Abstract
Purpose: To explore how speech-language pathologists and nurses share information about the communication support needs of stroke patients through structured information-sharing routes and to consider how the two disciplines view their roles and interdependencies in addressing these needs.
Method: Speech-language pathologist and nurse information-sharing was explored in context using ethnography. Ethnography has been used by researchers from other disciplines to understand the context of inpatient care, but the methodology has rarely been adopted within speech-language pathology. Fieldwork (357 hours) was carried out on three stroke wards in England for 40 weeks from 2015 to 2017. Data included fieldnotes, interviews with 43 members of speech-language pathology and nursing staff, and the patient records of 19 patients.
Result: The findings provide a thematically organised explanation for how information about communication travelled through structured routes on the wards (meetings, the patient record, bedside signs, education, and nursing handover). Limitations were identified that appear underpinned by disciplinary differences in (1) how speech-language pathologists and nurses engaged with the wards in time and space, and (2) perceptions of roles and interdependencies. Speech-language pathologists routinely used meetings and the patient record to share communication information, however these formal structures were not easily accessible during nurses’ caregiving roles. In addition, both speech-language pathologists (SLPs) and nurses were ambivalent about the usefulness of signage SLPs sometimes left at the bedside for supporting communication. There was little interdependency between SLP and nursing roles in meeting the communication support needs of patients.
Conclusion: In-depth exploration of the context within which SLPs and nurses share information has revealed limitations in the capacity of structured routes to enhance collective knowledge about patients’ communication support needs.
Introduction
Stroke unit care is underpinned by widespread acceptance that the coordinated efforts of stroke-specialist clinicians can improve outcomes for stroke survivors (Rudd, Bowen, Young, & James, Citation2016; Stroke Foundation, Citationn.d.). Integrated working by different professionals involves information exchange through various routes, synchronous and asynchronous (Conn et al., Citation2009). Interactions that occur in the same time frame, such as informal exchanges and meetings are synchronous and those that occur at different times, such as reading an entry in the patient record or leaving an advice sheet in the patient bedspace, are asynchronous. In-depth exploration of how communities (such as stroke teams or professional groups) are organised through the information-sharing routes available to them is helpful for understanding the influence of context on the routine ways professionals do or do not collaborate during their work on wards (Conn et al., Citation2009). Conn and colleagues, as well as other researchers of hospital care, have adopted ethnography to achieve deeper understanding for the complexities associated with interprofessional teamwork (Clarke, Citation2010; Conn et al., Citation2009). Ethnographic methodology aims to create understanding for taken-for-granted aspects of social life through participant observation, collection of different types of data and reflexive attention to the researcher (Hammersley & Atkinson, Citation2019).
Internationally, speech-language pathology research recognises the importance of ward context. Previous research has shown how the communication environment can impede interaction between people with communication support needs and staff in hospitals (e.g. Hersh, Godecke, Armstrong, Ciccone, & Bernhardt, Citation2016; O’Halloran, Hickson, & Worrall, Citation2008). This knowledge subsequently underpins speech-language pathology interventions for educating healthcare professionals to support people with aphasia to communicate whilst in hospital (e.g. Chu, Sorin-Peters, Sidani, De La Huerta, & McGilton, Citation2018). However, despite the known importance of context to the work of speech-language pathologists (SLPs), there is less empirical understanding within the speech-language pathology profession of the effect of context in its wider sense, that is how healthcare professionals operate at interprofessional boundaries to accomplish their roles within a system of care focussed on the patient. Ethnography is rarely used in speech-language pathology research, although SLPs have been participants in ethnographic research, as in a nurse-led ethnography on one stroke ward that revealed the central role of opportunistic interaction to interprofessional practice (Clarke, Citation2010). An example from speech-language pathology research of the strength of ethnography for understanding everyday experience is Susie Parr’s ethnographic observations of people with severe aphasia within their communities (Parr, Citation2007). The rich descriptions in this highly cited paper have been influential in increasing clinician and researcher understanding of the long-term effects of aphasia on social exclusion (Parr, Citation2007). The companion paper to the current manuscript used ethnography to provide an explanation for how synchronous, informal discussion between SLPs and nurses could be interruptive to nurses’ work, leading SLPs to self-limit the amount of information about communication they shared (Barnard, Jones, & Cruice, Citation2021). Arriving at this explanation was contingent upon contextual understanding, derived through immersion of the researcher in the working lives of participants (Barnard et al., Citation2021).
Communication difficulties are known to increase the vulnerability of patients during hospital admissions (NHS England, Citation2017) and there is growing international recognition of the relationship between communication difficulties and patient safety (Hemsley et al., Citation2019; NHS England, Citation2017). Communication-related risks include an increased likelihood of adverse events such as falls (Hemsley et al., Citation2019), risks from not having health needs met or not being involved in decisions (O’Halloran et al., Citation2008) and risks on transition home, such as not being able to alert services (Power et al., Citation2015). In response to such concerns and moves towards increasing patient involvement in healthcare decisions, the National Health Service (NHS) established a Standard for provision of communicatively accessible information in England. The Standard lays out legal requirements for “identifying, recording, flagging, sharing and meeting the information and communication support needs of patients, service users, carers and parents with a disability, impairment or sensory loss” (NHS England, Citation2017, p. 1). The need for patients to be communication-supported to be involved in their care is particularly high on stroke wards. A recent large-scale audit recorded the presence of aphasia and/or dysarthria in 64% of patients after 72 hours of their stroke admission (Mitchell et al., Citation2021). These figures suggest that a substantial proportion of stroke patients can be expected to have difficulties expressing themselves or understanding healthcare professionals. These patients also face less tangible, though equally present, emotional risks with respect to isolation and lack of connection with healthcare practitioners that can have a profound effect on their experience of inpatient stroke care (Clancy, Povey, & Rodham, Citation2020; Loft et al., Citation2019; Pound & Jensen, Citation2018).
Every clinician in the stroke team has a responsibility to communicate with patients in ways that support understanding and expression and meet relational needs (Bright, Kayes, McPherson, & Worrall, Citation2018). Of these team members, SLPs and nurses are arguably the people with most opportunity and capacity to influence patients’ experience of communication in hospital: SLPs through their specialist roles in identifying and managing communication disorders and nurses through continuous presence and proximity to patients. Communication difficulties can make routine nursing care much harder to provide (Clancy et al., Citation2020; Loft et al., Citation2017), for example, locating pain or knowing when patients need the toilet. Nurses aim to provide person-centred, compassionate care to all patients and to “adjust and apply the principles and processes for making reasonable adjustments” for those who are communicatively vulnerable (Nursing & Midwifery Council, Citation2018, p. 14). Provision of education to enable others in the stroke team to support patients’ communication is part of the SLP role (Rudd et al., Citation2016; Stroke Foundation, Citationn.d.), making them key professionals for providing information to nurses and other professionals to make the necessary adjustments.
The primary synchronous interprofessional information-sharing routes explored in stroke research include meetings (Ferguson, Worrall, & Sherratt, Citation2009; Tyson, Burton, & McGovern, Citation2014) and informal, opportunistic exchanges on the ward (Barnard et al., Citation2021; Clarke, Citation2010). Interprofessional meetings are commonly considered to be a key mechanism for integrating knowledge from various professionals, providing an opportunity to share information from assessments, discuss patient progress and plan for discharge (Tyson et al., Citation2014). With respect to information shared about communication in meetings, despite its relevance to all in the team, SLP contributions on this topic have been found to far outweigh those of other disciplines (Ferguson et al., Citation2009). An Australian study found communication to be the second most talked about topic in interprofessional case conferences by SLPs and the 10–13th by other professionals (Ferguson et al., Citation2009). An additional real-time route for sharing information across professional groups is interprofessional training. This has been the focus of most research at the speech-language pathology/nursing interface, through communication partner training for healthcare professionals (e.g. Chu et al., Citation2018).
The patient record is the primary asynchronous route used by clinicians, who may purposefully use written entries to compensate for deficiencies in verbal routes (Lingard et al., Citation2007). However, a recent systematic review found very few studies reporting communication of interprofessional information through writing (Paxino, Denniston, Woodward-Kron, & Molloy, Citation2020). One SLP-led study that did explore the written route reported that the communication-related entries of eight patients who had experienced an adverse event in hospital rarely included advice for how to support communication (Steel et al., Citation2019). A further routine way in which information is shared is nursing handover. Although this is a synchronous route for nurse-to-nurse knowledge-sharing, it is also a route through which interprofessional information passes. That is, nurses filter information gathered from various professionals across a shift when transferring information to colleagues on the next shift (Allen, Citation2014). To the authors knowledge, no previous research has explored the passage of speech-language pathology-relevant information through nursing handover.
Very little is known about how SLPs and nurses share information about patients’ communication support needs during everyday practice on stroke wards. The research questions guiding this paper build on a companion paper, which reported findings about information-sharing through the informal route (Barnard et al., Citation2021). The current paper explores (1) how SLPs and nurses share information through structured routes on stroke units, and (2) how SLPs and nurses perceive their roles and interdependencies with respect to the communication support needs of patients.
Method
This study employed ethnographic methodology. Ethnography was selected because it was anticipated that spending time amongst SLPs and nurses, observing them at work and asking them questions, would lead to in-depth understanding of their information-sharing practices. The methodology was underpinned by social constructionist epistemology. This is the belief that meaning is created through interaction and influenced by the socio-historical positioning of all parties (Crotty, Citation1998). In adopting this position, it is acknowledged that the SLPs and nurses in this study will have talked about and demonstrated their practice through disciplinary lenses, and that meaning so derived was filtered through the disciplinary lens of the researcher (Thorne, Citation2019). Subjectivity was managed through reflections of researcher position and techniques for enhancing credibility, as discussed below. The research objectives were to observe everyday verbal and written information-sharing by SLPs and nurses through fieldwork and to understand their perceptions of roles and interdependencies through interviews. The Standards for Reporting Qualitative Research have been used to ensure transparency, see Supplemental file (O’Brien, Harris, Beckman, Reed, & Cook, Citation2014). More expansive discussion of methods can be viewed in the companion publication (Barnard et al., Citation2021).
Data collection
All data were collected by RB, a SLP by profession with previous experience working in the Trusts but not on the studied wards (Trusts are organising units for NHS services, in this case by geography). It is conventional in ethnographic reporting to use the first person when fore-fronting the role of the researcher in constructing the interpretative account (Clifford, Citation1986). Fieldwork was conducted between 2015 and 2017 on three stroke wards in three hospitals across two inner city NHS Trusts in England for 12–16 weeks on each ward. Wards included one hyper-acute stroke unit (Keats) which accepted patients at stroke onset for around a week, and two acute stroke units (Brooke and Shelley) which accepted patients for continuing inpatient stroke care. Ward names are pseudonyms. Ethical approval was granted by the National Research Ethics Service (15/NW/0271) and the two host NHS Trusts. SLPs and nurses were informed about the research prior to commencing and during periods of fieldwork. The wider stroke team were informed of the study verbally by the consultant at team meetings and through posters on the ward. I distributed a simplified overview of the study to patients in areas I was observing which explained my presence on the wards and the focus on staff.
Participants included SLPs (15), SLP Assistant - SLPA (1), Registered Nurses (50), Nursing Assistants - NAs (7) and Patients (19). I talked potential participants through information sheets prior to obtaining written consent. All 16 SLP staff covering the wards over the fieldwork period were observed and 15 were interviewed (14 SLPs and one SLPA). Sampling was purposive for interviews with nursing staff (24 nurses and 4 NAs) to achieve diversity in gender and grade (in the NHS registered SLPs and nurses are employed at band 5 and above, with increments representing increasing seniority or specialism). The sample for observation of nurses (50) and NAs (7) was dictated by which of the consented nurses were on shift during fieldwork periods. One nurse and one NA declined to participate and one SLP left the Trust before I was able to interview them. Biographical information for staff is provided in composite in to protect identities and research sites. Patients provided written consent for their speech-language pathology and nursing entries in the patient record to be viewed. They were purposively sampled to include a range of severities. The sample included 19 patients, 9 men and 10 women. Of these, 18 had stroke-associated communication difficulties: mild (7), mild/moderate (1), moderate (6), moderate/severe (3), severe (1).
Table I. Participant information.
Fieldwork (357 hours) was conducted on all days of the week between 0715 and 2030, usually for 3–4 hours, ranging between 1 and 12 hours. I observed information-sharing through informal as well as formal, more structured routes. Findings relating to informal interactions have been previously reported (Barnard et al., Citation2021). This manuscript is focussed on structured routes: meetings, the patient record, bedside signs, interprofessional teaching and nursing handover. I noted down actual dialogue of relevance to work at the speech-language pathology-nursing boundary as well as broader contextual observations. I copied entries in the patient record written by SLPs and nurses about communication and swallowing into my notepad as part of the fieldnote data. All fieldnotes were anonymised at the point of collection and typed and expanded at the end of each day. Semi-structured interviews were 21–55 minutes long. They were conducted in quiet spaces away from the ward, audio recorded and personally transcribed. The topic guide evolved iteratively, it included broad topics covered with all participants (information-sharing practices, roles, relationships, and clinical interests in common), and questions generated through ongoing fieldwork, consistent with ethnographic methodology (Hammersley & Atkinson, Citation2019).
I aimed to position myself as an acceptable, yet marginal member of the speech-language pathology and nursing communities (Hammersley & Atkinson, Citation2019), choosing not to adopt a clinical role so as not to overly associate with either profession. I engaged in social interaction and was helpful where possible. I completed a reflexive diary each evening, in which I critically evaluated the influence of my speech-language pathology history on how I was seeing, how others might see me, and the potential impact on research findings. In common with other ethnographers with clinical backgrounds (e.g. Jacoby, Citation2017), I moved back and forth between insider and outsider positions throughout the study. This kept me sufficiently uncomfortable to remain observant of the familiar and the strange, the routine and the exceptional (Hammersley & Atkinson, Citation2019).
Data analysis
An iterative analytic approach was followed, as suggested by Hammersley and Atkinson (Citation2019) for analysing ethnographic data. Data were collected and analysed concurrently, using techniques from the constant comparative method, involving continuous comparisons with other data, both within and across data sources (Glaser & Strauss, Citation1967). Fieldnotes and transcripts were read repeatedly. Open coding was followed by more focussed coding, with continuous revision of categories as additional data were collected (Hammersley & Atkinson, Citation2019). Data management was supported with NVIVO 11 (Citation2015). Once fieldwork was complete, analysis switched to a more fluid paper-based search for patterns and relationships, in which concepts were mapped and patterns and contradictions explored (Thorne, Citation2019) to create a thematically organised explanation.
Techniques to enhance credibility included active search for negative cases, feedback from SLPs and nurses during presentations of preliminary findings, discussion of interpretations and themes with the supervisory team and keeping a reflexive diary. Transferability was increased through explanations that were sufficiently “thick” to enable meaning to be read from the description, and inclusion of multiple sites (Hammersley & Atkinson, Citation2019).
Result
The findings provide an explanation for how information about communication travelled through the formal structures for information-sharing on the stroke wards. Limitations were identified that appear to be underpinned by differences in (1) how the two disciplines engaged with the wards in time and space, and (2) perceptions of roles and interdependencies with respect to the communication support needs of patients. Extracts from observational data are marked as [FN (fieldnote) + date recorded] and quotes from interviews are titled by profession and marked as [pseudonym + (years of experience)]. Extracts from the patient record are marked by patient number and severity of communication disorder. Truncation of extracts is indicated by (…).
Disciplinary differences in experience of structured routes
SLPs were advantaged over nurses in their ability to engage with all structured information-sharing routes. They had more freedom to schedule their own time, giving them more capacity to attend meetings from beginning to end, read and write in the patient record and participate in interprofessional teaching. None of the routes SLPs used were particularly effective for conveying communication information in the context of nursing roles.
Information shared in writing
Written information included entries by SLPs and nurses in the patient record and signs posted by SLPs at the bedside. SLPs were usually observed to flank their sessions with patients by reading and then writing lengthy entries in the notes. Nurses related in interview that unless they had safety concerns (about swallowing), they usually only read what SLPs had written when they were writing their own entries, and in preparation for handover at the end of the shift. Nurses’ entries were usually short and mentions of communication were brief. Nurses consistently reported challenges accessing the patient record due to their need to stay responsive to patients, in physical proximity for most of their shift. Over the course of the shift, they jotted down information from interactions with SLPs and other professionals and referred to them when writing in the patient record. I commonly saw nurses write key bits of information in the margins of their handover sheets whilst SLPs shared information, but only for swallowing, for example “1–2 sips, syrup thick only” [FN18052017].
SLPs’ communication entries were much less clearly signalled as being written for the purpose of informing the work of others than swallowing entries. Of the patient records examined, communication information mostly comprised descriptions of assessments, interventions, or goal progress. Only 13/61 SLP communication entries (21%) included advice that appeared to be intended to advise how communication could be supported. This contrasts with entries about swallowing, in which 67/71 (94%) included an advisory component. Nurses’ entries about communication in the patient record revealed nursing-focussed assessment, through language such as “incomprehensible sounds” from the Glasgow Coma Scale, and labels such as “aphasia”, “word finding difficulty”, or “confusion”. Communication was loosely alluded to in entries such as “nil complaint of pain voiced or noted” or “call bell within reach”, however it was difficult to judge if these were purposeful attempts to share information about communication. Nurses occasionally referenced the impact of communication difficulty on emotion, such as “gets frustrated at times due to dysphasia”. Only one patient record was viewed that revealed intent from a nurse to share a communication support strategy:
Nurse entry in the patient record
Pt (patient) voices concerns successfully through writing (…) unable to speak words clearly (…) impaired verbal communication (…) to communicate needs through alternative ways (…) established rapport, introduced self to patient, patiently waits for patient to finish what he wants to say, provided pen and paper to assist patient in communicating his needs [P4 - severe dysarthria].
Although this was an exceptional case, it created an opportunity to examine what drove this higher level of written information about communication from nursing. There were two distinguishing factors. First, despite having significantly reduced intelligibility due to dysarthia, the patient had a strong need to communicate and would call staff over to him, rather than sit passively. Second, the patient’s use of writing was unambiguously helpful. Whilst seeking consent from the patient to view his notes, we chatted. There was no paper at the bedside and when I provided some he wrote: “I breath when some one talk to me (sic)”. His writing provided a window to his emotions that I found very affecting. I searched the six SLP entries in this patient’s record for reference to the strategy and found it mentioned in one entry (recorded in the “subjective” (S) component of the SOAP notes). The entry read “pt using gesture (ineffectively) and writing to communicate”. The remaining SLP communication entries focussed on describing his communication deficits within the “objective” (O) or “assessment” (A) sections. There was no reference to the strategy in the “plan” (P). In contrast, all six of the swallowing entries included swallowing advice under “P”.
An additional written route was a sign SLPs posted at the bedside. SLPs used signs consistently for swallowing and sometimes for communication. Nurses highly valued the swallowing signs but did not always notice, or make use of, communication signs. During a quiet time on the ward, I questioned a nurse about the signs:
Observation on the ward
She said she uses the swallowing signs. When I asked about the communication information, she said she hadn’t seen it much. I said that (patient name) has communication advice and she went over to the bed and came back and acknowledged it was there. I asked her why she doesn’t pay much attention to this advice, and she said that she goes to the patient and talks to them and that she knows to keep to yes and no. It seems that she basically just works it out for herself [FN01072016].
Nurses reported that they may be driven by expediency to focus on completing tasks, particularly when it was not clear how to make use of the advice given by SLPs. However, this came at a cost to nurses’ values for providing compassionate care. The following extract clearly conveys that signage is unlikely to positively impact on patient care if not adequately backed with verbal discussion or education.
Nurse interview
Even if they plan, and put it smart on the paper there, if they haven’t like coached us on how to do it, then we still won’t be able to communicate, we just go there and do and leave (…) because the nurse is also struggling on how to communicate, then you look like you don’t want to talk to people, whereas you don’t know how to communicate with a person [Nyasha 22y].
Sometimes SLPs left communication ramps (such as picture charts) for patients, however nurses were not always clear how to make use of them. One of the nurses gave an example of a time when she had not understood the SLP’s explanation of a patient’s communication difficulty and was therefore unsure how to use the communication chart left at the bedside.
Nurse interview
She then made him a, you know a chart, with the signs (…). It was a really, really, busy day, and I just remember thinking I don’t really know what this impairment is, I don’t really know how I’m going to use this chart (…) I don’t know if I’ve got the time to help him to get better in that way [Claire 1y]
Nonetheless, when I asked nurses in interview what might help them communicate with patients, they often mentioned charts and signs. One of the SLPs explained her perception that nurses valued charts because they created a sense of doing something. She thus continued to give them to patients despite lacking conviction that nurses would use them. When noticed, signs and charts appeared to function as a flag for the presence of a communication difficulty, with little power as a tool for supporting patients to communicate.
Information sharing through meetings: an uneven floor
SLPs and nurses worked different hours and differed in their responsibility for the same patients across the trajectory of their admission. This created an uneven floor in meetings. Nurses commonly presented information that was second-hand, either because they had only just started nursing the patient on that shift or because they represented the patients of other nurses. Other than when covering absence, SLPs usually presented their own patients and could draw on first-hand experience to share profession-specific knowledge. The following field extract is an example of the type of communication information commonly shared by SLPs.
Observation of SLP contribution in meeting
Still severely aphasic and possibly apraxic (…) some odd words but largely they’re jargon (…) family say he’s saying more with them [FN06102015]
Because nurses’ knowledge was often second-hand, it was harder for them to show certainty and expertise during team discussion, and they were commonly less forthcoming than other professionals in contributing experiential knowledge. For example, following the information presented by the SLP in the extract above, other professionals contributed perspectives on this patient’s level of understanding, but the nurse did not. When discussing a different patient in the same meeting it was a physiotherapist and not a nurse who extended discussion about how the patient communicated pain. After the meeting I asked the nurse what would lead him to contribute to discussions of this kind. He said he would contribute if he disagreed. He restricted his input to the meeting for reasons of brevity, adding that limited first-hand knowledge of patients made it difficult to share specialist knowledge. Nurses also had no real way of anticipating what would be considered relevant and thus they often shared information without conviction. For example, information about how well a patient slept was sometimes ignored by others, and sometimes considered relevant to another piece of rehabilitation information and picked up for discussion. When nurses passed information from the meeting back to their colleagues at the bedside, it was abbreviated and less nuanced.
A further difference between the disciplines related to nurses’ capacity to leave patient care to attend meetings. On Keats and Brooke, senior nurses stayed for the duration of the meeting and represented all the patients. On Shelley, the nurses allocated to the patients on that shift transitioned in and out of the meeting. On all wards nurses tended to keep working on the ward until the last moment. Often when everyone else was seated at the allotted meeting time, I would hear “do we have a nurse” and someone would go and search for one. Overall, interprofessional meetings appeared to be more useful to the clinical work of professionals who presented their own patients and were able to stay for the duration.
In keeping with the discharge-orientation of meetings, the bulk of the communication information SLPs presented was more focussed on diagnosis, prognosis or goal progression than advising staff on how to meet patients’ communication support needs. This was in line with the orientation of all professionals in the meeting towards succinct information focussed on describing the evolving conditions of patients and their progression towards discharge. SLPs did sometimes suggest how staff could meet patients’ communication support needs. For example, the SLP in the following extract concludes her confident assertion of the patient’s swallow-related needs with a suggestion of a route to connect with the patient, articulated with less conviction.
Observation of SLP contribution in meeting
I reassessed his swallow (…) has still got secretions that he coughed out (…). Can we keep going with the nebs (doctors discuss if this is needed, but SLT persists). Can we give him saline nebs (…) we’re putting him on half portions of puree with caution (…) so can you watch his chest (…), starting to vocalise now (…) if you want to get him chatting, he works as a [occupation] (spoken quietly, as an aside) [FN13102016]
Information sharing through education
Brooke and Shelley scheduled in-service interprofessional education each week, at which SLPs sometimes presented communication-related topics. However, nurses rarely attended. Nurses’ decision-making for attendance appeared to be based on a complex interplay between time, capacity, and calculations of the cost versus the benefit of taking time away from patients. The senior nurse in the following extract reveals logistical problems in releasing staff:
Nurse interview
I’m sorry but safety’s first, I can’t send anyone. Just one person? No. Because at that time somebody might be on break, two people are on break. Otherwise, we’ll be on breaks at 6 o clock in the afternoon [Grace 10y].
SLPs reported that their only teaching targeted towards nurses in their current posts related to swallowing. Few nurses could recall having received any post-registration education about communication and knowledge was often quite loose. For example, descriptors were often imprecise, such as writing or saying “confusion” or “slurred speech” for aphasia. Reduced knowledge had implications for the ongoing transfer of information. I heard a nurse transferring a patient to another hospital over the phone stating “expressive dysphagia” as a communication difficulty, revealing that inaccurate information recorded in the patient record and on handover sheets could carry through the patient admission and onto the nurse at the receiving hospital. SLPs attempted to provide education informally but could be tentative when sharing their specialist knowledge. The following extract reveals a concern for over-stepping the mark:
SLP Interview
I’ll say something like, “so they’ve probably got aphasia, so they’re having difficulty with understanding language or finding the right words”, so just very short little bits of education, which they may well know, but so trying not to say it in a way that I’m you know teaching them something they knew, but just kind of just reinforcing something [Amanda 5y].
During interview several nurses said they would welcome education to fill gaps in their knowledge, however, it was evident that such education would need to accommodate their limited capacity to leave patient care.
Perceptions of communication roles
The SLPs in this study considered assessment and management of communication to be integral to their roles and identity, as revealed in entries in the notes, contributions at meetings and reflections of their roles during interview. However, their concern for the communication support needs of patients existed in a context in which swallowing was prioritised.
SLP interview
The swallow screen standard makes you focus in on the swallowing, but you know, new communication disturbance is really, really, distressing for patients [Pam 27y].
Most, but not all, of the nursing staff interviewed were aware that SLPs had responsibility for communication. Nevertheless, speech-language pathology work with communication could be viewed as somewhat separate from nursing concerns:
Nurse interview
(SLP role with patients is) to help them communicate better and to express themselves as well, like maybe toilet, they want to go toilet and so they will practice with them to say like toilet, toilet, toilet, or even find different words to help them, but we’re not that involved with that to be honest [Fatima 1y].
During interview, nurses often found it hard to articulate a specific role with patients with communication difficulties. Their emphasis was on creating friendly relationships with all patients. Communication was seen as a taken-for-granted aspect of nursing care that was central to easing patients’ distress at being in hospital, increasing cooperation with care, and reducing frustration. Nurses reported that they would show care to patients with communication support needs by explaining what they were doing and skilfully observing them to determine their needs. A response was not necessarily expected.
Nurse interview
So we show them we are together, whatever you are going through we’re here for you (…) our job is to look at them as well, to look on their eyes, expression and then pick up some information from that (…) so if they can’t say they’re in pain and I see they become agitated, you start to look and do blood pressure, you try to find out if there is anything wrong (…) if there is medication on (the chart) you give their medication and see if it’s going to help (…) Sometimes it’s hard to get it right [Maryam 8y].
Observations during nursing handover indicated that nurses tended to treat communication-related issues as intra-nursing concerns, usually raised in the context of patient agitation, confusion, or refusal or when difficulties understanding patients slowed task completion. For example, when one nurse lamented to her colleagues that she had spent fifteen minutes trying to understand what a patient was trying to say, it was understood as a significant challenge to nursing tasks. Very occasionally nurses would direct nursing colleagues to communication advice in bedside signs during handover, but they rarely oriented to SLPs as a resource to support their work with patients with communication support needs. This contrasted with swallowing, where SLP recommendations and the need for SLP input were commonly flagged during handover.
Discussion
In-depth exploration of information-sharing between SLPs and nurses generated new understanding for how the two disciplines used structured routes to share information about communication and explained how the acute stroke context limited the effectiveness of these routes. Disciplinary experiences of information-sharing differed in accordance with access to the various routes and whether information related to communication or swallowing. The theoretical perspective applied to the findings is Orlikowski and Yates (Citation1994) contention that the social organisation of a community is revealed through how members communicate through the “genre repertoire” available to them, that is, the combination of information-sharing routes. Rhetorical genre studies view habitual use of genres as shaping and shaped by the actions and beliefs of members of a community; genres “teach users how to think and how to act in specific situations” (Varpio, Schryer, & Lingard, Citation2009, p. 478). Viewing information-sharing routes in this way goes beyond classification, it emphasises how genres interact to create, maintain, and potentially change, cultural practices (Orlikowski & Yates, Citation1994).
Although SLPs often had more capacity than nurses to make full use of the information-sharing routes available, the effectiveness of these routes for eliciting nurses’ views or informing them about communication support needs was limited. Determining whether information-sharing is synchronous or asynchronous is not as straightforward as it appears. A good illustration is interprofessional meetings, which are known to disadvantage nurses (Barnard, Jones, & Cruice, Citation2020). Given that interprofessional meetings are a key route for stroke professionals to build collective knowledge of patients (Tyson et al., Citation2014), it is important to forefront the extent to which nurses’ experience of this genre differs from that of other professionals. Because many nurses do not attend, a whole group of professionals routinely experience the information that passes through this genre as asynchronous. This uneven playing field is also true of other genres. Although on the face of it the patient record was an asynchronous genre available to all, nurses at the bedside had less time to read it. Similarly, nurses had less opportunity to attend scheduled teaching and learn alongside other professionals.
As in previous research, the SLPs in this study viewed communication roles as core to their professional identity despite acknowledging that others valued their swallowing roles more highly (Foster, O’Halloran, Rose, & Worrall, Citation2016). The patient record appeared to be the place where they could most expansively demonstrate their expertise with communication and assert their identity as communication specialists. However, the information shared was primarily deficit focussed. When professionals expect diagnostic labelling for classification or prognostic purposes to be positively received, they are likely to act in accordance with that perception (Abbott, Citation1988). This resonates with research in which SLPs perceived language assessment to be the aspect of their communication specialism that was most valued by others in acute care (Foster et al., Citation2016). SLP communication entries included much less information overtly intended to advise the actions of others than seen with swallowing information, consistent with previous research, which also found very little advice for supporting communication in the entries of patients with communication disorders (Steel et al., Citation2019). Their purpose appeared more archival than intentionally informative (Allen, Citation2014). The focus on deficit may reflect where SLPs direct their assessment attention. Increased advice for supporting communication might be seen if tools to assess communicative ability in the context of the inpatient environment were more commonly used, such as the Inpatient Functional Communication Interview (O’Halloran, Worrall, Toffolo, & Code, Citation2020).
Efforts by clinicians to overcome deficiencies in one route by exploiting another have been reported in previous research. For example, an ethnographic study across two general medical wards in Canada indicated that clinicians used the patient record to work around barriers to sharing information verbally (Lingard et al., Citation2007). However, use of writing to compensate for challenges with other genres may lack impact, given the difficulties experienced by nurses in accessing the patient record during direct care-giving roles. As Lingard and colleagues suggest “over time the problem and the workaround become a normalized part of team practice” (Lingard et al., Citation2007, p. 665). SLPs would benefit from considering the purpose of their entries in the patient record. If they are intended to influence the communicative experience of patients, advice for supporting communication should be signalled as such and supplemented through multiple genres, as seen with swallowing information.
The written information SLPs left at the bedside was, on the face of it, compatible with nurses’ need to stay proximal to patients. However, nurses paid little attention to signs about communication and SLPs themselves did not expect them to have much impact. In contrast, nurses consistently valued and used bedside signs for swallowing. Previous research has suggested that interprofessional information posted around the bedside may be little used by nurses unless there is some overlap with verbal information (Conn et al., Citation2009). SLPs routinely used overlapping genres for swallowing advice; they posted signs at the bedside, which they backed up verbally and through entries in the patient record. In comparison, communication signs were weakly related to other genres. The same genre (the bedside sign) was treated differently depending on its content (Varpio et al., Citation2009).
Nurses’ inattention to communication signs was set within a wider context in which neither SLPs nor nurses routinely saw the other as a key resource for managing communication support needs (Barnard et al., Citation2021). Interdependence is “the degree to which team members depend on each other for both individual and team task completion” (West & Lyubovnikova, Citation2013, p. 137). Interdependence was more evident in roles relating to swallowing. Disciplinary boundaries with communication roles may be harder to discern because communication is not a discrete activity. Whilst communication assessment and management are specific aspects of SLP role, communication is integral to all nurses’ activities with all patients.
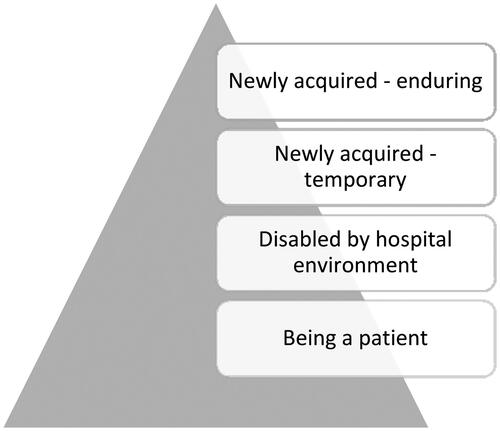
Communication support needs could be conceptualised as layered (). At the base layer are aspects that are universally important. Effective communication requires time spent talking to patients and nurturing compassionate, connected, caring relationships; the relational environment is important with or without communication impairment (Bridges et al., Citation2013; Bright et al., Citation2018; Pound & Jensen, Citation2018). Next are needs that are created or exacerbated by being a patient in hospital, such as speaking a different language or when proficient users of communication aids cannot access their devices (O’Halloran et al., Citation2008). Above this are newly acquired impairments that may be temporary. For example, speech lost due to mechanical ventilation in intensive care (O’Halloran et al., Citation2008). At the top are communication difficulties that may require lifelong adjustment, such as aphasia (Clancy et al., Citation2020; Loft et al., Citation2019). Because communication is intrinsic to nursing roles at every layer of the triangle, the nurses in this study may have found it anomalous to be asked to articulate a specific communication role with patients at the upper layer. Nurses aim to combine a compassionate approach with completion of nursing tasks with all patients (Bridges et al., Citation2013) and this requires skills in managing communication across every layer. If SLPs and nurses were to draw more effectively on the respective expertise of each other, their collective knowledge of the communication needs of the patients in their care could potentially increase.
Supporting communication in a context of time pressures and resource constraints can be challenging for all stroke professionals (Bright et al., Citation2018; Clancy et al., Citation2020; Loft et al., Citation2017). SLP advice for meeting patients’ communication support needs could be strengthened by bolstering the genre repertoire for communication information. However, for SLPs and nurses to routinely share knowledge with each other, both need to see the clinical value of investing the effort (Barnard et al., Citation2020). It is suggested that SLPs and nurses create some space to discuss what information about patients’ communication would be meaningful for execution of their roles and the most impactful way to share it. The profile of communication could potentially be raised if both disciplines fore fronted the physical and emotional risks of not addressing communication support needs (Hemsley et al., Citation2019; Loft et al., Citation2019). SLP assessment and treatment can inform specific strategies, and nursing knowledge of communication in-context and vulnerabilities can enhance holism (Pound & Jensen, Citation2018). Their combined forces have potential to enhance knowledge amongst the stroke team for improving the communicative experience of patients.
Limitations and future directions
The use of ethnography in this study made it possible to gather in-depth understanding of information-sharing in context on three different wards. This cannot be considered a comprehensive account of all that occurred during the field work periods as I was not present for every interaction that took place on the wards. However, the methodology enabled me to use interviews to ask participants if observations were routine or exceptional. The role of the researcher in shaping the knowledge created is both a limitation and a strength of ethnographic research. Practitioner-researchers inevitably filter experience through a disciplinary lens (Thorne, Citation2019). However, my socio-historical biography gradually shifted to incorporate nursing perspective and new ways of viewing my own profession as I commenced fieldwork on new wards. This generated unique insights that indicate the value of ethnography for understanding practice more generally. Healthcare professionals could learn much about the contexts they take for granted by spending time observing for the purpose of understanding, leaving professional agendas to one side. Bringing such learning into clinical supervision and cross-disciplinary discussion could be a catalyst for changes in practice. New understanding for the importance of context can inform future interventions. For example, ensuring communication partner training has support for embedding learning in-context built in (Chu et al., Citation2018) or routinely offering brief periods of education about communication within nursing space. Nurses could potentially be more involved in delivery of such education, drawing on their experience of patients’ communication at all layers of the triangle. Further research is recommended to explore how the genres available for sharing information about patients’ communication support needs could better underpin efforts to enhance the communication environment.
Conclusion
This ethnographic study has revealed limitations in the capacity of structured routes to enhance collective knowledge amongst SLPs and nurses about patients’ communication support needs. SLPs shared information describing deficits and progress more comprehensively than information intended to advise others in supporting communication. Overall, the potential for SLPs and nurses to influence the communication environment for patients was under-exploited.
Declaration of interest
No potential conflict of interest has been declared by the authors.
Supplemental material
Supplemental data for this article can be accessed at https://doi.org/10.1080/17549507.2022.2034944.
References
- Abbott, A. (1988). The system of professions: An essay on the division of expert labour. Chicago and London: University of Chicago Press.
- Allen, D. (2014). Re-conceptualising holism in the contemporary nursing mandate: From individual to organisational relationships. Sociology of Science and Medicine, 119, 131–138. doi:10.1016/j.socscimed.2014.07.036
- Barnard, R., Jones, J., & Cruice, M. (2020). Communication between therapists and nurses working in inpatient interprofessional teams: Systematic review and meta-ethnography. Disability and Rehabilitation, 42, 1339–1349. doi:10.1080/09638288.2018.1526335
- Barnard, R., Jones, J., & Cruice, M. (2021). When interactions are interruptions: An ethnographic study of information-sharing by speech and language therapists and nurses on stroke units. Disability and Rehabilitation, 2021, 785. doi:10.1080/09638288.2021.1871785
- Bridges, J., Nicholson, C., Maben, J., Pope, C., Flatley, M., Wilkinson, C., … Tziggili, M. (2013). Capacity for care: Meta-ethnography of acute care nurses’ experiences of the nurse-patient relationship. Journal of Advanced Nursing, 69, 760–772. doi:10.1111/jan.12050
- Bright, F.A.S., Kayes, N.M., McPherson, K.M., & Worrall, L.E. (2018). Engaging people experiencing communication disability in stroke rehabilitation: A qualitative study. International Journal of Language and Communication Disorders, 53, 981–994. doi:10.1111/1460-6984.12409
- Chu, C.H., Sorin-Peters, R., Sidani, S., De La Huerta, B., & McGilton, K.S. (2018). An interprofessional communication training program to improve Nurses’ ability to communicate with stroke patients with communication disorders. Rehabilitation Nursing, 43, E25–E34. doi:10.1097/rnj.0000000000000041
- Clancy, L., Povey, R., & Rodham, K. (2020). “Living in a foreign country”: Experiences of staff-patient communication in inpatient stroke settings for people with post-stroke aphasia and those supporting them. Disability and Rehabilitation, 42, 324–334. doi:10.1080/09638288.2018.1497716
- Clarke, D.J. (2010). Achieving teamwork in stroke units: The contribution of opportunistic dialogue. Journal of Interprofessional Care, 24, 285–297. doi:10.3109/13561820903163645
- Clifford, J. (1986). In J. Clifford & G. Marcus (Eds). Writing culture: The poetics and politics of ethnography. California: University of California Press.
- Conn, G.L., Lingard, L., Reeves, S., Miller, K., Russell, A., & Zwarenstein, M. (2009). Communication channels in general internal medicine: A description of baseline patterns for improved interprofessional collaboration. Qualitative Health Research, 19, 943–953. doi:10.1177/1049732309338282
- Crotty, M. (1998). The Foundations of Social Research. London: SAGE; 1998.
- Ferguson, A., Worrall, L., & Sherratt, S. (2009). The impact of communication disability on interdisciplinary discussion in rehabilitation case conferences. Disability and Rehabilitation, 31, 1795–1807. doi:10.1080/09638280902810984
- Foster, A., O’Halloran, R., Rose, M.L., & Worrall, L. (2016). “Communication is taking a back seat”: speech pathologists’ perceptions of aphasia management in acute hospital settings. Aphasiology, 30, 585–608. doi:10.1080/02687038.2014.985185
- Glaser, B.G., & Strauss, A.L. (1967). The discovery of grounded theory: Strategies for qualitative research. New York: Aldine.
- Hammersley, M., & Atkinson, P. (2019). Ethnography: Principles in practice. Oxon: Routledge.
- Hemsley, B., Steel, J., Worrall, L., Hill, S., Bryant, L., Johnston, L., … Balandin, S. (2019). A systematic review of falls in hospital for patients with communication disability: highlighting an invisible population. Journal of Safety Research, 68, 89–105. doi:10.1016/j.jsr.2018.11.004
- Hersh, D., Godecke, E., Armstrong, E., Ciccone, N., & Bernhardt, J. (2016). “Ward talk”: Nurses’ interaction with people with and without aphasia in the very early period post stroke. Aphasiology, 30, 609–628. doi:10.1080/02687038.2014.933520
- Jacoby, S.F. (2017). The insight and challenge of reflexive practice in an ethnographic study of black traumatically injured patients in Philadelphia. Nursing Inquiry, 24, e12172. doi:10.1111/nin.12172
- Lingard, L., Conn, L.G., Russell, A., Reeves, S., Miller, K.-L., Kenaszchuk, C., & Zwarenstein, M. (2007). Information work: Innovations in the use of the chart on internal medicine teams. Journal of Interprofessional Care, 21, 657–667. doi:10.1080/13561820701731817
- Loft, M.I., Martinsen, B., Esbensen, B.A., Mathiesen, L.L., Iversen, H.K., & Poulsen, I. (2019). Call for human contact and support: An interview study exploring patients’ experiences with inpatient stroke rehabilitation and their perception of nurses’ and nurse assistants’ roles and functions. Disability and Rehabilitation, 41, 396–404. doi:10.1080/09638288.2017.1393698
- Loft, M.I., Poulsen, I., Esbensen, B.A., Iversen, H.K., Mathiesen, L.L., & Martinsen, B. (2017). Nurses’ and nurse assistants’ beliefs, attitudes and actions related to role and function in an inpatient stroke rehabilitation unit-A qualitative study. Journal of Clinical Nursing, 26, 4905–4914. doi:10.1111/jocn.13972
- Mitchell, C., Gittins, M., Tyson, S., Vail, A., Conroy, P., Paley, L., & Bowen, A. (2021). Prevalence of aphasia and dysarthria among inpatient stroke survivors: Describing the population, therapy provision and outcomes on discharge. Aphasiology, 35, 950–960. doi:10.1080/02687038.2020.1759772
- NHS England. (2017). Accessible Information Standard. https://www.england.nhs.uk/ourwork/accessibleinfo/
- Nursing and Midwifery Council. (2018). Future nurse: Standards of proficiency for registered nurses. https://www.nmc.org.uk/globalassets/sitedocuments/education-standards/future-nurse-proficiencies.pdf
- NVIVO 11 (2015). QSR International Pty Ltd.
- O’Brien, B.C., Harris, I.B., Beckman, T.J., Reed, D.A., & Cook, D.A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine, 89, 1245–1251. doi:10.1097/ACM.0000000000000388
- O’Halloran, R., Hickson, L., & Worrall, L. (2008). Environmental factors that influence communication between people with communication disability and their healthcare providers in hospital: A review of the literature within the International Classification of Functioning, Disability and Health (ICF) framework. International Journal of Language & Communication Disorders, 43, 601–632. doi:10.1080/13682820701861832
- O’Halloran, R., Worrall, L., Toffolo, D., & Code, C. (2020). The inpatient functional communication interview: Screening, assessment, and intervention. San Diego: Plural Publishing Inc.
- Orlikowski, W.J., & Yates, J. (1994). Genre repertoire: The structuring of communicative practices in organizations. Administrative Science Quarterly, 39, 541–574. doi:10.2307/2393771
- Parr, S. (2007). Living with severe aphasia: Tracking social exclusion. Aphasiology, 21, 98–123. doi:10.1080/02687030600798337
- Paxino, J., Denniston, C., Woodward-Kron, R., & Molloy, E. (2020). Communication in interprofessional rehabilitation teams: A scoping review. Disability and Rehabilitation, 2020, 271. doi:10.1080/09638288.2020.1836271
- Pound, C., & Jensen, L.R. (2018). Humanising communication between nursing staff and patients with aphasia: Potential contributions of the humanisation values framework. Aphasiology, 32, 1225–1233. doi:10.1080/02687038.2018.1494817
- Power, E., Thomas, E., Worrall, L., Rose, M., Togher, L., Nickels, L., … Clarke, K. (2015). Development and validation of Australian aphasia rehabilitation best practice statements using the RAND/UCLA appropriateness method. BMJ Open, 5, e007641. doi:10.1136/bmjopen-2015-007641
- Rudd, A.G., Bowen, A., Young, G., James, M.A. (2016). National Clinical Guideline for Stroke: 5th edition. Clinical Medicine. https://www.rcplondon.ac.uk/guidelines-policy/stroke-guidelines
- Steel, J., Georgiou, A., Balandin, S., Hill, S., Worrall, L., & Hemsley, B. (2019). A content analysis of documentation on communication disability in hospital progress notes: Diagnosis, function, and patient safety. Clinical Rehabilitation, 33, 943–956. doi:10.1177/0269215518819717
- Stroke Foundation [internet]. (n.d.). Clinical Guidelines for Stroke Management. Australia: https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management
- Thorne, S. (2019). Interpretative Description. New York: Routledge. 2016.
- Tyson, S.F., Burton, L., & McGovern, A., (2014). Multi-disciplinary team meetings in stroke rehabilitation: An observation study and conceptual framework. Clinical Rehabilitation, 28, 1237–1247. doi:10.1177/0269215514535942
- Varpio, L., Schryer, C.F., & Lingard, L. (2009). Routine and adaptive expert strategies for resolving ICT mediated communication problems in the team setting. Medical Education, 43, 680–687. doi:10.1111/j.1365-2923.2009.03395.x
- West, M.A., & Lyubovnikova, J. (2013). Illusions of team working in health care. Journal of Health Organization and Management, 27, 134–142. doi:10.1108/14777261311311843