Abstract
Literature reports four successful cases where penile transplantation has been performed for cis men. To date, no penis transplantation has ever been attempted for trans men. Modern surgical techniques for penis reconstruction for (trans) men with gender incongruence present multiple drawbacks, and sometimes fail to meet patients' expectations. Penis transplantation could represent an alternative solution. With the aim of planning penis transplantation to trans men, a previous study from our same group suggested a surgical technique for explantation of penis and associated vessels, nerves and urethra en-bloc from a cadaver: further radiographic imaging of vascular anatomy was recommended. To measure length and diameter of the internal pudendal arteries at three set points in biological males, in order to confirm its viability for transplantation. A retrospective examination of existing CT images visualizing the internal pudendal arteries in 12 bodies, assigned male at birth, was performed. Diameters were measured in three points: 1. the take off of the artery; 2. distal to its rectal branch; and, 3. at the bifurcation of the two terminal branches of the artery, i.e. the bulbourethral artery and the dorsal artery of the penis. Mean diameters of the selected points were 2.4 mm, 1.9 mm, and 1.5 mm on both sides. Mean lengths of internal pudendal arteries were 111.2 mm on the left, and 120.1 mm on the right side. Diameters of the internal pudendal artery is sufficient for arterial anastomosis at all measured points. Lengths are sufficient to reach recipient vessels.
Introduction
Modern surgical techniques for penis reconstruction for trans men with gender incongruence present multiple drawbacks and often fail to meet patients' expectations [Citation1–4]. More specifically, some complications will result in poorly functioning genitalia [Citation1,Citation2,Citation5,Citation6]. Therefore, alternative reconstructive methods (e.g. bone-anchored penile epithesis [Citation7]) and surgical techniques comprising combinations of various flaps (e.g. anterolateral thigh flap and radial forearm free flap, or anterolateral thigh flap and superficial circumflex iliac artery perforator flap [Citation8]) have been developed and described, mostly for the transgender population. Among these innovations, specialized centers are ultimately developing programs for penis transplantation [Citation9,Citation10].
To the submission of this manuscript, literature has reported four successful cases, out of five attempts, where penile transplantation has been performed for cis men [Citation11–17]. Although the first cases of penis transplantation have been performed for cis men, programs for penis transplantation are also looking into expanding this procedure to trans men [Citation10,Citation18,Citation19]. Within these programs, investigations are being carried out at different levels, such as patient’s wishes [Citation20], ethical issues [Citation21–22], perioperative management [Citation23], and surgical anatomy [Citation18,Citation19,Citation24,Citation25].
Jacobsson et al. [Citation20] explored wishes for penis reconstruction aiming the trans men population and, among these, their interest for penis transplantation: out of the 47 patients who completed the questionnaire, 54% of the study population would consider a penis transplant from a deceased donor, whereas only 20% would not, and the rest being unsure; 48% anticipated the transplant would feel like their own, and only 9% would consider it as being foreign, the rest of the patients being unsure; finally, circa 20% of the patients would accept the increased risk of rejection, infection and long-term immunotherapy related cancer, and circa 50% of the patients were unsure on these issues.
The ethical issues related to penis transplantation (patient selection, transplantation for cis vs trans patients, evaluation of benefits and risks, the role of alternatives to transplantation, organ procurement, experimental surgery, and cost-effectiveness) have been identified and discussed by several authors [Citation21,Citation22], and are out of the aim of this study.
Previous anatomical studies aiming to penis transplantation for cis men focused on the vascular [Citation24,Citation25] and neurovascular anatomy [Citation19], and cadaveric dissection [Citation18,Citation19]. More specifically, prior to perform the first US case of penis transplantation to a cis man, Cetrulo et al. [Citation16] examined the vascular anatomy of one single patient, by using CT angiography and MR; however, no systematic anatomical vascular study has ever been performed on a larger scale of subjects.
In merit to penis dissection for transgender patients, Tiftikcioglu et al. [Citation10] concluded that the penis must be harvested deep to its root, and the arterial dissection should continue retrograde until internal pudendal artery should be divided at the point after it has given its rectal branches.
Following this research line, our same team has previously performed a cadaveric dissection study on male bodies with the aim of dissecting the penis for transplantation in trans men: we advised an en-bloc explantation of male genitalia, which included penis, blood vessels, nerves and urethra [Citation18]. As a conclusion to this anatomical study, it was suggested to further evaluate radiographic imaging of the vasculature of the prospective donors [Citation18].
Data on distal branches might be of use for transplantation to cis man as well; data on proximal branches are of use for transplantation to trans men only. In fact, when planning transplantation to a cis man, shorter urethra and shorter pedicle are needed; the entire penis can be based on a shorter vascular supply; thus, from the surgical anatomy viewpoint, there is no need to perform an en-bloc explantation. Differently, when planning transplantation to a trans man, in order to harvest a longer urethra (needed for the anastomosis to the female recipient counterpart) and a longer vascular pedicle, an en-bloc dissection is needed; thus, from the surgical anatomy viewpoint, it results necessary to know diameters more proximally in the vascular tree.
This study aims, therefore, to measure the length and diameter of the internal pudendal arteries (IPA) at three set points in biological males, in order to confirm its viability for transplantation using the en-bloc surgical dissection of the male genitalia, as previously published [Citation18].
Materials and methods
Ethical approval for the current study was obtained by the Sahlgrenska Academy IRB (ethical approval number: Dnr 2020-02160). Subjects’ consent was waived by the ethics committee.
A retrospective approach for examining internal pudendal arteries was chosen; this approach enabled examination of information already existing in the medical database. The study population consisted of people assigned male at birth (between the years 1970 and 2000), and who received a computer tomography (CT) scan in arterial phasing, visualizing the pelvic area.
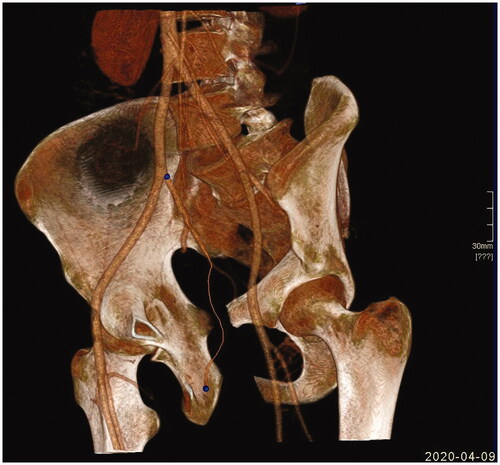
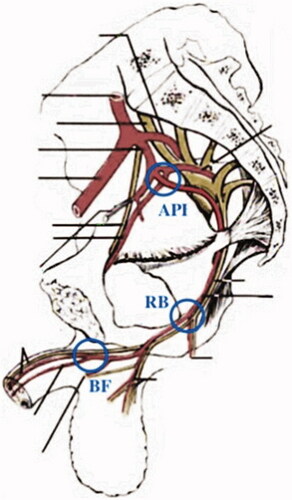
The search of the subjects was performed in the radiographic medical journals from Västra Götaland region, and the search engine Centricity Radiology RA 600 v8.0 (GE Healthcare) was used. The inclusion criteria were slice thickness <1.3 mm, and at least one fully visible IPA. CT scans from 12 subjects were identified. Mean age of the subjects was 37.75 years (range: 19−50). The material was then imported to Syngo XWP VD11B (Siemens Healthcare GmbH), where all measurements were taken. Measurements were taken on both of the internal pudendal arteries, on all patients. Diameters of the vessels were measured manually using the ‘Measure’ tool, at three different anatomical references: 1. at the origin of the IPA at its origin as terminal branch of the internal iliac artery; 2. immediately distal to the take-off of its rectal branch (RB); and 3. just proximally to the bifurcation (Bif) into the bulbourethral artery and into the dorsal artery of the penis. is showing these segments.
Figure 1. Set points of measurement along the internal pudendal artery. API: base of the internal pudendal artery. RB: distally to the rectal branch of the internal pudendal artery. BF: bifurcation of the bulbourethral artery and the dorsal artery of the penis.
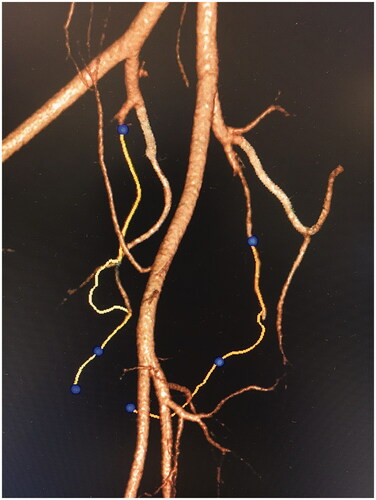
The length of the vessels was calculated using the ‘Embolization Guidance’ application, from the IPA’s origin all the way until the vessel bifurcate (Bif) into the dorsal artery of the penis and into the bulbourethral artery: also, segments of the IPA between its origin and the RB division, and between the RB division and IPA’s final bifurcation, were measured.
BMI from 10 subjects was obtained: 7 of them had a BMI under 30, and 3 had a BMI over 30; mean BMI was 26,85 (range: 17.4−37.5). Information regarding BMI of 2 patients were missing. Subjects were also divided in two subgroups, according to their BMI: one group for BMI < 30, and one for BMI > 30; comparisons were made.
Data were processed with IBM SPSS Statistics v. 26. Values such as mean, median, maximum and minimum were calculated using ‘Frequencies’ in the ‘Descriptive Statistics’ function under ‘Analyze’.
Results
All of the subjects had undergone CT scans with contrast in arterial phase, 7 of which were focusing on the aorta, 4 on the abdomen, and 1 on the pelvis and lower extremities. Indications for scans included: aortic dissection, trauma, internal bleeding, aortitis and aortic exploration. Slice thickness for the CT scans varied between 0.6–1.3 mm.
Diameter
Internal pudendal artery
Mean diameter at the origin of the left IPA was 2.4 mm (range: 2.0–3.7 mm), and the median was 2.1 mm. Mean diameter at the origin of the right IPA was 2.4 mm (range 1.9–3.6 mm), as was the median. Other diameters (just distally to the take-off of the rectal branch (RB), and just proximal to the IPA’s final bifurcation (Bif)) are reported in . One subject did not present a visible left IPA passed the perineal branch, and thus the diameter could not be measured at the Bif set point.
Table 1. Diameters of the left and right internal pudendal arteries (in millimeters).
is showing these measurements for the groups with BMI < 30 and BMI >30.
Table 2. Diameters of the left and right internal pudendal arteries for group with BMI under 30 in millimeters.
is showing the IPA from its offspring from the internal iliac artery to its final bifurcation.
Length
Left internal pudendal artery
Mean length of the left IPA (from its origin to its final bifurcation) was 111.2 mm (range: 75.6–173.3 mm; median: 105.2 mm). Mean length between its origin and its rectal branch (RB) was 63.0 mm (range 32.2–103.0 mm; median: 61.1 mm). Mean length between the take-off of its rectal branch and IPA’s final bifurcation (RB-Bif) was 51.4 mm (range: 34.1–70.3 mm; median 54.0 mm). One subject did not have a visible left IPA passed the perineal branch (it was possible to identify the rectal branch), and thus the length after its perineal branch could not be measured ().
Table 3. Lengths of the left and right internal pudendal arteries (in millimeters).
Mean total length of the right IPA was 120.1 mm (range 59.1–177.9; median: 116.4 mm). Mean length between IPA’s origin and the take-off of its rectal branch was 68.8 mm (range 34.0–150.8; median: 62.5 mm). Mean length between the take-off of the rectal branch and IPA’s final bifurcation (RB-Bif) was 51.3 mm (range: 17.8–100.9; median: 51.3 mm) ().
is showing these measurements for the groups with BMI < 30 and BMI >30.
Table 4. Lengths of the left and right internal pudendal arteries (in millimeters) and its segments for groups with MBI <30 and BMI > 30.
Discussion
Penis transplantation for cis men, to date, has been performed in Asia, South Africa, and USA. Four, out of a total of five attempts, have been confirmed successful [Citation11–17]. Parallel to the publications of these cases of penis transplantations, literature reports anatomical studies that focus on the surgical anatomy for penis transplantation for cis men [Citation19,Citation24,Citation25], as well as for trans men [Citation18]. More specifically, in a previous cadaveric dissection study from our same team, we advised an en-bloc explantation of the male genitalia, which included penis, blood vessels, nerves and urethra [Citation18]: in this dissection, first external pudendal vessels were attempted to be identified, dissected and followed to where they spread into the skin; next, the perineum was dissected, the crura of the corpora cavernosa were located; the bundle of vessels associated with the crura was assumed to contain the internal pudendal vessels. It was suggested that the abdomen could be dissected, and a greater length of the vessels could be preserved, by following the branches of the internal iliac vessels and meeting the dissection at the perineum. This would ensure the preservation of the entire lengths of vessels, which was supposed to reach the recipient vessels for the anastomosis. It was noted that vascular anatomy is subject to individual variations: for example, the internal pudendal vessels could have an aberrant course or have accessory vessels, and these accessory vessels might be the solely responsible of the blood supply to the corpora cavernosa [Citation24–26]. It was suggested, therefore, to further evaluate radiographic imaging of the vasculature of the prospective donors [Citation18]. Therefore, in the present study we measured lengths and diameters of left and right internal pudendal arteries at three set points in biological males, in order to confirm its viability for transplantation using the en-bloc surgical dissection of the male genitalia ().
Figure 3. 3D CT Angiogram of pelvic arteries processed on Siemens Syngo Embolization Guide platform. Left IPA pathway is highlighted correctly, while right IPA pathway was divergent and had to be adjusted manually.
Anatomy of the IPA is not known in details from previous literature; and, during surgery it might be the case that a longer pedicle is not necessary; therefore, rather than transplanting a longer pedicle, and risking its kinking (with subsequent higher chance of anastomosis failure [Citation27–28]), anastomosis could be performed and the sites where branches are taking off. Furthermore, the rectal branches could be used for additional anastomoses, if required. Thus, we measured the diameter of the vessels at two additional sites (distal to the rectal branch, and at the bifurcation of the 2 terminal branches). This does not mean that procurement should not include as much as possible.
Results from our investigation show that diameters of the internal pudendal arteries, at the measured set points (origin of the IPA, take-off of the rectal branch, and IPA’s final bifurcation) are large enough to allow for end-to-side arterial anastomosis to the recipient femoral artery or for end-to-end arterial anastomosis to other local vessels, such as externa pudendal, inferior epigastric or circumflex arteries. Furthermore, length of the IPA should allow to reach most of the above-mentioned recipient arteries. Still, the use of a vein graft could represent a salvage procedure, if needed.
We also divided patients in two subgroups in relation to their BMI (BMI <30 and BMI > 30), and checked for significant differences; however, the study population was too small to drawn significant conclusions.
Strengths and limitations
As this study may be the first of its kind, it was deemed of highest importance to minimize any risks posed on subjects, thus a retrospective radiographic approach was chosen. In this way, risks associated with radiation, contrast fluids and injections site trauma, were completely avoided.
In order to make accurate length measurements from CT scan images, the software Siemens Syngo XWP VD11B was chosen (and, more specifically, its ‘Embolization Guidance’ application); this implies a risk of error in the measurements [Citation29]. More specifically, it has been noted that, in clinical praxis, the software might slightly underestimate the size of the vessels.
Images were of high quality, even if they were not originally intended for examination of the internal pudendal arteries. Still, there were some inconsistencies visualizing the arteries, which were most likely due to varying contrast levels in the arteries, and/or varying slice thickness. This led to some difficulty in identifying the branches of the internal pudendal artery; therefore, we recognize the possibility of human errors in measurements. If this study were to be repeated, a prospective approach could minimize most of these errors, resulting in images taken for the purpose of examining the internal pudendal arteries, as well as consistent contrast levels and slice thickness.
Finally, this study reports on a small number of cases; also, there is a risk for selection bias, since only subjects with imaging visualizing the internal pudendal arteries were included. Nevertheless, this bias does not necessarily mean that some patients might not have adequate IPAs which are not adequate for transplantation and anastomosis; instead, this bias suggests that a prospected approach, possibly in brain dead candidates for transplantation, is warranted. For the purpose of studying IPA anatomy for future transplantation, either brain dead candidates for (any) transplantation, or potential brain dead donors, where angiography is performed for the diagnosis of brain death, could be used.
This study was not intended to analyze the external pudendal vessels, nor the venous drainage of the penis. In fact, found images did not include the external pudendal vessels, as most of the images were cut off before vessels take-offs. Also, images were captured while the contrast was in an arterial phase, which made the examination of the venous drainage impossible to perform.
Study subjects included patients with major abdominal arterial injury; this might present a source for bias since major abdominal injury might affect the diameter in studied vessels. Indeed, there is always a risk for vasoconstriction; nevertheless, the estimates will be of benefit to the recipient; i.e. any estimate would be on the low side, potentially not resulting in donation.
Future studies
We suggest to repeat the same study on the artery and, at the same, investigate on the vein anatomy of possible candidates, such as brain-dead organ donors. Findings of studies on vascular anatomy of brain-dead organ donors might highlight the importance of assessing the anatomy of the internal pudendal vessels prior to explantation, in order to plan and execute the most appropriate surgical methods (i.e. preparing for vessel grafts), or to identify donors unsuitable for penis donation. Finally, studies on the anatomy of pudendal vessels of brain-dead organ donors might conclude that pudendal artery and/or vein anatomy is inconstant and, therefore, only brain-dead organ donors should be used for penis transplantation, pending pre-operative vessels analysis, while dead donor could be unsuitable.
Selective arterial Cone beam CT (CBCT) gives an opportunity to get a good image of arterial three down to an organ of interest. To date, this is the only method in case of prostate embolization. With this method, it is possible to identify which arteries go to prostate, and those which go elsewhere to pelvic organs. Resolution of tiny arterial branches on selective arterial CBCT is superior to that of state-of-the-art conventional CT. There is still a question whether CBCT would give valuable information on veins, especially small ones such as plexa. Indeed, CBCT could pose larger risks for the subjects, as it involves the catheterization of the examined vessels, thus being more invasive than traditional CT scan [Citation30].
Age was not an inclusion criteria for this study. Indeed it was noticed, but no significant result in merit to IPA anatomy was achieved. Donor age inclusion criteria for penile transplant should be addressed in future research.
Also, this study was not intended to analyze the impact of long term illness (such as diabetes or hypertension) on the anatomy of the external pudendal vessels. Nevertheless, brain-dead donor candidates shall represent the best group of patients where the issue of long-term illness should be to extensively addressed.
Conclusion
The diameter of the internal pudendal artery, for its entire length from its origin to the final bifurcation, is large enough to allow surgical anastomosis, when planning penis transplantation onto trans men. In addition, this study shows a wide variation in the length of the internal pudendal artery, which could require alternative surgical solutions (such as vein grafts) to reach the vessels of the recipient. These findings fulfill the requirements needed for a successful en-bloc dissection of the penis with the purpose of penis transplantation.
We therefore suggest to repeat the same study on the artery and, at the same, investigate on the vein anatomy of possible candidates, such as brain-dead organ donors.
Author contributions
Gennaro Selvaggi: plannig, analysis of the results, discussion of the results, writing.
Kristiina Manner: collecting data, analysis of results, writing.
Augustinas Sakinis: collecting data, analysis of results, writing.
Michael Olausson: planning, discussion of the results, writing.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Wroblewski P, Gustafsson J, Selvaggi G. Sex reassignment surgery for transsexuals. Curr Opin Endocrinol Diabetes Obes. 2013;20:570–574.
- Selvaggi G, Elander A. Penile reconstruction/formation. Curr Opin Urol. 2008;18:589–597.
- Garaffa G, Raheem AA, Ralph DJ. An update on penile reconstruction. Asian J Androl. 2011;13:391–394.
- Garaffa G, Christopher NA, Ralph DJ. Total phallic reconstruction in female-to-male transsexuals. Eur Urol. 2010;57:715–722.
- Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg. 2009;124(2):510–518.
- Selvaggi G, Bellringer J. Gender reassignment surgery: an overview. Nat Rev Urol. 2011;8(5):274–282.
- Selvaggi G, Branemark R, Elander A, et al. Titanium-bone-anchored penile epithesis: pre-operative planning and immediate post-operative results. J Plast Surg Hand Surg. 2015;49(1):40–44.
- D’Arpa S, Claes K, Lumen N, et al. Uretrhal reconcstruction in anterolateral thigh flap phalloplasty: a 93-case experience. Plast Reconstr Surg. 2019;143(2):382e–392e.
- Campbell JD, Burnett AL. Surgery in 2017: moving towards succesfull penile transplantation programmes. Nat Rev Urol. 2018;15(2):75–76.
- Hawksworth DJ, Cooney DS, Burnett AL, et al. Penile allotransplantation: pushing the limits. Eur Urol Focus. 2019;5(4):533–535.
- Spoko NA, Tuffaha SH, Lough D, et al. Penile allotransplantation for complex genitourinary reconstruction. J Urol. 2017;198:1–7.
- Hu W-L, Lu J, Zhang L, et al. A preliminary report of penile transplantation. Eur Urol. 2006;50:851–853.
- Bateman C. World's first successful penis transplant at Tygerberg Hospital. S Afr Med J. 2015;105(4):251–252.
- Van der Merwe A, Zarrabi A, Zuhlke A, et al. Lessons learned from the world’s first successful penis allotransplantation. J Mater Sci Mater Med. 2017;28(2):27.
- Van der Merwe A, Graewe F, Zuhlke A, et al. Penile allotransplantation for penis amputation following ritual circumcision: a case report with 24 months of follow-up. Lancet. 2017;390(10099):1038–1047.
- Cetrulo CL, Jr., Li K, Salinas HM, et al. Penis transplantation: first US experience. Ann Plast Surg. 2018;267(5):983–988.
- Redett RJ, 3rd, Etra JW, Brandacher G, et al. Total penis, scrotum, and lower abdominal wall transplantation. New Eng J Med. 2019;381(19):1876–1878.
- Selvaggi G, Wesslen E, Elander A, et al. Penile transplantation in female-to-male sex reassignment surgery: a cadaveric study. BioMed Res Int. 2018:6754030. doi: https://doi.org/10.1155/2018/6754030
- Tiftikcioglu YO, Erenoglu CM, Lineaweaver WC, et al. Anatomic basis for penis transplantation: cadaveric microdissection of penile structures. Ann Plast Surg. 2016;76(6):729–734.
- Jacobsson J, Andreasson M, Kolby L, et al. Patients’ priorities regarding female-to-male gender affirmation surgery of the genitalia - a pilot study of 47 patients in Sweden. J Sex Med. 2017;14(6):857–864.
- Caplan AL, Kimberly LL, Parent B, et al. The ethics of penile transplantation: preliminary recommendations. Transplantation. 2017;101(6):1200–1205.
- Selvaggi G, Aas S. New frontiers in surgery: the case of uterus and penis transplantation. In: Simona Giordano S, Harris J, Piccirillo L, editors. Second anthology on scientific freedom. Manchester, UK: Manchester University Press; 2018.
- Tiftikcioglu YO, Cagil M, Erenoglu CM. Perioperative management of penile transplantation. Microsurgery. 2016;36:271–275.
- Tuffaha SH, Sacks JM, Shores JT, et al. Using the dorsal, cavernosal, and external pudendal arteries for penile transplantation: technical considerations and perfusion territories. Plast Reconstr Surg. 2014;134:111e–119e.
- Tuffaha SH, Budihardjo JD, Sarhane KA, et al. Expect skin necrosis following penile replantation. Plast Reconstr Surg. 2014;134(6):1000e–1004e.
- Walz J, Burnett AL, Costello AJ, et al. A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. Eur Urol. 2010;57(2):179–192.
- Selvaggi G, Salgarello M, Anicic S, et al. Effect of torsion on microvenous anastomotic patency in rat model and early thrombolytic phenomenon. Microsurgery. 2004;24(5):416–417.
- Selvaggi G, Anicic S, Formaggia L. Mathematical explanation of the buckling of the vessels after twisting of the microanastomosis. Microsurgery. 2006;26(7):524–528.
- Siemens Haalthcare GmbH. Syngo embolization guidance. Siemens Healthineers; 2020 [last access 2021 Mar 11]. Available from: https://www.siemens-healthineers.com/angio/options-and-upgrades/clinical-software-applications/syngo-embolization-guidance/features.
- Dencker D, Pedersen F, Engstrom T, et al. Major femoral vascular access complications after coronary diagnostic and interventional procedures: a Danish register study. Int J Cardiology. 2016;202:604–608.