ABSTRACT
Patients with end stage kidney disease (ESKD) with severely impaired cognitive function have no survival benefit from dialysis. We therefore undertook a survey to explore the renal physicians’ practices of withholding and withdrawal of dialysis treatment in vegetative state patients in the United Arab Emirates (UAE). A cross sectional survey of 29 nephrology practices in UAE exploring physicians’ practices in making decisions of withholding and withdrawal of dialysis treatment during provision end-of-life care for patients in persistent vegetative state (PVS).The majority of participants practice in governmental non-for-profit dialysis units (79%), and think they are well prepared to make decision with patients and family on issues of dialysis withdrawal and withholding (69%). If a chronic dialysis patient became permanently unconscious only few respondents (17%) indicated probability of stopping dialysis. On the other hand, more respondents (48%) reported that dialysis is likely to be withheld in PVS patients who develop kidney failure. In high risk or poor prognosis ESKD patients and given how likely they would consider each option independently, respondents reported they are likely to consider time-limited dialysis in 78% of the time followed by stopping (46%) or forgoing (27%) dialysis. Majority of the participants perceived that their decisions in providing renal care for PVS patients in UAE were influenced by the family sociocultural beliefs (76% of participants), the current hospital policies (72% of participants), and by Islamic beliefs (66% of participants). Only few perceived access to palliative care (30%) and treatment cost (17%) to have an impact on their decision making.Decisions of initiation and continuation of dialysis treatment to ESKD patients in PVS are prevalent among nephrology practices in UAE. Development of local guidelines based on the societal values along with early integration of palliative kidney failure management care would be required to improve the quality of provision of end-of-life renal care in UAE.
Abbreviations: ESKD: stage kidney disease; UAE: United Arab Emirates; PVS: persistent vegetative state; RPA: Renal Physicians Association; ASN: American Society of Nephrology; EMAN: Emirates Medical Association Nephrology Society; CPR: cardiopulmonary resuscitation.
1. Introduction
The number of patients with end stage kidney disease (ESKD) receiving dialysis treatment is increasing worldwide including United Arab Emirates (UAE) [Citation1,Citation2]. UAE recently expand its national dialysis service to meet the demand of increasing prevalence of chronic kidney diseases (CKDs). However, many patients with ESKD suffer from multiple comorbidities and have high symptom burdens [Citation3–Citation5]. The nephrologists would more often experience decisions of end-of-life renal care with or without dialysis treatment [Citation6–Citation8].
Therefore, nephrologists taking care of ESKD patients are encouraged to discuss prognosis and have an approach to advance care planning based on the patients and family expectations and the goals of dialysis treatment [Citation9–Citation11]. The aim is to provide the best possible patient care and to maintain quality of life. In this regard, the Renal Physicians Association (RPA) provided recommendations to facilitate the shared decision-making with patients and family in appropriateness of end-of-life renal care for patients with irreversible, profound neurologic impairment, and patients with no survival benefit from dialysis [Citation12].
Because of increased physicians’ awareness of end-of-life palliative renal care for ESKD patients, nowadays nephrologists are more likely to withdraw patients in persistent vegetative state (PVS) from dialysis and less likely to initiate PVS patients on chronic dialysis [Citation13]. Patients in a PVS have very little prospect of recovery are completely unaware of self and environment, and their quality of life considered to be worse than death [Citation14]. Nevertheless, a recent report highlighted, an increase in number of patients in PVS receiving regular dialysis treatment in UAE [Citation15].
Deciding to continue or stop dialysis when the patient no longer possesses the capacity to make decisions is particularly challenging for nephrologists, because the patients’ sociocultural and religious beliefs would shape the decision-making process and provision of end-of-life care [Citation16–Citation20]. Health care policies, available resources, and societal consensus on the management approach would also impact on the clinical decisions of withdrawing or withholding treatment for severely sick patients [Citation8,Citation21–Citation24]. We therefore undertook this survey to explore the renal physicians’ practices of withholding and withdrawal of dialysis treatment during provision of renal care at end-of-life for patients with ESKD in UAE.
2. Methods
This is a cross-sectional study based on an electronic survey of renal physicians practicing in UAE. A 29-item self-administered questionnaire was designed to determine the renal physicians’ practices during making decisions of withdrawal and withholding of dialysis treatment (21 questions) during provision of end-of-life renal care to patients in PVS (see Appendix). The other eight questions were used to identify the characteristics of the study participants. The themes of the questions were based on the clinical guidelines of Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis by the RPA and the American Society of Nephrology (ASN) in 2000. The questionnaire was reviewed by four nephrologists at the College of Medicine and Health Sciences, UAE University (UAEU) and Tawam Hospital, Abu Dhabi, UAE to assess face validity of the survey items and to provide feedback on the clarity and consistency of the questionnaire. We then distributed the questionnaire using an online survey program that allows respondents to answer the questions but does not allow duplicate responses. The link to the survey, along with a cover letter, was e-mailed to a test group of two nephrologists, and no problems were identified and therefore no changes were made to the questionnaire. The link to the online survey and the cover letter were then sent on 10 May 2015 by Emirates Medical Association Nephrology Society (EMAN) through e-mail to the society members and participation was voluntary. In June 2015 in the annual meeting of EMAN the members were reminded to participate in the online survey. Three subsequent email reminders were sent. The responses were anonymous and no identifying data were collected.
The survey first page contained information on the rationale of the study and statements ensuring the confidentiality of respondents. The participants were given the choice to decline or to proceed to answer the survey questions. The survey questions allow for no response as an option for every question, and the participants can stop participation at any time. Participants were restricted to those caring for dialysis patients in various settings, including for profit and nonprofit dialysis units in private and governmental hospitals. Completion of the survey signified informed consent. The Human Ethical Committee at Al Ain district, United Arab Emirates University approved this study (Protocol No.14/02-CRD 298/13).
Responses were collected from 10 May 2015 to 19 May 2016. A total of 29 nephrologists taking care of dialysis patients completed the online survey.
3. Statistical analysis
We summarized the questionnaire responses using descriptive statistics. The proportions were calculated based on the total number of respondents for each question. Chi-square test was used to assess the independence of categorical variables, as appropriate. All variables with a value of p < 0.1 in the univariate analysis were entered into a stepwise multiple regression analysis. Analyses were performed using SPSS version 18.0 (IBM Inc., Chicago, IL) and p values <0.05 were considered statistically significant.
4. Results
The survey was completed by 29 nephrologists taking care of patients with ESKD in UAE. From the data obtained from licensing authorities (Ministry of Health, Dubai Health Authority and Health Authority – Abu Dhabi) about licensed nephrologists and dialysis centers and from communications with nephrologists we were able to estimate a total number of 60 nephrologists in the country would be involved in taking care of dialysis patients in UAE and could have received the email invitation for participation in the study. This would give a response rate of at least 48%.
Twenty-three (79%) of the 29 respondents were practicing in governmental non-for-profit dialysis units, 25 (86%) were practicing medicine for more than 10 years, and 20 (69%) perceived to be well prepared to discuss with patients and families’ decisions to continue, withdraw, and withhold dialysis treatment, and 7 (24%) experienced dialysis withdrawal in prior 12-months (). Only 2 (7%) respondents confirmed the existence of written policy on dialysis withdrawal in their practices, and the majority (n = 23, 79%) have to perform cardiopulmonary resuscitation (CPR) on all patients who have a cardiac arrest in the dialysis unit regardless of age, comorbidity, and preferences.
Table 1. Demographics and characteristics of dialysis practices of 29 renal physicians who completed the survey.
The responses, to a hypothetical scenario of what will happen in their practice if one of their chronic dialysis patients progresses into unconscious state (PVS), were to continue dialysis treatment (n = 24, 82.8%) except a few (n = 5, 17.2%) of respondents who anticipated a dialysis withdrawal probably will happen. The probability of a decision to withhold dialysis treatment from a known PVS who developed severe kidney failure was only for 48% of the respondents.
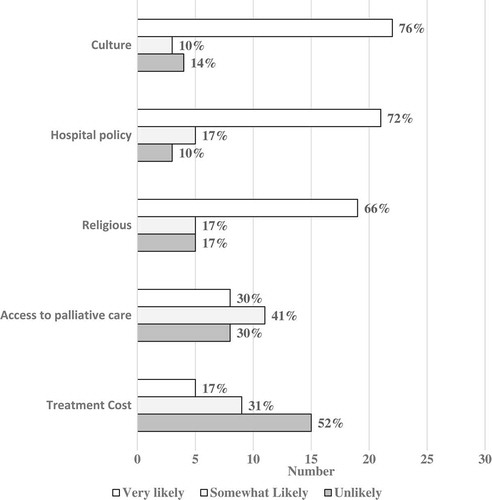
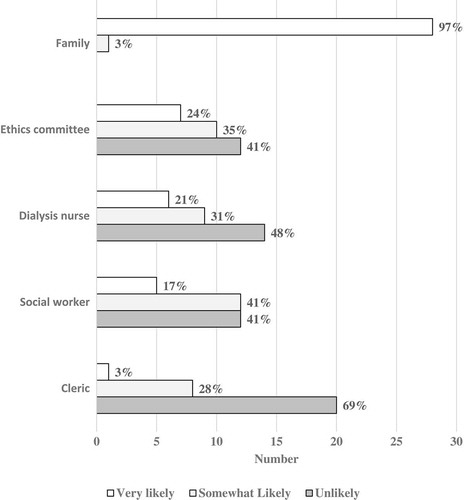
Ninety-six percent of respondents consult the family members () during the decision-making process regarding provision of end-of-life renal care to PVS patients. The dialysis nurses (21%), social workers (17%), and ethical committee (24%) were less likely to be consulted during the decision process.
Figure 1. Parties which renal physicians in UAE consult when making treatment decisions for ESKD patients in persistent vegetative state.
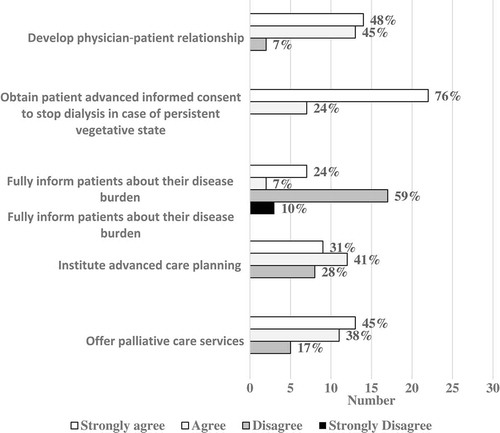
Most of the respondents (n = 27, 93%) agreed that in their practices, a physician–patient relationship is developed for shared decision-making (). For patients suffering from their disease burden, the majority of respondents reported that they fully inform patients about diagnosis, prognosis, and treatment options (n = 22, 76%), and offer palliative care (n = 25, 83%). In addition, most respondents institute an advanced care plan (n = 21, 72%) for these high-risk patients. Nevertheless, only few (n = 9, 31%) indicated an informed consent to stop dialysis treatment is likely to be obtained in advance.
Figure 2. Characteristics of the renal physicians shared decision-making process in the care of patients with ESKD.
shows that few respondents reported a very likely practice of considering forgoing (n = 5, 19%) or stopping dialysis (n = 7, 25%) for kidney failure patients with very poor prognosis or for whom dialysis cannot be provided safely.
Figure 3. Management of ESKD patients with very poor prognosis or for whom dialysis cannot be provided safely.
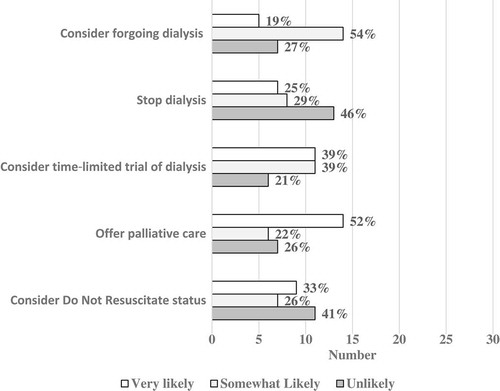
Majority of the respondents perceived the impact of the cultural and religious factors as well as the local hospital policies (76%, 66%, and 72%, respectively, ) to be very likely influencing factors on the clinical decision-making process during provision end-of-life renal care. Less than one-third of respondents perceived a significant impact of the treatment cost and access to palliative during the decisions-making process for provision end-of-life renal care.
5. Discussion
Health-care providers need to help minimize patients’ suffering and maximize comfort by offering appropriate and best medical care. The main long-term goal of dialysis treatment is to allow patient’s interaction with the world. Thus, provision of regular dialysis treatment to patients in permanent vegetative state who are unaware of self and the surrounding is considered inappropriate [Citation8,Citation20]. When physicians are certain that the dialysis treatment is unlikely to improve the condition or the quality of life, the widely accepted ethical decision is to initiate process of withholding or withdrawing dialysis treatment to relief the patients from the burden of the symptom and the unnecessary dialysis treatment [Citation8,Citation25,Citation26]. .
Nephrologists in UAE practice shared decision-making process and they almost always consult the family members during provision of end-of-life renal care to patients with ESKD. In UAE, as in other Arab Gulf countries, health-related decisions are shared family affair and the family members are the provider of the social and spiritual supportive care for the sick family member [Citation27,Citation28]. As such the family members are the primary decision makers for their very sick patients [Citation19,Citation29].
The high frequency of clinical decisions for providing dialysis treatment for kidney failure patients in PVS in UAE is perceived to be due to prevalent sociocultural beliefs. In the Gulf Arab region, the family members often need to be reassured that their sick family members are receiving the best medical care [Citation30]. The cultural value of hope, and not losing faith in cure might have driven the UAE family members to resist active withdrawal of a life supportive dialysis treatment and to insist in providing full medical support to their sick patients [Citation19,Citation31]. Furthermore, in situations with limited renal physician patient relationship, and because of fear of legal repercussions, renal physicians might avoid discussions of forgoing dialysis treatment. The former federal medical liability law (No. 10 of 2008) prohibited physicians from refraining to treat patients or discontinue the treatment even upon the request of the family members. Based on this law, the renal physicians perform CPR on all dialysis patients irrespective of age and comorbidity.
Nevertheless, the study participants perceived that their practices are more likely to withhold (48%), than stop (17%) dialysis treatment from PVS patients. It was reported elsewhere that physicians in UAE as well as in other countries have more comfort with withholding than with withdrawal of a life-supporting treatment in terminally ill patients [Citation28,Citation32,Citation33]. This could be also related to the difficulty in initiating discussions of withdrawal decisions, lack of hospital policies, and the fear of inducing premature death [Citation18,Citation22].
In our study, the majority of participating nephrologists reported that they fully inform high-risk patients on their prognosis and offer them palliative care; however, it is less likely to obtain an advanced informed consent to stop dialysis in case of deterioration. ESKD patients have multiple comorbidities and low survival rate, thus advance care planning would facilitate physicians’ decisions in provision of end-of-life renal care [Citation6]. Advance care planning services are not available officially and it is culturally challenging to integrate the concept of advanced care planning in the clinical practice in UAE [Citation28]. In addition, more involvement of other important health-care providers, nurses, and social workers in shared clinical decision process along with multiple conversations with the family members, would facilitate incorporation of conservative CKD care, and educate the patients’ family regarding the best appropriate medical care for their sick family member [Citation11,Citation34]. Under adequate palliative care and provision of CKD care other than dialysis, most uremic symptoms can be controlled to an acceptable level and dialysis treatment might need to be provided only in rare occasions of pulmonary edema [Citation35].
Health-care providers have professional responsibility to exercise clinical judgement and guide the family in decision-making by offering medically indicated options that offer a realistic clinical benefit to the patients [Citation8,Citation11]. The new medical liability law (Law No.4 of 2016) published in 15 August 2016, permits health care professionals to refrain from performing CPR on terminally ill or dying patients who are sufferings from incurable illnesses (Federal Law on Medical Liability (Law No. 4 of 2016)). Thus, clear health care policies and guidance are of paramount importance in shaping the decision-making process on appropriateness of dialysis treatment [Citation13]. Integration of conservative palliative care within the management plan of ESKD patients with multiple comorbidities as well as honoring a do-not-resuscitate orders facilitate clinical decisions for quality of end-of-life renal care [Citation11,Citation36,Citation37].
Limitations of our study include a small sample size constrained to renal physicians in UAE; thus, the results may not be generalizable to other neighboring countries because of possible difference in health care systems and resources [Citation38]. Despite vigorous efforts to generate a robust physician response rate, the nonresponse bias is a concern. It is possible that physicians with a heavy workload may not have had the time to complete the survey, as other similar international studies used online survey reported a low response rate of 8–13% [Citation13,Citation21,Citation23]. The low response rate could result in overestimation or underestimation of physician practices. However, the distribution of respondents across the country dialysis units would reflect the practices cross the UAE, and thus the nonresponse is most likely random. The other study limitation is the fact that the survey addresses reported rather than actual observed practices. The extent to which physicians would behave in the way they reported is open to question. Despite these limitations, the study provides crucial information about the provision of renal care at end-of-life, which might be considered to be inappropriate as it does not provide meaningful life quality. A thorough assessment of practices and policies for provision of renal care for terminally ill patients in UAE is needed.
6. Conclusions
Nephrologist practicing in UAE reported high frequency of clinical decisions that opt for provision of dialysis treatment to patients in PVS with kidney failure. A culturally sensitive clinical practice guideline is warranted to support the nephrologist in decision-making process about appropriateness of dialysis treatment for terminal renal care. Sociocultural and religious beliefs and hospital policies are major influencing factors during clinical decision-making process during provision of terminal CKD care. Future studies should examine the barriers to conservative management approach for terminal renal care in the UAE.
Recommendations
To develop a UAE clinical practice guidelines for shared decision-making for end-of-life renal care that account to patient’s family perspective in health decisions for critically ill patients.
To adopt principles for sound decision-making in process of withholding or withdrawing dialysis that is acceptable by health-care providers, patients, and their families in the UAE.
To facilitate early introduction of conservative CKD care by involving other CKD health care members and palliative care specialty during clinical decision-making process.
Ethics approval and consent to participate
The participants were given the choice to decline or to proceed to answer the survey questions and completion of the survey indicated informed consent.
Consent for publication
Completion of survey implied informed consent for publication of anonymous individual and aggregate data. All participants were adults.
Availability of data and material
No additional data are available
Authors’ Contribution
AC and OB designed the study. FA and OB analyzed the data and drafted the manuscript. MA and BB contributed to the design of the study and drafting of the manuscript. The manuscript was reviewed by all coauthors for comments and all authors approved this version and agree to be accountable for all aspects of the work ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Additional information
Funding
References
- Collins AJ, Foley RN, Herzog C, et al. US Renal Data System 2012 Annual Data Report. Am J Kidney Dis. 2013;61(1Suppl 1):1–8.
- Hassanien AA, Al-Shaikh F, Vamos EP, et al. Epidemiology of end-stage renal disease in the countries of the Gulf Cooperation Council: a systematic review. JRSM Short Rep. 2012;3(6):38.
- Ng YY, Hung YN, Wu SC, et al. Progression in comorbidity before hemodialysis initiation is a valuable predictor of survival in incident patients. Nephrol Dial Transplant. 2013;28(4):1005–1012.
- Neu S, Kjellstrand CM. Stopping long-term dialysis. An empirical study of withdrawal of life-supporting treatment. N Engl J Med. 1986;314(1):14–20.
- Findlay MD, Donaldson K, Doyle A, et al. Factors influencing withdrawal from dialysis: a national registry study. Nephrol Dial Transplant. 2016.
- Wong SP, Kreuter W, O’Hare AM. Treatment intensity at the end of life in older adults receiving long-term dialysis. Arch Intern Med. 2012;172(8): 661–663. discussion 663–664.
- Lyngaa T, Christiansen CF, Nielsen H, et al. Intensive care at the end of life in patients dying due to non-cancer chronic diseases versus cancer: a nationwide study in Denmark. Crit Care. 2015;19:413.
- Skold A, Lesandrini J, Gorbatkin S. Ethics and health policy of dialyzing a patient in a persistent vegetative state. Clin journal Am Soc Nephrol. 2014;9(2):366–370.
- Couchoud CG, Beuscart JB, Aldigier JC, et al. Development of a risk stratification algorithm to improve patient-centered care and decision making for incident elderly patients with end-stage renal disease. Kidney Int. 2015;88(5):1178–1186.
- Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin journal Am Soc Nephrol. 2010;5(2):195–204.
- Rosansky SJ, Schell J, Shega J, et al. Treatment decisions for older adults with advanced chronic kidney disease. BMC Nephrology. 2017;18(1):200.
- Galla JH. Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. J Am Soc Nephrol. 2000;11(7):1340–1342.
- Holley JL, Davison SN, Moss AH. Nephrologists’ changing practices in reported end-of-life decision-making. Clin journal Am Soc Nephrol. 2007;2(1):107–111.
- Gray K, Knickman TA, Wegner DM. More dead than dead: perceptions of persons in the persistent vegetative state. Cognition. 2011;121(2):275–280.
- Chaaban A, Ahmed M, Budruddin M, et al. continuation or withdrawal of dialysis in patients who developed vegetative state (vs): an ethical, legal and professional dilemma. Am J Kidney Dis. 2014;63(5):A1–A121.
- Lai CF, Tsai HB, Hsu SH, et al. Withdrawal from long-term hemodialysis in patients with end-stage renal disease in Taiwan. J Formos Med Assoc. 2013;112(10):589–599.
- Davison SN, Holley JL. Ethical issues in the care of vulnerable chronic kidney disease patients: the elderly, cognitively impaired, and those from different cultural backgrounds. Adv Chronic Kidney Dis. 2008;15(2):177–185.
- Bulow HH, Sprung CL, Reinhart K, et al. The world’s major religions’ points of view on end-of-life decisions in the intensive care unit. Intensive Care Med. 2008;34(3):423–430.
- Mobeireek AF, Al-Kassimi F, Al-Zahrani K, et al. Information disclosure and decision-making: the Middle East versus the Far East and the West. J Med Ethics. 2008;34(4):225–229.
- Manalo MFC. End-of-Life Decisions about Withholding or Withdrawing Therapy: Medical, ethical, and Religio-cultural considerations. Palliat care. 2013;7:1.
- Bito S, Asai A. Attitudes and behaviors of Japanese physicians concerning withholding and withdrawal of life-sustaining treatment for end-of-life patients: results from an Internet survey. BMC Med Ethics. 2007;8:7.
- Sprung CL, Maia P, Bulow HH, et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med. 2007;33(10):1732–1739.
- Kuehlmeyer K, Palmour N, Riopelle RJ, et al. Physicians’ attitudes toward medical and ethical challenges for patients in the vegetative state: comparing Canadian and German perspectives in a vignette survey. BMC Neurol. 2014;14(1):1–9.
- Yaguchi A, Truog RD, Curtis JR, et al. International differences in end-of-life attitudes in the intensive care unit: results of a survey. Arch Intern Med. 2005;165(17):1970–1975.
- Al-Bar MA, Chamsi-Pasha H. Contemporary bioethics: Islamic perspective. Cham, Switzerland: Springer Open; 2015.
- Sachedina A. End-of-life: the Islamic view. Lancet. 2005;366(9487):774–779.
- Wehbe-Alamah H. Bridging generic and professional care practices for Muslim patients through use of Leininger’s culture care modes. Contemp Nurse. 2008;28(1–2):83–97.
- Masood UR, Said A, Faris C, et al. Limiting intensive care therapy in dying critically Ill patients: Experience from a tertiary care center in United Arab Emirates. Int J Crit Illn Inj Sci. 2013;3(3):200–205.
- Asadi-Lari M, Madjd Z, Goushegir S. Gaps in the provision of spiritual care for terminally ill patients in Islamic societies—a systematic review. Adv Palliat Med. 2008;7(2):73–80.
- Al-Mutair AS, Plummer V, Clerehan R, et al. Needs and experiences of intensive care patients’ families: a Saudi qualitative study. Nurs Crit Care. 2014;19(3):135–144.
- Nasir LS, Abdul-Haq AK. Caring for Arab patients: a biopsychosocial approach. Oxford, UK: Radcliffe Publishing; 2008.
- Wenger NS, Lynn J, Oye RK, et al. Withholding versus withdrawing life-sustaining treatment: patient factors and documentation associated with dialysis decisions. J Am Geriatr Soc. 2000;48(5 Suppl):S75–83.
- Lazenby S, Edwards A, Samuriwo R, et al. End-of-life care decisions for haemodialysis patients - ‘We only tend to have that discussion with them when they start deteriorating’. Health expect. 2017;20(2):260–273.
- Puntillo KA, McAdam JL. Communication between physicians and nurses as a target for improving end-of-life care in the intensive care unit: challenges and opportunities for moving forward. Crit Care Med. 2006;34(11 Suppl):S332–340.
- Luckett T, Sellars M, Tieman J, et al. Advance care planning for adults with CKD: a systematic integrative review. Am J Kidney Dis. 2014;63(5):761–770.
- Morton RL, Kurella Tamura M, Coast J, et al. Supportive Care: Economic Considerations in Advanced Kidney Disease. Clin journal Am Soc Nephrol. 2016.
- Chandna SM, Da Silva-Gane M, Marshall C, et al. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant. 2011;26(5):1608–1614.
- Abudari G, Hazeim H, Ginete G. Caring for terminally ill Muslim patients: Lived experiences of non-Muslim nurses. Palliat Support Care. 2016;14(6):1–13.
Appendix
The Questionnaire items for appropriateness of withholding and withdrawal of dialysis treatment
Responses are reported as very likely/somehow likely/unlikely OR when appropriate the responses reported as strongly agree/agree/don’t agree/strongly do not agree.
In the last 12 months, how many of the patients for whom you are responsible to care had dialysis stopped either because of personal choice or a physician/family decision to stop?
In your institution, if one of your dialysis patients became permanently unconscious person (persistent vegetative state, PVS). What would usually happen?
In making the decision in the above question; please indicate how likely you would be to consult with each of the following: patient’s family/dialysis unit nurses/social workers /ethics committee/religious man (Sheikh)
If family asked not to stop dialysis, how would you usually handle the request?
If you were requested to begin dialysis of a permanently unconscious patient (persistent vegetative state), what would you usually do?
In the dialysis unit in which you have the most patients, is there a written unit policy on withdrawal of dialysis?
In the dialysis unit in which you have the most patients, is there a written unit policy on cardiopulmonary resuscitation (CPR)?
Does the unit policy state that CPR is to be performed on all patients who have a cardiac arrest in the dialysis unit regardless of patients’ age, comorbidity and preferences?
On the basis of your medical training, how well prepared do you feel to make decisions to continue, withdraw, and withhold dialysis with patients and families?
In your practice: A physician-patient relationship is developed for shared decision-making?
Your practice fully informs AKI, stage 4 and 5 CKD, and ESKD patients about their diagnosis, prognosis, and all treatment options?
Your practice offers palliative care services to all AKI, CKD, and ESKD patients who suffer from burdens of their disease?
Your practice institute advanced care planning for high-risk patients who suffer from burden of their disease?
Your practice follows clinical practice guideline for Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis?
Your practice uses a systematic approach to communicate about diagnosis, prognosis, treatment options, and goals of care?
Before starting dialysis for high risk patients, your practice obtains patient informed consent about stopping dialysis in case of persistent vegetative state (PVS).
In your practice: Management of patients with very poor prognosis or for whom dialysis cannot be provided safely: consider forgoing dialysis/consider time-limited trial of dialysis/offer palliative care/offer low efficacy dialysis/offer peritoneal dialysis/stop dialysis/consider Do Not Resuscitate status/
In your practice: The following impacts the decision-making process: religious background/culture background/cost of treatment/access to palliative care/local policy/