?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
To explore the relationship between serum levels of midkine and omentin-1 and the severity of sepsis in patients, and their prognostic value. A retrospective analysis was conducted on the clinical data of 180 sepsis patients. According to the severity of the patient’s condition, they were separated into sepsis group (n = 76), severe sepsis group (n = 59), and sepsis shock group (n = 45). Based on the survival within 28 days of admission, they were grouped into survivors group (n = 128) and nonsurvivors group (n = 52). The serum Midkine level and APACHE II score in the sepsis shock group were higher than those in the severe sepsis group and sepsis group, while the Omentin-1 level was lower than that in the severe sepsis group and sepsis group (p < 0.05). The serum Midkine level and APACHE II score in the severe sepsis group were higher than those in the sepsis group, while the Omentin-1 level was lower than that in the sepsis group (p < 0.05). The Midkine and APACHE II score in the nonsurvivors group was higher than those in the survivors group, while the Omentin-1 score was lower than that in the survivors group (p < 0.05). Midkine and APACHE II score were independent risk factors for the prognosis of sepsis patients, while Omentin-1 was a protective factor for the prognosis of sepsis patients (p < 0.05). The AUC of the combined prediction of serum Midkine and Ommentin-1 for the prognosis of sepsis patients was 0.880, with a sensitivity of 90.38% and a specificity of 72.66%. The combined prediction of serum Midkine and Ommentin-1 was better than that of individual prediction of Midkine and Ommentin-1. Serum Midkine is highly expressed and Omentin-1 is lowly expressed in sepsis patients, and the combination of the two has a high predictive power for the prognosis of sepsis patients.
1. Introduction
Sepsis is a global health issue and one of the most formidable complications for hospitalized patients, ultimately leading to death from infections. It is the common final pathway for fatal infections, directly or indirectly causing the death of approximately half of all hospitalized patients [Citation1]. Sepsis is a time-dependent disease; if not treated promptly, it can further deteriorate into septic shock, multiple organ failure, and is associated with anxiety, depression, and post-traumatic stress disorder, resulting in negative physiological, psychological, and economic outcomes [Citation2]. Host response biomarkers play a critical role in sepsis diagnosis, early identification of organ dysfunction, risk stratification, prognosis, and patient management. Biomarkers help not only in stratifying sepsis patients into biological phenotypes such as high inflammation and immunosuppression but also in identifying intestinal permeability, blood-brain barrier permeability, readmission probability, and long-term prognosis [Citation3]. Therefore, it is of great significance to identify serum biological markers associated with the severity and prognosis of sepsis. Midkine is a cysteine-rich polypeptide expressed in many locations, including the gastrointestinal tract, spleen, kidneys, lungs, and thyroid, but is expressed at low levels in healthy adults. It promotes chronic inflammation by enhancing the chemotaxis and tissue infiltration of neutrophils and macrophages, participating in the pathogenesis of autoimmune and autoinflammatory diseases, and can serve as an indicator and biomarker for these diseases [Citation4]. Omentin-1 is a novel adipocytokine highly expressed in visceral adipose tissue interstitial vascular cells, with antioxidative stress and anti-inflammatory effects in macrophages, endothelial cells, and adipocytes [Citation5]. Studies have shown that Omentin-1 plays an important role in the inflammatory and metabolic processes in Intensive Care Unit (ICU) patients, with higher levels of Omentin-1 in non-sepsis patients compared to sepsis and septic shock patients, and ICU survivors having higher levels of Omentin-1 than those who died [Citation6]. Furthermore, studies have found that serum Omentin-1 levels are elevated in SEP patients and are associated with the severity of SEP and the 28-day mortality rate [Citation7]. The expression of Midkine and Omentin-1 in the serum of SEP patients remains unclear.Based on this, our study aims to detect the expression of Midkine and Omentin-1 in the serum of sepsis patients, analyze their relationship with the severity and prognosis of sepsis patients, and provide references for improving the survival rate of sepsis.
2. Study subjects and methods
2.1. Study subjects
A retrospective analysis of the clinical data of 180 sepsis patients treated at our hospital from September 2021 to June 2023 was conducted. Based on the severity of the condition [Citation8], patients with hypotension, poor tissue perfusion, and organ dysfunction were classified into the severe sepsis group (n = 59), patients with persistent hypotension or uncorrectable tissue perfusion after fluid resuscitation were classified into the severe septic shock group (n = 45), and those without the above conditions were classified into the sepsis group (n = 76). Based on the survival status within 28 days of admission, they were divided into the survivors group (n = 128) and nonsurvivors group (n = 52). Inclusion criteria: (1) Conforming to sepsis [Citation9] diagnostic guideline standards; (2) Age over 18 years old; (3) The patient or family member voluntarily signed an informed consent. Exclusion criteria: (1) Patients with malignant tumors; (2) Patients with incomplete clinical data; (3) Patients with major organ dysfunction such as heart, brain, liver; (4) Patients who had undergone organ transplantation. This study was reviewed and approved by the ethics committee of our hospital and followed the Declaration of Helsinki. The case flow chart is shown in .
2.2. Methods
2.2.1. Sample collection
Approximately 3–5 mL of fasting venous blood from sepsis patients was collected within 24 hours of admission, centrifuged at 3500 r/min for 10 minutes, and the serum was separated and stored at −20°C for later analysis.
2.2.2. Serum Midkine, Omentin-1 level detection and APACHE II scoring
Midkine levels were measured using an ELISA kit (Catalog#: CSB-E08892h, Wuhan Epitope Biotechnology Co., Ltd.), the intra-assay coefficient of variation is 5.84%, the inter-assay coefficient of variation is 5.41%, and the detection range is 0.1 to 100 ng/mL;Omentin-1 levels were measured using an ELISA kit (Catalog#: XY2457A, Shanghai XuanYa Biotechnology Co., Ltd.), The intra-assay coefficient of variation is 5.91%, the inter-assay coefficient of variation is 5.77%, and the detection range is 10 to 1000 ng/mL. The severity of sepsis patients within 24 hours of admission was assessed using the APACHE II scoring system [Citation10].
2.3. Statistical methods
Data were analyzed using SPSS 25.0 software. Quantitative data (levels of Midkine, Omentin-1) following a normal distribution were described as mean ± standard deviation (SD), and comparisons between two groups were performed using independent sample t-tests, while comparisons among multiple groups were conducted using one-way ANOVA with further pairwise comparisons using Snk-q tests. Categorical data were presented as n (%) and analyzed using the Chi-square test. Multifactorial logistic regression analysis was conducted to identify factors affecting the prognosis of sepsis patients. ROC curve analysis evaluated the predictive value of serum Midkine and Omentin-1 for the prognosis of sepsis patients. A p-value < 0.05 was considered statistically significant.
3. Results
3.1. Comparison of baseline variables among the three groups
The serum Midkine levels and APACHE II scores in the septic shock group were higher than those in the severe sepsis group and the sepsis group, while the Omentin-1 levels were lower than those in the severe sepsis group and the sepsis group (p < 0.05). The severe sepsis group had higher serum Midkine levels and APACHE II scores compared to the sepsis group, and lower Omentin-1 levels compared to the sepsis group (p < 0.05). There were no significant differences among the three groups in terms of age, gender, BMI, smoking history, drinking history, TC, and TG (p > 0.05). See .
Table 1. Comparison of baseline variables among the three groups.
3.2. Comparison of baseline variables based on the prognosis of sepsis patients
The Midkine levels and APACHE II scores in the nonsurvivors group were higher than those in the survivors group, while Omentin-1 levels were lower in the nonsurvivors group compared to the survivors group (p < 0.05). There were no significant differences between the two groups in terms of age, gender, BMI, smoking history, drinking history, TC, and TG (p > 0.05). See .
Table 2. Comparison of baseline variables based on the prognosis of sepsis patients.
3.3. Analysis of factors influencing the prognosis of sepsis patients
Using the prognosis of sepsis patients as the dependent variable (death = 1, survival = 0), and Midkine, Omentin-1, and APACHE II scores (all continuous variables) as independent variables for multivariate logistic regression analysis, the results showed that Midkine and APACHE II scores were independent risk factors for the prognosis of sepsis patients, while Omentin-1 was a protective factor for the prognosis of sepsis patients (p < 0.05). See .
Table 3. Analysis of factors influencing the prognosis of sepsis patients.
3.4. Predictive value of serum Midkine and Omentin-1 levels for the prognosis of sepsis patients
The AUC for predicting the prognosis of sepsis patients using serum Midkine was 0.842, and for serum Omentin-1 was 0.783; the combined prediction of the prognosis of sepsis patients using both was 0.880. The combined prediction was superior to the individual predictions of Midkine and Omentin-1 alone (Zcombined-Midkine = 2.183, Zcombined-Omentin-1 = 3.317, p = 0.029, 0.001). See and .
Figure 2. ROC Curves for Predicting the Prognosis of Sepsis Patients Using Serum Midkine and Omentin-1 Levels.
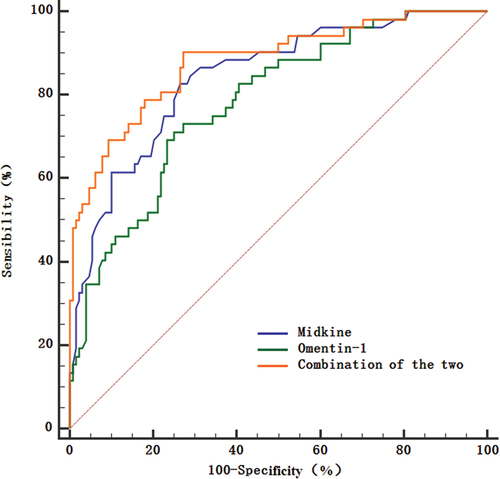
Table 4. Predictive value of serum midkine and omentin-1 levels for the prognosis of sepsis patients.
4. Discussion
Sepsis is a complex process caused by a dysregulated host response to infection. Globally, there are 48.9 million cases of SEP, leading to 11 million deaths annually. Sepsis is a significant contributor to the global burden of disease, with patients having an average hospital stay twice as long as those with any other fatal disease. Even after discharge, sepsis survivors have poor prognoses, with a 15% mortality rate within the first year after discharge and a 6–8% mortality rate in the subsequent five years [Citation11]. Therefore, identifying serum biological markers associated with the severity and prognosis of sepsis in patients is of great significance.
Midkine is a 13 kDa heparin-binding cytokine and growth factor involved in processes such as inflammation, angiogenesis, and tumor growth. It is significantly overexpressed in sepsis patients and is associated with disease severity, 28-day mortality, and lung and kidney injuries [Citation12]. Kekilli et al. [Citation13] found that Midkine levels in patients with Crohn’s disease, both during active and remission phases, were significantly higher than in healthy controls and significantly correlated with inflammation markers, making it a potential therapeutic target for Crohn’s disease treatment. Deng et al. [Citation14] discovered that Midkine was significantly overexpressed in a chronic obstructive pulmonary disease mouse model. The Midkine-Notch2 signaling pathway promotes inflammation and excessive proliferation of airway smooth muscle cells, leading to airway narrowing and progressive decline in lung function in patients with chronic obstructive pulmonary disease. Xu et al. [Citation15] found that Midkine was highly expressed in both sepsis patients and cecal ligation and puncture model mice in circulation and lungs and was related to severe lung injury. Inhibiting Midkine may involve the ACE/Ang II pathway induced by angiotensin-converting enzyme and the Notch 2 pathway, thereby improving lung injury caused by sepsis. Hohlstein et al. [Citation16] found that Midkine was highly expressed in the serum of SEP patients and related to bacterial inflammation, renal function, coagulation function, and insulin metabolism indicators. Krzystek-Korpacka et al. [Citation17]found that the expression of Midkine increases progressively from healthy inflammation, systemic inflammation, severe sepsis, to septic shock. Our study found that Midkine levels significantly increased with the worsening of sepsis conditions and were significantly higher in the nonsurvivors group than in the survivors group, suggesting that Midkine may contribute to the worsening of sepsis conditions and poor prognosis of patients by participating in the biological processes of cells, inflammation, metabolism, and other processes.
Omentin-1 is a newly discovered secreted protein selectively expressed in visceral adipose tissue, promoting macrophage differentiation into anti-inflammatory M2 phenotype, inhibiting inflammatory response and foam cell formation, thereby suppressing inflammatory response and playing an important role in various diseases [Citation18]. Kir et al. [Citation19] found that Omentin-1 expression levels were lower in patients with hypothyroidism combined with autoimmune thyroiditis and negatively correlated with thyroid-stimulating hormone, which is a key influencing factor in the occurrence of the disease. Ko et al. [Citation20] discovered that Omentin-1 levels in patients with osteoarthritis were significantly lower than those in the normal control group, and it can prevent cartilage degradation and bone erosion caused by anterior cruciate ligament transection by inhibiting the production of pro-inflammatory cytokines and promoting the polarization of M2 macrophages in the body, making it a potential therapeutic target for the treatment of osteoarthritis. Zhou et al. [Citation21] found that Omentin-1 was expressed at low levels in patients with idiopathic pulmonary fibrosis. Omentin-1 can prevent the activation of fibroblasts by reducing the expression of α-SMA in TGF-β-induced mouse and human primary fibroblasts, increasing the level of p-AMPK in the body, and alleviating bleomycin-induced pulmonary fibrosis, showing broad application prospects in the prevention and treatment of pulmonary fibrosis. Tao et al. [Citation22] discovered that Omentin-1 levels were reduced in the colitis patients and mouse models. Omentin-1 can effectively improve inflammation and intestinal barrier damage by activating Nrf2 to repair the intestinal barrier, thereby improving oxidative stress, inhibiting NF-κB signal transduction, reducing ROS and MDA levels, and increasing the production of GSH and SOD to regulate the redox balance. Gültekin et al. [Citation6] found that Omentin-1 levels were decreased in ICU patients and were associated with the severity of sepsis in patients, poor prognosis, and increased mortality in sepsis patients. This study found that serum Omentin-1 levels significantly decreased sequentially in the sepsis group, severe sepsis group, and septic shock group, and were significantly lower in the mortality group. This suggests that Omentin-1 may be associated with the occurrence, progression, and poor prognosis of sepsis. Additionally, Luedde et al. [Citation23] found no difference in Omentin-1 levels between ICU patients and healthy controls, but elevated Omentin-1 levels predicted long-term survival in patients with impaired sepsis. This contrasts with the results of this study, which may be related to differences in the time period of detection and the severity of the patients’ conditions.The AUC for the combined prediction of sepsis patient prognosis by serum Midkine and Omentin-1 was 0.880, with a sensitivity of 90.38% and a specificity of 72.66%. The combined prediction of sepsis patient prognosis by the two was superior to the individual predictions of Midkine and Omentin-1, suggesting that both Midkine and Omentin-1 may be involved in processes such as inflammatory response, mediating the poor prognosis of sepsis, and both can serve as serum biomarkers for the prognosis of sepsis patients. Further studies showed that Midkine and APACHE II scores were independent risk factors for the prognosis of sepsis patients, while Omentin-1 was a protective factor for the prognosis of sepsis patients, indicating that in clinical practice, attention should be paid to Midkine and Omentin-1 levels and APACHE II scores, and treatment measures should be adjusted in a timely manner to improve patient prognosis.
In conclusion, serum Midkine is highly expressed, and Omentin-1 is lowly expressed in sepsis patients, and The combination of these two biomarkers has a high predictive efficiency for the prognosis of sepsis patients, allowing for timely detection of disease progression and improved patient outcomes in clinical practice. However, this study has limitations, such as a small sample size, a single source of samples, and unclear mechanisms of how Midkine and Omentin-1 are involved in sepsis. Further research with redesigned experiments is needed.
Consent for publication
All authors give consent for publication.
Research involving human participants
The study was approved by Ganzhou People’s Hospital. Written informed consent to participate in this study was provided by the participants.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The original contributions presented in the study are included in the article.
Additional information
Funding
References
- Mirijello A, Tosoni A. On behalf of the internal medicine sepsis study G. New strategies for treatment of sepsis. Medicina (Kaunas). 2020;56(10):527. doi: 10.3390/medicina56100527
- Rababa M, Bani Hamad D, Hayajneh AA, et al. Sepsis assessment and management in critically Ill adults: a systematic review. PLOS ONE. 2022;17(7):e0270711. doi: 10.1371/journal.pone.0270711
- Barichello T, Generoso JS, Singer M, et al. Biomarkers for sepsis: more than just fever and leukocytosis-a narrative review. Crit Care. 2022;26(1):14. doi: 10.1186/s13054-021-03862-5
- Aynacıoğlu AŞ, Bilir A, Tuna MY. Involvement of midkine in autoimmune and autoinflammatory diseases. Mod Rheumatol. 2019;29(4):567–6. doi: 10.1080/14397595.2018.1523701
- Peschel G, Weigand K, Grimm J, et al. Serum omentin-1 is correlated with the severity of liver disease in patients with chronic hepatitis C. World J Hepatol. 2023;15(12):1315–1324. doi: 10.4254/wjh.v15.i12.1315
- Gültekin Y, İ B, Gojayev A, et al. Can omentin-1 be a prognostic marker in surgical intensive care patients? Turk J Med Sci. 2021;51(5):2485–2493. doi: 10.3906/sag-2009-158
- Karampela I, Vallianou NG, Tsilingiris D, et al. Diagnostic and prognostic value of serum omentin-1 in sepsis: a prospective study in critically Ill patients. Medicina (Kaunas). 2023;59(5):833. doi: 10.3390/medicina59050833
- Dugar S, Choudhary C, Duggal A. Sepsis and septic shock: guideline-based management. Cleve Clin J Med. 2020;87(1):53–64. doi: 10.3949/ccjm.87a.18143
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287
- Thakur R, Naga Rohith V, Arora JK. Mean SOFA score in comparison with APACHE II score in predicting mortality in surgical patients with sepsis. Cureus. 2023;15(3):e36653. doi: 10.7759/cureus.36653
- Arora J, Mendelson AA, Fox-Robichaud A. Sepsis: network pathophysiology and implications for early diagnosis. Am J Physiol Regul Integr Comp Physiol. 2023;324(5):R613–R24. doi: 10.1152/ajpregu.00003.2023
- Chang W, Peng F, Sun Q, et al. Plasma midkine is associated with 28-day mortality and organ function in sepsis. J Intensive Care Med. 2020;35(11):1290–1296. doi: 10.1177/0885066619861580
- Kekilli M, Tanoğlu A, Karaahmet F, et al. Midkine level may be used as a noninvasive biomarker in Crohn’s disease. Turk J Med Sci. 2020;50(2):324–329. doi: 10.3906/sag-1904-167
- Deng T, Huang Q, Lin K, et al. Midkine-Notch2 pathway mediates excessive proliferation of airway smooth muscle cells in chronic obstructive lung disease. Front Pharmacol. 2022;13:794952. doi: 10.3389/fphar.2022.794952
- Xu J-Y, Chang W, Sun Q, et al. Pulmonary midkine inhibition ameliorates sepsis induced lung injury. J Transl Med. 2021;19(1):91. doi: 10.1186/s12967-021-02755-z
- Hohlstein P, Abu Jhaisha S, Yagmur E, et al. Elevated midkine serum levels are associated with long-term survival in critically Ill patients. Int J Mol Sci. 2023;25(1):454. doi: 10.3390/ijms25010454
- Krzystek-Korpacka M, Mierzchala M, Neubauer K, et al. Midkine, a multifunctional cytokine, in patients with severe sepsis and septic shock: a pilot study. Shock. 2011;35(5):471–477. doi: 10.1097/SHK.0b013e3182086001
- Askin L, Duman H, A O, et al. Association between omentin-1 and coronary artery disease: pathogenesis and clinical research. Curr Cardiol Rev. 2020;16(3):198–201. doi: 10.2174/1573403X16666200511085304
- Kir S, Gorar S, Sari IK, et al. Omentin-1 levels in hypothyroid patients with autoimmune thyroiditis. J Coll Physicians Surg Pak. 2023;33(8):842–846.
- Ko C-Y, Lin Y-Y, Achudhan D, et al. Omentin-1 ameliorates the progress of osteoarthritis by promoting IL-4-dependent anti-inflammatory responses and M2 macrophage polarization. Int J Biol Sci. 2023;19(16):5275–5289. doi: 10.7150/ijbs.86701
- Zhou Y, Zhang Y, Cheng H, et al. Therapeutic effects of omentin-1 on pulmonary fibrosis by attenuating fibroblast activation via AMP-Activated protein kinase pathway. Biomedicines. 2022;10(11):2715. doi: 10.3390/biomedicines10112715
- Tao M, Yan W, Chen C, et al. Omentin-1 ameliorates experimental inflammatory bowel disease via Nrf2 activation and redox regulation. Life Sci. 2023;328:121847. doi: 10.1016/j.lfs.2023.121847
- Luedde M, Benz F, Niedeggen J, et al. Elevated omentin serum levels predict long-term survival in critically Ill patients. Dis Markers. 2016;2016:3149243. doi: 10.1155/2016/3149243