ABSTRACT
Identify pregnancy-related challenges and opportunities to improve maternal health care in the United States and understand the potential role of predictive analytics tool(s) in bridging the existing gaps, specifically, in CVD (cardiovascular disease) and depression. Experts in maternal health care, research, patient advocacy, CVD, psychiatry, and technology were interviewed during February and March of 2020. Additionally, published literature was reviewed to assess existing data, insights, and best practices that might help develop effective predictive analytics tool(s). The majority (78%) of the 18 experts interviewed were women. The feedback revealed several insights, including multiple barriers to diagnosis and treatment of pregnancy-related CVD and depression. In experts’ collective opinion, predictive analytics could play an important role in maternal health care and in limiting pregnancy-related CVD and depression, but it must be grounded in quality data and integrate with existing health management systems. A holistic approach to maternal health that factors in racial-ethnic, regional, and socioeconomic disparities is needed that starts with preconception counseling and continues through 1 year postpartum. Predictive analytics tool(s) that are based on diverse and high-quality data could bridge some of the existing gaps in maternal health care and potentially help limit pregnancy-related CVD and depression.
Introduction
Women in the United States are more likely to die from pregnancy-related causes or childbirth compared with women in other high-income countries.Citation1,Citation2 The number of pregnancy-related deaths per 100,000 live births in the United States increased from 7.2 in 1987 to 17.8 in 2009 and then stabilized through 2016 (16.9 deaths).Citation3 It is unclear whether the initial increase in pregnancy-related deaths was due to actual increase in the risk or it represented improved reporting over time.Citation3 Approximately 700 women die every year due to pregnancy-related causes in the United States.Citation1,Citation4 Data from Centers for Disease Control and Prevention (CDC) for 2011–2015 showed that approximately one-third of the deaths each occurred during pregnancy, at or within 1 week after delivery, and during 1 week through 1 year following childbirth; approximately 60% of these deaths were preventable.Citation5 The likelihood of pregnancy-related death is approximately 3 times higher in non-Hispanic Black and American Indian/Alaska Native women compared with non-Hispanic White women, although the proportion of preventable deaths does not differ by race/ethnicity.Citation5,Citation6
The leading cause of pregnancy-related deaths in the United States is cardiovascular conditions, which, according to CDC, includes coronary artery disease, pulmonary hypertension, valvular heart disease, vascular aneurisms, Marfan syndrome, conduction defects, vascular malformations, and other similar cardiovascular disorders but excludes cardiomyopathy, preeclampsia/eclampsia, and chronic hypertension; other frequent causes include hemorrhage, cardiomyopathy, and infection.Citation4–6 During 2006–2013, cardiovascular disease (CVD; includes cardiovascular conditions as defined above and cardiomyopathy) caused approximately 26% of all pregnancy-related deaths in the United States.Citation7,Citation8 Cardiomyopathy is the leading cause of CVD-related maternal deaths, which tends to occur during the late postpartum period.Citation9,Citation10 The leading causes of pregnancy-related deaths vary by state, education, age, and race.Citation4,Citation6 For example, data from 14 states during 2008–2017 showed that the leading causes of pregnancy-related deaths (>10% incidence) among non-Hispanic Black women were cardiomyopathy (13.9%), cardiovascular conditions (13.9%), preeclampsia/eclampsia (11.4%), hemorrhage (10.8%), embolism (10.1%), and infection (10.1%), while those among non-Hispanic White women were mental health conditions (14.9%), cardiovascular conditions (13.4%), hemorrhage (13.4%), and infection (12.4%).Citation6
Although a significant cause of maternal death globally,Citation11,Citation12 mental health conditions, including suicide and drug overdose, have not received much needed attention.Citation13 Mental health conditions are the leading cause of pregnancy-related deaths in non-Hispanic White women and cause 8.8% of all pregnancy-related deaths in the United States.Citation6 Furthermore, mental health conditions and substance-use disorder contribute to approximately 12.9% and 8.2% of pregnancy-related deaths, respectively, including approximately 6.5% of deaths by suicide, demonstrating that they are significant contributors even when they are not the primary cause of death.Citation4 Perinatal mood and anxiety disorders also contribute to maternal morbidity and have profound adverse impacts on the mother and her offspring and family.Citation14–16 A large, sequential case series study from an urban academic women’s hospital in Pittsburgh found that 14.0% of the women screened after childbirth had depression; of these, approximately two-thirds each had major depression and comorbid anxiety disorders, 22.6% had bipolar disorders, and 19.3% had ideation of self-harm.Citation17 Most instances of depressive episodes started perinatally (postpartum, 40.1%; during pregnancy, 33.4%), while 26.5% started before pregnancy; women with depression were more likely to be younger, single, African American, less well educated, and publicly insured.Citation17
Recommendations and guidelines exist for screening, treatment, and management of pregnancy-related CVD and perinatal depression, and multiple screening tools and safety bundles are available for both.Citation4,Citation9,Citation15,Citation18–20 However, gaps that contribute to preventable morbidity and mortality remain. For example, a relatively low proportion of women – even those with preexisting conditions – receive preconception counseling on family planning and/or CVD- and depression-related health risks, perinatal screening for CVD, and treatment for postpartum depression.Citation21–24 In addition, a relatively large number of women in the United States live in areas (over 5 million women in 1085 counties in 2016) with no obstetric care hospitals or providers – so-called maternity care desertsCitation25; these women also face inadequate access to routine health care.Citation26 Access to health insurance is another important factor that affects maternal health in the United States. During 2012–2014, a significantly smaller proportion of uninsured (36%) or Medicaid-covered (64%) women received adequate prenatal care, compared with privately insured women (84%).Citation27 These gaps ultimately result in missed diagnoses of perinatal CVD and depression.
Predictive analytics tool(s) could potentially bridge some of the existing gaps by providing opportunities for timely screening, diagnosis, and treatment. The objective of this study was twofold: 1) to identify pregnancy-related challenges and opportunities to improve maternal health in the United States, with a focus on perinatal CVD and depression, and 2) to understand the potential role of digital tool(s), specifically predictive analytics, that can help health-care providers identify and address health risks earlier in the perinatal period, thereby improving maternal health outcomes.
Methods
Published literature (primarily from CDC, The American College of Obstetricians and Gynecologists, and Medicaid) was analyzed to assess insights and best practices available and to provide background for and direct the interviews. To assess currently available digital technology in this context, we performed internet searches (nonsystematic) for maternal health tools designed for pregnant women and/or providers that offered guidance during and/or after pregnancy. Specifically, a Google search was performed to identify relevant international tools. Tool websites were examined, as well as news sources (blog posts and press releases) on their implementation and use. The authors’ prior knowledge of maternal health and existing tools was also used to identify apps to explore further. A total of 39 such digital health tools were identified from the search for further review.
Next, semi-structured interviews were conducted with several United States experts in the maternal health, CVD, and perinatal depression space during February and March of 2020 in 2 phases. Experts were chosen based on their professional backgrounds and areas of expertise within the maternal health field (eg, academia, government, clinical care, research, advocacy, technology). Questions were tailored to experts based on their areas of expertise. Pregnancy-related conditions of the newborn (eg, preterm birth) were not addressed in these interviews. In phase 1, exploratory interviews were conducted to understand the experts’ perceptions of the following: 1) potential barriers to improving maternal health in the United States, and how those could be addressed, 2) opportunities for improving diagnosis, care, and treatment of pregnancy-related CVD and perinatal depression, and 3) opportunities for technology to address unmet needs.
Phase 2 interviews were conducted to gather additional information, specifically on CVD and perinatal depression, and for vetting a potential predictive analytics tool. The goal of these interviews was twofold: 1) to understand providers’ perspectives on the challenges of diagnosing and treating pregnancy-related CVD and perinatal depression and 2) to identify the value of using technology and predictive analytics tool(s) to support more efficient screening, diagnosis, and treatment. The questions posed to the experts in both phase 1 and phase 2 interviews and some examples of their responses are shown in Supplementary Table 1.
Interview analysis was conducted as follows: a descriptive analysis of expert demographics was performed, transcripts were created, and areas of commonality between transcripts were identified and summarized using thematic analysis. To understand the range in responses around the role of technology in mental health, outlier responses were also included.
Results
Experts Demographics
Of 18 subject-matter experts interviewed, 5 (28%) were women’s health clinicians (1 each of general obstetrician-gynecologist, maternal fetal medicine specialist, women’s health nurse practitioner, perinatal nurse, and maternal–fetal mental health specialist), 4 (22%) were technology experts, including 1 who was also an obstetrician-gynecologist, 4 (22%) were scientific researchers, 3 (17%) were patient advocates, and 2 (11%) were non-women’s health specialists (a cardiologist and a psychiatrist) (). The majority of the experts (14 [78%]) were women. The interviews were focused on perinatal depression (six interviews), CVD (four interviews), broad/both areas (four interviews), and technology (three interviews with four experts).
Table 1. Demographic Characteristics of Interviewed Experts
Opportunities to Improve Maternal Health
The response from experts to the question about the greatest opportunities to improve maternal health in the United States provided several insights. One overarching recommendation was to use a holistic approach to maternal health – before, during and after the perinatal period. Preconception counseling is a critical and often missing service, and women are underserved during the 12 months postpartum; the fact that nearly half of pregnancies are unplanned makes the problem even more complex. Furthermore, availability of relatively few or even no providers in some areas (maternity care “deserts”) often leads to low and/or inconsistent quality of care throughout pregnancy and postpartum.Citation25 Several factors, such as lack of insurance coverage, competing priorities, and challenges transitioning to a new physician, contribute to the decline in women’s access to postpartum care.
An additional important insight that emerged was the need to improve coordination and collaboration among specialists caring for women during the perinatal period. For example, obstetricians may feel poorly prepared to manage non-obstetric conditions such as CVD or depression and non-obstetricians may not be prepared to care for patients with these conditions during pregnancy. Lack of coordination among providers can thwart the ability to efficiently manage high-risk pregnancies. However, coordinating care between specialists before, during, and after pregnancy is challenging, and inadequate referral systems between providers can lead to poor health outcomes. Experts also recommended developing care models that factor in racial-ethnic and socioeconomic disparities. Linkages between community care and health-care facilities are weak. For example, most providers are not formally trained to deliver patient-centered culturally sensitive care. Similarly, care models and data collection tools do not take social determinants of health into consideration.
Experts agreed that technology has a role to play, but also that it is only one small piece of a complex issue. Therefore, a consensus that emerged was that a multifaceted approach, including technology, is needed to address gaps in diagnosis and care to minimize maternal morbidity and mortality. Predictive analytics can add value to maternal health care, but only if designed using strong data and keeping integration with existing health management systems (eg, electronic health record [EHR]) in mind. This is because strong predictive analytic tools rely on algorithms that take numerous data points into consideration, and their integration with existing data systems and care models will ease providers’ workflow and increase usage, which in turn would further contribute to development of strong algorithms with more data points.
Disease-Specific Barriers to Diagnosis and Treatment
Experts identified several barriers to diagnosis and treatment of pregnancy-related CVD and depression. For CVD, these include a relative shortage of providers who specialize in both cardiology and maternal health (cardio-obstetricians), increase in the number of pregnant women with preexisting conditions and comorbidities, and inadequate preconception counseling for women with preexisting conditions. Furthermore, even when a risk is detected, patients do not always receive the indicated workup or referral. For perinatal depression, experts identified a relative shortage of mental health specialists, frequent changes in treatment and care protocols for depression as the pregnancy advances, requirement of personalized care plans for different coexisting conditions, and the stigma of a mental health diagnosis among patients and their communities, as well as within the health-care system.
Trends and Concerns Regarding Digital Technology for Maternal Health
In experts’ collective opinion, interest in predictive analytics is rising, and many data scientists are focusing on generating high-quality data, including biomarkers and risk factors, to build artificial intelligence. Experts held that the quality of the data and their integration with existing health systems are critical to the success of predictive analytics technologies designed to improve maternal health. They expressed concerns regarding the specificity and sensitivity of predictive tools; for example, false-positive results could increase fear and anxiety among pregnant women, unnecessary testing, and higher costs of care. Additional challenges identified were staffing gaps to introduce and use new tools, various roadblocks hindering health data exchange between patients and health-care facilities and between different facilities, and organizational planning and other challenges (eg, ease of use) that can keep providers from adopting new technology.
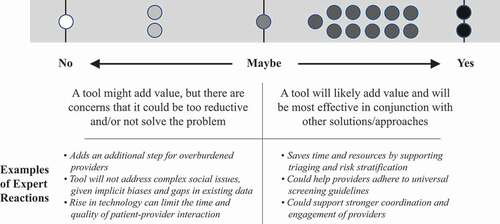
Most experts agreed that a predictive analytics tool would be valuable in curtailing risk for CVD and perinatal depression, but it should be a part of the broader efforts to improve coordination and quality of care. Among 18 experts, only 1 did not see any value of a predictive tool, 2 thought that a tool might add value but that it could be too reductive and/or not solve the problem, and 1 was indecisive (). Among four experts who did not see a positive value of predictive analytics tool(s), two were patient advocates/researchers and two were general clinical practitioners.
Existing Maternal Health Technology
Among the 39 existing maternal health digital tools that were identified from our search, most were designed for general maternal health care (32 [82%]) and consumer facing (30 [77%]) (Supplementary Table 2). Six tools – four consumer facing and two provider facing – were for mental health, including perinatal depression. Only one provider facing tool addressed CVD.
Data Considerations for Developing Predictive Analytics Tool(s)
A significant recommendation that emerged from the expert interviews was to use data from multiple sources, including a blend of claims data, historical medical records (from before prenatal counseling) and patient-reported outcomes. Additionally, understanding of the limitations of real-world data sources was considered important. For example, while the people-centered wearable health technologies (eg, Apple Watch®, Fitbit®) offer access to new patient data, the results should be interpreted with caution and must be verified by other independent data sources. To fill existing gaps, experts suggested digital innovation to generate new data, which can offer an opportunity to generate insights more quickly compared with clinical trials. For example, data can potentially be gathered from women who experience perinatal depression but have no record of mental health complications. Similarly, data can be collected to understand heterogeneity in presentation of CVD symptoms, and how they affect different populations (eg, woman vs men, or different demographics), as well as to understand social determinants of health and interpersonal dynamics.
Integration of New Digital Technology With Existing Health Systems
Experts agreed that a predictive analytics tool should fit into existing workflows and processes to ensure interoperability and minimize additional work for providers. Providers should be engaged throughout tool development, and feedback should be obtained from focus groups with representation from different clinical care settings (eg, public and private, types of hospitals), payors (eg, private and Medicaid), and providers (eg, generalists and specialists). Once a tool is initially implemented, built-in mechanisms should ensure that the algorithms are modified to address specific feedbacks and the implementation–feedback cycles repeated until all involved are satisfied. The tool should be embedded into existing data and communications systems, including EHRs and patient portals. Additional expert recommendations included incorporating screening tool(s) into education modules and trainings for all types of providers who are likely to interface with the tool, developing clear guidance on referrals and recommended next steps tailored to the specific health care systems (eg, contact information of or e-mail draft to specialist) in high-risk cases, and automatically sending reports to patients to minimize work for providers.
Potential Users of Predictive Analytics Tool(s)
Experts identified several individuals in the care pathway who could use predictive analytics tool(s) during screening or treatment. For screening, the potential users include obstetricians and other obstetric care providers (eg, nurse practitioners, certified nurse-midwives, patient care assistants), cardiologists who manage patients with preexisting cardiovascular conditions, pediatricians conducting postpartum depression screenings for mothers at well-child visits, and primary care clinicians conducting postpartum follow-up visits. For treatment, the potential users are care teams for patients with preexisting CVD or perinatal depression, including cardiologists, general obstetricians, consultative maternal–fetal medicine specialists, cardio-obstetricians, and mental health-care professionals providing pharmacological, behavioral, and psychiatric therapy.
Discussion
Maternal health experts (direct obstetric care clinicians, nurses, researchers, patient advocates, and technologists) were interviewed in order to understand the unmet needs of women and health-care providers related to pregnancy-related CVD and perinatal depression, as well as potential role of predictive analytics tool(s) in fulfilling those needs. Several insights were developed from these interviews. Maternal health must be assessed more holistically, from preconception through 1 year postpartum. Improved coordination and collaboration among maternal health providers is needed, with experts taking primary maternal care responsibility depending on the women’s individual health needs. Predictive analytics can play an important role in timely diagnosis and treatment and in improving efficiency, but it must be grounded in high-quality data from multiple sources and be integrated with the existing systems and processes; if needed, new data should be generated. Assessment of several existing maternal health tools revealed an unmet need for predictive analytics tools, especially for CVD, as well as additional provider-facing tools for both CVD and perinatal depression.
There is a relative shortage of maternal health-care providers in the United States,Citation28–31 and the number of women, especially those with preexisting conditions, is rising,Citation32,Citation33 As a consequence, maternal health-care providers are often overwhelmed with the amount of work. An effective predictive analytics tool could potentially bridge any gaps between providers’ limited time and prioritizing care for women with high-risk pregnancies. For example, the time to screen and diagnose may shorten, and generalists and less qualified providers may be able to screen high-risk patients faster. Importantly, risk prediction can help focus the clinical care on the most likely maternal risk conditions. The shortage of providers is also unevenly distributed in the country; nearly half of the United States counties – mostly rural – with approximately 8% of all women in the country in 2010, had no obstetricians,Citation28 and many metropolitan areas are likely to face a shortage in the near future.Citation31 New digital technology could help bridge the unmet need of these maternity care “deserts” through improved and timely transmission of health data and remote monitoring.Citation34
A successful new predictive analytics tool will need to follow the four established phases: acquire data, develop and validate, test in real-world setting, and disseminate for use. Data acquisition will need to adhere to federal guidelines on consent and privacy, ensure equitable representation and access, and allow harmonization of data from different sources. The development of the tool should include patient and provider perspectives and ensure transparency and replicability; validation should be performed against multiple datasets. Real-world testing will need to maintain appropriate protections and precautions for patients, as well as consider and protect against liability issues for providers and health-care systems. The end use of the tool will need to ensure equitable access and privacy, and it should continually monitor data so it can be dynamically refined and reconfigured to improve sensitivity and specificity.
An existing cardiovascular toolkit, Improving Health Care Response to Cardiovascular Disease in Pregnancy and Postpartum, was developed as a resource for obstetrics, primary care, and emergency medicine providers and includes a predictive algorithm to identify pregnant and postpartum women that are symptomatic or at high risk of CVD.Citation20 Similarly, Edinburgh Postpartum Depression Scale is a manually or digitally self-administered toolkit that was developed to identify women who may have postpartum depression.Citation35 However, these tools may not detect less straightforward symptoms that can potentially be misperceived as normal attributes of pregnancy, such as mood changes and shortness of breath.Citation36 A new predictive analytics tool could potentially address this problem by improving the accuracy of risk assessment for CVD or for postpartum depression by using a large dataset in its development.
Study Limitations and Future Work
This was an exploratory study with a relatively small sample size that was designed to identify initial trends. Larger studies will be needed to confirm the results presented here and to reveal any additional insights. Technical experts interviewed for this study were reluctant to share information about their data and how they are using them, likely because their data are the backbone of their product development, making it difficult to gather many real-world examples and insights.
Implications for Practice and/or Policy
The challenges facing maternal health care are complex and require a multifaceted and coordinated approach. Predictive analytics can be a powerful tool that can potentially close some existing gaps and improve maternal health care, especially in the areas of CVD and depression. However, the success of such tools would depend on several factors. For example, quality data that are unbiased and derived from diverse sources would be crucial; a tool developed based only on claims data is likely to miss subtle but significant patient signs and symptoms. Similarly, real-world data, including patient-reported outcomes could be critical to uncover new insights. Another significant factor would be early integration with existing health management systems (eg, EHR) to ensure acceptance among health-care providers, and to streamline the care pathway. More importantly, predictive analytics will supplement and not replace the armamentarium already available to the maternal health-care teams. A predictive analytics tool will not succeed in reducing pregnancy-related mortality and morbidity without other broader challenges being addressed, including access to maternity care, improvement of services at the point of care, racial and regional disparities, and training of providers to diagnose and care for women with pregnancy-related complications such as CVD and postpartum depression.
Conclusions
Feedback from diverse maternal health experts in maternal health care and research, patient advocacy, cardiology, psychiatry, and technology revealed several useful insights. The primary theme that emerged was that a predictive analytics tool could play an important role in maternal health care and in limiting the risk for perinatal CVD and depression as long as it is based on quality data, integrates with existing health management systems, and improves communication and coordination among caregivers. Several barriers to diagnosis and treatment of women with preexisting or pregnancy-related conditions, especially perinatal CVD and depression, were identified. An all-inclusive approach to maternal health that factors in racial-ethnic, regional, and socioeconomic disparities is needed that starts with preconception counseling and is continued through 1 year postpartum.
Acknowledgments
Authors thank Saroj Sedalia, Vice President, Rabin Martin, New York, NY, for her role in conducting some expert interviews and in data acquisition, and Joy Marini, Senior Director, Health of Women, Johnson & Johnson, for her insights into the framework used to interview experts for this study. Writing assistance was provided by Narender Dhingra, MBBS, PhD, CMPP, of System One, and funded by Janssen Global Services, LLC.
Disclosure statement
SVS and RRJ are employees of Johnson & Johnson and own stock and/or stock options. MM is an employee of Rabin Martin, the firm that conducted the expert interviews.
Data Availability Statement
All data generated or analyzed during this study are represented in this published article.
Additional information
Funding
References
- Centers for Disease Control and Prevention. Pregnancy-related deaths. 2019 [accessed 2020 July 14]. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-relatedmortality.htm.
- MacDorman MF, Declercq E, Cabral H, Morton C. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues. Obstet Gynecol. 2016;128(3):447–55. doi:10.1097/AOG.0000000000001556.
- Centers for Disease Control and Prevention. Pregnancy Mortality Surveillance System. 2020 [accessed 2020 July 14]. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html.
- Nine Maternal Mortality Review Committees Report. Building U.S. capacity to review and prevent maternal deaths. 2018 [accessed 2020 July 17]. https://www.cdcfoundation.org/sites/default/files/files/ReportfromNineMMRCs.pdf.
- Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, Syverson C, Seed K, Shapiro-Mendoza CK, and Callaghan WM, et al. Vital Signs: Pregnancy-Related Deaths, United States, 2011-2015, and Strategies for Prevention, 13 States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2019;68(18):423–29. doi:10.15585/mmwr.mm6818e1.
- Davis NL, Smoots AN, Goodman DA, Davis NL, Smoots AN, Goodman DA Pregnancy-related deaths: data from 14 U.S. Maternal Mortality Review Committees, 2008-2017. 2019 [accessed 2020 July 22]. https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/MMR-Data-Brief_2019-h.pdf.
- Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006-2010. Obstet Gynecol. 2015;125(1):5–12. doi:10.1097/AOG.0000000000000564.
- Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130(2):366–73. doi:10.1097/AOG.0000000000002114.
- The American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 212: pregnancy and heart disease. Obstet Gynecol. 2019;133(5):e320–e356. doi:10.1097/AOG.0000000000003243.
- Hameed AB, Lawton ES, McCain CL, Morton CH, Mitchell C, Main EK, Foster E. Pregnancy-related cardiovascular deaths in California: beyond peripartum cardiomyopathy. Am J Obstet Gynecol. 2015;213(3):379 e371–310. doi:10.1016/j.ajog.2015.05.008.
- Fuhr DC, Calvert C, Ronsmans C, Chandra PS, Sikander S, De Silva MJ, Patel V. Contribution of suicide and injuries to pregnancy-related mortality in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry. 2014;1(3):213–25. doi:10.1016/S2215-0366(14)70282-2.
- Khalifeh H, Hunt IM, Appleby L, Howard LM. Suicide in perinatal and non-perinatal women in contact with psychiatric services: 15 year findings from a UK national inquiry. Lancet Psychiatry. 2016;3(3):233–42. doi:10.1016/S2215-0366(16)00003-1.
- Mangla K, Hoffman MC, Trumpff C, O’Grady S, Monk C. Maternal self-harm deaths: an unrecognized and preventable outcome. Am J Obstet Gynecol. 2019;221(4):295–303. doi:10.1016/j.ajog.2019.02.056.
- Atkinson L, Paglia A, Coolbear J, Niccols A, Parker KC, Guger S. Attachment security: a meta-analysis of maternal mental health correlates. Clin Psychol Rev. 2000;20(8):1019–40. doi:10.1016/s0272-7358(99)00023-9.
- Kendig S, Keats JP, Hoffman MC, Kay LB, Miller ES, Moore Simas TA, Frieder A, Hackley B, Indman P, Raines C, et al. Consensus bundle on maternal mental health: perinatal depression and anxiety. Obstet Gynecol. 2017;129(3):422–30. doi:10.1097/AOG.0000000000001902.
- Murray L, Cooper P. Effects of postnatal depression on infant development. Arch Dis Child. 1997;77(2):99–101. doi:10.1136/adc.77.2.99.
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–98. doi:10.1001/jamapsychiatry.2013.87.
- The American College of Obstetricians and Gynecologists. ACOG committee opinion no. 757: screening for perinatal depression. Obstet Gynecol. 2018;132(5):e208–e212. doi:10.1097/AOG.0000000000002927.
- The American College of Obstetricians and Gynecologists. Council on Patient Safety in Women’s Health Care. Maternal mental health: perinatal depression and anxity. 2016 [accessed 2020 August 18]. https://safehealthcareforeverywoman.org/wp-content/uploads/2017/11/Maternal-Mental-Health-Bundle.pdf.
- Hameed AB, Morton CH, Moore A Improving health care response to cardiovascular disease in pregnancy and postpartum. Developed under contract #11-10006 with the California Department of Public Health. 2017 [accessed 2020 November 19]. https://www.cmqcc.org/resources-toolkits/toolkits/improving-health-care-response-cardiovascular-disease-pregnancy-and.
- Hillemeier MM, Weisman CS, Chase GA, Dyer AM, Shaffer ML. Women’s preconceptional health and use of health services: implications for preconception care. Health Serv Res. 2008;43(1 Pt 1):54–75. doi:10.1111/j.1475-6773.2007.00741.x.
- Pazol K, Robbins CL, Black LI, Ahrens KA, Daniels K, Chandra A, Vahratian A, Gavin LE. Receipt of selected preventive health services for women and men of reproductive age - United States, 2011-2013. MMWR Surveill Summ. 2017;66(20):1–31. doi:10.15585/mmwr.ss6620a1.
- Cheng D, Patel P. Optimizing women’s health in a Title X family planning program, Baltimore County, Maryland, 2001-2004. Prev Chronic Dis. 2011;8:A126.
- D’Angelo D, Williams L, Morrow B, Cox S, Harris N, Harrison L, Posner SF, Hood JR, Zapata L, For Disease C C, et al. Preconception and interconception health status of women who recently gave birth to a live-born infant–Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas, 2004. MMWR Surveill Summ. 2007;56(10):1–35.
- March of Dimes. Nowhere to go: maternity care deserts across the U.S. 2018 [accessed 2020 July 21]. https://www.marchofdimes.org/materials/Nowhere_to_Go_Final.pdf.
- Mager NA D, Zollinger TW, Turman JE ZJ Jr., Dixon BE. Routine healthcare utilization among reproductive-age women residing in a rural maternity care desert. J Community Health. 2020. doi:10.1007/s10900-020-00852-6.
- Medicaid and CHIP Payment Advisory Commission (MACPAC). Access in brief: pregnant women and medicaid. 2018 [accessed 2020 August 17]. https://www.macpac.gov/wp-content/uploads/2018/11/Pregnant-Women-and-Medicaid.pdf.
- Rayburn WF, Klagholz JC, Murray-Krezan C, Dowell LE, Strunk AL. Distribution of American Congress of Obstetricians and Gynecologists fellows and junior fellows in practice in the United States. Obstet Gynecol. 2012;119(5):1017–22. doi:10.1097/AOG.0b013e31824cfe50.
- Rayburn WF, Strunk AL, Petterson SM. Considerations about retirement from clinical practice by obstetrician-gynecologists. Am J Obstet Gynecol. 2015;213(3):335 e331–334. doi:10.1016/j.ajog.2015.03.027.
- Rayburn WF. The obstetrician-gynecologist workforce in the United States: facts, figures, and implications, 2017. American Congress of Obstetricians and Gynecologists; 2017. Book.
- Rosenberg J Physician shortage likely to impact OB/GYN workforce in coming years. 2019 [accessed 2020 November 19]. https://www.ajmc.com/newsroom/physician-shortage-likely-to-impact-obgyn-workforce-in-coming-years.
- Admon LK, Winkelman TNA, Moniz MH, Davis MM, Heisler M, Dalton VK. Disparities in chronic conditions among women hospitalized for delivery in the United States, 2005-2014. Obstet Gynecol. 2017;130(6):1319–26. doi:10.1097/AOG.0000000000002357.
- Jones EJ, Hernandez TL, Edmonds JK, Ferranti EP. Continued disparities in postpartum follow-up and screening among women with gestational diabetes and hypertensive disorders of pregnancy: a systematic review. J Perinat Neonatal Nurs. 2019;33(2):136–48. doi:10.1097/JPN.0000000000000399.
- Centers for Medicare and Medicaid Service. Improving access to maternal health care in rural communities. 2019 [accessed 2020 July 21]. https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/rural-health/09032019-Maternal-Health-Care-in-Rural-Communities.pdf.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(782–786):782–86. doi:10.1192/bjp.150.6.782.
- Morgan J Normal pregnancy symptoms: here’s what to expect. 2017 [accessed 2020 September 18]. https://utswmed.org/medblog/normal-pregnancy-symptoms/.