Abstract
Comparing complication rates between centres is difficult due to the lack of unanimous criteria regarding what adverse events should be defined as complications and how these events should be compiled. This study analysed all adverse events in a cohort of craniofacial (CF) operations over a 10-year period and applied three different scales (Clavien-Dindo, Leeds and Oxford) for systematic comparison. A total of 1023 consecutive CF procedures in 641 patients was identified. The Clavien-Dindo scale captured 74 complications in 74 procedures (7.2%), whereas the Leeds and Oxford scales captured 163 complications in 134 procedures (13.1%) and 85 complications in 83 procedures (8.1%), respectively. The Clavien-Dindo scale appeared less suitable for CF surgery, because it is predominantly adapted to severe complications and also regards blood transfusion as a complication. The Leeds scale provided a detailed picture of all complications, as well as minor events, whereas the Oxford scale captured all major complications well but applied less accurate definitions for the minor events. Our findings contribute to the benchmarking of complications between CF centres and suggest that both the Leeds and the Oxford scale appear relevant, depending on the emphasis required for major and minor complications and inter-centre audits, respectively.
Introduction
Craniofacial surgery (CFS) comprises both isolated and syndromic conditions encompassing diverse surgical techniques. As part of surgical quality control, evaluating and reporting complications is essential to decreasing surgical morbidity and improving surgical outcomes.
Few craniofacial (CF) centres present complication rates (CRs), and when reported, parameters and definitions vary greatly between institutions (e.g. blood loss could be reported as estimated blood-volume loss, in terms of transfusion or haemoglobin). Standard validated classifications are used in other surgical fields, but there is no consensus on a single system to grade complications in CFS. Additionally, there is a need to standardise the definition of complications in CFS, as these are often arbitrary, subjective and not always clinically relevant. For example, an adverse event might not be described as a complication if it does not extend a hospital stay or result in a significant change in management by certain centres [Citation1,Citation2].
Several well-designed classifications exist in the surgical literature to help define and evaluate complications; however, there has been no gold standard established in CFS across units. Clavien et al. [Citation3] were among the pioneers in establishing a structured system in general surgery (modified Clavien-Dindo classification). This classification differentiates any deviation from a normal postoperative course into complications, failure to cure, and sequelae. It grades complications in order of increasing severity based on the invasiveness of the therapy used. Although previously used in paediatric surgery [Citation4], it has not been previously applied to CFS.
Shastin et al. [Citation5] recently described a classification aimed at reporting the entire spectrum of complications within craniosynostosis (CS) surgery through systematic stratification into six grades and focusing on perioperative and postoperative time points. Each grade is further subdivided according to the length of hospital stay and the time elapsed after discharge.
In England, as part of the annual national audit for the National Health Service (NHS) contract for CF services, all surgical complications are reported using a grading system called the Oxford protocol. Developed by Mr. Stephen Wall of Oxford, UK, it is an unpublished classification for complications in CFS and used to record morbidity and mortality, as well as for auditing purposes. The Oxford protocol is used by the four supra-regionally funded centres currently performing CFS (Great Ormond Street, Oxford, Birmingham, and Liverpool hospitals in the UK). The system splits complications into five types according to increasing degrees of morbidity.
The aims of this study were to determine the applicability of three different complication classifications in CFS and perform a comparison between them.
Additionally, we present a review and classification of perioperative and postoperative complications in a consecutive 10-year series of 641 patients operated for CS or craniofacial syndromes at one centre.
Materials and methods
Patient case series
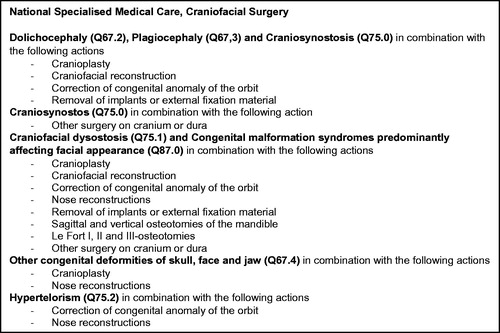
The Craniofacial Unit at Sahlgrenska University Hospital (Gothenburg, Sweden) is one of the two centres in Sweden that perform CFS and have been issued a licence for specialised care (known as National Specialised Medical Care (NSMC)) [Citation6]. The concept is similar to the NHS contract for CF service in England, where only certain centres are responsible for the care of CF patients within a multidisciplinary team setting. Specific procedures based on specific diagnoses under the licence were performed on patients with CS and CF syndromes, excluding trauma and tumours (). Patients with CF syndromes included those both with CS (e.g. Apert syndrome) and without CS (e.g. hemifacial macrosomia). Data concerning all CF patients undergoing surgery at our centre since the 1970s are available in the Gothenburg Craniofacial Registry. Between 2006 and 2015, 641 patients underwent procedures as defined by NSMC, and were identified in the Gothenburg Craniofacial Registry and subsequently reviewed.
Two investigators independently performed a retrospective review of all patient records. As standard, 30 days was set for acute complications. Patient demographics, perioperative details, length of hospital stay, and postoperative outcomes were noted from admission to postoperative follow-up at 1 month. Patients operated with temporary springs underwent an additional procedure for spring removal at 6 months [Citation7,Citation8] and were, therefore, followed until 30 days after spring removal. Any events that occurred after discharge (e.g. wound-healing problems) but communicated via phone/mail by a parent or local paediatrician were also included. Since the data were retrospectively analysed, we were able to include late sequelae for this group of patients extending to 10 years of complications.
The study was approved by the Ethical board of the University of Gothenburg (no. 784-11).
Procedures
We followed the NSMC criteria () and divided surgical procedures into eight categories:
cranioplasties – these comprised all types of cranial vault remodelling (CVR), including CVR with springs (e.g. cranioplasty with springs for metopic and bicoronal synostosis);
spring-assisted cranioplasty – craniotomy combined with springs was performed as previously described in patients with nonsyndromic sagittal synostosis [Citation9], with the group in the present study including two cases of lambdoid synostosis treated with springs;
midface corrections – Le Fort I, Le Fort II, Le Fort III and monobloc osteotomies, with and without distraction;
correction of hypertelorism – standard box and spectacle osteotomies [Citation10];
extractions of foreign material – this group included both planned extractions (e.g. spring extraction after 6 months and external fixators) and unplanned extractions (e.g. implants and wires);
secondary corrections with polymethylmethacrylate (PMMA) implants;
nose reconstructions; and
miscellaneous procedures included in the NSMC licence and that did not fit into other categories (e.g. aesthetic corrections, cheek implants, etc.).
For stratification of the patient population, all surgical procedures were sub-grouped according to patient diagnosis ().
Table 1. Presentation of diagnoses per procedure.
Calculation of CRs
We calculated our overall CR as the number of complications per procedure and not per patient, as several patients in this series underwent two-stage procedures.
Length of stay
For all calculations of length of stay, we applied the Leeds definition of prolonged length of stay throughout the study, defined as greater than 2 SD of the mean length of stay for a specific procedure.
Classifications
Clavien-Dindo
The modified Clavien classification system () measures postoperative morbidity and classifies complications via therapeutic consequence into five grades [Citation3].
Table 2. The Clavien–Dindo classification of complications.
We made a modification to Grade 2, which is defined as complications requiring pharmacologic treatment with drugs other than those allowed for Grade I complications, such as blood transfusions and infections requiring antibiotics. Since blood transfusions are an inherent part of most CF procedures, we modified this grade and excluded blood transfusions.
Follow-up can be divided into Clavien 30, 60 or 90 days; therefore, we used Clavien 30 days as the follow-up period. According to the definition, we only graded the most severe complication for every procedure in order to avoid simultaneously assigning a complication to more than one grade.
Leeds
The systematic approach associated with Leeds classification () was previously described in 2017 [Citation5]. The follow-up was 30 days. Blood loss was noted in the form of excessive blood transfusion (>60 ml/kg). In the present work, as in the original report, we calculated the mean and standard deviation (SD) for all procedures, with prolonged length of stay defined as >2 SD, and the definition of surgical complications as described in their study. If a procedure had more than one complication fitting several categories, all complications were registered.
Table 3. Leeds classification of complications associated with craniosynostosis surgery.
Oxford
The Oxford protocol () mentioned by Shastin et al. [Citation5] comprises five categories that divide complications according to whether they result in delayed discharge, reoperation, unexpected deficit/permanent disability, or death. The definition of what constitute surgical complications was not stated; therefore, we followed guidelines according to the other two classifications and defined delayed discharge using the Leeds criteria. Additionally, because no follow-up time was stated, we used 30 days, and unlike the Clavien-Dindo classification system, if a complication fit the criteria associated with more than one grade, it was included in both.
Table 4. Oxford protocol classification of complications associated with craniosynostosis surgery.
Results
During the 10-year study period, 1023 procedures were performed on 641 patients. Our CR was 7.2% according to Clavien-Dindo, 13.1% according to Leeds and 8.1% according to Oxford. There was no mortality.
Complications
Comparison of complications per classification
Clavien-Dindo classification
The Clavien-Dindo classification captured 74 complications in as many procedures (CR: 7.2%). Examples of Grade I complications (n = 19) were pyrexia, urinary retention, pneumothorax and transient plexus injury not requiring intervention. The Grade II complications (n = 27) primarily included infections that required antibiotics, ranging from urinary tract infections, aspiration pneumonia, wound infection and inhalation for obstructive airway. Grade III(a, b) complications (n = 19) included those requiring surgical intervention (e.g. suprapubic catheterisation, re-insertion of a halo ring, reoperation due to abscess, surgery for a displaced springs, and revision of an infected wound).
Grade IV(a) complications (n = 6) included airway obstruction requiring additional time in an intensive care unit (ICU) in five cranioplasty procedures and an unplanned tracheostomy in a Le Fort I procedure on a patient with Apert syndrome. Grade IV(b) complications (n = 3) included one case of Gram-negative sepsis following metopic cranioplasty in a patient with the Waardenburg syndrome, one case of central line-associated sepsis during cranioplasty in a patient with SZ, and multiple organ failure following Le Fort 3 in a patient with Apert syndrome and several comorbidities. Grade V, no mortality.
Leeds classification
The Leeds classification captured 163 complications in 134 procedures (13.1%). Group-0A complications included excessive blood transfusion (>60 ml/kg), with six procedures leading to this outcome (e.g. sinus tear in one patient and another undergoing midface correction). Group-0B complications included anaesthetic instability (n = 31), with four re-intubations in cranioplasty procedures due to desaturation and laryngospasm, two emergency tracheostomies, and one aspiration pneumonia associated with a midface correction. During two procedures, a previously unknown congenital heart disorder was discovered in the immediate preoperative period, resulting in the procedures being rescheduled until a sufficient work-up was completed. The most common problem in this group was minor respiratory difficulties immediately following extubation (n = 11). Group 0C included unplanned surgical interventions during the index admission (n = 5), with two procedures leading to acute reoperations for spring dislodgement, one case involving an abscess and one case of haematoma evacuation in a PMMA procedure. Group 1A included inpatient complications that did not cause a prolonged length of stay (n = 39) and represented the most common complications in our series (e.g. pyrexia, urinary tract infections and viral infections (calicivirus and rotavirus)). Group 1B–C complications comprised those resulting in a prolonged stay (n = 18), including the patient with the sinus tear that received an excessive transfusion (Group 0A) and, therefore, required a longer postoperative stay. Additionally, this group included one case of transient brachial plexus injury due to an extended operation time, one case of local infection requiring bedside irrigation, and one occurrence each of Haemophilus influenza sepsis and urinary retention. Moreover, this group included procedures resulting in prolonged stays due to comorbidity burden or geographical reasons. Group 2A–B included outpatients not requiring readmission (n = 25) and was dominated by wound-healing problems and wound infections. Group 3A–B (n = 3) included complications associated with persistent fever requiring intravenous (IV) antibiotics administration at either our hospital or a hospital local to the patient. Group 3C–D comprised complications that required surgical intervention (n = 31), including spring-assisted cranioplasties, 12 of which required premature removal of springs due to skin necrosis or spring dislocation. In Group 4A–B, although no complications were found associated with 4A, 4B (n = 5) included three cranioplasties resulting in persistent late cosmetic sequelae (>6 months) requiring correction with acrylate, one patient with scar revision and another with sequelae in the form of persistent pain in the temporal region following secondary acrylate correction. Group 5 included no mortality events.
Oxford protocol
This classification captured 85 complications in 83 procedures (8.1%).
Grade 1 complications (n = 35) were diverse, ranging from pneumonia, exanthema due to antibiotics to airway problems leading to a brief admission to the ICU but no delayed discharge. Grade 2 complications comprised those resulting in delayed discharge with no further surgery required (n = 14) and included excessive transfusion, central venous catheter-related septicaemia, emergency tracheostomy and prolonged IV antibiotics. Grade 3 complications comprised those associated with reoperation, but in the absence of long-term sequelae (n = 35), and included reoperations due to abscess, surgery for displaced springs and halo rings, revision of infected wounds, and secondary acrylate corrections. Grade 4 complications included one patient with unexpected long-term deficit or neurological impairment and involving persistent pain in the temporal region. There were no Grade 5 complications. In our series, 50 complications (4.9%) were Grades 2 through 4, which represent the only grades used for auditing purposes.
Discussion
CFS has advanced significantly in terms of mortality and morbidity [Citation1,Citation11,Citation12]. As a centralised Swedish centre performing CFS, we are annually required to submit data concerning quality performance indicators, such as mortality, blood loss, wound infections requiring antibiotics, circulatory shock within 48 h of surgery, extraordinary airway problems and the number of secondary corrections. A similar range of criteria are published by other centres and are open to subjective interpretation. This highlights the need for a reliable, systematic, standardised tool to classify complications, depicting the full panorama of postoperative burden associated with CFS.
Applicability of the classification systems
The Leeds classification is one of the few published classifications of complications associated with CS surgery and accounts for both perioperative and postoperative events.
Shastin et al. [Citation5] followed 103 patients with nonsyndromic CS prospectively, finding a CR of 35.9%. By contrast, the Leeds classification reported a CR of 13.1% in our study of 641 syndromic and nonsyndromic patients. Applying this system, brought to our attention an unexpectedly high rate of perioperative events. This classification also detects complications that may be considered trivial by some surgeons, such as delayed wound healing, resulting in their being dismissed; however, from a patient/parent perspective, these represent significant complications.
We found three weaknesses in the Leeds classification. First, the definition of excessive blood transfusion was >60 ml/kg (Group 0A); however; this represents a large volume, and we found only six procedures that fit these criteria. The ACS National Surgical Quality Improvement Program-Pediatric Database (NSQIP) identifies transfusion of volumes ≥25 ml/kg of whole blood or packed red cell as a significant bleeding [Citation13]. Shastin et al. chose transfusion >60 ml/kg as their threshold value based on a work by Chow et al., that demonstrated this to be an independent predictor of complications and length of stay in CFS [Citation14].
Interestingly, we also discovered that many of the transfused patients in this study received approximately the same amount of blood (i.e. 450 ml, equating to the blood volume per donor at our hospital). This suggests that anaesthesiologists were likely administering the entire volume once a transfusion was initiated. A blood transfusion to a child with a bodyweight of <∼7.5 kg is classified as a complication, whereas a transfusion to a child weighing >∼7.5 kg is not. Therefore, we suggest that the definition of Grade 0A be modified to ‘excessive blood loss >60 ml/kg’.
Second, the Leeds classification does not include dural tears as complications. There is debate regarding whether midline craniotomy performed directly over the closed suture during spring cranioplasty in sagittal synostosis suffers from such complications. Therefore, we suggest that dural tears be specified in the classification system in order to enable description of the safety of osteotomies performed in conjunction with spring cranioplasty [Citation15]. Third, Group 4A is debatable, given that the criteria associated with ‘long-term deficit’ and ‘resolved by 6 months’ partially conflict.
The modified Clavien-Dindo classification is a widely cited and internationally reproducible classification system [Citation3] that showed a rate of 7.2% in our series. As it is designed for use in adult surgery, it does not account for the need of increased intervention in paediatric surgery for the same procedure (e.g. simple wound revisions are not possible without anaesthesia in paediatric procedures, resulting in a higher CR than that in adults). Furthermore, given its basis on impact severity in adult surgery, Clavien-Dindo classification comprises entities, such as single-organ and multiple-organ failure (MOF); however, CFS rarely results in MOF. On the other hand, there is a much lower threshold for re-admission to the ICU, even for slight airway obstruction. Despite this frequently being reversible and accompanied by a short stay, as the underlying condition is not severe, it is classified as an ‘organ dysfunction’ according to Clavien-Dindo criteria.
Additionally, we were unable to apply the classification without modifying Grade II. Clavien-Dindo defines a blood transfusion as a complication; however, in CFS, a blood transfusion is more or less mandatory during most procedures, except those involving springs. At our centre, the average blood loss during spring-assisted surgery for sagittal synostosis is ∼60 ml, whereas for CVR, it is ∼280 ml (see Supplementary material S1). Therefore, blood transfusion is initiated prophylactically at the beginning of cranioplasties. Without this modification, all such procedures would be defined as having involved a complication. Similar modifications to the classification have also been made by other authors [Citation16].
Finally, Clavien-Dindo classification only rates postoperative events and disregards intraoperative events; however, intraoperative events should also be recorded, as they can confer postoperative burden to the patients. This is one explanation for our low Clavien-Dindo rate relative to that calculated according to Leeds classification, which includes intraoperative events. Another reason for the lower rate is that in patients with more than one complication, the Clavien-Dindo classification only records the most severe complication. To address this underestimation of the true postoperative burden, the Comprehensive Comorbidity Index (CCI) score was recently introduced [Citation17]. This metric integrates the postoperative course on a scale ranging from 0 (no complication) to 100 (death), thereby more accurately representing the overall postoperative burden by a single number.
The Oxford protocol was developed for auditing purposes and is simple to use. In our series, it showed a CR of 8.1%, and adequately covers the range of complications associated with CFS. One weakness of the Oxford protocol concerns the ambiguity of Grade 1, which captured a diverse range of complications from postoperative nausea to procedures leading to readmission to the ICU due to airway insufficiency. In the absence of delayed discharge, reoperation or long-term sequelae, a wide range of complication are classified as Grade 1. Since the classification is not published, our interpretation of Grade 1 was subjective, which could potentially lead to inter-evaluator variability. However, the Oxford protocol was precise in its description of complications related to Grades 2 through 5, given that these complications are more reproducibly defined.
The Oxford protocol is not time-specific, making details related to the extent of the delayed discharge and the timeline associated with reoperation difficult to extract. In summary, the Oxford protocol captures the major forms of morbidity that might occur in association with CFS; however, it is not time-specific and prone to inter-evaluator variability.
A standardised approach in reporting and evaluating complications in order to improve surgical outcomes associated with CFS would be desirable. A good starting point would be to synchronise what defines a complication in the context of CFS and standardise the reporting of complications by applying an appropriate classification system. For the purpose of CFS, such classification would ideally include both perioperative and postoperative events, be easily reproducible, and exhibit low variability. This would enable centres to compare outcomes and implement practices resulting in improved CR, as well as highlight rare events that might otherwise be underreported.
Complication panorama in the present study
Evaluation of CR per procedure indicated that our overall CR compared favourably with those reported by other centres [Citation5]. We found a trend in our cohort between extensive surgical intervention and a high frequency of complications. For example, spring-assisted correction of sagittal synostosis appeared to result in fewer complications than the more extensive pi-plasty correction. This agrees with a previous meta-analysis [Citation18] showing that CVR requires more reoperations due to acute bleeding than spring-mediated cranioplasty and strip craniectomy, whereas the latter procedures resulted in more reoperations due to under-correction. In the spring-assisted group, which mainly involved sagittal synostosis, only one patient was reoperated during the index stay, and 12 of 187 total surgeries performed were reoperated after discharge (10 were due to skin spring detachment or skin breach). There were no reoperations due to bleeding.
At our centre, sequential operations for syndromic cases, such as Crouzon and Pfeiffer, include frontal advancement combined with posterior springs at an early age, followed by ‘spectaclesplasty’ to correct exorbitism, and finally, Le Fort I or III to correct the midface and occlusion in adolescence. Such an approach spreads out the surgical trauma and makes the surgery less extensive than when all procedures are performed in a single operation. Our conservative use of Le Fort III and monobloc procedures might also have contributed to a lower CR than that seen in other centres [Citation19,Citation20]. In our material, there was no mortality. However, this has been reported [Citation1,Citation21]. A particular complication (i.e. prolonged wound healing), was relatively frequent in metopic synostosis as compared with other single-suture synostoses; however, this has not been previously described. One possible explanation could be the relatively tense skin closure after increase in the frontal volume achieved by frontal remodelling.
One weakness of the present study is that it is retrospective. Another limitation is the inclusion criteria that are, on one hand, well-defined but on the other hand include several different patient categories and several different surgical procedures. However, the study is not about a specific patient category or procedure per se but explores three tools for classification of complications in a wider sense. Another methodological issue was late sequelae, which usually require late correction of the head shape. We acknowledge that this might not always appear during the follow-up period. Nevertheless, a significant strength of the study was that the 1023 procedures represented a well-defined consecutive series with predefined criteria encompassing both syndromic and nonsyndromic cases.
In summary, Clavien-Dindo classification appears unsuitable for paediatric CFS, whereas the Leeds classification captures complications, both perioperative and postoperative, systematically. Although Leeds classification offers a highly detailed account of the complications, the Oxford classification highlights relevant complications within CFS and provides a broad overview suitable for auditing purposes. Therefore, depending on how one wishes to tabulate complications, and for what purpose, either the Leeds or Oxford classification seem to applicable to create a benchmark for CFS.
S1_Background_data_complications__rev_.docx
Download MS Word (15.5 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Jeong JH, Song JY, Kwon GY, et al. The results and complications of cranial bone reconstruction in patients with craniosynostosis. J Craniofac Surg. 2013;24:1162–1167.
- Lee HQ, Hutson JM, Wray AC, et al. Analysis of morbidity and mortality in surgical management of craniosynostosis. J Craniofac Surg. 2012;23:1256–1261.
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196.
- Guven S, Istanbulluoglu O, Gul U, et al. Successful percutaneous nephrolithotomy in children: multicenter study on current status of its use, efficacy and complications using Clavien classification. J Urol. 2011;185:1419–1424.
- Shastin D, Peacock S, Guruswamy V, et al. A proposal for a new classification of complications in craniosynostosis surgery. J Neurosurg Pediatr. 2017;19:675–683.
- Welfare NBoHa. National Specialised Medical Care. Craniofacial Surgery [Rikssjukvård viss kraniofacial kirurgi]. Stockholm; 2012; [cited 2016 Nov 17]. Available from: http://www.socialstyrelsen.se/rikssjukvard/visskraniofacialkirurgi
- Fischer S, Maltese G, Tarnow P, et al. Comparison of intracranial volume and cephalic index after correction of sagittal synostosis with spring-assisted surgery or pi-plasty. J Craniofac Surg. 2016;27:410–413.
- Lauritzen CG, Davis C, Ivarsson A, et al. The evolving role of springs in craniofacial surgery: the first 100 clinical cases. Plast Reconstr Surg. 2008;121:545–554.
- Maltese G, Fischer S, Strandell A, et al. Spring-assisted surgery in the treatment of sagittal synostosis: a systematic review. J Plast Surg Hand Surg. 2015;49:177–182.
- Lauritzen C, Tarnow P. Craniofacial surgery over 30 years in Göteborg. Scand J Surg. 2003;92:274–280.
- Czerwinski M, Hopper RA, Gruss J, et al. Major morbidity and mortality rates in craniofacial surgery: an analysis of 8101 major procedures. Plast Reconstr Surg. 2010;126:181–186.
- Esparza J, Hinojosa J. Complications in the surgical treatment of CS and craniofacial syndromes: apropos of 306 transcranial procedures. Childs Nerv Syst. 2008;24:1421–1430.
- American College of Surgeons National Surgical Quality Improvement Program; [cited 2018 Dec 20]. Available from: http://riskcalculator.facs.org/peds/
- Chow I, Purnell CA, Gosain AK. Assessing the impact of blood loss in cranial vault remodeling: a risk assessment model using the 2012 to 2013 pediatric National Surgical Quality Improvement Program data sets. Plast Reconstr Surg. 2015;136:1249–1260.
- Kölby D, Fischer S, Arab K, et al. Craniotomy of the fused sagittal suture over the superior sagittal sinus is a safe procedure. J Craniofac Surg. 2017;28:650–653.
- Parikh A, Washburn KW, Matsuoka L, et al. A multicenter study of 30 days complications after deceased donor liver transplantation in the model for end-stage liver disease score era. Liver Transpl. 2015;21:1160–1168.
- Slankamenac K, Graf R, Barkun J, et al. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1–7.
- Gerety PA, Basta MN, Fischer JP, et al. Operative management of nonsyndromic sagittal synostosis: a head-to-head meta-analysis of outcomes comparing 3 techniques. J Craniofac Surg. 2015;26:1251–1257.
- Esparza J, Hinojosa J, Garcia-Recuero I, et al. Surgical treatment of isolated and syndromic CS. Results and complications in 283 consecutive cases. Neurocirugia (Astur). 2008;19:509–529.
- Munro IR, Sabatier RE. An analysis of 12 years of craniomaxillofacial surgery in Toronto. Plast Reconstr Surg. 1985;76:29–35.
- Allareddy V. Prevalence and impact of complications on hospitalization outcomes following surgical repair for CS. J Oral Maxillofac Surg. 2014;72:2522–2530.