ABSTRACT
The cellular isoform of prion protein, designated PrPC, is a membrane glycoprotein expressed most abundantly in the brain, particularly by neurons, and its conformational conversion into the abnormally folded, amyloidogenic isoform, PrPSc, is an underlying mechanism in the pathogenesis of prion diseases, a group of neurodegenerative disorders in humans and animals. Most cases of these diseases are sporadic and their aetiologies are unknown. We recently found that a neurotropic strain of influenza A virus (IAV/WSN) caused the conversion of PrPC into PrPSc and the subsequent formation of infectious prions in mouse neuroblastoma cells after infection. These results show that IAV/WSN is the first non-prion pathogen capable of inducing the conversion of PrPC into PrPSc and propagating infectious prions in cultured neuronal cells, and also provide the intriguing possibility that IAV infection in neurons might be a cause of or be associated with sporadic prion diseases. Here, we present our findings of the IAV/WSN-induced conversion of PrPC into PrPSc and subsequent propagation of infectious prions, and also discuss the biological significance of the conversion of PrPC into PrPSc in virus infections.
Introduction
Conformational conversion of the cellular isoform of prion protein, designated PrPC, into its abnormally folded, amyloidogenic isoform PrPSc, is a key pathogenic event in prion diseases, or transmissible spongiform encephalopathies, a group of fatal neurodegenerative disorders including Creutzfeldt-Jakob disease (CJD) in humans and scrapie and bovine spongiform encephalopathy (BSE) in animals [Citation1–3]. PrPSc is a β-sheet-rich molecule, with propensity to easily aggregate to form fibrils, and is relatively protease-resistant and detergent insoluble [Citation4]. PrPC is a membrane glycoprotein anchored to the plasma membrane via a glycosylphosphatidylinositol moiety and expressed most abundantly in the brain, particularly by neurons, and to lesser extents in other various non-neuronal tissues [Citation5–7]. PrPC is detergent-soluble and sensitive to protease digestion and structurally consists of two domains, the flexible non-structural N-terminal domain and the globular C-terminal domain with two short β-sheets and three α-helices [Citation6,Citation7]. Structural transition from α-helices to β-sheets has been proposed to be an underlying mechanism of the conformational conversion of PrPC into PrPSc [Citation4].
Prion diseases in humans manifest as sporadic, hereditary, and acquired disorders [Citation8]. The most common human prion disease, accounting for 85–90% of the total cases, is sporadic CJD (sCJD) [Citation9–11]. The aetiologies of sCJD remain unknown. 10–15% of cases belong to hereditary prion diseases, such as familial CJD, Gerstmann-Sträussler-Scheinker syndrome, and fatal familial insomnia [Citation12,Citation13]. These diseases are causatively linked to specific mutations in the PrP gene (Prnp) [Citation12,Citation13]. It has been postulated that mutated PrP molecules are structurally unstable, thereby going through conformational changes to form a PrPSc structure. The remaining cases, accounting for less than 1%, are those of acquired prion diseases, which include iatrogenic CJD (iCJD), variant CJD (vCJD), and kuru [Citation14,Citation15]. These diseases are caused by intra- or inter-species transmission of proteinaceous infectious particles, termed ‘prions’, which are believed to mainly consist, if not entirely, of PrPSc molecules. PrPSc molecules assemble to form an oligomeric structure, which has been considered to be the molecular nature of a prion, functioning as a seed or scaffold to recruit PrPC and forcing its conformational conversion into PrPSc through a seeded polymerization mechanism [Citation16,Citation17]. iCJD is a disease caused by human-to-human transmission of prions via medical treatments or procedures [Citation14]. vCJD is believed to be caused by transmission of prions from BSE [Citation14]. Kuru is a disease spread among Fore people via ritualistic cannibalism in Papua New Guinea [Citation15].
Many recent lines of research have suggested that virus infections might be a risk factor for many neurodegenerative diseases, including Alzheimer’s disease and Parkinson’s disease [Citation18–22]. It has been also reported that virus glycoproteins, including SARS-CoV-2 spike S glycoprotein, could enhance intercellular spreading of the pathogenic protein aggregates in exosomes through interaction with their cognate cellular receptors [Citation23], further demonstrating the relevance of virus infections to the pathogenesis of protein aggregate-associated neurodegenerative disorders. We have recently found that infection with neurotrophic influenza A virus (IAV) induced the conformational conversion of PrPC into PrPSc and the subsequent formation of infectious prions in cultured neuronal cells [Citation24]. These results show that neurotropic IAV is the first non-prion pathogen that is able to induce the conversion of PrPC into PrPSc and propagate infectious prions in cultured cells, raising the intriguing possibility that IAV infection in neurons might be a cause of or be pathogenetically associated with sporadic prion diseases, including sCJD. Here, we introduce our current findings of the neurotropic IAV-triggered conversion of PrPC into PrPSc and formation of infectious prions, and discuss its biological significance in virus infections.
Neurotropic IAV infection in PrP conversion and prion propagation
Here, we pose the hypothesis that certain virus infections might affect the conformation of PrPC, thereby structurally destabilizing PrPC to undergo conformational conversion into PrPSc. Mouse neuroblastoma N2a cells are widely used for prion infection experiments because they are highly susceptible to various prions, provoking the conformational conversion of PrPC into PrPSc as well as propagating prions after prion infection [Citation25,Citation26]. The prion susceptibility of N2a cells is markedly enhanced by overexpressing PrPC in the cells [Citation26]. We previously established a N2a cell line, termed N2aC24, which expresses transduced mouse PrPC at high levels and showed that N2aC24 cells were highly susceptible to RML and 22 L scrapie prions, producing large amounts of PrPSc after prion infection [Citation27]. Therefore, to explore our hypothesis, we infected N2aC24 cells with a neurotropic strain of influenza A/WSN/33 (H1N1) virus (hereafter referred to as IAV/WSN) [Citation24]. We found that N2aC24 cells were highly susceptible to IAV/WSN infection, undergoing massive cell death after infection [Citation24]. To our surprise, proteinase K (PK)-resistant fragments of PrP were detectable in N2aC24 cells infected with IAV/WSN at a low multiplicity of infection of 0.01 at 7 and 8 days post-infection on Western blotting with large amounts of total proteins (300 μg proteins) from the cell lysate [Citation24]. Immunofluorescent staining of the cells with 132 anti-PrP monoclonal antibody, which has been demonstrated to specifically recognize PrPSc in prion-infected cells under partially denaturing conditions, also showed positive signals [Citation24]. These results indicate that IAV/WSN infection could destabilize the protein structure of PrPC, then triggering its conformational conversion into PrPSc in N2aC24 cells.
We found that a small portion of IAV/WSN-infected N2aC24 cells survived the infection and grew continuously. We termed the surviving cells as N2aC24R1 cells and passaged them at a 1:10 ratio. The PK-resistant PrP fragments became clearly detectable in N2aC24R1 cells on Western blotting even with lower amounts of total proteins (30 μg proteins) of the cell lysates at passage 1, and they were increased up to passage 10 [Citation24], indicating that the PK-resistant PrP molecules are propagating in N2aC24R1 cells. In contrast, no PK-resistant PrP was observed in N2aC24 cells even after IAV/WSN infection when IAV/WSN infection was blocked by anti-IAV/WSN mouse antisera or the anti-influenza agent oseltamivir [Citation24]. These results not only confirm that IAV/WSN infection is essential for inducing the conversion of PrPC into PrPSc in N2aC24 cells, but also rule out the possibility of the contamination of laboratory prions in the cell culture. We also showed that intracerebral inoculation with cell lysates from N2aC24R1 cells into mice caused prion disease, with PrPSc accumulation and spongiosis degeneration in their brains [Citation24]. Taken together, these results indicate that IAV/WSN infection could induce the conformational conversion of PrPC into PrPSc and the subsequent formation of infectious prions in N2aC24 cells.
Possible mechanism for IAV/WSN-induced PrP conversion
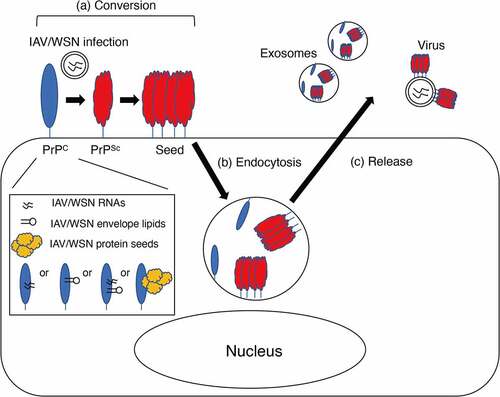
We showed that IAV/WSN infection induced the conversion of PrPC into PrPSc in parental N2a cells, which express only endogenous mouse PrPC [Citation24], indicating that overexpression of PrPC is dispensable for IAV/WSN infection to induce the conversion of PrPC into PrPSc. Interestingly, IAV/WSN proteins examined, including HA, NS and M2, were no longer detectable in N2aC24R1 cells [Citation24], indicating that persistent IAV/WSN infection is not necessary to maintain the conversion of PrPC into PrPSc in N2aC24R1 cells. It is thus conceivable that PrPSc molecules nascently converted from PrPC in N2aC24 cells after IAV/WSN infection might form oligomeric aggregates, or PrPSc seeds, subsequently recruiting other PrPC molecules to them to convert them into PrPSc without the help of IAV/WSN and thereby enabling the constitutive conversion of PrPC into PrPSc in N2aC24R1 cells even after IAV/WSN infection is cleared ()). IAVs are negative-stranded, segmented, enveloped RNA viruses [Citation28]. RNA and lipid molecules have been shown to bind to recombinant PrP and convert it into PK-resistant PrP [Citation29,Citation30]. Furthermore, in vitro PrPSc amplification techniques such as protein misfolding cyclic amplification (PMCA) or quaking-induced conversion techniques have shown that RNA and lipid molecules function as a cofactor for the conversion of PrPC into PrPSc and the propagation of infectious prions [Citation31]. It is thus possible that IAV/WSN-derived RNA or lipid molecules might play a role as a cofactor in the conversion of PrPC into PrPSc in IAV/WSN-infected N2aC24 cells ()). However, it was reported that RNA molecules from invertebrate species including bacteria, yeast, worms, and flies failed to convert PrPC into PrPSc in PMCA [Citation32]. It is thus interesting to investigate if IAV/WSN-derived RNA molecules might be able to function as a cofactor for the conversion of PrPC into PrPSc in PMCA. Protein sequence analysis of eukaryotic viruses have identified many prion-like domains in various viral proteins [Citation33]. Among IAV proteins, RNA-directed RNA polymerase catalytic subunit (PB1), polymerase basic protein 2 (PB2), and neuraminidase were shown to contain prion-like domains [Citation33]. It is thus interesting to speculate that the prion-like domains of these IAV proteins might function as a seed for PrPC to undergo conformational conversion into PrPSc ()).
Figure 1. Possible effects of virus infections on various steps of PrPSc propagation. (a) IAV/WSN infection induces the conversion of PrPC into PrPSc, subsequently forming PrPSc seeds. IAV/WSN-derived RNA or lipid molecules or the protein seeds of IAV/WSN-derived proteins, such as PB1, PB2, and neuraminidase, might bind to and convert PrPC into PrPSc. (b) Infection with murine parvovirus stimulates intracellular internalization of PrPSc seeds in mouse A9 fibroblasts. (c) Molony murine leukaemia virus facilitates the incorporation of PrPSc into virus particles or exosomes, thereby increasing the release of PrPSc from 22L scrapie prion-infected NIH3T3 cells. Vesicular stomatitis virus glycoprotein and SARS-CoV-2 spike S might enhance intercellular spreading of exosomal PrPSc through interaction with their cognate cellular receptors.
Other virus infections in PrP conversion
Several reports have shown that virus infections could affect the inter- and intra-cellular dynamics of PrPSc in prion-infected cells. Infection with murine minute DNA virus, a murine parvovirus, in mouse A9 fibroblasts was shown to enhance the binding of exogenously added PrPSc molecules on the cell surface and stimulate their intracellular internalization ()) [Citation34]. Molony murine leukemia virus was also reported to facilitate the incorporation of PrPSc into virus particles or exosomes, thereby increasing the release of PrPSc into the culture medium of 22L scrapie prion-infected NIH3T3 cells ()) [Citation35]. It is thus possible that virus infections might increase the conversion rate of PrPC into PrPSc, by increasing the accessibility of PrPC to PrPSc through enhancing the cell surface binding of PrPSc molecules and stimulating their internalization to lysosomal compartments, where PrPSc is supposed to convert PrPC into PrPSc, and/or increasing the release of PrPSc from prion-infected cells to prion-uninfected neighboring cells (). Indeed, co-infection with scrapie prions and mouse adenovirus was reported to accelerate prion disease in mice, compared to infection with scrapie prions alone [Citation36]. The Cork strain of caprine arthritis encephalitis virus, a small-ruminant lentivirus, was also shown to increase PrPSc levels in scrapie prion-infected primary sheep microglia [Citation37]. In mice developing prion disease after intracerebral inoculation with ME7 prions, microglia highly responded to intranasal infection with Piry arbovirus, markedly proliferating in their brains compared to those in control mice infected with Piry arbovirus alone [Citation38]. However, no data were available as to whether or not Piry arbovirus infection increased PrPSc levels in the brains [Citation38]. Interestingly, vesicular stomatitis virus glycoprotein and SARS-CoV-2 spike S were shown to enhance intercellular spreading of protein aggregates, including those of Tau and PrPSc, in exosomes into neighboring cells through interaction of the virus ligands with their cognate cellular receptors [Citation23]. It is thus possible that IAV/WSN glycoprotein, or HA, might also be able to stimulate intercellular spreading of the nascently generated PrPSc in IAV/WSN-infected cells through a similar mechanism. However, whether or not these virus infections except for IAV/WSN could cause the de novo conversion of PrPC into PrPSc remains unknown.
Are prions anti-virus proteins?
Prion-like self-templating aggregates have been identified for other cellular proteins in mammals and non-mammals such as yeast, and suggested to be involved in certain cellular functions. The yeast protein Sup35, a yeast translation terminator protein, forms prion-like aggregates, termed [PSI+] prions [Citation39]. It was indicated that [PSI+] prions could confer the yeast resistance to environmental changes through disturbing the translational termination of cellular proteins by impairing the normal function of Sup35 [Citation40,Citation41]. Mod5 also forms prion-like aggregates in yeast, thereby regulating the sterol biosynthetic pathway and eventually protecting the yeast from anti-fungal agents [Citation42]. In mammals, prion-like protein polymerization has been identified for an innate immunity-associated protein, termed apoptosis-associated speck-like protein containing a caspase activation and recruitment domain (ASC) [Citation43]. After virus infection, immune cells provoke prion-like polymerization of ASC to form the inflammatory signalling platform called inflammasome to elicit innate immunity against virus infection [Citation43]. It is thus possible that prion-like polymerization of certain cellular proteins could be a cellular mechanism transducing defence signals against environmental stress including virus infection. Interestingly, the transgenic model mice of familial Alzheimer’s disease, which develop Aβ amyloid plaques in the brains from two months of age, were reported to be more resistant to intracerebral infection with human herpes virus-1 (HHV-1), showing lower mortality than control mice after infection [Citation44]. These results suggest that Aβ peptides might function to be protective against virus infection, and that Aβ peptides might be produced as a cellular protective mechanism against virus infection. We previously showed that PrPC could provide protection against infection with IAVs, including IAV/WSN, by demonstrating that mice devoid of PrPC were highly vulnerable to IAV infections, succumbing to IAV-induced pneumonia with higher mortality than control mice [Citation45]. For understanding of the biological significances of the conversion of PrPC into PrPSc and the subsequent formation of infectious prions, it would be interesting to investigate whether the PrP conversion and the prion formation are associated with the cellular protective mechanism against virus infections.
Conclusion
Emerging lines of evidence suggest that virus infections are a risk factor for many neurodegenerative disorders including Parkinson’s disease and Alzheimer’s disease [Citation18–22]. Parkinson’s disease and Alzheimer’s disease are caused by accumulation of prion-like protein aggregates in the brain of disease-specific proteins, α-synuclein and Aβ, respectively [Citation46–49]. It was shown that infection of neurotropic IAV (H1N1) caused aggregation of α-synuclein in neuron-like Lund human mesencephalic cells and in olfactory bulb neurons of mice [Citation50]. Also, infection with the highly pathogenic, neurotropic H5N1 avian IAV has been shown to induce accumulation of phosphorylated α-synuclein in the substantia nigra pars compacta neurons in mice [Citation20]. HHV-1 and −2, cytomegalovirus, and mumps virus have been also suggested to be associated with the pathogenesis of Parkinson’s disease [Citation18,Citation19]. HHV-1 infection was reported to increase Aβ amyloid peptides in human neuroblastoma and glioblastoma cultured cells as well as in the brains of mice [Citation51]. We have shown that IAV/WSN infection induced the conversion of PrPC into PrPSc and the subsequent formation of infectious prions in neuronal cultures cells [Citation24], further highlighting the causative roles of virus infections in neurodegenerative disorders, including prion diseases.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Prusiner SB. Prions. Proc Natl Acad Sci U S A. 1998;95(23):13363–13383.
- DeArmond SJ, Prusiner SB. Etiology and pathogenesis of prion diseases. Am J Pathol. 1995;146(4):785–811.
- Scheckel C, Aguzzi A. Prions, prionoids and protein misfolding disorders. Nat Rev Genet. 2018;19(7):405–418.
- Pan KM, Baldwin M, Nguyen J, et al. Conversion of alpha-helices into beta-sheets features in the formation of the scrapie prion proteins. Proc Natl Acad Sci USA. 1993;90(23):10962–10966.
- Oesch B, Westaway D, Walchli M, et al. A cellular gene encodes scrapie PrP 27-30 protein. Cell. 1985;40(4):735–746.
- Prusiner SB. Molecular biology of prion diseases. Science. 1991;252(5012):1515–1522.
- Hackl S, Becker CFW. Prion protein-Semisynthetic prion protein (PrP) variants with posttranslational modifications. J Pept Sci. 2019;25(10):e3216.
- Prusiner SB. Biology of prion diseases. J Acquir Immune Defic Syndr. 1993;6(6):663–665.
- Brandel JP, Peckeu L, Haik S. The French surveillance network of Creutzfeldt-Jakob disease. Epidemiological data in France and worldwide. Transfus Clin Biol. 2013;20(4):395–397.
- Heinemann U, Krasnianski A, Meer B, et al. Creutzfeldt-Jakob disease in Germany: a prospective 12-year surveillance. Brain. 2007;130(5):1350–1359.
- Maddox RA, Person MK, Blevins JE, et al. Prion disease incidence in the United States: 2003-2015. Neurology. 2020;94(2):e153–e7.
- Webb TE, Poulter M, Beck J, et al. Phenotypic heterogeneity and genetic modification of P102L inherited prion disease in an international series. Brain. 2008;131(10):2632–2646.
- Cracco L, Appleby BS, Gambetti P. Fatal familial insomnia and sporadic fatal insomnia. Handb Clin Neurol. 2018;153:271–299.
- Will RG, Ironside JW, Zeidler M, et al. A new variant of Creutzfeldt-Jakob disease in the UK. Lancet. 1996;347(9006):921–925.
- Will RG. Acquired prion disease: iatrogenic CJD, variant CJD, kuru. Br Med Bull. 2003;66(1):255–265.
- Jarrett JT, Lansbury PT Jr. Seeding “one-dimensional crystallization” of amyloid: a pathogenic mechanism in Alzheimer’s disease and scrapie? Cell. 1993;73(6):1055–1058.
- Kocisko DA, Come JH, Priola SA, et al. Cell-free formation of protease-resistant prion protein. Nature. 1994;370(6489):471–474.
- Marttila RJ, Rinne UK, Halonen P, et al. Herpesviruses and parkinsonism. Herpes simplex virus types 1 and 2, and cytomegalovirus antibodies in serum and CSF. Arch Neurol. 1981;38(1):19–21.
- Vlajinac H, Dzoljic E, Maksimovic J, et al. Infections as a risk factor for Parkinson’s disease: a case-control study. Int J Neurosci. 2013;123(5):329–332.
- Jang H, Boltz D, Sturm-Ramirez K, et al. Highly pathogenic H5N1 influenza virus can enter the central nervous system and induce neuroinflammation and neurodegeneration. Proc Natl Acad Sci U S A. 2009;106(33):14063–14068.
- Jamieson GA, Maitland NJ, Wilcock GK, et al. Latent herpes simplex virus type 1 in normal and Alzheimer’s disease brains. J Med Virol. 1991;33(4):224–227.
- Readhead B, Haure-Mirande J-V, Funk CC, et al. Multiscale Analysis of Independent Alzheimer’s Cohorts Finds Disruption of Molecular, Genetic, and Clinical Networks by Human Herpesvirus. Neuron. 2018;99(1):64–82 e7.
- Liu S, Hossinger A, Heumuller SE, et al. Highly efficient intercellular spreading of protein misfolding mediated by viral ligand-receptor interactions. Nat Commun. 2021;12(1):5739.
- Hara H, Chida J, Uchiyama K, et al. Neurotropic influenza A virus infection causes prion protein misfolding into infectious prions in neuroblastoma cells. Sci Rep. 2021;11(1):10109.
- Butler DA, Scott MR, Bockman JM, et al. Scrapie-infected murine neuroblastoma cells produce protease-resistant prion proteins. J Virol. 1988;62(5):1558–1564.
- Nishida N, Harris DA, Vilette D, et al. Successful transmission of three mouse-adapted scrapie strains to murine neuroblastoma cell lines overexpressing wild-type mouse prion protein. J Virol. 2000;74(1):320–325.
- Fujita K, Yamaguchi Y, Mori T, et al. Effects of a brain-engraftable microglial cell line expressing anti-prion scFv antibodies on survival times of mice infected with scrapie prions. Cell Mol Neurobiol. 2011;31(7):999–1008.
- Ferhadian D, Contrant M, Printz-Schweigert A, et al. Structural and Functional Motifs in Influenza Virus RNAs. Front Microbiol. 2018;9:559.
- Adler V, Zeiler B, Kryukov V, et al. Small, highly structured RNAs participate in the conversion of human recombinant PrPSen to PrPRes in vitro. J Mol Biol. 2003;332(1):47–57.
- Wang F, Yang F, Hu Y, et al. Lipid Interaction Converts Prion Protein to a PrPSc-like Proteinase K-Resistant Conformation under Physiological Conditions. Biochemistry. 2007;46(23):7045–7053.
- Wang F, Wang X, Yuan CG, et al. Generating a prion with bacterially expressed recombinant prion protein. Science. 2010;327(5969):1132–1135.
- Deleault NR, Lucassen RW, Supattapone S. RNA molecules stimulate prion protein conversion. Nature. 2003;425(6959):717–720.
- Tetz G, Tetz V. Prion-like Domains in Eukaryotic Viruses. Sci Rep. 2018;8(1):8931.
- Haviv Y, Avrahami D, Ovadia H, et al. Induced neuroprotection independently from PrPSc accumulation in a mouse model for prion disease treated with simvastatin. Arch Neurol. 2008;65(6):762–775.
- Leblanc P, Alais S, Porto-Carreiro I, et al. Retrovirus infection strongly enhances scrapie infectivity release in cell culture. Embo J. 2006;25 (12):2674–2685.
- Ehresmann DW, Hogan RN. Acceleration of scrapie disease in mice by an adenovirus. Intervirology. 1986;25(2):103–110.
- Stanton JB, Knowles DP, O’Rourke KI, et al. Small-Ruminant Lentivirus Enhances PrPSc Accumulation in Cultured Sheep Microglial Cells. J Virol. 2008;82(20):9839–9847.
- Lins N, Mourao L, Trevia N, et al. Virus Infections on Prion Diseased Mice Exacerbate Inflammatory Microglial Response. Oxid Med Cell Longev. 2016;2016:3974648.
- Wickner RB, Masison DC, Edskes HK. [PSI] and [URE3] as yeast prions. Yeast. 1995;11(16):1671–1685.
- True HL, Berlin I, Lindquist SL. Epigenetic regulation of translation reveals hidden genetic variation to produce complex traits. Nature. 2004;431(7005):184–187.
- True HL, Lindquist SL. A yeast prion provides a mechanism for genetic variation and phenotypic diversity. Nature. 2000;407(6803):477–483.
- Suzuki G, Shimazu N, Tanaka M. A yeast prion, Mod5, promotes acquired drug resistance and cell survival under environmental stress. Science. 2012;336(6079):355–359.
- Ruland J. Inflammasome: putting the pieces together. Cell. 2014;156(6):1127–1129.
- Eimer WA, Vijaya Kumar DK, Navalpur Shanmugam NK, et al. Alzheimer’s Disease-Associated beta-Amyloid Is Rapidly Seeded by Herpesviridae to Protect against Brain Infection. Neuron. 2018;99(1):56–63 e3.
- Chida J, Hara H, Yano M, et al. Prion protein protects mice from lethal infection with influenza A viruses. PLoS Pathog. 2018;14:e1007049.
- d’Errico P, Meyer-Luehmann M. Mechanisms of Pathogenic Tau and Abeta Protein Spreading in Alzheimer’s Disease. Front Aging Neurosci. 2020;12:265.
- Billings LM, Oddo S, Green KN, et al. Intraneuronal Abeta causes the onset of early Alzheimer’s disease-related cognitive deficits in transgenic mice. Neuron. 2005;45(5):675–688.
- Jellinger KA. Neuropathological aspects of Alzheimer disease, Parkinson disease and frontotemporal dementia. Neurodegener Dis. 2008;5(3–4):118–121.
- Duda JE, Lee VM, Trojanowski JQ. Neuropathology of synuclein aggregates. J Neurosci Res. 2000;61(2):121–127.
- Marreiros R, Muller-Schiffmann A, Trossbach SV, et al. Disruption of cellular proteostasis by H1N1 influenza A virus causes alpha-synuclein aggregation. Proc Natl Acad Sci U S A. 2020;117(12):6741–6751.
- Wozniak MA, Itzhaki RF, Shipley SJ, et al. Herpes simplex virus infection causes cellular beta-amyloid accumulation and secretase upregulation. Neurosci Lett. 2007;429(2–3):95–100.
