Abstract
With delayed child-bearing age, there has been an increase in infertility rates globally and in the United States (US). Unsurprisingly, there has been a concomitant substantial increase in the number of individuals seeking infertility treatments over the last decade. This study aimed to examine the relationship between race/ethnicity and the utilization of different infertility treatments over the previous decade. We conducted this retrospective cohort study using the United States (US) Birth data files 2011–2019. We calculated the rates of infertility treatment and its subtypes over the study period. Descriptive statistics were utilized to examine the sociodemographic and birth characteristics for overall births and those associated with any infertility treatment and each of its subtypes. We calculated the level of association between race/ethnicity and utilization of infertility treatment and the subtypes using adjusted logistic regression models. We found that the rate of infertility treatments for all subtypes considered, had steadily increased by 63.7% within the past decade. In contrast, fertility enhancing drugs or Intrauterine Insemination (IUI) increased by 134%, and in vitro fertilization (IVF), gamete intrafallopian transfer (GIFT), and zygote intrafallopian transfer (ZIFT) treatments increased by 40% over the 9-year study period. Non-Hispanic (NH) Asian women had the highest rate of any infertility treatment with a rate of 25 per 1000 births whereas Hispanic women had the lowest rate of any infertility treatment at 5.8 per 1000 births. When compared with NH-White women, NH-Asian women had a modest 7% lower likelihood (OR = 0.93, 95% CI = 0.92–0.94) of receiving any infertility treatment while NH-Black and Hispanic women had about 70% lower likelihood of receiving any infertility treatment. Our report of increased assisted reproductive technology (ART) utilization rates, and marked racial/ethnic differences in ART utilization highlight the importance of expanding knowledge of inequities that continue to impact marginalized groups, a critical step for informing actionable strategy formulations (i.e., advocacy, policy change, patient education, provider training) to address these inequities.
Introduction
Infertility is defined as the inability to achieve clinical pregnancy after 12 consecutive months of unprotected sexual relations or after 6 months, if the woman is 35 years or older (Centers for Disease Control and Prevention Citation2021). This significant public health issue affects up to 186 million individuals globally, with some estimates suggesting that up to 15% of reproductive-aged couples suffer from some form of infertility (World Health Organization Citation2020). In the United States alone, approximately 20% of the reproductive-aged population report impaired fertility (Chandra et al. Citation2013). Although not life-threatening, infertility can heavily impact an individual's quality of life and cause economic, social, and psychological distress (Ethics Committee of the American Society for Reproductive Medicine Citation2015).
From 1990 to 2017, the global prevalence of infertility increased yearly by approximately 0.37% for females and 0.29% for males of reproductive age (Sun et al. Citation2019). The rising infertility rate and a subsequent reduction in birth rate are most evident in developed countries and are generally attributed to a complex combination of socio-economic factors. Importantly, the climbing infertility level is strongly associated with the increase in age of first-time parents; this is intensified by more women electing to postpone child-bearing, thereby reducing the biologic likelihood of reproducing (Schmidt et al. Citation2012; Berrington Citation2017). In 2020, 15% of the women who gave birth in the United States were over 35 years of age, compared to 11% in 2002 and 8% in 1990 (Assisted Reproductive Technology (ART) Market, Citation2020–2028). Additionally, the 2020 birth rate in the United States dropped by 4% from 2019, reaching an all-time low (Driscoll et al. Citation2021). Other factors contributing to increased levels of infertility include higher prevalence of diabetes (Szaboova and Devendra Citation2015), polycystic ovarian syndrome (PCOS) (Dennett and Simon Citation2015), obesity (Dağ and Dilbaz Citation2015), and stress (Pasch et al. Citation2016).
Unsurprisingly, there has been a substantial rise in the number of individuals seeking infertility treatments over the last decade. In the United States alone, the number of ART cycles performed nearly doubled from approximately 150,000 in 2009 to nearly 300,000 in 2019 (SART: Facts and Figures 1996–Citation2021). These treatments range from medical counseling to assisted reproductive technologies (ARTs) like use of fertility drugs, intrauterine insemination (IUI), and in-vitro fertilization (IVF). Despite the availability of ARTs, a complex interplay of factors, including high cost of care (Chambers et al. Citation2009), cultural/societal stigma (Missmer et al. Citation2011), and time constraints (Nachtigall et al. Citation2009) prevent all in-need individuals from equally accessing ARTs (Peterson Citation2005; Nangia et al. Citation2010). Importantly, previous research has established that different racial and socioeconomic groups experience disparate levels of infertility treatments (Chandra et al. Citation2013).
Despite preliminary results linking race/ethnicity to rates of infertility treatment in the past, there is a scarcity of information on this topic in recent years. This knowledge gap is likely secondary to the shortcomings of the mainstay national ART reporting approaches: National ART Surveillance System Data (NASS) and birth certificates have issues with insufficient racial/ethnic information and under-reporting of ART respectively. To begin to fill this gap while navigating the challenge of fragmentary national data this study aimed to examine the relationship between race/ethnicity and utilization of different types of infertility treatments over the previous decade.
Results
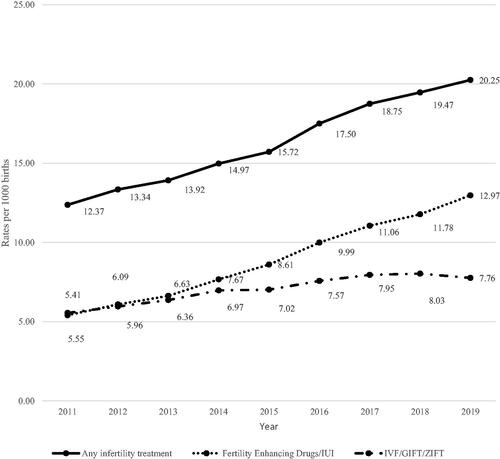
We analyzed 34,228,935 live births during 2011–2019, of which 554,995 (1.6%) were associated with infertility treatments. Of live births resulting from infertility treatments, 303,701 (54.7%) were from IVF/gamete intrafallopian transfer (GIFT)/zygote intrafallopian transfer (ZIFT) and 240,002 (43.2%) were from either fertility enhancing drugs or IUI. We found that the rate of infertility treatments, all subtypes considered, steadily increased from 12.37 per 1,000 live births in 2011 to 20.25 per 1,000 live births in 2019, corresponding to a 63.7% increase over the 9-year study period (). When considering different types of infertility treatment, the usage rates of IVF/GIFT/ZIFT and of fertility enhancing drugs/IUI were similar (about 5.5 per 1000 births) at the beginning of the study in 2011, but over time the rates of fertility enhancing drugs/IUI surpassed those of IVF/GIFT/ZIFT. Specifically, there was a 134% surge in the use of fertility enhancing drugs/IUI as demonstrated by an increase from a usage rate of 5.4 per 1000 live births to 12.97 per 1000 live births from 2011 to 2019 (). By comparison, we observed only a 40% increase in the usage rate of IVF/GIFT/ZIFT treatments rising from a rate of 5.6 per 1000 live births in 2011 to 7.8 per 1000 live births by 2019 ().
Figure 1. Rates of infertility treatment overall and by subtypes in the United States, 2011–2019. Solid line represents the trends in the rates of births from 'any type of infertility treatment' per 1000 births in the US during the study period. The types of infertility treatments were split into two groups: fertility enhancement drugs/IUI and IVF/GIFT/ZIFT. Dotted line represents the trends in the rates of births resulting from fertility enhancement drugs/IUI per 1000 births in the US. Chained line represents the trends in the rates of births from IVF/GIFT/ZIFT. IVF: in vitro fertilization; GIFT: gamete intrafallopian transfer; ZIFT: zygote intrafallopian transfer.
Evaluation of the sociodemographic characteristics of births associated with infertility treatments revealed that of all live births associated with any infertility treatment, 65.9% were in women 30–39 years old. Low birthweight was much more common with infertility treatment, and about 23.2% of neonates conceived with infertility treatment assistance were of low birthweight compared to only 8% of overall live births (). This was especially pronounced for the IVF/GIFT/ZIFT group where 24.9% of live births were of low birthweight. Multiple live births were also a more common occurrence in the infertility treatment group compared to the general population. Around 27.9% of live births associated with any infertility treatment resulted in twins compared to a mere 3.4% of twins in all US live births during this study period. For the IVF/GIFT/ZIFT group, more than one third (34.1%) of all associated live births were multiple births ().
Table 1. Socio-demographic characteristics of live births associated with infertility treatment and its subtypes, 2011–2019.
When assessed by racial/ethnic groups, NH-White was the most represented group for live births associated with any type of infertility treatment (53.2%) and NH-Black was the least represented (3.7%). About 54.8% of all live births associated with fertility enhancing drugs/IUI were in NH-White women, followed by Hispanics (7.4%), NH-Asians (6.2%), and NH-Blacks (3.4%). Of all live births associated with IVF/GIFT/ZIFT, 53.8% were NH-White compared to only 10.3% NH-Asian, 7.6% Hispanic, and 4% NH-Black (). Furthermore, we found that rates of infertility treatment differed significantly across racial/ethnic groups. NH-Asian women had the highest rate of any infertility treatment at 25 per 1000 births (). Hispanic women had the lowest rate of any infertility treatment at 5.8 per 1000 births ( and ). Similar observations were made for various subtypes of infertility treatment. NH-Asian women had the highest rate of IVF/GIFT/ZIFT use (17.2 per 1000 live births) and NH-White women had the highest rate of fertility enhancing drug use/IUI (9.9 per 1000 live births) (). In striking contrast, Hispanic women had the lowest rates of IVF/GIFT/ZIFT (3.3 per 1000 live births) and NH-Black women had the lowest utilization rates of fertility enhancing drugs/IUI (2.4 per 1000 live births) ().
Figure 2. Rates of infertility treatment and subtypes by race/ethnicity. The rates of any infertility treatment, fertility enhancement drugs/IUI and IVF/GIFT/ZIFT per 1000 live births are stratified by maternal racial/ethnic groups – non-Hispanic (NH) White, NH-Black, Hispanic, NH-Asian, and NH-Others. Any infertility treatment is shown in checkered pattern, fertility enhancement drugs/IUI in dotted pattern and IVF/GIFT/ZIFT in solid color. IUI: intrauterine insemination; IVF: in vitro fertilization; GIFT: gamete intrafallopian transfer; ZIFT: zygote intrafallopian transfer.
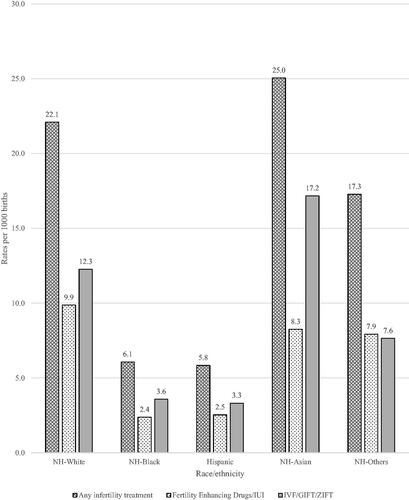
Figure 3. Rates of infertility treatment and subtypes by race/ethnicity across different time periods. Rates of infertility treatments per 1000 live births by maternal race/ethnicity (non-Hispanic [NH] White; NH-Black; Hispanic; NH-Asian; and NH-Others) are represented across three different time periods: 2011–2013; 2014–2016; and 2017–2019. NH-Whites are shown using solid colors, NH-Blacks using dotted pattern, Hispanics using slanted lines, Asians using checkered pattern and NH-Others using dashed lines. IUI: intrauterine insemination; IVF: in vitro fertilization; GIFT: gamete intrafallopian transfer; ZIFT: zygote intrafallopian transfer.
![Figure 3. Rates of infertility treatment and subtypes by race/ethnicity across different time periods. Rates of infertility treatments per 1000 live births by maternal race/ethnicity (non-Hispanic [NH] White; NH-Black; Hispanic; NH-Asian; and NH-Others) are represented across three different time periods: 2011–2013; 2014–2016; and 2017–2019. NH-Whites are shown using solid colors, NH-Blacks using dotted pattern, Hispanics using slanted lines, Asians using checkered pattern and NH-Others using dashed lines. IUI: intrauterine insemination; IVF: in vitro fertilization; GIFT: gamete intrafallopian transfer; ZIFT: zygote intrafallopian transfer.](/cms/asset/b55cdf30-ad2e-4686-801d-1afbdfeaca0a/iaan_a_2038718_f0003_b.jpg)
We also assessed whether there were racial/ethnic disparities in the likelihood for receipt of infertility treatment. We found that compared to NH-White women, NH-Asian women had a modest 7% lower likelihood (95% CI = 0.92–0.94) of receiving any infertility treatment. In comparison, NH-Black and Hispanic women had considerably lower likelihood (). Specifically, NH-Black and Hispanic women were approximately 70% less likely to receive any infertility treatment than NH-White women (NH-Black 95% CI = 0.26–0.29, Hispanic 95% CI = 0.28–0.3) (). On further examination of infertility treatment subtypes, non-White racial/ethnic groups were also significantly less likely to receive fertility enhancing drugs, IUI or IVF/GIFT/ZIFT, with one notable exception: NH-Asian women were 13% more likely (OR = 1.13, 95% CI = 1.12–1.14) to receive IVF/GIFT/ZIFT compared to NH-White women (). All comparisons were adjusted for maternal age, fetal birth weight and sex, and plurality.
Table 2. Association between race/ethnicity and subtypes of infertility treatment.
Discussion
Racial and ethnic disparities in infertility treatment access, outcomes, and underlying infertility risk factors have been reported by several groups (Bleil et al. Citation2014; Craig et al. Citation2019; Jackson-Bey et al. Citation2021). However, to our knowledge, this is the most extensive and up-to-date report of U.S. national utilization rates of various infertility treatment types and live birth outcomes with attention to disparate trends between NH-White women and historically excluded groups: NH-Black, Hispanic, and Asian women. There are invaluable strengths in our study, in which we assessed upwards of 34 million live births over a 9-year study period spanning 2011–2019. We present a comprehensive and current view of trends in ART utilization for the general population with sub-analyses focused on the disparate experiences of racially and ethnically diverse women. Our approach allowed for a robust analysis of national trends of utilization for various subtypes of infertility treatment, focusing on racial/ethnic disparities, which has not been previously described.
Consistent with a previous report of racial/ethnic disparities in infertility utilization from 2006–2010, we found that NH-Black and Hispanic women were approximately 70% less likely to utilize any form of infertility treatment (Chandra et al. Citation2014). Access to infertility care is likely the largest contributing factor to this disparity and is confounded by several sociodemographic factors such as education, income level, insurance coverage, institutionalized racism, and cultural stigmas associated with infertility (Missmer et al. Citation2011; Smith et al. Citation2011; Ceballo et al. Citation2015; Jackson-Bey et al. Citation2021; Kirubarajan et al. Citation2021). In the U.S., insurance companies seldom cover the cost of infertility treatment, forcing most women to cover the prohibitive costs out of pocket. The cost of a single IVF cycle has been estimated at more than 50% of the average person's annual disposable income, thereby effectively excluding this option for lower income couples who tend to be disproportionately ethnic and racial minorities (Chambers et al. Citation2009; Quinn and Fujimoto Citation2016; Citation2020).
Importantly, utilization of IVF services is higher in states with mandated partial or full coverage, but only one state requires coverage of services by Medicaid, thereby disproportionately reducing access by minority populations (Jain et al. Citation2002; Weigel et al. Citation2020). Although nineteen states require employers to cover some portion of infertility treatment, coverage varies widely from state to state. For example, IVF coverage between states range from one to three cycles, which is problematic as the success rate of one cycle is 35–40% (Wade et al. Citation2015) and the average woman under the age of 35 is expected to undergo at least three cycles (Witsenburg et al. Citation2005; Lande et al. Citation2011). Furthermore, self-insuring businesses fall under the federal Employee Retirement Income Security Act (ERISA Citation1974) jurisdiction, exempting them from adhering to state laws regarding ART coverage. Interestingly, even in areas with insurance mandates for infertility treatment coverage, NH-White women were more likely to utilize these services, with NH-Black women waiting for a longer duration of time before seeking treatment (Jain Citation2006). More recent reports show that NH-Black women had greater difficulty accessing infertility services compared to NH-Whites, in which NH-Black women were three times more likely to state their race/ethnicity as a barrier to care, and around 42% of NH-Black women expressed that their physician did not understand their cultural background (Galic, Negris et al. Citation2021; Galic, Swanson, et al. Citation2021).
Our findings suggest increased overall ART utilization from 2011 to 2019, agreeing with an earlier national ART surveillance report (Sunderam et al. Citation2019). In a more recent report of in vitro ART utilization and outcomes between 2004 and 2013, there was an overall increase in ART utilization rates among NH-White, NH-Black, Hispanic and Asian women. However, Asian women had lower fertility rates and the greatest increase in ART utilization (Shapiro et al. Citation2017). Similarly, we found that Asian women were significantly more likely to utilize IVF/GIFT/ZIFT than NH-White, Hispanic and NH-Black women (Shapiro et al. Citation2017). This trend can be partially explained by differences in the mean age of first-delivery and associated infertility issues; in 2013, Asian women delivered their first child at an average age of 29.4, whereas Hispanic and NH-Black women had their first delivery at 24 and 23.9 years of age, respectively (Shapiro et al. Citation2017).
Although disparate, the increase in ART utilization rates for all groups is likely driven by an interplay of several social and biological factors such as delayed childbearing, increased childbearing by individuals from dynamic family structures (i.e., same-sex couples, single parents) and improved access to ART nationally (Heck et al. Citation1997; Martinez et al. Citation2012; Daugherty and Copen Citation2016; Mathews and Hamilton Citation2016; Hamilton et al. Citation2019). Delayed childbearing by women obtaining higher education had been reported as early as 1997 and continues to hold true (Heck et al., Citation1997; Mathews and Hamilton Citation2016). Involvement in demanding occupations also contribute to postponed childbearing (Stentz et al. Citation2016; Simoni et al. Citation2017; Nasab et al. Citation2019). The total number of ART performing fertility clinics in the US increased from 451 in 2011 to 498 in 2017 and paired with a greater volume of procedures per clinic, likely has contributed to increased utilization (Sunderam et al. Citation2014, Citation2020).
We observed that low birth weight was about three times higher in the ART treatment groups, and the proportion of multiple live births was eight times greater than in the general population, which agrees with prior studies (Schieve et al. Citation2002; Berntsen et al. Citation2019; Sunderam et al. Citation2019). Others have shown that NH-Black, Hispanic, and NH-Asian women undergoing IVF have significantly decreased live birth rates and smaller infants compared to their NH-White counterparts (Feinberg et al. Citation2006; Fujimoto et al. Citation2010; Csokmay et al. Citation2011; McQueen et al. Citation2015; Crawford et al. Citation2017). The mechanisms driving lower birth weights in ART pregnancies seem to be independent of the increased occurrence of multiple gestations and are yet to be fully understood, but parental subfertility, the uterine hormonal environment, or ART techniques themselves may be contributing factors (Schieve et al. Citation2002; Kalra et al. Citation2011; Hayashi et al. Citation2012; Imudia et al. Citation2012; Kalra Citation2012; Kasdallah et al. Citation2017). Interestingly, our data show that rates of fertility enhancing drug and IUI utilization per 1000 live births has surpassed that of IVF/GIFT/ZIFT since 2014. The less invasive nature of fertility enhancing drugs and IUI may partly explain this trend. Considering this increased utilization of fertility enhancing drugs and IUI, investigating racial/ethnic disparities and outcomes of these treatments is another important future direction.
A limitation of this study is our inability to account for important sociodemographic factors such as income and insurance coverage, which are known to impact access and outcomes of ART (Chambers et al. Citation2009; Greil et al. Citation2010; Blanchfield and Patterson Citation2015; Quinn and Fujimoto Citation2016; Jackson-Bey et al. Citation2021). Some studies have shown persistent racial/ethnic disparities in ART utilization and outcomes between NH-Black and White women, and Hispanic vs. Non-Hispanic women despite adjusting for demographic characteristics such as socioeconomic status and maternal age (Feinberg et al. Citation2006; Xiong et al. Citation2013). Furthermore, some reports have shown that insurance mandates extending comprehensive insurance coverage of fertility treatment do not mitigate disparities in access (Jain and Hornstein Citation2005; Bitler and Schmidt Citation2006). Rather, IVF services are still mostly accessed by wealthy, highly educated NH-White women (Jain and Hornstein Citation2005; Bitler and Schmidt Citation2006). Thus, the racial/ethnic disparities in ART described by us and others represent a complex issue not solely explained by education, income, or healthcare coverage.
We realize that infertility treatment utilization may be under-reported in birth certificates compared to National ART Surveillance System Data (NASS) (Cohen et al. Citation2014; Thoma et al. Citation2014). Despite the potential under-reporting of ART utilization in our study, the usage of data from birth certificates allowed greater inclusivity of racial/ethnic information as NAAS has up to 35% of race/ethnicity information missing (Thoma et al. Citation2014). Thus, it is difficult to consider the potential implications of under-reporting on our racial/ethnic analyses. Lastly, birth certificate data allowed us to have a comparison group of non-ART live births, which was necessary to compare the odds of infertility treatment utilization among various races/ethnicities.
In conclusion, our results demonstrate that racial/ethnic disparities span various infertility treatment modalities and continue to affect women's reproductive health. These disparities are driven by complex intersectional issues, which can only be better understood through further study. Our report of increased ART utilization rates, and marked racial/ethnic differences in ART utilization serve as evidence for the importance of expanding knowledge of inequities that continue to impact marginalized groups, a critical step for informing actionable ways (i.e., advocacy, policy change, patient education, provider training) to address these inequities.
Materials and methods
This was a retrospective cohort study using the United States (US) Birth data files 2011–2019 made periodically and publicly available by the Centers for Disease Control and Prevention (CDC) through the National Vital Statistics System (NVSS) (NCHS' Vital Statistics Natality Birth Data Citation2020). These datasets contain information such as sociodemographic and health characteristics, maternal risk factors and comorbidities associated with each live birth. For this study, we included live births within 20–42 gestational weeks. Several subtypes of infertility treatments were assessed in this study and included fertility enhancing drugs, IUI, IVF, GIFT and ZIFT. To detect potential treatment-specific effects, we categorized treatments into two distinct groups: one group comprised of in vivo treatments (fertility enhancing drugs and IUI). The other group included treatments with ex vivo or in vitro components such as IVF/GIFT/ZIFT.
Maternal race/ethnicity was categorized into the following groups – non-Hispanic (NH) Whites, NH-Blacks, Hispanics, NH-Asians, and NH-Others (which composed of Native American and Alaskan Native, Native Hawaiian or Other Pacific Islander and other mixed races). All data analyses were conducted using R (version 3·5·1), RStudio (Version 1·1·423) and NCSS (Version 12·0·17).
The covariates included in our study were: maternal age categorized as <20 years, 20–29 years, 30–39 years, and ≥40 years of age; birthweight was classified as follows: low: <2500 g; normal: 2500–3999 g; and macrosomic: ≥4000 g; (Dongarwar et al. Citation2020), fetal sex (female and male); and plurality which was categorized as singleton, twins, and high-order multiples.
We calculated the rates of infertility treatment and its subtypes over the years 2011–2019. Descriptive statistics were utilized to examine sociodemographic and birth characteristics for overall births and those associated with any infertility treatment and its subtypes. Next, we calculated the rates of utilization of infertility treatment and its subtypes among racial/ethnic groups. Lastly, using adjusted logistic regression models, we quantified the magnitude of the association between race/ethnicity and utilization of infertility treatment including its phenotypes. The covariates used to adjust the model were mother's age and fetal birthweight, sex and plurality. All tests of hypotheses were all two-tailed with a type-1 error rate set at 5%.
Ethics approval
The Institutional Review Board at Baylor College of Medicine approved this study as exempt due to the use of de-identified, publicly available data. Informed Consent was not required in this study as the authors did not collect the data.
Authors’ contributions
Conceptualized the study: DD; conducted literature review: DD, VME, SAG, MLL; conducted all the data analyses: DD; drafted the manuscript: DD, VME, SAG, MLL; supervised the project: HMS; reviewed and edited the manuscript: DD, VME, SAG, MLL, HMS.
| Abbreviations | ||
| US | = | United States |
| IUI | = | intrauterine insemination |
| IVF | = | in vitro fertilization |
| GIFT | = | gamete intrafallopian transfer |
| ZIFT | = | zygote intrafallopian transfer |
| NH | = | non-Hispanic |
| ART | = | assisted reproductive technology |
| CDC | = | Centers for Disease Control and Prevention |
| NVSS | = | National Vital Statistics System |
| PCOS | = | polycystic ovarian syndrome |
Disclosure statement
None of the authors have any conflict of interest.
Additional information
Funding
References
- Assisted Reproductive Technology (ART) Market. (2020–2028). [accessed June 29, 2021]. https://www.reportsanddata.com/report-detail/assisted-reproductive-technology-art-market
- Berntsen S, Söderström-Anttila V, Wennerholm UB, Laivuori H, Loft A, Oldereid NB, Romundstad LB, Bergh C, Pinborg A. (2019). The health of children conceived by ART: 'the chicken or the egg? Hum Reprod Update 25:137–158.
- Berrington A. (2017). Childlessness in the UK. In: Kreyenfeld M, Konietzka D, editors. Childlessness in Europe: contexts, causes, and consequences. Cham: Springer International Publishing; p. 57–76.
- Bitler M, Schmidt L. (2006). Health disparities and infertility: impacts of state-level insurance mandates. Fertil Steril 85:858–865.
- Blanchfield BV, Patterson CJ. (2015). Racial and sexual minority women's receipt of medical assistance to become pregnant. Health Psychol 34:571–579.
- Bleil ME, Gregorich SE, Adler NE, Sternfeld B, Rosen MP, Cedars MI. (2014). Race/ethnic disparities in reproductive age: an examination of ovarian reserve estimates across four race/ethnic groups of healthy, regularly cycling women. Fertil Steril 101:199–207.
- Ceballo R, Graham ET, Hart J. (2015). Silent and infertile: an intersectional analysis of the experiences of socioeconomically diverse African American women with infertility. Psychol Women Q 39:497–511.
- Centers for Disease Control and Prevention. (2021). Infertility | Reproductive Health | CDC. [accessed June 29, 2021]. https://www.cdc.gov/reproductivehealth/infertility/index.htm.
- Chambers GM, Sullivan EA, Ishihara O, Chapman MG, Adamson GD. (2009). The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril 91:2281–2294.
- Chandra A, Copen CE, Stephen EH. (2013). Infertility and impaired fecundity in the United States, 1982–2010: data from the National Survey of Family Growth. Natl Health Stat Rep. :1–18.
- Chandra A, Copen CE, Stephen EH. (2014). Infertility service use in the United States: data from the National Survey of Family Growth, 1982–2010. Natl Health Stat Rep. :1–21.
- Cohen B, Bernson D, Sappenfield W, Kirby RS, Kissin D, Zhang Y, Copeland G, Zhang Z, Macaluso M, States Monitoring Assisted Reproductive Technology Collaborative. (2014). Accuracy of assisted reproductive technology information on birth certificates: Florida and Massachusetts, 2004–06. Paediatr Perinat Epidemiol 28:181–190.
- Craig LB, Peck JD, Janitz AE. (2019). The prevalence of infertility in American Indian/Alaska natives and other racial/ethnic groups: National Survey of Family Growth. Paediatr Perinat Epidemiol 33:119–125.
- Crawford S, Joshi N, Boulet SL, Bailey MA, Hood ME, Manning SE, McKane P, Kirby RS, Kissin DM, Jamieson DJ, for the States Monitoring Assisted Reproductive Technology (SMART) Collaborative. (2017). Maternal racial and ethnic disparities in neonatal birth outcomes with and without assisted reproduction. Obstet Gynecol 129:1022–1030.
- Csokmay JM, Hill MJ, Maguire M, Payson MD, Fujimoto VY, Armstrong AY. (2011). Are there ethnic differences in pregnancy rates in African-American versus white women undergoing frozen blastocyst transfers? Fertil Steril 95:89–93.
- Dağ Z, Dilbaz B. (2015). Impact of obesity on infertility in women. J Turk Ger Gynecol Assoc 16:111–117.
- Daugherty J, Copen C. (2016). Trends in attitudes about marriage, childbearing, and sexual behavior: United States, 2002, 2006–2010, and 2011–2013. Natl Health Stat Rep. :1–10.
- Dennett CC, Simon J. (2015). The role of polycystic ovary syndrome in reproductive and metabolic health: overview and approaches for treatment. Diabetes Spectr 28:116–120.
- Dongarwar D, Aggarwal A, Barning K, Salihu HM. (2020). Stillbirths among advanced maternal age women in the United States: 2003–2017. Int J MCH Aids 9:153–156.
- Driscoll A, Osterman M, Hamilton B, Martin J. (2021). Quarterly provisional estimates for selected birth indicators, Quarter 1, 2018–Quarter 4, 2020. National Center for Health Statistics. National Vital Statistics System, Vital Statistics Rapid Release Program [accessed June 29, 2021]. https://www.cdc.gov/nchs/nvss/vsrr/natality-dashboard.htm.
- Ethics Committee of the American Society for Reproductive Medicine. (2015). Disparities in access to effective treatment for infertility in the United States: an ethics committee opinion. Fertil Steril 104:1104–1110.
- ERISA (1974). Federal Employee Retirement Income Security Act of 1974: Hearings before the Subcommittee on Labor Standards of the Committee on Education and Labor, House of Representatives; Ninety-fourth Congress, First Session; on public law 93-406, the Employee Retirement Income Security Act of 1974; April 29, 30, May 1 and 6, 1975.
- Feinberg EC, Larsen FW, Catherino WH, Zhang J, Armstrong AY. (2006). Comparison of assisted reproductive technology utilization and outcomes between Caucasian and African American patients in an equal-access-to-care setting. Fertil Steril 85:888–894.
- Fujimoto VY, Luke B, Brown MB, Jain T, Armstrong A, Grainger DA, Hornstein MD, Society for Assisted Reproductive Technology Writing Group. (2010). Racial and ethnic disparities in assisted reproductive technology outcomes in the United States. Fertil Steril 93:382–390.
- Galic I, Negris O, Warren C, Brown D, Bozen A, Jain T. (2021). Disparities in access to fertility care: who's in and who's out. Fertil Steril Rep 2:109–117.
- Galic I, Swanson A, Warren C, Negris O, Bozen A, Brown D, Lawson A, Jain T. (2021). Infertility in the Midwest: perceptions and attitudes of current treatment. Am J Obstet Gynecol 225:61.e61–61–e11.
- Greil AL, Slauson-Blevins K, McQuillan J. (2010). The experience of infertility: a review of recent literature. Sociol Health Illn 32:140–162.
- Hamilton BE, Martin JA, Osterman MJK, Rossen LM. (2019). Births: provisional data for 2018. Vital Statistics Rapid Release; no 7. Hyattsville, MD: National Center for Health Statistics.
- Hayashi M, Nakai A, Satoh S, Matsuda Y. (2012). Adverse obstetric and perinatal outcomes of singleton pregnancies may be related to maternal factors associated with infertility rather than the type of assisted reproductive technology procedure used. Fertil Steril 98:922–928.
- Heck KE, Schoendorf KC, Ventura SJ, Kiely JL. (1997). Delayed childbearing by education level in the United States, 1969–1994. Matern Child Health J 1:81–88.
- Historical Income Tables: Households. (2020). [accessed July 02, 2021]. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-income-households.html.
- Imudia AN, Awonuga AO, Doyle JO, Kaimal AJ, Wright DL, Toth TL, Styer AK. (2012). Peak serum estradiol level during controlled ovarian hyperstimulation is associated with increased risk of small for gestational age and preeclampsia in singleton pregnancies after in vitro fertilization. Fertil Steril 97:1374–1379.
- Jackson-Bey T, Morris J, Jasper E, Velez Edwards DR, Thornton K, Richard-Davis G, Plowden TC. (2021). Systematic review of racial and ethnic disparities in reproductive endocrinology and infertility: where do we stand today? F&S Rev 2:169–188.
- Jain T, Harlow BL, Hornstein MD. (2002). Insurance coverage and outcomes of in vitro fertilization. N Engl J Med 347:661–666.
- Jain T, Hornstein MD. (2005). Disparities in access to infertility services in a state with mandated insurance coverage. Fertil Steril 84:221–223.
- Jain T. (2006). Socioeconomic and racial disparities among infertility patients seeking care. Fertil Steril 85:876–881.
- Kalra SK, Ratcliffe SJ, Coutifaris C, Molinaro T, Barnhart KT. (2011). Ovarian stimulation and low birth weight in newborns conceived through in vitro fertilization. Obstet Gynecol 118:863–871.
- Kalra SK. (2012). Adverse perinatal outcome and in vitro fertilization singleton pregnancies: what lies beneath? Further evidence to support an underlying role of the modifiable hormonal milieu in in vitro fertilization stimulation. Fertil Steril 97:1295–1296.
- Kasdallah N, Ben Salem H, Kbaier H, Bouguerra C, Blibech S, Douagi M. (2017). Premature birth, low birth weight and birth defects after assisted reproductive therapies. A 18-year comparative study. Tunis Med 95:103–108.
- Kirubarajan A, Patel P, Leung S, Prethipan T, Sierra S. (2021). Barriers to fertility care for racial/ethnic minority groups: a qualitative systematic review. F&S Rev 2:150–159.
- Lande Y, Seidman DS, Maman E, Baum M, Dor J, Hourvitz A. (2011). Couples offered free assisted reproduction treatment have a very high chance of achieving a live birth within 4 years. Fertil Steril 95:568–572.
- Martinez G, Daniels K, Chandra A. (2012). Fertility of men and women aged 15–44 years in the United States: National Survey of Family Growth, 2006–2010. Natl Health Stat Rep. :1–28.
- Mathews TJ, Hamilton BE. (2016). Mean age of mothers is on the rise: United States, 2000–2014. NCHS Data Brief. :1–8.
- McQueen DB, Schufreider A, Lee SM, Feinberg EC, Uhler ML. (2015). Racial disparities in in vitro fertilization outcomes. Fertil Steril 104:398–402. e391.
- Missmer SA, Seifer DB, Jain T. (2011). Cultural factors contributing to health care disparities among patients with infertility in Midwestern United States. Fertil Steril 95:1943–1949.
- Nachtigall RD, Castrillo M, Shah N, Turner D, Harrington J, Jackson R. (2009). The challenge of providing infertility services to a low-income immigrant Latino population. Fertil Steril 92:116–123.
- Nangia AK, Likosky DS, Wang D. (2010). Access to assisted reproductive technology centers in the United States. Fertil Steril 93:745–761.
- Nasab S, Shah JS, Nurudeen K, Jooya ND, Abdallah ME, Sibai BM. (2019). Physicians' attitudes towards using elective oocyte cryopreservation to accommodate the demands of their career. J Assist Reprod Genet 36:1935–1947.
- NCHS' Vital Statistics Natality Birth Data. (2020). [accessed July 12, 2021]. https://data.nber.org/data/vital-statistics-natality-data.html.
- Pasch LA, Holley SR, Bleil ME, Shehab D, Katz PP, Adler NE. (2016). Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil Steril 106:209–215.e2.02.
- Peterson MM. (2005). Assisted reproductive technologies and equity of access issues. J Med Ethics 31:280–285.
- Quinn M, Fujimoto V. (2016). Racial and ethnic disparities in assisted reproductive technology access and outcomes. Fertil Steril 105:1119–1123.
- SART: Facts and Figures. (1996–2021). [accessed July 1, 2021]. https://www.sart.org/patients/history-of-ivf/.
- Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. (2002). Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med 346:731–737.
- Schmidt L, Sobotka T, Bentzen JG, Nyboe Andersen A, ESHRE Reproduction and Society Task Force. (2012). Demographic and medical consequences of the postponement of parenthood. Hum Reprod Update 18:29–43.
- Shapiro AJ, Darmon SK, Barad DH, Albertini DF, Gleicher N, Kushnir VA. (2017). Effect of race and ethnicity on utilization and outcomes of assisted reproductive technology in the USA. Reprod Biol Endocrinol 15:44.
- Simoni MK, Mu L, Collins SC. (2017). Women's career priority is associated with attitudes towards family planning and ethical acceptance of reproductive technologies. Hum Reprod 32:2069–2075.
- Smith JF, Eisenberg ML, Glidden D, Millstein SG, Cedars M, Walsh TJ, Showstack J, Pasch LA, Adler N, Katz PP. (2011). Socioeconomic disparities in the use and success of fertility treatments: analysis of data from a prospective cohort in the United States. Fertil Steril 96:95–101.
- Stentz NC, Griffith KA, Perkins E, Jones RD, Jagsi R. (2016). Fertility and childbearing among American female physicians. J Womens Health (Larchmt)) 25:1059–1065.
- Sun H, Gong TT, Jiang YT, Zhang S, Zhao YH, Wu QJ. (2019). Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990–2017: results from a global burden of disease study, 2017. Aging (Albany NY)). 11:10952–10991.
- Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Barfield WD. (2014). Assisted reproductive technology surveillance – United States. MMWR Surveill Summ 63:1–28.
- Sunderam S, Kissin DM, Zhang Y, Folger SG, Boulet SL, Warner L, Callaghan WM, Barfield WD. (2019). Assisted reproductive technology surveillance – United States, 2016. MMWR Surveill Summ 68:1–23.
- Sunderam S, Kissin DM, Zhang Y, Jewett A, Boulet SL, Warner L, Kroelinger CD, Barfield WD. (2020). Assisted reproductive technology surveillance – United States, 2017. MMWR Surveill Summ 69:1–20.
- Szaboova R, Devendra S. (2015). Infertility in a young woman with Type 2 diabetes. London J Prim Care (Abingdon)) 7:55–57.
- Thoma ME, Boulet S, Martin JA, Kissin D. (2014). Births resulting from assisted reproductive technology: comparing birth certificate and National ART Surveillance System Data, 2011. Natl Vital Stat Rep 63:1–11.
- Wade J, MacLachlan V, Kovacs G. (2015). The success rate of IVF has significantly improved over the last decade. Aust NZ J Obstet Gynaecol 55:473–476.
- Weigel G, Ranji U, Long M, Salganicoff A. (2020). Coverage and use of fertility services in the U.S.; [updated Sep 9, 2020; accessed October 11, 2021]. https://www.kff.org/womens-health-policy/issue-brief/coverage-and-use-of-fertility-services-in-the-u-s/.
- Witsenburg C, Dieben S, Van der Westerlaken L, Verburg H, Naaktgeboren N. (2005). Cumulative live birth rates in cohorts of patients treated with in vitro fertilization or intracytoplasmic sperm injection. Fertil Steril 84:99–107.
- World Health Organization. (2020). Infertility. [accessed June 24, 2021]. https://www.who.int/news-room/fact-sheets/detail/infertility.
- Xiong X, Pridjian G, Dickey RP. (2013). Racial and ethnic disparities in preterm births in infants conceived by in vitro fertilization in the United States. Am J Obstet Gynecol 209:128.e1–21–126.
