The coronavirus disease 2019 (COVID-19) is a frequent respiratory infection disease, as of November 16th, 2021, 254728728 COVID-19 infections, and 5125685 COVID-19-related deaths (2.01%) had been reported worldwide (https://www.worldometers.info/coronavirus/). While the main clinical manifestations of acute COVID-19 are respiratory symptoms (eg; cough, sputum, and dyspnea), additional cardiac, muscular, and neurologic symptoms/complications (eg; chest pain, myocarditis fatigue, myalgia, myopathy, rhabdomyolysis, paresthesia, severe viral encephalitis) were reported [Citation1]. The issue with the acute COVID-19 is that even if patients are cured, 40–90% of them continue to experience several medium- to long-term effects [Citation2]. The latter patients are qualified as having a long COVID-19 [Citation3]. Long COVID-19 is defined by the persistence of symptoms beyond 12 weeks after acquiring the infection, with no alternative diagnosis, irrespective of the viral status [Citation3]. More than 50 symptoms have been identified for long COVID-19 [Citation4]. Some of the symptoms affect the chain implicated during adaptation to exercise, namely the respiratory (eg; dyspnea, cough, post activity polypnea), cardiovascular (eg; chest pain), muscular (eg; myalgia, fatigue), and neurological (eg; headache, dizziness) systems [Citation4]. Furthermore, a study from Norway demonstrated that three months after hospital discharge, one-third of long COVID-19 patients had a peak oxygen consumption <80 of their predicted normal values (ie; incapacity) [Citation5].
Nowadays, there are several recommendations/guidelines related to the management of long COVID-19 patient [Citation6–10]. These guidelines target the specialist physicians, mainly pulmonologists [Citation6], cardiologists [Citation8], physical medicine and rehabilitation specialists [Citation7], or a combination of different specialists [Citation9]. The cardiorespiratory rehabilitation (CRR), which is a pillar of the aforementioned guidelines [Citation10], significantly relieves the symptoms of dyspnea, anxiety and depression, and eventually improves the patients’ physical functions and quality of life [Citation11]. The first study aiming to evaluate the impacts of CRR (ie; 10 minutes sessions’, twice a week, for 6 weeks) on long COVID-19 elderly patients from China [Citation12], reported an improvement in respiratory function (eg; increase of the first second forced expiratory volume by 0.34 ± 0.17 l), endurance (eg; increase in 6-min walk distance by 49.6 ± 10.5 m), and quality of life (all dimensions of the SF36 scale). Furthermore, a recent German cohort including 28 long COVID-19 patients aged 66 years and more [Citation13], confirmed the findings of the Chinese study [Citation12]. The ‘ideal’ CRR program, which should be performed in special centers, contains several specific tests’ evaluation that should be performed pre- and post-CRR (eg; lung function tests, walking tests, cardiorespiratory exercise test, quality of life questionnaires).
In real practice, there is a paradox in the management of patients with long COVID-19. Indeed, general practitioners (GPs) are on the front line in the management process of long COVID-19 patients because as the pandemic evolves, more and more long COVID-19 patients will be in need of treatment/assistance [Citation14]. For long COVID‐19 patients, and according to the World Health Organization guidelines, CRR should be provided not only at tertiary- or secondary care, but mainly at primary‐care with a real implication of GPs [Citation15]. However, only few published papers related to the management of COVID-19 patients were addressed for GPs [Citation16]. For instance, a recent review recommended that GPs ask their long COVID-19 patients to perform an individualized CRR via a light aerobic exercise [Citation17]. Nevertheless, GPs are probably unable to perform (or demand) the aforementioned pre/post-CRR evaluations specific tests, or to correctly apply the full guidelines addressed for specialists [Citation6–9]. Therefore, an alternative including the CRR ‘minimal advice’ that a GP should provide to long COVID-19 patients, seems to be necessary to respond to the needs of GPs to face their involvement with long COVID-19 patients. Thus, this paper aimed to ‘report’ the CRR ‘minimal advice’ that should be provided by GPs managing long COVID-19 patients with incapacity (ie; alteration of the cardiorespiratory and muscular chain).
The CRR ‘minimal advice’ reported in this paper is mainly ‘inspired’ from the Stanford Hall consensus statement for post-COVID-19 rehabilitation [Citation9], the American Societies of Cardiology and Sports Medicine recommendations for the practice of physical activity in chronically ill patients being over 50 years old [Citation18], the British Association of Sport and Exercise Sciences consensus related to the ABC of physical activity in conditioned individuals [Citation19], and from the ‘minimum rehabilitation advice’ that any doctor can (and shall) prescribe in front of a chronic respiratory patient [Citation20]. The Stanford Hall consensus statement for post-COVID-19 rehabilitation [Citation9] was established by seven teams including a team of six GPs.
In practice, the authors ‘recommend’ that the GPs divide their long COVID-19 patients into small groups (n = 3–5 patients by group, for example), and to plan two meetings (ie; pre/post the CRR program) (). During the pre-CRR meeting, that can be scheduled few days before the CRR, the GPs should: i) explain the ‘minimal CRR program’, such as its content and items, ii) focus on patient education regarding general topics (eg; comorbidities, smoking cessation when applicable); iii) provide a psychological/emotional support and nutritional counseling, iv) ‘View’, if possible, videos/illustrations explaining the exercise-training modalities [Citation21], v) evaluate the patients’ dyspnea using the modified medical research council or the visual analogue scales [Citation22,Citation23] (), and vi) answer patient’s inquiries. The post-CRR meeting can be scheduled some days after the end of the CRR program, in order to check its results in terms of dyspnea, to get the patients’ feedback, and to encourage patients keeping the exercise-training program as long as possible ().
Figure 2. Methods of dyspnea evaluation. A. Visual analogue scale. B. Modified medical research council
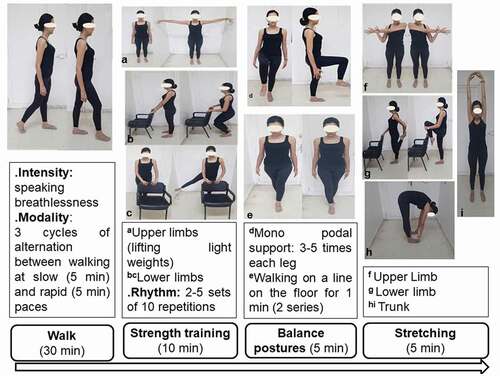
The exercise-training, which is the angular stone of the CRR program [Citation5], should ‘ideally’ include at least 12 sessions (ie; three sessions/week for four weeks) (). Each session duration is about 50 minutes. resumes a session of a ‘minimal’ exercise-training that GPs should recommend to their long COVID-19 patients. The typical exercise-training session should include the following 4 items.
1. Item 1. walking for 30 minutes
The intensity of walking can be evaluated by the ability of speaking during walk without being out of breath. The walking modality consists in three cycles of alternation between (i) walking at a slow pace (ie; without being out of breath) for 5 minutes and (ii) walking at a rapid pace (ie; near the breathlessness speaking threshold) maintaining this pace for five minutes. Therefore, the patient will walk for 30 minutes.
2. Item 2. strength training for 10 minutes
There are different types of muscle strength exercise for the upper and lower limbs [Citation21]. Three types of muscle strength exercises (one for upper limbs and two for lower limbs) are encouraged. For the upper limbs, a lightweight dumbbell or water’ bottle (eg; 0.5 kg or 0.5 l, respectively) are needed. The patient should hold one dumbbell/bottle in each hand. Starting with arms alongside the body; the patient should simultaneously raise arms to the side-up to shoulder height without bending elbows. Then, the patient should go back down slowly. The aforementioned movements can be done in the frontal/sagittal plans [Citation21]. For the lower limbs, the first exercise consists on standing with two legs extended slightly apart, both hands resting on the back of a chair. The patient should bend both knees, and hold the position for 5 seconds; then get up slowly (). During the second exercise, the patient should keep the same standing position behind a chair, alternatively raising the right then left lower limbs outstretched in the frontal plane to maximum amplitude, holding for a few seconds, and return to the starting position. For each muscle strength exercise, the patient should perform two to five sets of 10 repetitions each.
3. Item 3. balance posture for 5 minutes
This item includes two types of balance posture exercises. The first is the monopodal support. The patient should stand up feet slightly apart, keep upper body straight, raise one of the knees until placing thigh in a horizontal position for 10 seconds, and then lower back the knee towards the initial position. This exercise should be repeated 3–5 times on each leg [Citation21]. The second exercise is walking on a straight line of 10 meters for 1 minute, by doing straight line shuttles.
4. Item 4. stretching for 5 minutes
Some easy stretching exercises are recommended at the end of the workout [Citation21] (). In frail long-COVID-19 patients, stretching exercises may represent a muscular solicitation equivalent to a muscle strengthening solicitation [Citation24]. The recommended protocol is two × 20 seconds per exercise at 50% of the point of discomfort (ie; pain in the muscles/tendons).
A video illustrating a practical/standard session of daily exercise training for patients with a chronic respiratory condition is available online [Citation21]. GPs can show/recommend this video for their patients, in a way that patients can watch it several times if needed.
The proposed exercise-training program with its 4 items has several advantages. First, it is safe with no contraindication. Second, it is costless since it is a home/outdoor based program. Third, it doesn’t require expensive equipment. Fourth, the exercise-training sessions can be performed individually or in small groups or couples, which is motivating by creating a group dynamic. It is true that primary care is already a busy specialty, and the ‘idea” to ask GPs to provide the CRR’ ‘minimum advice’ for their long COVID-19 patients appears ‘wrongdoing’. However, as the World struggles with prolonged waves of acute COVID-19 (to date of the present exchanges), GPs need to be organized to care for patients presenting with long COVID-19 manifestations of this multifaceted disease [Citation16]. Key functions of GPs, such as person-focused care over time; and first contact/comprehensive/coordinated care, likely will prove to be the cornerstone of managing millions of patients who develop or will develop long COVID-19 [Citation16]. The authors call for a multicenter study to test our proposed exercise-training program in order to assess its suitability and reliability in primary care settings.
This paper is i) a call for action in order to popularize the CRR for long COVID-19 patients in general medicine; ii) an invitation to other researchers to contact us to justly, set a worldwide multicenter protocol altogether, and iii) a CRR primer for GPs taking care of long COVID-19 patients.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Behzad S, Aghaghazvini L, Radmard AR, et al. Extrapulmonary manifestations of COVID-19: radiologic and clinical overview. Clin Imaging. 2020;66:35–5.
- Carfi A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. Jama-J Am Med Assoc. 2020;324(6):603–605.
- Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869–875.
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Res Sq. 2021;11:1.
- Skjorten I, Ankerstjerne OAW, Trebinjac D, et al. Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. Eur Respir J. 2021;58(2):2.
- Andrejak C, Blanc F-X, Costes F, et al. Guide for follow-up of patients with SARS-CoV-2 pneumonia. Management proposals developed by the french-language respiratory medicine society. version of 10 May 2020. Rev Mal Respir. 2020;37(6):505–510.
- Stein J, Visco CJ, Barbuto S. Rehabilitation medicine response to the COVID-19 pandemic. Am J Phys Med Rehabil. 2020;99(7):573–579.
- European society of cardiology. Guidance for the diagnosis and management of CV disease during the COVID-19 pandemic. (2021 Nov 16). Available from: . https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance
- Barker-Davies RM, O’Sullivan O, Senaratne KPP, et al. The stanford hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54(16):949–959.
- Agostini F, Mangone M, Ruiu P, et al. Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med. 2021;53(1):jrm00141.
- Siddiq MAB. Pulmonary rehabilitation in COVID-19 patients: a scoping review of current practice and its application during the pandemic. Turk J Phys Med Rehabil. 2020;66(4):480–494.
- Liu K, Zhang W, Yang Y, et al. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract. 2020;39:101166.
- Hermann M, Pekacka-Egli A-M, Witassek F, et al. Feasibility and efficacy of cardiopulmonary rehabilitation After COVID-19. Am J Phys Med Rehabil. 2020;99(10):865–869.
- Atherton H, Briggs T, Chew-Graham C. Long COVID and the importance of the doctor–patient relationship. Br J Gen Pract. 2021;71(703):54–55.
- Negrini S, Mills J-A, Arienti C, et al. “Rehabilitation research framework for patients with COVID-19” defined by Cochrane rehabilitation and the world health organization rehabilitation programme. Arch Phys Med Rehabil. 2021;102(7):1424–1430.
- Greenhalgh T, Knight M. Long COVID: a Primer for Family Physicians. Am Fam Physician. 2020;102(12):716–717.
- Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infectious Diseases. 2021;53(10):737–754.
- American College of Sports M, American Heart A, Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American college of sports medicine and the American heart association. Circulation. 2007;116(9):1094–1105.
- O’Donovan G, Blazevich AJ, Boreham C, et al. The ABC of physical activity for health: a consensus statement from the British association of sport and exercise sciences. J Sports Sci. 2010;28(6):573–591.
- Prefaut C. Respiratory rehabilitation in chronic obstructive pulmonary disease (COPD). J Fran Viet Pneu. 2012;03(9):1–60.
- Daily exercise training. A practical session. (2021 Nov 16). Available from: http://www.respir-sud.com/english/rehabilitation/12/105/2/D%C3%A9monstration.html
- Fletcher CM, Elmes PC, Fairbairn AS, et al. The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br Med J. 1959;2(5147):257–266.
- Sergysels R, Hayot M. [Evaluation of exercise-induced dyspnea]. Revue de pneumologie clinique. 1997;53(5):278–282.
- Zha L, Xu X, Wang D, et al. Modified rehabilitation exercises for mild cases of COVID-19. Ann Palliat Med. 2020;9(5):3100–3106.