Abstract
Do people in other areas perceive less risk from the COVID-19 pandemic than those in Hubei Province in the pandemic area? Do people in communities with COVID-19 infections perceive a higher level of risk of the virus? What media do people use to get information about the pandemic, and how do the chosen information source influence risk perception? To answer these questions, this study conducted an online questionnaire survey among the public in Guangdong and Hubei Provinces (N = 407) between January and April 2020, and systematically analyzed the impact of proximity to the pandemic and different types of information media on pandemic risk perception. It found that during this period, there was no difference in residents' pandemic risk perception between Hubei and other provinces, and that the greater the number of relatives and friends infected with the virus, the higher people’s pandemic risk perception. Individual social media use positively influences perception, and it is the most powerful variable for predicting pandemic risk perception.
Introduction
COVID-19 is a deadly virus that has threatened the health of large quantities of people has threatened health in virtually every country on the globe (Chauhan and Singh Citation2020a). As of October 2021, 245 million people have become infected and nearly 5 million have died (WHO Citation2021). In 2020, most countries imposed complete to partial lockdowns, quarantines on infected people, and mask mandates to stop the spread of COVID-19 (Chauhan and Singh Citation2020b; Mishra et al. Citation2021). Although some people followed these provisions closely, others ignored the government orders and circulated in public places or congregated in crowds. This fact shows major differences in people’s perception of the risks of the pandemic, which varied across different regions (Cori et al. Citation2020; Cvetković et al. Citation2020; Zhou Citation2021). Because risk perception influences behavior, it may impact the number of infected persons and become a forceful regulator for the spread of infectious diseases.
Policymakers and researchers can improve people’s risk perception and even change their behaviors through understanding how people perceive the risks of events such as a pandemic (Wang et al. Citation2016; Wu et al. Citation2017; Sim et al. Citation2018). It is known from past pandemics that the success of policies to alleviate the spread of infectious diseases hinges partly on the public's accurate recognition of the relative risks (Slovic 2000). People who perceive greater risks are more likely to adopt protective behaviors (Bruen and Gebre Citation2001; de Bruin and Bennett Citation2020), such as frequent hand washing, keeping physical distance from others, and wearing a mask (Poletti et al. Citation2011; Rudisill Citation2013). Higher risk perception influences people's psychological states, and can even trigger depression (Lam et al. Citation2020). As a consequence, accurate perception of risk by the public is of great significance for the effective management of public health risks (Van Der Bles et al. 2020; Dryhurst et al. Citation2020).
A large number of studies have been done on the factors that influence risk perception, mainly focusing on natural disasters such as floods, volcanic eruptions and earthquakes. These studies have shown that media reports, age, gender, education, and past experiences all influence individual risk perception (Hung et al. Citation2007; Wachinger et al. Citation2013). Information media play a decisive role in people's risk perception; in fact, for most hazardous events, risk perception stems primarily from exposure to media information (Kasperson et al. Citation1988; Wiegman and Gutteling Citation1995; Ahmad and Murad Citation2020). However, some researchers hold the view that for excessive media users, media may not be a strong causal factor in individual risk perception, but only one of many factors (Wahlberg and Sjoberg Citation2000). Even some people who are directly experiencing some kind of risk tend to neglect mass media information, arguing that information from the media is inaccurate (Wiegman and Gutteling Citation1995). Therefore, people’s perception of the degree of risk during a pandemic might be more easily influenced by personal experiences and friends' experiences (Tyler Citation1984; Wahlberg and Sjoberg Citation2000). However, there is insufficient research comparing the impacts of direct and indirect experience or of different types of media on risk perception.
Our understanding of how people perceive risks associated with COVID-19 varies across countries, perhaps due to differences in how the pandemic has unfolded and cultural differences (Huynh Citation2020). The Chinese government implemented public health measures, including contact tracing, quarantines, isolation, and so on. This decisive and systematically implemented set of interventions contributed to rapid mitigation in 2020 (Tang et al. Citation2020). The Chinese people willingly cooperate with government public health orders, which may be a reflection of national identity and culture, specifically collectivism, which may incline them to adopt COVID-19 prevention behaviors (Huang et al. Citation2020; Van Bavel et al. Citation2021). Since the COVID-19 outbreak in China, social media such as Weibo and WeChat have become some of the most used sources for Chinese people to obtain information on the pandemic. WeChat is a primary source for COVID-19 information in China, and thus potentially has a major effect on people’s risk perceptions (Jia and Meng Citation2020; Qian and Hanser Citation2021; Zhong et al. Citation2021).
The study reported here sought to understand how people’s geographic proximity to the pandemic and their choice of information media influences their perception of the risks associated with the COVID-19 pandemic through a survey administered in Guangdong and Hubei Provinces (N = 407) between January and April 2020. This paper analyzes the impacts of people’s direct and indirect experiences of the pandemic and compares the degree of influence of pandemic proximity and media type.
2. Literature review
2.1. Pandemic risk perception
"Risk perception" is an unclear term with multiple implications, which is often attributed to researchers’ personal attitudes, beliefs, feelings, and perceptions of risk (Coleman,Citation1993). With respect to risk of infection, scholars are mainly practice oriented, assessing social epidemiology, especially psychological reaction of the general population or special groups (such as healthcare workers) to the threat of diseases like SARS or avian influenza, to predict the adoption of protective behaviors and provide data for future intervention programs. In the case of infectious diseases such as COVID-19, the infection might be fatal and a substantial number of people are simultaneously impacted within the same geographical area (Leppin and Aro Citation2009).
Risk perception in the COVID-19 pandemic can be understood as people’s sensitivity to the danger of becoming infected or dying and their judgment of the degree of danger (Ferrer and Klein Citation2015; Yang and Cho Citation2017).
Individuals' risk perception and judgment of the degree of risk are based to some extent on their experiences, whether direct or indirect. The direct experience involves being a participant in or victim of an event, or witnessing it. Indirect experience is external to the individual, such as news media and education (Wachinger et al. 2013). Since most people do not directly experience major risks like natural disasters, their assessment of risk relies more on media information. Wiegman and Gutteling (1995) argued that mass media reports influence risk perception among people who have not experienced specific risks. They indirectly experience these risks through media reports, and those reports become their standard of authenticity for judging risk. People with direct experiences, such as living near a nuclear power station, formulate their criteria for judging risks based on their own direct experiences. They use a self-verification test to judge the degree of risk: they will feel such risks themselves from the people around them or the environment where they live, and dilute or deny media information that is incompatible with their personal experiences. Therefore, direct and indirect experiences have different influences on individual risk perception.
This study roughly divides the influencing factors of pandemic risk perception into two categories: direct and indirect experience. Direct experience refers to the individuals who are experiencing pandemic risks, which is associated with their regional geographical location and the contagion risks of people around them during the pandemic. In contrast, indirect experience is mainly associated with media exposure, with different information channels having different impacts on risk perception (Brenkert-Smith et al. Citation2013). Therefore, this paper will discuss the factors that influence pandemic risk perception from two perspectives: the direct experience of pandemic proximity and the indirect experience of media use.
2.2. Pandemic proximity as the antecedent to pandemic risk perception
The spatial association is significant for risk perception. Some scholars believe that hazard proximity is the decisive factor in risk perception (Arias et al. Citation2017). Many researchers have examined the relationship between hazard proximity and risk perception. Some have found a positive correlation between the two; specifically, the closer people are to the risk area, the higher their perceived risk. Barberi et al. (Citation2008) surveyed 2488 participants living near the volcanoes in Italy, divided into red and yellow areas according to their risk levels from high to low, and discovered that residents living in the red area with higher risk perception of volcanic eruptions than those living in the yellow area (Barberi et al. Citation2008). Arias et al. (Citation2017) investigated perceptions of the 2013 tsunami in Chile, and discovered that the closer people lived to the coast, the more accurately they perceived the risks of the tsunami. However, some scholars have drawn the opposite conclusion: that people living near the source of danger may have a weaker awareness of risk than those who live farther away. Wiegman and Gutteling (Citation1995) reported that residents who lived far from nuclear power stations had a higher level of insecurity than those living near the stations. This might be because people who have direct personal experience with industrial hazards base their judgments of risk primarily on their own experiences, and are more likely to disbelieve news reports. Thus they are less negatively influenced by the media reports, whereas people who live far from a potential hazard must rely more on media reports, which produces a greater sense of fear. Brody et al. (Citation2004) drew a similar conclusion. They mapped spatial patterns of air quality in two cities, Dallas and Houston, Texas, using Geographic Information System (GIS). They discovered that even though Dallas and Houston had the most severe air pollution in the United States, people in Texas appear very optimistic that their local air quality is extremely good and have a lower risk perception of air pollution than residents of other American cities outside Texas. This may be associated with Texans being more inclined to identify with the cultural phenomena of their own state than the country as a whole.
There may be differences in the influences of geographic proximity on risk perception of different types of hazards (Arias et al. Citation2017). Lindell and Hwang (Citation2008) discovered that risk perception is associated with the distance from coastlines (hurricane risks) and chemical plants (pollution risks). However, there is nothing to do with the distance from rivers (flood risks), demonstrating that the nature of disasters also influences the relationship between geographic proximity and risk perception (Lindell and Hwang Citation2008). After the outbreak of the COVID-19 pandemic in China, Liu et al. (Citation2020) discovered that the closer people are to risk areas, the higher their risk perception. However, they only classified risky areas by the number of infected persons in the community, neglecting differences in infection rates in different provinces in China. In addition to the number of infected people in a community, the severity of the pandemic in different provinces may also influence people’s risk perception. Wuhan, the capital of Hubei Province, was the most severely affected area after the outbreak of the COVID-19 pandemic. The people of Hubei have likely had a higher risk of infection and this might impact their perception of the risk of the virus. Therefore, this study uses Hubei Province as a point of reference. In my interviews conducted at an earlier stage, it was found that when people they know well are infected with the virus, people more often feel nervous or fearful, and might have a stronger perception of pandemic risk.
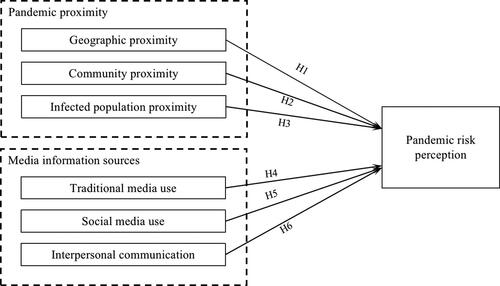
Based on the above studies, this study proposes the following hypotheses:
H1: People in other provinces have a lower pandemic risk perception than those in the pandemic area in Hubei Province.
H2: The greater the number of infected people in a community or within three kilometers, the higher people’s pandemic risk perception will be.
H3: The greater the number of people’s friends, relatives, or acquaintances who got COVID-19, the higher their pandemic risk perception will be.
People do not always directly experience the risks associated with health threats. When they lack direct experience, they often get information from the media or other people (Kasperson et al. Citation1988; Ader Citation1995). Especially when a new infectious disease emerges, people are inclined to acquire information about the disease from new media such as social media. From a sample of 391 Vietnamese respondents aged 15 to 47 years, Huynh (Citation2020) found that people’s frequency of using social media could positively impact risk perception of the COVID-19 virus. In addition to the internet, news media and interpersonal networks are two major channels of information transmission (Kasperson et al. Citation1988). Kasperson et al. (Citation1988) noted that it is possible for each message sender to alter information by enhancing, weakening, or filtering part of it. Therefore, the media are not merely neutral intermediaries, but also alter information in the course of transmission in order to influence the recipients of the information. Different media can have different influences on the audiences’ risk perception. Studies in recent years have also shown that even if the same information spreads through different media, it may have different influences on the public's risk perception due to the unique characteristics of different channels (Vyncke et al. Citation2017; Sim et al. Citation2018). Chan et al. (Citation2018) discovered that during the spread of the Zika virus in the United States, social media reports about the virus influenced people's risk perception, while traditional media reports were irrelevant. The reason for this might be the differences in the speed of propagation, information capacity, and the number of information sources between the two types of media.
In the context of infectious diseases, there are currently few comparative studies on the impact of different types of media on pandemic risk perception; more studies investigate the impact of one type of medium. Some researchers have found that newspaper reports impact people’s perceived risk of infectious disease (Fung et al. Citation2011). Extensive coverage on traditional media may add to individual perceived risk; sensational information on social media may also lead to public stress and panic and add to public perceived risk. Ali et al. (Citation2019) found that sensational reports about the Zika Virus on social media, such as references to the “Zika crisis” or the “Killer virus,” or terror-inducing photos posted on Facebook, may elevate the public’s perceived risk of this disease. Generally speaking, current studies on the impact of media information on the perception of risk put more emphasis on a certain media type, lack a comparison of different media, and focus on the perspective of media communicators rather than that of audience.
Besides traditional media and social media, interpersonal communication is often reported to have a significant impact on individual perceived risk (Mazur and Hall,1990; Binder et al. Citation2011; Lin and Lagoe, Citation2013). According to social contagion theory, perceived risk may become contagious through interpersonal communication, such that individuals in the same network have similar perceptions of risk (Mazur and Hall,Citation1990; Sim et al. Citation2018). The Social Amplification of Risk theory (Kasperson et al. Citation1988) also affirms that an individual’s interpersonal social network is a “site” where risk information is processed, and it can further amplify or weaken risk-related information (Binder et al. Citation2011). Morton and Duck (Citation2001) surveyed 117 students in Australian University and found that interpersonal communication may amplify the individual perceived risk of skin cancer: respondents who had discussed skin cancer with others were more likely to have a higher perception of the risk of getting skin cancer. Brenkert-Smith (Citation2013) et al. Investigated fire hazards in the Western United States, and found that people who discussed fires with neighbors perceived higher consequences of fires. However, Sim et al. (Citation2018) arrived at the opposite conclusion that a higher frequency of interpersonal communication is associated with lower perceived risk. They surveyed a small village and found that information acquired from villagers or relatives was negatively correlated with individual perceived risk of natural disasters such as fires, accidents, or floods. The different conclusions reached by researchers may be associated with the extent of information transmission. On the one hand, people who acquire more knowledge about a certain disease are more likely to perceive greater risk. On the other hand, excessive information access may also weaken perceived risk. A study by Renn (Citation2006) revealed that even when people are well aware of the health risks of behaviors such as smoking, they tend to downplay the hazards. Because such risk is believed to be put under control easily, they may consider themselves less vulnerable.
Many researchers have considered the impacts of different information transmission channels on individual perceived risk. There is less research on the impacts of traditional media, social media, and interpersonal communication on individual perceived risk concurrently and comparisons of the extent of the impact of these three channels from the perspective of intended recipient exposure in the context of a disease outbreak. From the above discussion, our further hypotheses are:
H4: The more people use traditional media to acquire information, the higher their pandemic risk perception.
H5: The more people use social media to acquire information, the higher their pandemic risk perception.
H6: The more people acquire information through interpersonal communication, the higher their pandemic risk perception.
Following these research hypotheses, the research model is proposed below ( and ).
3. Methods
3.1. Data collection
The hypotheses presented above were investigated by conducting a survey in the Chinese provinces of Hubei, where COVID-19 first broke out, and Guangdong, a coastal region that was subsequently affected by imported cases of the coronavirus from other countries beginning in late March 2020. Given that the survey coincided with the pandemic, it was not feasible to conduct an extensive nationwide survey. There are 17 municipal districts in Hubei and 21 in Guangdong. Thirty communities were selected from different urban areas of each province using a multistage sampling method.
The survey was conducted online using WeChat groups. During the COVID-19 pandemic, to facilitate community management and self-isolation, community workers established community WeChat groups, which proved very convenient for this study. The online questionnaires could be forwarded directly by community staff or local researchers through the WeChat groups. Questionnaires were distributed on the WeChat app because WeChat provided a primary information access channel for users during the COVID-19 outbreak (Zeng and Zhang Citation2020) and also because with many residents having to quarantine at home, WeChat groups provided the main method of information exchange. The survey team distributed questionnaires from 1 April 2020 to 1 May 2020. A total of 432 questionnaires were returned, 407 of which were valid.
Over the two months preceding the start of the questionnaire (during the early part of the outbreak of COVID-19, in February and March 2020), 163 respondents (40.05%) were located in Hubei, 149 (36.61%) were in Guangdong, and 95 (23.34%) were in other provinces. Nearly one-quarter of the respondents from other provinces worked or lived permanently in Guangdong or Hubei, but had returned to their hometown during the Lunar New Year Festival and were prevented by the pandemic from returning to their primary place of residence or work.
Of the 407 respondents, 51.84% were male and 48.16% were female; 148 were in the 25 to 30 age group and 147 were aged 31 to 40. During the pandemic, 57.49% of respondents were located in urban areas and 42.51% were in rural areas. In terms of education, 24.32% had below a bachelor’s degree, 36.12% had a bachelor’s level of education, and 39.56% had higher than a bachelor’s degree.
3.2. Measurement
3.2.1. Pandemic proximity
This study's measurement of pandemic proximity is divided into three dimensions: geographical proximity, community proximity, and infected population proximity.
Geographical proximity
In January 2020, cases of COVID-19 initially came mainly from Hubei Province, which became the province with the highest numbers of infections and deaths. Therefore, this province is identified as the most infected area since the outbreak of the pandemic (as of November 15, 2020, the cumulative cases reached 68,148) (Baidu Citation2020). In late March 2020, with the development of the outbound pandemic, Guangdong Province, with its large export trade, began to be influenced by overseas outbreaks, and the growing number of infections primarily came from overseas. The pandemic in Guangdong Province gradually worsened, with Guangdong becoming the province with the second-largest number of cases (as of November 15, 2020, the cumulative cases reached 1,966, far behind Hubei). Because direct experience can influence risk perception, we selected two areas of Hubei and Guangdong Provinces as the survey locations to compare the impact of different locations on people's risk perceptions. The period from the initial outbreak to the spread of the pandemic (between January and March 2020) coincided with the traditional Chinese Spring Festival (January 25), a peak season for population flow. About half of the 11 million people in Wuhan, the capital of Hubei, left the city before the Spring Festival. As the most important province for the Chinese economy, Guangdong has the largest floating population in China due to migrant workers. After the Spring Festival (mid to late February), a very large number of migrant workers swarmed into Guangdong. Thus part of the respondents in this study lived in provinces beyond Hubei and Guangdong, and they returned to their hometowns during the Spring Festival. As Hubei Province was the most severely impacted pandemic area in China, as well as the area where the pandemic was first discovered, this study mainly used Hubei Province as a point of reference to compare pandemic risk perception in Guangdong Province and the flow of people in both areas. Considering the characteristics of population mobility before and after the Spring Festival, this study emphasized analyzing the places where the respondents were located during the period between the outbreak and the spread of the pandemic. The survey question read, "Where have you mainly stayed from since the outbreak until now (January to April)? (Please fill in the provinces and cities where you have stayed for more than two months.).” The response options included “Hubei Province,” “Guangdong Province,” “and other provinces and cities (M = 2.67, SD = 1.56).”
Community proximity
During the pandemic, people could learn about the number of infected people within the community through the community residents committee or use the Baidu Maps app to find the locations of infected people, check the pandemic situation around them, and find out the number of infected people within the scope of three surrounding kilometers. To this end, the survey asked, community proximity in this study is: “What is the number of infected people in your community or within the scope of three kilometers?” The options were “None, 1–5, 6–10, 11–15, and more than 15” (M = 2.14, SD = 1.68).
Population proximity
When the pandemic began, our research team happened to be in Xiantao, a City about 100 kilometers from Wuhan, where the pandemic was most severe. Through interviews our team conducted, we found that when friends or relatives are infected, people are more likely to be nervous and afraid, and their pandemic risk perception is stronger. Therefore, this study confirmed participants’ proximity to COVID-19 infections by asking, “In this pandemic, are relatives, friends, or acquaintances around you infected?" The response options included no, 1–5, 6–10, 11–15, and more than 15 (M = 1.17, SD = 0.66).
3.2.3. Use of different information media
In this study, we measured the use of different informational media based on the crisis-information-seeking scale designed by Lee and Jin (Citation2019) for information-seeking behaviors in a public health crisis. To design options for the scale, three media categories used in China were considered: traditional media, social media, and interpersonal communication. The respondents were asked to indicate their frequency of the specific behaviors on a 5-point Likert scale (ranging from 1 = NA to 5 = on a daily basis). For traditional media the options were (1) I get pandemic information from traditional news media, such as reading newspapers and magazines and watching TV, or (2) I get pandemic information from community radio (M = 6.14, SD = 2.25). For social media the options were (1) I get pandemic information from Weibo, (2) I get pandemic information from WeChat/QQ/Facebook, or (3) I get pandemic information from TikTok and Kuaishou short videos (M = 8.54, SD = 3.24). For interpersonal communication the options were (1) I get pandemic information from face-to-face talk or phone calls from family, relatives and friends or (2) I get pandemic information from community service workers (M = 5.71, SD = 2.16).
3.2.4. Pandemic risk perception
Pandemic risk perception was measured using Park’s (Citation2019) for Zika virus research and the measurement scales of perceived emergency risk designed by Gutteling and De Vries (Citation2017). Participants were asked whether they agreed or disagreed with the following statements: “The community where I am living has endured serious pandemic risk”; “The community where I am living may be subject to pandemic risk in future”; and “I am very worried about being infected by the virus.” The items were measured using a 5-point Likert scale ranging from 1 = strongly disagree to 2 = strongly agree. The Cronbach's α was 0.83, the Kaiser-Meyer-Olkin (KMO) test for sampling adequacy was 0.71, and Bartlett’s test of sphericity was p < 0.001, which suggests a good reliability and validity of the test.
3.3. Control variables
The control variables in our study were age (M = 3.53, SD = 1.20), gender (male: 51.85%, female: 48.15%), education (M = 4.83, SD =1.33; range = 1 [primary school or below] to 5 [master’s degree or above]), and region (urban area = 57.49%; rural area = 42.51%).
3.3. Data analysis
This study uses a nested regression model between variables using the statistical software Stata to elucidate the causality between different variables. The dependent variable is pandemic risk perception. The independent variables are the three dimensions of pandemic proximity (geographical, community, and population) and the frequency of use of three types of transmission of pandemic information (traditional medial, social media, and interpersonal communication). In the regression model, first the control variables and then the independent variables are substituted into the regression model.
4. Results
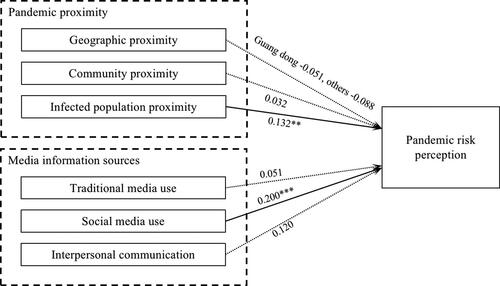
Hypothesis 1 proposes that people in other provinces of China have a lower pandemic risk perception than those in Hubei, the pandemic area. The correlation analysis () shows that there is a significant negative correlation between the areas where people are located and their pandemic risk perception (r = −.146, p < .05). However, the regression equation (, M1) shows that during the pandemic, there was no difference in pandemic risk perception between people in Hubei and those in other provinces (, M3). This demonstrates that people's perception of risk was not affected by their geographical location. Therefore, H1 is rejected.
Table 1. Descriptive statistics and bivariate correlations between key variables.
Table 2. Regression analysis of pandemic risk perception.
Hypothesis 2 assumes that the greater the number of people infected with the pandemic in the community or within three kilometers, the higher people’s pandemic risk perception will be. Correlation analysis () concludes that there is no relationship between community proximity and pandemic risk perception. Regression analysis further verified that the regression between community proximity and pandemic risk perception was not significant (, M3). Thus, H2 is rejected.
Hypothesis 3 suggests that the greater the number of people’s relatives, friends, or acquaintances who are infected with COVID-19 virus, the higher their pandemic risk perception. Correlation analysis() shows that there is a significant positive correlation between knowing infected people and risk perception (r = .152, p < .05). Regression analysis (, M3) further verified that knowing infected people can positively predict thepeople’s pandemic risk perception (β = .132, SE = .265, p < .05). Hence, the findings support H3.
Hypothesis 4 assumes that the more individuals use traditional media to acquire information, the higher their pandemic risk perception. Correlation analysis discovered a significant positive correlation between traditional media use and risk perception (r = .199, p < .05). However, the regression analysis results do not draw a regression relation between the two. Thus, H4 is unsupported.
Hypothesis 5 proposes that the more individuals use social media to acquire information, the higher their pandemic risk perception. Correlation analysis shows a significant positive correlation between social media use and risk perception (r = .267, p < .05). The regression equation (, M3) also shows a significant effect of social media use on pandemic risk perception is significant (p < .001), and the direction of application is positive (β = .200, SE =.057). Therefore, H5 is supported. It is noteworthy that social media use is the variable that has the greatest impact on the risk perception in regression equation model 3 (M3).
Hypothesis 6 predicts that the more people acquire information through interpersonal communication, the higher their pandemic risk perception will be. The correlation analysis shows a significant positive correlation between interpersonal communication and risk perception (r = .248, p < .05). However, the regression equation (, M3) shows that the regression of interpersonal communication to risk perception is insignificant (p> .05). Hence, H6 is rejected.
Based on the pandemic proximity variable module (M2) and the media-use module (M3), it is found that the variation was increased by 8.55%, which indicates that media use had a significant influence. Moreover, media use has a greater influence on the pandemic-risk perception than pandemic proximity does. Interestingly, after we added the media use module, the impact of proximity to an infected population on the pandemic risk perception was also greater, indicating that people’s pandemic risk perception may be simultaneously influenced by the infected population near them and their social media use.
5. Discussion
By investigating people's risk perception during the COVID-19 pandemic in China, this study attempted to understand the factors that influenced their perception of the risk of the pandemic based, first, on their direct experiences, namely, their geographical proximity to the pandemic, and second, their indirect experiences, specifically, the media through which they obtained information about the pandemic.
The results showed that people’s proximity to their knowing infected people could predict their pandemic risk perception, and social media use will also positively influence pandemic risk perception. Generally speaking, the indirect experience of acquiring pandemic information through social media has a greater impact on people's pandemic risk perception than their direct experiences of the pandemic.
This study found that people who have more relatives, friends, or acquaintances who have been infected with COVID-19 have a higher perception of the risk of the virus. The infected population proximity has a significant influence on the risk perception. This confirms the findings of some previous studies. Liu et al. (Citation2020) found that due to the high infectiousness of COVID-19, people who personally knew someone infected with the virus were more susceptible to anxious thoughts than others. Risk perception is also a psychological state and thus is impacted by feelings of fear (Paek et al. Citation2016). If relatives and friends in the vicinity are infected, this may cause panic and anxiety for those who know them. The fact that COVID-19 is easily transmitted through close contact can increase people’s stress and anxiety and subsequently their risk perception. Social contagion theory indicates that individual risk perception is formed based on connections with others. Over time, people’s risk perceptions become more and more similar to each other (Scherer and Cho Citation2003).
However, the study found no difference in risk perception between people in Hubei and other provinces, and no difference in risk perception relative to community proximity. This further shows that people’s perception of risk during a pandemic stems more from psychological factors than from their physical distance from the crisis. In other words, spatial proximity to risk was found to have no influence on people’s risk perception during the COVID-19 outbreak (Zielinski-Gutierrez and Hayden Citation2006). A possible explanation for this is that soon after the outbreak, most provinces in China launched a high-level response with response to the pandemic in succession in late January 2020, and many communities called upon people to be quarantined in their homes. Given the strong Chinese collective identity, people tend to follow public health measures (Van Bavel et al. Citation2021). Also, more than three-quarters of the respondents came from Hubei Province, where the pandemic was most severe. Guangdong and other provinces were influenced by the outbound pandemic later. People’s pandemic risk perception might be relatively similar during the whole period, resulting in no difference in people's pandemic risk perception in different communities.
The study found that social media use positively influences pandemic risk perception. That is, the more people use social media to acquire information about the pandemic, the higher their risk perception. After the sudden onset of a major event, people's mentalities are markedly different, depending on their choice of media (Sugimoto et al. Citation2013). Due to the uncertainty posed by the pandemic, people will actively look for and continually update information through a variety of channels. Because of the rapid expansion of technology, new media models such as social media have already become important sources of risk and relevant health information (Westerman et al. Citation2014). Media, especially social media, played a particularly important role in impacting the public response to COVID-19, as most Chinese people were quarantined at home, and the increased exposure to pandemic-related information leads to more anxiety (Kim et al. Citation2011; Liu et al. Citation2020). Social media provides a potentially powerful new platform for people to look for this kind of information (Spence et al. Citation2016; Moon and Shim Citation2019). Moreover, searching for information on social media magnifies people’s emotions and enhances their risk perception (Chong and Choy Citation2018). It is also easier to provoke discussion about negative events related to the pandemic on social media, thereby increasing people’s risk perception.
It is noteworthy that compared with interpersonal communication and social media, traditional media such as television, newspapers, and radio were the most popular media for the respondents during the pandemic. However, the traditional media variables only presented a significant correlation with pandemic risk perception, and did not generate regression causality. This result reflects the high frequency with which Chinese people use traditional media, the internet, and interpersonal relationships to acquire health information, and further confirms that social media plays an important role in developing a new media environment. Social media also plays a role in amplifying risk (Moon and Shim 2019). On the one hand, due to technological challenges and censorship, as well as high dependence on official information, traditional media with delay in reporting pandemic news to a great degree (Chong and Choy Citation2018). Conversely, frontline information about the pandemic often comes from social media in the pandemic area, so that the public can promptly obtain up-to-date pandemic information and evaluate the level of risk. On the other hand, pandemic news reported through traditional media is more balanced and rational, rather than emphasizing emotional viewpoints. Compared with traditional media, social media amplifies emotions, which can further influence risk perception (Chong and Choy Citation2018). In addition, most of the information about the pandemic issued by China's traditional media needs to wait for approval from authorities, such as the Pandemic Prevention and Control Command Center and government publicity departments. In crisis events, the government's information control has resulted in restrictions on media performance (Zhang et al. 2020), which has made traditional media more cautious when transmitting information about the pandemic. This also helps traditional media avoid triggering panic. Therefore, it needs time for the public to perceive the pandemic risk through traditional media channels.
6. Conclusions
Although some studies have analyzed people’s pandemic risk perception from the point of view of psychological factors and media information sources, including community platforms and community workers (He et al. Citation2021; Zhong et al. Citation2021), few have compared the influence of direct and indirect experience on pandemic risk perception from the perspective of pandemic proximity and different kinds of media information sources simultaneously. This study fills this research gap by empirically investigating the impact of pandemic proximity and information sources on risk perception during the COVID-19 pandemic in the context of Chinese media. The study found that information acquired through social media can significantly influence people’s risk perception, which indicates that exposure to COVID-19 information on social media might increase preventive behaviors (Oh et al. Citation2021; Zeballos Rivas et al. Citation2021). Some researchers have found that media does not influence risk perception and argue that personal experience is the influencing factor (Tyler Citation1984). However, in the context of the COVID-19 pandemic in China, this study demonstrated that people’s indirect experience of acquiring information through social media has a greater influence on risk perception than their direct experience with the pandemic. This is probably because after the outbreak of the COVID-19 pandemic, many Chinese people self-isolated at home and practiced social distancing. This type of stronger protection awareness makes them avoid close contact with people infected with COVID-19 and gather in public places, resulting in relatively limited pandemic risk perceived by individuals from the real environment around them. This causes their pandemic risk perception to be more influenced by the information transmission from social media. Moreover, social media use is the biggest factor influencing risk perception, which also indicates the popularity of social media in China and demonstrates how social media has become the major channel for obtaining information during the pandemic. Therefore, the spread of pandemic information via social media can improve people's pandemic risk perception, strengthen public preventive behaviors, and slow the spread of the pandemic (Kim et al. Citation2011).
The study has two policy implications. First, people in different regions and communities may have relatively consistent pandemic risk perceptions. Therefore, to avoid spreading panic, the government should publish accurate and timely COVID-19 information so that people in different regions are fully informed. Second, because social media has a significant impact on people's perception of risk, and is a major conduit for spreading health misinformation (Chen et al. Citation2021), the government and social media platforms should strictly control false information.
This study has three limitations. First, the pandemic was still ongoing when this survey was conducted. Therefore, it only investigated risk perception during this early period (between January and April 2020), while control measures were taking hold in China. Whether there were any differences in the factors that influenced risk perception between the earlier and later periods remains to be investigated. Second, this research was conducted in infected areas during the COVID-19 pandemic, which may limit the generalizability of the findings. Finally, this study tested pandemic proximity and media use, but did not take into account other possible environmental factors on the public’s pandemic risk perception. Future studies should measure and explore more influencing factors.
Disclosure statement
No potential conflict of interest was reported by the authors.
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- Ader CR. 1995. A longitudinal study of agenda setting for the issue of environmental protection. Journalism Mass Commun Quart. 72(2):300–311.
- Ahmad AR, Murad HR. 2020. The impact of social media on panic during the COVID-19 pandemic in Iraqi Kurdistan: online questionnaire study. J Med Internet Res. 22(5):e19556.
- Ali K, Zain-Ul-Abdin K, Li C, Johns L, Ali AA, Carcioppolo N. 2019. Viruses going viral: impact of fear-arousing sensationalist social media messages on user engagement. Sci Commun. 41(3):314–338.
- Arias JP, Bronfman NC, Cisternas PC, Repetto PB. 2017. Hazard proximity and risk perception of tsunamis in coastal cities: Are people able to identify their risk? PLoS One 12(10):e0186455.
- Baidu. 2020. Retrieved from https://voice.baidu.com/act/newpneumonia/newpneumonia/?from=osari_aladin_banner.
- Barberi F, Davis MS, Isaia R, Nave R, Ricci T. 2008. Volcanic risk perception in the Vesuvius population. J Volcanol Geotherm Res. 172(3-4):244–258.
- Brenkert-Smith H, Dickinson KL, Champ PA, Flores N. 2013. Social amplification of wildfire risk: the role of social interactions and information sources. Risk Anal. 33(5):800–817. doi:10.1111/j.1539-6924.2012.01917.x
- Binder AR, Scheufele DA, Brossard D, Gunther AC. 2011. Interpersonal amplification of risk? Citizen discussions and their impact on perceptions of risks and benefits of a biological research facility. Risk Anal. 31(2):324–334. doi:10.1111/j.1539-6924.2010.01516.x
- Brody SD, Peck BM, Highfield WE. 2004. Examining localized patterns of air quality perception in Texas: a spatial and statistical analysis. Risk Anal. 24 (6):1561–1573.
- Bruen M, Gebre FA. (2001, November). Worldwide public perception of flood risk in urban areas and its consequences for hydrological design in Ireland. Paper presented at the National Hydrology Seminar on Flood Risk Management: Impacts and Development, Ireland.
- Cvetković VM, Nikolić N, Radovanović Nenadić U, Öcal A, K Noji E, Zečević M. 2020. Preparedness and preventive behaviors for a pandemic disaster caused by COVID-19 in Serbia. IJERPH. 17(11):4124.
- Chan MPS, Winneg K, Hawkins L, Farhadloo M, Jamieson KH, Albarracín D. 2018. Legacy and social media respectively influence risk perceptions and protective behaviors during emerging health threats: A multi-wave analysis of communications on Zika virus cases. Soc Sci Med. 212:50–59.
- Chauhan A, Singh RP. 2020. Effect of lockdown on HCHO and trace gases over India during March 2020. Aerosol Air Qual Res. 21.
- Chauhan A, Singh RP. 2020. Decline in PM2. 5 concentrations over major cities around the world associated with COVID-19. Environ Res. 187:109634.
- Chen K, Luo Y, Hu A, Zhao J, Zhang L. 2021. Characteristics of misinformation spreading on social media during the COVID-19 outbreak in China: A descriptive analysis. Risk Manage Healthc Policy. 14:1869–1879.
- Chong M, Choy M. 2018. The social amplification of haze-related risks on the Internet. Health Commun. 33(1):14–21.
- Coleman CL. 1993. The influence of mass media and interpersonal communication on societal and personal risk judgments. Commun Res. 20(4):611–628.
- Cori L, Fabrizio B, Ennio C, Carmen A. 2020. Risk Perception and COVID-19. IJERPH. 17(9):3114. doi:10.3390/ijerph17093114.
- de Bruin WB, Bennett D. 2020. Relationships between initial COVID-19 risk perceptions and protective health behaviors: a national survey. Am J Prev Med. 59(2):157–167.
- Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, Spiegelhalter D, van der Linden S. 2020. Risk perceptions of COVID-19 around the world. J Risk Res. 23(7-8):913–994.
- Ferrer RA, Klein WM. 2015. Risk perceptions and health behavior. Curr Opin Psychol. 5:85–89.
- Fung TK, Namkoong K, Brossard D. 2011. Media, social proximity, and risk: A comparative analysis of newspaper coverage of avian flu in Hong Kong and in the United States. J Health Commun. 16(8):889–907.
- Gutteling JM, De Vries PW. 2017. Determinants of seeking and avoiding risk-related information in times of crisis. Risk Anal. 37(1):27–39. doi:10.1111/risa.12632
- He S, Chen S, Kong L, Liu W. 2021. Analysis of risk perceptions and related factors concerning COVID-19 epidemic in Chongqing, China. J Community Health. 46(2):278–285.
- Huang F, Ding H, Liu Z, Wu P, Zhu M, Li A, Zhu T. 2020. How fear and collectivism influence public’s preventive intention towards COVID-19 infection: a study based on big data from the social media. BMC Public Health. 20(1):1–9.
- Hung HV, Shaw H, Kobayashi M. 2007. Flood risk management for the RUA of Hanoi: Importance of community perception of catastrophic flood risk in disaster risk planning. Disaster Prev Manage. 16(2):245–258.
- Huynh TLD. 2020. Does culture matter social distancing under the COVID-19 pandemic? Saf Sci. 130:104872.
- Huynh TL. 2020. The COVID-19 risk perception: A survey on socioeconomics and media attention. Econ Bull. 40(1):758–764.
- Jia Z, Meng T. 2020. Information as the axis: Media use, information needs and media trust during the COVID-19 pandemic. E-Government 209(5):14–27.
- Kasperson RE, Renn O, Slovic P, Brown HS, Emel J, Goble R, Kasperson JX, Ratick S. 1988. The social amplification of risk: A conceptual framework. Risk Anal. 8(2):177–187.
- Kim JH, Lo FK, Cheuk KK, Kwong MS, Goggins WB, Cai YS, Lee SS, Griffiths S. 2011. Knowledge of avian influenza (H5N1) among poultry workers, Hong Kong, China. Emerg Infect Dis. 17(12):2319–2321.
- Lam SC, Arora T, Grey I, Suen LKP, Huang EYZ, Li D, Lam KBH. 2020. Perceived risk and protection from infection and depressive symptoms among healthcare workers in Mainland China and Hong Kong during COVID-19. Front Psychiatry. 11:686.
- Lee YI, Jin Y. 2019. Crisis information seeking and sharing (CISS): Scale development for measuring publics’ communicative behavior in social-mediated public health crises. JICRCR. 2(1):13–38.
- Leppin A, Aro AR. 2009. Risk perceptions related to SARS and avian influenza: theoretical foundations of current empirical research. International journal of behavioral medicine. 16(1): 7–29.
- Lindell MK, Hwang SN. 2008. Households' perceived personal risk and responses in a multihazard environment. Risk Anal. 28(2):539–556.
- Lin CA, Lagoe C. 2013. Effects of news media and interpersonal interactions on H1N1 risk perception and vaccination intent. Commun Res Rep. 30(2):127–136.
- Liu M, Zhang H, Huang H. 2020. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health. 20(1):1–8.
- Liu M, Zhang H, Huang H. 2020. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC public health. 20(1): 1–8.
- Li Y and Zhu L. 2020. The influence of bias of media news sources on early risk warning - taking the early report of COVID-19 in representative media as an example. Press Circles. 2020(7):12–20.
- Mazur A, Hall GS. 1990. Effects of social influence and measured exposure level on response to radon. Sociolog Inquiry 60(3):274–284. doi:10.1111/j.1475-682X.1990.tb00145.x
- Mishra R, Chauhan A, Singh RP, Mishra NC, Mishra R. 2021. Improvement of atmospheric pollution in the capital cities of US during COVID-19. Model Earth Syst Environ. 9:1–18.
- Morton TA, Duck JM. 2001. Communication and health beliefs: Mass and interpersonal influences on perceptions of risk to self and others. Commun Res. 28(5):602–626.
- Moon M, Shim JC. 2019. Social media effects? Exploring the relationships among communication channels, scientific knowledge and BSE risk perceptions. JCOM. 23(4):281–297.
- Oh SH, Lee SY, Han C. 2021. The effects of social media use on preventive behaviors during infectious disease outbreaks: The mediating role of self-relevant emotions and public risk perception. Health Commun. 36(8):972–981.
- Paek H-J, Oh S-H, Hove T. 2016. How fear-arousing news messages affect risk perceptions and intention to talk about risk. Health Commun. 31(9):1051–1062.
- Park S, Boatwright B, Avery EJ. 2019. Information channel preference in health crisis: Exploring the roles of perceived risk, preparedness, knowledge, and intent to follow directives. Public Relat Rev. 45(5):101794. doi:10.1016/j.pubrev.2019.05.015.
- Poletti P, Ajelli M, Merler S. 2011. The effect of risk perception on the 2009 H1N1 pandemic influenza dynamics. PLoS One 6(2):e16460.
- Qian Y, Hanser A. 2021. How did Wuhan residents cope with a 76-day lockdown? Chin Sociolog Rev. 53(1):55–86.
- Renn O. 2006. Risk communication–Consumers between information and irritation. J Risk Res. 9(8):833–849.
- Rudisill C. 2013. How do we handle new health risks? Risk perception, optimism, and behaviors regarding the H1N1 virus. J Risk Res. 16(8):959–980.
- Scherer CW, Cho H. 2003. A social network contagion theory of risk perception. Risk Anal. 23(2):261–267. doi:10.1111/1539-6924.00306
- Slovic P, editor. 2000. Risk, society, and policy series. The perception of risk. New York: Earthscan Publications.
- Sim T, Hung LS, Su GW, Cui K. 2018. Interpersonal communication sources and natural hazard risk perception: a case study of a rural Chinese village. Nat Hazards 94(3):1307–1326.
- Spence PR, Lachlan KA, Edwards A, Edwards C. 2016. Tweeting fast matters, but only if I think about it: Information updates on social media. Commun Quart. 64(1):55–71. doi:10.1080/01463373.2015.1100644
- Sugimoto A, Nomura S, Tsubokura M, Matsumura T, Muto K, Sato M, Gilmour S. 2013. The relationship between media consumption and health-related anxieties after the fukushima daiichi nuclear disaster. PLoS One 8(8):e65331. doi:10.1371/journal.pone.0065331
- Tang B, Xia F, Bragazzi NL, Wang X, He S, Sun X, Tang S, Xiao Y, Wu J. 2020. Lessons drawn from China and South Korea for managing COVID-19 epidemic: Insights from a comparative modeling study. medRxiv. Retrieved from https://www.medrxiv.org/content/10.1101/2020.03.09.20033464v1.
- Tyler TR. 1984. Assessing the risk of crime victimization: the integration of personal victimization experience and socially transmitted information. J Soc Issues 40(1):27–38.
- Wahlberg AA, Sjoberg L. 2000. Risk perception and the media. J Risk Res. 3(1):31–50.
- WHO. 2021. WHO coronavirus (COVID-19) dashboard. Retrieved from https://covid19.who.int/.
- Wiegman O, Gutteling JM. 1995. Risk appraisal and risk communication: Some empirical data from the Netherlands reviewed. Basic Appl Soc Psych. 16(1):227–249.
- Van Bavel JJ, Cichocka A, Capraro V, Sjåstad H, Conway J. 2021. National identity predicts public health support during a global pandemic: Results from 67 nations. Nature Communications. Retrieved from https://psyarxiv.com/ydt95.
- Van Der Bles AM, van der Linden S, Freeman AL, Spiegelhalter DJ. 2020. The effects of communicating uncertainty on public trust in facts and numbers. Proc Natl Acad Sci USA. 117(14):7672–7683.
- Vyncke B, Perko T, Van Gorp B. 2017. Information sources as explanatory variables for the Belgian health-related risk perception of the Fukushima nuclear accident. Risk Anal. 37(3):570–582.
- Wachinger G, Renn O, Begg C, Kuhlicke C. 2013. The risk perception paradox-implications for governance and communication of natural hazards. Risk Anal. 33(6):1049–1065.
- Wang F, Wei J, Huang S-K. 2016. Public reactions to the 2013 Chinese H7N9 influenza outbreak: perceptions of risk, stakeholders, and protective actions. J Risk Res. 1–25:809–833.
- Westerman D, Spence PR, Van Der Heide B. 2014. Social media as information source: Recency of updates and credibility of information. J Comput-Mediat Comm. 19(2):171–183.
- WHO. WHO coronavirus dashboard. https://covid19.who.int/.
- Wu H-C, Greer A, Murphy HC, Chang R. 2017. Preparing for the new normal: Students and earthquake hazard adjustments in Oklahoma. Int J Disaster Risk Reduct. 25:312–323.
- Yang S, Cho SI. 2017. Middle East respiratory syndrome risk perception among students at a university in South Korea, 2015. American journal of infection control. 45(6):e53–e60.
- Zeng M, Zhang X. 2020. Field reconstruction and mainstream reshaping: User media information contact, cognition and dissemination in epidemic situation. J Commun Univ China 5:65–74.
- Zhang H, Shen f, Li h, Jia Q. 2020. The impact of proximity on the rumors' trust: an analysis of the mediating effect of the communication channels during the 2019-nCov epidemic. Press Circles 4:46–48.
- Zhong Y, Liu W, Lee TY, Zhao H, Ji J. 2021. Risk perception, knowledge, information sources and emotional states among COVID-19 patients in Wuhan. Nurs Outlook 69(1):13–21.
- Zeballos Rivas DR, Lopez Jaldin ML, Nina Canaviri B, Portugal Escalante LF, Alanes Fernández AMC, Aguilar Ticona JP. 2021. Social media exposure, risk perception, preventive behaviors and attitudes during the COVID-19 epidemic in La Paz, Bolivia: A cross sectional study. PLoS One 16(1):e0245859.
- Zhou S. 2021. Impact of perceived risk on epidemic information seeking during the outbreak of COVID-19 in China. J Risk Res. 24(3-4):477–491.
- Zielinski-Gutierrez EC, Hayden MH. 2006. A model for defining West Nile virus risk perception based on ecology and proximity. EcoHealth 3(1):28–34.