Abstract
Introduction
Treatment of individuals who have committed sexual offences with Testosterone-Lowering Medication (TLM) is a comparatively intrusive kind of intervention, which regularly takes place in coercive contexts. Thus, the question of efficacy, but also the question of who should be treated, when and for how long, are of great importance.
Methods
Recidivism rates of TLM-treated high-risk individuals (+TLM; n = 54) were compared with high-risk individuals treated with psychotherapy only in the same forensic outpatient clinic (−TLM; n = 79).
Results
Group differences suggested a higher initial risk of + TLM (e.g. higher ris-assessment, previous convictions). Despite the increased risk, after an average time at risk of six years, +TLM recidivated significantly less often and significantly later than − TLM (27.8% vs. 51.9%). Such an effect was also found for violent (1.9% vs. 15.2%), but not for sexual (5.6% vs. 10.1%) and serious recidivism (5.6% vs. 10.1%), which could be explained partly by the small number of cases. In the course of treatment, TLM proved to be a significant variable for a positive process, whereas a high risk-assessment score indicated a rather negative course. In total, n = 19 individuals had stopped their TLM treatment, of these 31.6% recidivated.
Conclusion
The results support the efficacy of TLM, particularly in the group of high-risk offenders.
Introduction
In attempt to further reduce the recidivism risk of individuals convicted of sexual offences, most Western countries have invested intensively in treatment programs in recent decades. According to the heterogeneity of offences and offenders, very different forms of treatment have been emerged (Schmucker and Lösel Citation2015). Besides psychotherapeutic treatment, testosterone lowering medication (TLM) has been established during the last decades as a promising alternative to irreversible and ethically hardly justifiable surgical castration (Laschet and Laschet Citation1967). By lowering testosterone level, sex drive and thus (deviant) sexual fantasies and behaviours are supposed to be reduced (Eher et al. Citation2007; Turner et al. Citation2013), and thus preventing recidivism with a sexual offence. However, TLM is one of the most intrusive forms of treatment for individuals who committed sexual offences, so empirical evidence on for whom and under what conditions such treatment works is essential. This applies even more if the individuals to be treated live in a coercive context such as prisons or forensic hospitals, where the course of treatment can have an influence on release options, and thus an at least subjectively perceived pressure to consent to medication cannot be precluded.
While in Europe patients were mainly treated with cyproterone acetate (CPA), in the United States medroxyprogesterone acetate (MPA) has been used predominantly. In 1973, CPA was officially approved as a medication for the treatment of individuals who committed sexual offences in Germany. In the 1990s, gonadotropin-releasing-hormone (GnRH)-agonists, considered to be more efficient, were trialled for sex drive suppressing treatment (Eher et al. 2007). In 2009, Triptorelin was also officially approved in Germany for the treatment of individuals who offended sexually diagnosed with a severe paraphilic disorder (Turner et al. Citation2013). Since a higher dosage is required for an effective treatment with CPA/MPA and the side effects of this type of medication are at least in part considered to be more serious, GnRH agonists are currently used more frequently (Rösler and Witztum Citation2000; Turner et al. Citation2013; Thibaut et al. Citation2020). GnRH-agonists are considered to be more effective due to the reduction of testosterone to castration-levels and are mainly used in high-risk individuals (Thibaut et al. Citation2020). Furthermore, GnRH-agonists are used when testosterone production cannot be reliably reduced by CPA/MPA.
Due to serious side effects (Hill et al. Citation2003; Champeaux-Depond et al. Citation2021), and resulting ethical concerns, TLM should only be administered under certain conditions: First, a paraphilic disorder must have been diagnosed and the medication must address specific clinical symptoms and behaviours. Second, the individual represents a serious risk to themselves or others without treatment, and no less intrusive form of treatment appears promising. As with any other treatment, the individual to be treated must give their consent (Thibaut et al. Citation2020). The type and duration of medication must be carefully considered, especially when treating individuals who are in a coercive context. Therefore, international guidelines of the pharmacological treatment of paraphilic disorders (Thibaut et al. Citation2020) published by the World Federation of Societies of Biological Psychiatry (WFSBP) in 2020 recommend a risk/need/responsivity-adapted approach. Depending on the severity of paraphilic disorder and the risk to show (again) sexually violent behaviours, medications of different intensity can be used in addition to psychotherapy: (1) selective serotonin reuptake inhibitors (SSRIs), (2) CPA, (3) GnRH-agonists, and in most severe cases (4) GnRH-agonists in combination with CPA. Treatment should last two years, five years or longer if needed and if there is a persistent high risk for sexual offences (Thibaut et al. Citation2020).
Although patients’ self-reports were used in most studies (Briken et al. Citation2003), it can be presumed that CPA/MPA and GnRH-agonists are able to reduce sex drive as well as nondeviant and deviant sexual fantasies and behaviours (Laschet and Laschet Citation1967; Rösler and Witztum Citation1998; Moulier et al. Citation2012; Ahn et al. Citation2013; Koo et al. Citation2014). Studies using more objective measurement variables like clinical assessment of erection and masturbation (Cooper Citation1981), visual reaction time, penile plethysmograph, and self-reports involving polygraph (Schober et al. Citation2005) or eye tracking and fMRT (Jordan et al. Citation2014) came to similar conclusions. In line with these results, significantly higher increases in (sexual) regulation abilities, as measured by Stable-2007 (Hanson et al. Citation2007), were found in those treated with TLM (Sauter et al. Citation2021). However, evidence was also found that treatment duration had a significantly positive, and Factor-1-scores of the Psychopathy-Checklist-Revised (PCL-R (Hare Citation2003)) a significantly negative impact on this measured change in risk (Sauter et al. Citation2021).
Regarding effectiveness in terms of reducing sexual recidivism, to date no clear evidence exists. So far, not enough studies of sufficient quality were conducted to include and integrate them in meta-analyses (Khan et al. Citation2015; Schmucker and Lösel Citation2015). Apart from low base rates, the feasibility of randomised controlled trials (RCTs) is often queried because it is usually considered to be ethically hardly justifiable by official authorities not to provide a potentially recidivism risk reducing treatment to a control group (see Briken et al. Citation2017). The existing studies, which date back several decades, indicated a positive effect (Emory et al. Citation1992; Hall Citation1995; Rösler and Witztum Citation1998; Maletzky et al. Citation2006). Lately, a number of quasi-experimental studies have been published, which are also optimistic regarding the potential risk-reducing effects of TLM (Gallo et al. Citation2019; Colstrup et al. Citation2020; Sauter et al. Citation2021).
Recently, the first double-blind placebo controlled RCT on the effectiveness of GnRH-antagonist Degarelix® was published (Landgren et al. Citation2020). Degarelix-acetate is a GnRH-antagonist that lowers testosterone-levels to castration levels within a few days. Since GnRH-antagonists can decrease testosterone in a very short time, short-term study duration (measurements after two and ten weeks) was sufficient. The measured risk score as well as sexual preoccupation decreased significantly compared to the placebo group (Landgren et al. Citation2020). However, in contrast to GnRH agonists, GnRH antagonists have not yet been considered in the above-mentioned international guidelines. And the sample used is not a sample of high-risk offenders. Furthermore, a standardised risk score and not recidivism was used as a criterion for effectiveness.
Overall, the current state of research can still be described as scarce. Within the present study, it was possible for the first time to compare officially registered recidivism-rates across a large sample of high-risk offenders treated with TLM with a comparison sample of high-risk offenders treated with psychotherapy only.
Materials and methods
Study design
The Forensic Therapeutic Outpatient Clinic in Berlin, Germany (Forensisch Therapeutische Ambulanz, abbreviated: FTA) provides multi-professional services, which involves psychiatric, psychotherapeutic and social work support. Individuals released from correctional facilities, forensic psychiatry, or preventive detention may be ordered by court to receive forensic follow-up treatment (for an overview of the German forensic treatment system see (Briken et al. Citation2019).
In this retrospective study, all individuals who were or are currently being treated at the FTA, had committed a sexual offence, and already had been released by the cut-off date of December 31, 2019, were included. Treatment files, which contained the sentences and expert opinion reports, were used to collect sociodemographic data, variables about the criminal history and treatment including diagnoses according to International Classification of Diseases-10th Revision (ICD-10). As a standardised assessment of the initial risk of recidivism at the time of release from the closed facility Static-99R (Rettenberger et al. Citation2013; Phenix et al. Citation2016) was rated.
The ethical review board of the Charité - Universitätsmedizin Berlin, Germany, approved the present study (EA 1/210/18).
Participants
Until reporting date (December 31, 2019) FTA provided professional follow-up treatment to N = 231 individuals (225 male, six female). Among those, 146 (all male) had been convicted of a sexual offence. At the time of data collection, 13 had passed away. Of the remaining 133 individuals (study sample), 79 (59.4%) received psychotherapeutic treatment only (Comparison Group [−TLM]) and 54 (40.6%) received additionally TLM-treatment (Treatment Group [+TLM]). With 45 (83.3%), the majority was treated with a GnRH-agonist (Salvacyl®), three of them (5.6%) were additionally treated with SSRI. Exclusively CPA (Androcur®) was given to nine individuals (16.6%). Of the 54 individuals, a total of 19 (35.2%) had stopped TLM-treatment, which had lasted for many years (for more information see 30,31). All others were pharmacologically treated at least until the end of forensic outpatient treatment. By the cut-off date (December 31, 2019), +TLM had a time at risk (time between the latest release and the cut-off date) of M = 6.3 years (SD = 3.7, Min-Max = 0.1–13.6) and − TLM M = 6.6 years (SD = 3.9, Min-Max = 0.4–15.8; see ).
Table 1. Differences between individuals with (+TLM; n = 54) and without (−TLM; n = 79) TLM-treatment.
Measures
The Static-99R (Phenix et al. Citation2016) is the revised version of the Static-99 (Hanson and Thornton Citation2000; Harris et al. Citation2003), the internationally most commonly used actuarial risk assessment instrument for adult males who have committed a sexual offence. The Static-99R consists of ten mostly static items, scores can range from −3 to 12 points and are transferred into nominal risk levels from ‘very low risk’ (equivalent to −3 and −2 points) to ‘well above average risk’ (equivalent to 6 points and larger). The Static-99R is considered a reliable and valid risk assessment instrument for recidivism with a sexual or violent offence after a five-year follow-up period with predictive validities ranging from AUC = .720 to .715 (Helmus et al. Citation2012). Interrater reliability is known to be high (e.g. intraclass correlation coefficient [ICC] = .89 (McGrath et al. Citation2012),). For the present study, Static-99R was rated by the first author, who has successfully completed an officially certified training workshop. The German version of the Static-99R received high effect sizes regarding the interrater reliability and (predictive) validity (Rettenberger et al. Citation2013).
The Central Federal Registers were requested at the Federal Office of Justice in February 2018 and sent in June 2020. The documents include all convicted offences for which a legally final judgement has been passed. All offences with a final conviction since the last release from prison or forensic hospital and up to the reporting date of December 31, 2019, were counted. These were recorded as follows:
General Recidivism included all reconvictions, regardless of its type or severity.
Serious Recidivism included all reconvictions which resulted in a new sentence of two years or more.
Sexual Recidivism included all sexual reconvictions, regardless of its type or severity (incl. non-contact sexual offences).
Violent Recidivism included all violent reconvictions, regardless of its type or severity (excl. all types of sexual offences).
Statistical analyses
One-way multivariate analyses of variance (MANOVA) and χ2-analyses were performed to calculate group differences. Survival time analyses using the offence date of re-offences were calculated and presented with the Kaplan-Meier curve. To be able to include the different lengths of treatment duration and time at risk periods in the calculation, but also to be able to compare the effect sizes between the predictors, a Cox-regression was calculated with TLM treatment as a time-dependent covariate, controlling for the initial risk measured by Static-99R. The hazard function h(t) can be interpreted as the risk per time unit for recidivism at time point t (Fox Citation2002; Ziegler et al. Citation2007). For comparing two groups, hazard ratio (HR) can be calculated, a ratio of the two hazard functions of the groups. This is a measurement of the risk of one group in relation to the risk of the other group, with a HR of 1 indicating an equal risk. A HR > 1 represents that the study group is more likely, a HR < 1 represents that the study group is less likely to have a shorter time at risk period compared to the reference group (Chan Citation2004).
Results
Differences between individuals with and without TLM-treatment
+TLM showed significantly more sexual offences in their criminal history than − TLM (see ). While TLM-treated individuals were significantly more often convicted of child sexual abuse, −TLM were more often convicted of rape/sexual assault (see ).
Table 2. Index offence, kind of former imprisonment, treatment status at the FTA and diagnoses according to ICD-10 of the treatment group with (+TLM; n = 54) and without TLM (−TLM; n = 79).
+TLM was over five years longer in prison or forensic psychiatry than − TLM, and correspondingly significantly older at the time of release (M = 48.1 vs. 42.4 years). At the time of release, +TLM had a Static-99R score almost one point higher, although they were significantly older (see ). Prior to release, with 64.8% (35 of 54) compared to 16.5% (13 of 79) significantly more TLM-treated individuals had been in forensic psychiatry, and still in treatment at the FTA at the cut-off date of December 19, 2019, were n = 30 (58.8%) of + TLM and n = 21 (26.2%) of − TLM (see ). With a mean difference of MDiff = 2.1 years, individuals released from forensic psychiatry received significantly longer follow-up treatment than those released from prison (n = 48, M = 4.9, SD = 2.5, range = 0.5–9.0 vs. n = 85, M = 2.8, SD = 1.9, range = 0.3–7.6; t[131] = −5.527, p < 001). More individuals released from forensic psychiatry than those released from prison were treated with TLM (see ).
TLM-treated individuals have been diagnosed with a paraphilic disorder significantly more often (92.6% vs. 45.6%, see ). A paedophilic disorder was diagnosed most frequently. A similar picture emerges when sadistic disorders are considered, albeit with far lower case numbers and therefore not meaningfully assessable.
No significant difference was observed in terms of personality disorders, the most frequently diagnosed comorbid disorder, or regarding intellectual disability.
Recidivism rates
Recidivism rate for general recidivism was significantly lower in + TLM (see ). There was no significant difference regarding serious recidivism. When considering re-offences of violent and sexual offences, there was a significant difference for violent, but not for sexual re-offences. As expected, the number of serious and sexual recidivism was generally low, 25% of cells having a frequency <5.
Table 3. Recidivism rates of the treatment group with TLM (+TLM; n = 54) and without TLM (−TLM; n = 79).
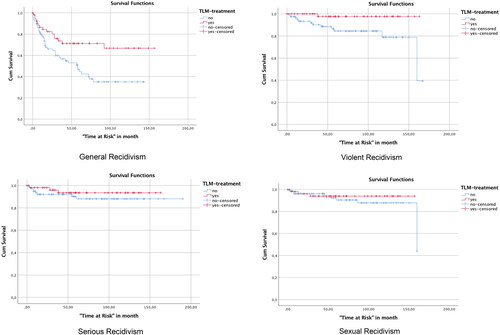
Calculation of survival time analysis showed that + TLM spent significantly longer time in freedom without re-offending than − TLM, with an estimated survival time of M = 113.6 months (SE = 9.4, 95%-CI = 95.2–132.0 vs. −TLM: M = 69.4, SE = 7.3, 95%-CI = 55.0–83.8; Log Rank Test: χ2(1,133)=7.393, p=.007, see ). Same applied to violent recidivism data, with + TLM spending on average M = 160.0 months (SE = 2.9, 95%-CI = 154.3–165.8) and − TLM M = 140.0 months in freedom (SE = 6.8, 95%-CI = 126.7–153.3; Log Rank Test: χ2(1,133)=6.207, p=.013). With regard to serious recidivism no such effect could be demonstrated (+TLM: M = 154.0 months, SE = 5.0, 95%-CI = 144.1–163.9; −TLM: M = 170.3, SE = 6.6, 95%-CI = 157.3–183.2; Log Rank Test: χ2(1,133)=0.812, p=.368). Since, in addition to the low number of cases, the preconditions necessary to conduct this analysis were not fulfilled for sexual recidivism, it was not possible to perform a valid calculation (see crossing curves in ).
Figure 1. Kaplan-Meier curves of the + TLM (n = 54) and the − TLM (n = 79) regarding different forms of recidivism.
Regarding the calculation of the Cox-regression on the prediction of general recidivism with TLM-treatment as a time-dependent covariate and controlled for the initial risk measured by Static-99R, there was a significant effect for both, time during TLM-treatment and Static-99R-score. Thus, across all individuals the probability of recidivism decreased during TLM-treatment and increased with higher Static-99R-scores (see ).
Table 4. Cox-regression on the prediction of general recidivism with TLM- treatment as time-dependent covariate, controlled for Initial risk at the time of release measured by static-99R for the + TLM (n = 54) and the − TLM (n = 79).
Recidivism rate of those who stopped TLM-treatment in the outpatient setting was 31.6% (6 of 19). This was higher than the recidivism rate of those treated with TLM (25.7%, 9 of 35; χ2(1,54) = 0.211, φ = .09, p = .753), but below − TLM (51.9%, 41 of 79; χ2(1,98) = 2.534, φ = .16, p = .131). However, the differences were not significant.
For post hoc identification of indicators for or against re-offending after stopping TLM-treatment, those who recidivated were compared with those who did not (see ). Those who recidivated after treatment-dropout showed more than twice as many previous convictions. In addition, their Static-99R-score of 5.7 points was in the high-risk category and on average 2.3 points higher than scores of non-recidivists, although this result did not reach significance level (p = .055).
Table 5. Differences between individuals who stopped TLM-treatment and recidivated (treatment withdrawal-recidivism, TWR; n = 13) and individuals who stopped TLM-treatment and did not recidivate (treatment withdrawal-no recidivism, TWnR; n = 6) TLM-treatment.
Discussion
Within the present retrospective study, it was possible for the first time, to compare officially registered recidivism rates of a large sample of high-risk offenders treated with TLM with a sample of high-risk offenders treated with psychotherapy only. Despite a higher initial risk, +TLM recidivated significantly less often and later than − TLM. TLM was associated with lower rates of recidivism compared to the psychotherapy only group after controlling for Static-99R. Higher scores on Static-99R continued to predict recidivism after controlling for TLM-status.
Considering criminal history, TLM-treated individuals showed significantly more sexual offences and the length of imprisonment was on average almost six years longer. According to the legal procedure it can therefore be assumed that + TLM had committed more serious offences than − TLM. In addition, noting that + TLM had a significantly higher Static-99R-score at the time of release—despite their significantly higher age—they showed a higher initial risk. Other than provided in the guidelines for the pharmacological treatment of paraphilic disorders (Thibaut et al. Citation2020), four individuals (7.4%) were treated without paraphilic disorder. The estimated recidivism risk may have been the decisive factor and/or the purpose of administering the medication was to treat hypersexuality (Briken and Turner Citation2021).
Overall + TLM showed lower recidivism rates than − TLM. After a time at risk of about six years, general recidivism of + TLM was 27.8%. This is well below the 40% nationwide recidivism rate of all individuals who offended sexually in Germany at nearly the same point in time (Jehle et al. Citation2013), and nearly like the recidivism rate in the retrospective observational study without comparison group conducted in Denmark and Greenland last year (30.6%) (Colstrup et al. Citation2020). In contrast, the comparison group had a substantially higher general recidivism rate of 51.9%. While in + TLM only one person had committed a new violent offence (1.9%), violent recidivism rate in − TLM was 15.2%. The finding of fewer violent offences among individuals treated with GnRH-agonists was already shown with very similar figures in the study by Gallo and colleagues (Gallo et al. Citation2019) with 4.0% (1 of 25) versus 18.2% (4 of 22). Regarding sexual recidivism, +TLM showed lower, but not significantly lower, rates than those treated with psychotherapy only (5.6% vs. 10.1%). This could be due to the generally low base-rates, but it can be noted that the rate of the TLM-treated group documented in this study is rather at the lower end of the nationally and internationally reported sexual recidivism rates. In a nationwide study (n = 6,826) after six years the rate was 5% for those who had previously committed a sexually violent offence, and 7% for those who had committed sexual abuse of children (Jehle et al. Citation2013). In Austria, after a five-year follow-up it was 6% for rather high-risk-sample similar to the one used here (Rettenberger et al. Citation2015). And contrary to the nonmedicated comparison group, +TLM was below the internationally measured 10% recidivism rate (Hanson and Bussière Citation1998; Harris and Hanson Citation2004; Soothill Citation2010).
The estimated overall survival time of + TLM with 9.5 years was significantly higher than those of − TLM with 5.8. Thus, TLM-treated individuals not only recidivated significantly less often but also later. Contrary to what was initially expected, TLM not only affects sex drive but appears to improve overall self-regulation abilities (Sauter et al. Citation2021). This could explain why there is such a significant group difference regarding general and violent recidivism, which frequently occurs impulsively. While medication can reduce general sexual urges and sexual fantasies, current research indicates that paraphilic content does not change (Schober et al. Citation2005; Sauter et al. Citation2021). Perhaps because of this, sexual recidivism did not differ between the two study groups or from the nationwide average. As explained in detail above, it should be noted that the study group comprises a group of high-risk offenders. As such, a reduction of the recidivism risk to the average level can certainly be seen as a positive result.
The increased likelihood of recidivism among individuals who had stopped TLM shown in previous studies (Emory et al. Citation1992; Colstrup et al. Citation2020) was not observed in the present study. Although the recidivism rate was higher compared to those who continued treatment (31.6% vs. 27.8%), it was lower than in the comparison group (51.9%), with neither difference reaching statistical significance. Post hoc, it could be identified that those with significantly more previous convictions (average 8) as well as an above-average Static-99R-score of 5.7 recidivated after withdrawal. Previous studies could show that a high PCL-R-score, especially Factor-1-scores, can negatively influence the course of treatment (Sewall and Olver Citation2019; Sauter et al. Citation2021). Accordingly, experts recommended considering many other variables to continue medication in the presence of a PCL-R-score above 25 (Briken et al. Citation2018). To be able to better differentiate within the group of high-risk offenders, for whom such medication is administered in the first place, a high number of previous convictions as well as high values in Static-99R are particularly useful. Nevertheless, the results show that the majority of those who stopped TLM-treatment – all after long psychotherapeutic treatment and forensic rehabilitation – did not recidivate. After a thorough forensic assessment and under close, intense, and neat monitoring, considering well-established risk factors, withdrawal attempts could be possible and justifiable. Regarding the side effects of TLM and the associated ethical concerns, this could be a possible option. Based on the insufficient state of research, it seems understandable and comprehensible that in practice, although guidelines recommend a two-to-five-year treatment duration, hardly any withdrawal attempts are made (Voß et al. Citation2016; Sauter et al. Citation2018; Colstrup et al. Citation2020). If the patient stops TLM-treatment, he usually does so without the professional monitoring and risk-management that forensic outpatient follow-up can offer (Voß et al. Citation2016; Sauter et al. Citation2018). Future studies should focus more on potential indicators for or against withdrawal. In addition, it is not yet known how many and which individuals will stop TLM after legal control expires.
As with most studies on the effectiveness of TLM, the present design is no RCT. Nonetheless, the design implemented made it possible to refer to a fairly similar comparison group as well as to a nationwide survey covering almost the same time period (Jehle et al. Citation2013). Moreover, it should be noted that the Static-99R was only rated by the first author (McGrath et al. Citation2012). The criterion of recidivism used was new convictions, as this is known to be the most objective criterion. Since not all offences are reported or then investigated, and since some time passes between the commission of the offence and the conviction, it is possible that recidivism has been underestimated. It is an inherent necessity that the present sample is rather small, which limits the generalisability of the study. However, to date, it has not been possible to examine larger groups of TLM-treated individuals. Individuals who offended sexually recidivate less frequently but over a longer period (Hall Citation1995). With an average time at risk of more than six years, this was sufficiently considered. However, it must be critically noted that at the time of data collection, more than half of + TLM and about a quarter of − TLM were still in forensic treatment. Thus, it cannot be ruled out that the effects can partly be attributed to the current psychotherapeutic treatment and the control function associated with it. It would therefore be useful to re-examine this sample at a later point in time.
Overall, the results support the efficacy of TLM, particularly in the group of high-risk offenders diagnosed with a paedophilic disorder and deficits in (sexual) self-regulation.
Author contribution
Julia Sauter: Conceptualisation, Methodology, Writing – original draft preparation. Laura M. Lingenti: Data Curation, Writing – original draft preparation. Martin Rettenberger: Conceptualisation, Methodology, Supervision, Writing – Reviewing. Daniel Turner: Conceptualisation, Methodology, Supervision, Writing – Reviewing. Peer Briken: Writing – Reviewing. Tatjana Voß: Supervision, Editing.
Ethical approval statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
The data reported in this manuscript were collected as part of a larger project to evaluate the effectiveness of forensic outpatient clinics. The results of the data collection have not been published elsewhere. The study was not preregistered. The recruitment began before March 1, 2019.
Data availability
The data that support the findings of this study are available from the corresponding author, JS, upon reasonable request. The data are not publicly available due to restrictions as their containing information that could compromise the privacy of research participants.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ahn J, Shim G, Lee J, Lee J, Lee T, Roh I. 2013. Preliminary study of effect of leuprolide acetat treatment on sexual fantasy of sex offenders. Korean J Leg Med. 37(3):139–144. doi: 10.7580/kjlm.2013.37.3.139.
- Briken P, Boetticher A, Krueger RB, Kismödi E, Reed GM. 2019. Current legal situation for patients with paraphilic disorders and implications of the ICD-11 for paraphilic disorders in Germany. J Sexual Med. 16(10):1615–1622. doi: 10.1016/j.jsxm.2019.07.011.
- Briken P, Hill A, Berner W. 2003. Pharmacotherapy of paraphilia with long-acting agonists of luteinizing hormone-releasing hormone: a systematic review. J Clin Psychiatry. 64:890–897. https://www.psychiatrist.com/jcp/depression/sexual-dysfunction/pharmacotherapy-paraphilias-long-acting-agonists-luteinizing/.
- Briken P, Müller JL, Berner W, Bödeker R-H, Vollmann J, Kasperk C, Koller M. 2017. Vom Scheitern einer Studie in Maßregelvollzugskrankenhäusern. Klinische Prüfung zum additiven Effekt von Triptorelin auf die Wirksamkeit von Psychotherapie [Failure of a study in forensic psychiatric hospitals. Clinical trial to investigate the additive effect of triptorelin on the efficacy of psychotherapy]. Nervenarzt. 88(5):480–485. doi: 10.1007/s00115-017-0301-7.
- Briken P, Turner D, Thibaut F, Bradford J, Cosyns P, Tozdan S. 2018. Validation of the Change or Stop Testosterone-Lowering Medication (COSTLow) Scale using Delphi method among clinical experts. J Sex Martial Ther. 24:1– 25. doi: 10.1080/0092623X.2018.1491910.
- Briken P, Turner D. 2021. Pharmacotherapy for patients with compulsive sexual behavior disorder (CSBD). In: Balon R, Briken P, editors. Compulsive sexual behavior disorder: understanding, assessment, and treatment. Washington, DC: American Psychiatric Association Publishing. Chap. 7. pp. 95–108.
- Champeaux-Depond C, Weller J, Froelich S, Sartor A. 2021. Cyproterone acetate and meningioma: a nationwide-wide population based study. J Neurooncol. 151(2):331–338. doi: 10.1007/s11060-020-03672-9.
- Chan YH. 2004. Biostatistics 203. Survival analysis. Singapore Med J. 45(6):249–256.
- Colstrup H, Larsen ED, Mollerup S, Tarp H, Soelberg J, Rosthøj S. 2020. Long-term follow-up of 60 incarcerated male sexual offenders pharmacologically castrated with a combination of GnRH agonist and cyproterone acetate. J Forensic Psychiatry Psychol. 31(2):241–254. doi:10.1080/14789949.2020.1711957.
- Cooper AJ. 1981. A placebo-controlled trial of the antiandrogen cyproterone acetate in deviant hypersexuality. Compr Psychiatry. 22(5):458–465. doi:10.1016/0010-440X(81)90034-1.
- Eher R, Gnoth A, Birklbauer A, Pfäfflin F. 2007. Antiandrogene Medikation zur Senkung der Rückfälligkeit von Sexualstraftätern: ein kritischer Überblick [The effects of antiandrogenic medication on relapse rates of sex offenders: a review]. Recht & Psychiatrie. 25(3):103–111. Retrieved from https://psychiatrie-verlag.de/product/eher-r-gnoth-a-birklbauer-a-pfaefflin-f-antiandrogene-medikation-zur-senkung-der-rueckfaelligkeit-von-sexualstraftaetern-ein-kritischer-ueberblick-einzelartikel-aus-rp-3-2007/.
- Emory LE, Cole CM, Meyer WJ. III. 1992. The Texas experience with depo-Provera: 1980. J Offender Rehabil. 18(3–4):125–140. doi: 10.1300/J076v18n03_11.
- Fox J. 2002. Cox proportional-hazards regression for survival data. Appendix to An R and S-PLUS companion to applied regression. https://socialsciences.mcmaster.ca/jfox/Books/Companion-1E/appendix-cox-regression.pdf.
- Gallo A, Abracen J, Looman J, Jeglic E, Dickey R. 2019. The use of leuprolide acetat in the management of high-risk sex offenders. Sex Abuse. 31(8):930–951. doi: 10.1177/1079063218791176.
- Hall GCN. 1995. Sexual offender recidivism revisited: a meta-analysis of recent treatment studies. J Consult Clin Psychol. 63(5):802–809. https://psycnet.apa.org/buy/1996-93501-001. doi: 10.1037/0022-006x.63.5.802.
- Hanson RK, Bussière MT. 1998. Predicting relapse: a meta-analysis of sexual offender recidivism studies. J Consult Clin Psychol. 66(2):348–362. doi: 10.1037//0022-006x.66.2.348.
- Hanson RK, Harris AJR, Scott T-L, Helmus LM. 2007. Assessing the risk of sexual offenders on community supervision (User Report No. 2007-05). Ottawa: Public Safety and Emergency Preparedness Canada.
- Hanson RK, Thornton D. 2000. Improving risk assessments for sex offenders: a comparison of three actuarial scales. Law Hum Behav. 24(1):119–136. doi: 10.1023/A:1005482921333.
- Hare RD. 2003. Manual for the psychopathy checklist-revised. 2nd ed. Toronto: Multi Health Systems.
- Harris A, Phenix A, Thornton D, Hanson RK. 2003. STATIC-99: Coding rules revised–2003. Ottawa: Solicitor General.
- Harris AJR, Hanson RK. 2004. Sex offender recidivism: a simple question (User Report No. 2004-03). Ottawa: Public Safety and Emergency Preparedness Canada.
- Helmus LM, Thornton D, Hanson RK, Babchishin KM. 2012. Improving the pre- dictive accuracy of STATIC-99 and STATIC-2002 with older sex offenders: revised age weights. Sex Abuse. 24(1):64–101. doi: https://doi.org/10.1177/1079063211409951.
- Hill A, Briken P, Kraus C, Strohm K, Berner W. 2003. Differential pharmacological treatment of paraphilias and sex offenders. Int J Offender Ther Comp Criminol. 47(4):407–421. https://journals.sagepub.com/doi/pdf/?casa_token=hzn85Q34vxYAAAAA:g74nXHSkEKS1oIPvGvaQ32OhqsSItZQaPZ8cV515-l0HIOSL5DRfOkUE7ghKExqViWpwe7X37frH. doi: 10.1177/0306624X03253847.
- Jehle J-M, Albrecht H-J, Hohmann-Fricke S, Tetal C. 2013. Legalbewährung nach strafrechtlichen Sanktionen. Eine bundesweite Rückfalluntersuchung 2007 bis 2010 und 2004 bis 2010 [Legal probation after criminal penalties. A Nationwide Recidivism Survey 2007 to 2010 and 2004 to 2010]. Mönchengladbach: Forum Verlag Godesberg GmbH. https://www.bmj.de/SharedDocs/Archiv/Downloads/Legalbwaehrung_nach_strafrechtlichen_Sanktionen_2007_2010_u_2004_2010.pdf?__blob=publicationFile&v=3.
- Jordan K, Fromberger P, Laubinger H, Dechent P, Müller JL. 2014. Changed processing of visual sexual stimuli under GnRH-therapy – a single case study in pedophilia using eye tracking and fMRT. BMC Psychiatry. 14(1):142. doi: 10.1186/1471-244X-14-142.
- Khan O, Ferriter M, Huband N, Powney MJ, Dennis JA, Duggan C. 2015. Pharmacological interventions for those who have sexually offended or are at risk of offending (review). Cochrane Database Syst Rev. (2); Art. No: CD0079789. doi: 10.1002/14651858.CD007989.
- Koo KC, Ahn JH, Hong SJ, Lee JW, Chung BH. 2014. Effects of chemical castration on sex offenders in relation to the kinetics of serum testosterone recovery: implications for dosing schedule. J Sex Med. 11(5):1316–1324. doi: 10.1111/jsm.12492.
- Landgren V, Malki K, Bottai M, Arver S, Rahm C. 2020. Effect of gonadotropin-releasing hormone antagonist on risk of committing child sexual abuse in men with pedophilic disorder. A randomized clinical trial. JAMA Psychiatry. 77(9):897–905. doi: 10.1001/jamapsychiatry.2020.0440.
- Laschet U, Laschet L. 1967. Antiandrogentherapie der pathologisch gesteigerten und abartigen Sexualität des Mannes [Antiandrogen therapy of pathologically increased and abnormal sexuality of man]. Klin Wochenschr. 45(6):324–325. doi: 10.1007/BF01747114.
- Maletzky BM, Tolan A, McFarland B. 2006. The Oregon depo-Provera program: a five-year follow-up. Sex Abuse. 18(3):303–316. doi: 10.1007/s11194-006-9021-4.
- McGrath RJ, Lasher MP, Cumming GF. 2012. The Sex Offender Treatment Intervention and Progress Scale (SOTIPS) psychometric properties and incremental predictive validity with Static-99R. Sex Abuse. 24(5):431–458. doi: 10.1177/1079063211432474.
- Moulier V, Fonteille V, Pélégrini-Issac M, Cordier B, Baron-Laforêt S, Boriasse E, Durand E, Stoléru S. 2012. A pilot study of the effects of Gonadotropin-Releasing Hormone Agonist therapy on brain activation pattern in a man with pedophilia. Int J Offender Ther Comp Criminol. 56(1):50–60. doi: 10.1177/0306624X10392191.
- Phenix A, Helmus M, Hanson RK. 2016. STATIC-99R: evaluators’ Workbook–2016. Ottawa: Solicitor General.
- Rettenberger M, Briken P, Turner D, Eher R. 2015. Sexual offender recidivism among a population-based prison sample. Int J Offender Ther Comp Criminol. 59(4):424–444. doi: 10.1177/0306624X13516732.
- Rettenberger M, Haubner-MacLean T, Eher R. 2013. The contribution of age to the Static-99 risk assessment in a population-based prison sample of sexual offenders. Crim Justice Behav. 40(12):1413–1433. doi: 10.1177/0093854813492518.
- Rösler A, Witztum E. 1998. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 338(7):416–422. doi: 10.1056/NEJM199802123380702.
- Rösler A, Witztum E. 2000. Pharmacotherapy of paraphilias in the next millennium. Behav Sci Law. 18(1):43–56. doi: 10.1002/(SICI)1099-0798(200001/02)18:1<43::AID-BSL376>3.0.CO;2-8.
- Sauter * J, Stasch * J, Klemke K, Emmerling A, Voß T. 2018. Das Absetzen antiandrogener Medikation im ambulanten Setting. Fortsetzungsbericht über die Auslassversuche der Berliner Stichprobe [Discontinuing antiandrogenic treatment in a forensic outpatient setting. A follow-up report of withdrawal trials of a Berlin sample]. Forens Psychiatr Psychol Kriminol. 12(4):352–359. doi: 10.1007/s11757-018-0498-8.
- Sauter J, Turner D, Briken P, Rettenberger M. 2021. Testosterone-lowering medication and its association with recidivism risk in individuals convicted of sexual offenses. Sex Abuse. 33(4):475–500. doi: 10.1177/1079063220910723.
- Schmucker M, Lösel F. 2015. The effects of sexual offender treatment on recidivism: an international meta-analysis of sound quality evaluations. J Exp Criminol. 11(4):597–630. doi: 10.1007/s11292-015-9241-z.
- Schober JM, Kuhn PJ, Kovacs PG, Earle JH, Byrne PM, Fries RA. 2005. Leuprolide acetate suppresses pedophilic urges and arousability. Arch Sex Behav. 34(6):691–705. doi: 10.1007/s10508-005-7929-2.
- Sewall LA, Olver ME. 2019. Psychopathy and treatment outcome: results from a sexual violence reduction program. Personal Disord. 10(1):59–69. doi: 10.1037/per0000297.
- Soothill KL. 2010. Sex offender recidivism. Crime Justice. 39(1):145–211. https://www.jstor.org/stable/. doi: 10.1086/652385.
- Thibaut F, Cosyns P, Fedoroff JP, Briken P, Goethals K, Bradford JMW. 2020. The World Federation of Societies of Biological Psychiatry (WFSBP) 2020 guidelines for the pharmacological treatment of paraphilic disorders. World J Biol Psychiatry. 21(6):412–490. doi: 10.1080/15622975.2020.1744723.
- Turner D, Basdekis-Jozsa R, Briken P. 2013. Prescription of testosterone-lowering medications for sex offender treatment in German forensic-psychiatric institutions. J Sex Med. 10(2):570–578. doi: 10.1111/j.1743-6109.2012.02958.x.
- Voß T, Klemke K, Schneider-Njepel V, Kröber H-L. 2016. Wenn ja, wie lange? – Dauer antiandrogener Behandlung von Sexualstraftätern mit paraphilen Störungen: klinische Erfahrungen aus Auslassversuchen in der forensischen Nachsorgepraxis [When yes, for how long? – Duration of antiandrogenic treatment of sexual offenders with paraphilic disorders]. Forens Psychiatr Psychol Kriminol. 10(1):21–31. doi: 10.1007/s11757-015-0346-z.
- Ziegler A, Lange S, Bender R. 2007. Überlebenszeitanalyse: survival analysis: cox regression. Dtsch Med Wochenschr. 132(1):e42–e44. doi: 10.1055/s-2007-959039.
