ISNs) have gradually been established for older people in the province of Quebec (Canada).Citation1,Citation2 Despite many improvements in how our health-care system is organized, some gaps associated with assessing, planning, and delivering health care and social services that reflect personal values and preferences have emerged.Citation3–7 To resolve this situation, we have conducted significant research leading to content development for care pathways (CPs) specifically designed to meet the needs of frail and disabled older adults.Citation8 These CPs consist of a home-based comprehensive assessment and long-term care management process supported by an interdisciplinary team. They aim at promoting fair access for persons with complex long-term needs and at providing support and proactive care by identifying and preventing risks such as falls. CPs are person-centered, promoting independence in daily life for community-dwelling individuals. As multiple home-care providers across various disciplines work as a team in communicating and providing care, another goal was to increase the quality of interprofessional responses to a person’s overall needs based on their clinical profiles within a context of ISNs. The clinical process consists of five phases: (1) comprehensive home assessment of older adults and their caregivers carried out by a healthcare professional (usually a nurse, social worker, or other professionals with appropriate training); (2) data-collection summary and goal identification based on a patient-centered process; (3) planning of actions/interventions appropriate to the clinical situation and expectations of the person and caregivers; (4) coordination, delivery, and follow-up; and (5) identification of variances/gaps as well as review and adjustment of plans, as required. CPs constitute a core decision-support system providing guidance on appropriate actions for the specific clinical circumstances reflected by assessment and overview data.
Based on finding in the literature,Citation9–12 the research team quickly recognized that incorporating CPs into a user-friendly, highly effective computerized system providing clinical teams with feedback via real-time data processing was essential to successful CP implementation.Citation8 In our case, this could support: (1) the creation, storage, aggregation, and exchange of valid health data supporting the provision and local coordination of care and services; (2) the real-time consultation and updating of information; (3) the accessibility of information from multiple integrated sources; and (4) optimizing the time of healthcare professionals with real-time access to data and decision support.
In 2012, an initial electronic prototype incorporating the first two CP phases (assessment and summary) were developed in a clinical system (Dossier Clinique Informatisé or DCI) through close collaboration between a health and social services center (Center de santé et services sociaux or CSSS) and the research team at the Sherbrooke Research Center on Aging (Center de Recherche sur le Vieillissement or CdRV). Since 2014, the first three CP phases have been integrated into another system through collaboration between the provincial Ministry of Health and Social Services (Ministère de la Santé et des Services sociaux or MSSS), the Sherbrooke Center for Health Expertise (Center d’expertise en santé de Sherbrooke or CESS), developers with the information-technology branch of the ministry (Direction Générale des Technologies de l’Information du MSSS or DGTI/MSSS), and the research team. The second version of the prototype was released as a new tool available to end users in the current version of the RISPA clinical and management computerized solution (French acronym: RSIPA for Réseau de services intégrés pour les personnes adultes), already in use in all home health care and social services in the province of Quebec. summarizes the chronology of CCP development and deployment.
Implementing such a complex clinical and management system requires both a rigorous software engineering process and the involvement of users as diverse as researchers, managers, and healthcare professionals. Designing and developing computerized health systems without engaging users as partners in the process often result in major system failures not always related to flawed technology but rather to lack of consideration of clinical workflow and human factors.Citation13,Citation14 User involvement into the development, testing and evaluation process of systems make these systems more suitable to user needs and desires/expectations.Citation15–18 Considering user experience in the design/development process is thereby important for technology acceptance and enhancing its usefulness.Citation19–23
Various software methodologies have been developed over the years, such as the modified waterfall modelCitation24 and the AGILE SCRUM method applied to software-development.Citation25 Each has its own advantages and limitations.Citation26,Citation27 Selecting the appropriate methodology for a specific project is crucial to its success, with timeframe and resources often being the determinants. While not always easy,Citation28,Citation29 combining methodologies can help overcome the limitations of a specific method.
This paper describes the software design and development process culminating in an improved RSIPA solution (2016 version) based on the 2012 prototype integrating these CPs, using combined software-development methodologies. It also presents some advantages and limitations of this process in the context of home care.
Materials and methods
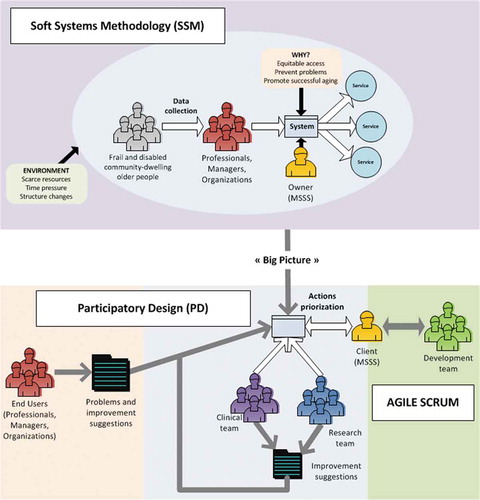
Multiple software-development methodologies were used to design a system that addressed the various clinical requirements. AGILE methodology using SCRUM applied to software development is increasingly gaining recognition.Citation30 It provides many advantages such as rapid iterations with new features being available to end users in each sprint and the ability to adapt to new requests. Basically, the methodology uses an incremental, iterative work cadence – known as sprints of about four to six weeks – to respond to required modifications. DGTI/MSSS (project development team) was quite familiar with the method. Using this approach for a large, complex project can be challenging in terms of keeping the project scope in focus and not losing innovation because of time constraints.Citation31 Since AGILE methodology doesn’t require a careful design and CCP implementation requires a multidisciplinary team, Soft Systems Methodology (SSM)Citation32 was used for the initial system design; participatory design (PD)Citation33 was added to the traditional AGILE-SCRUM methodology to involve stakeholders and end users.
summarizes the CCPs design pattern, combining SSM, PD, and AGILE SCRUM.
SSM is basically best at modeling complex situations to converge toward a coherent problem definition, which is then used to design a system meeting the identified needs.Citation32 When applied to CP design, it provided a global model of the software. While AGILE doesn’t require such modeling beforehand, SSM yields a global plan, providing a project overview before AGILE is applied. This approach has been used, offering promising avenues for improving the AGILE process in some cases.Citation34 The research team led SSM modeling and integrated inputs from end users of the system under development (healthcare professionals, managers, organizations). SSM process was used only in the initial phase of the development process.
In contrast, the PD approach aims at involving project stakeholders and end users in the process. Typically, AGILE involves a client and developers. The idea behind a larger participatory approach in CP development was to achieve a final solution that would satisfy the needs of all participants. Combining AGILE and PD has already proven to be an effective approach.Citation29 PD has also been used successfully in health-related projects,Citation35 in particular in the development of an electronic “Individual Care Plan” or e-ICP.Citation22 The PD approach provided regular feedback for the AGILE SCRUM process. A team of clinical experts provided feedback and input on CCP clinical validity and the user-friendly interface as the computerization process was ongoing. The research team was also involved in PD, providing scientific support and ensuring that CCPs conformed to the state-of-the-art. Both teams suggested improvements that were used to prioritize development and define AGILE sprints. End users constituted another important group involved in PD, serving as beta sites for the new RSIPA system, including CPs. End users had released versions of the system and provided feedback on its usability, features, information display, problems encountered, and improvements.
End users came from the three beta sites located across Quebec. The beta phase started in 2016; provincial deployment ran from the end of 2018 to the beginning of 2019.
The SSM model as well as feedback from end users, the clinical and research teams, and CESS were considered by the development team’s client: MSSS. Having a model in which the client is not the system end user is typical in AGILE software development.Citation36 Group outputs were combined and available resources weighed (time, human, and financial) to prioritize actions, which were sent to the development team for evaluation and integration into future sprints. The development team provided feedback to the client as well as to the clinical and research teams as sketches of proposed feature implementation and software releases.
The study was approved by the Research-Ethics Committee (Comité d’éthique à la recherche – CÉR du CIUSSS de l’Estrie – CHUS).
Results
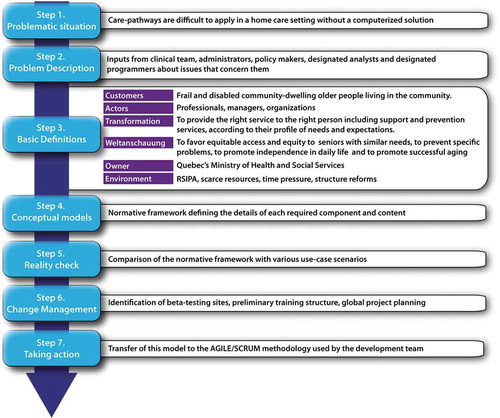
Application of soft systems methodology: the model
presents the various SSM steps applied to CCPs. In developing the initial electronic prototype, the research team partnered with a clinical team, administrators, policy makers, designated analysts, and programmers. We tried to take into consideration their expectations to better understand the system-development context. The purpose was to achieve a consensus on what an information system (IS) integrating CPs should be to ensure that it would support the day-to-day practices of service providers, while facilitating managers’ access to data useful in decision-making. The normative framework was a main outcome of the SSM process. The framework consists of a reference document supporting the entry of standardized data into a computerized solution as well as its use for informational purposes. The results from the last step of the SSM model were used as inputs for the next steps when we started our partnership with MSSS to design the improved 2016 version of RSIPA integrating CPs.
Use of PD and Agile methods
The process for developing the main features (lasting a year) included regular, one-hour telephone meetings every two weeks and a three-hour face-to-face meeting every 4–6 weeks between the end users and the Ministry’s development team in addition to regular individual consultations with healthcare professionals from clinical settings. During each meeting, the research team had the opportunity to explain its vision to ensure that the expected CP features were preserved. Each design/development phase was built on the preceding one, requiring the research team to provide feedback on a series of models and prototypes. A decision log kept for each meeting recorded the required system changes or additions. The discussion focused on functional features (i.e., signaling gaps); content requirements (i.e., text or visual format coupled to the five CP phases); interaction design (i.e., user interaction with the system during the decision-making process); information architecture and navigation design (i.e., information organization to facilitate workflow during assessment, planning, and monitoring); and interface design (i.e., display organization to facilitate identification of sections and subsections).Citation37 MSSS organized testing sessions to collect similar inputs from expert trainers. In addition, terminology adjustments were made with a committee of older people. MSSS then accepted or rejected all these discussions and feedback, and transferred the discussions to the backlog of the AGILE SCRUM development team.
RSIPA system 2016 version including CPs
The improved 2016 version of the RSIPA system including CPs was developed to support clinical and management processes in home healthcare settings and across the continuum of services with the following design specifications. The system is basically a secured web-based platform, available online to the healthcare professionals using a web browser, either from home with an older person or from their workplace. Professionals can prepare their visits at home and access their workload directly in the system. Appropriate backup systems have been put into place. Access management is simple: for a given home-care client, a professional can either be a reader (read only) or author (full access). The system is available in French and English.
Clinical process
When collecting the required data for home care as part of the CP process, a healthcare professional begins by visiting the older adult’s living setting. Family or caregivers are encouraged to join in, especially when older persons have difficulties expressing themselves. The process requires close partnership between the person receiving care and the healthcare professional. The system’s user interface presents information in a way that allows the professional to share the computer screen with the person throughout the various phases of the clinical process. This gets the person involved in each step and culminates in a consensual home-care assessment and plan.
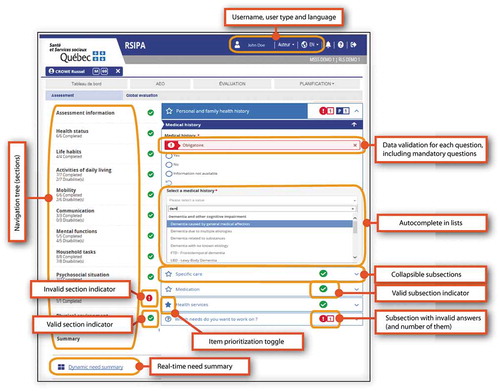
Phase 1: Comprehensive assessment
The first phase consists of an overall assessment questionnaire, the Multiclientele Assessment Tool (French acronym: OEMC for Outil d’évaluation multiclientèle),Citation38 consisting of various sections, including: (1) health status; (2) lifestyle; (3) functional autonomy (SMAF)Citation39; (4) psychosocial situation (including Social-SMAF)Citation40,Citation41; (5) economic conditions; and (6) physical environment. OEMC is traditionally a hardcopy assessment, but computerization has allowed the addition of improved, standardized content such as additional questions enabling professionals to better understand the person’s situation. While OEMC now has 163 mandatory questions, it provides for more than 700 questions related to all sections, which allows assessors to refine a situation or specify more details.
All this information is captured through the online system. shows the user interface for the process and describes the various features in the solution. A navigation tree simplifies navigation through the various sections (left side). A dynamic summary of each identified need is provided to remind the healthcare professional to support discussion with the person as the assessment progresses. The system includes various features helping with data entry such as data-validation indicators (for sections, subsections and specific questions), autocomplete features (for example, when using lists as inputs), unit converters (for example, from feet to meters), and online help. The system lets the person to provide input in the evaluation process. This involves a feature that – with the assistance of her healthcare professional – allows the person to determine if a specific element is important or if he or she wishes to work on that element (identified with stars in the user interface).
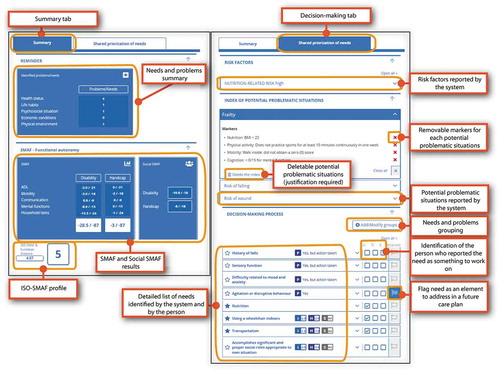
Phase 2: Data-collection summary and goals identification based on a patient-centered process
Each comprehensive assessment produces a module concisely summarizing the person’s care needs, which serve as the basis for decision-making with the person and his or her caregiver. presents the user interface and features available in this phase. A summary section identifies the people involved in the process (older adult, healthcare professional, caregivers) with the results calculated by OEMC (such as the SMAF scores and Iso-SMAF profiles).Citation42 A section on dynamic needs prioritization serves as a worksheet to identify goals with the person.
To help the healthcare professional focus on potentially problematic situations (such as frailty or fall risks) and identified risk factors (such as malnutrition), several algorithms have been developed based on the global assessment. They are used to process OEMC content and generate warnings about problems. The warnings can be expanded to display specific markers, as needed, and can be dismissed by the healthcare professional if the situation doesn’t apply, as long as justification is provided.
The system supports the prioritization process by displaying items for identified problems or items the user wants to work on. The professional determines the person’s priority needs. The professional can discuss the specific element, add any of the person’s other expectations, categorize the elements into custom groups and identify which elements must be retained (addressed in a future home-care plan), and specify whether the user (U), relative (R), or evaluator (E) retained the element.
Phase 3: Planning of appropriate actions/interventions for the clinical situation and expectations of the person and caregivers
After the needs have been prioritized, a care plan is created. Plans range from a general plan of services to disciplinary plans. They include actions required to fulfill the person’s needs according to their preferences, while taking into account clinical characteristics and identifying relevant resources. While this process predates CCPs, better integration was achieved, allowing healthcare professionals to directly transfer the needs prioritized in phase 2 to a working care plan. Professionals can use this feature to select the type of plan required, objectives to work on, and the resources needed (care providers) based on the person’s and caregivers’ needs.
Phase 4: Implementation of the plan, coordination, delivery, and monitoring of responses to the plan
Once care specific to the person’s needs has been determined, feedback monitoring must be implemented to assess plan compliance and provide for dynamic adjustments in any subsequent phases. This requires access to the person’s various healthcare records in order to gain a complete picture of what was planned, what was done, when, and where.
The current implementation of CCPs does not fully feature this phase. While information about the various plans is available to professionals, an external system (I-CLSC) is still used to monitor plan scheduling and execution, thereby limiting overview, such as having a common dashboard and interface. This is, however, a planned feature as it is an essential component in providing unified and supportive CCPs.
Phase 5: Identification of variances/gaps as well as plan reviews and adjustments, as required
In the fifth phase, the degree to which goals have been reached and variances between the expected and completed pathways should be available. Plans can then be adjusted and reviewed; each intervention can be modified. Since phase 4 hasn’t been fully implemented in the current CCPs, each plan must be reviewed manually. The subsequent full implementation will include automatic issue alerts to inform users of a lack of action or delay in treatment or consultation. These variances could also be aggregated for the purposes of administrative analysis. This would be useful to service providers in readjusting the expected pathway, the team in optimizing the process, and managers in reengineering service organization. Plans can currently be monitored individually as well as for conducting a full reassessment of the person, using the baseline assessment for the review, thereby shortening the reassessment time.
Discussion
Combining the different software-development methodologies produced benefits and challenges. Using a large-scale participatory design with multiple groups helped build a final system shaped according to needs and practice on the ground. Constant input served to fine-tune the system to broadly cover each CCP element but with adequate clinical detail. Given the project’s significant constraints (such as a short timeline, small development-team size, and limited financial resources), some difficulties were encountered into addressing each of the groups’ propositions and suggestions. While the AGILE SCRUM methodology allows for such adjustments in each iteration,Citation43 the client (MSSS) had to make constraint-related choices, resulting in some of the user input being postponed. Consequently, end users, healthcare professionals, managers, and research-team members (many of whom were experts in their fields or experienced system end users) felt that their input wasn’t given due consideration. Something similar was reported when the client wasn’t the end user involved in the PD process.Citation28 The use of a computerized system not adapted to the needs of the target audiences might become the impediment to CCPs being integrated into Quebec’s health and social services system.Citation20 MSSS is committed to making the necessary improvements in future releases. In the interim, the delays in producing these improvements could increase skepticism about the technology, reduce user acceptance, and negatively affect the perceived benefits of person-centered needs assessments and better clinical processes.Citation44,Citation45
Using the SSM model as a first step proved beneficial and will help assess the final system by comparing it to the model and validating if it addresses all the specifications. The model provided a general framework, allowing the groups involved in the PD process and the development team to focus on the target. Between August 2016 and December 2018, 6370 persons at the 3 beta sites were assessed with the CCPs, including 1404 reassessments (total of 7774 assessments), involving more than 720 healthcare professionals.
The possibility of aggregating assessment data (OEMC) to support shared decision-making and automatically transfer identified needs to the particular plan are features that were highlighted by the chosen software-development methodology and implemented in the current system. Since 2018, using combined methodology has yielded a fully functional system used by the various healthcare professionals throughout home-care settings in Quebec. It has also been adapted and used for people older than 18 years requiring long-term care. Considering resource scarcity and time constraints (development over two years, including one year for developing the main features), rigorous methods clearly were a factor contributing to the system’s success. This is true even if each CP phase hasn’t been fully implemented in a completely user-friendly and assistive way. Developments should continue, however, until 2022.
Aggregating these data over needs and services and analyzing the variances in CCPs enable managers to better determine met and unmet needs in their populations; make informed choices in supporting a diversified offering adapted to these needs; offer a continuum of clinical information using certain performance indicators in order to monitor the performance and continuous improvement of practices; foster the complementarity of services; and enter into appropriate agreements with public, private, and community partners.Citation46
Conclusion
Computerization is a key component for successful CP implementation. While still under development, the system’s current state fully supports the processes and functionalities of the first 3 phases of the CP process. It has, however, proven less effective with respect to the other 2 phases. Nevertheless, the system constitutes an interactive solution to support CPs between clients and the various healthcare professionals in home-care settings.
The system presented herein streamlines the collection of essential data in clinical settings while offering a way to control the source and quality of the data entered; facilitates the aggregation, viewing, and extraction of these data according to user needs; and, lastly, offers the possibility to merge this information in a clinically helpful way. It also facilitates the exchange of information between healthcare professionals, persons, and caregivers in using the clinical decision-making process. Once aggregated in future software developments, the data will also support managers in organizing teamwork and follow-up for home-care clients.
Using multiple software-development methodologies to cope with the shortcomings of a specific method proved to be an efficient approach in the CCP project, delivering a fully functional, efficient system given the project’s very limited resources.
The new Quebec RSIPA solution incorporating our CCPs is a promising example of technologies that support integrated-care delivery through better assessment, planning, organization, and monitoring.
Acknowledgments
The authors would like to acknowledge the help given by Isabelle Labrecque, former MSSS project manager; Valérie Guillot, current MSSS project manager; and the other MSSS team members involved in the CCP project.
The authors wish to thank Sébastien Lessard, DGTI/MSSS project leader, and his team members for their contribution to the development of the system and revision of a previous version of this article.
Moreover, the authors would like to acknowledge the collaboration of Joanne Guilbeault, former CESS managing director, and CESS trainers and clinical specialists, with whom they interacted while building the normative framework and preparing CCP training. The authors are also grateful to all former CdRV research team members for any contributions to CCP development.
Lastly, the 2012 prototype was developed through CSSS collaboration (Jardins-Roussillon), which the authors gratefully acknowledge. Specifically, the authors wish to thank Stéphane Dubuc, department director; Julie Aupin, nurse clinical IT advisor; and many other managers and stakeholders for their contributions.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- MacAdam M. PRISMA: Program of Research to Integrate the Services for the Maintenance of Autonomy. A system-level integration model in Quebec. Int J Integr Care. 2015;15:e018. doi:10.5334/ijic.2246.
- Breton M, Gray CS, Sheridan N, Shaw J, Parsons J, Wankah P, Kenealy T, Baker R, Belzile L, Couturier Y, et al. Implementing community based primary healthcare for older adults with complex needs in Quebec, Ontario and New-Zealand: describing nine cases. Int J Integr Care. 2017;17:12. doi:10.5334/ijic.2506.
- Somme D, Bonin L, Lebel P, Hebert R, Blanchard F. Development of an individualized service plan tool and rules for case management in Quebec. Care Manag J. 2009;10:89–99. doi:10.1891/1521-0987.10.3.89. Epub 2009/ 09/24.
- Soucy H L’implantation des réseaux de services intégrés pour les personnes âgées au Québec. In Texte publié dans les Actes du congrès Démarche SMAF - de l’évaluation à la prestation et la gestion des services, pour de meilleures pratiques auprès des personnes en perte d’autonomie. Québec; Nov 17–18; 2011. p. e1–11.
- Vedel I, Monette M, Beland F, Monette J, Bergman H. Ten years of integrated care: backwards and forwards. The case of the province of Québec, Canada. Int J Integr Care (IJIC). 2011;11 Spec Ed:e004–e.
- Demers L. Mergers and integrated care: the Quebec experience. Int J Integr Care. 2013;13:e002. doi:10.5334/ijic.1140. Epub 2013/ 05/21.
- Protecteur du citoyen du Québec. Rapport d’enquête - Chez soi: toujours le premier choix? L’accessibilité aux services de soutien à domicile pour les personnes présentant une incapcité significative et persistante. Québec, Canada: Gouvernement du Québec; 2012, p. 32
- Dubuc N, Bonin L, Tourigny A, Mathieu L, Couturier Y, Tousignant M, Corbin C, Delli-Colli N, Raîche M. Development of integrated care pathways: toward a care management system to meet the needs of frail and disabled community-dwelling older people. Int J Integr Care. 2013;13:e017. doi:10.5334/ijic.976. Epub 2013/ 07/25.
- de Luc K, Todd J. e-Pathways: computers and the patient’s journey through care. Oxon, UK: Radcliffe medical press; 2003. p. 197.
- Damiani G, Pinnarelli L, Colosimo SC, Almiento R, Sicuro L, Galasso R, Sommella L, Ricciardi W. The effectiveness of computerized clinical guidelines in the process of care: a systematic review. BMC Health Serv Res. 2010;10:2. doi:10.1186/1472-6963-10-2. Epub 2010/ 01/06.
- Gooch P, Roudsari A. Computerization of workflows, guidelines, and care pathways: a review of implementation challenges for process-oriented health information systems. J Am Med Inform Assoc. 2011;18:738–48. doi:10.1136/amiajnl-2010-000033. Epub 2011/ 07/05.
- Hyde E, Murphy B. Computerized clinical pathways (care plans): piloting a strategy to enhance quality patient care. Clin Nurse Spec. 2012;26:277–82. doi:10.1097/NUR.0b013e31825aebc1. Epub 2012/ 08/21.
- Saleem JJ, Savoy A, Etherton G, Herout J. Investigating the need for clinicians to use tablet computers with a newly envisioned electronic health record. Int J Med Inform. 2018;110:25–30. doi:10.1016/j.ijmedinf.2017.11.013.
- Karsh B-T, Weinger MB, Abbott PA, Wears RL. Health information technology: fallacies and sober realities. J Am Med Inf Assoc. 2010;17:617–23. doi:10.1136/jamia.2010.005637.
- Swallow V, Carolan I, Smith T, Webb NJ, Knafl K, Santacroce S, Campbell M, Harper-Jones M, Hanif N, Hall A. A novel Interactive Health Communication Application (IHCA) for parents of children with long-term conditions: development, implementation and feasibility assessment. Inform Health Soc Care. 2016;41:20–46. doi:10.3109/17538157.2014.948174. Epub 2014/ 08/15.
- Ozel D, Bilge U, Zayim N, Cengiz M. A web-based intensive care clinical decision support system: from design to evaluation. Inform Health Soc Care. 2013;38:79–92. doi:10.3109/17538157.2012.710687. Epub 2012/ 09/11.
- Raptis DA, Graf R, Peck J, Mouzaki K, Patel V, Skipworth J, Oberkofler C, Boulos PB. Development of an electronic web-based software for the management of colorectal cancer target referral patients. Inform Health Soc Care. 2011;36:117–31. doi:10.3109/17538157.2010.520420. Epub 2011/ 08/19.
- Demiris G, Thompson H, Boquet J, Le T, Chaudhuri S, Chung J. Older adults’ acceptance of a community-based telehealth wellness system. Inform Health Soc Care. 2013;38:27–36. doi:10.3109/17538157.2011.647938. Epub 2012/ 05/11.
- Holden RJ, Asan O, Wozniak EM, Flynn KE, Scanlon MC. Nurses’ perceptions, acceptance, and use of a novel in-room pediatric ICU technology: testing an expanded technology acceptance model. BMC Med Inform Decis Mak. 2016;16:145. doi:10.1186/s12911-016-0388-y.
- Wixom BH, Todd PA. A theoretical integration of user satisfaction and technology acceptance. Inf Syst Res. 2005;16:85–102. doi:10.1287/isre.1050.0042.
- Tremblay M, Vallee C, Carignan M, Provencher V, Delli-Colli N, Poulin V, Giguere A, Careau E, Giroux D. Design and implementation of the Competency Assessment Tool (CAT): user experience usability study. Inform Health Soc Care. 2020;45:57–76. doi:10.1080/17538157.2018.1550414. Epub 2018/ 12/14.
- Bjerkan J, Hedlund M, Helleso R. Patients’ contribution to the development of a web-based plan for integrated care - a participatory design study. Inform Health Soc Care. 2015;40:167–84. doi:10.3109/17538157.2014.907803. Epub 2014/ 05/03.
- Valimaki M, Anttila M, Hatonen H, Koivunen M, Jakobsson T, Pitkanen A, Herrala J, Kuosmanen L. Design and development process of patient-centered computer-based support system for patients with schizophrenia spectrum psychosis. Inform Health Soc Care. 2008;33:113–23. doi:10.1080/17538150802127207. Epub 2008/ 07/08.
- McConnell S. Rapid development : taming wild software schedules. Redmond (Wash): Microsoft Press; 1996. p. xix, 647.
- Schwaber K, Beedle M. Agile software development with Scrum. Upper Saddle River (NJ): Prentice Hall; 2002. p. xvi, 158.
- Petersen K, Wohlin C. A comparison of issues and advantages in agile and incremental development between state of the art and an industrial case. J Syst Software. 2009;82:1479–90. doi:10.1016/j.jss.2009.03.036.
- Munassar NMA, Govardhan A, A comparison between five models of software engineering. IJCSI Int J Comput Sci Issues. 2010;7:94–101.
- Bordin S, De Angeli A. Communication breakdowns in the integration of user-centred design and agile development. In: Cockton G, Lárusdóttir M, Gregory P, Cajander Å, editors. Integrating user-centred design in agile development. Human–computer interaction series. Cham (Switzerland): Springer, 2016, p.137–161.
- Kautz K Participatory design activities and agile software development. In: Pries-Heje J, Venable J, Bunker D, Russo NL, DeGross JI, editors. Human Benefit through the Diffusion of Information Systems Design Science Research TDIT 2010. IS Design Science Research, IFIP AICT ed. Berlin, Heidelberg: Springer, 2010, p. 303–16.
- Salah D, Paige RF, Cairns P A systematic literature review for agile development processes and user centred design integration. In: Engineering EEaAiS, editor. 18th International Conference on Evaluation and Assessment in Software Engineering London, England: EASE ‘14 Evaluation and Assessment in Software Engineering; 2014.
- Turk D, France R, Rumpe B. Limitations of Agile Software Processes. In Third International Conference on Extreme Programming and Flexible Processes in Software Engineering, XP2002. Alghero, Italy; 2002, p. 43–46.
- Checkland P. Soft Systems Methodology : A thirty year retrospective. Syst Res Behav Sci. 2000;17:S11–S58.
- Grudin J. Interactive systems: bridging the gaps between developers and users. Computer. 1991;24:59–69. doi:10.1109/2.76263.
- Bustard D, Keenan F. Soft systems methodology: an aid to agile development? In: Wojtkowski W, Wojtkowski G, Lang M, Conboy K, Barry C, editors. Information systems development. Boston (MA): Springer; 2009. p. 25–38.
- van Velsen L, Illario M, Jansen-Kosterink S, Crola C, Di Somma C, Colao A, Vollenbroek-Hutten M. A community-based, technology-supported health service for detecting and preventing frailty among older adults: a participatory design development process. J Aging Res. 2015;2015:216084. doi:10.1155/2015/216084.
- Martin A, Biddle R, Noble J. The XP customer role in practice: three studies. In Agile Development Conference (ADC’04). Salt Lake City (UT): IEEE Institute of Electrical and Electronics Engineers; 2004.
- Garrett JJ. The elements of user experience : user-centered design for the Web and beyond. 2nd ed. Berkeley (CA): New Riders; 2011. p. xviii, 172.
- Québec (Province). Comité aviseur sur l’adoption d’un outil d’évaluation intégré des besoins des personnes en perte d’autonomie et de détermination des services requis notamment en institution ou à domicile. Québec, Canada: Ministère de la santé et des services sociaux; 2000, p. 84.
- Hébert R, Guilbeault J, Desrosiers J, Dubuc N. The functional autonomy measurement system (SMAF): a clinical-based instrument for measuring disabilities and handicaps in older people. Geriatrics Today. 2001;4:141–47.
- Pinsonnault E, Desrosiers J, Dubuc N, Kalfat H, Colvez A, Delli-Colli N. Functional autonomy measurement system: development of a social subscale. Arch Gerontol Geriatr. 2003;37:223–33. doi:10.1016/S0167-4943(03)00049-9. Epub 2003/ 09/27.
- Pinsonnault E, Dubuc N, Desrosiers J, Delli-Colli N, Hebert R. Validation study of a social functioning scale: the social-SMAF (social-Functional Autonomy Measurement System). Arch Gerontol Geriatr. 2009;48:40–44. doi:10.1016/j.archger.2007.10.001. Epub 2007/ 12/07.
- Dubuc N, Hebert R, Desrosiers J, Buteau M, Trottier L. Disability-based classification system for older people in integrated long-term care services: the Iso-SMAF profiles. Arch Gerontol Geriatr. 2006;42:191–206. doi:10.1016/j.archger.2005.07.001. Epub 2005/ 08/30.
- Highsmith J. what is agile software development? J Def Soft Engi. 2002;15:4–9.
- Marangunic N, Granic A. Technology acceptance model: a literature review from 1986 to 2013. Universal Access Info Soc. 2015;14:81–95. doi:10.1007/s10209-014-0348-1.
- Hallikainen H, Laukkanen T. How technology readiness explains acceptance and satisfaction of digital services In B2B Healthcare Sector? In Pacific Asia Conference on Information Systems (PACIS) 2016 Proceedings 294. Chiayi, Taiwan: Association for Information Systems AIS Electronic Library (AISeL); 2016.
- Abedjan Z, Boujemaa N, Campbell S, Casla P, Chatterjea S, Consoli S, Costa-Soria C, Czech P, Despenic M, Garattini C. Data science in healthcare: benefits, challenges and opportunities. In: Consoli S, Reforgiato Recupero D, Petkovic M, SpringerLink, et al., editors. Data science for healthcare methodologies and applications. Cham, Switzerland: Springer International Publishing : Imprint: Springer; 2019. 3–38.