Abstract
Studies on the impact of cleft palate surgery on speech with stringent methodology are called for, since we still do not know the best timing or the best method for surgery. The purpose was to report on speech outcome for all Swedish-speaking 5-year-olds born with a non-syndromic unilateral cleft lip and palate (UCLP), in 2008–2010, treated at Sweden’s six cleft palate centres, and to compare speech outcomes between centres. Speech was assessed in 57 children with percent consonants correct adjusted for age (PCC-A), based on phonetic transcriptions from audio recordings by five independent judges. Also, hypernasality and perceived velopharyngeal function were assessed. The median PCC-A for all children was 93.9, and medians in the different groups varied from 89.9 to 96.8. In the total group, 9 children (16%) had more than mild hypernasality. Twenty-two children (38.5%) were perceived as having competent/sufficient velopharyngeal function, 25 (44%) as having marginally incompetent/insufficient velopharyngeal function, and 10 children (17.5%) as having incompetent/insufficient velopharyngeal function. Ten children were treated with secondary speech improving surgery and/or fistula surgery. No significant differences among the six groups, with eight to ten children in each group, were found. The results were similar to those in other studies on speech of children with UCLP, but poorer than results in normative data of Swedish-speaking 5-year-olds without UCLP. Indications of differences in frequency of surgical treatment and speech treatment between centres were observed.
Keywords:
Introduction
National and international efforts to evaluate the effect of cleft palate surgery on speech are still called for since we do not know the best timing or the best method for surgery [Citation1–4]. Several authors have emphasized it is of the utmost importance that research on speech outcomes related to cleft palate surgery utilizes stringent methodology, in terms of always making assessments from audio or video recordings, using standardized speech stimulus and more than one listener for assessment, reporting results on reliability, and not mixing different types of clefts and ages [Citation2,Citation5–7]. Without this stringency in research methodology, one cannot draw conclusions on best practice of intervention.
This is the first article to report on speech outcome for children with unilateral cleft lip and palate (UCLP) at 5 years of age, in a prospective longitudinal intercentre study including all cleft lip and palate (CLP) centres in Sweden. In Sweden, about 200 children are born with cleft palate ± lip every year [Citation8]. The teams are multidisciplinary, and each of the six centres covers a regional area. All children are referred to the regional centre soon after birth, and followed up until the age of 19 with few families dropping out. The cleft surgery is carried out according to different methods at the centres. Currently, the cleft in the palate is closed in either one stage at 9–12 months or at ∼18 months, or in two stages, with soft palate closure at ∼6 months of age and hard palate closure at about 24 months. The age of 5 years is important for follow-up of speech, since our goal is good speech at the start of school at 6 years of age. We also know that typically developing children have mostly developed adult-like speech at the age of 5 years, except for simplification of /r/ and /s/ [Citation9]. Therefore, in Sweden, 5 years of age has been agreed on for follow-up at all CLP centres.
At 4–5 years of age, 50–60% of the children with cleft palate ± lip can be expected to have good speech, and the group with isolated cleft palate to have better results than groups with other cleft types [Citation10–12]. Two large studies on UCLP speech outcomes at 5 years of age have been published recently: The Cleft Care UK study including 248 children [Citation4], and the Scandcleft trials including 448 children [Citation2,Citation3]. In the Cleft Care UK, 10% presented with hypernasality [Citation13], and about 25% had a history of secondary VPI surgery [Citation4]. The rate of hypernasality in the Scandcleft trials was 22–45%, and no significant differences between the three local surgical methods were found [Citation2]. The surgical methods included a one-stage surgery and different timing and sequence of two-stage surgeries of the palate. The rate of pharyngeal flaps performed before 5 years of age varied between 0 and 23% [Citation2]. In earlier Swedish studies, 18–40% of the 5-year-olds with UCLP have been reported with moderate to severe hypernasality and 0–17% had a history of secondary VPI surgery [Citation12,Citation14–16].
In the Scandcleft trials, the median score for correct articulation in a restricted word list in the total group was 80% [Citation3]. The only statistically significant difference related to surgical method, was between two surgical methods within the same centre, with poorer results after hard palate closure at 36 months of age than at 12 months. In the Cleft Care UK study, no score of correct articulation was reported, but almost 15% of children had posterior articulation pattern (backed to velar/uvular) and 10% had non-oral articulation [Citation13]. In the most recent Swedish study, the median of percent consonants correct adjusted for age (PCC-A) was 97% and the median of non-oral errors 0% [Citation12].
Other factors than the cleft might influence speech outcome, e.g. hearing [Citation17]. Tengroth et al. [Citation18] showed that 24% of 33 Swedish children with UCLP had hearing threshold levels >20 dB on frequencies of 500, 1000, 2000 and 4000 Hz, at 4–7 years of age. The possible negative impact of hearing on speech has been discussed [Citation19], and hearing needs to be taken into account when reporting speech outcome in children with cleft palate. Furthermore, little evidence has been found to support any specific intervention of speech-language therapy in children with cleft palate ± lip [Citation20].
Participation in international multicentre studies, such as the randomized controlled trials Scandcleft [Citation2,Citation3] and TOPS [Citation21], has resulted in the Swedish CLP centres having the same recording equipment available for research. On the basis of previous studies, including the Cleft Care UK Study [Citation4,Citation13], it was decided to perform a Swedish intercentre study. The purpose of the study was to report on speech outcome for all Swedish 5-year-olds born with a non-syndromic UCLP during the time period of 2008–2010, and to make comparisons of speech outcome between the six different CLP centres.
Material and methods
The study was prospective and approved by the Regional Ethics Committee in Stockholm (Reference number: 2012/1991-31/3).
Participants
The aim was to recruit a consecutive series of 10 children with complete UCLP, born 2008–2010, from each of the six Swedish CLP centres, in conjunction with the routine 5-year follow-up. The included children were native Swedish-speakers and had no known additional malformations or syndromes. The children were not examined by any clinical geneticist. A total of 57 children were included: from Gothenburg 10 (three girls, seven boys; one child was missed in the original consecutive series), from Linköping eight (six girls, two boys; there were just nine children in the time period and one child was excluded from the original consecutive series due to technical problems), from Malmö nine (one girl, eight boys; one child in the original series did not show up for assessment), from Stockholm 10 (four girls, six boys; one child in the original series denied participation, another was excluded due to technical problems, and the two following children in the consecutive series were added), from Umeå 10 (three girls, seven boys), and from Uppsala-Örebro 10 (three girls, seven boys).
The prevalence of known hearing impairment, defined as >20 dB hearing threshold level, was 23% for the whole group and varied between 0 to 50% among the centres (). The two children with hearing impairment from Linköping, and one from Gothenburg, had hearing threshold levels just above 40 dB, and the remaining children had mild hearing impairment with hearing thresholds within 21–40 dB.
Table 1. Number of children with hearing impairment, >20–45 dB hearing threshold level, at the time of speech assessment.
Number and type of speech-language pathologist (SLP) visits for each child was collected using a questionnaire, filled in by the SLPs at the local hospitals and the SLPs at the CLP centres (). Eight out of the 57 children (14%) were reported to having a language disorder (including phonological disorder). Speech therapy was initiated when the SLPs decided it was needed when the children’s speech was followed up at the CLP centres or by the SLPs at the local hospitals. In the total group 53% had received therapy by an SLP, 6 due to language impairment, 21 due to articulation problems, and 3 due to a combination of language impairment and articulation problems. For distribution in the subgroups see .
Table 2. Number of speech-language pathologist (SLP) reviews and number of children who had received speech treatment by an SLP or speech therapist, up to 5 years of age.
Palatal surgery
Gothenburg (n = 10): Six children had lip-nose surgery together with soft palate surgery at mean age 7.2 months (range = 5–12), and due to a wide cleft, four had lip adhesion together with soft palate surgery at mean age 6.3 months (range = 6–7). The latter four children underwent lip-nose surgery at 12–14 months of age. Hard palate surgery was performed in nine children at mean age 24 months (range = 20–27). One child with a wide palatal cleft had hard palate surgery in two stages at 24 and 36 months of age. The surgical technique of the soft and hard palate in all patients were according to the Gothenburg protocol [Citation22]. In all, four surgeons performed the primary palatal surgery. Two children had postoperative fistulas. One of them underwent fistula surgery and another child had fistula surgery in combination with velopharyngeal flap surgery before 5 years of age. In addition, another child underwent velopharyngeal flap surgery before 5 years of age.
Linköping (n = 8): The children had lip-nose surgery at mean age 4.3 months (range = 3–8), and soft and hard palate surgery at mean age 19.5 months (range = 16–30). The Bardach technique [Citation23] was used for palatal surgery. One surgeon performed all surgeries. There were no postoperative fistulas in the group, and no children underwent velopharyngeal flap surgery before 5 years of age.
Malmö (n = 9): The children had lip–nose surgery at mean age 3.9 months (range = 3–6), and soft and hard palate surgery at mean age 11.3 months (range = 10–12). Muscle reconstruction according to Sommerlad [Citation24] was used for palatal surgery. One surgeon performed all surgeries. There were no postoperative fistulas, but one child had a large alveolar residual cleft, that was treated after 5 years of age. No children underwent velopharyngeal flap surgery before 5 years of age.
Stockholm (n = 10): The children had lip–nose surgery at mean age 4.6 months (range = 4–6), and soft and hard palate surgery at mean age 12.5 months (range = 12–13). For five children, minimal incision technique with muscle reconstruction was used [Citation25], for one von Langenbeck technique with muscle reconstruction, for three von Langenbeck technique without muscle reconstruction, and for one a combination of Veau-Wardill Kilner technique and von Langenbeck technique. In all, three surgeons performed the primary palatal surgery. Five children had postoperative fistulas, and one of them underwent fistula closure before 5 years of age. Another child underwent fistula closure in combination with a velopharyngeal flap surgery at two occasions before 5 years of age. One child underwent re-repair of the soft palate because of a rupture, at three occasions before 5 years of age, and at the third occasion in combination with a velopharyngeal flap. In addition, two other children underwent velopharyngeal flap surgery before 5 years of age.
Umeå (n = 10): Eight children had lip–nose surgery at mean age 3.9 months (range = 3–7) months, soft palate surgery at mean age 7.5 months (range = 6–10), and hard palate surgery at mean age 26 months (range = 24–31). Two children had soft palate surgery together with lip–nose surgery at 5 or 7 months, and hard palate surgery at 24 or 25 months. Muscle reconstruction according to Sommerlad [Citation24] was used in 8 of 10 patients. For two children veloplasty was performed using the previous Gothenburg method [Citation22]. One surgeon performed all surgeries. Two out of 10 children hade untreated palatal fistulas. No children received a velopharyngeal flap before 5 years of age.
Uppsala-Örebro (n=10): The children had lip–nose surgery at mean age 4.2 months (range = 4–5), soft palate surgery at mean age 7.1 months (range = 6–8), and hard palate surgery at mean age 26.2 months (range = 24–39). Muscle reconstruction according to Sommerlad [Citation24] was used for palatal surgery. In all three surgeons performed the primary palatal surgery. There were no postoperative fistulas in the group. One child had a re-repair of the soft palate after rupture, followed by a velopharyngeal flap surgery, and another child a velopharyngeal flap surgery only, before 5 years of age.
Documentation
The children were audio recorded at a mean age of 5 years and 1 month (range = 58–64 months), in a quiet room at one of the University Hospitals participating in the study (Sahlgrenska University Hospital Gothenburg, Linköping University Hospital, Skåne University Hospital Malmö, Karolinska University Hospital Stockholm, Umeå University Hospital, Uppsala University Hospital). The children’s speech was documented with an audio recorder (Zoom H4n, Hauppauge, NY; TASCAM HD-P2, Montebello, California) or a PC with Soundswell software (Saven Hitech, Stockholm, Sweden). All of the children were recorded with a condenser microphone (Røde NT4, Sydney, Australia; Sony ECM-MS957, Tokyo, Japan; Pearl CC3, Åstorp, Sweden).
The Swedish articulation and nasality test SVANTE was used [Citation9]. SVANTE consists of a single-word test by picture naming and a sentence repetition task, where each sentence contains a recurring consonant. Eight sentences contain different consonants requiring high intra-oral pressure, two sentences low-pressure consonants, one sentence nasal consonants, and finally two sentences transitions from nasals to stops. For elicitation of conversational speech, a retelling task was used [Citation26].
Editing
All of the recordings were saved in .wav format, de-identified and edited in Audacity (Free Software, General Public License GPL) to three audio files: one with words from the word test, one with sentence repetition and one with connected speech from the retelling task. In the word files, the child's production of the target word was followed by the test leader's repetition of the target word, except when the child repeated the target word after the test leader. If a child produced the target word several times, e.g. due to self-correction the second time, the word with the most correct pronunciation was selected for analysis. Recordings of 18 randomly selected children were duplicated for the assessment of intra-judge reliability.
Perceptual assessment
Six SLPs, one from each participating centre, independently performed perceptual assessment of the entire material with headphones (AKG K271, Vienna, Austria; Sennheiser HD 280 Pro, Wedemark, Germany, Yamaha HPH-MT7, Rellingen, Germany; Sony MDR-V700, Tokyo, Japan, Creative Aurvana Live, Creative Technology Ltd, Singapore). The SLP’s experience with cleft palate speech varied from 1 year to 15 years. All SLPs specialized in cleft palate speech meet annually to update themselves in the area, to discuss definitions of speech variables, and for calibration. Thus, also the SLP with least experience of cleft palate speech was well introduced to the area. The target consonants in the word test were transcribed with “semi-narrow” transcription according to the International Phonetic Alphabet [Citation27,Citation28], which means that supplemental diacritics were used for characteristics common in cleft palate speech. Hypernasality was rated on a four-point ordinal scale with the scale values ‘normal’, ‘mild’, ‘moderate’ and ‘severe’, based on the sentence repetition [Citation9]. Overall perceived velopharyngeal function (PVPF), i.e. an estimation of the velopharyngeal function based on speech symptoms, such as hypernasality, audible nasal air leakage and weak articulation, was rated based on all the included speech material, on a three-point scale with the scale values ‘competent/sufficient’, ‘marginally incompetent/insufficient’ and ‘incompetent/insufficient’ [Citation9].
Analysis of transcriptions
Based on the phonetic transcriptions of target consonants in the first 59 words of SVANTE’s word test, PCC-A was calculated for each SLP and child, by dividing the number of correct consonants with the total number of elicited consonants. In PCC-A, age-appropriate simplifications of /s/ and passive cleft speech characteristics marked with diacritics (e.g. audible nasal air leakage, nasal realization and weak articulation) were scored as correct [Citation12,Citation29].
Reliability
Intra-judge agreement for 18 randomly selected children and inter-judge agreement for all children was calculated. The strength of agreement was interpreted according to Cicchetti [Citation30]. One SLP with moderate intra-judge agreement for hypernasality was excluded from the results analysis. Exact agreement of PCC-A was calculated by the average measures intra-class correlation coefficient (ICC) with two-way inter-effect model. Intra-judge agreement was excellent for PCC-A, with ICC values ranging between 0.993 and 0.996. Also, Inter-judge agreement was excellent (ICC 0.990). Inter- and intra-judge agreement for hypernasality and PVPF were calculated with quadratic weighted Kappa. Intra-judge agreement for hypernasality was excellent (0.752–0.864), and for PVPF good to excellent (0.643–1). Inter-judge agreement was calculated for two SLPs at a time, and varied from moderate to excellent; for hypernasality from 0.511 to 0.864, and for PVPF from 0.519 to 0.832.
Statistical analysis
The analyses were based on the results of the five SLPs with good to excellent intra-judge agreement for all variables. Nonparametric statistics were used since the group sizes were small and the distributions of data were skewed. Descriptive data were presented by median, mean and range values. The Kruskal–Wallis test was used for group comparisons. p < 0.05 (two-tailed) was considered to indicate significant differences.
Results
Percent consonants correct adjusted for age
The mean of the five SLP assessments were used for analysis. No statistically significant differences were seen between groups regarding PCC-A (). The median PCC-A for all children was 93.9, and medians in the different groups varied from 89.9 to 96.8 (; ).
Figure 1. Boxplots showing results of percent consonants correct adjusted for age (PCC-A) in the groups of children from different centres. Medians, ranges, outliers (º) and extreme cases (*) are presented.
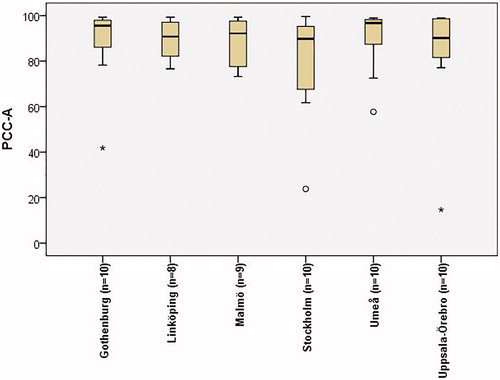
Table 3. Descriptive statistics and results from statistical analyses of percent consonants correct adjusted for age (Kruskal–Wallis test).
Hypernasality and perceived velopharyngeal function
The results were based on the medians of the five SLPs’ assessments (). In the total group, 36 children (63%) had no hypernasality, 12 children (21%) mild, 7 children (12%) moderate, and two children (4%) severe hypernasality (). Twenty-two children (38.5%) were perceived as having competent/sufficient velopharyngeal function, 25 (44%) as having marginally incompetent/insufficient velopharyngeal function, and 10 children (17.5%) as having incompetent/insufficient velopharyngeal function (). No statistically significant differences among groups were seen regarding hypernasality and PVPF ().
Figure 2. The number of children with hypernasality (A) and perceived velopharyngeal function (B) in the groups from different centers. (A) Dark green refers to normal, light green to mild, amber to moderate, and red to severe. (B) Green refers to competent/sufficient, amber to marginally incompetent/insufficient and red to incompetent/insufficient.
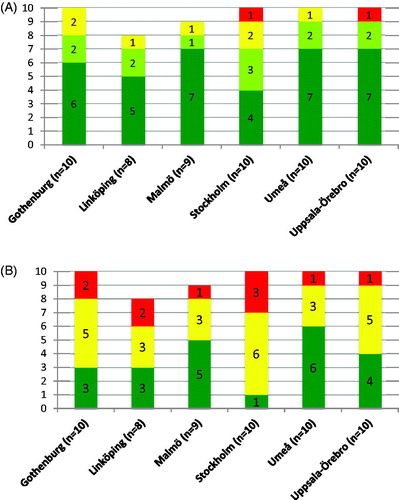
Table 4. Descriptive statistics and results from statistical analyses of hypernasality and perceived velopharyngeal function (Kruskal–Wallis test).
Discussion
The purpose of this prospective inter-centre study was to report on speech outcome for all Swedish 5-year-olds born with a non-syndromic UCLP in a specific time period, and also to compare speech outcomes between centres. An assumption for this was that the Swedish CLP teams have common routines for follow-up at specific ages, including audio recording of standardized speech material.
No significant differences between the centres were found, verifying the findings reported in the Scandcleft trials [Citation2,Citation3]. Furthermore, and in similarity with the findings in the Scandcleft trials, the speech was poorer than in normative data of peers born without orofacial clefts. In normative data of SVANTE [Citation9], data of percent consonants correct (PCC), based on a minimum set of 30 words, is presented. PCC is similar to PCC-A, but not adjusted for age. In the normative data, mean PCC was 96.3 (SD 5.44), and no child had values below 83. The mean PCC-A of the children in the present study was 1.96 standard deviations below the mean in the normative data, and the mean would probably have been even lower if age-appropriate consonant processes had been scored as incorrect. Among the children with UCLP in the present study, 25 (43.9%) had PCC-A values below 1 SD from the mean PCC in the normative data, and 20 (35.1%) had PCC values below 2 SD. Fifteen children (26.3%) had PCC-A values below 83.
The range of the PCC-A scores in the total group was wide, varying between 14.6 and 99.7%. There were two outliers and two extreme cases distributed over four different centres, which made the mean PCC-A score in the total group decrease. All of them were treated with secondary surgery before 5 years of age. Two of four children had postoperative fistulas, one had a rupture of the palate, and the fourth child had received a pharyngeal flap. All four children were rated as having incompetent/insufficient PVPF. Two had been in SLP therapy due to articulatory problems, and one due to phonological disorder. Thus, one can assume that the speech output as reflected by the PCC-A scores in these children was negatively affected by primary problems to separate the oral and nasal cavities.
Poor speech results in 5-year-olds with UCLP compared with peers without UCLP have been seen in earlier Swedish studies [Citation14,Citation29]. When taking into account that age-appropriate consonant processes were scored as incorrect in the measure of PCC in the Scandcleft trials, where the mean of the total group was 80% [Citation3], the results in this study seem to be comparable with those in the Scandcleft trials. In the Scandcleft trials, the proportions of competent/sufficient PVPF varied between 35 and 61% in the different groups [Citation2]. In this study, the range was wider, and the proportion of children with competent/sufficient PVPF varied between 10 and 60% at the different centres. In the Cleft Care UK study only 10% of the children were rated as having hypernasality [Citation13], compared to 22–45% in the Scandcleft trials [Citation2]. In the present study, the range was even wider with a proportion of children rated as having hypernasality varying between 22.2 and 60%. The much lower hypernasality rate in the Cleft Care UK study compared to both the Scandcleft trials and this study could be due to different rating standards in different countries, or just better surgical results. Further research, where raters from different countries are compared, are needed to be able to draw clear conclusions.
Furthermore, although no statistically significant differences among centres regarding speech were revealed in this study, the proportion of children rated as having competent/sufficient PVPF varied largely among centres. The prevalence of rupture/fistulas varied from 0 to 6, and the rate of velopharyngeal flaps from 0 to 4. It was not the case that the centre, undertaking the most secondary speech improving surgery before 5 years of age, had the best speech results. No differences were found in the Scandcleft trials either, except for higher prevalence of oral consonant errors in the group with later timing of hard palate repair (3 years) compared to earlier (1 year) [Citation2,Citation3]. The non-significant differences in this study may be true also even if the group sizes were larger. However, it is possible that significant differences had been detected if the group sizes were larger. According to Williams et al. [Citation31], studies have shown clear advantages in speech outcomes for children who were operated by surgeons who do large numbers of palatal surgery. Thus, individual surgical skill and learning curve are potential important factors that may influence speech results.
Although the results should be interpreted with caution since the groups were too small to draw any conclusions, one can reflect on the variations of postoperative complications between centres. It is a well-known fact that surgical experience improves surgical results and that new methods have learning curves before they are fully mastered [Citation31]. At the three centres where only one surgeon performed the primary palatal surgery, no children underwent secondary palatal surgery before 5 years of age. The centre, which had the most postoperative complications during this period, also used several different surgical procedures for palatal repair. In 2012, a new surgical protocol was introduced at this centre, to overcome the problems. The results are systematically followed up within the Swedish national quality registry for CLP [Citation32] and will be reported separately.
Other factors than the cleft may influence speech outcome, and the possible negative impact of hearing impairment [Citation17,Citation19], should not be overlooked. In this study, the reported prevalence of hearing impairment (mild) at time of assessment varied between 0 and 50%. However, when reviewing the results, higher prevalence of hearing impairment was not related to poorer speech. Further studies with more participants are needed to be able to evaluate any impact of hearing or language disorders. Also, the number of children with a language impairment including a phonological disorder varied between centres, and as the subgroups were small the prevalence of phonological disorders might have influenced the results. The results will be followed up at 7 and 10 years.
The number of studies on impact of intervention of speech-language therapy in children with cleft palate ± lip is small [Citation23], and there is a need to pay attention to speech therapy in cleft palate speech research. The number of children who had received SLP therapy varied between three and eight among centres. In this study, the two centres with the highest number of children who had received SLP therapy also were the ones with a lower number of children with competent/sufficient PVPF. This is in line with the results of the Scandcleft trials, where a high number of speech therapy visits correlated with speech problems [Citation2]. This was interpreted as an indication that children with large problems were identified but number of therapy visits was not related to improvement. On the other hand, in the Cleft Care UK study, speech therapy was related to fewer speech problems, and this was interpreted as an indication that the speech intervention had positive effect on speech [Citation13]. However, this is not in line with the conclusion by Bessell et al. [Citation23], who in their review found little evidence to support any specific intervention of speech language therapy in children with cleft palate ± lip. The effect of speech therapy needs to be further investigated.
Intelligibility is an important measure of functional speech. There is a shortage of valid and reliable intelligibility tests and questionnaires for parents are often used. No such instrument was used at the time of this study but has been added in clinical practice now. The children participating in this study are followed at 7 and 10 years of age, and their parents’ reports of intelligibility at 10 years of age will be reported later, as well as information about phonological awareness at 7 years of age and reading abilities at 10 years of age.
Conclusions
The results were similar to those in other studies on speech of children with UCLP, but poorer than results in normative data of Swedish-speaking 5-year-olds without UCLP. Indications of differences in frequency of surgical treatment and speech treatment between centres were observed.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and the writing of the article. The procedures followed while conducting this study were in accordance with the ethical standards of the Helsinki Declaration of 1975, as revised in 1983.
References
- Leow AM, Lo LJ. Palatoplasty: evolution and controversies. Chang Gung Med J. 2008;31:335–345.
- Lohmander A, Persson C, Willadsen E, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: speech outcomes in 5-year-olds – velopharyngeal competency and hypernasality. J Plast Surg Hand Surg. 2017;51:27–37.
- Willadsen E, Lohmander A, Persson C, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: speech outcomes in 5-year-olds – consonant proficiency and errors. J Plast Surg Hand Surg. 2017;51:38–51.
- Sell D, Southby L, Wren Y, et al. Centre-level variation in speech outcome and interventions, and factors associated with poor speech outcomes in 5-year-old children with non-syndromic unilateral cleft lip and palate: the Cleft Care UK study. Part 4. Orthod Craniofac Res. 2017;2 Suppl 2:27–39.
- Brunnegård K, Lohmander A. A cross-sectional study of speech in 10-year-old children with cleft palate: results and issues of rater reliability. Cleft Palate Craniofac J. 2007;44:33–44.
- Sell D. Issues in perceptual speech analysis in cleft palate and related disorders: a review. Int J Lang Commun Disord. 2005;40:103–121.
- Chapman KL, Baylis A, Trost-Cardamone J, et al. The Americleft Speech Project: a training and reliability study. Cleft Palate Craniofac J. 2016;53:93–108.
- Hagberg C, Larson O, Milerad J. Incidence of cleft lip and palate and risks of additional malformations. Cleft Palate Craniofac J. 1998;35:40–45.
- Lohmander A, Lundeborg I, Persson C. SVANTE – The Swedish Articulation and Nasality Test – Normative data and a minimum standard set for cross-linguistic comparison. Clin Linguist Phon. 2017;31:137–154.
- Lohmander A. Surgical intervention and speech outcomes in cleft lip and palate. In: S. Howard, A. Lohmander, editors. Cleft palate speech: assessment and intervention. Chichester (UK): Wiley-Blackwell; 2011. p. 55–85.
- Britton L, Albery L, Bowden M, et al. A cross-sectional cohort study of speech in five-year-olds with cleft palate +/− lip to support development of national audit standards: benchmarking speech standards in the United Kingdom. Cleft palate Craniofac J. 2014;51:431–451.
- Klintö K, Falk E, Wilhelmsson S, et al. Speech in 5-year-olds with cleft palate with or without cleft lip treated with primary palatal surgery with muscle reconstruction according to Sommerlad. Cleft Palate Craniofac J. 2018;55:1399–1408.
- Sell D, Mildinhall S, Albery L, et al. The Cleft Care UK study. Part 4: perceptual speech outcomes. Orthod Craniofac Res. 2015;18(Suppl 2):36–46.
- Lohmander A, Persson C. A longitudinal study of speech production in Swedish children with unilateral cleft lip and palate and two-stage palatal repair. Cleft Palate Craniofac J. 2008;45:32–41.
- Nyberg J, Peterson P, Lohmander A. Speech outcomes at age 5 and 10 years in unilateral cleft lip and palate after one-stage palatal repair with minimal incision technique – a longitudinal perspective. Int J Pediatr Otorhinolaryngol. 2014;78:1662–1670.
- Lohmander A, Friede H, Lilja J. Long-term, longitudinal follow-up of individuals with unilateral cleft lip and palate after the Gothenburg primary early veloplasty and delayed hard palate closure protocol: speech outcome. Cleft Palate Craniofac J. 2012;49:657–671.
- Hardin-Jones MA, Jones DL. Speech production of preschoolers with cleft palate. Cleft Palate Craniofac J. 2005;42:7–13.
- Tengroth B, Hederstierna C, Neovius E, et al. Hearing thresholds and ventilation tube treatment in children with unilateral cleft lip and palate. Int J Pediatr Otorhinolaryngol. 2017;97:102–108.
- Roberts JE, Rosenfeld RM, Zeisel SA. Otitis media and speech and language: a meta-analysis of prospective studies. Pediatrics. 2004;113:e238–e248.
- Bessell A, Sell D, Whiting P, et al. Speech and language therapy interventions for children with cleft palate: a systematic review. Cleft Palate Craniofac J. 2013;50:e1–e17.
- Timing of primary surgery for cleft palate (TOPS) [Internet]. Liverpool: TOPS trial; [cited 2018 Oct 31]. Available from: http://www.tops-trial.org.uk/
- Friede H, Lilja J, Lohmander A. Two-stage palatal surgery with early veloplasty and delayed hard palate repair: a balanced view on speech and midfacial growth outcome. In: Berkowitz S, editor. Cleft lip and palate. Berlin, Heidelberg (Germany): Springer; 2013. p. 413–437.
- Bardach J. Two-flap palatoplasty: Bardach's technique. In: Salyer KE, Bardach J, editors. Salyer & Bardach's atlas of craniofacial & cleft surgery. Volume II: cleft surgery. Philadelphia (PA): Lippincott-Raven; 1999.
- Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112:1542–1548.
- Mendoza M, Molina F, Azzolini C, et al. Minimal incision palatopharyngoplasty. A preliminary report. Scand J Plast Reconstr Surg Hand Surg. 1994;28:199–205.
- Svensson Y, Tuominen-Eriksson AM. Bussagan [The Bus Story]. Gothenburg (Sweden): Specialpedagogiska institutet Läromedel; 2002. Swedish.
- The International Phonetic Alphabet (IPA) [Internet]. International Phonetic Association; 2015 [cited 2018 Oct 31]. Available from: https://www.internationalphoneticassociation.org/sites/default/files/IPA_Kiel_2015.pdf
- IPA. extIPA Symbols for Disordered Speech [Internet]. International Phonetic Association; 2008 [cited 2018 Oct 31]. Available from: https://www.internationalphoneticassociation.org/sites/default/files/extIPAChart2008.pdf
- Klintö K, Salameh EK, Lohmander A. Phonology in Swedish-speaking 5-year-olds born with unilateral cleft lip and palate and the relationship with consonant production at 3 years of age. Int J Speech Lang Pathol. 2016;18:147–156.
- Cicchetti DV. The precision of reliability and validity estimates re-visited: distinguishing between clinical and statistical significance of sample size requirements. J Clin Exp Neuropsychol. 2001;23:695–700.
- Williams AC, Sandy JR, Thomas S, et al. Influence of surgeon’s experience on speech outcome in cleft lip and palate. Lancet. 1999;13:1697–1698.
- LKG-registret [CLP registry] [Internet]. Lund: LKG-registret; 2018 [cited 2018 Oct 31]. Available from: https://lkg-registret.se/
