Abstract
Aim: What is the prevalence of using lubricants and medication to enhance erectile function among older adults, and what predicts such use?
Methods: Survey data were collected in probability samples among 60–75 year olds in Norway, Denmark, Belgium, and Portugal.
Results: In men, the use of medication was highest in Norway (26%) and lowest in Portugal (12%). In women, the use of lubricants was highest in Norway (31%), and lowest in Belgium (3%). Compared to those who had no sexual difficulties, the use of medication/lubricants were higher in individuals with sexual difficulties.
Conclusion: The findings contribute to an increased attention to the sexual health of older adults.
Introduction
Research has consistently shown that significant barriers exist for seeking help for sexual difficulties in older adults (Nicolosi et al., Citation2006). For various reasons, including the fear of offending the older patient, health professionals often wait for patients to bring up the topic themselves (Hinchliff & Gott, Citation2004; Traeen & Schaller, Citation2010). Patients, on the other hand, also face barriers, such as not feeling there is enough time to bring up the topic during consultations for other medical conditions or being in a place or context that is ill-suited for discussions related to sexuality (Schaller et al., Citation2018).
Sexual activity often ceases or decreases following major illness (Allen & Desille, Citation2017; DeLamater, Citation2012; Erens et al., Citation2019; Steptoe et al., Citation2016; Traeen et al., Citation2017, Citation2018). According to Erens et al. (Citation2019), 26.9% of British men and 17.1% of British women aged 55–74 years reported having a health condition or problem that negatively impacted their sexual activity or satisfaction. Of those, 38.0% of the men and 45.7% of the women had not been sexually active in the past 6 months, and only two in five men and women indicated that they were satisfied with their sex lives. Furthermore, among those with a health condition affecting their sexuality, 28.6% of men and 20.5% of women reported having sought help or advice about their sex life in the past year (Erens et al., Citation2019), and 33.1% of men reported taking medication (e.g., sildenafil) in the past year to enhance erectile function. The use of sildenafil or other medication was not significantly associated with sexual satisfaction, however, perhaps because the use of sildenafil or other medication was associated with varying degrees of improvement of erectile function and with varying degrees of satisfaction (Erens et al., Citation2019).
Erectile function can be impacted by a number of factors, including aging, health problems and disease (or their treatment), lifestyle, and psychological states such as anxiety or depression (Allen & Desille, Citation2017; Traeen et al., Citation2017). Most studies show that the prevalence of erection difficulties increases with age (Erens et al., Citation2019; Field et al., Citation2013; Rosen et al., Citation2016; Schick et al., Citation2010). In a representative population-based survey from Norway, the incidence of erectile problems ranged from 2% among men aged 18–29 to 34% among men aged 60–67 years (Traeen & Stigum, Citation2010). Similarly, findings based on a national representative study in Denmark showed an increase in erectile difficulties from 1% among those under 50 years of age to 15% among men age 60 years or older (Christensen et al., Citation2011). That the prevalence of erectile dysfunction increases with age seems to be a consistent finding across countries (Laumann et al., Citation2005; Lee et al., Citation2016; Lindau et al., Citation2007). However, the extent to which older men use medications to enhance erectile function is understudied and poorly understood.
In the AARP Survey of Midlife and Older Adults, approximately 5% of men aged 45 or older reported that they had taken any prescription medication to enhance erectile function in the previous 6 months (Fisher, Citation2010). In another study, based on a nationally representative probability sample of older adults from the U.S., roughly one in seven men aged 57–85 years reported taking medication or supplements to increase erectile function in the past year (Lindau et al., Citation2007). Similarly, findings from the National Survey of Sexual Health and Behavior (NSSHB), also based on a nationally representative probability sample, found that 17% of men (50+) had taken medication to enhance erectile function during the latest partnered sexual encounter (Schick et al., Citation2010). Moreover, the use of such medications increased from 8% at ages 50–59 years to 30% at ages 60–69 years but dropped to 23% among 70–79 year olds. Among men who had engaged in partnered sexual activity in the past year, the use of erectile medication significantly predicted erectile difficulty.
In women, the vaginal mucosa becomes thinner, and thus more vulnerable to ruptures during vaginal intercourse. A common finding among aging women is a higher probability of lubrication difficulties with increasing age (Field et al., Citation2013; Lee et al., Citation2016; Schick et al., Citation2010). In a multi-country study, including 13,882 adult women age 40–80 years from 29 countries, Laumann et al. (Citation2005) found a curvilinear association between age and the probability of lubrication problems in all world regions, with the exception of South America and Southeast Asia. Compared to women aged 40–49 years the likelihood of experiencing lubrication difficulties was approximately three times higher among women age 60–69 years during perimenopause and menopause across most regions, including Northern and Southern Europe (OR = 2.8), the non-European West (OR = 1.6), the Middle East (OR = 3.2), and East Asia (OR = 3.3). Yet, women age 70 or older were no more likely to experience problems with lubrication than women aged 40–49 years. These findings seem to be quite similar to the pattern of lubricant use in aging women. A recent, nationally representative population-based survey conducted in the U.S. found that older women more frequently use lubricants than younger women, with the exception of women above 70 years (Herbenick et al., Citation2014). Among the oldest age group (70+ years) only 55% of women had ever used any lubricant, while roughly 7 in 10 women (63–73%) in the younger cohorts (25–69 years) reported some lifetime lubricant use. The most frequently reported motive why older women initially started to use lubricants was “to make sex more comfortable” (55% among those aged 60–69 years and 64% among those aged 70+ years). “Approaching menopause” and “to make sex feel more wet” were also frequently mentioned. In addition to age, Herbernick et al. (2014) also found that lubricant use was significantly higher among women who were Caucasian, had higher education, and who engaged in sexual intercourse more frequently.
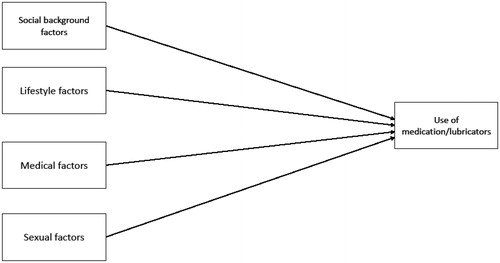
The current study aimed to assess the prevalence of using medication to enhance erectile function and use of lubricants among older adults across Europe, and to explore predictors of such use. The statistical analyses were guided by the conceptual model presented in . In this exploratory gender-specific model, the use of medication to enhance erectile function in men, and the use of lubricants during intercourse in women, is considered to be influenced by four sets of factors: social background factors, lifestyle factors, medical factors, and sexual factors. Social background factors were operationalized as age and level of education; lifestyle factors as weekly alcohol consumption; medical factors as cardio-vascular diseases, diabetes, prostate cancer in men, and in women ovary and breast cancer and use of hormone replacement therapy, and lastly, sexual factors were operationalized as sexual activity during the past month and the experience of sexual difficulties for at least 3 months during the past year (erectile difficulties in men, pain during intercourse in women).
Figure 1. A conceptual model for use of medication to enhance erectile function (in men), and use of lubricators during sex (in women). Note: Social background factors are operationalized as age and level of education; lifestyle factors are weekly alcohol consumption; medical factors (cardio-vascular diseases, diabetes, prostate cancer in men/ovary and breast cancer and use of hormone replacement therapy in women); sexual factors are sexual intercourse activity during the past month, and experience of sexual difficulties of at least 3 months duration the past year (erectile difficulties in men, pain during intercourse in women).
Methods
Participants
The Department of Psychology at the University of Oslo, in cooperation with the poll organization IPSOS (Institut de Publique Sondage d’Opinion Secteur), led a multinational survey on the sexual lives of 60–75-year-olds in probability samples of the population in Norway, Denmark, Belgium, and Portugal. The net sample size in Norway was n = 1271, Denmark n = 1045, Belgium n = 991, and Portugal n = 509. The majority of participants identified as heterosexual, and only 1.9% were identified as gay, lesbian or bisexual, and 3.2% marked themselves as “other”.
Procedure and Recruitment
Based on previous studies on potentially sensitive topics, the data collection was carried out by means of anonymous postal questionnaire questionnaires. The questionnaire consisted of 66 main questions. Most of the included questions and scales in the questionnaire were adapted from previous studies among the target group, for instance from NATSAL-3 (Mitchell et al., Citation2013). An overview of the included questions and scales is given elsewhere (Traeen et al., Citation2018). The questionnaire was developed in English and subsequently translated into local languages translated by the principal investigators and persons employed by IPSOS in each country.
After the translation of into native languages was finalized, randomized telephone recruitment of participants started from October to December 2016. Trained interviewers at IPSOS made the phone calls after guidance. The interviewer introduced himself/herself and the project, and asked to talk 2–3 min with a person in the household who was aged 60–75 years. All answers were treated confidentially and no names could be connected to the answers given. Those who agreed to participate were told they would receive a questionnaire send by mail along with a stamped, preaddressed envelope. They were told the questionnaire would take about 20 min to fill in, and that the answers given were treated strictly confidential, in the sense that no names were to be written on the questionnaire and no one would be able to link the responses to individuals. It was emphasised that replies from singles were equally important as replies from people living as couples, and answers from those who have no sex life were as important as from those who have. Further, participants were asked if they lived with alone or with a spouse. Those who lived with a partner in the age 60–75 years were asked if their partner also would like to participate in the survey. If the participant’s response was affirmative, the trained interviewer contacted the spouse. The questionnaires were to be filled independently and returned separately. Due to the possibility of interdependence, all analyses are conducted separately for men and women.
National phone registries were used for recruitment in Norway, Denmark, and Belgium. Nearly the whole population in these countries is accessible by telephone (landline and mobile phone numbers). This enabled IPSOS to draw random and representative samples of the target group, provided that the names, addresses and age of the person specified correspond to the telephone subscriber. Thus, the initial gross samples were selected with the same quality as samples from national population registers in all countries except Portugal. In Portugal, a complete and updated telephone register does not exist. For this reason, IPSOS used the “common routine” for telephone surveys in Portugal when recruiting as follows: (1) telephone numbers were first randomly selected from fixed phone directories and IPSOS’ own database of phone numbers; (2) to obtain a distribution representative of the population, participants were selected by age and gender; and (3) due to illiteracy problems, participants who had not completed primary school (ISCED 1) were excluded from the sample.
The gross sample comprised 7607 persons (1865 in Norway, 2000 in Denmark, 1742 in Belgium, and 2000 in Portugal). The study was conducted among all who had agreed to participate in the telephone interview. The questionnaires were sent back by a freepost envelope to return the completed questionnaire. Two reminders were sent starting one week after the questionnaire was received. Following further discussion with IPSOS in Portugal, it was decided to provide reminders by phone. Unfortunately, 502 potential participants could not be reached by phone. Of the 1498 individuals contacted by phone, 561 refused to participate after having seen the questionnaire. Overall, the response rates were 68% in Norway, 52% in Denmark, 57% in Belgium, and 26% in Portugal.
Ethics approval was handled by IPSOS in accordance with European standards. The ethical procedures followed the standards of The European Society for Opinion and Market Research (ESOMAR), as stated in the general contract with the University of Oslo. By the standards of ESOMAR, IPSOS is obliged to follow national and international rules and guidelines for what is recognized as a professionally sound market analysis. The rules comprise treatment of confidentiality, respondent anonymity, questionnaires and databases and methods for data collection etc. It is also referred as the ethical rules for The Norwegian Association of Marketing and Opinion Research. All participants who returned completed questionnaires received a small gift from IPSOS for their efforts.
Measures
Outcome variables
Use of lubricants was assessed by the question, “In general, do you and your partner use any lubricants during sexual activity?” The response categories were 0 = No and 1 = Yes.
Use of medication was assessed by the question, “Have you or your partner ever taken any type of medicine or pills to assist your sexual performance, for example Viagra, Cialis, Levitra or Spedra?” The response categories were 0 = No and 1 = Yes.
Predictor variables
Age was measured as a continuous variable in years.
Level of education was assessed as the highest level of formal education. In three countries, the response categories were 1 = Primary school (6–8 years at school), 2 = Lower secondary school (9–10 years at school), 3 = Higher secondary school, high school (12–13 years at school), 4 = College, lower university level (bachelor’s degree level or similar), and 5 = Higher university level (master’s degree, PhD or similar). In Belgium, additional response alternatives were added to mirror the educational system in the country. To allow for cross-cultural comparisons, the variable was recoded into 1 = Primary (1), 2 = Secondary (2 + 3), and 3 = Tertiary education (4 + 5).
Alcohol consumption was assessed by the question “On average, how many alcoholic beverages do you consume in a typical week? Number of glasses of beer?/Number of glasses of wine?/Number of glasses of Port wine, Sherry etc?/Number of glasses of spirits?” The variable was created as a sum score of the responses to the four sub questions.
Medical factors were assessed by sub-questions under the heading “Has a doctor ever told you that you have any of the medical conditions listed below? Tick all that apply.” The variable Cardio-vascular diseases was created from those who ticked affirmatory for Arthritis/Heart attack/Coronary artery disease, angina, other form of heart disease/Hypertension, also known as high blood pressure/Stroke. Those with experience of cardio-vascular diseases were coded 1, and those with no experience were coded 0. With regard to Diabetes, those with the disease were coded 1, and those without disease 0. Prostate cancer—men who ticked for benign prostatic hypertrophy and prostate cancer were coded 1, and men with no disease were coded 0. In women, those who ticked for cancer in the uterus or ovaries, and breast cancer, were coded 1, and those with no disease were coded 0 (Ovary and breast cancer). Another question raised for women were “Have you ever taken hormone replacement therapy (HRT)?” The response categories were 0 = No, and 1 = Yes.
Sexual difficulties were measured under the heading “In the last year, have you experienced any of the following for a period of 3 months or longer?” Eight items of sexual difficulties were presented to the respondents. Both men and women responded to the item “Felt physical pain as a result of sex.” Only men were presented with the item “Had trouble getting or keeping an erection,” and only women with the item “Had an uncomfortably dry vagina.” The response categories to all items were 0 = No, and 1 = Yes.
Sexual activity was assessed by the question: “How many times have you had or attempted sexual intercourse (vaginal, anal or oral sex) during the past month?” Response options for the question ranged from 1 = None to 7 = More than once a day, and as very few ticked for the latter category, the variable was recoded to 6 = Daily.
Statistical analysis
Using SPSS 24.0, bivariate and multivariate logistic regression analyses were carried out on weighted data (DuMouchel & Duncan, Citation1983). Based on census data, weighting was used to adjust for the unequal probabilities of selection in terms of age and gender. All data analyses were performed separately for men and women to avoid intercorrelations due to inclusion of heterosexual couples. For each country, we used binary logistic regression to calculate age-adjusted odds ratios to investigate how reporting of the outcome variable varied by the predictors.
Results
shows the prevalence of the use of medication to enhance erectile function in men, and the use of lubricants during sex in women. The use of medication was highest in Norwegian men (26.2%) and lowest in Portuguese men (12.4%) (p < 0.001). There were no other statistically significant differences in the reporting. However, women’s reporting of lubrication was systematically higher than men’s reporting, and men’s reporting of erectile enhancement medication was systematically higher than women’s reporting.
Table 1. Use of lubricants and use of drugs like Viagra, Cialis, Levitra, or Spedra to assist erectile function in 60–75-year-old men and women (%).
shows the prevalence of the use of medication to enhance erectile function and lubricants in men with and without erectile difficulties. In men with erectile difficulties, the use of medication was highest in Norwegian men (41.6%) and lowest in Portuguese men (17.7%). Except for Norwegian men, there were no other statistically significant differences in the reporting of use of lubrication. More Norwegian men with erectile difficulties (29.9%) than without erectile difficulties (19.3%) used lubricants.
Table 2. Use of lubricants during sexual activity, and if men ever have taken any type of medicine or pills such as Viagra, Cialis, Levitra, or Spedra to assist erectile function, in 60–75-year-old males with and without erection difficulties (%).
shows the prevalence of the use of medication to enhance erectile function and lubricants in women with and without lubrication difficulties. There were statistically significant differences in the use of lubricants between women with and without lubrication difficulties in all countries, but no difference in the reporting of use of medication. In women with lubrication difficulties, the use of lubricants was highest in Norwegian women (47.5%) and lowest in Portuguese women (41.6%). There were no other statistically significant differences in the reporting of use of medication.
Table 3. Use of lubricants during sexual activity, and men ever have taken any type of medicine or pills such as Viagra, Cialis, Levitra, or Spedra to assist erectile performance, in 60–75-year-old females with and without lubrication difficulties (%).
shows the bivariate relationships between the use of medication and selected predictors in men. In Norwegian, Belgian and Portuguese men, the use of medication was significantly higher in men who had had prostate cancer compared to men who did not have cancer. In Danish and Belgian men, the use of medication was higher among those who had had cardio-vascular diseases and diabetes. Frequency of sexual intercourse was also associated with use of medication in Belgian men. Lastly, alcohol consumption was lowest in Norwegian men and highest in Danish and Belgian men, and the level of anxiety was fairly equal across countries. The multivariate logistic regression analysis in men () showed that compared to Norwegian men, use of medication was 0.4 times lower in Portugal and 0.6 times lower in Belgium. Compared to men who had no erectile difficulties, the odds of using medication were 5.8 times higher for those with erectile difficulties. Furthermore, compared to men who did not have diabetes, the likelihood of using medication was 1.95 times higher in diabetes patients. Lastly, the likelihood of using medication increased with 1.02 for every glass increase in weekly alcohol consumption, and with 1.22 for every unit increase in intercourse frequency the past month.
Table 4. The use of medication to improve erectile function in 60–75-year-old men, by selected predictors (n = 1027).
Table 5. The use of medication to improve erectile function in 60–75-year-old men, by selected predictors (n = 1027).
shows the bivariate relationships between use of lubricants and selected predictors in women. Across all countries, more women who had pain difficulties during intercourse than those who did not report the use of lubrication. Even so, it is worth noticing that 41–55% of women with pain issues did not use lubricants. In Danish and Portuguese women, the use of lubricants was more prevalent in those who had been in hormone replacement therapy than their counterparts. The multivariate logistic regression analysis in women () showed that compared to women who did not have pain difficulties, the odds of using lubricants were 3.81 times higher in those with pain difficulties. Furthermore, compared to women who did not have hormone replacement therapy, the likelihood of using lubricants was 1.74 times higher in those who were on hormonal replacement therapy. The likelihood of using lubricants increased with 1.17 for every unit increase in intercourse frequency.
Table 6. The use of lubricants during sex in 60–75-year-old women, by selected predictors.
Table 7. The use of lubricants during sex in 60–75-year-old women, by selected predictors (n = 829).
Discussion
This study set out to explore the prevalence of the use of medication to enhance erectile function among older adult men, and the use of lubricants among older women in Norway, Denmark, Belgium, and Portugal. It is somewhat difficult to compare the results from this study directly with other studies, as the use of medication and lubricants are measured differently. However, the findings on both the use medication (Erens et al., Citation2019; Fisher, Citation2010; Lee et al., Citation2016; Schick et al., Citation2010), and lubricants (Laumann et al., Citation2005), in this study are within the same range as what is found in previous studies. Interestingly, women’s reporting of lubrication use was systematically higher than men’s, and men’s reporting of the use of erectile medication was systematically higher than women’s. This suggests that the use of lubricants and erectile medication is still a sensitive and secretive topic in many relationships, something perceived as private and not to be shared with one’s partner.
We found cross-cultural difference in the use of medication to enhance erectile function in men. We found that more than twice as many men in Norway than men in Portugal, both in total and for those reporting erectile difficulties, had used medication. The multivariate logistic regression analysis in men showed that compared to Norwegian men, the use of erectile function enhancing medication was significantly lower in Portugal and Belgium. The cross-cultural differences in use of medication may be due to differences in accessibility of medication, or healthcare personnel’s awareness of sexual problems in older adult patients.
The findings from this study indicate that the use of medication to enhance erectile function is higher in groups of men who had been diagnosed with diseases known to be associated with erectile difficulties. For instance, bivariate analyses showed that in Norway, Belgium, and Portugal, the use of medication was significantly higher in men who had had prostate cancer as compared to men who did not have cancer. In Danish and Belgian men, the use of medication was higher among those who had had cardiovascular disease or diabetes. The multivariate analysis showed that the odds of using medication were higher for those with erectile difficulties, in diabetes and prostate cancer patients, higher in men who had a higher weekly consumption of alcohol, and higher in those with more frequent sexual activity compared to their respective counterparts. The cross-cultural differences in the use of medication may be due to differences in accessibility of medication, or healthcare personnel’s awareness of sexual problems in older adult patients. It is also possible that differences in men’s reports of medication use could be the result of reporting bias, and that the use of medication is more stigmatized in more southern European countries.
We found no statistically significant cross-cultural difference in women’s reporting of use of lubricants. However, also in women the use of lubricants was higher with sexual problems. Significantly more women with lubrication difficulties than without such problems reported use of lubricants. Across all countries, women with pain difficulties during intercourse were more likely to use lubricants than those who did not experience pain problems; however, nearly one out of two women with pain issues did not use lubricants. The multivariate analysis in women showed that, after controlling for other factors, the use of lubricants was significantly higher in women who had pain difficulties, who were on hormone replacement therapy, and those who reported higher frequencies of sexual activity. The latter finding confirms previous findings which have found that lubricant use was significantly higher among women who engaged in sexual intercourse more frequently (Herbenick et al., Citation2014).
Lastly, it is worth noticing that women’s reporting of lubricants was systematically higher than men’s reporting, and men’s reporting of erectile enhancement medication was systematically higher than women’s reporting of such use. This indicates that men tend to underestimate lubricant use, and women tend to underestimate men’s use of medication.
Some limitations of this four-country study should be considered. It is likely that individuals holding more liberal views around sexuality have been more willing to participate in the study than those more traditional-minded (Dunne, Citation2002). Such a bias may be reflected in the results, implying underestimated rates of use of medication and lubricants. One issue related to cross-cultural differences and similarities may be important; namely, that of the use of medication and lubricants were not explicitly defined for the participants, and people from different countries may have interpreted the questions differently. Furthermore, this study was not designed to study of use of medication and lubricants per se, and thus contained only a single broad question utilized in exploring such use. Accordingly, we have no knowledge of the type of medication used, and the frequency of use. Finally, owing to a small number of aging non-heterosexual persons, generalizations of findings to self-identified non-heterosexuals, or other sexual minorities, may be precluded (de Vries, Citation2007).
Conclusion
Ideally, healthcare personnel should ask their patients about their sex life, and erectile function in older people should be taken seriously (Worly et al., Citation2018). Even though sexuality is important to many older adults’ well-being and quality of life, sexual health in older men and women has received little public health attention (DeLamater, Citation2012; Erens et al., Citation2019; Gott & Hinchliff, Citation2003). The findings from this study may contribute to an increased attention to the sexual health of older adults, and how to improve it.
Funding
This research was fully financed by the Norwegian Research Council under the grant number 250637.
Additional information
Funding
References
- Allen, M. S., & Desille, A. E. (2017). Health-related lifestyle factors and sexual functioning and behavior in older adults. International Journal of Sexual Health, 29 (3), 273–277. https://doi.org/10.1080/19317611.2017.1307301
- Christensen, B. S., Grønbaek, M., Osler, M., Pedersen, B. V., Graugaard, C., & Frisch, M. (2011). Sexual dysfunctions and difficulties in Denmark: Prevalence and associated sociodemographic factors. Archives of Sexual Behavior, 40(1), 121–132. https://doi.org/https://doi.org/10.1007/s10508-010-9599-y
- de Vries, B. (2007). LGBT couples in later life: A study in diversity. Generations, 31, 18–23.
- DeLamater, J. (2012). Sexual expression in later life: A review and synthesis. Journal of Sex Research, 49(2–3), 125–141. https://doi.org/https://doi.org/10.1080/00224499.2011.603168
- DuMouchel, W. H., & Duncan, G. J. (1983). Using sample survey weights in multiple regression analyses of stratified samples. Journal of the American Statistical Association, 78, 535–543. https://doi.org/https://doi.org/10.1080/01621459.1983.10478006
- Dunne, M. P. (2002). Sampling considerations. In M. W. Wiederman & B. E. Whitley Jr. (Eds.), Handbook for conducting research on human sexuality (pp. 85–112). Mahwah, NJ: Lawrence Erlbaum.
- Erens, B., Mitchell, K. R., Gibson, L., Datta, J., Lewis, R., Field, N., & Wellings, K. (2019). Health status, sexual activity and satisfaction among older people in Britain: A mixed methods study. PLOS One, 14(3): e0213835. https://doi.org/https://doi.org/10.1371/journal.pone.0213835
- Field, N., Mercer, C. H., Sonnenberg, P., Tanton, C., Clifton, S., Mitchell, K. R., Erens, B., Macdowall, W., Wu, F., Datta, J., Kyle G Jones, K. G., Stevens, A., Prah, P., Copas, A. J., & Johnson, A. M. (2013). Associations between health and sexual lifestyles in Britain: Findings from the third national survey of sexual attitudes and lifestyles (natsal-3). The Lancet, 382(30), 1830–1844. https://doi.org/https://doi.org/10.1016/S0140-6736(13)62222-9
- Fisher, L. (2010). Sex, romance and relationships: AARP survey of midlife and older adults. AARP.
- Gott, M., & Hinchliff, S. (2003). How important is sex in later life? The views of older people. Social Science & Medicine, 56(8), 1617–1628. https://doi.org/https://doi.org/10.1016/S0277-9536(02)00180-6
- Herbenick, D., Reece, M., Schick, V., Sanders, S. A., & Fortenberry, J. D. (2014). Women’s use and perceptions of commercial lubricants: Prevalence and characteristics in a nationally representative sample of American adults. Journal of Sexual Medicine, 11(3), 642–652. https://doi.org/https://doi.org/10.1111/jsm.12427
- Hinchliff, S., & Gott, M. (2004). Perceptions of well-being in sexual ill health: what role does age play? Journal of Health Psychology, 9(5), 649–660.
- Laumann, E. O., Nicolosi, A., Glasser, D. B., Paik, A., Gingell, C, Moreira, E., & Wang, T. for the GSSAB Investigators’ Group (2005). Sexual problems among women and men aged 40-80 years: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. International Journal of Impotence Research, 17, 39–57. https://doi.org/https://doi.org/10.1038/sj.ijir.3901250
- Lee, D., Nazroo, J., O’Connor, D., Blake, M., & Pendleton, N. (2016). Sexual health and well-being among older men and women in England: Findings from the English Longitudinal Study of Ageing. Archives of Sexual Behavior, 45(1), 133–144. https://doi.org/https://doi.org/10.1007/s10508-014-0465-1
- Lindau, S. T., Schumm, L. P., Laumann, E. O., Levinson, W., O’Muircheartaigh, C. A., & Waite, L. J. (2007). A study of sexuality and health among older adults in the United States. The New England Journal of Medicine, 357(8), 762–774. https://doi.org/https://doi.org/10.1056/NEJMoa067423
- Mitchell, K. R., Mercer, C. H., Ploubidis, G. B., Jones, K. G., Datta, J., Field, N., Copas, A. J., Tanton, C., Erens, B., Sonnenberg, P., Clifton, S., Macdowall, W., Phelps, A., Johnson, A. M., & Wellings, K. (2013). Sexual function in Britain: Findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). The Lancet, 382, 1817–1829. DOI: https://doi.org/10.1016/S0140-6736(13)62366-1
- Nicolosi, A., Buvat, .J, Glasser, D. B., Hartmann, U., Laumann, E. O., & Gingell, C. (2006). Sexual behaviour, sexual dysfunctions and related help seeking patterns in middle-aged and elderly Europeans: The global study of sexual attitudes and behaviors. World Journal of Urology, 24(4), 423–428. https://doi.org/https://doi.org/10.1007/s00345-006-0088-9
- Rosen, R., Heiman, J., Long, J., Fisher, W., & Sand, M. (2016). Men with sexual problems and their partners: Findings from the International Survey of Relationships. Archives of Sexual Behavior, 45(1), 159–173. https://doi.org/https://doi.org/10.1007/s10508-015-0568-3
- Schaller, S., Traeen, B., & Kvalem, I. L. (2018). Barriers and facilitating factors in helpseeking: A qualitative study on how older adults experience talking about sexual issues with healthcare personnel. International Journal of Sexual Health. https://doi.org/https://doi.org/10.1080/19317611.2020.1745348
- Schick, V., Herbenick, D., Reece, M., Sanders, S. A., Dodge, B., Middlestadt, S. E., & Fortenberry, J. D. (2010). Sexual behaviors, condom use, and sexual health of Americans over 50: Implications for sexual health promotion for older adults. The Journal of Sexual Medicine, 7(1), 315–329. https://doi.org/https://doi.org/10.1111/j.1743-6109.2010.02013.x
- Steptoe, A., Jackson, S. E., & Wardle, J. (2016). Sexual activity and concerns in people with coronary heart disease from a population-based study. Heart, 102(14), 1095–1099. pmid:27126394
- Traeen, B., Hald, G. M., Graham, C. A., Enzlin, P., Janssen, E., Kvalem, I. L., Carvalheira, A., & Štulhofer, A. (2017). Sexuality in older adults (65+) – An overview of the literature, part 1: Sexual function and its difficulties. International Journal of Sexual Health, 29(1), 1–10. https://doi.org/https://doi.org/10.1080/19317611.2016.1224286
- Traeen, B., & Schaller, S. (2010). Sexual well-being in Norway 2008. International Journal of Sexual Health, 22, 180–194.
- Traeen, B. & Stigum, H. (2010). Sexual problems in 18-67-year-old Norwegians. Scandinavian Journal of Public Health, 38(5), 445–456. https://doi.org/https://doi.org/10.1177/1403494810371245
- Traeen, B., Štulhofer, A., Janssen, E., Carvalheira, A. A., Hald, G. M., Lange, T., & Graham, C. (2018). Sexual activity and sexual satisfaction among older adults in four European countries. Archives of Sexual Behavior, 48(3), 815–829. https://doi.org/10.1007/s10508-018-1256-x
- Traeen, B., Štulhofer, A., Jurin, T., & Hald, G. M. (2018). Seventy-five years old and stillgoing strong: stability and change in sexual interest and sexual enjoyment in men and women across Europe. International Journal of Sexual Health, 30(4), 323–336. https://doi.org/10.1080/19317611.2018.1472704
- Worly, B., Manriquez, M., Stagg, A., Blanchard, M. H., Ogburn, T., Carson, S., & Woodland, M. B. (2018). Sexual health education in OB-Gyn residencies – The program Directors’ survey. International Journal of Sexual Health, 30(4), 390–397. https://doi.org/10.1080/19317611.2018.1527425
