Abstract
Purpose: The aim was to investigate, describe and analyse speech characteristics, intelligibility, orofacial function and co-existing neurodevelopmental symptoms in children with SSD of unknown origin, persisting after six years of age.
Method: The study included 61 children with SSD (6–17 years) of unknown origin, referred for a speech and oral motor examination. The severity of SSD was estimated using Percentage Consonants Correct (PCC) and Percentage Vowels Correct (PVC) and assessments of resonance based on Swedish Articulation and Nasality Test (SVANTE). Orofacial function was screened using the Nordic Orofacial Test-Screening (NOT-S). Parents completed the Intelligibility in Context Scale (ICS) and a questionnaire including questions about heredity, medical and neurodevelopmental conditions, and speech development.
Result: SSD varied according to PCC (8–95%) and PVC (55–100%) measurements. Percentages of co-occurring disorders included: 51% resonance deviations, 90% intelligibility issues, and 87% orofacial difficulties. The most affected orofacial domains were “Chewing and swallowing” (41%), “Masticatory muscles and jaw function” (38%) and “Sensory function” (38%). The majority (64%) had co-existing dysfunctions relating to general motor and neurodevelopmental disorders.
Conclusion: Children with persistent SSD are at risk for orofacial dysfunction, general motor difficulties and other neurodevelopmental disorders and therefore should be screened for co-occurring disorders.
Introduction
Speech Sound Disorders (SSD) are relatively common in the developing child. The prevalence of reported SSD changes depending on the definition of SSD and age (Shriberg, Tomblin, & McSweeny, Citation1999). Shriberg et al. (Citation1999) report a variation in the occurrence of SSD between two and 13% in children aged six to eight years. Wren, Miller, Peters, Emond, and Roulstone (Citation2016) report a prevalence of 3.6% of persistent SSD in eight-year-old children. Speech difficulties in children rarely exist in isolation (Eising et al., Citation2018, Gillberg, Citation2010). A shared genetic foundation may explain complex neurodevelopment brain disorders such as speech- and language disorders, Childhood Apraxia of Speech (CAS), reduced cognitive function and deficits in motor development (Eising et al., Citation2018). In a study of twins, children with both speech and language disorders were also at the greatest risk for fine motor disorders (Bishop, Citation2002).
Multiple studies have investigated gross- and fine-motor skills in children with SSD and report a relationship between poor motor skills and speech and language impairments (Hill, Citation2001; Visscher, Houwen, Scherder, Moolenaar, & Hartman, Citation2007). Redle et al. (Citation2015) reported that children with SSD exhibited poorer oral- and fine-motor skills compared with typically developing children. Using functional magnetic resonance imaging (fMRI), they found that children with persistent speech disorders displayed an over-activation in the cerebellum during motor tasks. This was assumed to be related to a subtle abnormality in the motor neural circuitry which could affect fine-motor praxis. Kent (Citation2015) suggests that co-existing language and motor impairments should be seen as co-occurring symptoms of a common underlying disorder rather than a causal link.
Persistent SSD
Typical speech development requires intact motor, cognitive and linguistic skills and problems in any area can lead to speech impairment (Wren et al., Citation2016). SSD is used as an umbrella term for speech sound difficulties of both known and unknown origin. Children with SSD can have difficulty with articulation, phonology or motor speech, including CAS (International Expert Panel on Multilingual Children’s Speech, Citation2012). The age at which SSD is regarded as persistent varies in the literature. Wren et al. (Citation2016) includes children from eight years of age in the term “persistent SSD”. They also exclude children with the most common distortions from the definition.
It is suggested that persistent overt speech errors are correlated with impaired motor skills (Lewis et al., Citation2015). However, phonological processing difficulties have also been described in children with persistent SSD (Preston & Edwards, Citation2007). In a longitudinal study, Wren et al. (Citation2016) found that early motor skill deficits, such as weak sucking at four weeks of age and a history of suspected motor co-ordination difficulties, were correlated to persistent SSD at eight years of age. The most common persistent speech difficulties are distortion errors that affect intelligibility, sometimes to a minor extent (Flipsen, Citation2015).
Orofacial dysfunction and speech sound development
Deviant or delayed general development may be associated with orofacial dysfunction (Bergendal, Bakke, McAllister, Sjögreen, & Åsten, Citation2014). Chewing and swallowing, saliva control, nose breathing, sensory function, facial expression and speech are all vital orofacial functions. A well-coordinated sensory-motor function of the mimic muscles, lips, jaw and tongue is important for eating, drinking, swallowing, articulation and saliva control (Martinez & Puelles, Citation2011). Typically developing children have good oral motor control before the age of four (Martinez & Puelles, Citation2011), but the development continues and is refined throughout childhood. In speech the co-ordination of a number of muscles and neural subsystems is necessary to be able to produce intelligible speech without distortions and with the dynamic and temporal requirements for typical voice and resonance (Smith & Zelaznik, Citation2004).
Studies of the relationship between language development and oral motor development in typically developing children indicate a relationship between language and motor skills (Alcock, Citation2006). The development of speech sounds follows oral motor development (Green, Moore, Higashikawa, & Steeve, Citation2000). Less motorically challenging sounds thus develop at an earlier stage (Lohmander, Lundeborg, & Persson, Citation2017). Most oral motor skills relevant to speech have reached an adult-like pattern at around 14 years of age (Smith & Zelaznik, Citation2004).
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), proposes that the most frequently misarticulated sounds, the so-called “late eight” (/l/, /r/, /s/, /ʃ/, /ʒ/, /ð/, /θ/, /z/), should be produced correctly before the age of eight years (American Psychiatric Association, Citation2013). In Swedish, all consonants, including /r/ and /s/ sounds, are expected to be established by the age of six years (Blumenthal & Lundeborg Hammarström, Citation2014), similar to English-speaking five-year olds (Dodd, Holm, Hua, & Crosbie, Citation2003). Most vowels are expected to be established at the age of three years and, at four years of age all vowels in Swedish are expected to be established (Blumenthal & Lundeborg Hammarström, Citation2014). The Swedish speech sound system consists of 18 different consonants and nine distinct vowels that can be pronounced both long and short (McAllister, Citation1998). For vowels, there is a quality difference between the long and short realisation.
Overlap of co-existing motor and neurodevelopmental disorders
The Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations (ESSENCE) concept, developed by Gillberg (Citation2010), offers a model describing the interaction between different neurodevelopmental disorders. Gillberg proposes that specific disorders, such as language disorders, Attention Deficit Hyperactivity Disorder (ADHD) and Developmental Co-ordination Disorder (DCD), should not be seen as separate but instead as a combination of symptoms that largely overlap. Miniscalco, Nygren, Hagberg, Kadesjö, and Gillberg (Citation2006) found that, in a group of children identified with language problems through a child health screening at 2.5 years of age in Sweden, 72% had neuropsychiatric or learning disorders at the age of seven years (Miniscalco et al., Citation2006). DCD is regarded as one of the most common neurodevelopmental disorders and is thought to be highly underdiagnosed (Gillberg, Citation2010). In the study by Miniscalco et al. (Citation2006), a third of the children with early detected language disorders met the criteria for DCD at seven years of age.
Study aims
Based on the authors’ clinical experience of working with children with SSD and the results of earlier studies (Bishop, Citation2002; Eising et al., Citation2018; Hill, Citation2001; Lewis et al., Citation2015; Redle et al., Citation2015; Visscher et al., Citation2007), the hypothesis behind the present study was that children with persistent SSD of unknown origin may have co-occurring orofacial dysfunction and that the speech difficulties rarely exist as isolated symptoms but rather in a cluster of co-existing neurodevelopmental disorders (ADHD, Attention Deficit Disorder (ADD), Autism Spectrum Disorder (ASD) and DCD/general motor difficulties) in accordance with the ESSENCE-framework and that the severity of SSD could not be explained by age alone.
The aims of the present study of children with SSD of unknown origin, persisting after the age of six years were:
To investigate speech characteristics, intelligibility, and orofacial functions, including chewing and swallowing, saliva control, nose breathing, oral sensory function, and facial expression.
To describe the occurrence of parent reported co-existing motor and neurodevelopmental disorders.
To analyse the relationship between speech characteristics, orofacial functions, parent reported co-existing motor and neurodevelopmental disorders and age and sex.
Method
Participants
The inclusion criteria for the present study were children with SSD persisting after the age of six. This age range was selected as Swedish-speaking children are expected to manage all Swedish speech sounds at the age of six (Blumenthal & Lundeborg Hammarström, Citation2014). The exclusion criteria were moderate to severe intellectual disability, cerebral palsy and/or severe Autism Spectrum Disorder. Sixty-two consecutive patients who were referred to a national orofacial resource centre for a speech and oral motor examination in 2014–2016 and met the inclusion criteria were offered to participate in the study. In total, 61 children participated, aged 6:0–16:7 years (mean age 8:5), 14 girls and 47 boys. Thirty-six (59%) children were below the age of 8:0 years of age (See Supplementary Table I). Referrals came from speech-language pathologists (SLPs) (n = 47), physicians (n = 7), school health services (n = 6) and self-referral (n = 1). The reasons for referral were requesting an oral motor examination and/or a second opinion, as the child had not improved from previous speech-language interventions.
All participants were children with SSD of unknown origin where speech difficulties had not resolved at the age of six years, despite long-term contact with an speech-language pathologist (SLP). The median age for the first SLP visit was 4:0 years (2:0–7:3 years). Thirteen per cent of the parents were unable to remember how old their child was at his/her first appointment with an SLP. Almost all children in Sweden participate in a nurse-administered general health screening programme at child health-care centres at 2:6–3 years and at four years of age. If a child is identified as having speech, language and communication difficulties at this screening, a referral is sent to the local speech-language pathology clinic for further assessments (Fäldt, Nordlund, Holmqvist, Lucas, & Fabian, Citation2018).
Five participants were raised in bilingual homes but had Swedish as their first language and two children were adopted internationally at 2:6 and three years of age. Three sibling pairs were included. All participants but one were following the regular curriculum for compulsory schooling.
Study design
An SLP (ÅM) with 20 years’ experience of working with assessment and treatment of children with SSD and oral sensory-motor disorders performed the data collection and all the assessments in a clinical setting. Speech production was assessed using the Swedish Articulation and Nasality Test (SVANTE) (Lohmander et al., Citation2017). Orofacial function was screened using the Nordic Orofacial Test-Screening (NOT-S) (Bakke, Bergendal, McAllister, Sjögreen, & Åsten, Citation2007). Both examinations were video recorded (Canon Legria HF S11; Canon, Japan) with an external microphone (Canon DM-100; Canon, Japan). In addition, the speech assessment was audio recorded (Tascam HD-P2; Tascam, USA) using a stereo microphone (SONY ECM-MS957; Sony, Japan). The parents filled out the Intelligibility in Context Scale (ICS) (McLeod, Harrison, & McCormack, Citation2012) and a background questionnaire prior to the visit.
Consonant and vowel production
SVANTE is a validated test for the assessment of speech production, including consonant proficiency and consonant errors (Lohmander et al., Citation2017). It consists of 86 single words (48 monosyllabic and 38 disyllabic) elicited via pictures. It also includes sentence repetition to assess connected speech. All Swedish consonants are included, and most occur in three possible realisations in the initial, medial and final position. The consonants /ɕ/ and /h/ only exist in initial positions and/ ŋ /only exists in medial and final positions according to Swedish phonotaxis. An analysis of the speech material was made in accordance with instructions (Lohmander et al., Citation2017). The outcome measurements were consonant proficiency (Percentage Consonants Correct (PCC)), Percentage Vowels Correct (PVC) and consonant inventory. A narrow phonetic transcription of single words was performed from the audio recordings. The consonants and vowels were scored as correct or not correct, according to instructions in Shriberg et al. (Shriberg, Austin, Lewis, McSweeny, & Wilson, Citation1997). When scoring PCC, all distortions were rated as incorrect, but all Swedish allophones of /r/ were rated as correct. Typically developing five and seven-year-old Swedish children have a mean PCC of 96.3 and 97.8% on the SVANTE-test, respectively (Lohmander et al., Citation2017). At 19 years, the mean PCC is almost 100% (99.4). For the consonant inventory, a 90% threshold was used in accordance with Blumenthal and Lundeborg Hammarström (Citation2014). A consonant phoneme is regarded as established if it is correctly produced in 90% or more possible realisations. SVANTE is originally not designed for assessing vowels, but it includes all Swedish vowels, except for /ʏ/. Most vowels are realised several times but /I/, /y:/, /ʊ/, /oe:/, and /oe/ only exist once. Typically developing children have a 100% PVC from the age of four years (Blumenthal & Lundeborg Hammarström, Citation2014).
Resonance
Recordings of sentence repetitions in SVANTE were used to assess resonance. Nasality variables were rated on a four-point ordinal scale (no, mild, moderate or severe deviance), according to Lohmander et al. (Citation2017). The parameters that were assessed were hypernasality, hyponasality, audible nasal air leakage and reduced pressure on consonants. The parameter mixed/varying nasality was added to the original scale. A blinded second assessor and SLP listened to 19 (31%) of the recordings and rated resonance features.
Intelligibility
The Intelligibility in Context Scale (ICS) is a questionnaire measuring functional intelligibility of children with SSD (McLeod et al., Citation2012). It consists of seven items where parents rate the degree of their child’s intelligibility in different contexts in everyday life on a five-point scale. Earlier studies have reported a mean score of 4.49 for typically developing children and 3.97 for children with SSD, aged three to six years (Neumann, Rietz & Stenneken, Citation2017). According to McLeod et al. (Citation2012), the ICS has been found to correlate positively with other established and valid measurements of speech severity, such as PCC. The ICS questionnaire has been translated into Swedish, but to date no norm data have been published. Two families did not complete the ICS questionnaire.
Orofacial function
The NOT-S is a validated screening test developed to assess orofacial function (Bakke et al., Citation2007). The NOT-S is regarded as a comprehensive test that covers several orofacial functions. It consists of a structured interview (NOT-S Interview) and a clinical examination (NOT-S Examination). The screening is divided into 12 domains (six domains in the interview part and six in the examination part) addressing “Sensory function”, “Breathing”, “Habits”, “Chewing and swallowing”, “Drooling” and “Dryness of the mouth” in the structured interview and “Face at rest”, “Nose breathing”, “Facial expression”, “Masticatory muscles and jaw function”, “Oral motor function” and “Speech” in the clinical examination. Each domain includes one to five items depending on complexity. The scoring is based on “yes” or “no” and the criteria are well defined in the manual. One or more positive answers in a domain generate a “dysfunction score”. The maximum NOT-S score is 12, one score for each domain. Typically developing children (>5 years) have a mean score of <2 (McAllister & Lundeborg, Citation2013). In the present study, interviews were conducted with the parents of participants aged <12 years and with participants >12 supported by parents.
Co-existing motor and neurodevelopmental disorders
A questionnaire was sent to the families (n = 61) prior to the first visit to collect information on medication, general disabilities (hearing, vision, epilepsy, presence of neurodevelopmental condition, general motor difficulties), a family history of speech and language disorders and delayed speech and language development. The questionnaire for one child was not returned despite two reminders.
Reliability
The percentage of point-by-point exact comparison was used to assess inter- and intra-rater agreement (). For calculations of the intra- and inter-rater reliability of consonant and vowel production (PCC, PVC), 23% of the recordings from the speech assessments and 31% of the recordings of resonance and NOT-S assessments were randomly selected and reassessed. Inter- and intra-rater agreement varied between good and excellent (). Three items were not possible to assess from the video recordings alone and were therefore excluded from inter- and intra-reliability assessment (nose breathing, palpation of the jaw muscles and intra- oral examination of the soft palate). Three assessors, all SLPs participated, one for consonant and vowel production, one for resonance and one for the NOT-S assessments. They all had research experience and were blinded to the study objectives and participant characteristics.
Table I. Median and range of intra- and inter-reliability calculated using the percentage of point-by-point agreement of the PCC, PVC, resonance and NOT-S test in children with SSD (n = 61).
Statistical analysis
The data were analysed using the Statistical Package for the Social Sciences (SPSS statistics 22). The level of significance was set at p < 0.05 throughout. Descriptive statistics were used for the background features, age and sex of the participants. Non-parametric tests were used for comparisons due to non-normal distributions, Spearman’s rho was used for correlation analysis (age, PCC, PVC, number of established consonants, ICS) and the Mann-Whitney U-test was used for analyses of the significances of two independent samples. Significance tests were conducted on differences in PCC and PVC between boys and girls, between participants with and without a confirmed neurodevelopmental disorder, between participants with and without orofacial dysfunction, differences in NOT-S results between boys and girls and between participants with and without a confirmed neurodevelopmental disorder. Bivariate analyses were performed to determine the parameters that could be expected to influence speech production and orofacial function. A linear regression analysis, using the enter option, was conducted to examine the predictive ability of the independent variables, age and NOT-S, on the dependent variables, PCC and PVC respectively.
Ethical considerations
The study was approved by the regional ethical review board in Gothenburg. All the participants received both oral and written information about the study. The children received a simplified version of the information also including pictorial support. All the children were involved in the discussion about their participation, but younger children were involved to a lesser degree than adolescents. The parents signed informed consent to their child’s participation before any assessments took place.
Result
Speech characteristics, intelligibility, and orofacial functions
Speech characteristics – consonant and vowel production
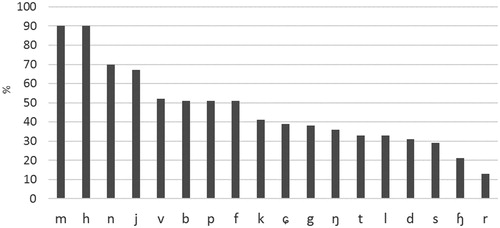
Impaired consonant production assessed by PCC varied from 8 to 95 (median 71, mean 66 (SD 22.1)). Vowel production assessed by PVC varied from 55 to 100 (median 95, mean 91 (SD 10.1)). Five participants had a PVC of 100 and six had a PVC of 99. The assessment of established consonants showed that the motorically challenging sounds in Swedish (/r/, /ɧ/, /ɕ/, /s/, /l/) were affected the most, but /t/ and /d/ were also among the less established (). No single consonant was fully established in all participants. The older participants (10–17 years) had a larger number of established consonants (see Supplementary Table II).
Speech characteristics – resonance
Thirty-one participants (51%) were found to have deviant resonance, according to a perceptual evaluation. Sixteen (26%) of those were assessed as having hypernasality, 10 (16%) hyponasality and five (8%) mixed/varying nasality. According to the four-point ordinal scale, 20 participants had mild and 11 had moderate/severe deviations. Eight participants with hypernasality were also assessed as having audible nasal air leakage. In addition, eight were assessed as having reduced pressure on consonants, two in combination with hypernasality and one in combination with hyponasality.
Intelligibility
According to the ICS questionnaire, filled out by the parents, intelligibility was affected in 90% (53/59) of the children. The mean ICS score was 3.72 (SD 0.60).
Orofacial function.
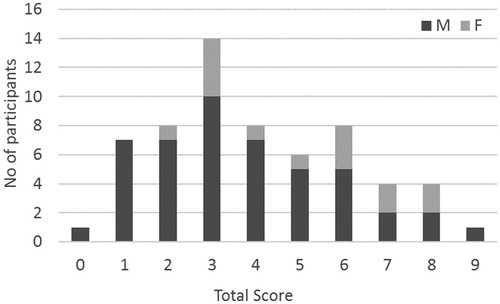
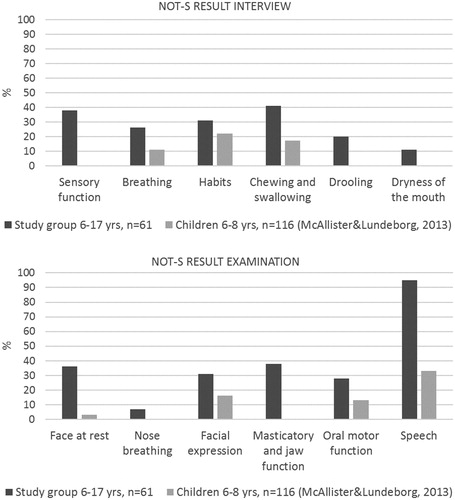
The majority (87%) displayed difficulties with orofacial functions in more domains than expected for their age (total NOT-S score ≥2). Eight participants (13%) were considered to have typical orofacial function related to age (total NOT-S score <2). The variation within the group was large and ranged from a total NOT-S score of 0–9 (). The most affected domains apart from “Speech” were “Chewing and swallowing” (41%), “Masticatory muscles and jaw function” (38%), “Sensory function” (38%) and “Face at rest” (36%) ().
Figure 3. Distribution of NOT-S scores in different domains in children with SSD (n = 61). The results are compared with 116 typically developing children, aged six to eight years, from McAllister and Lundeborg (Citation2013).
Co-existing motor and neurodevelopmental disorders
Co-existing gross-motor difficulties and confirmed neurodevelopmental disorders, such as ADHD, and ASD, were common (). A family history of speech and language disorders was reported in 40 (67%) participants. In all, the parents of 39 (64%) participants reported one or more co-existing symptoms (). Motor difficulties were reported in 17 participants (28%) and confirmed or suspected hypermobility in joints was reported in 25 (42%) participants. A total of 34 (56%) participants reported motor difficulties and/or confirmed or suspected hypermobility in joints.
Table II. Parent-reported background information collected from a questionnaire in children with SSD (n = 60).
Relationship between variables
Age correlated significantly with PCC, the number of established consonants, PVC, the ICS score and NOT-S examination (). The ICS score correlated with all the speech parameters (PCC, established consonants, PVC) and all the speech measurements correlated with each other (). NOT-S examination correlated with all speech measurements but intelligibility ().
Table III. Correlations (Spearman’s rho) between age, speech parameters, intelligibility and results from NOT-S testing in children with SSD (n = 61).
Participants without orofacial dysfunction (n = 8) (total NOT-S score <2) differed significantly from participants with orofacial dysfunction (n = 53) (total NOT-S score ≥2) on PVC (U = 104, z = –2.314, p = 0.021) but not on the other speech parameters (PCC, number of established consonants, resonance).
Comparisons between boys (n = 47) and girls (n = 14) showed that there was no significant difference regarding PCC (U = 288, z = –0.704, p = 0.482) and PVC (U = 283.5, z = –0.783, p = 0.434). However, girls scored higher than boys on the NOT-S (U = 209, z = –2.081, p = 0.037).
There was no significant difference between children with (n = 9) or without (n = 51) a confirmed neurodevelopmental disorder regarding PCC (U = 216.5, z = –0.356, p = 0.722), PVC (U = 196, z = –0.775, p = 0.438) or resonance (U = 216.5, z = –0.411, p = 0.681). Children with a confirmed neurodevelopmental disorder obtained significantly higher scores on the total NOT-S (U = 201, z = –0.691, p = 0.035). The differences were mainly found in the interview part (U = 110, z = –2.583, p = 0.010) in the domains of “Sensory function” (U = 93.5, z = –3.403, p = 0.001), “Chewing and swallowing” (U = 133, z = –2.411, p = 0.016) and “Drooling” (U = 166, z = –2.008, p = 0.045).
Children with parent reported motor difficulties and/or confirmed or suspected hypermobility in joints (n = 34) had resonance deviations to a higher degree compared with children without parent- reported motor difficulties (n = 26) (U = 315, z = –2.414, p = 0.016). No other speech parameters (PCC, PVC, number of established consonants) differed between the two groups. Children with parent- reported motor difficulties scored higher than children without motor difficulties on the total NOT-S (U = 258.5, z = –2.943, p = 0.003). The domains that differed the most were “Chewing and swallowing” (U = 304.5, z = –2.633, p = 0.008) and “Drooling” (U = 358, z = –2.130, p = 0.033) in the NOT-S interview and “Masticatory and jaw function” (U = 331.5, z = –2.205, p = 0.027) in the NOT-S examination.
A linear regression analysis was conducted to further investigate the association between PCC and orofacial dysfunction and PVC and orofacial dysfunction. PCC and PVC were selected as speech characteristic measurements, as both correlated highly significantly with both the number of established consonants and intelligibility as measured with the ICS. NOT-S examination scores and age together explained 25% of the variability in PCC (R2 adjusted = 0.250, p = 0.003) and 21.8% of the variability in PVC (R2 adjusted = 0.218, p = 0.001). Age alone explained 13.7% of the variability in PCC and 6.7% of the variability in PVC (See Supplementary Tables III and IV).
Discussion
The results showed that orofacial dysfunction was common in this group of children with SSD of varying severity, persisting after the age of six years. These results add to the growing body of evidence relating to the relationship between speech development and oral sensory-motor development in children with SSD. Difficulties with masticatory and jaw function were the most common oral motor difficulties in the study group. The orofacial muscles are used in a variety of complex functions (Kent, Citation2015). There is an ongoing discussion about how this overlap of functions and muscle control should be interpreted. Some argue that oral motor difficulties, language and speech difficulties should be interpreted as symptoms of the same underlying disorder (Kent, Citation2015). Others argue that speech is specific to the domain of linguistic expression and that those functions cannot be compared (Ziegler & Ackermann, Citation2013). The overlap of different symptoms in the present study group, such as SSD, parent reported general motor difficulties, hypermobility in joints and neurodevelopmental disorders (including ASD and ADHD), connects to the theory of ESSENCE (Gillberg, Citation2010). According to the ESSENCE concept, different symptoms are seen as combinations of symptoms rather than separate disorders and these symptoms could share biological and genetic markers.
Speech characteristics and intelligibility
Speech production and intelligibility were affected in all participants but to varying degrees. The speech difficulties included both impaired consonant and vowel production and deviant resonance and together they influenced intelligibility to a large degree. There were significant correlations between consonant and vowel production and age, but age alone did not explain the variability in consonant and vowel production. No single consonant was established in all participants. Not even the earliest developed speech sounds were fully established, considering the age range. All the participants had difficulties with speech production and the phonetic placement of one or more speech sounds. Vowels were affected in the majority of the participants. Accurate vowel production is considered to be present already at an early age in typically developing children. Vowel errors are highly associated with speech motor planning difficulties such as CAS (Iuzzini-Seigel & Murray, Citation2017). In the present study there was a significant difference between the participants with and without orofacial dysfunction regarding vowel production, where participants with orofacial dysfunction obtained lower scores on PVC.
In addition to difficulties with consonant and vowel production, many participants also exhibited deviant resonance. Some of the participants had low-pressure consonant production. The deviations in resonance could be related to lack of energy, low muscle tone and low subglottal and oral pressure during speech. In a study assessing adolescents with persistent SSD, around 25% had “abnormal resonance” (Lewis et al., Citation2015). The authors suggest “a motor-based articulatory deficit in addition to the phonological processing deficits” based on the co-occurrence of abnormal resonance and oral motor imitation difficulties in the participants. There was a significant difference between participants with and without parent reported motor difficulties regarding resonance, where participants with motor difficulties displayed deviant resonance to a higher degree.
In the present study, intelligibility was assessed by a parental questionnaire (ICS). The mean ICS score was lower than that in an earlier study of younger children (3–6 years) with SSD (Neumann et al., Citation2017), which indicates that some of the participants in the present study had extensive difficulties with intelligibility. The ICS score and the PCC score correlated, which is in accordance with earlier studies (McLeod et al., Citation2012).
All participants were schoolchildren who had been in contact with an SLP for assessments and interventions over a period of several years. However, the speech difficulties remained, despite intervention. There is no agreed-upon classification system for SSD (Waring & Knight, Citation2013) and differential diagnostics of motor speech disorders are known to be difficult due to co-occurring symptoms (Iuzzini-Seigel & Murray, Citation2017). The difficulties with vowels, motorically challenging speech sounds and deviations in resonance could all be signs of underlying motor speech difficulties
Orofacial function
The NOT-S was used to assess orofacial function. This was the first time NOT-S had been used to assess a group of children with SSD. NOT-S covers several orofacial functional domains and is regarded as a comprehensive test, including several aspects of orofacial function. This could explain why the majority of the children with persistent SSD were identified as having an orofacial dysfunction. Apart from speech, difficulties with “Chewing and swallowing”, “Masticatory muscles and jaw function”, “Sensory function” and “Face at rest” were the most affected domains. This matches the theory that jaw muscles are important for speech and oral motor development (Green et al., Citation2000). The jaw muscles may also be related to the lack of saliva control (drooling) observed in the present group. When controlling for age, the strength of the correlation between NOT-S examination and PCC and PVC increased.
Co-existing motor and neurodevelopmental disorders
More than half the parents reported that their child had general motor difficulties (). The results indicate that SSD, orofacial dysfunction and motor difficulties often co-occur. Forty-two per cent reported hypermobility in joints in combination with a history of gross-motor difficulties, which is in accordance with previous studies of hypermobility in joints and poor motor co-ordination (Adib, Davies, Grahame, Woo, & Murray, Citation2005; Kirby & Davies, Citation2007). Adib et al. (Citation2005) found that around 14% reported a diagnosis of speech and learning difficulties in a group of children with joint hypermobility syndrome. In the present study, nine of the 14 girls (64%) reported confirmed or suspected hypermobility in joints, which was almost twice as many as in the boys. Hypermobility in joints is more common in females than in males and it is a common symptom in many genetic syndromes, such as Down syndrome, Williams syndrome, Ehlers-Danlos syndrome, Marfan syndrome and Fragile X, among others (Adib et al., Citation2005). The large proportion of participants with motor difficulties is also in accordance with previous studies. Visscher et al. (Citation2007) reported that children with speech and language disorders had more motor difficulties than children with only language disorders.
A larger proportion than expected (15%) () reported that they were not right- or left-handed. Nor were they truly ambidextrous, rather their handedness was unclear – so-called mixed handedness (Rodriguez et al., Citation2010). Mixed handedness exists in about 1% of the population (Rodriguez et al., Citation2010) and has been suggested as a clinical marker for early detection of children at risk of neurodevelopmental disorders.
All the participants but one were in the regular curriculum for compulsory schooling. Fifteen per cent had a confirmed neurodevelopmental disorder. In the questionnaire, the parents were only able to answer “yes” or “no” to the question, but several parents added comments such as “we think that he has ADHD” or “we are waiting for an assessment but don’t know yet”. These answers were not included in the statistics but indicate that the number of participants with neurodevelopmental disorders could be higher than presented. However, the results show that children with a confirmed neurodevelopmental disorder did not differ from those without regarding speech impairment.
The genetics behind speech and language disorders constitute a growing field of research and recent findings point to a shared genetic foundation for several neurodevelopmental disorders, such as speech and language disorders, reduced cognitive function and deficits in motor development (Eising et al., Citation2018). The majority of the participants had a known heredity for speech and language difficulties and three pairs of siblings participated. This is in agreement with the theories of a genetic cause behind SSD.
Limitations
The study comprised children referred for a speech and oral motor examination. This selection may have influenced the results. However, the orofacial dysfunction and the suspected motor speech disorder had not been addressed until referral, despite the participants’ age and long-term contact with an SLP. The lack of progress in intervention was often the cause of referral. In this study, the inclusion criteria were generous, resulting in a heterogenic yet clinically representative group. The study group reflects an ecologically valid clinical sample.
The majority of participants (59%), were between six and eight years of age. This could influence the results, as younger children often have more severe speech difficulties. Persistent SSD has been defined differently in different studies and, in several studies, only children over the age of eight years are included in the definition (Wren et al., Citation2016; Flipsen, Citation2015). In the present study we included children from six years as all Swedish speech sounds are expected to be established at the age of six years. Children in Sweden also start school at six years of age and in some geographical areas they no longer receive service from the local speech-language pathology clinic- at that point. This could also be the reason why more children in the younger age groups were referred for assessment. Age correlated with the PCC, PVC, ICS score and the NOT-S examination which indicates that the younger children had more severe difficulties. However, the linear regression analysis revealed that, when controlling for age, age was not the only explanation of the results on the PCC and PVC. It would have been preferable to have a more evenly distributed study group in terms of age, but this was not possible, as a consecutive approach was used to reflect common clinical populations. The results relating to age should therefore be interpreted with some caution.
There was also an imbalance between the number of male and female participants, where only 23% were female. Males are often in majority in studies of congenital speech and language disorders. Based on a national database in the United Kingdom, Dockrell and colleagues (Citation2014) reported higher odds (2.5) of “speech, language and communication needs” in boys than in girls. The cohort study by Wren et al. (Citation2016) also reported a higher prevalence of boys with persistent SSD (odds ratio 1.6).
NOT-S is a screening test and mild oral motor impairments may therefore have been undetected. The same is true for the speech production test, SVANTE, consisting mostly of monosyllabic and disyllabic words including few clusters. It would have been beneficial to use more complex speech material, especially among the older participants. On the other hand, none of the participants obtained an age-appropriate PCC result and no single speech sound was established in all participants.
Background data on hearing, vision, cognition and general motor function were collected using a parental questionnaire. The findings would have been more reliable if these variables had been systematically tested. Language assessments would also have added valuable knowledge. To fully explore the correlation between language impairment, speech characteristics and orofacial function a more in-depth analysis of speech and language is needed. Moreover, as it was common to have a family history of speech and language disorders in the study group, this could justify further genetic analysis.
The sample size was based on a convenience procedure. Data were collected during a two- year period and included all individuals referred to the clinic that met the inclusion criteria. For practical reasons and due to the time aspects, the study group could not be extended. This may reflect a limitation of the study.
Clinical implications
Oral sensory-motor difficulties may affect many aspects of communication, such as facial expression, voice and resonance. They may also affect eating, saliva control and dental occlusion. Resonance deviations also need to be taken into account in the clinical work, as these difficulties affect intelligibility and could indicate oral sensory-motor deviations. When orofacial functions are affected in children with SSD, a sensory-motor perspective should be included when considering intervention strategies. There is a growing body of evidence for treating children with motor speech disorders with treatment methods based on principles of motor learning (Maas, Gildersleeve-Neumann, Jakielski, & Stoeckel, Citation2014).
Based on the occurrence of co-existing symptoms in children with speech and language disorders, a multi-professional approach is necessary to ensure appropriate care. Clinicians working with children with SSD need to have knowledge and awareness of this co-occurrence. The results of this study can be interpreted as a need for further screening for co-existing general motor difficulties and neurodevelopmental disorders. An assessment of orofacial function is also important when describing the characteristics of children with SSD and it could add valuable information in differential diagnostics and in future genetic testing.
Conclusion
Orofacial dysfunction and general motor difficulties were common in this group of children with persistent SSD. The results provide an insight into the characteristics of co-existing orofacial dysfunction in children with persistent SSD and demonstrate that consonant and vowel production could not be explained by age alone. These children should therefore be screened for co-existing orofacial dysfunction. The use of a comprehensive and reliable screening test for orofacial function, including chewing and jaw function, sensory function, and face at rest, such as the NOT-S, is relevant in the assessments of children with persistent SSD.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Supplementary material
Supplemental data for this article can be accessed at http://dx.doi.org/10.1080/17549507.2019.1701081.
Supplemental table I
Download MS Word (13 KB)Supplemental table II
Download MS Word (12.9 KB)Supplemental table III
Download MS Word (19.4 KB)Supplementary table IV
Download MS Word (13.1 KB)Acknowledgements
The authors would like to thank the children who participated in the study, together with their families. Special thanks to SLPs AnnaKarin Larsson and Ann Nordberg for their contribution with assessments of resonance and speech-sound production. The authors also thank Professor Magnus Hakeberg for statistical advice.
Additional information
Funding
References
- Adib, N., Davies, K., Grahame, R., Woo, P., & Murray, K.J. (2005). Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology (Oxford, England), 44, 744–750. doi:10.1093/rheumatology/keh557
- Alcock, K. (2006). The development of oral motor control and language. Downs Syndr Res Pract, 11, 1–8. doi:10.3104/reports.310
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Retrieved from 10.1176/appi.books.9780890425596
- Bakke, M., Bergendal, B., McAllister, A., Sjögreen, L., & Åsten, P. (2007). Development and evaluation of a comprehensive screening for orofacial dysfunction. Swedish Dental Journal, 31, 75–84.
- Bergendal, B., Bakke, M., McAllister, A., Sjögreen, L., & Åsten, P. (2014). Profiles of orofacial dysfunction in different diagnostic groups using the Nordic Orofacial Test (NOT-S) – A review. Acta Odontologica Scandinavica, 72, 578–584. doi:10.3109/00016357.2014.942874
- Bishop, D.V. (2002). Motor immaturity and specific speech and language impairment: Evidence for a common genetic basis. American Journal of Medical Genetics, 114, 56–63. doi:10.1002/ajmg.1630
- Blumenthal, C., & Lundeborg Hammarström, I. (2014). LINUS – Linköpingsundersökningen. – [in Swedish]. A phonological test for children from 3 years of age. Retrieved from http://liu.divaportal
- Dockrell, J., Lindsay, G., Roulstone, S., & Law, J. (2014). Supporting children with speech, language and communication needs: An overview of the results of the Better Communication Research Programme. International Journal of Language and Communication Disorders, 49, 543–557. doi:10.1111/1460-6984.12089
- Dodd, B., Holm, A., Hua, Z., & Crosbie, S. (2003). Phonological development: A normative study of British English-speaking children. Clinical Linguistics & Phonetics, 17, 617–643. doi:10.1080/0269920031000111348
- Eising, E., Carrion-Castillo, A., Vino, A., Strand, E.A., Jakielski, K.J., Scerri, T.S., … Fisher, S.E. (2018). A set of regulatory genes co-expressed in embryonic human brain is implicated in disrupted speech development. Molecular Psychiatry, 24, 1065–1078. doi:10.1038/s41380-018-0020-x
- Fäldt, A., Nordlund, H., Holmqvist, U., Lucas, S., & Fabian, H. (2018). Nurses’ experiences of screening for communication difficulties at 18 months of age. Acta Pædiatrica, 108, 1651–2227. doi:10.1111/apa.14557
- Flipsen, P. Jr. (2015). Emergence and prevalence of persistent and residual speech errors. Seminars in Speech and Language, 36, 217–223. doi:10.1055/s-0035-1562905
- Gillberg, C. (2010). The ESSENCE in child psychiatry: Early symptomatic syndromes eliciting neurodevelopmental clinical examinations. Research in Developmental Disabilities, 31, 1543–1551. doi:10.1016/j.ridd.2010.06.002
- Green, J.R., Moore, C.A., Higashikawa, M., & Steeve, R.W. (2000). The physiologic development of speech motor control: Lip and jaw coordination. Journal of Speech, Language, and Hearing Research, 43, 239–255. doi:10.1044/jslhr.4301.239
- Hill, E.L. (2001). Non-specific nature of specific language impairment: A review of the literature with regard to concomitant motor impairments. International Journal of Language and Communication Disorders, 36, 149–171. doi:10.1080/13682820010019874
- International Expert Panel on Multilingual Children’s Speech Multilingual children with speech sound disorders (2012). Position paper. Research Institute for Professional Practice, Learning and Education (RIPPLE), Charles Sturt University, Bathurst, NSW, Australia. Retrieved from: http://www.csu.edu.au/research/multilingual-speech/position-paper
- Iuzzini-Seigel, J., & Murray, E. (2017). Speech assessment in children with childhood apraxia of speech. Perspectives of the ASHA Special Interest Groups, 2, 47–60. doi:10.1044/persp2.SIG2.47
- Kent, R.D. (2015). Nonspeech oral movements and oral motor disorders: A narrative review. American Journal of Speech-Language Pathology, 24, 763–789. doi:10.1044/2015_AJSLP-14-0179
- Kirby, A., & Davies, R. (2007). Developmental coordination disorder and joint hypermobility syndrome–overlapping disorders? Implications for research and clinical practice. Child: Care, Health and Development, 33, 513–519. doi:10.1111/j.1365-2214.2006.00694.x
- Lewis, B.A., Freebairn, L., Tag, J., Ciesla, A.A., Iyengar, S.K., Stein, C.M., … Taylor, H.G. (2015). Adolescent outcomes of children with early speech sound disorders with and without language impairment. American Journal of Speech-Language Pathology, 24, 150–163. doi:10.1044/2014_AJSLP-14-0075
- Lohmander, A., Lundeborg, I., & Persson, C. (2017). SVANTE – The Swedish Articulation and Nasality Test – Normative data and a minimum standard set for cross-linguistic comparison. Clinical Linguistics & Phonetics, 31, 137–154. doi:10.1080/02699206.2016.1205666
- Maas, E., Gildersleeve-Neumann, C., Jakielski, K.J., & Stoeckel, R. (2014). Motor-based intervention protocols in treatment of childhood apraxia of speech (CAS). Current Developmental Disorders Reports, 1, 197–206. doi:10.1007/s40474-014-0016-4
- Martinez, S., & Puelles, E. (2011). Functional anatomy of the oromotor system. In M. Roigh-Quilis, Pennington, L. (Eds.), Oromotor disorders in childhood (pp. 5–21). Barcelona: Viguera.
- McAllister, A., & Lundeborg, I. (2013). Oral sensorimotor functions in typically developing children 3 to 8 years old; assessed by the Nordic orofacial test, NOT-S. Journal of Medical Speech-Language Pathology, 22, 51–55.
- McAllister, R. (1998). Talkommunikation. Lund: Studentlitteratur (in Swedish).
- McLeod, S., Harrison, L.J., & McCormack, J. (2012). The intelligibility in context scale: Validity and reliability of a subjective rating measure. Journal of Speech, Language, and Hearing Research, 55, 648–656. doi:10.1044/1092-4388(2011/10-0130)
- Miniscalco, C., Nygren, G., Hagberg, B., Kadesjö, B., & Gillberg, C. (2006). Neuropsychiatric and neurodevelopmental outcome of children at age 6 and 7 years who screened positive for language problems at 30 months. Developmental Medicine and Child Neurology, 48, 361–366. doi:10.1017/S0012162206000788
- Neumann, S., Rietz, C., & Stenneken, P. (2017). The German Intelligibility in Context Scale (ICS-G): Reliability and validity evidence. International Journal of Language & Communication Disorders, 52, 585–594. doi:10.1111/1460-6984.12303
- Preston, J.L., & Edwards, M.L. (2007). Phonological processing skills of adolescents with residual speech sound errors. Language, Speech, and Hearing Services in Schools, 38, 297–308. doi:10.1044/0161-1461(2007/032)
- Redle, E., Vannest, J., Maloney, T., Tsevat, R.K., Eikenberry, S., Lewis, B., … Holland, S.K. (2015). Functional MRI evidence for fine motor praxis dysfunction in children with persistent speech disorders. Brain Research, 1597, 47. 2014.11.047 doi:10.1016/j.brainres
- Rodriguez, A., Kaakinen, M., Moilanen, I., Taanila, A., McGough, J.J., Loo, S., … Jarvelin, M.R. (2010). Mixed-handedness is linked to mental health problems in children and adolescents. Pediatrics, 125, e340–348. doi:10.1542/peds.2009-1165
- Shriberg, L.D., Austin, D., Lewis, B.A., McSweeny, J.L., & Wilson, D.L. (1997). The percentage of consonants correct (PCC) metric: Extensions and reliability data. Journal of Speech, Language, and Hearing Research, 40, 708–722. doi:10.1044/jslhr.4004.708
- Shriberg, L.D., Tomblin, J.B., & McSweeny, J.L. (1999). Prevalence of speech delay in 6-year-old children and comorbidity with language impairment. Journal of Speech, Language, and Hearing Research, 42, 1461–1481. doi:10.1044/jslhr.4206.1461
- Smith, A., & Zelaznik, H.N. (2004). Development of functional synergies for speech motor coordination in childhood and adolescence. Developmental Psychobiology, 45, 22–33. doi:10.1002/dev.20009
- Visscher, C., Houwen, S., Scherder, E.J., Moolenaar, B., & Hartman, E. (2007). Motor profile of children with developmental speech and language disorders. Pediatrics, 120, e158–163. doi:10.1542/peds.2006-2462
- Waring, R., & Knight, R. (2013). How should children with speech sound disorders be classified? A review and critical evaluation of current classification systems. International Journal of Language & Communication Disorders, 48, 25–40. doi:10.1111/j.1460-6984.2012.00195.x
- Wren, Y., Miller, L.L., Peters, T.J., Emond, A., & Roulstone, S. (2016). Prevalence and predictors of persistent speech sound disorder at eight years old: Findings from a population cohort study. Journal of Speech, Language, and Hearing Research, 59, 647–673. doi:10.1044/2015_JSLHR-S-14-0282
- Ziegler, W., & Ackermann, H. (2013). Neuromotor speech impairment: It’s all in the talking. Folia Phoniatrica et Logopedica, 65, 55–67. doi:10.1159/000353855