Abstract
In the past 15 years, a major research enterprise has emerged that is aimed at understanding associations between geographic and contextual features of the environment (especially the built environment) and elements of human energy balance, including diet, weight and physical activity. Here we highlight aspects of this research area with a particular focus on research and opportunities in the United States as an example. We address four main areas: (1) the importance of valid and comparable data concerning behaviour across geographies; (2) the ongoing need to identify and explore new environmental variables; (3) the challenge of identifying the causally relevant context; and (4) the pressing need for stronger study designs and analytical methods. Additionally, we discuss existing sources of geo-referenced health data which might be exploited by interdisciplinary research teams, personnel challenges and some aspects of funding for geospatial research by the US National Institutes of Health in the past decade, including funding for international collaboration and training opportunities.
1. Introduction
Chronic non-infectious diseases are manifest worldwide and are increasingly replacing infectious diseases as the leading causes of death, albeit with considerable variation among regions of the world (Murray et al. Citation2012). A major focus of public health research is identifying causes of unhealthy behaviours and then developing approaches to change these by addressing the modifiable subset of these causes. Modifiable risk factors involving energy balance, namely diet, weight and physical activity (PA), which influence incidence, morbidity and mortality associated with many chronic diseases, are a critical target for research and intervention. Individual behaviours, genetics and physiology continue to be a primary focus of energy balance research due to a long history of behavioural research demonstrating that interventions resulting in weight loss or increases in PA can be developed and delivered with positive effects on behaviour and health. However, when the intervention ends, participants generally regain the lost weight or return to their sedentary habits (Stevens Citation2001).
An alternative approach to behaviour change and to understanding the causes of unhealthy energy balance focuses on the environment (Hill and Peters Citation1998). In this view, environmental rather than genetic changes are posited as responsible for the population-wide epidemic of obesity, and gene-environment interactions act to influence individual susceptibility to overweight, obesity, lower activity levels or sedentary lifestyles (Ogden et al. Citation2007). Thus, efforts to promote healthy energy balance should focus on both the environment and individual approaches, but increased focus on changing environments may be warranted. Support for this idea comes from the substantial heterogeneity in obesity and PA levels at a range of scales. For example, Latvians are slimmer than Qataris (https://apps.who.int/infobase/), Coloradans are more active than Californians (http://www.cdc.gov/physicalactivity/downloads/pa_state_indicator_report_2014.pdf), and the residents of Portland, Oregon, are more likely to walk or bicycle to work than those of Philadelphia (http://www.census.gov/prod/2014pubs/acs-25.pdf). Many contrasts such as these can be identified, and the presence of such variation, coupled with the frequent failure of individual-level interventions to produce sustained energy balance-related behaviour change (Fjeldsoe et al. Citation2011), indicate that more research attention should be focused on understanding the environmental and contextual causes of obesity, diet, PA and sedentary time. Of course, determining their relative importance compared to genetic and individual factors remains a research challenge; nevertheless, environmental changes that make the healthy choice the easy choice have the potential to have a broad population impact (Hill Citation2003; Sallis, Owen, and Fisher Citation2008).
Geographic and geospatial perspectives and methods are key elements of the effort to understand environmental and contextual causes of health behaviours related to energy balance. This article highlights aspects of recent geospatial health research we deem important to strengthening the integration of geospatial and health perspectives on environment- and energy balance-related health behaviours. We define the environment broadly in the context of a socioecological model of health (Sallis, Owen, and Fisher Citation2008) to include aspects of the built, policy, social, natural and economic environments. Health researchers are already using a variety of geospatial tools and approaches to understanding prevention and disease, but the level of sophistication of such use varies enormously and has not sufficiently penetrated the full spectrum of health topics or research designs (Thornton, Pearce, and Kavanagh Citation2011).
This article was conceived of in the context of a recent workshop (Fostering International Geospatial Health Research Collaborations: Challenges and Opportunities, 16–18 June 2014, held at the Chinese University of Hong Kong) designed to explore and foster international collaboration in geospatial health research. We touch on needs for data harmonization and novel data elements, the challenge of identifying causally relevant environments, the push from public health research for stronger study design related to causal inference, personnel and infrastructure challenges, and a short discussion of recent funding by the US National Institutes for Health in this area. Our examples are largely, but not entirely, from the US. Nevertheless, we hope these ideas and links will be useful to geographers and health scientists using geospatial approaches to design studies with environmental variation in a variety of countries to better understand energy balance and how to improve it.
2. Data challenges and promising data elements: examples from the US and beyond
Comparative studies across diverse geographic regions may contribute to causal inference by increasing the observed range(s) of putative causal factor(s). However, comparative studies depend on the collection of comparable measurements. Height, weight and obesity have standardized objective measures that are applied worldwide, but data standardization is more challenging for diet and PA and the environmental variables that might influence them. The World Health Organization and other groups have used standardized survey questions to collect harmonized data concerning activity and sedentary behaviour. However, comparative studies of PA in the US versus Sweden using objective measurements give different results than do comparisons based on responses to questionnaires (Hagströmer et al. Citation2010). Questionnaires probably measure something very different about PA than do objective measurement devices, and are highly sensitive to cultural context (Troiano et al. Citation2014). Thus, great care must be taken to collect harmonized and valid data in comparative and geospatial analyses of energy balance, and cultural differences combined with cognitive challenges may make questionnaire-based comparisons of the frequency and duration of complex behaviours difficult. The use of self-reported data for surveillance and epidemiological studies of PA (e.g. Troiano et al. Citation2008; Atienza et al. Citation2011) and diet (e.g. Vandevijvere et al. Citation2013) is coming under increasing scrutiny. Continued efforts to clarify the complementary roles of self-report and objective measurement of environments and behaviours are prominent features of the diet and PA research communities. These efforts are probably relevant to diverse aspects of how environment and behaviour interact to influence health and well-being. In particular, further development of objective techniques to classify behaviours in specific contexts is warranted.
Just as geospatial researchers probably need collaboration with health researchers to ensure they are using the best possible data concerning diet, PA and weight, health researchers clearly need collaboration with geospatial and other subject-matter experts to ensure that their comparative and spatial analyses are using the best possible spatial data, theoretical constructs and analytical methods. The types of geo-referenced data currently being applied to the research agenda are diverse. Each data set comes with particular strengths and weaknesses that can be leveraged most effectively through robust collaborations across disciplines. Health researchers do not always appreciate the technical challenges and personnel costs associated with obtaining and developing comparable geographic information system (GIS) data across sites, even within a single country with relatively ubiquitous and inexpensive data, such as the US. The International Physical Activity and Environment Network (IPEN, http://www.ipenproject.org/) is a recent and important example of efforts to integrate sophisticated GIS-based analyses using the best possible harmonized health data across the globe (Adams et al. Citation2014). More such efforts are needed, and attention should be given to standardizing environmental and health data. Generally, environmental data that are flexible with respect to geographic scale, updated frequently and available at no or low cost are desirable in studies on the environment and energy balance, particularly to create standardized measures for comparative studies (see for comparisons of some common US data sources). Nevertheless, it is important to remember that even when data are free, personnel and expertise are required to match, integrate, clean and analyse data, and these costs are easy to underestimate (Lohr Citation2014).
Table 1. Common data sources for information on environmental conditions in the US.
As new or underused data sources are leveraged to increase our understanding of the relationship between environment and energy balance, it is important to properly leverage the work of subject-matter experts in diverse disciplines. For example, a number of recent papers have proposed the use of property appraisal values as a measure of neighbourhood characteristics (Moudon et al. Citation2011; Coffee et al. Citation2013). This is an interesting path because property appraisal values are available in many countries and updated frequently. Furthermore, these may offer a sensitive indicator of some combination of the relative local value of a home, the land it rests on, and an aggregate measure of environmental characteristics and amenities at a highly flexible geographic scale (). A promising approach is the use of hedonic price regression models of appraisal or rental data to develop reliable new measures of neighbourhood conditions (Drewnowski et al. Citation2014). Appraisal data should also be viewed as part of a sophisticated GIS, for which urban economists have developed a robust understanding (Rosen Citation1974; Brookshire et al. Citation1982; Can Citation1992; Smith and Huang Citation1995; Irwin Citation2002; Anderson and West Citation2006). Careful analytical work is required to identify and extract appropriate measures of environments based on appraisal value, home characteristics and other potential confounding environmental and individual-level variables. Collaboration between health, geospatial and economic researchers could accelerate this work. Appraisal data may not be useful in places that lack open markets, or where rates of home sales or renegotiation of rental rates are low.
One particularly valuable feature of property appraisal data is that it could be used to describe environments at various, flexible spatial scales, including, but not limited to, census tracts, counties and other administrative units. This is important because much of the current literature on neighbourhood deprivation and health is based on data from administrative units, making it difficult to explore other definitions of the relevant environment and bringing the Modifiable Areal Unit Problem (see discussion later) to the fore (Chaix, Merlo, and Chauvin Citation2005). Remotely sensed imagery is another underutilized resource for exploring environmental variables potentially related to energy balance that does not require analysis of administrative units. Although traditionally used for physical sciences, satellite remote sensing has been applied to derive quality-of-life index assessments, home value estimation, vulnerability assessment and neighbourhood delineation (Stow, Lippitt and Weeks Citation2010; Patino and Duque Citation2013), as well as sidewalk and vegetation indices. Patino and Duque provide a very detailed overview of this area and emphasize that growing public availability of high-resolution imagery is creating important new possibilities for integrating remote-sensing data into diverse analyses of health and the environment.
3. Defining causally relevant (uncertain) geographic contexts
Health researchers have long taken a keen interest in neighbourhood and contextual effects on health behaviours. Some of this interest can be traced to efforts to understand the health consequences of poverty and neighbourhood deprivation. Much work in this area has involved the analysis of administrative units, such as census tracts in the US. Currently, many investigators are interested in better defining the ‘true causally relevant’ geographic area (Diez Roux and Mair Citation2010). Mei-Po Kwan (Citation2012a, Citation2012b) have called this the ‘Uncertain Geographic Context Problem’, or UGCOP (Kwan Citation2012a, Citation2012b). Like the Modifiable Areal Unit Problem, this issue arises when potential causal relationships are explored using data aggregated into specific areas, such as buffers, administrative units or neighbourhoods; however, these are delineated. The UGCOP arises from a lack of understanding of mechanisms linking environment and behaviour, rather than as a consequence of dividing up regions into various geographic areas and then estimating rates or other aggregate measures from events occurring in these regions.
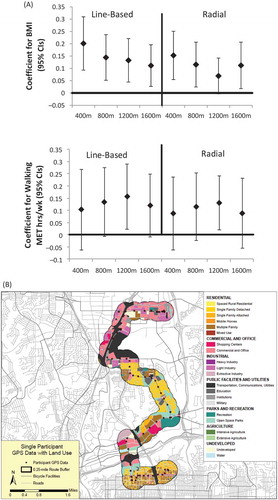
For example, if consumption of fast food is related to exposure to such restaurants, then residence location (a standard focus of studies of the food and PA environments) or any specific aggregated area around the residence may be a poor measure of exposure because exposures can occur at other locations in a study subject’s ‘activity space’ (loosely defined as the area in which usual activities occur). of Thornton, Pearce and Kavanagh (Citation2011) neatly illustrates this point. Sensitivity analyses examining associations between outcomes and properties of buffers of varying shape and size () are one way to document the UGCOP. Alternatively, examination of actual locations of subjects in time and space using activity space studies () might provide insight into differential exposures and their consequences (Jankowska, Schipperijn, and Kerr Citation2014). However, model fit, as in , is not a definitive indicator that a better or best ‘context’ has been identified (Spielman and Yoo Citation2009). Using epidemiological vocabulary, this is because unmeasured covariates or confounders could be responsible for the better fit for a specific buffer size. Stronger experimental or longitudinal study designs are required to address this problem by more clearly identifying causal and policy relevant associations. Additionally, as suggested by Spielman and Yoo (Citation2009), perhaps it is time to forego spatial frames (such as a buffered neighbourhood) and move toward ‘frame-free’ analysis. Of course, no study design can ever eliminate the possibility that some unexamined spatial delineation plays a role in determining behaviour, but identifying plausible causal relationships can guide policy, even with incomplete understanding of the web of causality.
Figure 1. (A) Coefficients of the association between walking/BMI and intersection count for line-based and radial buffers of different diameters (James et al. Citation2014). (B). Portion of the activity space of a person in San Diego and its association with land use mix (Haislip Citation2011).
Further work concerning geographic contexts is needed, especially to better understand how to define and analyse activity space in large health studies. It is not yet clear whether it is possible to identify buffers or collections of buffers that provide adequate measures of meaningful exposures (Zenk et al. Citation2011; Chaix et al. Citation2013). Recently, Boone-Heinonen and Gordon-Larsen (Citation2012) described lessons learned from diverse analyses of environmental influences on obesity in the Add Health Study, a large prospective cohort of adolescents in the US (Resnick Citation1997; Boone-Heinonen and Gordon-Larsen Citation2012). They emphasized both the value of integrating GIS into longitudinal cohort studies and the fact that better delineation of the area that influences diet, PA and obesity is only one of many problems for analyses of energy balance and environment in longitudinal studies. Studies of natural experiments such as changes to the built, transportation or food environment can address some of these problems and indeed are the subject of recent funding opportunities from the US National Institutes of Health (NIH) (e.g. Program Announcement PA-13-110 Obesity Policy Evaluation Research).
Methodologies developed in space–time analytics to identify causal relationships between environment, diet, weight and PA may also complement epidemiological analyses of cohort data. Health research with a spatial emphasis could benefit from more discussion and focus on the causal mechanisms linking health behaviours and outcomes with the environment and how these mechanisms may be represented or modelled. Careful thinking about the relative contributions of ‘ambient’ exposures, such as policies or neighbourhood socioeconomic deprivation, and ‘concrete’ exposures, such as spatially located elements of the built environment to health behaviours and outcomes, could strengthen space- and place-based analyses of health (Spielman and Yoo Citation2009). Clearly, such ‘ambient’ and ‘concrete’ exposures interact and are collinear, hence the need for thoughtful analyses.
4. Stronger experimental designs
Recent commentaries concerning spatial approaches to health issues have emphasized the need for better effect identification, more experiments and greater effort to obtain both retrospective and prospective place data (e.g. Matthews, Moudon and Daniel Citation2009; Oakes Citation2013). Some progress has been made on these topics. For example, respondent home addresses from many of the major US health surveys such as Add Health, the California Health Interview Survey (CHIS), the National Health and Nutrition Examination Survey (NHANES) and cohort studies, such as the Nurses’ Health Study (NHS), the Multi-Ethnic Study of Atherosclerosis (MESA), the NCI-American Association of Retired Persons (AARP) cohort, the Women’s Health Initiative and the Los Angeles Family and Neighborhood Survey, have been geocoded and many geospatial analyses are complete or in progress (e.g. CHIS, Huang et al. Citation2009; NHANES, Wen and Kowaleski-Jones Citation2012; NHS, James et al. Citation2013; MESA, Hirsch et al. Citation2014; NCI-AARP, Major et al. Citation2010; WHI, Kerr et al. Citation2014). This exciting and important advance reflects the fact that the idea of spatial and contextual approaches has captured the imagination of chronic disease and health behaviour researchers. Cohort studies outside the US are also incorporating spatial data layers, especially in Europe and Australia (e.g. Giles-Corti et al. Citation2008; Schipperijn et al. Citation2014). It could be useful to convene researchers incorporating spatial data in cohort studies to discuss the potential for data pooling to increase power via larger sample sizes and greater environmental variability in the underlying data.
Continued efforts to engage geographers and exploit space–time methods in this work could accelerate progress in clarifying causal relationships between environment and health behaviours, as well as strengthen interventions. More detailed measurement of where people spend their time (e.g. via use of global positioning system (GPS)) may not achieve the goal of conclusively demonstrating causal associations between environmental variables and health behaviours (Boone-Heinonen and Gordon-Larsen Citation2012), but greater engagement with geographers could help improve the conceptualization of spatial constructs relevant to health (Thornton, Pearce, and Kavanagh Citation2011; Chaix et al. Citation2013).
In addition to diverse cross-sectional analyses, more and more longitudinal analyses (Ewing, Brownson, and Berrigan Citation2006; Powell-Wiley et al. Citation2014), analyses examining respondents who move (Hirsch et al. Citation2014; Knuiman et al. Citation2014) and studies of natural experiments (Fitzhugh, Bassett and Evans Citation2010) are appearing in the health sector. Such studies can strengthen the case that environmental modifications can lead to changes in health behaviours. Policy change requires more than just evidence that an intervention can result in improved health; among other features, the proposed intervention may receive greater support if it is cost-effective. To date, few cost–benefit analyses have been conducted that link changes to the built or policy environment and health (National Institute for Health and Clinical Excellence Citation2008; McKinnon et al. Citation2009). More such studies could accelerate progress in addressing the global problem of unhealthy energy balance.
Much more work is also needed to illustrate how geospatial approaches can inform and improve behavioural interventions. For example, building on prior work (Zenk et al. Citation2009), Tarlov and Zenk have recently received funding from the NIH to examine the extent to which built environment attributes influence response to a weight management programme. Specifically, they will examine 200,000 US military veterans who participated in a weight management programme and a similar number of matched controls, with the aim of determining the extent to which specific attributes of the residential environment are associated with weight loss at 6 months and weight loss maintenance at 18 and 60 months. While this study will be able to measure environmental change over time due to actual changes in the environment (e.g. a new supermarket opens near a study participant’s home) as well as moves (e.g. a study participant moves from an environment with a supermarket to one without a supermarket), estimates of the moderating effects of the environment on responses to the intervention might not be fully generalizable in a study of this type, depending on the design, because study participants choose their own neighbourhoods.
Nevertheless, if studies of how neighbourhoods moderate effects of behavioural interventions are successful in identifying neighbourhood features that help or hinder response to weight loss or other interventions, these could lead to improvements in such interventions. For example, investigators could add different elements to help overcome negative environmental effects and target individuals living in communities where the impact of the current intervention was greatest. Recent work suggests that interactions between the environment and response to energy balance may play out in other ways. For example, Kerr et al. (Citation2010) report that individual interventions helped overcome environmental barriers to PA (Kerr et al. Citation2010). Development of a clear taxonomy of how environment and individual interventions might interact for different target behaviours could help guide research in this area. Individual interventions could also include environmental change and employ GPS devices to determine whether activity locations changed due to improved access or facilities (Kerr et al. Citation2014). Other initiatives at the NIH, such as the Mobile Data to Knowledge grants, will include location-based prompts where interventions can occur when a participant enters a health-risk area, such as a restaurant serving largely unhealthy food or a tobacco outlet.
5. Personnel and infrastructure challenges
Research using spatial data to understand health behaviours related to energy balance is growing rapidly; however, the quality of this research is highly variable. Some of this heterogeneity is due to lack of personnel with appropriate training in geospatial thinking across the health research sector. These needs have also been discussed in some detail by geographers and demographers interested in health (Matthews Citation2012; Matthews and Yang Citation2013; Shoval et al. Citation2014). Expertise in geography and geospatial thinking is growing in the health arena, but schools of public health, state and county health departments, cancer research centres and many NIH institutes often lack a deep pool of researchers and analysts with geospatial expertise. Thus, more opportunities for collaboration, education and training are needed to build on existing efforts such as the Communities Putting Prevention to Work (CPPW, http://www.cdc.gov/nccdphp/dch/programs/CommunitiesPuttingPreventiontoWork/) programme and the Active Living Research (ALR) programme (Barker and Gutman Citation2014). The CPPW mission is to ‘… help large cities, small towns, rural communities, and tribal areas make environmental changes that make healthy living easier’. Similarly, ALR has placed a major emphasis on ‘communities, active transportation, schools and parks and recreation’ (http://activelivingresearch.org/about).
Achieving the goals of ALR, CPPW and other calls to improve health via contextual and environmental approaches requires incorporation of new data into the analyses of health behaviours and health-related interventions. Currently in health research, a great deal of duplication of effort appears to occur in the creation of data layers, confidentiality issues and analysis of administrative units. Calls to address these problems by creating ‘… distributed, interoperable spatial data infrastructures …’ have been made, but substantial work remains to define this goal and mobilize key health research stakeholders to invest in such infrastructure (Richardson et al. Citation2013). Useful intermediate goals, such as improving methods for handling confidential health and spatial data and developing protocols for including or linking spatial data and Electronic Health Record (EHR) data, may help move the field toward a comprehensive and efficient system for collecting, sorting and sharing spatial data (Comer et al. Citation2011; Simpson and Novak Citation2013).
There is considerable interest throughout the health sector in the potential for better environmental and spatial data to contribute to better health. A recent abstract illustrates this interest and the need for more trained personnel to fulfil the promise of geospatial data in health. In the abstract, Pruitt (Citation2014) states that ‘Duke Medicine has incorporated geospatial information within its EHRs, which add thousands of new “big-geo-data” elements to a patients clinical record’. It is important to acknowledge the considerable effort that will be required to define, harmonize and carry out useful research with such a large number of data elements. These data elements are probably obtained from census and other administrative sources and, as discussed earlier, they may not be the most useful, meaningful or causally relevant contextual variables. Additionally, adequate infrastructure to help address confidentiality, for example, via data enclaves or data centres, is not yet widely available.
Nevertheless, there are some fields where the public health research community has significant expertise in geospatial tools and concepts. Examples include research communities related to cancer mapping, infectious disease and pollution modelling, as well as research related to built environment, transportation and PA. These communities are scattered haphazardly across institutes and institutions and are not yet sufficiently expansive to support the integration of geospatial perspectives in all areas where they could contribute. Similarly, research areas such as regional science have not historically focused on health but have the potential to make significant conceptual contributions to understanding how national or global processes influence health (http://www.regionalscience.org/). Thus, further challenges include how to coordinate existing expertise, establish best practices and increase communication across disciplines. The Robert Wood Johnson Foundation’s ALR programme provides an example of the level of effort required to create a community of researchers focused on environmental influences on PA that has resulted in growing public health sector expertise in geospatial analyses (Barker and Gutman Citation2014).
6. US National Institutes of Health funding, including international projects and training
Over the past decade, the NIH has funded considerable research on geospatial approaches to energy balance. Examples of these grants are listed in . Some of these grants were submitted in response to calls for proposals related to spatial uncertainty, obesity policy research and geographic and contextual influences on energy balance-related health behaviours; others were investigator-initiated submissions. Additional grants have been funded through unsolicited submission, conference grant mechanisms and special initiatives such as the NCI Provocative Questions initiative (http://provocativequestions.nci.nih.gov/). A general introduction to NIH grants is available (http://grants.nih.gov/grants).
Table 2. Examples of recent grants concerning geospatial and contextual analyses of energy balance from the United States National Institutes of Health. Abstracts of these and other grants can be searched for and accessed via the NIH Reporter (http://projectreporter.nih.gov/reporter.cfm).
A number of features of the NIH funding system are worth noting in the context of fostering further research on spatial and contextual aspects of health, especially in an international context. First, because geospatial activities cut across multiple institutes at the NIH, it can be difficult to track funding activities and opportunities in this area. Personal contact with an NIH Program Officer is very helpful for prospective grantees. Specific grants, grant abstracts, funding institutes and other details, including the name of the Program Officer, can be accessed through NIH RePORTER (http://projectreporter.nih.gov/reporter.cfm). This system facilitates identifying Program Officers who have handled grants on similar topics.
Second, a potentially salient model for US funding of international research concerning spatial and environmental influences on energy balance is IPEN, which has received funding from NIH’s National Cancer Institute and National Heart, Lung, and Blood Institute. The IPEN team has effectively argued that causal inference concerning associations between built environment and PA could be strengthened by a research programme emphasizing the use of common measures across more diverse built and cultural environments than are available in any one country (Kerr et al. Citation2013; van Dyck et al. Citation2014). Third, NIH funding spans a continuum (), ranging from studies of exposures related to regional or national policies (e.g. Nanney, Datar) to diverse studies addressing potential effects of exposures associated with specific geographic units or locations (e.g. Wen), as well as specific spatially located features of the environment (e.g. Saelens). This continuum is related to the idea of place versus space in geographic thinking, to the distinction between ‘ambient’ and ‘concrete’ exposures in analyses of context and energy balance, and to study designs focusing on people in multiple spaces versus those tracking individuals across spaces. Health research could benefit from further discussion addressing exposure in the context of these ideas (Chaix et al. Citation2013).
Opportunities exist for international researchers through collaboration with US-based investigators, investigator-initiated grants from overseas and diverse training programmes. Many of these activities are organized by NIH’s Fogarty International Center (http://www.fic.nih.gov/). The recently established National Cancer Institute’s Center for Global Health (http://www.cancer.gov/aboutnci/organization/global-health) also offers a variety of research and training opportunities emphasizing cancer control and training for investigators from low- to middle-income countries. This short introduction to US NIH funding highlights the need for a more overarching international exchange concerning research questions, funding opportunities and paths to international collaboration in this research area.
7. Conclusion
At its heart, public health research is an applied science, with social justice through health and healthy environments as one of its key goals (McKinnon et al. Citation2012; Lee et al. Citation2012). Currently, Fogarty International Center describes its vision as ‘a world in which the frontiers of health research extend across the globe and advances in science are implemented to reduce the burden of disease, promote health, and extend longevity for all people’ (http://www.fic.nih.gov/). Strengthening international geospatial health research is a logical element of such a vision, and given the negative trends in diet, weight and PA across the globe, a focus on energy balance appears timely. Comparative studies can strengthen causal inference (Kerr et al. Citation2013) and transdisciplinary teams can improve scientific productivity (Hall et al. Citation2012). Of course, it is hoped that fostering international collaboration will accelerate scientific discovery, but it remains to be seen whether this will occur. This article has emphasized the need for conceptual clarity, valid and harmonized data and better study designs in order to better understand causal pathways and to improve evaluation of interventions. These factors are always desirable in health research, but geospatial research on energy balance is ripe for progress on all of these fronts. Continued international collaboration between health and geospatial researchers should help accelerate this progress.
Disclosure statement
No potential conflict of interest was reported by the authors.
Acknowledgements
We thank the organizers of the Forum where this work was originally presented, Anne Rodgers for editorial assistance and Penny Randall-Levy for formatting the bibliography.
Additional information
Funding
References
- Adams, M. A., L. D. Frank, J. Schipperijn, G. Smith, J. Chapman, L. B. Christiansen, N. Coffee, et al. 2014. “International Variation in Neighborhood Walkability, Transit, and Recreation Environments Using Geographic Information Systems: The IPEN Adult Study.” International Journal of Health Geographics 13 (1): 43. doi:10.1186/1476-072X-13-43.
- Anderson, S. T., and S. E. West. 2006. “Open Space, Residential Property Values, and Spatial Context.” Regional Science and Urban Economics 36 (6): 773–789. doi:10.1016/j.regsciurbeco.2006.03.007.
- Atienza, A. A., R. P. Moser, F. Perna, K. Dodd, R. Ballard-Barbash, R. P. Troiano, and D. Berrigan. 2011. “Self-Reported and Objectively Measured Activity Related to Biomarkers Using NHANES.” Medicine and Science in Sports and Exercise 43 (5): 815–821. doi:10.1249/MSS.0b013e3181fdfc32.
- Barker, D. C., and M. A. Gutman. 2014. “Evaluation of Active Living Research: Ten Years of Progress in Building a New Field.” American Journal of Preventive Medicine 46 (2): 208–215. doi:10.1016/j.amepre.2013.10.003.
- Boone-Heinonen, J., and P. Gordon-Larsen. 2012. “Obesogenic Environments in Youth: Concepts and Methods from a Longitudinal National Sample.” American Journal of Preventive Medicine 42 (5): e37–e46. doi:10.1016/j.amepre.2012.02.005.
- Brookshire, D. S., M. A. Thayer, W. D. Schulze, and R. C. Darge. 1982. Valuing Public Goods: A Comparison of Survey and Hedonic Approaches. American Economic Review 72 (1): 165–177.
- Can, A. 1992. “Specification and Estimation of Hedonic Housing Price Models.” Regional Science and Urban Economics 22 (3): 453–474. doi:10.1016/0166-0462(92)90039-4.
- Chaix, B., J. Méline, S. Duncan, C. Merrien, N. Karusisi, C. Perchoux, A. Lewin, K. Labadi, and Y. Kestens. 2013. “GPS Tracking in Neighborhood and Health Studies: A Step Forward for Environmental Exposure Assessment, A Step Backward for Causal Inference?” Health & Place 21: 46–51. doi:10.1016/j.healthplace.2013.01.003.
- Chaix, B., J. Merlo, and P. Chauvin. 2005. “Comparison of a Spatial Approach with the Multilevel Approach for Investigating Place Effects on Health: The Example of Healthcare Utilisation in France.” Journal of Epidemiology and Community Health 59 (6): 517–526. doi:10.1136/jech.2004.025478.
- Coffee, N. T., T. Lockwood, G. Hugo, C. Paquet, N. J. Howard, and M. Daniel. 2013. “Relative Residential Property Value as a Socio-Economic Status Indicator for Health Research.” International Journal of Health Geographics 12: 22. doi:10.1186/1476-072X-12-22.
- Comer, K. F., S. Grannis, B. E. Dixon, D. J. Bodenhamer, and S. E. Wiehe. 2011. Incorporating Geospatial Capacity within Clinical Data Systems to Address Social Determinants of Health. Public Health Reports 126 (Suppl. 3): 54–61.
- Diez Roux, A. V., and C. Mair. 2010. “Neighborhoods and Health.” Annals of the New York Academy of Sciences 1186: 125–145. doi:10.1111/j.1749-6632.2009.05333.x.
- Drewnowski, A., A. Aggarwal, C. D. Rehm, H. Cohen-Cline, P. M. Hurvitz, and A. V. Moudon. 2014. “Environments Perceived as Obesogenic Have Lower Residential Property Values.” American Journal of Preventive Medicine 47 (3): 260–274. doi:10.1016/j.amepre.2014.05.006.
- Ewing, R., R. C. Brownson, and D. Berrigan. 2006. “Relationship between Urban Sprawl and Weight of United States Youth.” American Journal of Preventive Medicine 31 (6): 464–474. doi:10.1016/j.amepre.2006.08.020.
- Fitzhugh, E. C., D. R. Bassett Jr., and M. F. Evans. 2010. “Urban Trails and Physical Activity: A Natural Experiment.” American Journal of Preventive Medicine 39 (3): 259–262. doi:10.1016/j.amepre.2010.05.010.
- Fjeldsoe, B., M. Neuhaus, E. Winkler, and E. Eakin. 2011. “Systematic Review of Maintenance of Behavior Change following Physical Activity and Dietary Interventions.” Health Psychology 30 (1): 99–109. doi:10.1037/a0021974.
- Giles-Corti, B., M. Knuiman, A. Timperio, K. Van Niel, T. J. Pikora, F. C. L. Bull, T. Shilton, and M. Bulsara. 2008. “Evaluation of the Implementation of a State Government Community Design Policy Aimed at Increasing Local Walking: Design Issues and Baseline Results from RESIDE, Perth Western Australia.” Preventive Medicine 46 (1): 46–54. doi:10.1016/j.ypmed.2007.08.002.
- Hagströmer, M., R. P. Troiano, M. Sjostrom, and D. Berrigan. 2010. “Levels and Patterns of Objectively Assessed Physical Activity–A Comparison between Sweden and the United States.” American Journal of Epidemiology 171 (10): 1055–1064. doi:10.1093/aje/kwq069.
- Haislip, L. D., 2011. “An Examination of Utilitarian Bicycle Trip Route Choice Preference in San Diego.” Thesis, San Diego State University School of Public Affairs. Accessed September 2, 2014. http://libpac.sdsu.edu/search/X?laura+haislip
- Hall, K. L., D. Stokols, B. A. Stipelman, A. L. Vogel, A. Feng, B. Masimore, G. Morgan, R. P. Moser, S. E. Marcus, and D. Berrigan. 2012. “Assessing the Value of Team Science: A Study Comparing Center- and Investigator-Initiated Grants.” American Journal of Preventive Medicine 42 (2): 157–163. doi:10.1016/j.amepre.2011.10.011.
- Hill, J. O. 2003. “Obesity and the Environment: Where Do We Go from Here?” Science 299 (5608): 853–855. doi:10.1126/science.1079857.
- Hill, J. O., and J. C. Peters. 1998. “Environmental Contributions to the Obesity Epidemic.” Science 280 (5368): 1371–1374. doi:10.1126/science.280.5368.1371.
- Hirsch, J. A., A. V. Diez Roux, K. A. Moore, K. R. Evenson, and D. A. Rodriguez. 2014. “Change in Walking and Body Mass Index following Residential Relocation: The Multi-Ethnic Study of Atherosclerosis.” American Journal of Public Health 104 (3): e49–e56. doi:10.2105/AJPH.2013.301773.
- Huang, L., D. G. Stinchcomb, L. W. Pickle, J. Dill, and D. Berrigan. 2009. “Identifying Clusters of Active Transportation Using Spatial Scan Statistics.” American Journal of Preventive Medicine 37 (2): 157–166. doi:10.1016/j.amepre.2009.04.021.
- Irwin, E. G. 2002. “The Effects of Open Space on Residential Property Values.” Land Economics 78 (4): 465–480. doi:10.2307/3146847.
- James, P., D. Berrigan, J. E. Hart, J. Aaron Hipp, C. M. Hoehner, J. Kerr, J. M. Major, M. Oka, and F. Laden. 2014. “Effects of Buffer Size and Shape on Associations between the Built Environment and Energy Balance.” Health & Place 27: 162–170. doi:10.1016/j.healthplace.2014.02.003.
- James, P., P. J. Troped, J. E. Hart, C. E. Joshu, G. A. Colditz, R. C. Brownson, R. Ewing, and F. Laden. 2013. “Urban Sprawl, Physical Activity, and Body Mass Index: Nurses’ Health Study and Nurses’ Health Study II.” American Journal of Public Health 103 (2): 369–375. doi:10.2105/AJPH.2011.300449.
- Jankowska, M. M., J. Schipperijn, and J. Kerr 2014. A Framework for Using GPS Data in Physical Activity and Sedentary Behavior Studies. Exercise and Sport Sciences Review 43 (1): 48–56. doi:10.1249/JES.0000000000000035.
- Kerr, J., G. Norman, R. Millstein, M. A. Adams, C. Morgan, R. D. Langer, and M. Allison. 2014. “Neighborhood Environment and Physical Activity among Older Women: Findings from the San Diego Cohort of the Women’s Health Initiative.” Journal of Physical Activity & Health 11 (6): 1070–1077. doi:10.1123/jpah.2012-0159.
- Kerr, J., G. J. Norman, M. A. Adams, S. Ryan, L. Frank, J. F. Sallis, K. J. Calfas, and K. Patrick. 2010. “Do Neighborhood Environments Moderate the Effect of Physical Activity Lifestyle Interventions in Adults?” Health & Place 16 (5): 903–908. doi:10.1016/j.healthplace.2010.05.002.
- Kerr, J., J. F. Sallis, N. Owen, I. D. Bourdeaudhuij, E. Cerin, T. Sugiyama, R. Reis, et al. 2013. Advancing Science and Policy through a Coordinated International Study of Physical Activity and Built Environments: IPEN Adult Methods. Journal of Physical Activity & Health 10 (4): 581–601.
- Knuiman, M. W., H. E. Christian, M. L. Divitini, S. A. Foster, F. C. Bull, H. M. Badland, and B. Giles-Corti. 2014. “A Longitudinal Analysis of the Influence of the Neighborhood Built Environment on Walking for Transportation: The RESIDE Study.” American Journal of Epidemiology 180 (5): 453–461. doi:10.1093/aje/kwu171.
- Kwan, M.-P.. 2012a. “How GIS Can Help Address the Uncertain Geographic Context Problem in Social Science Research.” Annals of GIS 18 (4): 245–255. doi:10.1080/19475683.2012.727867.
- Kwan, M.-P.. 2012b. “The Uncertain Geographic Context Problem.” Annals of the Association of American Geographers 102 (5): 958–968. doi:10.1080/00045608.2012.687349.
- Lee, I.-M., E. J. Shiroma, F. Lobelo, P. Puska, S. N. Blair, and P. T. Katzmarzyk. 2012. “Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy.” The Lancet 380 (9838): 219–229. doi:10.1016/S0140-6736(12)61031-9.
- Lohr, S., 2014. “For Big-Data Scientists, ‘Janitor Work’ Is Key Hurdle to Insights.” The New York Times. Accessed December 15, 2014. http://www.nytimes.com/2014/08/18/technology/for-big-data-scientists-hurdle-to-insights-is-janitor-work.html?_r=0
- Major, J. M., C. A. Doubeni, N. D. Freedman, Y. Park, M. Lian, A. R. Hollenbeck, A. Schatzkin, B. I. Graubard, R. Sinha, and J. S. Ross. 2010. “Neighborhood Socioeconomic Deprivation and Mortality: NIH-AARP Diet and Health Study.” PLoS One 5 (11): e15538. doi:10.1371/journal.pone.0015538.
- Matthews, S. A. 2012. “Thinking about Place, Spatial Behavior, and Spatial Processes in Childhood Obesity.” American Journal of Preventive Medicine 42 (5): 516–520. doi:10.1016/j.amepre.2012.02.004.
- Matthews, S. A., A. V. Moudon, and M. Daniel. 2009. “Work Group II: Using Geographic Information Systems for Enhancing Research Relevant to Policy on Diet, Physical Activity, and Weight.” American Journal of Preventive Medicine 36 (4): S171–S176. doi:10.1016/j.amepre.2009.01.011.
- Matthews, S. A., and T.-C. Yang. 2013. “Spatial Polygamy and Contextual Exposures (Spaces): Promoting Activity Space Approaches in Research on Place and Health.” American Behavioral Scientist 57 (8): 1057–1081. doi:10.1177/0002764213487345.
- McKinnon, R. A., C. T. Orleans, S. K. Kumanyika, D. Haire-Joshu, S. M. Krebs-Smith, E. A. Finkelstein, K. D. Brownell, J. W. Thompson, and R. Ballard-Barbash. 2009. “Considerations for an Obesity Policy Research Agenda.” American Journal of Preventive Medicine 36 (4): 351–357. doi:10.1016/j.amepre.2008.11.017.
- McKinnon, R. A., J. Reedy, D. Berrigan, and S. M. Krebs-Smith. 2012. “The National Collaborative on Childhood Obesity Research Catalogue of Surveillance Systems and Measures Registry: New Tools to Spur Innovation and Increase Productivity in Childhood Obesity Research.” American Journal of Preventive Medicine 42 (4): 433–435. doi:10.1016/j.amepre.2012.01.004.
- Moudon, A. V., A. J. Cook, J. Ulmer, P. M. Hurvitz, and A. Drewnowski. 2011. “A Neighborhood Wealth Metric for Use in Health Studies.” American Journal of Preventive Medicine 41 (1): 88–97. doi:10.1016/j.amepre.2011.03.009.
- Murray, C. J., T. Vos, R. Lozano, M. Naghavi, A. D. Flaxman, C. Michaud, M. Ezzati, et al. 2012. “Disability-Adjusted Life Years (Dalys) for 291 Diseases and Injuries in 21 Regions, 1990-2010: A Systematic Analysis for the Global Burden of Disease Study 2010.” Lancet 380 (9859): 2197–2223.
- National Institute for Health and Clinical Excellence. 2008. Physical Activity and the Environment. Costing report: implementing NICE guidance. National Institute for Health and Clinical Excellence. Accessed September 4, 2014.www.nice.org.uk/guidance/ph8/resources/physical-activity-and-the-environment-cost-report2
- Oakes, J. M. 2013. “Invited Commentary: Paths and Pathologies of Social Epidemiology.” American Journal of Epidemiology 178 (6): 850–851. doi:10.1093/aje/kwt144.
- Ogden, C. L., S. Z. Yanovski, M. D. Carroll, and K. M. Flegal. 2007. “The Epidemiology of Obesity.” Gastroenterology 132 (6): 2087–2102. doi:10.1053/j.gastro.2007.03.052.
- Patino, J. E., and J. C. Duque. 2013. “A Review of Regional Science Applications of Satellite Remote Sensing in Urban Settings.” Computers, Environment and Urban Systems 37: 1–17. doi:10.1016/j.compenvurbsys.2012.06.003.
- Powell-Wiley, T. M., C. Ayers, P. Agyemang, T. Leonard, D. Berrigan, R. Ballard-Barbash, M. Lian, S. R. Das, and C. M. Hoehner. 2014. “Neighborhood-Level Socioeconomic Deprivation Predicts Weight Gain in a Multi-Ethnic Population: Longitudinal Data from the Dallas Heart Study.” Preventive Medicine 66: 22–27. doi:10.1016/j.ypmed.2014.05.011.
- Pruitt, S., 2014. “Big-GEO-Data EHR Infrastructure Development for On-Demand Analytics.” In Healthcare Analytics Symposium July 14-16, 2014. Chicago, IL: HealthData Management. Accessed September 2, 2014. http://www.healthdatamanagement.com/conferences/1_5/big-geo-data-ehr-infrastructure-development-for-on-demand-analytics-47627-1.html
- Resnick, M. D. 1997. “Protecting Adolescents from Harm. Findings from the National Longitudinal Study on Adolescent Health.” Journal of the American Medical Association 278 (10): 823–832. doi:10.1001/jama.1997.03550100049038.
- Richardson, D. B., N. D. Volkow, M.-P. Kwan, R. M. Kaplan, M. F. Goodchild, and R. T. Croyle. 2013. “Medicine. Spatial Turn in Health Research.” Science 339 (6126): 1390–1392. doi:10.1126/science.1232257.
- Rosen, S. 1974. “Hedonic Prices and Implicit Markets: Product Differentiation in Pure Competition.” Journal of Political Economy 82 (1): 34–55. doi:10.1086/260169.
- Sallis, J. F., N. Owen, and E. B. Fisher (2008) “Ecological Models of Health Behavior.” In Health Behavior and Health Education: Theory, Research, and Practice edited by K. Glanz, B. K. Rimer, and K. Viswanath, 4th ed., 465–486. San Francisco, CA: Jossey-Bass.
- Schipperijn, J., M. Ried-Larsen, M. S. Nielsen, A. F. Holdt, A. Grøntved, A. K. Ersbøll, and P. L. Kristensen. 2014. “A Longitudinal Study of Objectively Measured Built Environment as Determinant of Physical Activity in Young Adults - the European Youth Heart Study.” Journal of Physical Activity & Health. doi:10.1123/jpah.2014-0039.
- Shoval, N., M.-P. Kwan, K. H. Reinau, and H. Harder. 2014. “The Shoemaker’s Son Always Goes Barefoot: Implementations of GPS and Other Tracking Technologies for Geographic Research.” Geoforum 51: 1–5. doi:10.1016/j.geoforum.2013.09.016.
- Simpson, C. L., and L. L. Novak. 2013. “Place Matters: The Problems and Possibilities of Spatial Data in Electronic Health Records.” AMIA Annual Symposium Proceedings 2013: 1303–1311.
- Smith, V. K., and J.-C. Huang. 1995. “Can Markets Value Air Quality? A Meta-Analysis of Hedonic Property Value Models.” Journal of Political Economy 103 (1): 209–227. doi:10.1086/261981.
- Spielman, S. E., and E.-H. Yoo. 2009. “The Spatial Dimensions of Neighborhood Effects.” Social Science & Medicine 68 (6): 1098–1105. doi:10.1016/j.socscimed.2008.12.048.
- Stevens, V. J. 2001. “Long-Term Weight Loss and Changes in Blood Pressure: Results of the Trials of Hypertension Prevention, Phase II.” Annals of Internal Medicine 134 (1): 1–11. doi:10.7326/0003-4819-134-1-200101020-00007.
- Stow, D. A., C. D. Lippitt, and J. R. Weeks. 2010. “Geographic Object-Based Delineation of Neighborhoods of Accra, Ghana Using Quickbird Satellite Imagery.” Photogrammetric Engineering & Remote Sensing 76 (8): 907–914. doi:10.14358/PERS.76.8.907.
- Thornton, L. E., J. R. Pearce, and A. M. Kavanagh. 2011. “Using Geographic Information Systems (GIS) to Assess the Role of the Built Environment in Influencing Obesity: A Glossary.” International Journal of Behavioral Nutrition and Physical Activity 8: 71. doi:10.1186/1479-5868-8-71.
- Troiano, R. P., D. Berrigan, K. W. Dodd, L. C. Mâsse, T. Tilert, and M. Mcdowell. 2008. “Physical Activity in the United States Measured by Accelerometer.” Medicine and Science in Sports and Exercise 40 (1): 181–188. doi:10.1249/mss.0b013e31815a51b3.
- Troiano, R. P., J. J. McClain, R. J. Brychta, and K. Y. Chen. 2014. “Evolution of Accelerometer Methods for Physical Activity Research.” British Journal of Sports Medicine 48 (13): 1019–1023. doi:10.1136/bjsports-2014-093546.
- van Dyck, D., E. Cerin, I. De Bourdeaudhuij, E. Hinkson, R. S. Reis, R. Davey, O. L. Sarmiento, et al. 2014. International Study of Objectively Measured Physical Activity and Sedentary Time with Body Mass Index and Obesity: IPEN Adult Study. International Journal of Obesity (London) 39 (2): 199–207.
- Vandevijvere, S., C. Monteiro, S. M. Krebs-Smith, A. Lee, B. Swinburn, B. Kelly, B. Neal, W. Snowdon, and G. Sacks. 2013. “Monitoring and Benchmarking Population Diet Quality Globally: A Step-Wise Approach.” Obesity Reviews 14 (Suppl 1): 135–149. doi:10.1111/obr.12082.
- Wen, M., and L. Kowaleski-Jones. 2012. “The Built Environment and Risk of Obesity in the United States: Racial-Ethnic Disparities.” Health & Place 18 (6): 1314–1322. doi:10.1016/j.healthplace.2012.09.002.
- Zenk, S. N., A. J. Schulz, S. A. Matthews, A. Odoms-Young, J. Wilbur, L. Wegrzyn, K. Gibbs, C. Braunschweig, and C. Stokes. 2011. “Activity Space Environment and Dietary and Physical Activity Behaviors: A Pilot Study.” Health & Place 17 (5): 1150–1161. doi:10.1016/j.healthplace.2011.05.001.
- Zenk, S. N., J. Wilbur, E. Wang, J. McDevitt, A. Oh, R. Block, S. McNeil, and N. Savar. 2009. “Neighborhood Environment and Adherence to a Walking Intervention in African American Women.” Health Education & Behavior 36 (1): 167–181. doi:10.1177/1090198108321249.
