Abstract
Carpal tunnel syndrome (CTS) is the most frequently operated neurological disorder of the hand. Incidence of patients remaining symptomatic has been reported up to 30% after primary release. Revision surgery remains challenging although multiple surgical options have been described. In this case series a simple novel technique, the palmaris longus interposition, is described for the treatment of recurrent and persistent CTS. Patients who underwent PLI between October 2013 and 2018 and without underlying neurological or hand disorders severely affecting the operated hand were eligible for inclusion. All were preoperatively diagnosed with recurrent or persistent CTS based on clinical assessment. Eighteen patients with 20 operated hands consented to the study. Patient characteristics were retrospectively reviewed, including nerve conduction studies and ultrasound scans. Patients were postoperatively asked to classify their symptoms as resolved, improved, not improved or worsened. In addition, postoperative symptom severity and functional status were assessed using the Boston Carpal Tunnel Questionnaire. Ten hands showed recurrent symptoms while the other 10 showed persistent symptoms. The average follow-up was 15 months. No improvement was reported in 5 hands, whereas improvement or complete relief of symptoms was reported in 15 hands. The mean total score of the Boston Carpal Tunnel Questionnaire postoperatively was 2.29 and ranged between 1.26 and 4.32. These results suggest that using the palmaris longus tendon as interposition graft between the leaves of the flexor retinaculum may be a suitable technique for the management of patients with mild to moderate symptoms of recurrent and persistent CTS. Further research should investigate whether this technique has better outcome compared to other procedures.
Introduction
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy of the upper extremity and affects approximately 10% of the population [Citation1–4]. Although various conservative treatment options are available, patients often need a surgical procedure to provide decompression of the median nerve. Carpal tunnel release has become the most frequently performed procedure of the hand [Citation5–7]. It is considered technically undemanding and generally very successful. Nevertheless, a group of patients remains symptomatic after primary release with a reported incidence up to 30% [Citation1,Citation3,Citation6–9]. The presence of postoperative symptoms is commonly described as recalcitrant CTS [Citation1,Citation2,Citation10].
Recalcitrant CTS comprises both recurrent and persistent CTS, in which ‘recurrent’ implies a return of symptoms after an undefined symptom-free interval [Citation5,Citation9]. In general, persistent symptoms can be attributed to an incomplete release of the flexor retinaculum or in rare cases to double crush syndrome or incorrect diagnosis, and the current concept of recurrence is that symptoms mostly result from perineural fibrosis and tethering of the median nerve within the carpal tunnel. Symptoms may also recur in the context of proliferative tenosynovitis or neuromas of the palmar cutaneous branch of the median nerve, although the latter is identifiable on thorough examination [Citation1–3,Citation5,Citation6,Citation8].
Recalcitrant CTS necessitates revision surgery in 5–10% of the patients, for which repeated decompression with external or internal neurolysis have been reported as the standard technique [Citation3,Citation4,Citation6]. However, this approach is often insufficient to prevent recurrent perineural adhesions. Many different surgical techniques are available for enveloping the median nerve with vascularized tissue to provide coverage to prevent recurrent scarring and to create a gliding plane for the nerve [Citation2,Citation3,Citation6,Citation8]. Coverage can be achieved by using synovium [Citation5,Citation10], fascia flaps [Citation5,Citation9], fat flaps [Citation2,Citation8], muscle flaps [Citation11,Citation12], free flaps [Citation13,Citation14], vein wraps [Citation15,Citation16] or synthetic implants [Citation7,Citation17]. Nevertheless, none of these techniques has been shown to be superior to the others [Citation1–3,Citation6].
The other theoretical option is prevention of compression by creating more volume in the carpal tunnel. In this case series a new technique for the management of recalcitrant CTS is proposed, based on the idea of creating more volume in the carpal tunnel: the palmaris longus interposition (PLI). The purpose of this study was to describe this technique and to evaluate the outcome of PLI in patients with recalcitrant CTS.
Material and methods
Study population
Patients who underwent PLI for recalcitrant CTS between October 2013 and October 2018 at our academic center with a minimal follow-up of 6 months were eligible for inclusion. When the operated hand was severely affected by other underlying neurological or hand disorders, patients were excluded. Diagnosis of recalcitrant CTS was based on history taking and physical exam. Nerve conduction studies (NCS) and ultrasound scans were used for characterization of CTS. The neurologist classified NCS changes as normal, mild, moderate or severe CTS based on sensory nerve conduction velocity and distal motor latency [Citation18]. Ultrasonography was considered abnormal when the cross-sectional area of the median nerve in the carpal tunnel was greater than 11 mm2 [Citation19].
A total of 25 patients (28 hands) with recalcitrant CTS were treated with PLI by a single European board-certified hand surgeon, of whom 4 were excluded. One hand was excluded because of a follow-up shorter than 6 months, one because of severe trigger fingers which affected the BCTQ scores, one because of cervical radiculopathy and the last because of a lesion in the palmar cutaneous branch of the median nerve instead of compression of the median nerve. All other patients were invited by telephone, of whom 3 refused to participate. The remaining 18 patients (20 hands) gave their written informed consent. The study was approved by the local Institutional Review Board.
The following data were retrospectively retrieved from the medical charts: age, sex, BMI, affected side, type of symptoms (persistent or recurrent), relevant comorbidities, number of previous surgeries, time between first carpal tunnel release and PLI, results from preoperative NCS and ultrasound scans of the median nerve, and intraoperative findings. We classified recurrent symptoms as a symptom-free interval after surgery of at least 3 months. When symptoms persisted directly after surgery or returned within 3 months, they were classified as persistent.
All participating patients were asked to classify their symptoms as resolved, improved, not improved or worsened. In addition, the self-reported outcomes after PLI were determined using the Dutch translation of the Boston Carpal Tunnel Questionnaire (BCTQ) [Citation20], derived from the original, validated BCTQ [Citation21]. The BCTQ is an international standardized questionnaire that has been developed specifically for patients with CTS. The BCTQ is divided into 2 distinct scales, the symptom severity scale (SSS) and the functional status scale (FSS). The SSS comprises 11 multiple-choice questions, scored from 1 (mildest) to 5 points (most severe). The FSS consists of 8 activities commonly affected by CTS, which must be rated from 1 (no difficulty with the activity) to 5 points (cannot perform the activity at all). The final score of each scale and total score are presented as the arithmetic mean of the individual scores, with higher scores indicating more severe CTS.
Surgical technique
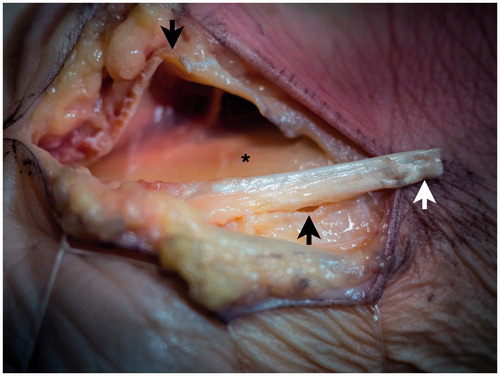
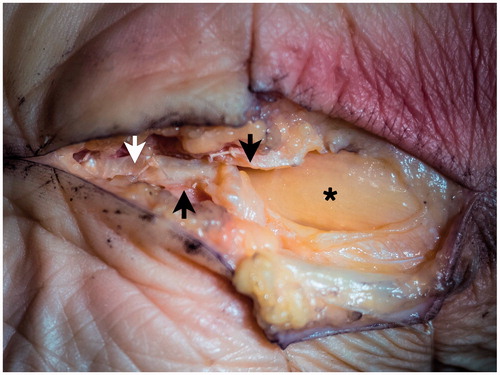
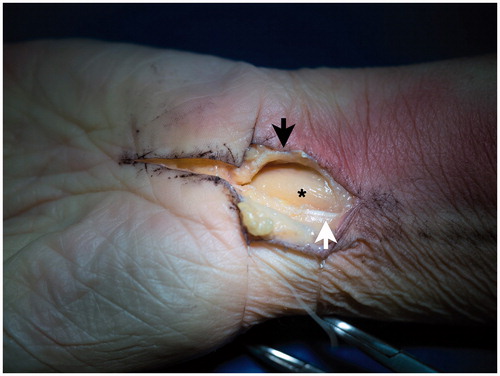
All patients underwent extended open CTR. The previous incision is always used and extended proximally with approximately 4 cm, with a break of the incision at the wrist in ulnar direction. Subsequently, the forearm fascia is opened proximally on one side of the palmaris longus (PL) tendon, depending on where the previous incision was placed. The median nerve is released in the forearm (if necessary), and only when the nerve is seen, the dissection is continued distally. Next, the palmar fascia is incised, again depending on the previous incision and the flexor retinaculum can then be easily transected again, from proximal to distal (). The release should be completed distally. Subsequently, the PL tendon is released from its compartment in the forearm fascia, leaving the epitenon around the tendon intact. The tendon is transected sufficiently proximal to reach the end of the carpal tunnel when flipped distally (). The tendon is then sutured between the two edges of the flexor retinaculum with Vicryl 4-0, with three to four sutures on each side of the retinaculum (). As this lengthens the flexor retinaculum, it should increase the volume in the carpal tunnel. Sutures are placed on the outside of the carpal tunnel to avoid contact with the median nerve. In addition, the epitenon is left in place with hope of diminishing adhesions. The skin is closed with Ethilon 4-0. A slight volar cock-up Plaster of Paris is applied directly postoperatively, and the wrist is immobilized for three weeks. Patients are referred to the hand therapists for finger exercises initially and nerve gliding and range of motion exercises following the three weeks of immobilization.
Figure 1. The incision in a cadaver. The previous incision is extended proximally and the carpal tunnel is opened. *: median nerve; Black arrow: ulnar leaf of flexor retinaculum; White arrow: palmaris longus tendon.
Results
Patient characteristics are shown in . Ten women and 8 men underwent PLI, of whom 2 patients were operated bilaterally. Mean age was 54 years (range 22–74 years). Nine patients underwent previous revision surgery for CTS. The median time between first carpal tunnel release and PLI was 30 months (range 7–432 months). Recurrent symptoms of CTS were seen in 10 hands and persistent symptoms in the other 10.
Table 1. Patient characteristics of the study sample (n = 20 hands).
All patients underwent NCS and all except one underwent an ultrasonography before PLI (). NCS was abnormal in 19 hands, of which 9 had severe changes, 4 had moderate changes and 6 had mild changes. Ultrasonography showed an abnormal median nerve cross-sectional area regarding recalcitrant CTS in 16 of the 19 hands, while 2 it was borderline enlarged in 2 patients (11 mm2). During PLI, perineural fibrosis surrounding the median nerve was seen in 7 patients but was not considered severe enough to warrant flap surgery. In 4 hands the flexor retinaculum seemed incompletely released, possibly causing the persistence or recurrence of symptoms. A partial neuroma-in-continuity was unexpectedly found in one hand after 2 previous CTRs. It was found proximal in the carpal tunnel. The neuroma was then excised and the nerve was sutured there. The remaining 8 hands showed no particular findings during surgery. Patients were followed up for an average of 15 months (range, 7–26 months). Complete relief of symptoms after PLI was seen in 5 hands and improvement of symptoms in 10 hands. Symptoms were not improved in the remaining 4 hands and worsened in 1 hand. When analyzing hands with recurrent and persistent symptoms separately, we found that of the 10 hands with recurrent symptoms, 3 had complete relief, 5 had improvement and 2 had no improvement. In comparison, of the 10 hands with persistent symptoms, 2 hands had complete relief, 5 had improvement, 2 had no improvement and one had worsening of symptoms. Regarding the number of previous CTRs, of the 8 hands with 1 previous CTR, 2 had complete relief, 5 had improvement and one had worsening of symptoms. Ten hands had 2 previous CTRs and of those 3 had complete relief, 4 had improvement and 3 had no improvement of symptoms. Only 2 hands had more than 2 revision surgeries, of whom one showed improvement and one did not. Postoperatively, the average BCTQ SSS score was 2.25 and ranged between 1.09 and 4.45, and the average BCTQ FSS score was 2.18 and ranged between 1.25 and 4.13. The BCTQ total score ranged between 1.26 and 4.32 with a mean of 2.22 ().
Table 2. Pre- and intraoperative findings and postoperative outcomes.
Discussion
In this study PLI is proposed as a simple novel technique for the management of recalcitrant CTS, in which the PL tendon is used to prevent compression of the median nerve by increasing the volume in the carpal tunnel, without extra donor site morbidity. Improvement or complete relief of symptoms was seen in 15 of the 20 hands (75%), while no improvement or worsening of symptoms was seen in 5 hands. Although comparison of the success percentages with other studies is difficult to interpret, we found our success percentage within the range of the included studies as described by Soltani et al. [Citation6] The lowest success percentages reported in this meta-analysis are 53% after external and internal neurolysis and 63% after synovial and hypothenar fat pad flap coverage, but success percentages of the other included studies range predominantly between 80 and 100%. In addition, the study of Cobb et al. [Citation22] and Sun et al. [Citation23] reported mean BCTQ SSS and FSS scores between 1.91 and 1.95 after repeated decompression, compared to 2.30 and 2.27 in the present study. The lower success in this study might be explained by more severe CTS in our patients. This is reflected by the number of prior operations; Sun et al. had an average of 1.11 prior operations, and the flap and the nonflap cohort in the meta-analysis of Soltani et al. [Citation6] had averages of respectively 1.57 and 1 prior operations, whereas our cases had an average of 1.75. Patients with more than one prior operation have been found to have higher odds of not changing or worsening outcome after revision surgery [Citation24,Citation25], which might have caused less improvement in our study.
Three hands with persistent symptoms and 1 hand with recurrent symptoms seemed to have had an incomplete release of the flexor retinaculum. Whether these hands truly had an incomplete release or whether the flexor retinaculum was partially healed could not be determined with certainty. Five hands with recurrent symptoms and 2 hands with persistent symptoms had perineural fibrosis. This is partially in line with the theory that persistent symptoms are ascribed mostly to incomplete release, and recurrent symptoms to perineural fibrosis [Citation5,Citation25]. About a quarter of each group of patients with perineural fibrosis, incomplete release and no particular intraoperative findings had no improvement, therefore it seemed that outcome of PLI was not influenced by intraoperative findings. Improvement between the recurrent and persistent group were almost similar, in favor of the group with recurrent symptoms: respectively complete relief in 3 and improvement in 5 hands versus complete relief in 2 and improvement in 5 hands.
The authors realize that diagnosis of recurrent and persistent symptoms is challenging, especially because NCS and ultrasonography findings frequently remain abnormal, even in patients who had successful carpal tunnel surgery [Citation26,Citation27]. Therefore, abnormalities in these tests do not always represent a continuing problem with the median nerve.
All patients were seen by both a neurologist and a European board-certified hand surgeon, who diagnosed patients based on their symptoms. Two patients had either normal NCS or normal ultrasonography and both had no improvement, possibly due to another underlying neurological cause. Also, the one patient with worsened symptoms had just mild NCS severity and borderline abnormal cross-sectional area of the median nerve. The flexor retinaculum seemed incompletely released in this patient, therefore the expectation was that by releasing it symptoms would improve. Since this was not the case, it is possible that this patient might also had another cause for the persistent symptoms.
Palmaris longus interposition is not aimed at the multiple operated patient with severe CTS, but rather at the patient with mild to moderate CTS after a first or second release, since extensive scarring should still need some form of flap surgery. It is a technically simple procedure that does not sacrifice functional tissue nor create an extra donor site, as the same extended incision is used as for repeated decompression. Furthermore, the PL has been described as an independent risk factor for CTS [Citation28–30], thus cutting it might have an extra beneficial effect on the development of CTS. When performing PLI for the first time, it is important to check whether the patient has a PL and to harvest the PL with adequate length to reach the distal part of the flexor retinaculum.
Our study has several limitations. First, we do not have preoperative BCTQ scores, therefore it was not possible to determine the severity of CTS and whether there was a significant improvement in our patients. Secondly, we did not have enough data to match controls to the PLI patients, so we cannot draw any conclusions regarding PLI being superior over other treatments. Unfortunately, patient history and physical examination were not recorded in a consistent manner, thus we were not able to present those data. However, all patients had clinical signs of CTS. Furthermore, due to a low rate of recalcitrant CTS this study has a small sample size. This also caused the study population to be heterogenous, therefore the outcome of PLI is difficult to interpret and no definitive conclusions can be made about the effectiveness of this technique. It should also be considered that by suturing the PL in the carpal tunnel pressure might be increased. However, although the leaves of the flexor retinaculum may be retracted after a prior CTR, the PL is sutured between both leaves without tension and will therefore not narrow the carpal tunnel or increase pressure. By adding tissue between the leaves extra space is created, which should widen the carpal tunnel and prevent the flexor retinaculum from growing back together. Last, a clinical problem is that not all patients have a PL. Palmaris longus agenesis is seen in 10% to 15% of the population, although this can be different between ethnic groups [Citation31]. If the PL is absent, a strip of the flexor carpi radialis tendon, as is used for the three-ligament tenodesis procedure as described by Garcia-Elias et al. [Citation32] could also be utilized as interposition graft.
In conclusion, this case series described a simple promising technique for the treatment of recalcitrant CTS by using the PL tendon as interposition graft to increase the volume of the carpal tunnel. Palmaris longus interposition may be of value in patients with mild to moderate disease severity who go for second or third carpal tunnel release. Further prospective, comparative research between PLI and other revision techniques is warranted to determine the distinct value of PLI in the treatment of recalcitrant CTS.
Acknowledgements
The authors thank all patients who participated and allowed their data to be anonymously used for the present study.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Abzug JM, Jacoby SM, Osterman AL. Surgical options for recalcitrant carpal tunnel syndrome with perineural fibrosis. Hand (New York, N,Y). 2012;7(1):23–29.
- Fusetti C, Garavaglia G, Mathoulin C, et al. A reliable and simple solution for recalcitrant carpal tunnel syndrome: the hypothenar fat pad flap. Am J Orthop (Belle Mead NJ). 2009;38(4):181–186.
- Rodrigues RL, Shin AY. Treatment options for recurrent carpal tunnel syndrome: local flaps. Tech Orthop. 2006;21(1):61–74.
- Unglaub F, Wolf E, Goldbach C, et al. Subjective and functional outcome after revision surgery in carpal tunnel syndrome. Arch Orthop Trauma Surg. 2008;128(9):931–936.
- Jones NF, Ahn HC, Eo S. Revision surgery for persistent and recurrent carpal tunnel syndrome and for failed carpal tunnel release. Plast Reconstr Surg. 2012;129(3):683–692.
- Soltani AM, Allan BJ, Best MJ, et al. A systematic review of the literature on the outcomes of treatment for recurrent and persistent carpal tunnel syndrome. Plast Reconstr Surg. 2013;132(1):114–121.
- Soltani AM, Allan BJ, Best MJ, et al. Revision decompression and collagen nerve wrap for recurrent and persistent compression neuropathies of the upper extremity. Ann Plast Surg. 2014;72(5):572–578.
- Craft RO, Duncan SF, Smith AA. Management of recurrent carpal tunnel syndrome with microneurolysis and the hypothenar fat pad flap. Hand (New York, N,Y). 2007;2(3):85–89.
- Mahmoud M, El Shafie S, Coppola EE, et al. Perforator-based radial forearm fascial flap for management of recurrent carpal tunnel syndrome. J Hand Surg Am. 2013;38(11):2151–2158.
- Murthy PG, Abzug JM, Jacoby SM, et al. The tenosynovial flap for recalcitrant carpal tunnel syndrome. Tech Hand up Extrem Surg. 2013;17(2):84–86.
- Reisman NR, Dellon AL. The abductor digiti minimi muscle flap: a salvage technique for palmar wrist pain. Plast Reconstr Surg. 1983;72(6):859–865.
- Rose EH, Norris MS, Kowalski TA, et al. Palmaris brevis turnover flap as an adjunct to internal neurolysis of the chronically scarred median nerve in recurrent carpal tunnel syndrome. J Hand Surg Am. 1991;16(2):191–201.
- Dahlin LB, Lekholm C, Kardum P, et al. Coverage of the median nerve with free and pedicled flaps for the treatment of recurrent severe carpal tunnel syndrome. Scand J Plast Reconstr Surg Hand Surg. 2002;36(3):172–176.
- Goitz RJ, Steichen JB. Microvascular omental transfer for the treatment of severe recurrent median neuritis of the wrist: a long-term follow-up. Plast Reconstr Surg. 2005;115(1):163–171.
- Sotereanos DG, Giannakopoulos PN, Mitsionis GI, et al. Vein-graft wrapping for the treatment of recurrent compression of the median nerve. Microsurgery. 1995;16(11):752–756.
- Varitimidis SE, Riano F, Vardakas DG, et al. Recurrent compressive neuropathy of the median nerve at the wrist: treatment with autogenous saphenous vein wrapping. J Hand Surg Br. 2000;25(3):271–275.
- Bilasy A, Facca S, Gouzou S, et al. Canaletto implant in revision surgery for carpal tunnel syndrome: 21 case series. J Hand Surg Eur Vol. 2012;37(7):682–689.
- Werner RA, Andary M. Electrodiagnostic evaluation of carpal tunnel syndrome. Muscle Nerve. 2011;44(4):597–607. Epub 2011/09/17.
- Visser LH, Smidt MH, Lee ML. High-resolution sonography versus EMG in the diagnosis of carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 2008;79(1):63–67. Epub 2007/05/02.
- Smits FVM, Ottenhof M, Feitz R, et al. Nederlandse vertaling van de 'Boston Carpal Tunnel Questionnaire' voor evaluatie van het carpale tunnelsyndroom (BCTQ-DLV). Ned Tijdschr Plast Chir. 2014;5(2):71–73.
- Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–1592.
- Cobb TK, Amadio PC, Leatherwood DF, et al. Outcome of reoperation for carpal tunnel syndrome. J Hand Surg Am. 1996;21(3):347–356.
- Sun PO, Selles RW, Jansen MC, et al. Recurrent and persistent carpal tunnel syndrome: predicting clinical outcome of revision surgery. J Neurosurg. 2019;1–9. Epub 2019/02/17.
- Djerbi I, Cesar M, Lenoir H, et al. Revision surgery for recurrent and persistent carpal tunnel syndrome: Clinical results and factors affecting outcomes. Chir Main. 2015;34(6):312–317.
- Zieske L, Ebersole GC, Davidge K, et al. Revision carpal tunnel surgery: a 10-year review of intraoperative findings and outcomes. J Hand Surg Am. 2013;38(8):1530–1539.
- Kim JK, Koh YD, Kim JO, et al. Changes in clinical symptoms, functions, and the median nerve cross-sectional area at the carpal tunnel inlet after open carpal tunnel release. Clin Orthop Surg. 2016;8(3):298–302.
- Vögelin E, Nüesch E, Jüni P, et al. Sonographic follow-up of patients with carpal tunnel syndrome undergoing surgical or nonsurgical treatment: prospective cohort study. J Hand Surg Am. 2010;35(9):1401–1409.
- Acikel C, Ulkur E, Karagoz H, et al. Effort-related compression of median and ulnar nerves as a result of reversed three-headed and hypertrophied palmaris longus muscle with extension of Guyon's canal. Scand J Plast Reconstr Surg Hand Surg. 2007;41(1):45–47.
- Keese GR, Wongworawat MD, Frykman G. The clinical significance of the palmaris longus tendon in the pathophysiology of carpal tunnel syndrome. J Hand Surg Br. 2006;31(6):657–660.
- Park MJ, Namdari S, Yao J. Anatomic variations of the palmaris longus muscle. Am J Orthop (Belle Mead NJ). 2010;39(2):89–94.
- Pekala PA, Henry BM, Pekala JR, et al. Congenital absence of the palmaris longus muscle: A meta-analysis comparing cadaveric and functional studies. J Plast Reconstr Aesthet Surg. 2017;70(12):1715–1724.
- Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg Am. 2006;31(1):125–134.