Abstract
The current study aims to assess the reliability of 6 range-of-motion measurement methods for the thumb carpometacarpal joint: Pollexograph-thumb, Pollexograph-metacarpal, radius-metacarpal goniometry, intermetacarpal goniometry, intermetacarpal distance, and thumb-distal-interphalangeal distance. A senior hand surgeon, an experienced resident, and a less experienced research fellow evaluated the dominant hands of 29 healthy subjects. All 6 methods were performed for radial adduction, radial abduction, and palmar abduction, but only distance methods were measured for palmar adduction. Intrarater and interrater reliability were computed using intraclass correlation coefficient, standard error of measurement, and smallest detectable difference. Pollexograph-thumb method showed the highest active range of movement for radial adduction (12°) and abduction (71°), while all the other angular methods resulted in approximately 20° for radial adduction and 50° for radial abduction. Distance methods showed comparable mean results for radial and palmar range of motion (adduction/abduction): intermetacarpal distance (50 mm/60 mm) and thumb-distal-interphalangeal distance (50 mm/120 mm). Interrater reliability using the results of the intraclass correlation coefficient demonstrates that Pollexograph-thumb and Pollexograph-metacarpal showed excellent reliability for radial adduction and abduction, whereas Pollexograph-thumb method revealed the best reliability for palmar abduction. Moreover, thumb-distal-interphalangeal distance also showed excellent reliability for radial and palmar abduction. Conventional goniometry showed a large variety of reliability results, ranging from poor to excellent. No clinical benefit can be derived from assessing the palmar adduction. We found that the Pollexograph-thumb showed excellent reliability results throughout all measurements. Thumb-distal-interphalangeal-joint distance is especially valuable for assessing radial and palmar abduction.
Introduction
The unique anatomy of the thumb carpometacarpal (CMC) joint, whose movement axes are not located in the common anatomical planes, has frequently raised discussions as to how to best describe its range of motion (ROM) [Citation1]. Functionally-speaking, the outstanding feature of the CMC joint is the ability to rotate the metacarpal around the longitudinal thumb axis, which is enabled by the incongruence of both articulating surfaces in combination with the capsuloligamentous arrangement of this joint [Citation2]. This supination/pronation movement has an enormous impact on the thumb and the hand’s gripping function, i.e. the ability to oppose the thumb. In particular, opposition is defined as the position of the thumb pad diametrically opposite to the distal pad of the middle finger [Citation3]. Compared with this, circumduction describes the sequence of movements from the thumb in full supination (thumb in maximal palmar adduction) to full pronation (thumbnail parallel to the plane of the palm), which encompasses an interaction of complex movements in all three degrees of freedom of the thumb CMC joint [Citation3].
In clinical practice, radial and palmar abduction measurements, [Citation4–6] whose terms imply their respective movement planes (i.e. parallel and perpendicular to the palm), currently represent the most frequently applied methods for examining restrictions of ROM caused by thumb CMC conditions, e.g. osteoarthritis or rheumatoid arthritis. Moreover, comparison between pre- and postoperative ROM is of utmost importance for monitoring the functional outcome in the course of follow-up appointments and for scientific reporting to the medical literature.
Although experimental studies have revealed the joint’s precise kinematics and movement axes, these results are difficult to convert into clinical practice [Citation1,Citation7,Citation8]. Historically, a wide variety of different techniques for measuring ROM have been developed and are described in the literature using terms such as ‘radial abduction,’ [Citation4–6] ‘palmar abduction,’ [Citation4–6] ’flexion-extension,’ [Citation9,Citation10] ‘abduction-adduction,’ [Citation9,Citation11] or ‘anteposition-retroposition’ [Citation4,Citation11]. However, there is no clear consensus on how these terms are exactly defined; hence, there is even less consensus on the method with which they should be measured. [Citation3] Some measurement techniques, such as the 3-dimensional video camera system, theoretically adopt a valuable approach, but their complexity impedes their common use in stressful clinical everyday life [Citation12,Citation13]. Besides the widespread use of various types of goniometers, some methods include calipers [Citation14]; a protractor, especially developed for the thumb CMC joint by Kraker, Selles et al. [Citation15]; cylinders with different diameters [Citation16].
Further, this heterogeneity of outcome data acquisition, whose accuracy and reliability is scrutinized by only few authors, renders a comparison of absolute values in publications difficult [Citation17,Citation18].
Although pollux adductus is a well-described deformity [Citation2], and the adduction test [Citation19] has proven to be a sensitive diagnostical tool for this condition, measurement results of adduction ROM are hardly included in clinical studies. To assess if any reliable, clinically valuable information can be derived from evaluating the adduction of the thumb CMC joint, we have included this measurement in the present study, besides evaluating the joint’s maximal active abduction.
The present study aims to compare intrarater and interrater reliability of 4 angular and 2 distance methods for both active radial and palmar adduction/abduction (AD/AB) measurement.
Materials and methods
Subjects
We measured the dominant hand of 29 healthy subjects (28 right-handed and 1 left-handed) recruited at the local medical university. All subjects confirmed not to have any prior injury to the dominant upper extremity or any systemic condition affecting the musculoskeletal or nervous system. The group consisted of 16 women and 13 men. The median age was 24 years, with a range of 20 to 34 years.
This study was approved by the medical ethics committee, and written informed consent was obtained from each subject. Moreover, we adhered to the declaration of Helsinki.
Measurements
Prior to ROM measurements, the lead author assessed the subject’s hand width and length as well as the surgical glove size.
All measurements were performed twice by an experienced senior hand surgeon, by an orthopedic surgery resident, and by a research fellow in a microsurgical training center. The study subjects were randomly allocated to one of the three examiners, who wrote down their 20 measurement results on a new study form per each subject and subsequently threw the forms in a locked box. Average time to measure all values by one examiner was approximately 9 min per subject. The retest was performed 13 days after the first round.
We obtained 6 measurement methods for active ROM, which only differ in the plane applied for radial and for palmar ROM assessment: ‘Radial’ indicates a measurement plane parallel to the palm, and ‘palmar’ a plane perpendicular to the palm. We performed 12 measures for radial AD/AB and 8 for palmar AD/AB, because we did not include angular measurements for palmar adduction in our study.
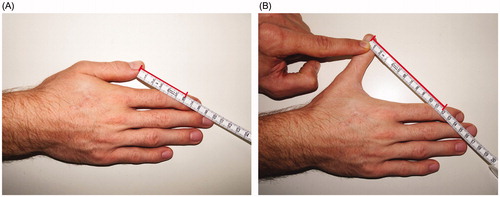
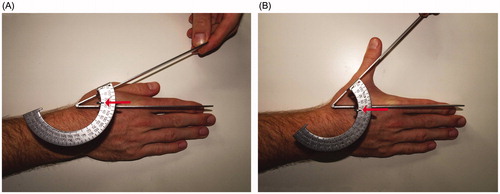
Pollexograph-thumb measurements were principally performed in the same setting as that published by Kraker et al. [Citation15] albeit with small modifications [Citation15], i.e. we refrained from marking anatomical points, because we deemed that marking all patients’ hands would probably be unrealistic in an everyday clinical setting. Moreover, maximal active adduction () and abduction () measures were read from the radial edge of the thumb at the distal phalanx. We applied this modification, because the middle distal part of the nail would be more difficult to define during radial AD/AB measurement, due to the 45° palmar tilting of the CMC joint [Citation20].
Figure 1. Position of the hand during Pollexograph-thumb angle measurement. Radial adduction (A) and radial abduction (B) are assessed at the radial edge of the thumb, indicated by the red arrow.
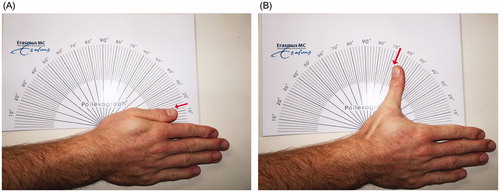
Placing a ruler along the first metacarpal axis, we evaluated maximal adduction () and abduction () while reading the value on the protractor.
Figure 2. A Pollexograph-metacarpal angle measurement; radial adduction (A) and radial abduction (B) are evaluated using a ruler, which is placed along the first metacarpal axis (red arrow).
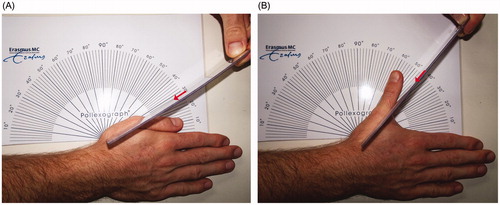
Radius-metacarpal angle was assessed by determining the longitudinal axis of the radius and the first metacarpal in maximal adduction () and abduction () using a conventional Moeltgen goniometer. We performed these measures in supination while taking care that the wrist remained in a neutral position.
Figure 3. Radius-metacarpal angle was measured with the subject’s hand in a supinated position using a Moeltgen goniometer, which is placed along the longitudinal axis and the first metacarpal for assessing radial adduction (A) and radial abduction (B) (red arrow).
Intermetacarpal angle was assessed as the Moeltgen goniometer’s pivot was placed over the thumb CMC joint and the 2 branches were aligned to the mid-dorsal points of the first and second metacarpal heads in maximal adduction () and abduction ().
Figure 4. For intermetacarpal angle, the goniometer was aligned with the first and second metacarpal heads for evaluating radial adduction (A) and radial abduction (B) (red arrow).
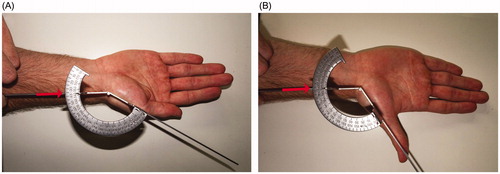
Intermetacarpal distance was evaluated by using a measurement method for the thumb web space, introduced by Murugkar et al. [Citation14]. In contrast to the original publication, however, we used a measurement tape and refrained from marking anatomical points ().
Figure 5. During radial adduction (A) and radial abduction (B), we assessed the intermetacarpal distance between the mid-dorsal points of the first and second metacarpal heads, indicated by the red bar.
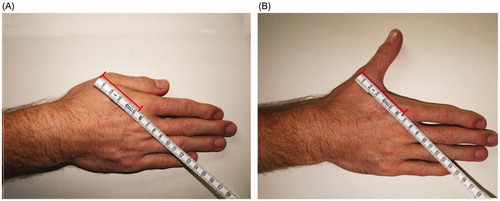
For the thumb-DIP distance measurement, we slightly modified the method described by Itoh, Miura, et al. [Citation16] We assessed the distance between the distal-ulnar thumb nail fold and the radial edge of the flexion crease of the index finger distal interphalangeal joint in maximal adduction () and abduction ().
Statistical methods
Means, standard deviation (SD), and the ranges of every method based on all measurement results were calculated.
Intrarater reliability, which represents the ability of a single examiner to obtain consistent results during repetitive measurements, and interrater reliability, which assesses the degree of congruence between measurements by different examiners, were assessed. Intraclass correlation coefficient (ICC) and its 95% confidence interval (CI) were calculated ICC ranges from 0 to 1, whereby 0 equals no test-retest agreement and 1 means perfect test-retest reliability. Cincetti considered an ICC value less than 0.40 as poor, between 0.40 and 0.59 as fair, between 0.60 and 0.74 as good, and between 0.75 and 1.00 as excellent [Citation21].
Moreover, standard error of measurement (SEM), which indicates the spread of measurement errors when estimating the subject’s true score from the measured values, and smallest detectable difference (SDD), which represents a clinically valuable index, because only a difference between two measurements exceeding this value can be considered as a true change and not a measurement error [Citation22].
Results
Mean values
Mean hand length was 182 ± 11 millimeters and mean hand width 84 ± 6 millimeters. We evaluated a median surgical glove size of 7.0 with a range of 5.5 to 8.5.
presents means, SDs, and ranges of all methods for radial and palmar AD/AB, using the values measured by all 3 examiners. It can be seen that the Pollexograph-thumb means reach the smallest values in adduction measurement and the largest values in abduction angular measurements. All other angular methods range from 20° to 27° for radial adduction and 51° to 55° for radial abduction. Palmar abduction angular measurements results are comparable to the one’s for radial abduction, ranging from 47° to 57° for Pollexograph-metacarpal, radius-metacarpal, and intermetacarpal angle techniques.
Table 1. Means, SDs, and ranges for radial and palmar adduction/abduction measurement methods.
Moreover, average distances for radial AD/AD are comparable with mean measurements for palmar AD/AB. Mean adduction measurements are between 49 and 51 millimeters for all 4 distance methods. Concerning abduction measurement, intermetacarpal distances are 60 to 61 millimeters, and thumb-DIP distances both show 120 millimeters as mean value.
Reliability data for radial AD/AB
Intrarater and interrater reliability for radial AD/AB measurement methods are displayed in . It can be seen that intrarater reliability values for radial adduction among all examiners show 2 poor, 2 fair, 5 good, and 9 excellent results, whereby thumb-DIP is twice, and radius-metacarpal once, the best method. However, interrater analysis shows excellent ICC values only for Pollexograph methods. Concerning radial abduction, intrarater analysis demonstrates almost exclusively excellent ICC results, ranging from 0.79 to 0.96, because only 1 fair and 1 good result could be detected. Interrater analysis for radial abduction indicates that the Pollexograph-thumb angle and thumb-DIP distance show comparably excellent ICC values and, therefore, prove to be the most reliable measurement techniques.
Table 2. Reliability data of radial Adduction and Abduction with use of ICC including 95% CI, SEM and SDD.
Reliability data for palmar AD/AB
shows intra and interrater reliability for palmar AD/AB measurements. For palmar adduction distance measurements, intrarater reliability reveals 2 fair, 2 good, and 2 excellent results, whereas overall intrarater reliability eventuates in 2 poor results. Concerning palmar abduction, intrarater reliability shows 1 poor, 5 fair, 5 good, and 7 excellent results. Interrater reliability reveals similar results as that for radial abduction: Pollexograph-thumb angular method and the thumb-DIP distance are the most reliable methods, with an ICC value of 0.835 and 0.772 respectively.
Table 3. Reliability data of palmar adduction and abduction with use of ICC including 95% CI, SEM and SDD.
Discussion
This study aims to compare 6 ROM measurement methods for active radial and palmar AD/AB and determine the ones, which are clinically most applicable, i.e. reveal the highest ICC values, for thumb CMC joint’s physical examination.
Although conventional goniometry is commonly used in clinical practice, several previous reliability studies corroborate our findings that goniometry, which we assessed using radius-metacarpal and intermetacarpal method, its unreliable in assessing palmar abduction [Citation14,Citation16,Citation17,Citation23,Citation24]. Accordingly, authors who collect data by use of these methods and compare palmar abduction ROM values are at high risk of reporting false significant or false insignificant results due to measurement errors rather than true clinical change.
For interrater reliability analysis, both the study by de Kraker et al. [Citation23] and our survey present the Pollexograph-thumb method with the highest ICC values within all angular methods for palmar abduction measurement. This coefficient even exceeds that by de Kraker et al. [Citation23] (0.66), which is surprising because we initially expected a slight loss of accuracy caused by refraining from marking anatomical landmarks. Given the highest ICC values and lowest SDD values within our study, we recommend the Pollexograph-thumb method for assessing palmar abduction.
Regarding distance methods, we found the best interrater reliability for the thumb-DIP method. This finding underlines the result of Itoh et al. [Citation16], who report the highest ICC value of 0.81 in their study when using a very similar method.
Concerning palmar adduction, we decided prior to the study not to assess angular values, because adjusting the right plane of the thumb and determining the osseous reference point between bulging soft tissue is a demanding task through which hardly any reasonable measurements could have been obtained. The results of our distance outcomes reveal a similar result: Interrater analysis showed poor ICC results with unacceptably high SDD values. Therefore, palmar adduction measurement seems not to gain clinically valuable information in assessing thumb CMC joint’s ROM.
Latest kinematic studies have reported that flexion-extension axis and the AD/AB axes are not perpendicular to each other [Citation1,Citation8]. Thus, the AD/AB plane approximately corresponds with the plane perpendicular to the palm, in which we measured palmar AD/AB in the present study. However, flexion-extension axis is tilted 30° to the dorsum of the hand [Citation1,Citation8]. Therefore, comparing normative data acquired in this plane, that is, 45° ± 15° by Crisco et al., can hardly be compared to our radial AD/AB results. Moreover, no prior study that assessed the reliability of thumb CMC joint’s ROM methods has investigated radial AD/AB; hence, no normative or comparison data are available. Considering the overall best method for both radial AD/AB, Pollexograph-thumb measurements reveals the most reliable interrater ICC results with the lowest SDD values. However, it must be said that radial adduction value is also dependent on the metacarpophalangeal and interphalangeal joint position. Because these joints are usually slightly flexed, this measurement does not explicitly display information about the thumb CMC joint. Therefore, Pollexograph-metacarpal angle has the advantage of providing excellent interrater ICC values, and its anatomical reference points are directly derived from the thumb CMC joint. Moreover, we found that thumb-DIP distances showed the best ICC values for radial AD/AB for radial abduction.
Moreover, Pollexograph-thumb angle and thumb-DIP distance methods yield a very individual result, whose absolute values have little clinical significance. These measures should be assessed relatively, i.e. compared to prior measures for each patient individually, because they are dependent from various factors (hand size, hypermobility or conditions of adjacent joints or soft tissue) besides the thumb CMC joint to be evaluated. In thumb CMC osteoarthritis patients, pollux adductus deformity usually implies a compensatory hyperextension of metacarpophalangeal joint, which increases both the measured Pollexograph-thumb angle and thumb-DIP distance and hence conceals a pathologically decreased ROM of the thumb CMC joint [Citation2]. Therefore, clinical assessment of thumb CMC conditions should include a ROM assessment of the metacarpophalangeal joint [Citation2,Citation4].
Furthermore, intrarater ICC values are highly dependent from the examiner’s clinical experience, as the senior hand surgeon and the resident, who both assess ROM data nearly every day in the course of their clinical work, reached slightly higher values than the less experienced research fellow. In further consequence, interrater ICC values are the main outcome parameters of the present study. This is also because ROM examination is often performed by different clinicians in the course of patients’ follow-up appointments, hence, the clinical significance of these measurements ought not to be biased by methods with poor interrater reliability.
A limitation of the present study is that Pollexograph measurements for radial AD/AB have not been validated yet. Moreover, reliability testing was performed in a relatively small group of 29 young subjects with physiological anatomy of the hand. Moreover, due to our healthy study cohort, whose subjects do not suffer from any thumb CMC condition, and thus no pathological ROM impairment, we were not able to assess opposition ROM measurement methods, because all subjects would have reached 10 points in the Kapandji Score [Citation25] or 0 centimetre distance between the thumb tip and the fifth metacarpophalangeal joint [Citation6]. Future studies are required to validate the usefulness, applicability, and reliability of all the investigated methods for patients suffering from any condition concerning the thumb CMC joint. Moreover, it should be noted that the retest was performed after 13 days, and the reliability data were collected on the basis of equivalent anatomy. Thus, if any retest is performed after a few years, deformities or changes in adjacent joint, which co-affect a measurement, especially Pollexograph-thumb angle and thumb-DIP distance, may lead to a biased measurement and have to be considered.
In conclusion, we recommend Pollexograph-thumb method for radial AD/AB and palmar abduction measurement. If isolated radial and palmar abduction measurement is performed, thumb-DIP distance presents excellent reliability. Moreover, Pollexograph-metacarpal seems to be an excellent radial AD/AB measurement, especially for long-term studies, because its value is directly derived from the thumb CMC joint.
Ethical issues
This study was approved by the medical ethics committee.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Crisco JJ , Halilaj E , Moore DC , et al. In Vivo kinematics of the trapeziometacarpal joint during thumb extension-flexion and abduction-adduction. J Hand Surg Am. 2015;40(2):289–296.
- Merle M. Trapeziometacarpal joint arthritis. In: Merle M , Lim A , editors. Elective hand surgery; Singapore: World Scientific Publishing Co. Pte. Ltd, 2011. p. 29–66.
- Tonkin M. Thumb opposition: its definition and my approach to its measurement. J Hand Surg Eur Vol. 2020;45(3):315–317.
- Cebrian-Gomez R , Lizaur-Utrilla A , Sebastia-Forcada E , et al. Outcomes of cementless joint prosthesis versus tendon interposition for trapeziometacarpal osteoarthritis: a prospective study. J Hand Surg Eur Vol. 2019;44(2):151–158.
- Kaszap B , Daecke W , Jung M. Outcome comparison of primary trapeziectomy versus secondary trapeziectomy following failed total trapeziometacarpal joint replacement. J Hand Surg Am. 2013;38(5):863.e3–871.e3.
- Froschauer SM , Holzbauer M , Hager D , et al. Elektra prosthesis versus resection-suspension arthroplasty for thumb carpometacarpal osteoarthritis: a long-term cohort study. J Hand Surg Eur Vol. 2020;45(5):452–457.
- Wang KK , Zhang X , McCombe D , et al. Quantitative analysis of in-vivo thumb carpometacarpal joint kinematics using four-dimensional computed tomography. J Hand Surg Eur Vol. 2018;43(10):1088–1097.
- D'Agostino P , Dourthe B , Kerkhof F , et al. In vivo biomechanical behavior of the trapeziometacarpal joint in healthy and osteoarthritic subjects. Clin Biomech (Bristol, Avon). 2017;49:119–127.
- Ulrich-Vinther M , Puggaard H , Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am. 2008;33(8):1369–1377.
- Avisar E , Elvey M , Tzang C , et al. Trapeziectomy with a tendon tie-in implant for osteoarthritis of the trapeziometacarpal joint. J Hand Surg Am. 2015;40(7):1292–1297.
- Martin-Ferrero M. Ten-year long-term results of total joint arthroplasties with ARPE® implant in the treatment of trapeziometacarpal osteoarthritis. J Hand Surg Eur Vol. 2014;39(8):826–832.
- Davis TRC , Brady O , Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29(6):1069–1077.
- Itoh S , Miura T , Oka H , et al. Reproducibility of measurements of thumb abduction. Hand Surg. 2010;15(1):7–10.
- Kraker M , de, Selles RW , Schreuders TAR , et al. Palmar abduction: reliability of 6 measurement methods in healthy adults. J Hand Surg Am. 2009;34(3):523–530.
- Kuhns CA , Emerson ET , Meals RA. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: a prospective, single-surgeon study including outcomes measures. J Hand Surg Am. 2003;28(3):381–389.
- Kuo L-C , Cooney WP , Kaufman KR , et al. A quantitative method to measure maximal workspace of the trapeziometacarpal joint-normal model development. J Orthop Res. 2004;22(3):600–606.
- Su F-C , Kuo L-C , Chiu H-Y , et al. Video-computer quantitative evaluation of thumb function using workspace of the thumb. J Biomech. 2003;36(7):937–942.
- Murugkar PM , Brandsma JW , Anderson AM , et al. Reliability of thumb web measurements. J Hand Ther. 2004;17(1):58–63.
- M de K , Selles RW , Schreuders TAR , et al. The Pollexograph: a new device for palmar abduction measurements of the thumb. J Hand Ther. 2009;22(3):271–276.
- Roebroeck ME , Harlaar J , Lankhorst GJ. Reliability assessment of isometric knee extension measurements with a computer-assisted hand-held dynamometer. Arch Phys Med Rehabil. 1998;79(4):442–448.
- Gelberman RH , Boone S , Osei DA , et al. Trapeziometacarpal arthritis: a prospective clinical evaluation of the thumb adduction and extension provocative tests. J Hand Surg Am. 2015;40(7):1285–1291.
- Rongieres M. Anatomie et physiologie de l’articulation trapézométacarpienne humaine [Anatomy and physiology of the human trapezometacarpal joint]. Chir Main. 2004;23(6):263–269.
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6(4):284–290.
- Kraker M , de Selles RW , Molenaar TM , et al. Palmar abduction measurements: reliability and introduction of normative data in healthy children. J Hand Surg Am. 2009;34(9):1704–1708.
- Kapandji A. Cotation clinique de l’opposition et de la contre-opposition du pouce [Clinical test of apposition and counter-apposition of the thumb]. Ann Chir Main. 1986;5(1):67–73.