Abstract
Purpose
Patients admitted to critical care (CC) are at risk of impaired swallowing and communication function. Speech-language pathologists (SLPs) play an important role in this context. In Ireland and internationally speech-language pathology CC guidelines are lacking, with possible variations in practice. To compare clinical practices in dysphagia, communication and tracheostomy management among SLPs working in adult CC units in Ireland and internationally, and explore their perspectives on training, skills and resources.
Method
Participants were SLPs working in CC. An international online survey sought information on (i) SLP workforce demographics and staffing levels, (ii) current dysphagia and communication assessment and management practices, (iii) practices and perspectives on training, skills and resources.
Result
366 responses were received across 29 countries. 18.03% (66/366) of these respondents worked in Ireland. Findings showed similarities and differences in practices. Total CC SLP whole-time equivalent (WTE) at each staff grade was lower (mean difference: −0.21 to −0.65 WTE p <.001) than desired for optimal service delivery. Negative effects of under-staffing were reported. Recommendations that all tracheostomised patients receive SLP input was unmet in 66% (220/334) of services.
Conclusion
SLP input in CC is limited in terms of dedicated posts, multidisciplinary team (MDT) involvement, consistent management approaches and training opportunities internationally. Implications of findings are discussed.
Introduction
Critical care (CC) provides “curative and life support treatment for the critically ill patient” (Joint Faculty of Intensive Care Medicine of Ireland (JFICMI), Citation2011, p. 4) through the provision of specialised, continuous and multidisciplinary care (Faculty of Intensive Care Medicine (FICM) and The Intensive Care Society (ICS), Citation2019). Due to medical and technological advances, there is increased survival of the critically ill patient (Vincent & Creteur, Citation2015). The presence of dysphagia and communication difficulties and the need for proactive rehabilitation has been highlighted by the change in CC culture from predominantly sedated and ventilated patients to increased tracheostomy insertions and less sedation use (McRae, Montgomery, Garstang, & Cleary, Citation2019).
Critically ill patients who have difficulty with swallowing and/or communication require timely access to speech-language pathology services (Royal College of Speech and Language Therapists (RCSLT), Citation2014). Speech-language pathologists (SLPs) address the increasingly complex swallowing, tracheostomy weaning and communication needs of patients. Although the underlying mechanisms of dysphagia in critically ill patients are not conclusively known (Zuercher, Moret, Dziewas, & Schefold, Citation2019), the aetiology is considered multifactorial with factors including trauma from endotracheal or tracheostomy tubes, neuromuscular weakness, altered oropharyngeal or laryngeal sensation, altered sensorium from delirium or sedation, gastroesophageal reflux or uncoordinated breathing and swallowing (Macht, Wimbish, Bodine, & Moss, Citation2013). Communication may be hindered not only by the presence of a tracheostomy or endotracheal tube but also by potential laryngeal injuries that can occur in up to 58–83% of tracheostomised or ventilated CC patients (Miles et al., Citation2018).
There is increasing recognition of the significant implications for a patient’s psychosocial wellbeing, medical stability and quality of life (QOL) that dysphagia and communication deficits have in CC (Freeman-Sanderson, Morris, & Elkins, Citation2019; Thomas & Rodriguez, Citation2011). These negative implications extend beyond the patient to having substantial health and cost burdens on healthcare systems (Attrill, White, Murray, Hammond, & Doeltgen, Citation2018; Matsuo, Yoshimura, Ishizaki, & Ueno, Citation2017). Dysphagia is associated with a significantly longer length of stay, increased medical costs, a higher likelihood of discharge to post-acute care facility and higher inpatient mortality rates (Patel et al., Citation2018). However, challenges exist in CC dysphagia and communication management.
In terms of dysphagia, the reported prevalence of post-extubation dysphagia (PED) varies considerably from 3% to 90% (Marvin, Thibeault, & Ehlenbach, Citation2019; McIntyre, Doeltgen, Dalton, Koppa, & Chimunda, Citation2021) and there is a lack of international consensus on many issues. For example, there are few recognised and validated bedside swallowing screening tools to identify CC patients at aspiration risk from PED (Johnson et al., Citation2018; Perren, Zürcher, & Schefold, Citation2019) and a lack of consistency in the use of swallow screening tools (Ginnelly & Greenwood, Citation2016). There is no clear consensus about the timing of swallowing evaluations post-extubation, with times varying from immediately after to up to 48 hours post-extubation (Omura, Komine, Yanagigawa, Chiba, & Osada, Citation2019). Moreover, given concern of increased aspiration risk with nasal high flow oxygen modes (Ferrara et al., Citation2017; Hori, Isaka, Oonishi, Yabe, & Oku, Citation2016), patient specific instrumental assessment is advisable but availability and use of instrumental assessments remain highly variable amongst CC SLPs (Brodsky et al., Citation2017; Macht et al., Citation2013).
In terms of communication management, there is an overwhelming lack of research exploring communication screening in CC despite the fact that communication difficulties can occur in approximately one third of critical care patients (Freeman-Sanderson et al., Citation2019). Loss of voice can have a substantial negative effect on patient mood, restrict patients’ level of autonomy, and lead to difficulty participating in care planning and rehabilitation (Freeman-Sanderson, Togher, Elkins, & Phipps, Citation2016; Tembo, Higgins, & Parker, Citation2015). Early facilitation of different non-verbal and verbal communication options improves the recovery process, instils a sense of normality and may reduce delirium (Green et al., Citation2018; Mobasheri et al., Citation2016). SLP input in CC combined with access for multidisciplinary team (MDT) staff training in communication enhancement, enablement and augmentative and alternative communication (AAC) use should result in improved patient communication (Freeman-Sanderson et al., Citation2019). SLPs have a role in educating and training patient families and CC colleagues in the recommended strategies to facilitate patient communication (Tembo et al., Citation2015).
The value of SLPs as integral members of the CC MDT is gaining increasing worldwide recognition (Freeman-Sanderson et al., Citation2021; FICM and ICS, Citation2019; Health Service Executive (HSE), 2014; National Confidential Enquiry into Patient Outcomes and Death (NCEPOD), Citation2014; RCSLT, 2014; McGrath & Wallace, Citation2014). A common theme in available guidelines is that SLPs should be fully integrated members of the CC team, “contributing to all multidisciplinary ward rounds, tracheostomy teams, clinical governance groups, audit, research, education and policy development” (FICM and ICS, Citation2019, p. 57).
However, there are a lack of international guidelines outside of the UK with no known adult CC position paper in Ireland, the USA, Canada, Australia or New Zealand at this time. Furthermore, service provision guidelines vary from country to country. For example, in Ireland, the most up to date Irish National Clinical Programme for Critical Care (HSE, Citation2014) recommend a staffing level of 0.06 WTE (whole time equivalent) per CC bed at a Senior Grade or higher who have specialised postgraduate training. This is significantly lower than the UK Guidelines for the Provision of Intensive Care Services (GPICS) (FICM and ICS, Citation2019) which recommends a minimum staffing level of 0.1 WTE per CC bed. Of note, at the time of this survey in Ireland, there were 257 ICU beds across 26 hospital sites nationally (HSE, Citation2020). The number of SLPs providing services to these units was unknown.
It is hypothesised due the lack of specific, standardised guidelines to inform clinical practice and workforce planning despite a growing body of international research in this area, there may be variations and inconsistencies in clinical practice patterns worldwide. In addition, SLP perspectives on current practice and ongoing development needs of the profession are largely not documented.
Study aims
To compare clinical practice in dysphagia, communication and tracheostomy management among SLPs working in adult CC units in Ireland and internationally, and explore their perspectives on training, skills and resources.
Method
The Consensus-Based Checklist for Reporting of Survey Studies (Sharma et al., Citation2021) is used to report this research. Ethical approval for this study was obtained from the School of Linguistic, Speech and Communication Sciences Research Ethics Committee, Trinity College Dublin. An anonymous, cross-sectional survey design was developed to capture SLP practice patterns and service provision in CC.
Survey development
The survey was designed and disseminated using Qualtrics, an online survey tool (http://www.qualtrics.com). Survey questions were developed based on a review of the literature, a revised draft of a similar survey by the RCSLT Tracheostomy Clinical Excellence Network (CEN) and personal experience of the senior authors working in CC. The survey was divided into four sections: (i) workforce demographics, access to SLP and SLP respondents’ staffing levels, (ii) SLP respondents’ current dysphagia assessment and management practices, (iii) SLP respondents’ current communication assessment and management and (iv) SLP respondents’ practices and perspectives on training, skills and resources. The survey contained 39 numbered questions, 66 in total including branched sub-questions based on skip logic (Supplementary material, A1). It took approximately fifteen minutes to complete. Closed question formats included binary yes–no, multiple forced-choice and 5-point Likert scales.
The survey introduction was written to meet the requirements of informed consent and acting as a modified participant information leaflet (PIL). The survey was piloted twice on four SLPs working internationally in the area of CC to enhance the content validity, improve responder reliability and help reduce the chance of measurement error or non-response errors in the live survey. Minor revisions to wording for clarification were made to the survey based on feedback from pilot testing. The survey did not seek any identifying information from the participant such as their workplace name. Internet Protocol addresses of participants were not collected. Although not anticipated, any confidential information disclosed in the survey was removed from data collected.
Recruitment
SLPs working in adult CC settings in Ireland and internationally were identified as the target population. Inclusion criteria were SLPs with a recognised professional qualification and clinical experience in dysphagia management, working clinically or have recent experience working in CC within the last 3 years (excluding medical observational units, high dependency units or acute observational units). SLPs who had not worked in a CC setting in the past 3 years were excluded to make sure the data collected was reflective of recent and current practices. Non-probable, purposive sampling was used to recruit survey participants. The researchers sent information on the project by email or Twitter to secretaries or chairpersons of relevant national and international professional bodies, persons responsible for hosting SLP communication forums, networks and special interest groups (SIGs). These were invited to act as gatekeepers to send the PIL and the survey link to potential participants. The survey information was also emailed to the co-researchers’ professional networks who were invited to act as gatekeepers and email the information to SLPs in their region. The survey was live over a ten-week period from November 2019 to January 2020.
Data analysis
Descriptive statistics were completed using the Qualtrics “report”. Given that on occasion some participants did not answer certain questions, responses were reported as a percentage of the total number of answers, including a percentage of non-responses. Inferential statistics using SPSS v25 Statistics software was also used to test a hypothesis and draw conclusions about a population, based on the survey sample. A p-value of less than 0.05 was considered statistically significant across all tests. Furthermore, inductive, qualitative content analysis (Elo & Kyngas, Citation2008; Vaismoradi, Turunen & Bondas, Citation2013) was used to analyse data recorded in narrative comment boxes in the survey.
Result
Demographics
In total, 366 SLPs responded to the survey and 264 participants (72%) completed it in full. SLPs practising in the UK were not invited to participate given that an initial version of this survey was recently disseminated by the RCSLT tracheostomy CEN. However, 13 SLPs from the UK responded and were included in the data analysis because they were not listed in the exclusion criteria.
The sample was diverse in location, employment setting and years of experience. Participants from 29 countries responded (). The most common types of hospitals respondents worked in (multiple choice was permitted) were academic teaching/university (30.69%, 155/505), public (27.92%, 141/505) and regional/district general hospitals (22.77%, 115/505). Charity hospitals were the least common workplace setting reported (1.98%, 10/505). Respondents had similar length of experience across countries; 54.47% (36/66) of SLPs working in Ireland had between 1 and 5 years of experience, 22.73% (15/66) between 6 and 10 years of experience and 22.73% (15/66) greater than 10 years’ experience. This is compared to 51% (189/300), 18.33% (55/300) and 30.67% (92/300) from other countries.
Table I. Country of practice of speech-language pathologist respondents.
Critical care workforce demographics and level of service provision
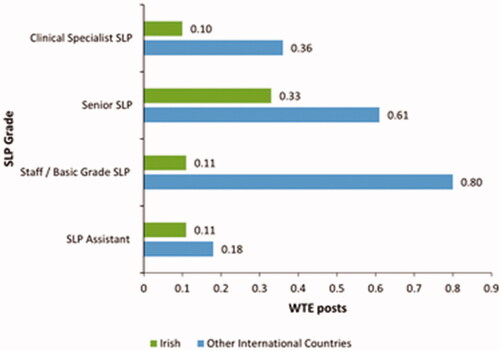
There was a difference reported in WTE staffing levels for Irish CC units compared to other countries ().
Figure 1. The mean WTE figure of SLP posts currently employed in Irish (n = 66) and other international (n = 300) CC services.
These differences also extend to the mean number of SLPs per grade that respondents believe should be employed in their CC unit to provide an optimal service ().
Figure 2. The mean WTE figure of posts SLPs working in Ireland (n = 50) and other international CC services (n = 226) believe should be solely designated to CC to provide an optimal SLP service.
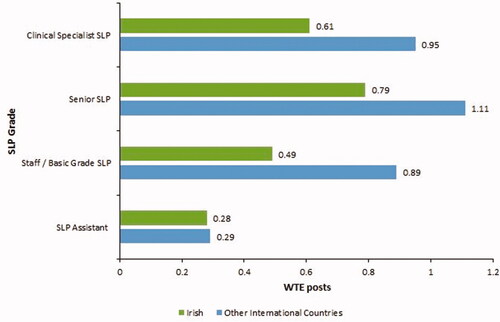
The total CC SLP whole-time equivalent (WTE) at each grade was statistically significantly lower (mean difference: −0.21 to −0.65 (95% CI, average 0.54–0.31) WTE, p <0.001) than what was reportedly needed to provide an optimal service.
Similar CC SLP staffing trends over the past 3 years in Ireland and other international countries were reported. In Irish CC settings, 65.15% (43/66) of SLP respondents reported staffing levels staying the same over the past 3 years with only 27.27% (18/66) reporting improvements. This is comparable to 53.67% (161/300) of respondents from other international countries reporting static staffing levels and 35% (105/300) reporting improvements.
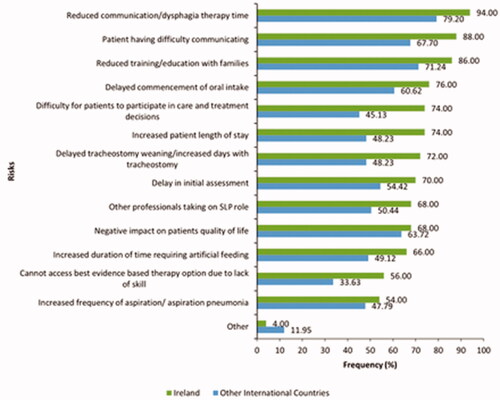
SLPs reported several risks they perceived these reduced staffing levels in CC was having on patients and families ().
Critical care SLP referrals and caseload
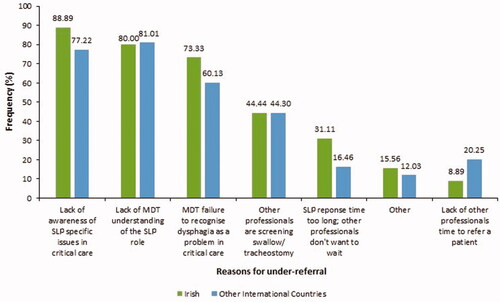
Fewer SLP respondents working in Ireland (46.15%, 30/65) reported receiving referrals in a timely manner compared with SLPs in other international countries (64.18%, 181/282). The most common reported reasons across countries accounting for late referrals were lack of awareness of when is appropriate timing to refer to SLP (33.52%, 118/352) and lack of MDT understanding of SLP role (29.26%, 103/352). Overall, more SLPs (26.08%) outside Ireland reported that they could respond to referrals on the same working day. Similarities were seen in the frequency of cohorts of patients referred to SLP CC in both Irish and other international SLP CC units ().
Figure 4. Reasons SLPs working in Ireland (n = 45) and other countries (n = 158) believe under-referral is a problem: multiple-choice permitted.
In terms of caseload, 95.45% (63/66) of SLPs working in Ireland had a mixed caseload with only 4.55% (3/66) working solely in CC. This contrasted with other countries, where nearly double this amount (10%, 30/300) reported to be working solely in CC.
Exploring the intensity of SLP rehabilitation input available, statistical analysis was completed to determine if there were differences in the capacity of respondents to provide intensive CC SLP rehabilitation (45 min, 5 days a week) between country of work (Ireland and other international countries). Using Mann Whitney U Test, reported capacity to provide intensive CC SLP rehabilitation was statistically significantly lower in Ireland (mean rank = 114.8) compared to that reported in other international countries (mean rank = 189.3), U = 5318, z = −5.503, p < 0.001.
Current dysphagia assessment and management practices
Overall, 11.94% (42/352) of survey respondents across all countries believed dysphagia service provision in their CC unit was “very poor/poor”, 22.44% (79/352) “fair” and 65.63% (231/352) “good/very good”. SLP respondents working in Ireland perceived CC dysphagia service provision to be less adequate overall when compared with other countries.
Dysphagia screening
9.52% (6/63) of respondents working in Ireland and 45.90% (123/268) working in other international countries reported the use of screening tools by nurses or medical doctors to identify PED.
1.72% (1/58) of SLPs working in Ireland reported assessing every patient’s swallow function post-extubation compared to 10.04% (26/259) SLPs working in other countries. There were mixed reports as to whether SLP services had a protocol regarding timing of swallow assessment post-extubation with 42.31% (11/26) of all respondents reporting “yes” and the other 57.69% (15/26) responding “no”. Of the respondents who did have a timing protocol to assess PED, the most common timeframe to wait was reported as “<12 hours” (72.73%, 8/11), followed by “12-24 hours” (18.18%, 2/11) and “24-48 hours” (9.09%, 1/11) across data. No respondents reported a protocol timeframe of “48-72 hours”. The frequency of used PED screening tools reported was counted (Supplementary material, A2).
Dysphagia assessment
Cough reflex testing, as part of dysphagia assessment in CC, was not routinely used according to SLPs working in Ireland (8.62%, 5/58) and those in other international countries (28.24%, 72/255). Fiberoptic endoscopic evaluation of swallowing (FEES) assessments were reported as available for CC patients in 38.98% (23/59) of SLP respondents working in Ireland and 59.61% (152/255) in other international services. Most FEES assessments in CC were reported as being SLP-led in Irish (91.30%, 21/23) and other international services (86.49%, 128/148). Overall, the wait-time for CC patients to receive a portable SLP-led FEES assessment were reported as longer in Irish services than in other international countries. The highest reported barriers for not having access to portable FEES in CC from all SLP respondents across countries (n = 135) was equipment costs (65.19%), SLP endoscopy scoping training (51.11%) and equipment operational care/decontamination (37.04%). This order was consistent for both responses from Ireland and the other international countries group.
Dysphagia rehabilitation
The most common dysphagia rehabilitation technique reported as “always” used across countries were “pharyngeal strengthening exercises” (6.21%, 18/290), “laryngeal elevation exercises” (4.50%, 13/289), “thermal tactile” (2.08%, 6/289) and “oro-motor exercises” (2.06%, 6/291). The dysphagia rehabilitation tools most commonly reported as “never” used across countries were “pharyngeal electrical stimulation” (93.03%, 267/287), “surface electromyography (sEMG)” (88.03%, 250/284), “deep pharyngeal stimulation (DPNS)” (86.27%, 245/284) and “neuromuscular electrical stimulation (NMES)” (81.25%, 234/288).
Current tracheostomy assessment and management practices
A fifth (20.8%, 73/351) of respondents from all countries rated their CC tracheostomy service provision as “very poor/poor”, 29.63% (104/351) “fair” and the majority 49.57% (174/351) “good/very good”. SLPs working in Ireland reported their CC tracheostomy service provision as more adequate overall when compared with other international SLP respondents.
Tracheostomy referral
Over half of SLP respondents working in Ireland reported that they self-refer or receive referrals for all patients with a tracheostomy 54.69% (35/64). This was nearly twice as many as that reported by other international services (29.26%, 79/270). Overall, the most common time points at which patients with a tracheostomy are referred to SLP services were “when patients have been weaned to CPAP/high flow/lower pressure support levels and is not requiring control ventilation” (46.65%, 153/328), “when patients are tolerating cuff deflation” (42.99%, 141/328) and “when patients have a tracheostomy and are ventilated” (42.68%, 140/328). The least frequent point of referral reported across all respondents was “when decision is made to insert tracheostomy/prior to tracheostomy insertion” (12.5%, 41/328). Similar trends in the timing of referrals to SLP for tracheostomy patients were seen in SLPs working in Ireland and other international countries responses.
Tracheostomy screening
The use of screening tools by nurses or medical doctors for swallowing disorders in tracheostomised patients was reported by only 4.76% (3/63) of SLP respondents working in Ireland. This compares with 26.12% (70/268) of respondents from other international countries. The frequency of screening tools used for swallowing in tracheostomised patients reported was counted (Supplementary material, A3).
Tracheostomy assessment practices
Almost two-thirds of SLPs working in Ireland (62.07%, 36/58) reported they contribute to cuff deflation tracheostomy and swallow/speaking valve trials while patients are on ventilation compared to 54.58% (137/251) of SLP respondents from other countries. Overall, a greater percentage of international SLP services reported the use of sub-glottic suction tracheostomy tubes more frequently than SLPs working in Ireland ().
Table II. Frequency of speech-language pathologist working in Ireland (N = 53) and other international countries (n = 245) use of sub-glottic suction tracheostomy tubes.
The majority of SLP respondents from all countries reported they do not routinely allow patients to have oral intake with an inflated tracheostomy cuff (87.21%, 259/297). Examples of exceptions to this case reported were “comfort-risk feeding at aspiration risk for QOL” (81.08%, 30/37), “if eating/drinking has been shown to be safe on an instrumental FEES swallow assessment” (72.97%, 27/37) or a “long term ventilation dependent patient” (64.86%, 24/37). Other times when SLPs allowed patients oral intake with an inflated tracheostomy cuff were reported as “at times I don’t recommend but consultant will overrule and cite QOL reasons” (n = 1) and “after a videofluoroscopy” (n = 1) in an open coded question.
Current communication assessment and management practices
Communication screening
Use of communication screening by nurses or other professionals across four different conditions was explored. A similar percentage of SLPs working in Ireland reported the use of communication screening tools for both patients on non-invasive ventilation (15.38%, 8/52) and intubated patients (17.31%, 9/52) in their CC units as in other international countries (15.13%, 36/238), (18.14%, 43/237). A further similarity was seen in the use of communication screening tools patients with tracheostomy (23.08%, 12/52) in Irish CC units and in other countries (21.01%, 50/238). Overall, a lower percentage of SLPs working in Ireland (7.69%, 4/52) reported the use of communication screening tools for all patients in their CC unit compared with other international SLP respondents (14.04%, 33/235).
Augmentative and alternative communication (AAC)
SLPs working in Ireland reported higher perceived agreement with the following statements regarding communication management than respondents working in other countries;
“Patients who are non-speaking are always referred to SLT”: Ireland (42.31%, 22/52), other countries (35.02%, 83/237).
“If family or nurses are not able to set up a communication method for nonspeaking patients, then SLT are consulted”: Ireland (78.85%, 41/52), other countries (62.87%, 149/237).
“If patients are expected to be non-speaking for more than a few days then they are always referred to SLT”: Ireland (40.39%, 21/52), other countries (35.02%, 83/237).
“Nurses lead the way trialling methods to facilitate communication”: Ireland (44.23%, 23/52), other countries (40.92%, 97/237).
This was in contrast with (9.61%, 5/52) of respondents working in Ireland agreeing with the statement “SLPs give regular training slots on facilitating communication to other staff in critical care” compared with (24.48%, 58/237) of respondents working in other countries. A full breakdown is seen in Appendix 4 of the Supplementary online materials.
A higher percentage of respondents from SLPs working in Ireland (73.08%, 38/52) reported providing communication aids for staff to trial with patients out of working hours in CC than working in other countries (65.82%, 156/237). A similar percentage frequency of use was reported for different AAC methods across Ireland and other international countries.
Practices and perspectives on training, skills and resources
There was a lack of consistency across respondents whether the SLP CC education and training received was adequate. Overall, 28.49% (90/351) of respondents from all countries rated this as “very poor/poor”, 33.62% (118/351) “fair” and 37.89% (133/351) “good/very good”. SLPs working in Ireland believed the education and training service provision in their CC unit was less adequate overall when compared with other international countries.
In terms of CC non-clinical meetings, a Mann-Whitney U test was run to determine if there were differences in attendance at these meeting types and country of work (Ireland versus other international countries). There was a significant difference in attendance at medical team wards rounds, with Ireland (mean rank = 120.4) being significantly lower than in other international countries (mean rank = 144.0), U = 5623, z = −2.148, p = 0.032. However, attendance at CC quality/audit/research meetings collectively was significantly higher in Ireland (mean rank = 148.6) than in other international countries (mean rank = 125.3), U = 4808, z = −2.290, p = 0.022.
A higher percentage of SLPs respondents working in Ireland reported having a Tracheostomy Team or Tracheostomy Steering Group in their CC service (53.85%, 28/52) than respondents from other international countries (27.90%, 65/233). The majority of SLPs working in Ireland (92.00%, 23/25) and other international countries (87.69%, 57/65) reported they were part of this Tracheostomy Team or Tracheostomy Steering Group in their service.
SLPs working in Ireland reported lower perceived agreement with the following professional practice statements than respondents working in other countries;
“I feel fully professionally satisfied working as a CC SLP” Ireland (18.75%, 9/48), other countries (52.88%, 119/225).
“I feel fully competent and skilled working as an SLP in CC” Ireland (37.5%, 18/48), other countries (60.89%, 137/225).
“I feel fully supported as an SLP working as part of a CC team” Ireland (22.92%, 11/48), other countries (37.78%, 85/225).
Supplementary online materials (Appendices 5–7) give a full breakdown of the level of agreement/disagreement of SLPs working in Ireland (n = 48) and other international (n = 225) countries with the above statements.
Overall, most SLP respondents from all countries reported the need for “creation of dysphagia/communication standardised screening tools/algorithms to flag appropriate SLP referrals” (80.46%, 210/261), “the provision of supplementary training specific to CC” (78.93%, 206/261), “more funding for SLP staff in CC” (75.48%, 197/261) and “a national position paper on the role of SLP in CC & clinical practice guidelines” (70.88%, 185/261).
Discussion
Critical care workforce demographics and level of service provision
SLP staffing recommendations “reflects the need to provide frequent SLP intervention in line with the expected risks of dysphagia (49%), dysphonia (76%) and other communication problems in critically ill ventilated patients” (FICM and ICS, Citation2019, p. 57) along with facilitating direct involvement with clinical and strategic decisions as part of the wider MDT (McRae et al., Citation2019). It was beyond the scope of this study to investigate if international CC service provision guidelines (FICM and ICS, Citation2019; HSE, Citation2014) are being met. However, survey findings showed a large variation in staffing exists depending on service and the total WTE of SLP staffing at each level was significantly lower than the total WTE of staffing that respondents desired. Various clinical risks due to reduced SLP staffing levels in CC were identified by SLP respondents. National and international staffing standards should be met to enable the delivery of a consistent, safe and reliable service.
Critical care SLP referrals and caseload
Similar to Australian study findings (Cardinal, Freeman-Sanderson, & Togher, Citation2020; Ward, Morgan, McGowan, Spurgin, & Solley, Citation2012), the current speech-language pathology provision for CC patient needs across countries was reported as inequitable and not fully and specifically funded for this client group. Nearly all SLPs in this survey reported carrying a mixed caseload. As per McRae et al. (Citation2019), this limits both clinical development and professional involvement within teams. The majority of respondents reported that they were “sometimes” or “rarely” able to meet National Institute for Health and Clinical Excellence [NICE] (Citation2009) guidance that patients receive 45 minutes of daily SLP therapy, for a minimum of 5 days a week, at a level that enables the patient to meet rehabilitation goals. Statistical analysis showed a significantly lower capacity as reported by respondents in Irish services compared to other international countries to provide this amount of therapy. These shortfalls and inconsistency of practice could prevent patients from receiving optimal care and may place them at risk of serious complications. For example, increased risk of aspiration pneumonia and subsequent mortality (Patel et al., Citation2018) or low patient mood, motivation, and stress levels associated with lack of ability to communicate (Freeman-Sanderson et al., Citation2019) that can contribute to decreased health-related QOL beyond hospital discharge (Tembo et al., Citation2015).
Current dysphagia assessment and management practices
Screening procedures for dysphagia can streamline effective workflows (Cardinal et al., Citation2020) and detect dysphagia early, preventing associated complications. The lack of recognised and validated bedside swallowing screening tools to identify patients at aspiration risk in CC (Johnson et al., Citation2018; Perren et al., Citation2019) might explain in part why fewer than 10% of respondents working in Ireland and 50% working in other international countries reported screening tools by nurses or medical doctors to identify PED. These findings align with international reports (van Snippenburg et al., Citation2019). Moreover, there is an inconsistency in swallow screening tools used across settings with 15 different protocols reported in the survey. This is consistent with other areas of practice (Walshe, Ryan, & Regan, Citation2017).
There is no clear consensus about the timing of swallowing evaluations in the literature which was reflected in this survey, with times varying from immediately after to up to 48 hours post-extubation (Omura et al., Citation2019). As suggested by Perren et al. (Citation2019), future research should validate respective clinical screening tools and algorithms in critically ill patients given the importance of early interdisciplinary screening to address potential complications from PED (Brodsky, Pandian, & Needham, Citation2020). However, the high prevalence of silent aspiration and the risk of secondary pulmonary consequences in this population further supports the need for expert instrumental swallowing assessment, particularly given the vulnerability of these critically ill patients (Marvin et al., Citation2019).
Benefits of instrumental assessments such as FEES to expedite safe feeding and tracheostomy weaning decisions have been widely reported (McGrath & Wallace, Citation2014). However, FEES may not be available in all CC settings (Brodsky et al., Citation2017; NCEPOD, 2014). Consistent with the literature, the survey findings showed less than 40% of SLP respondents from services in Ireland and less than 60% from other international services reported access to FEES assessment for CC patients.
Evidence for dysphagia treatment in CC patients is limited. Macht et al. (Citation2013) found that treatment in CC usually focussed on dietary texture modifications and postural changes/compensatory manoeuvres rather than on direct rehabilitation to improve swallowing function. This was consistent with findings from this survey, where low frequency of direct swallowing rehabilitation techniques use was reported. Perhaps this may be in part due to challenging practicalities of dysphagia rehabilitation in CC for example, fluctuating patient medical stability, neurological and respiratory status (Duncan et al., Citation2020). Furthermore, the fact dysphagia rehabilitation evidence to date is relatively under-explored in critically ill patients may be impacting the lack of direct dysphagia practice on the ground. Nonetheless, as per National Institute for Health and Clinical Excellence [NICE] (Citation2017) guidelines, each CC patient should have a rehabilitation prescription completed within 72 hours outlining their impairments and planned interventions, which adds weight to the idea that dysphagia rehabilitation in CC is overlooked and should be a priority focus of future research.
Current tracheostomy assessment and management practices
Fewer respondents reported using swallow screening tools for patients with a tracheostomy. In contrast to reports by van Snippenburg et al. (Citation2019, p. 224), where screening is performed more in the majority of Dutch ICUs in patients who received a tracheostomy, Ginnelly and Greenwood (Citation2016) also found varied practice and a lack of consistency in the use of swallow screening assessments by tracheostomy MDTs in the UK. This survey mirrors these findings, where over 10 different swallow screening tools for these patients were reported.
In terms of referral to SLP, one UK report (NCEPOD, 2014) found that 51% of patients with a tracheostomy were referred “early” to SLP (within 48 h). Given that every day spent by patients in CC reduces the likelihood of dysphagia recovery, there is a need for SLPs to start assessment and treatment early (Brodsky et al., Citation2017). In this survey, just over one-third of all respondents reported they receive referrals for all patients with a tracheostomy. This means overall, there is a lack of ability to meet GPICS (FICM and ICS, Citation2019) guidance of SLP input for all patients with a tracheostomy.
Nearly double the percentage of respondents working in Ireland reported having a Tracheostomy Team or Steering Group in their CC service compared to respondents working in other countries. However, most survey respondents stated that they were part of these teams if they were established in their service. This is in keeping the increased recognition for SLPs to be key members of tracheostomy MDTs (McGrath & Wallace, Citation2014).
Current communication assessment and management practices
A low percentage of survey respondents reported the use of communication screening tools for all patients in their CC unit, which reflects the paucity of research addressing communication screening in CC. This is concerning given prompter facilitation of communication improves patient QOL and autonomy (Thomas & Rodriguez, Citation2011).
There was mixed agreement with the statement “patients who are non-speaking are always referred to SLP” despite the fact that early facilitation of different non-verbal and verbal communication options improve the recovery process, instil a sense of normality and may reduce delirium (Green et al., Citation2018; Mobasheri et al., Citation2016). Enhanced patient communication is a combination of SLP input in CC and access for MDT staff training (Freeman-Sanderson et al., Citation2019). It seems that there are improvements to be made in educating and training patient families and CC colleagues in strategies to facilitate patient communication (Tembo et al., Citation2015).
Practices and perspectives on training, skills and resources
Gaps in professional needs and a lack of resources and development opportunities were reported by respondents and it must be noted that dissatisfaction with staffing levels, time, training, clinical resources and support has been a common outcome in comparable profession focussed survey studies (Moloney & Walshe, Citation2019; Northcott, Simpson, Moss, Ahmed, & Hilari, Citation2017; O’Reilly & Walshe, Citation2015).
Most respondents reported “never” participating in listed non-clinical CC meetings surveyed, although attendance at regular MDT CC ward rounds are imperative to help to review, discuss and collaboratively plan a coordinated rehabilitation plan and set achievable goals to improve outcomes (McRae et al., Citation2019). They also present as an opportunity to increase education on the SLP role to the MDT, a reported learning goal of CC physicians in a recent international survey (Marian, Dunser, Citerio, Kokofer, & Dziewas, Citation2018).
Clinical implications
The evolving role in SLP and barriers reported in this survey should be used as an initial step in developing quality improvement initiatives to facilitate the optimum delivery of speech-language pathology in CC services. There are four key clinical implications from this study spanning from improved resourcing, recognition of SLP role, training and research.
Firstly, this study highlights the insufficient funding for dedicated CC SLP staffing across all countries, not just Ireland, and the risks that this poses in terms of substandard care for swallowing and tracheostomy weaning, reduced patient outcomes and reduced QOL for patients (FICM and ICS, Citation2019). This has resource implications and services should be ready to address this through new business cases or skill mix, employing adequate staff to increase the intensity of therapy and using patient data to drive change and improve clinical outcomes. There is a strong need for the continuous appraisal of service provision and quality by auditing unmet need or collecting research data. Commissioners should also ensure that SLP services are incorporated into service planning and development (RCSLT, 2014).
Secondly, this study explores the inadequate incorporation of SLPs within CC teams worldwide and the need for a culture shift so there is collaborative management across disciplines. Increased awareness of the role and specialist skills of SLPs amongst team members is needed which have been reported to be poorly understood. SLPs must also do more to empower and educate fellow team members and patient families about tracheostomy and swallowing and participate in MDT activities.
Moreover, the variability in clinical practices shown also supports the need for establishing SLP CC competency frameworks to ensure staff are appropriately trained, skilled and competent in this specialist area. A reported lack of training opportunities demonstrates a need for improving the professional development of this area and highlighting a gap in targeted postgraduate learning opportunities.
Finally, the need for increased evidence to support the effectiveness of SLP involvement in CC rehabilitation and the development of standardised referral criteria and protocols is emphasised. Although randomised control trials and meta-analyses are lacking in this area, this should not delay development of necessary guidelines to enable effective clinical decision making (Swisher, Citation2010). This starting point is vital in informing clinical reasoning and mitigating unnecessary variation in practices highlighted in this study (Hollon et al., Citation2014).
Limitations
There were some limitations to this study. The survey was not translated into other languages due to time constraints, thus only people who were proficient in English could complete it. As with all survey designs, there is a potential bias as SLPs with an interest in the topic are more likely to respond and responses may not reflect all SLP perspectives. Furthermore, a response rate for the survey could not be determined given:
The survey was disseminated via snowball sampling on SLP social media platforms, so it was not possible to determine how many SLPs accessed the survey link.
Information on the size of SLP membership in the different professional bodies and SIGs contacted could not be obtained.
There are no national or other international records of the number of SLPs working in CC settings.
It should be also acknowledged that responses are respondents’ professional opinions and not reflective of best practice clinical guidelines. Furthermore, as there were not enough respondents from each country to look at differences between individual countries, the research team therefore amalgamated data from all countries outside of Ireland as one. Thus, caution must be taken not to over-generalise the results. This is especially relevant for the inferential statistics given the survey captured a small, diverse group and the fact responses may vary from setting to setting rather than country to country. This limitation of respondent bias must be accounted for.
Conclusion
Although the results of this study cannot be used to infer causality, the findings identify areas of consistency and variation in CC speech-language pathology practice patterns and service provision, not just in Ireland but internationally. It provides preliminary insights into the perspectives of SLPs towards facilitators and barriers to best practice, especially important in this COVID-19 era. In the absence of clinical practice and training guidelines in Ireland and further afield, this study provides preliminary support for further professional development for SLPs working in CC and the development of strategies to enhance MDT's working in this environment. Future research should focus on the impact of the previously discussed variations and challenges on patient outcomes.
To conclude, variability of practices along with lack of adequate service provision, CPD and training opportunities suggest that this specialist area of clinical practice is in need of urgent direction and guidance.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental material
Supplemental data for this article can be accessed at https://doi.org/10.1080/17549507.2022.2032346
References
- Attrill, S., White, S., Murray, J., Hammond, S., & Doeltgen, S. (2018). Impact of oropharyngeal dysphagia on healthcare cost and length of stay in hospital: A systematic review. BMC Health Services Research, 18, 594–612.
- Brodsky, M., Huang, M., Shanholtz, C., Mendez-Tellez, P., Palmer, J., Colantuoni, E., & Needham, D. (2017). Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-year longitudinal study. Annals of the American Thoracic Society, 14, 376–383.
- Brodsky, M., Pandian, V., & Needham, D. (2020). Post‑extubation dysphagia: A problem needing multidisciplinary efforts. Intensive Care Medicine, 46, 93–96. doi:10.1007/s00134-019-05865-x
- Cardinal, L., Freeman-Sanderson, A., & Togher, L. (2020). The speech pathology workforce in intensive care units: Results from a national survey. Australian Critical Care, 33, 250–258.
- Duncan, S., Mcauley, D., Walshe, M., Gaughey, J., Anand, R., Fallis, R., & Blackwood, B. (2020). Interventions for oropharyngeal dysphagia in acute and critical care: A systematic review and meta-analysis. Intensive Care Medicine, 46, 1326–1338. doi:10.1007/s00134-020-06126-y
- Elo, S. and Kyngäs, H. (2008), The qualitative content analysis process. Journal of Advanced Nursing, 62, 107–115. doi:10.1111/j.1365-2648.2007.04569.x
- Faculty of Intensive Care Medicine (FICM) and The Intensive Care Society (ICS) ( 2019). Guidelines for the Provision of Intensive Care Services (GPICS) version 2. Retrieved from https://www.ficm.ac.uk/sites/default/files/gpics_v2-public-consultation-draft-october-2018_0.pdf
- Ferrara, L., Bidiwala, A., Sher, I., Pirzada, M., Barlev, D., Islam, S., … Hanna, N. (2017). Effect of nasal continuous positive airway pressure on the pharyngeal swallow in neonates. Journal of Perinatology, 37, 398–403.
- Freeman-Sanderson, A., Morris, K., & Elkins, M. (2019). Characteristics of patient communication and prevalence of communication difficulty in the intensive care unit: An observational study. Australian Critical Care, 32, 373–377.
- Freeman-Sanderson, A., Togher, L., Elkins, M., & Phipps, P. (2016). Quality of life improves with return of voice in tracheostomy patients in intensive care: An observational study. Journal of Critical Care, 33, 186–191.
- Freeman-Sanderson, A., Ward, C., Miles, A., de Pedro Netto, I., Duncan, S.A., Inamoto, Y., … Brodsky, M. (2021). A consensus statement for the management and rehabilitation of communication and swallowing function in the ICU: A global response to COVID-19. Archives of Physical Medicine and Rehabilitation, 102, 835–842. doi:10.1016/j.apmr.2020.10.113
- Ginnelly, A., & Greenwood, N. (2016). Screening adult patients with a tracheostomy tube for dysphagia: A mixed-methods study of practice in the UK. International Journal of Language and Communication Disorders, 51, 285–295.
- Green, S., Reivonen, S., Rutter, L., Nouzova, E., Duncan, N., Clarke, C., … Tieges, Z. (2018). Investigating speech and language impairments in delirium: A preliminary case- control study. PLoS ONE, 13, e0207527. doi:10.1371/journal.pone.0207527
- Health Service Executive (2014). Model of care for adult critical care: National clinical programme for critical care. Retrieved from https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/model-of-care-for-adult-critical-care.pdf
- Health Service Executive (2020). National adult critical care capacity census report 2020. Retrieved from https://www.hse.ie/eng/about/who/cspd/ncps/critical-care/national-adult-critical-care-capacity-census-2020.pdf
- Hollon, S.D., Areán, P.A., Craske, M.G., Crawford, K.A., Kivlahan, D.R., Magnavita, J.J., … Kurtzman, H. (2014). Development of clinical practice guidelines. Annual Review of Clinical Psychology, 10, 213–241. doi:10.1146/annurev-clinpsy-050212-185529
- Hori, R., Isaka, M., Oonishi, K., Yabe, T., & Oku, Y. (2016). Coordination between respiration and swallowing during non-invasive positive pressure ventilation. Respirology, 21, 1062–1067.
- Johnson, K., Speirs, L., Mitchell, A., Przybyl, H., Anderson, D., Manos, B., … Winchester, K. (2018). Validation of a postextubation dysphagia screening tool for patients after prolonged endotracheal intubation. American Journal of Critical Care, 27, 89–96.
- Joint Faculty of Intensive Care Medicine of Ireland (JFICMI) (2011). National standards for adult critical care services. Retrieved from https://www.anaesthesia.ie/attachments/article/57/JFICMI_Minimum_Standards%20Rev-01.pdf
- Macht, M., Wimbish, T., Bodine, C., & Moss, M. (2013). ICU-acquired swallowing disorders. Critical Care Medicine, 41, 2396–2405.
- Marian, T., Dunser, M., Citerio, G., Kokofer, A., & Dziewas, R. (2018). Are intensive care physicians aware of dysphagia? The MADICU survey results. Intensive Care Medicine, 44, 973–975. doi:10.1007/s00134-018-5181-1
- Marvin, S., Thibeault, S., & Ehlenbach, W.J. (2019). Post-extubation dysphagia: Does timing of evaluation matter? Dysphagia, 34, 210–219.
- Matsuo, H., Yoshimura, Y., Ishizaki, N., & Ueno, T. (2017). Dysphagia is associated with functional decline during acute-care hospitalization of older patients. Geriatrics & Gerontology International, 17, 1610–1616. doi:10.1111/ggi.12941
- McGrath, B., & Wallace, S. (2014). The UK national tracheostomy safety project and the role of speech and language therapists. Current Opinion in Otolaryngology and Head & Neck Surgery, 22, 181–187.
- McIntyre, M., Doeltgen, S., Dalton, N., Koppa, M., & Chimunda, T. (2021). Post-extubation dysphagia incidence in critically ill patients: A systematic review and meta-analysis. Australian Critical Care, 34, 67–75. doi:10.1016/j.aucc.2020.05.008
- McRae, J., Montgomery, E., Garstang, Z., & Cleary, E. (2019). The role of speech and language therapists in the intensive care unit. Journal of the Intensive Care Society, 0, 1–5.
- Miles, A., McLellan, N., Machan, R., Vokes, D., Hunting, A., McFarlane, M., … Lynn, K. (2018). Dysphagia and laryngeal pathology in post-surgical cardiothoracic patients. Journal of Critical Care, 45, 121–127. doi:10.1016/j.jcrc.2018.01.027
- Mobasheri, M., King, D., Judge, S., Arshad, F., Larsen, M., Safarfashandi, Z., … Darzi, A. (2016). Communication aid requirements of intensive care unit patients with transient speech loss. Augmentative and Alternative Communication, 32, 261–271.
- Moloney, J., & Walshe, M. (2019). Managing and supporting quality-of-life issues in dysphagia: A survey of clinical practice patterns and perspectives in the UK, Ireland and South Africa. International Journal of Language & Communication Disorders, 54, 41–49. doi:10.1111/1460-6984.12429
- National Confidential Enquiry into Patient Outcomes and Death (NCEPOD). (2014). On the Right Trach? A review of the care received by patients who underwent a tracheostomy. Retrieved from http://www.ncepod.org.uk/2014tc.html
- National Institute for Health and Clinical Excellence (NICE) guideline: Rehabilitation after Critical Illness (2009). CG83. London: National Institute for Health and Clinical Excellence. Retrieved from https://www.nice.org.uk/guidance/cg83
- National Institute for Health and Clinical Excellence (NICE) guideline: Rehabilitation after Critical Illness (2017). QS158. London: National Institute for Health and Clinical Excellence. Retrieved from https://www.nice.org.uk/guidance/qs158/resources/rehabilitation-after-critical-illness-in-adults-pdf-75545546693317
- Northcott, S., Simpson, A., Moss, B., Ahmed, N., & Hilari, K. (2017). How do speech-and-language therapists address the psychosocial well-being of people with aphasia? Results of a UK online survey. International Journal of Language & Communication Disorders, 52, 356–373. doi:10.1111/1460-6984.12278
- O’Reilly, A.C., & Walshe, M. (2015). Perspectives on the role of the speech and language therapist in palliative care: an international survey. Palliative Medicine, 29, 756–761.
- Omura, K., Komine, A., Yanagigawa, M., Chiba, N., & Osada, M. (2019). Frequency and outcome of post-extubation dysphagia using nurse-performed swallowing screening protocol. Nurse Critical Care, 24, 70–75.
- Patel, D., Krishnaswami, S., Steger, E., Conover, E., Vaezi, M., Ciucci, M., & Francis, D. (2018). Economic and survival burden of dysphagia among inpatients in the United States. Diseases of the Esophagus, 31, 1–7. doi:10.1093/dote/dox131
- Perren, A., Zürcher, P., & Schefold, J. (2019). Clinical approaches to assess Post-extubation Dysphagia (PED) in the critically ill. Dysphagia, 34, 475–486.
- Royal College of Speech and Language Therapists (RCSLT) (2014). Speech and language therapy in adult critical care - position paper. Retrieved from http://www.rcslt.org/members/publications/publications2/provision_for_critical_care_
- Sharma, A., Minh Duc, N.T., Luu Lam Thang, T., Nam, N.H., Ng, S.J., Abbas, K.S., … Karamouzian, M. (2021). A consensus-based checklist for reporting of survey studies (CROSS). Journal of General Internal Medicine, 36, 3179–3187. doi:10.1007/s11606-021-06737-1
- Swisher, A. (2010). Practice-based evidence. Cardiopulmonary Physical Therapy Journal, 21, 4–4.
- Tembo, C., Higgins, I., & Parker, V. (2015). The experience of communication difficulties in critically ill patients in and beyond intensive care: Findings from a larger phenomenological study. Intensive Critical Care Nursing, 31, 171–178.
- Thomas, L., & Rodriguez, C. (2011). Prevalence of sudden speechlessness in Critical Care units. Clinical Nurse Research, 20, 439–447. doi:10.1177/1054773811415259
- van Snippenburg, W., Kröner, A., Flim, M., Hofhuis, J., Buise, H., Hemler, R., & Spronk, P. (2019). Awareness and management of dysphagia in dutch intensive care units: A nationwide survey. Dysphagia, 34, 220–228. doi:10.1007/s00455-018-9930-7
- Vaismoradi, M., Turunen, H., & Bondas, T. (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing & Health Sciences, 15, 398–405. doi:10.1111/nhs.12048
- Vincent, J., & Creteur, J. (2015). Paradigm shifts in critical care medicine: The progress we have made. Critical Care, 19, 1–6. doi:10.1186/cc14728
- Walshe, M., Ryan, M., & Regan, J. (2017). Screening for dysphagia: Perspectives and practices of speech and language therapists in the republic of Ireland. Folia Phoniatrica et Logopaedica, 69, 226–238. doi:10.1159/000486031
- Ward, E., Morgan, T., McGowan, S., Spurgin, A., & Solley, M. (2012). Preparation, clinical support, and confidence of speech-language therapists managing clients with a tracheostomy in the UK. International Journal of Language and Communication Disorders, 47, 322–332.
- Zuercher, P., Moret, C., Dziewas, R., & Schefold, J. (2019). Dysphagia in the intensive care unit: epidemiology, mechanisms, and clinical management. Critical Care, 23, 1–11. doi:10.1186/s13054-019-2400-2