ABSTRACT
Background: Oral microbiota has been at the center of cultural attention in recent years. In daily clinical practice, orthodontic appliances may be associated with an increased cariogenic risk and a worsening of preexisting periodontal diseases.
Objective: The purpose of this review is to investigate the available evidence regarding the association between orthodontic appliances and changes in the quality and quantity of the oral microbiota.
Design: The research included every article published up to October 2017 featuring the keywords ‘Orthodontic appliance* AND (microbiological colonization OR periodontal pathogen* OR Streptococcus mutans OR Lactobacillus spp. OR Candida OR Tannerella forsythia OR Treponema denticola OR Fusobacterium nucleatum OR Aggregatibacter actinomycetemcomitans OR Prevotella intermedia OR Prevotella nigrescens OR Porphyromonas gingivalis)’ and was conducted in the major medical databases. The methodological quality of selected papers was scored using the ‘Swedish Council on Technology Assessment in Health Care Criteria for Grading Assessed Studies’ (SBU) method.
Results: Orthodontic appliances influence the oral microbiota with an increase in the counts of S. mutans and Lactobacillus spp. and in the percentage of potentially pathogenic gram-negative bacteria.
Conclusions: There is moderate/high evidence regarding the association between orthodontic appliances and changes in the oral microbiota.
PROSPERO registration number CRD42018091589.
Introduction
Periodontal health is crucial and requires special attention when performing an orthodontic treatment plan, both in adult and pediatric patients [Citation1]. Preserving the integrity of periodontal tissues is one of the main concerns of orthodontics specialists, which has led to the definition of specific hygiene protocols for orthodontic patients [Citation2]. Since 1985, the scientific community has been very concerned about the interaction between orthodontic devices and oral bacteria [Citation3,Citation4]; in fact, the first studies to analyze the oral microbiota and conventional braces (CB) took place in this period. In 2012, Freitas et al. published a systematic review regarding the alteration of the oral microbiota caused by fixed appliances [Citation5]. The authors concluded that ‘The literature revealed moderate evidence that the presence of fixed appliances influences the quantity and quality of oral microbiota’. However, the authors included papers that analyzed bacteria from appliance surfaces and from oral mucosa, without distinction.
Furthermore, a significant number of studies have been published since 2012. Our review aims to update the research of Freitas et al., focusing on studies that have analyzed the microbiota collected from oral sites and not directly from appliances, and including all appliance types (self-ligating braces, invisalign aligners, sports-mouthguards, and other removable appliances) and not only fixed appliances.
Thus, the clinical research questions were as follows:
Do orthodontic appliances influence the quality and quantity of the oral microbiota?
What are the effects of orthodontic devices on the different bacterial species in the oral cavity?
Materials and methods
A search of the keywords Orthodontic appliance* AND (microbiological colonization OR periodontal pathogen* OR Streptococcus mutans OR Lactobacillus spp. OR Candida OR Tannerella forsythia OR Treponema denticola OR Fusobacterium nucleatum OR Aggregatibacter actinomycetemcomitans OR Prevotella intermedia OR Prevotella nigrescens OR Porphyromonas gingivalis) was conducted in PubMed, PMC, Scopus, Lilacs, Scielo, Cochrane Trial Library, Web of Science. All articles published up to October 2017 were included. The Preferred Reporting Items for Reporting Systematic reviews and the Meta Analyses protocol were adopted for this systematic review [Citation6].
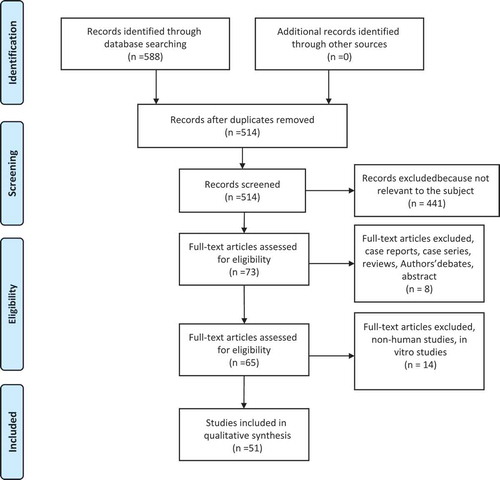
During the first phase, all the articles were selected by title and abstract by two of the authors and duplicate exclusion was performed. In the next phase, the full texts of potentially relevant papers were evaluated to determine if they met the eligibility criteria. Articles were selected on the basis of the criteria listed in . The article selection process is illustrated in . Discussions were held to resolve any disagreements; when a resolution could not be found, a third review was consulted. Data extraction from the selected papers was performed independently by two review authors who adopted a template similar to that of Freitas et al. [Citation5]. The template was adapted to the necessities of our study and is shown in [Citation5].
Table 1. Study selection criteria
Table 2. Characteristics of studies included in the review
Extracted data included first author, year of publication, study design, sample size, age of the patients, type of appliance analyzed, collection time of the study, collection methods, microbial analysis methods, and quality of the study.
Quality analysis
The methodological quality is ‘the extent to which the design and conduct of a study are likely to have prevented systematic errors (bias)’. Variation in quality can explain variation in the results of studies included in a systematic review. More rigorously designed (better ‘quality’) trials are more likely to yield results that are closer to the ‘truth’ [Citation7].
The methodological quality of selected papers was scored using the ‘Swedish Council on Technology Assessment in Health Care Criteria for Grading Assessed Studies’ (SBU) method, which was also used to assess the level of evidence for the conclusions of this review. The SBU method divided the methodological quality of the articles into three grades: grade A – high value of evidence, grade B – moderate value of evidence, and grade C – low value of evidence; once a score had been assigned to each study, the review’s level of evidence was stated in four grades: grade 1 – strong scientific evidence (at least two studies assessed at level A), grade 2 – moderate scientific evidence (one level A study and at least two studies at level B), grade 3 – limited scientific evidence (at least two studies at level B), and grade 4 – insufficient scientific evidence (fewer than two studies at level B) (–) [Citation8].
Table 3. Swedish council on technology assessment in health-care (SBU) criteria for grading assessed studies
Table 4. Definitions of evidence level
Results
From the initial 588 articles, 51 were selected [Citation3,Citation4,Citation9–Citation57].
Quality of evidence
In 37 of the 52 articles presented with moderate methodological quality [Citation9–Citation21,Citation24–Citation26,Citation28,Citation29,Citation31–Citation33,Citation35–Citation39,Citation41–Citation46,Citation51–Citation53,Citation56,Citation57], the major concern was the absence of repeatability tests. One article had a high quality [Citation40] and the remaining 13 papers were classified as having a low quality [Citation3,Citation4,Citation22,Citation23,Citation27,Citation30,Citation34,Citation47–Citation50,Citation54,Citation55]. Due to the lack of homogeneity in the study settings, a meta-analysis could not be applied and a systematic review realized.
CB
Of the 29 articles that studied CB [Citation3,Citation4,Citation10,Citation12,Citation13,Citation19–Citation23,Citation26–Citation30,Citation32,Citation34,Citation35,Citation38,Citation41,Citation44,Citation46–Citation48,Citation50,Citation51,Citation54,Citation44,Citation57], the majority showed a significant increase in BOP and PI. Two studies [Citation10,Citation52] investigated the differences between the use of elastomeric or steel ligatures, revealing contradictory results on BOP and PI at different times. Ristic’s studies [Citation44,Citation45] highlighted that maximum values of PI and BOP were reached 3 months after appliance placement, followed by a decrease in these parameters 6 months after treatment began. Six studies assessed the increase of Candida at different times [Citation12,Citation13,Citation22,Citation23,Citation56,Citation57].
Twenty studies highlighted the increase of gram-positive bacteria, in particular S. mutans and Lactobacillus spp. [Citation3,Citation4,Citation12,Citation19–Citation21,Citation27–Citation30,Citation32,Citation34,Citation35,Citation42,Citation46,Citation47,Citation50,Citation51,Citation54,Citation57]. Three studies [Citation43,Citation44,Citation48] detected significant increases of gram-negative bacteria, respectively, at 3 and 6 months, followed by a decrease at 6 and 12 months. Ten studies [Citation10,Citation20,Citation21,Citation26,Citation30,Citation37,Citation41,Citation43,Citation44,Citation48] detected an increase in the percentage of gram-bacteria and A. actinomycetemcomitans. The study conducted by Alves de Souza et al. [Citation10] revealed a significant increase in gram-species with the use of elasticomeric rings ().
Table 5. Conventional braces results
Self-ligating braces
Eigh studies analyzed self-ligating braces (SLB) [Citation9,Citation14,Citation24,Citation37–Citation40,Citation54]. Two studies [Citation14,Citation40] revealed no differences for BOP and PI between SLB and CB, while Nalçac et al. and Uzuner et al. [Citation54] demonstrated a worsening in SLB. Two studies considered the use of SLB with or without elastomeric rings, observing an increase in gram-concentration [Citation24,Citation38]. One other study [Citation14] showed an increase of S. mutans and Lactobacillus spp. at 3 months with the use of SLB compared to controls. One study [Citation41] showed less S. mutans with SLB compared to CB ().
Table 6. Self-ligating braces results
Lingual braces
Four studies analyzed lingual braces (LB) [Citation15,Citation16,Citation33,Citation45] and three of these highlighted a worsening of PI and BOP [Citation15,Citation16,Citation33]. Two studies [Citation16,Citation33] revealed an increase of S. mutans and A. actinomycetemcomitans after 4 weeks ().
Table 7. Lingual braces results
Removable appliances
Six studies analyzed removable devices [Citation11,Citation17,Citation18,Citation31,Citation49,Citation52]. One study analyzed different interceptive removable appliances [Citation49], demonstrating an increase in both S. mutans and Lactobacillus spp.
The invisalign study, conducted by Levrini et al. [Citation31], revealed lower values of PI, BOP, and bacterial component at 3 months for the invisalign group.
In the two studies with thermoplastic retainers, Türköz et al. [Citation52] showed an increase of S. mutans and Lactobacillus spp. while Farhadian et al. [Citation18] observed that the addition of silver nanoparticles reduced the levels of S. mutans after 7 weeks.
In one study [Citation11], the use of space maintainers defined an increase in BOP in the number of bacteria and in Candida. Furthermore, D’Ercole et al. [Citation17] pointed out that the use of sports mouthguards produced an increase in BOP and PI ().
Table 8. Removable appliances results
Other appliances
Two studies investigated other kinds of orthodontic appliances [Citation25,Citation56]: one fixed interceptive orthodontic appliance and one esthetic brace. In a study that analyzed fixed interceptive appliances, Ortu et al. [Citation56] demonstrated an increase in S. mutans and Lactobacillus spp. ().
Table 9. Other appliances results
Discussion
The present systematic review agreed with the conclusions arrived at by Freitas et al. [Citation5], which could be extended to any type of orthodontic appliance. The evidence of the selected sample was of medium-high level due to the lack of error of measurements analysis for the collection of material from oral sites. Though this lack of standardization may influence the outcomes, due to the difficulty in obtaining a high repeatability in this procedure, it would not represent a major concern for the studies’ quality. In our sample, the use of orthodontic devices resulted in an increase in oral bacterial counts in patients, with significant differences between appliance type, depending on whether they were removable or not.
Previous studies have assessed the role of biomaterials in the regulation of the oral microbiota [Citation58]. As stated by Antonelli et al. [Citation59], the simplest surfaces for bacteria to colonize are hard ones as mucous membranes tend to scale off and, therefore, do not guarantee a stable adhesion. The only exception to this is the tongue, which is highly colonized even if it is a mucosal surface because of the irregular surfaces of papillae [Citation60]. Consequently, the introduction of a biomaterial into this open system creates a further retentive surface on which bacterial species are able to reproduce and where there is an increased difficulty in maintaining oral hygiene [Citation58]. As revealed by the Øilo and Bakken [Citation58] literature review, the presence of biomaterials results in an increase in plaque and alterations in the oral microbiota.
Thus, on the basis of these assessments, it seems reasonable to state that the grade of bacterial colonization related to orthodontic appliances is affected by the energy and roughness of the appliance surfaces, as well as their design and dimensions. This may be a key factor in efficiently performing hygiene procedures [Citation58].
Another significant variable for microbiota alterations is the amount of time the appliance is worn in the oral cavity, with removable appliances having significantly less impact on oral bacteria than fixed appliances [Citation61].
The quantitative alteration of the oral microbiota is related to an increase in clinical parameters, PI and BOP, which are risk indicators for oral pathologies [Citation62].
Together with the quantitative change, there is also a qualitative variation; indeed, there is an increase in gram-positive and gram-negative more aggressive bacteria, such as: S. mutans and Lactobacillus spp. (gram-positive) and P. gingivalis, Tforsythia, and T. denticola (gram-negative); and these bacteria are closely associated with, respectively, enamel and dentin pathologies (e.g. demineralizations or caries) and with periodontal disease [Citation63]. Recent papers have highlighted the complexity of periodontal disease etiology, with a special focus on the identity of bacteria which are responsible for this pathology [Citation64–Citation66]. Thus, authors have stated that the presence alone of specific micriobial species seems insufficient in causing gingivitis and periodontal disease, and that the change in biofilm equilibrium is another key factor in the development of these diseases [Citation64–Citation66]. Oral microbiota alterations registered in orthodontic patients appear to be consistent with the modifications occurring in patients with poor oral hygiene presenting gingivitis and/or periodontal diseases. In addition, orthodontic devices could represent a direct risk factor for periodontal diseases as they are often related to an increase in periodontopathogenic species [Citation24,Citation34,Citation43,Citation44,Citation48]. However, it seems reasonable to state that the susceptibility of each subject, as well as other factors that may alter the biofilm balance, may play a key role in determining the entity of periodontal sequelae.
Even though changes in the microbial system involve all types of orthodontic appliance, more rapid modifications occur during fixed orthodontic treatment. These alterations may be recorded even 1 month after the beginning of treatment and may lead to a decrease in patients’ periodontal health perception [Citation41]. Even so, as stated by Perinetti et al. [Citation41], the role of subgingival bacteria in periodontal modifications needs to be evaluated together with the action of enzymes activated in response to the stimuli of orthodontic forces.
If it is true that all appliances increase the bacterial component, it is also the case that mobile devices make minor changes as they are removable and can be completely cleaned, resulting in better oral hygiene minimizing retentive artifacts. It should also be emphasized that, of these appliances, the use of mouthguards is limited to a small population and they are carried only for limited periods of time, involving a less pathogenic effect.
Less devastating results from changes in the oral microbiota emerged from studies on functional appliances and on aligners, which are used up to 22 h a day [Citation61]. So, it seems more important to be able to remove the appliance and wash both it and the teeth rather than the length of time the device is worn.
In view of the changes in microbiota that occurred with the introduction of biomaterials into the oral cavity, and more specifically of the orthodontic devices, it would be appropriate for patients undergoing dedicated hygiene protocols to keep the oral bacterial charge under control and then to reduce the risk of the carious process and periodontal disease, as evidenced by various authors [Citation2,Citation67,Citation68].
Conclusions
The overall evidence quality level was moderate-to-high, thus significant conclusions could be drawn.
Orthodontic appliances significantly influence the oral microbiota, independent of appliance type.
Significant alterations of the microbiota were registered 1 month after the start of treatment.
Removable appliances had less impact on oral bacteria than fixed ones.
Personalized professional and daily hygiene protocols are recommended for orthodontic patients from the beginning of treatment.
Acknowledgments
We would like to thank: L. Bondemark, A.K. Holm, K. Hansen, S. Axelsson, B. Mohlin, V. Brattstrom, G. Paulin, and T. Pietila, who gave us a reference for the ‘SBU’ method and R. Burioni for his evaluable support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Alfuriji S, Alhazmi N, Alhamlan N, et al. The effect of orthodontic therapy on periodontal health: a review of the literature. IntJDent. 2014;2014:1.
- Migliorati M, Isaia L, Cassaro A, et al. Efficacy of professional hygiene and prophylaxis on preventing plaque increase in orthodontic patients with multibracket appliances: a systematic review. Eur JOrthod. 2015;37(3):297–22.
- Mattingly JA, Sauer GJ, Yancey JM, et al. Enhancement of Streptococcus mutans colonization by direct bonded orthodontic appliances. JDent Res. 1983;62(12):1209–1211.
- Sinclair PM, Berry CW, Bennett CL, et al. Changes in gingiva and gingival flora with bonding and banding. Angle Orthod. 1987;57(4):271–278.
- Freitas AO, Marquezan M, Nojima Mda C, et al. The influence of orthodontic fixed appliances on the oral microbiota: a systematic review. Dental Press J Orthod. 2014;19(2):46–55.
- Moher D, Liberati A, Tetzlaff J, et al. The PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Facey K, Topfer LA, Chan L. Health technology assessment (HTA) glossary. Sweden: INAHTA Secretariat, c/o SBU Stockholm; 2006.
- Bondemark L, Holm AK, Hansen K, et al. Long-term stability of orthodontic treatment and patient satisfaction. Angle Orthod. 2007;77(1):181–191.
- Al-Anezi SA. Dental plaque associated with self-ligating brackets during the initial phase of orthodontic treatment: a 3-month preliminary study. J Orthod Sci. 2014;3:7–11.
- Alves de Souza R, Borges de Araújo Magnani MB, Nouer DF, et al. Periodontal and microbiologic evaluation of 2 methods of archwire ligation: ligature wires and elastomeric rings. Am J Orthod Dentofacial Orthop. 2008;134(4):506–512.
- Arikan V, Kizilci E, Ozalp N, et al. Effects of fixed and removable space maintainers on plaque accumulation, periodontal health, Candidal and Enterococcus faecalis carriage. Med Princ Pract. 2015;24(4):311–317.
- Arab S, Nouhzadeh Malekshah S, Abouei Mehrizi E, et al. Effect of fixed orthodontic treatment on salivary flow, pH and microbial count. JDent (Tehran). 2016;13(1):18–22.
- Arslan SG, Akpolat N, Kama JD, et al. One-year follow-up of the effect of fixed orthodontic treatment on colonization by oral Candida. JOral PatholMed. 2008;37(1):26–29.
- Baka ZM, Basciftci FA, Arslan U. Effects of 2 bracket and ligation types on plaque retention: A quantitative microbiologic analysis with real-time polymerase chain reaction. Am J Orthod Dentofacial Orthop. 2013;144:260–267.
- Demling A, Demling C, Schwestka-Polly R, et al. Influence of lingual orthodontic therapy on microbial parameters and periodontal status in adults. Eur J Orthod. 2009;31(6):638–642.
- Demling A, Demling C, Schwestka-Polly R, et al. Short-term influence of lingual orthodontic therapy on microbial parameters and periodontal status. A Preliminary Study. Angle Orthod. 2010;80:480–484.
- D’Ercole S, Martinelli D, Tripodi D. Influence of sport mouthguards on the ecological factors of the children oral cavity. BMC Oral Health. 2014;14:97.
- Farhadian N, Usefi Mashoof R, Khanizadeh S, et al. Streptococcus mutans counts in patients wearing removable retainers with silver nanoparticles vs. those wearing conventional retainers: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2016;149(2):155–160.
- Forsberg CM, Brattström V, Malmberg E, et al. Ligature wires and elastomeric rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and Lactobacilli. Eur J Orthod. 1991;13(5):416–420.
- Van Gastel J, Teughels W, Quirynen M, et al. Longitudinal changes in gingival crevicular fluid after placement of fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2011;139(6):735–744.
- Ghijselings E, Coucke W, Verdonck A, et al. Long-term changes in microbiology and clinical periodontal variables after completion of fixed orthodontic appliances. Orthod Craniofac Res. 2014;17(1):49–59.
- Hägg U, Kaveewatcharanont P, Samaranayake YH, et al. The effect of fixed orthodontic appliances on the oral carriage of Candida species and Enterobacteriaceae. Eur J Orthod. 2004;26(6):623–629.
- Hernández-Solís SE, Rueda-Gordillo F, Flota-Alcocer AD, et al. Influence of orthodontic appliances on the occurrence of Candida spp. in the oral cavity. Rev Chilena Infectol. 2016;33(3):293–297. (Article in Spanish).
- Ireland AJ, Soro V, Sprague SV, et al. The effects of different orthodontic appliances upon microbial communities. Orthod Craniofac Res. 2014;17:115–123.
- Jurela A, Repic D, Pejda S, et al. The effect of two different bracket types on the salivary levels of S mutans and S sobrinus in the early phase of orthodontic treatment. Angle Orthod. 2013;83(1):140–145.
- Kim SH, Choi DS, Jang I, et al. Microbiologic changes in subgingival plaque before and during the early period of orthodontic treatment. Angle Orthod. 2012;82(2):254–260.
- Kupietzky A, Majumdar AK, Shey Z, et al. Colony forming unit levels of salivary Lactobacilli and Streptococcus mutans in orthodontic patients. J Clin Pediatr Dent. 2005;30(1):51–53.
- Lara-Carrillo E, Montiel-Bastida NM, Sánchez-Pérez L, et al. Changes in the oral environment during four stages of orthodontic treatment. Korean J Orthod. 2010;40(2):95–105.
- Lara-Carrillo E, Montiel-Bastida NM, Sánchez-Pérez L, et al. Effect of orthodontic treatment on saliva, plaque and the levels of Streptococcus mutans and Lactobacillus. Med Oral Patol Oral Cir Bucal. 2010;15(6):e924–9.
- Leung NM, Chen R, Rudney JD. Oral bacteria in plaque and invading buccal cells of young orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;130(6):698.e11-8.
- Levrini L, Mangano A, Montanari P, et al. Periodontal health status in patients treated with the Invisalign® system and fixed orthodontic appliances: a 3 months clinical and microbiological evaluation. Eur J Dent. 2015;9(3):404–410.
- Liu J, Bian Z, Fan MW, et al. Typing of mutans streptococci by arbitrarily primed PCR in patients undergoing orthodontic treatment. Caries Res. 2004;38(6):523–529.
- Lombardo L, Ortan YÖ, Gorgun Ö, et al. Changes in the oral environment after placement of lingual and labial orthodontic appliances. Prog Orthod. 2013;14:28.
- Maret D, Marchal-Sixou C, Vergnes JN, et al. Effect of fixed orthodontic appliances on salivary microbial parameters at 6 months: a controlled observational study. J Appl Oral Sci. 2014;22(1):38–43.
- Miura KK, Ito IY, Enoki C, et al. Anticariogenic effect of fluoride-releasing elastomers in orthodontic patients. Braz Oral Res. 2007;21(3):228–233.
- Nalçacı R, Özat Y, Çokakoğlu S, et al. Effect of bracket type on halitosis, periodontal status, and microbial colonization. Angle Orthodont. 2014;84:479–485.
- Pandis N, Papaioannou W, Kontou E, et al. Salivary Streptococcus mutans levels in patients with conventional and self-ligating brackets. Eur J Orthod. 2010;32(1):94–99.
- Paolantonio M, Festa F, di Placido G, et al. Site-specific subgingival colonization by Actinobacillus actinomycetemcomitans in orthodontic patients. Am J Orthod Dentofacial Orthop. 1999;115(4):423–428.
- Pejda S, Varga ML, Milosevic SA, et al. Clinical and microbiological parameters in patients with self-ligating and conventional brackets during early phase of orthodontic treatment. Angle Orthodont. 2013;83:133–139.
- Pellegrini P, Sauerwein R, Finlayson T, et al. Plaque retention by self-ligating vs elastomeric orthodontic brackets: quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence. Am J Orthod Dentofacial Orthop. 2009;135:426.e1-426.e9.
- Perinetti G, Paolantonio M, Serra E, et al. Longitudinal monitoring of subgingival colonization by Actinobacillus actinomycetemcomitans, and crevicular alkaline phosphatase and aspartate aminotransferase activities around orthodontically treated teeth. J ClinPeriodontol. 2004;31(1):60–67.
- Peros K, Mestrovic S, Anic-Milosevic S, et al. Salivary microbial and nonmicrobial parameters in children with fixed orthodontic appliances. Angle Orthodont. 2011;81(5):901–906.
- Ristic M, Vlahovic Svabic M, Sasic M, et al. Clinical and microbiological effects of fixed orthodontic appliances on periodontal tissues in adolescents. Orthod Craniofac Res. 2007;10:187–195.
- Ristic M, Vlahovic Svabic M, Sasic M, et al. Effects of fixed orthodontic appliances on subgingival microflora. Int J Dent Hyg. 2008;6:129–136.
- Sfondrini MF, Debiaggi M, Zara F, et al. Influence of lingual bracket position on microbial and periodontal parameters in vivo. JAppl Oral Sci. 2012;20(3):357–361.
- Shukla C, Maurya RK, Singh V, et al. Evaluation of changes in Streptococcus mutans colonies in microflora of the Indian population with fixed orthodontics appliances. DentResJ (Isfahan). 2016;13(4):309–314.
- Sudarević K, Jurela A, Repić D, et al. Oral health changes during early phase of orthodontic treatment. Acta Clin Croat. 2014;53:399–404.
- Thornberg MJ, Riolo CS, Bayirli B, et al. Periodontal pathogen levels in adolescents before, during, and after fixed orthodontic appliance therapy. Am J Orthod Dentofacial Orthop. 2009;135(1):95–98.
- Topaloglu-Ak A, Ertugrul F, Eden E, et al. Effect of orthodontic appliances on oral microbiota—6 month follow-up. JClin Ped Dent. 2011;35(4):433–436.
- Torlakovic L, Paster BJ, Øgaard B, et al. Changes in the supragingival microbiota surrounding brackets of upper central incisors during orthodontic treatment. Acta Odontol Scand. 2013;71(6):1547–1554.
- Turkkahraman H, Sayın MO, Bozkurt FY, et al. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthodont. 2005;75:231–236.
- Türköz C, Canigür Bavbek N, Kale Varlik S, et al. Influence of thermoplastic retainers on Streptococcus mutans and Lactobacillus adhesion. Am J Orthod Dentofacial Orthop. 2012;141(5):598–603.
- Uzuner FD, Kaygisiz E, Cankaya ZT. Effect of the bracket types on microbial colonization and periodontal status. Angle Orthodont. 2014;84:1062–1067.
- Wichelhaus A, Brauchli L, Song Q, et al. Prevalence of Helicobacter pylori in the adolescent oral cavity: dependence on orthodontic therapy, oral flora and hygiene. J Orofac Orthop. 2011;72(3):187–195.
- Zheng Y, Li Z, He X. Influence of fixed orthodontic appliances on the change in oral Candida strains among adolescents. JDent Sci. 2014;11(1):17–22.
- Ortu E, Sgolastra F, Barone A, et al. Salivary Streptococcus Mutans and Lactobacillus spp. levels in patients during rapid palatal expansion. Eur J Paediatr Dent. 2014;15(3):271–274.
- Shukla C, Maurya R, Singh V, et al. Evaluation of role of fixed orthodontics in changing oral ecological flora of opportunistic microbes in children and adolescent. J Indian Soc Pedod Prev Dent. 2017;35(1):34–40.
- Øilo M, Bakken V. Biofilm and dental biomaterials. Materials. 2015;8:2887–2890.
- Antonelli G, Clementi M, Pozzi G, et al. Principi di microbiologia medica. II ed. Milano: Casa Editrice Ambrosiana; 2012.
- Hall MW, Singh N, Ng KF, et al. Inter-personal diversity and temporal dynamics of dental, tongue, and salivary microbiota in the healthy oral cavity. NPJ Biofilms Microbiomes. 2017 Jan 26;3:2.
- Rossini G, Parrini S, Castroflorio T, et al. Periodontal health during clear aligners treatment: a systematic review. Eur J Orthod. 2015;37(5):539–543.
- Lindhe J, Lang NP. Parodontologia clinica e implantologia orale. IV ed. Milano: Edi-Ermes; 2016.
- Wong BK, McGregor NR, Butt HL, et al. Association of clinical parameters with periodontal bacterial haemolytic activity. JClin Periodontol. 2016;43(6):503–511.
- Larsen T, Fiehn NE. Dental biofilm infections – an update. APMIS. 2017;125:376–384.
- Vieira Colombo AP, Magalhães CB, Hartenbach FA, et al. Periodontal-disease-associated biofilm: a reservoir for pathogens ofmedical importance. Microb Pathog. 2016;94:27–34.
- Sanz M, Beighton D, Curtis MA, et al. Role of microbial biofilms in the maintenance of oral health and in the development of dental caries and periodontal diseases. Consensus report of group 1 of the Joint EFP/ORCA workshop on the boundaries between caries and periodontal disease. J Clin Periodontol. 2017;44(Suppl 18):S5–S11.
- Lucchese A, Gherlone E. Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances. EurJOrthod. 2013;35:664–668.
- Hamdan AM, Maxfield BJ, Tufekci E, et al. Preventing and treating white-spot lesions associated with orthodontic treatment: a survey of general dentists and orthodontists. J Am Dent Assoc. 2012;143(7):777–783.