ABSTRACT
Background: It is unknown whether remotely delivered intensive trauma-focused therapy not only is an effective treatment for PTSD, but also for Complex PTSD.
Objective: Testing the hypothesis that a brief, fully remotely administered intensive trauma-focused treatment programme for individuals with PTSD and Complex PTSD would be safe, and associated with a significant decline of the corresponding symptoms and diagnostic status.
Method: The treatment sample consisted of 73 consecutive patients diagnosed with PTSD according to the CAPS-5. According to the ITQ (n = 70) 33 (47.1%) patients also fulfilled the diagnostic criteria of Complex PTSD. The 4-day treatment programme contained a combination of prolonged exposure, EMDR therapy, physical activities and psycho-education. Treatment response was measured using the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5), the PTSD Checklist for DSM-5 (PCL-5), and the International Trauma Questionnaire (ITQ) for classifying Complex PTSD and indexing disturbances in self-organization (DSO).
Results: Overall CAPS-5, PCL-5, and ITQ-DSO scores decreased significantly from pre- to post-treatment (Cohen’s ds 2.12, 1.59, and 1.18, respectively), while the decrease was maintained to six months follow-up. At post-treatment, 60 patients (82.2%) no longer met the diagnostic criteria of PTSD, while the proportion of patients with Complex PTSD decreased from 47.1% to 10.1%. No drop out, and no personal adverse events occurred.
Conclusions: The results support the notion that intensive, trauma-focused treatment is feasible, safe and associated with a large decrease in PTSD and Complex PTSD symptoms, even when it is brief, and applied fully remote.
HIGHLIGHTS
Second study to examine the effectiveness of a fully remote intensive trauma-focused treatment for PTSD and Complex PTSD.
Significant decrease of DSO symptoms.
Over 80 percent of the patients no longer met the diagnostic criteria of PTSD and Complex PTSD following treatment.
Antecedentes: Se desconoce si la terapia centrada en el trauma intensiva entregada remotamente no es solo un tratamiento efectivo para el TEPT, sino que también para el TEPT Complejo.
Objetivo: Testear la hipótesis de que un programa de tratamiento centrado en el trauma para individuos con TEPT y con TEPT Complejo, intensivo, administrado completamente de forma remota y breve es seguro, y se asocia con una disminución significativa de los síntomas correspondientes y el cambio del estado diagnóstico.
Método: La muestra del tratamiento consistió en 73 pacientes consecutivos diagnosticados con TEPT de acuerdo a la entrevista CAPS-5. De acuerdo al ITQ (n = 70), 33 (47.1%) pacientes también cumplieron los criterios diagnósticos para TEPT Complejo. El programa de tratamiento de cuatro días comprende una combinación de exposición prolongada, terapia EMDR, actividades físicas y psicoeducación. La respuesta al tratamiento fue medida usando la Escala de TEPT Administrada por el Clínico para el DSM-5 (CAPS-5 en su sigla en inglés), la Lista de Chequeo de TEPT para el DSM-5 (PCL-5 en su sigla en inglés), y el Cuestionario Internacional de Trauma (ITQ en su sigla en inglés) para clasificar TEPT Complejo y las distorsiones en la auto-organización (DSO en su sigla en inglés) asociadas.
Resultados: En general, los puntajes de CAPS-5, PCL-5, y ITQ-DSO disminuyeron significativamente desde el pre al post tratamiento (Cohen’s ds 2.12, 1.59, and 1.18, respectivamente), mientras que la disminución se mantuvo en el seguimiento de los seis meses. Al término del tratamiento, 60 pacientes (82.2%) ya no cumplieron con los criterios diagnósticos de TEPT, mientras que la proporción de pacientes con TEPT Complejo disminuyó desde 47.1% a 10.1%. No ocurrieron abandonos ni eventos adversos personales.
Conclusiones: Los resultados apoyan la noción de que tratamiento centrado en el trauma intensivo es factible, seguro y está asociado con una gran disminución en los síntomas de TEPT y TEPT Complejo, incluso cuando es breve, y es aplicado de forma completamente remota.
背景:目前尚不清楚远程提供的聚焦创伤强化治疗是否不仅是治疗 PTSD 的有效治疗方法,也适用于复杂性 PTSD 。
目的:检验以下假设,即一项简短、完全远程管理的针对 PTSD 和复杂性 PTSD 患者的聚焦创伤强化治疗方案是安全的,并且与相应症状和诊断状态的显著下降相关。
方法:治疗样本由 73 名根据 CAPS-5 诊断为 PTSD 的连续患者组成。根据 ITQ (n = 70) , 33 名 (47.1%) 患者也符合复杂性 PTSD 的诊断标准。为期 4 天的治疗计划包含延长暴露、EMDR 治疗、体育活动和心理教育的组合。使用DSM-5临床用 PTSD 量表 (CAPS-5)、DSM-5 PTSD 检查表 (PCL-5) 和用以对复杂性 PTSD 进行分类和索引自组织障碍(DSO)的国际创伤问卷 (ITQ) 测量治疗反应。
结果:总体 CAPS-5、PCL-5 和 ITQ-DSO 评分从治疗前到治疗后显著下降(Cohen’s d 分别为 2.12、1.59 和 1.18),而下降保持到 6 个月的随访。治疗后,60 名患者(82.2%)不再符合PTSD诊断标准,而复杂性PTSD患者比例从 47.1%下降到10.1%。没有流失,也没有发生个人不良事件。
结论:结果支以下观点,即强化的聚焦创伤治疗是可行的、安全的,并且与 PTSD 和复杂性 PTSD 症状的大幅减少相关,即使它是短暂且完全远程施行的。
1. Introduction
Lately several forms of remotely administered psychotherapy have been developed that enhance access to psychological treatment when needed (Hilty et al., Citation2013; Varker, Brand, Ward, Terhaag, & Phelps, Citation2018). Online psychotherapy has been shown to be a safe alternative that may elicit high levels of user satisfaction (Backhaus et al., Citation2012; Mohr, Burns, Schueller, Clarke, & Klinkman, Citation2010; Olthuis et al., Citation2016). More specifically, there is evidence showing that online psychotherapy can encourage individuals to disclose more information with the therapist because they feel less intimidated than in face-to-face contact (Tachakri & Rajani, Citation2002; Wootton, Yellowlees, & McLaren, Citation2003). Therefore, remotely administered psychotherapy may well be suited for the treatment of post-traumatic stress disorder (PTSD). For example, while one of the key features of PTSD is avoidance of situations that may trigger the recall of the traumatic event (including talking about what happened), the physical distance between the patient and the therapist during online treatment makes the disclosure of information easier (Thorp, Fidler, Moreno, Floto, & Agha, Citation2012).
In line with these advantages, in several uncontrolled studies, both trauma-focused cognitive behavioural therapy (CBT; e.g. Germain, Marchand, Bouchard, Drouin, & Guay, Citation2009; Tuerk, Yoder, Ruggiero, Gros, & Acierno, Citation2010), and EMDR therapy (one single case description; Todder & Kaplan, Citation2007) have been shown to be effective in alleviating PTSD symptoms by means of telehealth-delivered care. What is more, randomized controlled studies (Acierno et al., Citation2016; Acierno et al., Citation2017; Morland et al., Citation2014; Morland et al., Citation2020) and meta-analytic data (Turgoose, Ashwick, & Murphy, Citation2018) show that PTSD treatment via telehealth delivered in either a clinical setting or at home yields similar treatment outcomes compared to traditional face-to-face contact.
To accomplish a more rapid recovery of PTSD symptoms several intensive treatments have been developed and examined in terms of applicability and effectiveness (Wachen, Dondanville, Evans, Morris, & Cole, Citation2019). Such brief, trauma-focused, treatments seem to produce a faster reduction of symptoms compared to the standard therapy, while the results appear to sustain after therapy (Bongaerts, Van Minnen, & De Jongh, Citation2017; Ehlers et al., Citation2014; Van Woudenberg et al., Citation2018). This treatment mode, typically without any preparation phase prior to therapy to improve emotion regulation and interpersonal skills, has been shown to be a safe, feasible, and a well-tolerated alternative with low levels of drop out and symptom exacerbation (Sciarrino, Warnecke, & Teng, Citation2020). This also has been proved to be true for patients suffering from PTSD who have been exposed to a wide variety of traumatic events, including childhood sexual abuse (Wagenmans, Van Minnen, Sleijpen, & De Jongh, Citation2018), patients who suffer from emotion regulation difficulties (Van Toorenburg et al., Citation2020), dissociative symptoms (Zoet, De Jongh, & van Minnen, Citation2021; Zoet, Wagenmans, Van Minnen, Sleijpen, & De Jongh, Citation2018), high rates of comorbidity including symptoms of borderline personality (De Jongh et al., Citation2020), or suicidal ideation (Van Woudenberg et al., Citation2018), and even for patients suffering from Complex PTSD (Voorendonk, De Jongh, Rozendael, & Van Minnen, Citation2020).
With regard to the latter category of PTSD patients, according to the most recent version of the International Classification of Diseases (11th Revision, ICD-11; Maercker et al., Citation2013) individuals fulfil the diagnostic criteria of Complex PTSD if they can be classified as having PTSD supplemented by three symptom clusters, indicating difficulties in regulating emotions, problems in establishing and maintaining interpersonal relationships, and the presence of negative beliefs about self, others, or the world (Maercker et al., Citation2013). In the literature on Complex PTSD these three symptom clusters are collectively referred to as the DSO (Disorders of Self Organization) construct (Ford, Citation2020). Because Complex PTSD is often due to early childhood interpersonal trauma (McLean, Toner, Jackson, Desrocher, & Stuckless, Citation2006) it has been argued that adults with symptoms characteristic of Complex PTSD would respond poorly to trauma-focused interventions. Accordingly, it has been recommended that the treatment of these individuals should be phased, according to the so-called three-phase model (Cloitre et al., Citation2012). In recent years, however, evidence is mounting that an immediate trauma-focused approach in the treatment of symptoms of Complex PTSD, without a stabilization phase, is safe and effective (De Jongh et al., Citation2016; Karatzias et al., Citation2019; Oprel et al., Citation2021; Van Vliet, Huntjens, van Dijk, & De Jongh, Citation2021).
In reaction to the outbreak of the COVID-19 pandemic, we delivered this intensive trauma-focused therapy programme for individuals with PTSD and Complex PTSD using home-based telehealth. In a recent study, we explored the first results of this fully remote-controlled therapy programme (Bongaerts, Voorendonk, Van Minnen, & De Jongh, Citation2021). Six people attended the programme in their own home, or at a place guaranteeing enough privacy. Patients suffered from PTSD due to exposure to several traumatic events, usually during early childhood. Four of them were diagnosed with Complex PTSD. PTSD severity scores diminished significantly from pre-treatment to four weeks follow-up, with a large effect size. Four of the six patients lost either their PTSD or Complex PTSD diagnostic status after participating in the treatment programme. No one dropped out, and no other adverse effects occurred. However, the main limitation of this feasibility study was that the study had few participants, and that no follow-up data were available. Hence, studies of remotely delivered intensive trauma-focused therapy with a follow-up period longer than only four weeks are lacking, but are necessary to verify whether this treatment modality can be a feasible alternative to face-to-face administered intensive trauma-focused treatment.
Therefore, the purpose of the present study was to replicate these first and promising results using another and larger, independent sample with a longer follow-up period. We hypothesized that the online variant of our intensive treatment programme would be safe (i.e. an absence of significant worsening of symptoms, no occurrence of personal adverse events, and a low dropout rate), also that patients’ (Complex) PTSD symptom severity (including the DSO symptom cluster, i.e. affective dysregulation, negative self-concept, and disturbances in relationships) would diminish significantly, and that at six months follow-up these results could be maintained. Given the brevity of the therapy programme we were also interested to explore patients’ change of diagnostic status (PTSD and Complex PTSD classification) (Maercker et al., Citation2013).
2. Method
2.1. Participants
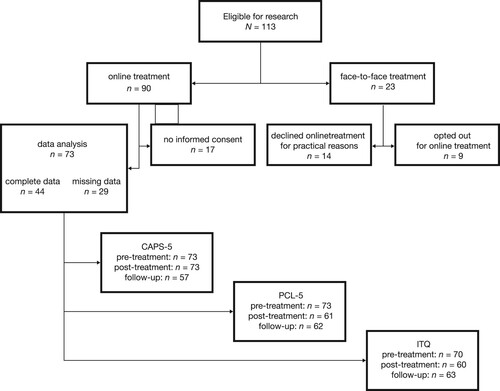
This study was carried out at the Psychotrauma Expertise Centre (PSYTREC), a mental health centre in Bilthoven, The Netherlands. From April 2020, at the beginning of the COVID-19 pandemic, until August 2020, 113 patients were treated within a four-day programme (i.e. 90 online, 23 face-to-face). Of the latter, for 14 patients online treatment was not an option due to practical reasons (no experience in using a computer, family circumstances, or no place with enough privacy to follow the programme), and 9 patients opted out for online treatment. Of the total of 90 patients who were eligible for research, 17 patients did not provide informed consent for research, and from 29 patients there were missing data of at least one measurement. Accordingly, for the purpose of the present study and depending on available data for different analyses, the results of at most 73 patients were analysed ( shows the patient flow). The mean age of this group of participants was 37.16 years (SD = 11.82, age range 19–63), and 62 (85%) were female. According to the LEC-5, all 73 participants had been exposed to multiple traumatic events. At baseline 86.3% of the 73 patients of this study also suffered from at least one other, comorbid mental health condition (i.e. depressive disorders 53.4%, anxiety disorders 54.8%). Of these participants, 19 (26.0%) reported moderate to high suicidal risk based on the M.I.N.I. PLUS. All 73 patients suffered from PTSD according to the CAPS-5. Furthermore, 33 (47.1%, n = 70) participants fulfilled all diagnostic criteria for Complex PTSD according to the ITQ. Mean scores of the three instruments along with the descriptives can be found in .
Table 1. Descriptives of the total sample of patients at baseline: Mean scores of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5), PTSD Checklist for DSM-5 (PCL-5), and International Trauma Questionnaire (ITQ), age and sex, PTSD and Complex PTSD diagnosis, traumatic events according to the Life Events Checklist for DSM-5 (LEC-5), comorbidity, suicidal ideation.
2.2. Procedure
Written informed consent was obtained from all study participants at intake. A medical ethical exemption has been granted (IRB00002991, FWA00017598). After reference to the institution by a psychologist, a psychiatrist or their general practitioner, participants were invited for an intake procedure (two sessions). During the two (mostly online) intake sessions assessment took place whether the participants fulfilled the DSM-5 criteria for PTSD-diagnosis, and participants were checked for eligibility. The inclusion criteria for the treatment programme were: a classification of PTSD, 18 years or older, and an adequate understanding of the Dutch language. The only exclusion criterion for the treatment was an attempted suicide within three months before the first intake.
In the first (online) intake session trained clinical psychologists administered the Life Events Checklist for DSM-5 (LEC-5; Boeschoten, Bakker, Jongedijk, & Olff, Citation2014a), the Dutch version of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5; Boeschoten et al., Citation2018), and the Mini International Neuropsychiatric Interview (M.I.N.I. PLUS; Overbeek, Schruers, & Griez, Citation1999). Between intake session one and two self-report instruments, such as the PTSD Checklist for DSM-5 (PCL-5; Boeschoten, Bakker, Jongedijk, & Olff, Citation2014b), and the International Trauma Questionnaire (ITQ; Eidhof, Ter Heide, Boeschoten, & Olff, Citation2018) were sent online to be filled out by the participants as self-reports using computer assisted web interviewing (CAWI). In the second (online) intake session a case conceptualization and a personal treatment plan were drawn up. The therapists and other staff members monitored attrition and adverse events during the study. The participants received four days of the remotely administered intensive trauma-focused treatment (Bongaerts et al., Citation2021). At post-treatment, eight days after the last treatment day, patients were requested to complete the PCL-5, and the ITQ using a link to these questionnaires online. Also, the CAPS-5 was administered online by an independent clinical psychologist who were not blind to the treatment stage. At follow-up, six months after treatment, the CAPS-5 was administered by telephone by a research assistant, and the PCL-5, and the ITQ were administered online again.
2.3. Treatment
The treatment consisted of a brief and intensive remotely administered trauma-focused treatment programme (see Bongaerts et al., Citation2021). Patients attended the programme from their home or from a place where privacy was guaranteed to receive the psychotherapy and psycho-education sessions, and where they were able to participate in the physical activities. Psychotherapy consisted of four consecutive days of one daily individually online administered prolonged exposure therapy session (90 min) and one EMDR therapy session (90 min). Furthermore, the treatment consisted of six hours of physical activities in between the therapy sessions, and about three hours of psycho-education during the day and in the evening. The treatment programme was offered without a preparation or stabilization phase. The programme as described by Van Woudenberg et al. (Citation2018) was adapted for administration via telehealth. The patients were sent a secure videoconferencing link (Zoom.us) a few minutes before the therapy session. According to the principles of ‘therapist rotation’ (Van Minnen et al., Citation2018) each session was administered by a different therapist who worked either at home or at the centre, and the therapists were trained in both prolonged exposure therapy and/or EMDR therapy.
2.4. Assessment instruments
Information about the experienced type of traumatic events was obtained by the Life Events Checklist for DSM-5 (LEC-5; Boeschoten, Bakker, Jongedijk, & Olff, Citation2014a; Weathers et al., Citation2013). This is a self-report measure that assesses exposure to 17 events known to potentially result in PTSD.
To establish the PTSD diagnosis based on the DSM-5 and to measure the severity of PTSD symptoms, the Dutch version of the CAPS-5 (Boeschoten et al., Citation2018) was used as the primary outcome measure. At pre-treatment and at six months follow-up, the CAPS-5 month version was administered, at post-treatment the CAPS-5 week version was used. The Dutch version of the CAPS-5 has good internal consistency and reliability (Boeschoten et al., Citation2018). Cronbach’s alpha of this clinical interview in the present study was 0.76.
To measure PTSD symptom severity, the Dutch version of the PTSD Checklist (PCL-5; Boeschoten, Bakker, Jongedijk, & Olff, Citation2014b; Bovin et al., Citation2016) was used as a self-report measure at pre-treatment, at post-treatment, and at six months follow-up. The PCL-5 is based on the PTSD diagnostic criteria of the DSM-5 and consists of 20 items with a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). The total score ranges from 0 to 80. Cronbach’s alpha of this questionnaire in the present study was 0.86.
To be able to establish a Complex PTSD (CPTSD) diagnosis based on the ICD-11, the Dutch version of the International Trauma Questionnaire (ITQ) was used at pre- and post-treatment, and at six months follow-up (Cloitre et al., Citation2018; Eidhof et al., Citation2018). The ITQ is a self-report measure of 12 items consisting of three symptom clusters referring to PTSD (re-experiencing, avoidance and sense of threat) and three additional symptom clusters referring to DSO (Disturbances in Self Organization: affective dysregulation, disturbances in relationships and negative self-concept). A Complex PTSD diagnosis is based on a combination of both PTSD and DSO symptom clusters. The total severity score of the DSO-symptoms was calculated by adding the scores of all six DSO-symptoms (ITQ-DSO; range 0-24; Hyland et al., Citation2017). The 12-item version has been proved to be a valid measure to assess CPTSD based on the ICD-11 (Cloitre et al., Citation2018). Cronbach’s alpha of this questionnaire in the present study was 0.73.
The Dutch version of Mini-International Neuropsychiatric Interview (M.I.N.I. PLUS; Lecrubier et al., Citation1997; Overbeek et al., Citation1999; Sheehan et al., Citation1998) is a structured well-validated diagnostic interview to assess psychiatric disorders and suicide risk (suicide attempts in the previous month and/or lifetime). For each disorder, dichotomous scores could be obtained (yes or no) and suicidal risk was categorized in ‘low’, ‘moderate’ and ‘high’.
Safety of treatment was defined as the absence of worsening of PTSD symptoms, no personal adverse events, such as suicidal attempts, serious self-injurious behaviour (injuries that needed medical care), and no drop out.
2.5. Statistical analysis
To determine whether data were missing at random, Little’s MCAR test was performed. In addition, t-tests and χ2-tests were conducted to determine whether participants with complete data (n = 44) differed significantly from participants with missing data. To make a comparison between the CAPS-5 and PCL-5 scores before treatment, after treatment and at six months follow-up, several multi-level regression models were performed. For each of these two measures, the same steps were taken. Corresponding assumptions were checked and were met. Additionally, paired samples t-tests were conducted with data from all 73 participants to check for specific differences between measurement points. Paired samples t-tests were also conducted with data from both the patients suffering from PTSD only, and those suffering from CPTSD at pre-treatment. For within-group effect sizes for these groups, Cohen’s ds were calculated using the pre-treatment, post-treatment and six months follow-up means, and standard deviations of the relevant outcome measures. To determine whether the proportion of patients with either PTSD or Complex PTSD, who responded to the treatment, would differ at any of the measurement time points, McNemar’s tests were used. The level of significance for all statistical analyses was set at α = .05. All main analyses were conducted with the software program R (Version 4.0.3; R Core Team, Citation2020), and the ‘nlme’ package (Pinheiro, Bates, DebRoy, Sarkar & R Core Team, Citation2020); missing value analysis (MVA) was performed with SPSS 25 (IBM SPSS).
3. Results
3.1. Participants
A non-significant Little’s MCAR test (χ²[95] = 76.35, p = .92) indicated that missing data appeared in a random way. No differences in characteristics were found between participants with or without missing data at baseline, barring age (M = 39.39; SD = 12.22 and M = 33.79; SD = 10.52, respectively; t[71] = 2.02, p = .047). Furthermore, no significant differences at post-treatment or follow-up could be detected between the participants with complete scores and those with some missing data on the CAPS-5 or the PCL-5.
3.2. CAPS-5
The addition of predictors and covariates to the random intercept model improved the fit significantly, (Δχ²[6] = 189.59, p < .001). Adding a random slope for ‘measurement time point’ improved the fit of the model again (Δχ²[5] = 53.37, p < .001), which led to our main models 1 and 2 (see ). The intercept for Model 1 (b0 = 35.79, SE = 1.41) represents the estimated mean value for the reference group at pre-treatment (reference group is ‘woman of average age, without Complex PTSD at pre-treatment and no missing data for the three instruments). On average, men and women showed a similar score pattern on all three measurements. Also, age did not have a significant effect on CAPS-5 score (b = 0.06, SE = 0.07, p = .40).
Participants with some missing data on the three instruments did not score differently on any of the three measurements. On all three measurements (pre-treatment, post-treatment, follow-up), participants with Complex PTSD at pre-treatment scored systematically higher compared to participants without Complex PTSD at pre-treatment.
Overall, the difference in mean CAPS-5 score between pre-treatment and post-treatment was significant (b = −25.81, p < .001), showing a large effect size (d = 2.12). The difference between pre-treatment and six months follow-up proved also significant (b = −23.15, p < .001; d = 1.61). Adding the interaction term between measurement time point and Complex PTSD had no significant impact on model fit (, ).
Figure 2. Predicted mean scores of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) for patients with PTSD and patients with Complex PTSD across the three measurement points (n = 70). Error bars represent 95% CI’s for the mean.
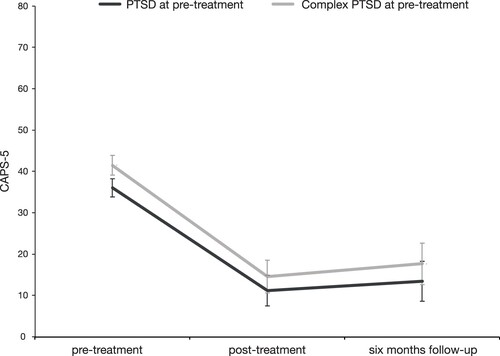
Table 2. Multilevel regression analyses of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5) by measurement moment, age and sex, and Complex PTSD.
Paired samples t-tests performed for the whole sample showed a significant decrease (23.16 points, t[56] = 12.14, p < .001, d = 1.61) between pre-treatment to six months follow-up. While the scores decreased significantly between pre-treatment and post-treatment (25.59 points, t[72] = 18.11, p < .001, d = 2.12), a small (2.84 points), but significant increase from post-treatment to six months follow-up was found (t[56] = 2.31, p = .025, d = 0.31; see ). Paired samples t-tests, separately performed for the subgroups of patients with either PTSD or CPTSD at pre-treatment, showed no differences between the mean scores at post-treatment and at six month follow-up (t[27] = 1.33, p = .19, d = 0.25, and t[26] = 1.66, p = .11, d = 0.32, respectively; see and ).
3.3. PCL-5
For the PCL-scores the same analytic procedure was applied with a similar pattern of findings for the multilevel analyses (see , ). Paired samples t-tests conducted using the data of the whole sample showed a significant decrease between pre-treatment and six months follow-up (22.52 points, t[61] = 11.04, p < .001, d = 1.40). It appeared that from pre-treatment to post-treatment the PCL-5 scores decreased significantly (25.82 points, t[60] = 12.42, p < .001, d = 1.59), while from post-treatment to six months follow-up a small, marginally significant, relapse occurred (3.20 points, t[54] = 2.05, p = .045, d = 0.28; see ). A paired samples t-test showed no increase in PCL-5 scores of patients with PTSD between post-treatment and six months follow-up, (t[27] = 0.58, p = .56, d = 0.11), whereas regarding those who suffered from CPTSD a small, but significant increase was found (4.85 points, t[25] = 2.10, p = .046, d = 0.41; and ).
Figure 3. Predicted mean scores of the PTSD Checklist for DSM-5 (PCL-5) for patients with PTSD and patients with Complex PTSD across the three measurement points (n = 70). Error bars represent 95% CI’s for the mean.

Table 3. Multilevel regression analyses of the PTSD Checklist for DSM-5 (PCL-5) by measurement moment, age and sex, and Complex PTSD.
Table 4. Pairwise comparisons of pre-, post-treatment and follow-up scores for the whole sample.
Table 5. Pairwise comparisons of pre-, post-treatment and follow-up scores for patients with PTSD at pre-treatment.
Table 6. Pairwise comparisons of pre-, post-treatment and follow-up scores for patients with complex PTSD at pre-treatment.
3.4. ITQ-DSO
Paired samples t-tests performed on the data of the whole sample showed a significant reduction of the ITQ-DSO scores from pre-treatment to six months follow-up (5.69 points, t[61] = 7.21, p < .001, d = 0.92). From pre-treatment to post-treatment the scores decreased significantly (6.73 points; t[58] = 9.04, p < .001, d = 1.18), whereas a small marginally significant increase from post-treatment to six months follow-up (1.31 points, t[54] = 2.01, p = .049, d = 0.27) was found (See ).
Paired samples t-tests were conducted to compare the ITQ-DSO mean scores between the different measurement time points for the two groups separately (see and ). For both the patients with PTSD only, and those with CPTSD the average ITQ-DSO scores decreased significantly from pre- to post-treatment (4.58 points, t[30] = 5.34, p < .001, d = 0.96 and 9.11 points, t[27] = 8.30, p < .001, d = 1.57, respectively). From post-treatment to six months follow-up changes did not reach significance ( and ).
3.5. Loss of diagnoses
Overall, at post-treatment, of the 73 participants with PTSD, 82.2% no longer met the diagnostic criteria for this condition (according to the CAPS-5). More specifically, from pre- to post-treatment, the percentage of participants fulfilling the diagnostic criteria of PTSD dropped significantly from 100% to 17.8% (McNemar’s test: χ²[1] = 58.02, p < .001). From post-treatment to six months follow-up (with 57 pairs of available data of which 8 [14%] participants with PTSD) this percentage increased, albeit not significantly, to 24.6% (McNemar’s test, χ²[1] = 2.50: p = .11). At pre-treatment 33 (47.1%) of the 70 patients met the diagnostic criteria of CPTSD according to the ITQ. At post-treatment, seven patients (10.1%) met the diagnostic criteria of CPTSD, and 53 (75.7%) did not. Due to missing data, of 10 patients (14.3%) the diagnostic status could not be determined. At six months follow-up, of the 70 patients, 12 (17.1%) fulfilled the diagnostic criteria of CPTSD, 51 (72.9%) did not fulfil these criteria and of seven patients (10,0%) the diagnostic status was unknown due to missing data. Using only available data McNemar’s test for comparison of paired proportions showed that from pre- to post-treatment (59 pairs of available data) the number of participants with Complex PTSD, according to the ITQ-DSO, decreased significantly from 28 (47.1%) to 6 (10.2%; McNemar’s test, χ²[1] = 16.96: p < .001). From post-treatment to six months follow-up (with 55 pairs of available data) the number of participants with Complex PTSD non-significantly increased from 6 (10.9%) to 11 (20.0%) (McNemar’s test, χ²[1] = 2.29: p = .13).
3.6. Safety
Limited technical problems occurred during the online treatment programme. In the course of the COVID-19 pandemic and the remotely administered intensive trauma-focused therapy programme, therapists became inventive in solving small technical issues. This may have led to the fact that participants did not leave the session or were otherwise disengaging from the therapeutic communication in an inappropriate way. Furthermore, neither adverse events such as suicidal attempts, nor serious self-injuries associated with the remotely administered treatment were reported, and no participants dropped out of treatment before completion of the four treatment days.
4. Discussion
This study was conducted to determine the feasibility, safety and effects of a brief, fully remotely administered intensive trauma-focused treatment for patients with chronic PTSD and Complex PTSD. Overall, the results of the present study replicate those of a previous study among six patients with similar complexity (Bongaerts et al., Citation2021), and are supportive of our hypothesis that remotely delivered intensive trauma-focused treatment is safe and that patients’ PTSD symptom severity would decrease significantly following treatment. This conclusion is not only underlined by a large decrease in symptoms, both regarding core features of PTSD and so-called disturbances in self-organization, but also by a significant loss of both PTSD and Complex PTSD diagnoses, and a remarkable lack of occurrence of personal adverse events, and attrition.
The present results are in accordance with other studies showing that remotely administered psychotherapy is a useful, effective and an efficient treatment alternative (Acierno et al., Citation2016, Citation2017; Germain et al., Citation2009; Morland et al., Citation2014, Citation2020; Tuerk et al., Citation2010; Turgoose et al., Citation2018). The results are also in line with an increasing number of studies showing that brief, intensive trauma-focused treatment programmes are capable of yielding a fast decline in PTSD symptoms (Bongaerts, Van Minnen, & De Jongh, Citation2017, Ehlers et al., Citation2014; Sciarrino et al., Citation2020; Van Woudenberg et al., Citation2018; Wachen et al., Citation2019), and Complex PTSD symptoms (Voorendonk et al., Citation2020), without a stabilization phase, within just one or two weeks. What is more, the effect sizes in our study are at least not worse and, if anything, larger than those in our previous related studies with face-to-face intensive trauma-focused treatment in other samples consisting of a comparable patient group of patients with both PTSD and Complex PTSD (Van Toorenburg et al., Citation2020; Voorendonk et al., Citation2020). Interestingly, given that our intensive trauma-focused treatment online programme was found to be associated with a large symptom decline for most of the patients with elevated levels of ITQ-DSO severity, and that treatment resulted in a significant decrease in the ITQ-DSO symptom cluster, the present results do not support the notion that patients with Complex PTSD would need a phase-based approach to yield positive treatment outcomes (see also De Jongh et al., Citation2016; Oprel et al., Citation2021; Van Vliet et al., Citation2021). Conversely, a small percentage of patients continued to meet the criteria for PTSD (17.8%) (n = 73) or Complex PTSD (11.7%) (n = 60) at post-treatment.
The results showed significant decreases of the CAPS-5, the PCL-5, and the ITQ-DSO scores with large effect sizes, which were maintained from pre-treatment to six months follow-up. At the same time, a small, but significant, relapse was observed between post-treatment and six months follow-up. The finding that the t-tests performed on smaller subgroups of patients with either PTSD or CPTSD did not reach significance, in the case of the CAPS-5 and ITQ-DSO scores, could be explained by a type 2 error. Conversely, it seems that the slight relapse observed is explained mainly by the patients with CPTSD (albeit only when a self-report measure of PTSD symptoms – PCL-5 – is used). To this end, it is conceivable that the mere presence of DSO symptoms (including the damaging effects of trauma exposure to patients’ self-esteem) in patients with CPTSD could make individuals more vulnerable to symptom relapse than PTSD only, particularly because the treatment programme is fully focused on targeting memories of A-criterion traumatic events and not, for example, on those involving emotional abuse, neglect or other types of memories.
A strength of the present study is the use of a combination of different self-report measures (ITQ-DSO and PCL-5) and a clinical interview (CAPS-5) to measure the same constructs. However, our study suffered from several limitations that need to be noted as well. These include the fact that of the 90 patients only 73 gave their informed consent for research and that a considerable number of patients (n = 29) had missing data on at least one measurement point. Although it appeared that data were missing at random and, except for age, the groups with and without missing data did not differ on relevant factors at baseline, post-treatment and follow-up, we cannot guarantee that the results are generalizable to populations other than we studied. We tried to resolve this by using a mixed effect model.
On the other hand, and most importantly, the study lacked a control group and randomization to ensure that the outcomes can be attributed to the intervention being tested and that the results are not due to spontaneous changes that may occur with the passage of time. Although it is very unlikely that the severity of PTSD based on early childhood trauma decreases spontaneously over a period of four days, it is important that in future studies the effectiveness of remotely administered intensive treatment programmes are compared directly to standard face-to-face intensive treatment packages for (Complex) PTSD using a randomized controlled design.
Also, important to note is that the fact that our intensive treatment programme was forced to switch to a remote variant was forced by the global COVID-19 pandemic, and the resulting lockdown. In fact, none of the therapists nor any of the patients had had any previous experience with online therapy. Also, from the perspective of the patient, it was a novel experience. Some patients afterwards indicated that they found treatment via a computer screen initially quite unusual, and did not expect this result, or as one patient expressed it: ‘I am very happy that we were able to do this online. It works!’. Others indicated that they liked to be able to stay at home and confront the traumatic memories from their safe, and day-to-day environment, not having to travel long distances to the clinic, and not having to face a group of unknown fellow patients, thus being able to focus on their own process. This notion is supported by the patients’ mean subjective evaluation score of the treatment programme (8.6, on a scale ranging from 0 to 10) and dovetails with research suggesting that it is less likely that patients feel intimidated during online therapy than during personal interactions (Chae, Park, Cho, Hong, & Cheon, Citation2000; Tachakri & Rajani, Citation2002), and that online treatment offers a more comfortable therapeutic distance between the patient and the therapist (Simpson & Reid, Citation2014).
In conclusion, although online delivered treatment is not possible for all patients, the results of the present study suggest that a brief, fully remotely administered intensive trauma-focused programme, using prolonged exposure, EMDR therapy, physical activities and psycho-education, is feasible, and a potentially safe treatment alternative for PTSD and Complex PTSD that merits more clinical and research attention.
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly.
Disclosure statement
Agnes Van Minnen receives income for published book chapters on PTSD and for the training of postdoctoral professionals in prolonged exposure. Ad De Jongh receives income from published books on EMDR therapy and for the training of postdoctoral professionals in this method. The other authors do not have competing interests.
Correction Statement
This article was originally published with errors, which have now been corrected in the online version. Please see Correction (http://dx.doi.org/10.1080/20008066.2024.2355052)
Additional information
Funding
References
- Acierno, R., Gros, D. F., Ruggiero, K. J., Hernandez-Tejada, M. A., Knapp, R. G., Lejuez, C. W., et al. (2016). Behavioral activation and therapeutic exposure for posttraumatic stress disorder: A non-inferiority trial of treatment delivered in person vs. Home-based telehealth. Depression and Anxiety, doi:10.1002/da.22476
- Acierno, R., Knapp, R., Tuerk, P., Gilmore, A. K., Lejuez, C., Ruggiero, K., … Foa, E. B. (2017). A non-inferiority trial of prolonged exposure for posttraumatic stress disorder: In person versus home-based telehealth. Behaviour Research and Therapy, 89, 57–65. doi:10.1016/j.brat.2016.11.009
- Backhaus, A., Agha, Z., Maglione, M., Repp, A., Ross, B., Zuest, D., … Thorp, S. (2012). Videoconferencing psychotherapy: A systematic review. Psychological Services, 9(2), 111–131. doi: 10.1037/a0027924
- Boeschoten, M. A., Bakker, A., Jongedijk, R. A., & Olff, M. (2014a). Life events checklists for DSM-5 (LEC-5)-Dutch Version. Diemen, The Netherlands: Arq Psychotrauma ExpertGroep.
- Boeschoten, M. A., Bakker, A., Jongedijk, R. A., & Olff, M. (2014b). PTSS Checklist voor de DSM-5 (PCL-5) [PTSDchecklist for the DSM-5(PCL-5)]. Diemen: ArqAcademy.
- Boeschoten, M. A., Van der Aa, N., Bakker, A., Ter Heide, F. J. J., Hoofwijk, M. C., Jongedijk, R. A., & Olff, M. (2018). Development and evaluation of the Dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). European Journal of Psychotraumatology, 9(1), 1546085. doi:10.1080/20008198.2018.1546085
- Bongaerts, H., Van Minnen, & De Jongh, A. (2017). Intensive EMDR to treat PTSD patients with severe comorbidity: A case series. Journal of EMDR Practice and Research, 11(2), 84–95. doi:10.1891/1933-3196.11.2.84
- Bongaerts, H., Voorendonk, E. M., Van Minnen, A., & De Jongh, A. (2021). Safety and effectiveness of intensive treatment for complex PTSD delivered via home-based telehealth. European Journal of Psychotraumatology, 12(1), 1860346. doi:10.1080/20008198.2020.1860346
- Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28, 1379.
- Chae, Y. M., Park, H. J., Cho, J. G., Hong, G. D., & Cheon, K. A. (2000). The reliability and acceptability of telemedicine with schizophrenia in Korea. Journal of Telemedicine and Telecare, 6, 83–90. doi:10.1258/1357633001935095
- Cloitre, M., Courtois, C. A., Ford, J. D., Green, B. L., Alexander, P., & Briere, J. (2012). The ISTSS expert consensus treatment guidelines for complex PTSD in adults. http://www.istss.org/AM/Template.cfm?Section=ISTSS_Complex_PTSDTreatment_Guidelines&Template=/CM/ContentDisplay.cfm&ContentID=5185.
- Cloitre, M., Shevlin, M., Brewin, C., Bisson, J., Roberts, N., Maercker, A., … Hyland, P. (2018). The international trauma questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138, 536–546. doi:10.1111/acps.12956
- De Jongh, A., Groenland, G.N., Sanches, S., Bongaerts, H., Voorendonk,,E.M., & Van Minnen, A. (2020). The impact of brief intensive trauma-focused treatment for PTSD on symptoms of borderline personality disorder. European Journal of Psychotraumatology. doi:10.1080/20008198.2020.1721142
- De Jongh, A., Resick, P. A., Zoellner, L. A., van Minnen, A., Lee, C. W., Monson, C. M., … Bicanic, I. A. E. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33, 359–369.
- Ehlers, A., Hackmann, A., Grey, N., Wild, J., Liness, S., Albert, I., … Clark, D. M. (2014). A randomized controlled trial of 7-Day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. American Journal of Psychiatry, 171, 294–304.
- Eidhof, M., Ter Heide, F., Boeschoten, M., & Olff, M. (2018). Internationale Trauma Vragenlijst: Zelfrapportage vragenlijst voor ICD-11 PTSS en CPTSS. Nederlandstalige versie. [Internet]. Uitgave Arq Psychotrauma Expert groep, Diemen. p. 1–5. http://www.psychotraumadiagnostics.centrum45.nl/.
- Ford, J. D. (2020). New findings questioning the construct validity of complex posttraumatic stress disorder (cPTSD): let’s take a closer look. European Journal of Psychotraumatology, 11(1), 1708145. doi:10.1080/20008198.2019.1708145
- Germain, V., Marchand, A., Bouchard, S., Drouin, M., & Guay, S. (2009). Effectiveness of cognitive behavioural therapy administered by videoconference for posttraumatic stress disorder. Cognitive Behaviour Therapy, 38, 42–53. doi:10.1080/16506070802473494
- Hilty, D., Ferrer, D., Parish, M., Johnston, B., Callahan, E., & Yellowlees, P. (2013). The effectiveness of telemental health: A 2013 review. Telemedicine and e-Health, 19(6), 444–454.
- Hyland, P., Shevlin, M., Brewin, C., Cloitre, M., Downes, A., Jumbe, S., … Roberts, N. (2017). Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the international trauma questionnaire. Acta Psychiatrica Scandinavia, 136: 313–322.
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., … Hutton, P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 1–15. doi:10.1017/S0033291719000436
- Lecrubier, Y., Sheehan, D. V., Weiller, E., Amorim, P., Bonora, I., Harnett Sheehan, K., … Dunbar, G. C. (1997). The mini international neuropsychiatric inter-view (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12, 224–231.
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Reed, G. M., Ommeren, M. V., … Saxena, S. (2013). Proposals for mental disorders specifically associated with stress in the international classification of diseases-11. The Lancet, 381(9878), 1683–1685.
- McLean, L. M., Toner, B., Jackson, J., Desrocher, M., & Stuckless, N. (2006). The relationship between childhood sexual abuse, complex post-traumatic stress disorder and alexithymia in two outpatient samples: Examination of women treated in community and institutional clinics. Journal of Child Sexual Abuse, 15(3), 1–17. doi:10.1300/J070v15n03_01
- Mohr, D., Burns, M., Schueller, S., Clarke, G., & Klinkman, M. (2010). Behavioral intervention technologies: Evidence review and recommendations for future research. General Hospital Psychiatry, 35(4), 332–228. doi:10.1016/j.genhosppsych.2013.03.008
- Morland, L. A., Mackintosh, M. A., Greene, C. J., Rosen, C. S., Chard, K. M., Resick, P., & Frueh, B. C. (2014). Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: A randomized noninferiority clinical trial. The Journal of Clinical Psychiatry, 75(5), 470–476.
- Morland, L. A., Wells, S. Y., Glassman, L. H., Greene, C. J., Hoffman, J. E., & Rosen, C. S. (2020). Advances in PTSD treatment delivery: Review of findings and clinical considerations for the use of telehealth interventions for PTSD. Current Treatment Options in Psychiatry, 7, 221–241. doi:10.007/s40501-020-00215-x
- Olthuis, J. V., Wozney, L., Asmundson, G. J. G., Cramm, H., Linley-Pottie, P., & McGrath, P. J. (2016). Distance-delivered interventions for PTSD: A systematic review and meta-analysis. Journal of Anxiety Disorders, 44, 9–26. DOI: 10.1016/j.janxdis.2016.09.010
- Oprel, D. A. C., Hoeboer, C. M., Schoorl, M., De Kleine, R. A., Cloitre, M., Wigarde, I. G., … Van der Does, W. (2021). Effect of prolonged exposure, intensified prolonged exposure and STAIR + prolonged exposure in patients with PTSD related to childhood abuse: A randomized controlled trial. European Journal of Psychotraumatology, 12), doi:10.1080/20008198.2020.1851511
- Overbeek, T., Schruers, K., & Griez, E. (1999). Mini international neuropsychiatric interview: Nederlandse Versie 5.0.0 [Dutch Version]. Maastricht, Netherlands: Universiteit van Maastricht.
- Pinheiro, J., Bates, D., DebRoy, S., Sarkar, D., & R Core Team (2020). _nlme: Linear and nonlinear mixed effects models_. R package version 3.1-149, <URL: https://CRAN.R-project.org/package = nlme>.
- R Core Team. (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
- Sciarrino, N. A., Warnecke, A. J., & Teng, E. J. (2020). A systematic review of intensive empirically supported treatments for posttraumatic stress disorder. Journal of Traumatic Stress, 00, 1–12.
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. C. (1998). The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diag-nostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59, 22–33.
- Simpson, S. G., & Reid, C. L. (2014). Therapeutic alliance in videoconferencing psychotherapy: A review. Australian Journal of Rural Health, 22, 280–299. doi:10.1111/ajr.12149
- Tachakri, S., & Rajani, R. (2002). Social presence in telemedicine. Journal of Telemedicine and Telecare, 8(4), 226–230. doi 10.1258/135763302320272202
- Thorp, S. R., Fidler, J., Moreno, L., Floto, E., & Agha, Z. (2012). Lessons learned from studies of psychotherapy for posttraumatic stress disorder via video teleconferencing. Psychological Services, 9, 197–199.
- Todder, D., & Kaplan, Z. (2007). Rapid eye movements for acute stress disorder using video conference communication. Telemedicine and e-Health, 13, 461–463. doi:10.1089/tmj.2006.0058
- Tuerk, P. W., Yoder, M., Ruggiero, K. J., Gros, D. F., & Acierno, R. (2010). A pilot study for prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. Journal of Traumatic Stress, 23, 116–123. doi:10.1002/jts.20494
- Turgoose, D., Ashwick, R., & Murphy, D. (2018). Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. Journal of Telemedicine and Telecare, 24(9), 575–585. doi:10.1177/1357633X17730443
- Van Minnen, A., Hendriks, L., de Kleine, R., Hendriks, G.-J., Verhagen, M., & De Jongh, A. (2018). Therapist rotation: A novel approach for implementation of trauma-focused treatment in post-traumatic stress disorder. European Journal of Psychotraumatology, 9, 1. doi:10.1080/20008198.2018.1492836
- Van Toorenburg, M.M., Sanches, S.A., Linders, B., Rozendaal, L., Voorendonk, E. M., Van Minnen, A. & De Jongh, A. (2020) Do emotion regulation difficulties affect outcome of intensive trauma-focused treatment of patients with severe PTSD? European Journal of Psychotraumatology, 11(1), 1724417. doi:10.1080/20008198.2020.1724417
- Van Vliet, N. I., Huntjens, R. J. C., van Dijk, M. K., & De Jongh, A. (2021). Phase-based treatment versus immediate trauma-focused treatment for post-traumatic stress disorder due to childhood abuse: Randomised clinical trial. British Journal of Psychiatry Open, 7(e211), 1–7. doi:10.1192/bjo.2021.1057
- Van Woudenberg, C., Voorendonk, E. M., Bongaerts, H., Zoet, H. A., Verhagen, M., Van Minnen, A., … De Jongh, A. (2018). The effectiveness of an intensive treatment programme combining prolonged exposure and EMDR for severe posttraumatic stress disorder (PTSD). European Journal of Psychotraumatology, 9, 1. doi:10.1080/20008198.2018.1487225
- Varker, T., Brand, R., Ward, J., Terhaag, S., & Phelps, A. (2018). Efficacy of synchronous telepsychology interventions for people with anxiety, depression, posttraumatic stress disorder, and adjustment disorder: A rapid evidence assessment. Psychological Services. Available from, doi:10.1037/ser0000239
- Voorendonk, E. M., De Jongh, A., Rozendael, L., & Van Minnen, A. (2020). Trauma-focused treatment outcome for complex PTSD patients: Results of an intensive treatment programme. European Journal of Psychotraumatology, 11, 1. doi: 10.1080/20008198.2020.1783955
- Wachen, J. S., Dondanville, K. A., Evans, W. R., Morris, K., & Cole, A. (2019). Adjusting the timeframe of evidence-based therapies for PTSD-massed treatments. Current Treatment Options in Psychiatry, 6, 107–118. doi:10.1007/s40501-019-00169-9
- Wagenmans, A., Van Minnen, A., Sleijpen, M., & De Jongh, A. (2018). The impact of childhood sexual abuse on the outcome of intensive trauma-ftocused treatment for PTSD. European Journal of Psychotraumatology, 9(1), 1430962. doi:10.1080/20008198.2018.1430962
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov.
- Wootton, R., Yellowlees, P., & McLaren, P. (2003). Telepsychiatry and E-mental health. Psychological Medicine, 33(8), 1488–1489. doi:10.1017/s0033291703238964
- Zoet, H. A., Wagenmans, A., Van Minnen, A., Sleijpen, M., & De Jongh, A. (2018). Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology, 9(1), doi:10.1080/20008198.2018.1468707
- Zoet, H.A., De Jongh, A. & van Minnen. (2021). Somatoform dissociative symptoms have no impact on the outcome of trauma-focused treatment for severe PTSD. Journal of Clinical Medicine 2021, 10, 1553. doi:10.3390/jcm10081553