ABSTRACT
Aim: The aim of this study was to compare the subgingival microbiota of people with Alzheimer´s disease (AD), mild cognitive impairment (MCI), subjective cognitive decline (SCD) and cognitively healthy individuals.
Materials and methods: The study population was recruited from 2013 to 2017 and comprised 132 cases recently diagnosed with AD (n = 46), MCI (n = 40) or SCD (n = 46), and 63 cognitively healthy controls. Subgingival samples were collected, and the microbiotas were characterized by 16S rRNA gene sequencing.
Results: The relative abundance of the ten most common genera did not differ between the cases and control groups. However, the microbial richness and evenness were higher in cases than in controls and differed across the four groups. The variables with the greatest influence on the microbial community composition were related to periodontal disease followed by body mass index, study group affiliation and smoking. Ten taxa exhibited significant differences between case participants and controls. Two Operational Taxonomic Units were particularly abundant in AD compared to controls: Slackia exigua, which was also associated with deep periodontal pockets, and a Lachnospiraceae [G-7] bacterium.
Conclusion: It is concluded that in individuals with cognitive impairment or AD, the subgingival microbiota exhibits shifts typical of periodontal disease.
Introduction
Alzheimer´s disease (AD) is the most prevalent of the dementia disorders and leads to multidomain cognitive dysfunction [Citation1]. The mechanisms underlying AD pathophysiology, leading to brain atrophy and impaired cognitive functions, are not fully understood [Citation2]. Despite considerable progress in identifying dementia risk factors in recent years [Citation3], much of the risk remains unexplained. Preventive healthcare may lead to a reduction in dementia incidence [Citation4]. Thus, the identification of modifiable risk factors and preventive factors relevant to dementia can have important public health implications.
Whether infectious agents represent a true causal effect in AD aetiology has been debated for several decades [Citation5]. Recently, it has been proposed that perturbations or alterations of the intestinal microbiome play a role in AD development [Citation6]. Changes in the gut microbial community may alter the permeability of the gut barrier and induce systemic inflammation through several different pathways [Citation7].
Periodontitis, a complex chronic oral inflammatory disease, has been associated with dementia in observational and experimental studies [Citation8]. The distinctive pathological features of periodontitis are inflammation of the periodontal tissues and subgingival microbiota dysbiosis [Citation9,Citation10]. Both components drive disease progression, eventually leading to loss of tooth-supporting tissues and ultimately to loss of teeth [Citation11]. It has been demonstrated that transmission and colonisation of oral bacteria can be extensive and can influence the gut microbiota [Citation12]. Indeed, the oral cavity is the starting point of the gastrointestinal tract. Moreover, in a number of studies Porphyromonas gingivalis, a bacterium associated with periodontitis, has been implicated in dementia [Citation13,Citation14]. It has been suggested that P. gingivalis is capable of modulating the gut microbiome [Citation15].
The aim of the present study was to compare the subgingival microbiota in individuals with cognitive dysfunction and in cognitively healthy individuals. We hypothesized that differences in the subgingival microbiota exist between individuals with and without cognitive dysfunction.
Materials and methods
Study design
This explorative study of the human oral subgingival microbiota was based on biological samples and data collected as part of a recent case-control study, conducted in Sweden from 2013 to 2017. The study design and preliminary findings have been published previously [Citation16]. Critical components of relevance relating to this investigation are outlined in the following section. The study is reported in compliance with the STROME-ID Statement guidelines [Citation17]. Ethical approval was obtained from the Regional Ethical Review Board in Stockholm (2012/652–31/1). The study conforms to institutional and international (Declaration of Helsinki) standards. Written informed consent was obtained from all participants.
Data collection
The study population comprised 154 case participants (50–80 years old) diagnosed with AD (n = 52), mild cognitive impairment (MCI [n = 51]) or subjective cognitive decline (SCD [n = 51]); 76 individuals served as cognitively healthy controls. Case participants were enrolled from the Karolinska Memory Clinic at the Karolinska University Hospital in Huddinge, Sweden, after diagnosis at a multidisciplinary consensus conference, using diagnostic data from an extensive medical and neurocognitive assessment. Diagnostic criteria for AD were mainly based on the NIA-AA diagnostic guidelines due to probable AD [Citation18]. MCI diagnosis was set in accordance with the Winblad criteria [Citation19] and for SCD the pre-MCI SCD criteria were used [Citation20].
Controls were frequency-matched for age and sex, identified and enrolled from the population register in Huddinge, Sweden. To be considered eligible, the controls were required not to have sought medical attention for memory loss or experienced memory loss. In addition, controls underwent cognitive screening (excluded if < 28 on the Mini-Mental State Examination [MMSE] test and/or if failing the clock-drawing test [CDT]) before inclusion.
The following exclusion criteria were applied to all participants, i.e. case participants and controls alike: severe medical conditions i.e. brain tumours, clinically significant liver, kidney or lung dysfunction, chronic inflammatory disease and psychiatric diseases [Citation16]. All study participants completed a questionnaire about personal data (medical, dental, financial, educational information etc.).
Following case inclusion and control recruitment, all participants underwent a dental examination at the Department of Dental Medicine, Karolinska Institutet, Huddinge, Sweden. The dental examination comprised a comprehensive assessment of the oral soft and hard tissues including a periodontal examination and a panoramic radiograph using a ProMax® (Planmeca Oy, Helsinki, Finland) according to a standard protocol. Probing pocket depth (PPD) was measured in millimeters using a periodontal probe (UNC 15, Hu-Friedy, Chicago, IL) at six sites on all existing teeth. Bleeding on pocket probing (BoP) was also recorded at six sites on all existing teeth. Radiographically verified marginal alveolar bone loss was classified in the following manner: no/mild (loss of supporting bone < 1/3 of the root length), localized (loss of supporting bone tissue ≥ 1/3 the root length in < 30% of the teeth) or generalized (loss of supporting bone tissue ≥ 1/3 the root length in ≥30% of the teeth). The variable PPD ≥ 6 mm was defined as having ≥1 site with PPD of ≥6 mm.
After completion of the periodontal examination, the deepest or the most representative periodontal pocket was selected in each quadrant for subgingival microbial sampling. One sample was collected per quadrant. If no teeth or dental implants were present in the quadrant, no sample was collected. The quadrant to be sampled was isolated with cotton rolls/pads and a saliva ejector. Supragingival plaque was carefully removed at the selected sampling site using a sterile curette, leaving the subgingival dental biofilm undisturbed. All samples were taken with a new individual sterile curette with a single pull, in a coronal direction, from the base of the periodontal pocket. The procedure was repeated in all four quadrants. The samples were pooled in 1.5 mL microcentrifuge tubes (Thermo Fisher Scientific®) containing PCR grade water (Roche®) and stored at −80°C until further processing.
Sample processing and microbiome profiling
DNA extraction, PCR amplification and sequencing of the V3-V4 regions of the 16S rRNA gene were undertaken at the DNA Sequencing and Genomics Laboratory of the Institute of Biotechnology, University of Helsinki, following a previously published protocol [Citation21] and primers [Citation22]. Dual-indexes, selected with BARCOSEL [Citation23], were added to samples in the second PCR step. All samples were combined in a single pool and sequenced twice with Illumina MiSeq (paired-end; read lengths: forward: 326; reverse: 278).
The raw data consisted of 35, 171, 514 sequence reads, which are available in the European Nucleotide Archive (accession: PRJEB35923). Primers were trimmed from reads with cutadapt (v. 1.8.3 [Citation24]). Further quality control, taxonomic classification and Operational Taxonomic Unit (OTU; a computational equivalent to species) clustering were undertaken with mothur [Citation25] following the standard operating procedure (SOP) for MiSeq data [Citation26,Citation27]Citation40. The reference databases were Silva (v. 132) for alignment and HOMD (v. 15.1 [Citation28]) for taxonomy. Singleton sequences were removed from data during the mothur analysis.
Statistical data analysis
Statistical analysis of clinical data was undertaken in Stata (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC). The limit for statistical significance was set at 5%. Contingency tables were created to explore frequency distribution of case participants and controls in categories of demographic, socioeconomic and dental variables. Intergroup comparisons were determined by a chi-squared test or Fisher’s exact test for categorical variables and Mann-Whitney test or Kruskall-Wallis test for continous variables.
Statistical analyses involving microbial data were performed in R (v. 3.6.2; R Core Team, 2019). OTUs with fewer than six sequence reads in the entire data were removed. The R package decontam (v. 1.6.0 [Citation29]) was used for detecting contaminant taxa, making use of negative control samples; the contaminants and control samples were trimmed out. Samples with a low number of sequence reads (<24,000), or an unusually high number of sequence reads (>120,000) were also trimmed out. After these steps, the final number of good quality sequences was 16, 048, 390 (mean ± SD: 77, 528 ± 20, 889 per sample).
Phyloseq (v. 1.30.0 [Citation30]) was used for data management and calculating alpha diversity measures (observed richness and Shannon index). Alpha diversity comparisons included Kruskal-Wallis tests (initial testing for categorical variables), Pearson correlations (initial testing for continuous variables), Wilcoxon rank-sum tests (post hoc testing between diagnostic groups) and linear regression (combined model with multiple variables). The R package vegan (v. 2.5–6 [Citation31]) was used for beta diversity analysis: contrasting Bray-Curtis dissimilarities with PERMANOVA and visualization with non-metric multidimensional scaling (NMDS). All diversity comparisons were run on microbiota data subsampled to the smallest number of reads in a sample (24 275).
Differences in abundance of specific bacterial taxa were tested with DESeq2 ([v. 1.26.0 [Citation32]) focusing on OTUs, genera and families that had more than one read in more than one fourth of the samples. All case participants versus controls (two study groups) and diagnostic case subgroups versus controls (all four study groups) were tested with adjustment for age, body mass index (BMI) and PPD ≥ 6. Current smokers (n = 12) were excluded from the DESeq2 comparisons.
The purpose of the study was not to describe the microbiota in periodontitis. Since PPD ≥ 6 mm was found to be the most influential clinical measure on subgingival microbial diversity, we used this variable as a proxy for periodontal health status.
Results
Clinical features of the study population
After a careful quality control, the final study sample in this analysis comprised 195 (84.8% of the original population) participants (63 controls and 132 case participants) with complete subgingival microbiome information (). The diagnostic case subgroups comprised participants diagnosed with AD (n = 46), MCI (n = 40) or SCD (n = 46). Six participants had both dental implants and teeth sites sampled. The reasons for exclusion were a low number of sequence reads (n = 17), an unusually high number of sequence reads (n = 10), edentulousness (n = 1), or fewer than four sampling sites (n = 7).
Figure 1. Flow chart demonstrating selection of study participants. Note: AD: Alzheimer´s disease. MCI: Mild cognitive impairment. SCD: Subjective cognitive decline
Demographic, socioeconomic and clinical data for the participants are presented in (). The median age of cases was 66 years (interquartile range [IQR] 12) and for controls 69 years (IQR 9). The median age of diagnostic case subgroups was: AD 71 (IQR 11), MCI 70 (IQR 10) and SCD 61 years (IQR 7). Proportion of males was 49.2% among cases and 44.4% among controls and ranged between 45.7% and 52.5% in diagnostic case subgroups. Annual income, marital status, diabetes status, medications, and smoking habits did not differ between cases and controls. However, the control group had higher BMI compared with the cases. The case participants had more often sites with PPD ≥ 6 mm and BoP, and an increased prevalence of marginal alveolar bone loss.
Table 1. Distribution of demographic, socioeconomic and clinical characteristics
Microbial diversity
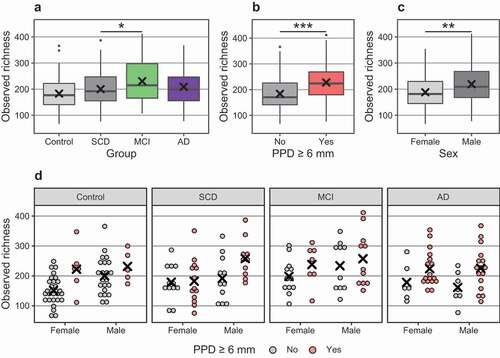
The richness and evenness of the microbial communities (alpha diversity) were estimated by using observed richness (number of OTUs) and Shannon index (). By using either index, diversity was higher in cases than in controls (p = 0.008 and p = 0.010) and differed across the four groups (p = 0.018 and p = 0.002). As seen in ()), the subgingival microbiome was especially rich with a high diversity among participants with MCI. Among the possible confounders, alpha diversity (both indices) was higher in males than in females, and observed richness was higher in participants with PPD ≥ 6 mm (; )). The association between alpha diversity and cognitive dysfunction was examined by using a linear regression model (Table S1). Male sex and PPD ≥ 6 mm were positive predictors of alpha diversity (Table S1; ) also in these analyses. However, even after adjusting for sex and presence of PPD ≥ 6 mm, MCI was significantly (p = 0.014) associated with alpha diversity (Table S1).
Table 2. P-values for differences in microbial alpha and beta diversity measures between variables of interest and potential confounders
Figure 2. Differences in observed richness (number of detected bacterial OTUs) between groups. Note: x: mean. In boxplots, box hinges: 1st and 3rd quartiles, whiskers: box hinge to 1.5 * interquartile range. (a). Controls and diagnostic subgroups; (b). PPD ≥ 6 mm; (c). Sex; (d). Diagnostic subgroups, sex and PPD ≥ 6 mm
Differences in the microbial community composition (beta diversity) between the study groups were analysed using PERMANOVA. The differences were significant both between cases and controls (p = 0.014) and across the four groups (p = 0.041) (; ). Among the possible confounders, beta diversity differed most between the participants with or without PPD ≥ 6 mm (p < 0.001; Figure S1), but also between participants with different education levels, BMI or smoking habits. The association of beta diversity with cognitive dysfunction was further investigated with confounder-corrected models (Table S2). Also, in these analyses, BMI, smoking and PPD ≥ 6 were all associated with beta diversity (Table S2). However, after adjusting for possible confounders, the study group affiliation was associated with beta diversity (p = 0.030).
Figure 3. Non-metric multidimensional scaling plots based on Bray-Curtis dissimilarity. Each point corresponds to one participant; the closer the points, the more similar their samples. Ellipses represent 95% confidence intervals. (a). Colors and shapes for diagnostic case subgroups groups, ellipses for study group affiliation (all cases and controls). (b). Plot split by PPD ≥ 6 mm, with colors and shapes for diagnostic case subgroups and ellipses for study group affiliation (all cases and controls)

Specific bacterial taxa
Cognitive dysfunction
The relative abundance of the detected subgingival bacteria was analysed next. The most common genera in the whole population were Fusobacterium, Porphyromonas, Capnocytophaga, Treponema, Prevotella, Campylobacter and Streptococcus, and their profiles did not differ between cases and controls ().
Table 3. Relative abundance (%, mean ± SD) for the ten most common bacterial genera in groups of participants
The package DESeq2 was applied to further search for intergroup differences in OTUs, genera and families. After adjustment for age, BMI and PPD ≥ 6 mm, ten taxa differed significantly in abundance between case participants and controls (Table S3). Most notable among the OTUs, Rothia aeria (log2 fold change: −2.68, p < 0.001), Corynebacterium durum (log2 fc: −2.35, p < 0.001) and several members of Actinomyces genus (log2 fc: −1.56 − −1.04, p < 0.05) were more abundant in controls than in case participants. Only Prevotella oulorum (log2 fc: 1.80, p < 0.001) was more abundant in case participants than in controls. Similar differences were observed when the AD group was compared to controls. Moreover, two OTUs were specifically more abundant in the AD group than in controls: Slackia exigua (log2 fc: 2.80, p = 0.019), which was also associated with PPD ≥ 6 mm, and Lachnospiraceae [G-7] bacterium (log2 fc: 5.78, p < 0.001) (Table S3A).
The results at the family level were similar to the genus and OTU levels; for example, the family Actinomyces was less common in AD than in control participants (Table S3A).
Periodontal conditions
Subjects with PPD ≥ 6 mm had a higher abundance of 15 genera and a lower abundance of 13 genera (Figure S2, Table S3B). Among participants with PPD ≥ 6 mm, the highest log2-fold changes were identified for Porphyromonas (log2 fc: 2.80, p < 0.001) and Peptostreptococcaceae [XI] [G-5] (log2 fc: 2.52, p = 0.034). A total of 29 different OTUs were elevated in subjects with PPD ≥ 6 mm and the highest log2-fold changes were for P. gingivalis (log2 fc: 3.79, p < 0.001) and Prevotella intermedia (log2 fc: 2.55, p = 0.028). Several OTUs occurred less frequently in participants with PPD ≥ 6 mm than in those without, especially Actinomyces massiliensis (log2 fc: −2.12, p < 0.001), Haemophilus parainfluenzae (log2 fc: −2.08, p < 0.001), and Streptococcus mutans (log2 fc: −1.77, p = 0.021) (Table S3).
Discussion
This study was undertaken in order to investigate the subgingival microbiota in persons with cognitive dysfunction (i.e. AD, MCI and/or SCD) in comparison with cognitively healthy controls. Overall, moderate intergroup differences emerged. Confounder-corrected models suggested that using either alpha or beta diversity measures, the cognitive dysfunction is a significant determinant of subgingival microbial composition and it is associated with higher microbial richness. In addition, the abundance of ten taxa differed significantly between case participants and controls.
However, the strongest determinant of the microbial diversity was periodontal disease, i.e. PPD ≥ 6 mm. This pathology was associated with a higher alpha diversity, observed richness and abundance of typical periodontitis-associated genera. These findings are in accordance with earlier studies [Citation9]. The subgingival compartment is a highly specific niche in which the microbiota is to a large extent influenced by periodontal disease [Citation33]. Prior studies have described the oral microbiota of the elderly, showing that age is associated with shifts in the microbiota [Citation34]. In the present study, Actinomyces and Rothia were more common among controls with healthier periodontal status than in the diagnostic subgroup of AD with poorer periodontal status. The result is in accordance with earlier reports of an association between periodontal health and a greater abundance of Actinomyces and Rothia [Citation9,Citation35].
There is little published research on the subgingival microbiome in relation to cognitive function and dementia. One cross-sectional study using 16S rRNA gene sequencing reported an association between impaired cognitive function and alterations in the subgingival microbiome [Citation36]. Although the small sample size and study design precluded generalizable conclusions, the results suggested that there are consistent alterations in the microbiota among participants with dementia compared with those without dementia. An interesting finding in the present study is the increased abundance of Lachnospiraceae. This taxon has also been shown to be increased in the gut microflora of AD patients [Citation37] and to associate with several inflammatory conditions, such as metabolic syndrome, obesity, diabetes, liver diseases, inflammatory bowel disease and chronic kidney disease [Citation38].
Studies using other approaches to detect microbial signatures have shown that increased systemic levels of antibodies against specific periodontal pathobionts are associated with impaired cognitive function. In a large study, individuals with the highest serum P. gingivalis antibody levels were at increased risk of impaired cognitive function [Citation14]. A study analysing postmortem brain tissue reported that P. gingivalis lipopolysaccharides (LPS) could reach the brain [Citation39]. Also, spirochetes, especially Treponema species, have been implicated in AD pathogenesis [Citation40]. In our previous study, we showed that signs of periodontal disease were more common in the case groups, especially the AD group [Citation16]. In the present study, PPD ≥ 6 mm was associated with several OTUs representing established periodontal pathogens, such as P. gingivalis, Tannerella forsythia, Treponema denticola and P. intermedia. This provides support that these bacteria are linked with AD. Future studies will show whether oral dysbiosis, dysfunctional host response or both, contribute to AD risk.
In interpreting the results of this study, several limitations should be considered. As periodontal disease was more common in case participants than in controls, an independent association between cognitive impairment and microbial signatures cannot be determined. In order to distinguish microbial signatures more readily, future microbial surveys exploring the subgingival microbiota in AD should aim to recruit participants in whom the periodontitis burden is more evenly distributed. Furthermore, the participants were recruited irrespective of smoking status or previous antibiotic or periodontal treatment, all of which have profound impact on the subgingival microbiota [Citation41]. Another limitation is the sampling method. Subgingival samples were obtained using curette sampling from the deepest periodontal pockets. This does not result in a quantitative sample representing all subgingival microbiota. However, different methods for subgingival sampling seem to show good agreement [Citation42].
Conclusion
The results provide evidence for differences in the subgingival microbiota between individuals with cognitive dysfunction and cognitively healthy individuals. The alterations are mainly attributable to the higher prevalence of periodontal disease in the groups with different degrees of cognitive dysfunction. Altogether, these findings are of relevance to our understanding of the association between periodontal disease and cognitive dysfunction.
Conflict of interest
None of the authors reports conflicts of interest related to this study.
Supplemental Material
Download Zip (566.8 KB)Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Prince M, Comas-Herrera A, Knapp M, et al. (2016). World Alzheimer report 2016 improving healthcare for people living with dementia: coverage, quality and costs now and in the future. Alzheimer’s Disease International (ADI), 1–8. Retrieved from https://www.alz.co.uk/research/world-report–2016
- Scheltens P, Blennow K, Breteler MMB, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–517.
- Imtiaz B, Tolppanen AM, Kivipelto M, et al. Future directions in Alzheimer’s disease from risk factors to prevention. Biochem Pharmacol. 2014;88(4):661–670.
- Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10(9):819–828.
- Panza F, Lozupone M, Solfrizzi V, et al. Time to test antibacterial therapy in Alzheimer’s disease. Brain. 2019. DOI:https://doi.org/10.1093/brain/awz244
- Sochocka M, Donskow-Łysoniewska K, Diniz BS, et al. The gut microbiome alterations and inflammation-driven pathogenesis of Alzheimer’s disease—a critical review. Mol Neurobiol. 2019;56(3):1841–1851.
- Kowalski K, Mulak A. Brain-gut-microbiota axis in Alzheimer’s disease. J Neurogastroenterol Motil. 2019;25(1):48–60.
- Kamer AR, Craig RG, Niederman R, et al. Periodontal disease as a possible cause for Alzheimer’s disease. Periodontol 2000. 2020;83(1):242–271.
- Abusleme L, Dupuy AK, Dutzan N, et al. The subgingival microbiome in health and periodontitis and its relationship with community biomass and inflammation. ISME J. 2013;7(5):1016–1025.
- Hong BY, Araujo MVF, Strausbaugh LD, et al. Microbiome profiles in periodontitis in relation to host and disease characteristics. PLoS ONE. 2015;10(5):1–14.
- Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:1–14.
- Schmidt TSB, Hayward MR, Coelho LP, et al. Extensive transmission of microbes along the gastrointestinal tract. Elife. 2019;8. DOI:https://doi.org/10.7554/eLife.42693.
- Kamer AR, Craig RG, Pirraglia E, et al. TNF-alpha and antibodies to periodontal bacteria discriminate between Alzheimer’s disease patients and normal subjects. J Neuroimmunol. 2009;216(1–2):92–97.
- Noble JM, Scarmeas N, Celenti RS, et al. Serum IgG antibody levels to periodontal microbiota are associated with incident alzheimer disease. PLoS ONE. 2014;9(12):1–14.
- Olsen I, Yamazaki K. Can oral bacteria affect the microbiome of the gut? J Oral Microbiol. 2019;11(1):1586422.
- Holmer J, Eriksdotter M, Schultzberg M, et al. Association between periodontitis and risk of Alzheimer′s disease, mild cognitive impairment and subjective cognitive decline: A case–control study. J Clin Periodontol. 2018;45(11):1287–1298.
- Field N, Cohen T, Struelens MJ, et al. Strengthening the reporting of molecular epidemiology for infectious diseases (STROME-ID): an extension of the STROBE statement. Lancet Infect Dis. 2014;14(4):341–352.
- McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia. 2011;7(3):263–269.
- Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment–beyond controversies, towards a consensus: report of the international working group on mild cognitive impairment. J Intern Med. 2004;256(3):240–246.
- Jessen F. Subjective and objective cognitive decline at the pre-dementia stage of Alzheimer’s disease. Eur Arch Psychiatry Clin Neurosci. 2014;264(1):3–7.
- Pereira PAB, Aho VTE, Paulin L, et al. Oral and nasal microbiota in Parkinson’s disease. Parkinsonism Related Disord. 2017;38:61–67.
- Aho VTE, Pereira PAB, Voutilainen S, et al. Gut microbiota in Parkinson’s disease: temporal stability and relations to disease progression. EBioMedicine. 2019;44:691–707.
- Somervuo P, Koskinen P, Mei P, et al. BARCOSEL: A tool for selecting an optimal barcode set for high-throughput sequencing. BMC Bioinf. 2018;19(1):4–9.
- Martin M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J. 2011;17(1):10.
- Schloss PD, Westcott SL, Ryabin T, et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl Environ Microbiol. 2009;75(23):7537–7541.
- Kozich JJ, Westcott SL, Baxter NT, et al. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the miseq illumina sequencing platform. Appl Environ Microbiol. 2013;79(17):5112–5120.
- Mothur MiSeq SOP [Internet]. [cited 2018 Mar 18]. Available from: https://www.mothur.org/wiki/MiSeq_SOP
- Chen T, Yu WH, Izard J, et al. The human oral microbiome database: a web accessible resource for investigating oral microbe taxonomic and genomic information. Database J Bio Databases Curation. 2010;2010:1–10.
- Davis NM, Proctor DM, Holmes SP, et al. Simple statistical identification and removal of contaminant sequences in marker-gene and metagenomics data. Microbiome. 2018;6(1):1–39.
- McMurdie PJ, Holmes S. Phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE. 2013;8(4):e61217.
- Oksanen J, Blanchet FG, Friendly M, et al. Vegan: community ecology package. R Package Version. 2019;2:5–6.
- Love MI, Huber W, Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15(12):1–21.
- Bosshardt DD. The periodontal pocket: pathogenesis, histopathology and consequences. Periodontol 2000. 2017;76:43–50.
- Feres M, Teles F, Teles R, et al. The subgingival periodontal microbiota of the aging mouth. Periodontol 2000. 2016;72(1):30–53.
- Griffen AL, Beall CJ, Campbell JH, et al. Distinct and complex bacterial profiles in human periodontitis and health revealed by 16S pyrosequencing. ISME J. 2012;6(6):1176–1185.
- Cockburn AF, Dehlin JM, Ngan T, et al. High throughput DNA sequencing to detect differences in the subgingival plaque microbiome in elderly subjects with and without dementia. Investig Genet. 2012;3(1):19.
- Vogt NM, Kerby RL, Dill-McFarland KA, et al. Gut microbiome alterations in Alzheimer’s disease. Sci Rep. 2017;7(1):1–11.
- Vacca M, Celano G, Calabrese FM, et al. The controversial role of human gut lachnospiraceae. Microorganisms. 2020;8(4):1–25.
- Poole S, Singhrao SK, Kesavalu L, et al. Determining the presence of periodontopathic virulence factors in short-term postmortem Alzheimer’s disease brain tissue. J Alzheimers Dis. 2013;36(4):665–677.
- Miklossy J. Alzheimer’s disease - a neurospirochetosis. analysis of the evidence following Koch’s and Hill’s criteria. J Neuroinflammation. 2011;8(1):90.
- Mason MR, Preshaw PM, Nagaraja HN, et al. The subgingival microbiome of clinically healthy current and never smokers. ISME J. 2015;9(1):268–272.
- Jervøe-Storm P-M, AlAhdab H, Koltzscher M, et al. Comparison of curet and paper point sampling of subgingival bacteria as analyzed by real-time polymerase chain reaction. J Periodontol. 2007;78(5):909–917.
