ABSTRACT
Background: Music therapy, an innovative approach that has proven effectiveness in many medical conditions, seems beneficial also in managing surgical patients. The aim of this study is to evaluate its effects, under general anesthesia, on perioperative patient satisfaction, stress, pain, and awareness.
Methods: This is a prospective, randomized, double-blind study conducted in the operating theatre of visceral surgery at Sahloul Teaching Hospital over a period of 4 months. Patients aged more than 18 undergoing a scheduled surgery under general anesthesia were included. Patients undergoing urgent surgery or presenting hearing or cognitive disorders were excluded. Before induction, patients wore headphones linked to an MP3 player. They were randomly allocated into 2 groups: Group M (with music during surgery) and group C (without music). Hemodynamic parameters, quality of arousal, pain experienced, patient’s satisfaction, and awareness incidence during anesthesia were recorded.
Results: One hundred and forty patients were included and allocated into 2 groups that were comparable in demographic characteristics, surgical intervention type and anesthesia duration. Comparison of these two groups regarding the hemodynamic profile found more stability in group M for systolic arterial blood pressure. A calm recovery was more often noted in group M (77.1% versus 44%, p < 10–3). The average Visual Analog Scale (VAS) score was lower in the intervention group (33.8 ± 13.63 versus 45.1 ± 16.2; p < 10–3). The satisfaction rate was significantly higher among the experimental group (81.4% versus 51.4%; p < 10–3). The incidence of intraoperative awareness was higher in group C (8 cases versus 3 cases) but the difference was not statistically significant.
Conclusion: Music therapy is a non-pharmacological, inexpensive, and non-invasive technique that can significantly enhance patient satisfaction and decrease patients’ embarrassing experiences related to perioperative stress, pain, and awareness.
RESPONSIBLE EDITOR Amin Bredan, VIB Inflammation Research Center & Ghent University, Belgium, Belgium
1. Introduction
Music is very old, even older than language. Musical instruments carved in animal bones dating back over 40,000 years have been found, while the oldest evidence demonstrating verbal exchange between humans goes back only to 35,000 years [Citation1]. Areas for use of music have multiplied with the evolution of humans, including therapeutic use [Citation2–Citation4]. The advent of psychoanalysis in the 20th century fully gives music its therapeutic contribution as a non-pharmacological, inexpensive, and safe technique. This approach uses the relaxing properties of music to restore, maintain, or improve social, mental, and physical capacities of individuals [Citation2,Citation5]. The scientific basis of the effects of music therapy was the subject of several neurophysiology studies; the results of which established some evidence particularly on the effect of music on hormonal secretions and nociceptive reflexes [Citation2,Citation6].
Surgery and anesthesia are generally unpleasant experiences for patients and are the source of stress and anxiety that can hinder the desired therapeutic goal [Citation7,Citation8]. Several experimental studies have evaluated the effects of music therapy in improving the quality of perioperative care [Citation2,Citation5].
Despite the long history of beneficial use of music for therapeutic goals, this harmless tool is not yet well exploited in daily anesthesia practice, reflecting the lack of recommendations. This paradoxical situation justifies the need for further studies encouraging the clinical use of music therapy in this stressful field.
Furthermore, one of the frequent and serious mishaps of the perioperative period is awareness during general anesthesia, which could have a better outcome with music therapy.
The aim of this study is to evaluate the effects of music therapy under general anesthesia on patient satisfaction, anxiety levels, intraoperative awareness, and the intensity of pain during recovery from abdominal surgery.
2. Methods
After obtaining institutional ethic committee approval and patients’ informed consent, this prospective randomized double-blind study was conducted in the operating theatre of visceral surgery in Sahloul teaching hospital over a 4-month period (from 1 January to 30 April, 2016).
Considering the α risk to be 0.05, the power of the study 80%, the π2–10% and hoping an improvement of at least 30% in patient satisfaction, the minimum sample size was estimated at 92 patients, enrolled into 2 groups of 46 patients each. (The calculation of the sample was made online at: http://marne.u707.jussieu.fr/biostatgv/).
All patients scheduled for abdominal surgery, aged more than 18 years and who agreed to participate in the trial were included. Exclusion criteria were cognitive or psychiatric disorders, hearing-impairing diseases, and chronic treatment with analgesics.
Patients were randomized into two groups: an intervention group (group M) and a control group (group C). The patients operated on during even days were included in the experimental group while the patients operated during odd days were included in Group C. In the operating room, all patients had standard monitoring (electrocardiogram, noninvasive blood pressure, and pulse oximetry). All patients had a headphone linked to an MP3 player with different types of music samples to satisfy all tastes. Patient choice was respected in all cases. Instrumental music was chosen by the anesthesiologist involved in the study for patients who had no particular preference. Anesthesia induction was carried out by Fentanyl at the dose of 3 µ/kg, propofol titration, and eventually cisatracurium at a dose of 0.15 mg/kg if a tracheal intubation was considered. Anesthesia was maintained by isoflurane in a mixture of 50% oxygen and 50% air. Fentanyl and cisatracurium were reinjected depending on intervention duration and neuromuscular blockade monitoring.
The music was started immediately after anesthesia induction for group M patients and the volume was set at 65 decibels by a standard sound level meter, compatible with prolonged listening without hearing risk.
Music was maintained throughout the surgery until the end of the intervention. Anticipation of analgesia was made by 1 g of paracetamol and 20 mg of nefopam infusion 30 minutes before the end of the surgical procedure. After waking and tracheal extubation, patients were transferred to the post-anesthesia care unit.
We collected sociodemographic parameters, data related to surgery (type and duration of surgery) and hemodynamic parameters (heart rate, systolic, diastolic and mean arterial blood pressure) at the entrance to the operating room, immediately after induction of anesthesia and every 15 minutes until the end of the procedure. We also assessed the quality of awakening by Riker scale (Appendix) [Citation9], pain on waking by Visual Analogue Scale (VAS), patient satisfaction by EVAN-G scale [Citation10], and intraoperative awareness 24 hours after surgery.
The primary end point was patient satisfaction 24 hours after surgery. Secondary end points were intraoperative hemodynamic stability, intraoperative awareness, postoperative pain and anxiety.
Data were analyzed by IBM SPSS Statistics software. Categorical variables were investigated by Chi-square test and numerical variables were by ANOVA. The significance level was set at 0.05.
3. Results
In this study, 140 patients were included and assigned into two groups of 70 patients each. The comparison between the two groups regarding demographic characteristics and surgical interventions did not find statistically significant differences ().
Table 1. Comparison of group M and group C based on demographic parameters and surgical interventions characteristics.
The most frequently chosen music by our patients was Tunisian music (30 cases). Eastern and Western music were chosen by 25 and 11 patients, respectively. The anesthesiologist chose instrumental music for only 4 patients who had no preference.
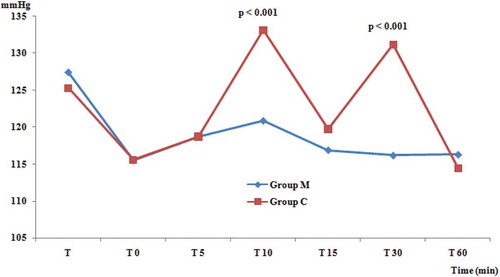
The comparison of the two groups regarding the hemodynamic profile found more stability in group M only for systolic arterial blood pressure, particularly at 10 and 30 minutes after anesthesia induction (). However, for the mean and diastolic arterial blood pressure, both groups were comparable.
Figure 1. Changes, in systolic arterial blood pressure, related to music therapy. Group M: music intervention; Group C: control group.
A calm recovery, defined as a Riker score <5, was noted in 60.7% of cases. It characterized mainly patients in group M (p < 10–3). The average VAS score for pain was lower in the intervention group (33.8 ± 13.63 versus 45.1 ± 16.15; p < 10–3). The satisfaction rate was significantly higher in group M (81.4% versus 51.4; p < 10–3). The incidence of intraoperative awareness was higher in group C (8 cases versus 3 cases) but the difference was not statistically significant ().
Table 2. Effects of music therapy on recovery quality, VAS during recovery, patient satisfaction and intraoperative awareness.
4. Discussion
Music is a very old therapeutic mean the effectiveness of which has been essentially proven in the treatment of physical and mental stress related to certain neuropsychiatric disorders [Citation2,Citation11,Citation12]. We tried in this study to evaluate its effects under general anesthesia on patient satisfaction, reduced anxiety levels, intraoperative awareness, and the intensity of pain during recovery from abdominal surgery.
Our results show a significant improvement in patient satisfaction in group M. Palmer et al. evaluated patient satisfaction with a five-item score. Although there was no significant difference for each item taken separately, the overall score was significantly higher in the intervention group than in the control group [Citation13]. Dubois et al. in a study published in CHEST in 1995 assessed the general anesthetic effect of music on the satisfaction of patients scheduled for bronchoscopy. An intervention group (21 patients) was compared to a control group (28 patients). Satisfaction was significantly greater in the intervention group (p = 0.02) [Citation14]. Similar results were found by Bechtold et al. in a study enrolling patients intended for colonoscopy under general anesthesia (85 patients treatment group versus 81 patients control group). The frequency of patients claiming music in subsequent colonoscopy was significantly higher in the intervention group (96.3% versus 56.1%; p < 0.0001) [Citation15]. In a meta-analysis published in 2009 on 8 randomized trials including 712 patients who underwent colonoscopy under general anesthesia with or without music therapy, satisfaction was significantly greater in the intervention group [Citation16].
Jayaraman et al. also confirmed the beneficial effects of music therapy on patient satisfaction. Music therapy improves satisfaction directly by its relaxing effect, and indirectly through its effects on other dissatisfaction factors such as perioperative pain and stress and postoperative nausea and vomiting. This effect is seen essentially when the music used is chosen by the patient [Citation17].
Another beneficial effect of music therapy was intraoperative hemodynamic stability evidenced by greater variation in systolic arterial blood pressure in Group C. Binns-Turner et al. demonstrated this effect on the hemodynamic profile especially for mean arterial blood pressure. As for heart rate, there was less acceleration in the intervention group but the difference was not statistically significant [Citation18]. In a study published in 2007, Jaber et al. found that music therapy provides a significant reduction in heart rate (88 ± 15 versus 82 ± 15 bpm, p < 0.05) and systolic arterial blood pressure (137 ± 17 versus 128 ± 14 mm Hg, p < 0.05) [Citation19]. Similar findings were reported by Mary Kay Williams in his Master’s thesis entitled ‘The effect of music therapy on anxiety for surgical patients’ [Citation20] and by Steelman VM et al. in an article published in 1990 [Citation21].
However, other studies have found different results with no hemodynamic changes [Citation22–Citation24]. The observed discrepancies are explained by the type of music used and the timing of its introduction. According to Binns-Turner et al., this beneficial effect is observed especially when patients are allowed to choose their music and when it is started from the preoperative period [Citation18]. The mechanism of action of music on the blood pressure profile could be modulation of the neurohormonal response [Citation6]. However, Wang et al. and Migneault et al. reviewed this neurohormonal impact related to intraoperative stress by repeated plasma levels of norepinephrine, epinephrine, cortisol, and ACTH without finding significant differences between the two groups [Citation23,Citation24].
In our study, the recovery quality was better in the intervention group, who showed a significant reduction in the level of stress and anxiety. Similar results have been published in the literature, although the tools used in the evaluation of this stress were very heterogeneous. Binns-Turner et al. showed a significant reduction of stress and anxiety in the music therapy group. An average decrease of ‘Spielberger State Anxiety Scale’ of 10.8 ± 7.7 in the intervention group versus an increase in the stress level of 11.6 ± 7.8 in the control group were found [Citation18].
Jaber et al. conducted a study enrolling 30 intensive care unit patients divided into two groups. The first group included 15 non-intubated patients without any neurological or respiratory distress criterion. The second group included 15 intubated patients during weaning from mechanical ventilation. The authors evaluated the effect of music therapy on agitation-sedation using Richmond scale (RASS −5 to +4). The RASS values decreased significantly in both groups under the effect of music therapy [Citation19]. Palmer et al. evaluated the effect of music therapy on perioperative anxiety in a study published in 2015 in the Journal of Clinical Oncology and involving women scheduled for diagnostic or therapeutic breast cancer surgery under general anesthesia. The patients were randomly assigned to three groups: a live music group (n = 69), a recorded music group (n = 70), and a control group (n = 68). The assessment of anxiety was made by ‘Global Anxiety – Visual Analogue Scale.’ The authors found a significant reduction in stress levels in both treatment groups [Citation13].
Wang et al. have confirmed this beneficial effect on stress and anxiety using the ‘State-Trait Anxiety Inventory’ [Citation23]. According to Palmer et al., perioperative anxiety is due to a conflict between a real event and a scheduled event that will activate the sympathetic nervous system to bring up the signs of anxiety. Intraoperative music therapy, when it is chosen by the patient, will act by modulation of this conflict, which will give a relaxation by activating the parasympathetic nervous system [Citation13].
Intraoperative music therapy also significantly reduced the pain intensity during recovery period. Binns-Turner et al. evaluated the VAS preoperatively and at discharge from the post-anesthesia care unit for all patients. Average VAS at discharge was significantly lower in the intervention group (41.5 ± 30.2 versus 64.9 ± 20.9; p = 0.007). Morphine consumption was lower in the intervention group but the difference was not significant (17.7 versus 22.1; p = 0.538) [Citation18]. Jayaraman et al. evaluated the analgesic effect of music therapy on 111 patients who underwent laparoscopic surgery for gallstones. Patients were randomly divided into two groups with or without music therapy. The intensity of pain measured by VAS was significantly higher in the control group [Citation17].
In 2001, Nilsson et al. published a paper about 90 women scheduled for hysterectomy under general anesthesia. These patients were assigned into three groups: two intraoperative music therapy groups and a control group. The authors concluded to a lesser analgesic consumption and a faster mobilization in both treatment groups [Citation25].
Ikonomidou et al., in a study published in 2004 and evaluating the effect of music on vital signs and postoperative pain, found that postoperative opioid use was significantly lower in the intervention group than in the control one [Citation26]. Similar results were also found by Tse et al. in a study enrolling patients scheduled for nasal surgery. An intervention group of 27 patients was compared to a control group of 30 patients. The level of pain assessed by VAS and analgesic consumption were significantly lower in the intervention group [Citation27].
This analgesic effect was also demonstrated in critically ill patients in the study published by Jaber et al. [Citation19]. The mechanism of action of music therapy on pain is multifactorial, involving attenuation of the conduction in the afferent fibers, mnemonic encoding, stimulation of endorphin production and action on psychomotility [Citation28].
The last point we examined in our study is the relationship between music therapy and intraoperative awareness. This complication of general anesthesia is common and serious in particular because of its psychological consequences such as post-traumatic stress disorder [Citation29]. Its incidence was less frequent in the intervention group but the difference was not significant. Several pharmacological and non-pharmacological means have been evaluated to prevent this complication. The most validated tool seems to be bispectral index monitoring (BIS) in order to ensure a level of hypnosis incompatible with auditory perception [Citation30].
Since 1994, Kiviniemi suggested music therapy under general anesthesia as a preventive measure because it can interfere with auditory stimuli [Citation29]. However, our research in Medline using keywords like ‘general anesthesia,’ ‘awareness’ and‘ music therapy’ did not find any results. So it appears that no studies have evaluated the effect of music therapy on intraoperative awareness. A larger study using BIS monitoring can be helpful to reaching clear conclusions. Even if the incidence cannot be changed by such intervention, the psychological impact is likely to be less important.
We also present the main results of a large meta-analysis recently published in Lancet. Seventy-three randomized controlled studies with samples ranging from 20 to 458 participants were included. Hole et al. found a significant reduction in post-operative pain, anxiety, and use of analgesics with significant improvement in overall patient satisfaction. According to the meta-analysis, these beneficial effects are present even under general anesthesia [Citation28].
We have to acknowledge that our study has some limitations that should be considered. Although most of our objectives have been analyzed in the literature, we are the first to study the relationship between awareness and music therapy during general anesthesia in this randomized, double-blind trial.
Indeed we only included patients operated in visceral surgery, which could impede the generalization of results. Moreover, hearing and cognitive disorders, which are among the exclusion criteria, were checked only by questionnaire with low sensitivity and specificity. Specialized ENT examination with audiometry and assessment of mental status by validated tests such as the Mini-Mental Scale Examination should be achieved for all patients. The absence of BIS monitoring is also an important limitation that could interfere with the use of anesthetics and the occurrence of intraoperative awareness with recall. Finally, the choice of music can also be criticized. Should we have chosen the same music for all the patients? Should we have used instrumental music rather than songs? Should we have excluded religious music especially as several papers point to a specific effect of religion? [Citation31]. Nevertheless, the free choice facilitated patient adhesion to our trial and the answer to all these questions requires a large study comparing various types of music.
5. Conclusion
Music therapy, an innovative approach that has proven effectiveness in many medical conditions, is beneficial also in managing surgical patients, even those operated under general anesthesia. This simple, non-pharmacological, inexpensive and noninvasive technique can significantly enhance patient satisfaction, and decrease the awkward experiences of patients related to perioperative stress, pain, and awareness. Most studies, some of which are of considerable scientific power, advocate for the implementation of intraoperative music therapy in the treatment protocols.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Conard NJ, Malina M, Münzel SC. New flutes document the earliest musical tradition in southwestern Germany. Nature. 2009;460(7256):1–6.
- Édith Lecourt. Découvrir la musicothérapie. Paris: Groupe Eyrolles; 2005.
- Conrad C. Music for healing: from magic to medicine. Lancet. 2010;376(9757):1980–1981.
- Davison JTR. Music in medicine. Lancet. 1899;154(3974):1159–1162.
- Emmanuel Bigand. Le Cerveau Mélomane. Ed Belin; 2013.
- Conrad C, Niess H, Jauch K-W, et al. Overture for growth hormone: requiem for interleukin-6? Crit Care Med. 2007;35(12):2709–2713.
- Iwasaki M, Edmondson M, Sakamoto A, et al. Anesthesia, surgical stress, and “long-term” outcomes. Acta Anaesthesiol Taiwan. 2015;53(3):99–104.
- Giannoudis PV, Dinopoulosa H, Chalidisa B, et al. Surgical stress response. Injury. 2006;37(5):S3–S9.
- Riker RR, Picard JT, Fraser GL. Prospective evaluation of the sedation-agitation scale for adult critically ill patients. Crit Care Med. 1999;27(7):1325–1329.
- Pernoud N, Bruder N, Simeoni MC, et al. Development and validation of a perioperative satisfaction questionnaire. Anesthesiology. 2005;102(6):1116–1123.
- Munro S, Mount B. Music therapy in palliative care. Can Med Assoc J. 1978;119(9):1029–1034.
- Cook JD. The therapeutic use of music: a literature review. Nurs Forum. 1981;20(3):252–266.
- Palmer JB, Lane D, Mayo D, et al. Effects of music therapy on anesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: a randomized controlled trial. J Clin Oncol. 2015;33(28):3162–3168.
- Dubois JM, Bartter T, Pratter MR. Music improves patient comfort level during outpatient bronchoscopy. Chest. 1995 Jul;108(1):129–130.
- Bechtold M-L, Perez R-A, Puli S-R, et al. Effect of music on patients undergoing outpatient colonoscopy. World J Gastroenterol. 2006;12(45):7309–7312.
- Bechtold ML, Puli SR, Othman MO, et al. Effect of music on patients undergoing colonoscopy: a meta-analysis of randomized controlled trials. Dig Dis Sci. 2009;54(1):19–24.
- Jayaraman L, S S, Sethi N, et al. Does intraoperative music therapy or positive therapeutic suggestions during general anesthesia affect the postoperative outcome ?. A double blind randomised controlled trial. Indian J Anaesth. 2006;50(4):258–261.
- Binns-Turner PG, Wilson LL, Pryor ER, et al. Perioperative music and its effects on anxiety, hemodynamics, and pain in women undergoing mastectomy. AANA J. 2011;79(4):21–27.
- Jaber S, Bahloul H, Guétin CG, et al. Effects of music therapy in intensive care unit without sedation in weaning patients versus non-ventilated patients. AFAR. 2007;26(1):30–38.
- Williams MK. The effects of music therapy on anxiety in surgical patients [Masters Theses]. 2000. Available from: http://scholarworks.gvsu.edu/theses.
- Steelman VM. Intraoperative music therapy. Effects on anxiety, blood pressure. AORN J. 1990;52(5):1026–1034.
- Patil Kalyani N, GhodkiPoonam G, ThombareShalini K. Impact of intraoperative music therapy on the anesthetic requirement and stress response in laparoscopic surgeries under general anesthesia. Ain-Shams J Anesthesiol. 2015;8:580–584.
- Wang S-M, Kulkarni L, Dolev J, et al. Music and preoperative anxiety: a randomized, controlled study. Anesth Analg. 2002;94(6):1489–1494.
- Migneault B, Girard F, Albert C, et al. The effect of music on the neurohormonal stress response to surgery under general anesthesia. Anesth Analg. 2004;98(2):527–532.
- Nilsson U, Rawal N, Unestahl LE, et al. Improved recovery after music and therapeutic suggestions during general anaesthesia: a double-blind randomised controlled trial. Acta Anaesthesiol Scand. 2001;45(7):812–817.
- Ikonomidou E, Rehnström A, Naesh O. Effect of music on vital signs and postoperative pain. AORN J. 2004;80(2):269–274, 277–278.
- Tse MM, Chan MF, Benzie IF. The effect of music therapy on postoperative pain, heart rate, systolic blood pressures and analgesic use following nasal surgery. J Pain Palliat Care Pharmacother. 2005;19(3):21–29.
- Hole J, Hirsch M, Ball E, et al. Music as an aid for postoperative recovery in adults: a systematic review and meta-analysis. Lancet. 2015;386(10004):1659–1671.
- Kiviniemi K. Conscious awareness and memory during general anesthesia. AANA J. 1994;62(5):441–449.
- Bruchas RR, Kent CD, Wilson HD, et al. Anesthesia awareness: narrative review of psychological sequelae, treatment, and incidence. J Clin Psychol Med Settings. 2011;18(3):257–267.
- Beiranvand S, Noparast M, Eslamizade N, et al. The effects of religion and spirituality on postoperative pain, hemodynamic functioning and anxiety after cesarean section. Acta Med Iran. 2014;52(12):909–915.
