ABSTRACT
Background: Women who have had miscarriages or stillbirths are known to have a high risk for enduring grief. However, the course and frequency of enduring grief in this subgroup are not fully understood.
Objective: Our aims were to assess the intensity of grief and its course in women with miscarriages or stillbirths and to estimate the frequency of severe grief reactions in this population. Additionally, we compared subgroups with miscarriages versus stillbirths and with single versus recurrent pregnancy loss.
Method: A systematic literature search of the databases MEDLINE, psycINFO and PSYNDEX was conducted to consider all studies published between 2000 and 31 March 2022 in English or German on the prevalence and intensity of grief in women who had miscarriages or stillbirths. Studies that used validated assessment methods were included in this systematic review. The PRISMA guidelines were followed.
Results: Study characteristics and grief data were extracted independently by two investigators from 13 cross-sectional and eight longitudinal studies from 11 countries (N = 2597). All studies used self-reporting instruments. According to 17 of 21 studies (81%), grief is markedly elevated in women after miscarriages or stillbirths. The studies are very heterogeneous regarding the samples, the length of pregnancies and the time of assessment regarding grief after miscarriages. Most studies document intense grief and frequent severe grief reactions – with a decrease over time – in women who have had miscarriages or stillbirths. Clear conclusions regarding corresponding differences between women with miscarriages and stillbirths or single and recurrent pregnancy losses cannot be drawn.
Conclusions: Pronounced grief is frequent in women who had miscarriages or stillbirths. More longitudinal studies are needed to examine the course of grief in this group and to identify those women who develop prolonged grief disorder, depression or other mental-health problems.
HIGHLIGHTS
Pronounced grief is frequent in women who had miscarriages or stillbirths.
More longitudinal studies are needed to examine the course of grief in this group and to identify those women who develop prolonged grief disorder, depression or other mental-health problems.
Antecedentes: Se sabe que las mujeres que han tenido abortos espontáneos o mortinatos tienen un alto riesgo de sufrir un duelo persistente. Sin embargo, el curso y la frecuencia del duelo persistente en este subgrupo no se conocen del todo.
Objetivo: Nuestros objetivos fueron evaluar la intensidad del duelo y su curso en mujeres con abortos espontáneos o mortinatos y estimar la frecuencia de las reacciones de duelo graves en esta población. Además, comparamos subgrupos con abortos espontáneos frente a mortinatos y con pérdidas de embarazo únicas frente a recurrentes.
Método: Se realizó una búsqueda bibliográfica sistemática en las bases de datos MEDLINE, psycINFO y PSYNDEX para considerar todos los estudios publicados entre el año 2000 y el 31 de marzo de 2022 en inglés o alemán sobre la prevalencia e intensidad del duelo en mujeres que tuvieron abortos espontáneos o mortinatos. Se incluyeron en esta revisión sistemática los estudios que utilizaron métodos de evaluación validados. Se siguieron las directrices PRISMA.
Resultados: Dos investigadores extrajeron de forma independiente las características de los estudios y los datos sobre el duelo de 13 estudios transversales y ocho longitudinales de once países (N=2597). Todos los estudios utilizaron instrumentos de autorreporte. Según 17 de 21 estudios (81%), el duelo es muy elevado en las mujeres después de un aborto espontáneo o un mortinato. Los estudios son muy heterogéneos en cuanto a las muestras, la duración de los embarazos y el momento de la evaluación del duelo tras los abortos espontáneos. La mayoría de los estudios documentan un duelo intenso y frecuentes reacciones de duelo severas -con una disminución en el tiempo- en mujeres que han tenido abortos espontáneos o mortinatos. No se pueden extraer conclusiones claras sobre las diferencias correspondientes entre las mujeres con abortos espontáneos y mortinatos o con pérdidas de embarazos únicos y recurrentes.
Conclusiones: El duelo prolongado es frecuente en las mujeres que han tenido abortos espontáneos o mortinatos. Se necesitan más estudios longitudinales para examinar el curso del duelo en este grupo e identificar a las mujeres que desarrollan un trastorno de duelo prolongado, depresión u otros problemas de salud mental.
背景:众所周知,流产或死产的女性承受哀伤的风险很高。然而,该亚组中持续哀伤的过程和频率尚不完全清楚。
目的:我们旨在评估流产或死产女性的哀伤强度及其过程,并估计该人群中严重哀伤反应的频率。此外,我们比较了流产与死产以及单次流产与周期性流产的亚组。
方法:对数据库 MEDLINE、psycINFO 和 PSYNDEX 进行了系统的文献检索,以考虑 2000 年至 2022 年 3 月 31 日期间以英语或德语发表的所有关于流产或死产女性的哀伤流行率和强度的研究。本系统综述纳入了使用经过验证的评估方法的研究。遵循了 PRISMA 指南。
结果:研究特征和哀伤数据由来自 11 个国家 (N=2597) 的 13 个横断面研究和 8 个纵向研究,由两名研究人员独立提取。所有研究都使用自我报告工具。根据 21 项研究中的 17 项 (81%),流产或死产后女性的哀伤感显著升高。这些研究在样本、怀孕时间和流产后哀伤评估时间方面存在很大差异。大多数研究记录了流产或死产的女性强烈的哀伤和频繁的严重哀伤反应随着时间的推移而减少。无法就流产和死产或单次和周期性流产的女性之间的相应差异得出明确结论。
结论:流产或死产的女性经常表现出明显的哀伤。需要更多的纵向研究来考查这一群体的哀伤过程,并识别那些会出现延长哀伤障碍、抑郁或其他心理健康问题的女性。
1. Introduction
Miscarriages are very common, with about 23 million miscarriages occurring worldwide per annum (Quenby et al., Citation2021). According to a recent review, about 15% of all recognized pregnancies result in a miscarriage (Quenby et al., Citation2021). The population prevalence of females who were affected by one miscarriage was 10.8% (Quenby et al., Citation2021); this prevalence is markedly lower for women who had at least two miscarriages (two: 1.9%; three or more: 0.7%) (Quenby et al., Citation2021). Regarding stillbirths, their annual frequency is about 2.6 million worldwide (Burden et al., Citation2016; Heazell et al., Citation2016). According to Cook and Phillips (Cook & Phillips, Citation1995), the death of a child is the most severe loss experienced by a human being. The loss of an unborn child, though often not well acknowledged, is associated with high levels of distress. In line with these findings, many individuals (both women and men) have told about their experience of intense grief resulting from pregnancy loss (Brier, Citation2008). Thus, it is not surprising that miscarriages, which are frequently taboo can be risk factors for severe psychological problems (Bellieni & Buonocore, Citation2013; Murphy et al., Citation2012; Rowlands & Lee, Citation2010). In spite of these facts, social acceptance of longer-lasting grief following a miscarriage is still low since there is a strong tendency to characterize such grief as exaggerated; thus, the barrier to asking for help is high for affected parents due to fear of further stigmatization (Cook & Phillips, Citation1995). Similar findings were found for stillbirths: According to Heazell et al. (Citation2016), adverse ‘experiences including stigma, social isolation, and disenfranchised grief are widespread among parents whose baby is stillborn and need to be addressed through focused interventions and supportive activities including parents, communities, care providers, and relevant stakeholders’ (p. 104). Following a systematic review by Wool (Citation2011), intense grief reactions are very common after diagnosis of a foetal anomaly, too – regardless of subsequent termination of pregnancy.
Although miscarriage is frequently defined as the spontaneous death of an embryo or foetus within the first 20 weeks of gestation, whereas foetal deaths after 20 weeks of pregnancy are referred to as stillbirths (Jauniaux & Simpson, Citation2021), there is no standard definition of miscarriages or stillbirths (Kolte et al., Citation2015). Due to a lack of standard definition across studies (and across countries), there is overlap in the definitions used across some studies, e.g. earlier stillbirths as defined by some authors may be categorised as miscarriages in other studies and vice versa.
In summary, according to several studies, a sizable proportion of women who have had miscarriages or stillbirths experience corresponding grief reactions (Brier, Citation2008). However, the actual prevalence and intensity of grief are still unclear. In a previous review by Brier (Citation2008) on grief after an early miscarriage, the studies (published before 2008) were summarized, with the aim of examining the nature, frequency, intensity, and duration of grief and to explore potential moderators. For our review, we considered grief in women with different types of previous miscarriages and stillbirths published between 2000 and end of March 2022. Thus, our review clearly extends the scope of the study by Brier (Brier, Citation2008).
Clear estimates of the prevalence of grief in women after miscarriages or stillbirths are important. So far, the proportion of women who cope adequately with grief and the percentage who will develop a prolonged grief disorder or other mental disorders such as depression are unknown. The same is true for the time course of grief following miscarriages or stillbirths. Such data are very important in view of the lack of knowledge regarding the corresponding prevalence of prolonged grief disorder, a diagnosis that was introduced in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5 (American Psychiatric Association, Citation2013)) in 2013. Therefore, we conducted a systematic review of published studies of grief in women who had miscarriages or stillbirths in the recent past.
Our aims were to assess the intensity of grief and its course in women with miscarriages or stillbirths and to estimate the frequency of severe grief reactions in this population. Additionally, we compared subgroups with miscarriages versus stillbirths and with single versus recurrent pregnancy loss. These aims were partly achieved.
2. Materials and methods
2.1. Study design
The present review represents a systematic review of both cross-sectional and prospective longitudinal studies (published between 2000 and the end of March 2022) addressing the effects of miscarriages or stillbirths on grief in affected women. Publications from the period 2000–2022 were selected since conclusions should be based on more recent thematically relevant studies. The study protocol had not been published.
2.2. Search strategy and study eligibility
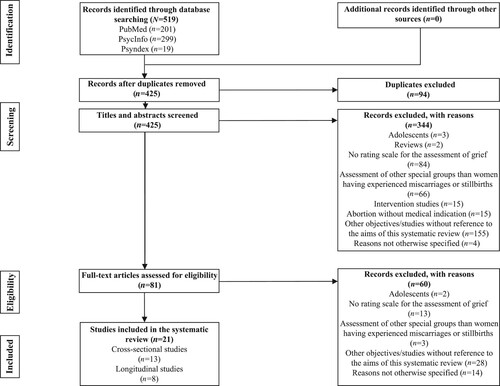
Two reviewers independently identified both cross-sectional and longitudinal studies published between 2000 and 31 March 2022 which contained information about the prevalence or intensity of grief in females who had miscarriages or stillbirths, using the widely used databases MEDLINE, psycINFO and Psyndex for systematic literature searches (for complete details regarding the search strategy see S1 Methods). These databases refer to different scientific publications from medicine and psychology in the English and German languages. Further, they screened the reference lists of identified publications. This procedure is in accordance with the recommendations described in the Preferred Reporting Items for Systematic Reviews and Meta-analyses and Meta-analysis of Observational Studies in Epidemiology reporting (PRISMA) guidelines (Moher et al., Citation2009) which have been followed in this review. The date of the last search was in April 2022.
The inclusion criteria were as follows: publications in English or German; original studies; investigations of adult women after a miscarriage or a stillbirth; use of validated grief rating scales with established cut-off scores. The exclusion criteria referred to: female adolescents after a miscarriage or stillbirth; lack of established criteria for the assessment of grief; reviews or meta-analyses; clinical trials; special groups with reference to women after a miscarriage or stillbirths (e.g. nurses, male partners of affected women); publications in languages other than English and German; termination of pregnancy without any medical indication.
2.3. Study yield
Five hundred nineteen potentially eligible studies were identified. After removal of duplicates and screening of titles and abstracts of the remaining publications, a total of 81 full-text articles were assessed for eligibility. After exclusion of 60 records, 21 studies were included in the final analysis (see the PRISMA flow chart in ).
2.4. Data extraction and quality assessment
Two reviewers independently extracted the following information from each publication by using a standardized form: study design; geographic location; years of survey; miscarriage or stillbirth as defined by the authors of the original studies; mean duration of gestation (in weeks); proportion of women with prior pregnancy loss; proportion of women with (living) children; time after a miscarriage or a stillbirth; unexposed comparison group; sample size; number of female participants; average age; assessment tool used; outcome definition (i.e. cut-off score of a grief screening instrument or rating scale and/or means plus standard deviation of corresponding sum scores); reported prevalence estimates of grief. When studies involved the same population of women after a miscarriage or stillbirth, only the most comprehensive or recent corresponding publication was included in this systematic review.
The same two reviewers independently assessed the risk of bias of the included studies by using a modified version of the Newcastle–Ottawa scale (Wells et al., Citation2021) (for details see S2 Methods).
The identification of studies suitable for inclusion in this systematic review and the assessment of the risk of bias for the included studies had been completed in May 2022. A third reviewer resolved any discrepancies by discussion and adjudication.
Data were collated if possibly by applying appropriate descriptive statistics depending on the scale level of the selected variable (e.g. median for rang-scaled variables and arithmetic means for metric variables).
2.5. Assessment tools for grief
In the 21 included studies, five different tools for the assessment of grief had been applied: the Perinatal Grief Scale-33 (PGS-33) (Potvin et al., Citation1989), the Munich Grief Scale (original German title: ‘Münchner Trauerskala’ (MTS) (Beutel et al., Citation1995)), the Inventory of Complicated Grief Scale (ICG) (Prigerson et al., Citation1995), adjusted versions of the Texas Grief Inventory (TGI) (Nikcevic et al., Citation1999) and the Inventory of Traumatic Grief (Prigerson & Jacobs, Citation2001) which had been adapted for miscarriages (for details see S3 Methods).
2.6. Ethics
As this is a review of secondary data, this article does not contain any studies with human participants performed by any of the authors. An Institutional Review Board approval was therefore not necessary.
3. Results
3.1. Basic characteristics of the studies
Thirteen of 21 studies (62%) were cross-sectional studies (Black et al., Citation2021; Das et al., Citation2021; De Montigny et al., Citation2017; Hanschmidt et al., Citation2018; Keefe-Cooperman, Citation2005; Kersting et al., Citation2005; Krosch & Shakespeare-Finch, Citation2017; Kulathilaka et al., Citation2016; Lafarge et al., Citation2017; Nazaré et al., Citation2012; Rich Citation2000; Serrano & Lima, Citation2006; Séjourné et al., Citation2016) and 8 (38%) were prospective longitudinal studies (Burgoine et al., Citation2005; Conway & Russell, Citation2000; Gozuyesil et al., Citation2022; Güçlü et al., Citation2021; Johnson & Johnston, Citation2021; Köneş & Yildiz, Citation2021; Scheidt et al., Citation2012; Volgsten et al., Citation2018).
In seven of the 13 cross-sectional studies (54%) (Hanschmidt et al., Citation2018; Krosch & Shakespeare-Finch, Citation2017; Lafarge et al., Citation2017; Nazaré et al., Citation2012; Rich Citation2000; Serrano & Lima, Citation2006; Séjourné et al., Citation2016), only one sample had been investigated consisting of women affected by miscarriages or stillbirths. Among the eight prospective longitudinal studies, five (63%) (Conway & Russell, Citation2000; Gozuyesil et al., Citation2022; Güçlü et al., Citation2021; Köneş & Yildiz, Citation2021; Scheidt et al., Citation2012) consisted of only one group of affected females. In nine studies, at least two groups (subgroups or control groups) were considered. From these studies, four had a control group design (two of the cross-sectional studies (15%) (Kersting et al., Citation2005; Kulathilaka et al., Citation2016) and two of the prospective longitudinal studies (25%) (Johnson & Johnston, Citation2021; Volgsten et al., Citation2018)).
The basic characteristics of the 21 included studies are summarized in .
Table 1. Basic characteristics and risk of bias for the included studies.
3.2. Frequencies of extracted variables
Regarding the pre-specified variables of this systematic review, only two (sample size and the kind of pregnancy loss (miscarriage, stillbirth, TOPFA = Termination of Pregnancy for Foetal Anomaly)) could be extracted from all 21 included studies. The average age of the sample was given in all included studies except for one prospective longitudinal study by Conway and Russell (Conway & Russell, Citation2000). The following variables were seldom presented or did not occur at all in the included studies: the proportion of women with recurrent pregnancy losses, psychiatric comorbidity, corresponding pre-diagnoses, the prevalence of complicated grief and the frequencies of severe grief scores in corresponding inventories or rating scales. presents frequencies of extracted variables regarding the 21 included studies.
Table 2. Extracted variables and their frequencies
3.3. Risk of bias
Overall, nine of 21 studies (43%) had a high risk of bias according to the sum score of the modified Newcastle–Ottawa scale (≤2). Of these, three out of 13 cross-sectional studies (23%) (Kersting et al., Citation2005; Nazaré et al., Citation2012; Serrano & Lima, Citation2006) and six of eight prospective longitudinal studies (75%) had a high risk of bias (≤2; see ). Correspondingly, the remaining 10 cross-sectional studies and two of eight longitudinal studies were characterized by a low risk of bias (>2).
3.4. Extracted variables
3.4.1. Demographic variables and pregnancy characteristics
The sample size (without control groups) of the cross-sectional studies varied from 30 (Serrano & Lima, Citation2006) to 328 (Krosch & Shakespeare-Finch, Citation2017) with a median of 143, and of the prospective longitudinal studies from 33 (Scheidt et al., Citation2012) to 215 (Köneş & Yildiz, Citation2021) with a median of 56.5. For the cross-sectional studies, the mean age of the bereaved women at the time of pregnancy loss ranged between 29.0 (Séjourné et al., Citation2016) and 35.6 years (Lafarge et al., Citation2017) with a median of 29.5 years, for the prospective longitudinal studies between 28.1 (Johnson & Johnston, Citation2021) and 35.2 (Scheidt et al., Citation2012) years. In one of the four prospective longitudinal studies (Conway & Russell, Citation2000), the average age was not given, but the majority of the participants was 31 years old at the time of pregnancy loss. In one cross-sectional study (Das et al., Citation2021), only the median year (25 years) was presented. The complete information is presented in Table S1.
Additionally, samples were very heterogeneous regarding the included types of pregnancy loss (miscarriages, TOPFA, stillbirths) and mean duration of pregnancy (see Table S2).
3.4.2. Scales, inventories and measurement times
An overview of the entire set of instruments used in the included studies can be found in Table S3.
Details of measurement times are shown in Table S4.
3.4.3. Mean grief scores and frequencies for severe grief scores
According to 17 of 21 studies included in this review (81%) grief scores were clearly elevated in women after a miscarriage or stillbirth. The comparably low grief scores in two other studies – both being cross-sectional studies (De Montigny et al., Citation2017; Hanschmidt et al., Citation2018) – were associated with a long interval since pregnancy loss (several years).
Regarding the 13 cross-sectional studies, only four studies (31%) provided specific data for the frequency of grief scores above the corresponding cut-off score ((Hanschmidt et al., Citation2018) for TOPFA; (Kulathilaka et al., Citation2016) for miscarriages; (Nazaré et al., Citation2012) for TOPFA; (Das et al., Citation2021) for stillbirths). The frequency range was wide (17.60% for a period of 3.6 years on average since pregnancy loss (Hanschmidt et al., Citation2018) and 80% for six to nine months after stillbirths (Das et al., Citation2021)). The frequency of high grief scores in the study by Nazaré et al. (Citation2012) focussing on TOPFA for a period of 2.4 months on average since pregnancy loss was between these extremes (32.6%).
One study (Das et al., Citation2021) provided data from subgroup analyses: According to these authors, the median PGS-33 sum score for women with stillbirths (107) indicated severe grief and was significantly higher than for mothers with child or neonatal deaths (86). The latter was also true for PGS-33 scores reflecting despair.
Seven of 13 cross-sectional studies (54%) suggest noticeably high grief scores in women after pregnancy losses if the corresponding cut-off scores are applied to estimate the intensity of grief (Das et al., Citation2021; Keefe-Cooperman, Citation2005; Kersting et al., Citation2005; Krosch & Shakespeare-Finch, Citation2017; Lafarge et al., Citation2017; Rich Citation2000; Séjourné et al., Citation2016) (for details see ).
Table 3. Mean grief scores and frequencies for severe grief scores.
Only two cross-sectional studies (Kersting et al., Citation2005; Kulathilaka et al., Citation2016) used control groups; however, it is not possible to compare the grief scores in the group of women after a pregnancy loss and the corresponding scores in the control group because they were not available for the latter group.
For the longitudinal studies, the following picture emerges:
The prospective longitudinal study by Burgoine et al. (Citation2005) used the PGS-33 (Potvin et al., Citation1989) at two measurement times after pregnancy loss (4 months, 12 months) to record the grief scores of two groups distinguished by the type of pregnancy loss for medical reasons (D&E (Dilation and Evacuation for second-trimester pregnancy termination) versus IOL (Induction of Labour for second-trimester pregnancy termination)). For both groups, the mean grief scores at the second measurement time had decreased slightly. The frequency of grief scores above the cut-off score decreased slightly for one group (IOL) but increased for the other (D&E).
In the study by Conway and Russell (Citation2000), the grief scores were assessed using the PGS-33 at two measurement times after pregnancy loss (as soon as possible up to a maximum of three weeks or two to four months). At first, the mean grief value was 88.7, just below the corresponding cut-off score. At the later time, it was significantly higher at 125.7 and thus considerably above the cut-off score.
The study by Volgsten et al. (Citation2018) used the PGS-33 at two measurement times after pregnancy loss (one week, four months). The medians decreased for all three subscales from the first to the second measurement time. This difference was only significant for the Active Grief and Difficulty Coping subscales.
Scheidt et al. (Citation2012) used the MTS (Beutel et al., Citation1995) at three measurement times after pregnancy loss (one month, six months, nine months). The mean grief score was initially 3.3, then 3.1 and finally 3.0. It was not reported whether the measurement time differences were significant.
Gozuyesil et al. (Citation2022) applied the PGS-33 at four measurement times after a miscarriage or stillbirth (≤48 h, months 3, 6 and 12). Regarding women with a miscarriage, their median grief score was initially above the threshold for severe grief (94.5), then continuously decreasing and finally reaching 48. Similar findings were present for women with a stillbirth (median grief scores: initially 92, then continuously declining and finally reaching 45). The time effect was significant. Further analyses revealed that women aged 20–29 years had significantly higher median PGS-33 sum scores three months after pregnancy termination (77) than older women (30–39 years: 70; 40–49 years: 57). Moreover, childless women had significantly higher PGS sum scores (median: 80) than women with living children (median: 71.5) three months after their pregnancy loss. In contrast, differences between women with different numbers of pregnancy loss (one, two, three or more) regarding PGS-33 sum scores at the four measurement times failed to be statistically significant.
Güclü et al. (Citation2021) used the PGS-33 at three measurement times for women with TOPFA (week 6 and months 6 and 12 after pregnancy termination). The initial mean grief score (after six weeks) was below the threshold for severe grief (75.4), but significantly higher than in month 6 (67.5) and month 12 (63.8).
Johnson & Johnston (Citation2021) investigated two groups of women with the first pregnancy outcome being a miscarriage: women with a second miscarriage and women with a subsequent live birth. For this purpose, they selected the PGS-33 and four measurement times (week 6 following the first pregnancy outcome; week 6, month 6 and month 12 following the second pregnancy outcome). Women from the miscarriage/miscarriage group were found to have mean PGS-33 sum scores below the threshold for severe grief at the first two measurement times (86.66 and 84.59, respectively) and corresponding scores above this threshold at months 6 and 12 following the second miscarriage (99.23 and 93.45, respectively). In contrast, a continuous decrease of mean PGS-33 sum scores (week 6 following the first pregnancy outcome: 86.48; month 12 following the subsequent live birth: 61.19) was characteristic for the miscarriage/livebirth group.
Könes & Yildiz (Citation2021) used the PGS-33 at four measurement times after perinatal loss (first 48 h, week 1, months 1 and 3 after the loss). Whereas PGS-33 scores for active grief were significantly lower in the third month after perinatal loss as compared with the prior measurement times, the opposite was the case for PGS-33 scores regarding difficulty of coping and despair. The sample consisted of women with miscarriages, stillbirths, termination of pregnancy for other reasons, TOPFA and postnatal death; specific data for miscarriages (in the sense of the spontaneous death of an embryo or foetus) or stillbirths were not given so that clear conclusions for these types of perinatal loss were not possible. In summary, six of eight longitudinal studies (75%) suggest a decline of grief over the course of several months in women after pregnancy losses (for details see ).
3.4.4. Co-occurrence of grief and symptoms of mental disorders and history of symptoms of mental disorders
Only four studies provided information on the co-occurrence of grief and symptoms of mental disorders (mainly depression) in women with pregnancy losses, in which the range for depressive symptoms above cut-off scores derived from different depression rating scales was high (10.8% (Hanschmidt et al., Citation2018) – 48.8% (Séjourné et al., Citation2016); for details see Table S5).
Only one cross-sectional study (Séjourné et al., Citation2016) provided information on the history of symptoms of mental disorders. Specifically, 18% of the participants had reported depressive symptoms in the past.
Data concerning psychiatric comorbidity and a history of mental disorders were not available for mourning women who had miscarriages or stillbirths. Prolonged grief disorders had not been addressed at all. None of the afore-mentioned studies reported diagnoses of mental disorders in the past as risk factors for enduring grief.
5. Discussion
5.1. Summary of evidence
In summary, most studies document intense grief and frequent severe grief reactions in women who have had miscarriages or stillbirths. The majority of prospective longitudinal studies suggest a decrease of grief over time in this population. Clear conclusions regarding corresponding differences between women with miscarriages and stillbirths or single and recurrent pregnancy losses cannot be drawn. According to one study (Gozuyesil et al., Citation2022), these differences failed to be significant; however, due to the limited sample size (N = 70) these findings have to be interpreted with caution.
Seventeen of 21 studies included in this review (81%) indicate that grief-related stress is markedly elevated in women after a miscarriage or stillbirth. Regarding the comparably low grief scores in two other studies (De Montigny et al., Citation2017; Nikcevic et al., Citation1999), these can be explained by the long interval of several years since pregnancy loss in both studies. Moreover, the study findings reflect the importance of the measurement time for the interpretation of grief in women suffering from the consequences of miscarriages or stillbirths. In addition, the studies suggest an increase of grief during the first weeks after pregnancy loss as well as a slight decrease of grief from this high level in the months to years after this critical life event. The opposite seems to be the case in women having a second miscarriage (Johnson & Johnston, Citation2021); however, this finding has to be replicated. So far, the study results are too preliminary to allow clear conclusions about different effects of miscarriages and stillbirths on grief intensity. It has to be further investigated whether recurrent pregnancy loss increases grief intensity. TOPFA does not seem to go along with significantly more intense grief than miscarriages; however, this finding is based on only one study (Keefe-Cooperman, Citation2005).
5.2. Discussion of the included studies
The main advantage of the included studies is that they address a broad spectrum of research questions and corresponding additional data (e.g. risk and protective factors regarding grief after miscarriages or stillbirths).
A major methodological limitation of the included studies lies in the extreme differences between studies regarding the interval since pregnancy loss (range: less than three weeks to several years). Thus, the results cannot be consistently interpreted inasmuch as a decline of grief scores over a longer period can be expected. If such a decrease does not occur, a prolonged grief disorder can be assumed.
Another fundamental methodological limitation is the fact that most of the selected measurement times are not appropriate for the definition of complicated grief (ICD-11 (World Health Organization, Citation2021): at least six months; DSM-5 (American Psychiatric Association, Citation2013): at least 12 months).
Further, most included studies only report mean grief scores for the total samples. Frequencies for grief scores above a predefined cut-off score reflecting the proportion of women with severe grief scores after a miscarriage or stillbirth are often missing. Only the sample of Burgoine et al. (Citation2005) fulfilled the time criterion for complicated grief. Therefore, these are the only values that can be reported as indicating a prevalence for complicated grief (subgroup with dilation and evacuation for second-trimester pregnancy termination: 27%; subgroup with induction of labour for second-trimester pregnancy termination: 38%).
Data concerning psychiatric comorbidities and pre-diagnoses in women with previous miscarriages or stillbirths as risk factors for long or especially intense grief reactions are not available so far; only a few study findings were reported regarding the co-occurrence of grief and symptoms of mental disorders (especially depression) as well as a history of depressive symptoms. In some studies (e.g. Gozuyesil et al., Citation2022), a history of symptoms of mental disorders was an exclusion criterion.
An additional methodological limitation of the included studies refers to the fact that only four studies (19%) used control groups (Johnson & Johnston, Citation2021; Kersting et al., Citation2005; Kulathilaka et al., Citation2016; Volgsten et al., Citation2018). Grief scores were not available for any of these groups since they showed no significant experiences of a personal loss, with the exception of one study (Johnson & Johnston, Citation2021) showing that women with a subsequent miscarriage were characterized by an increase of grief resulting in a clinically relevant intensity 6 and 12 months after the second pregnancy outcome, whereas a decrease of grief was present at these measurement times in women with a live birth after a miscarriage.
Further methodological limitations of the included studies are (partly) very small sample sizes, frequently large standard deviations of the selected grief scores and (partly) high dropout rates. Overall, the prospective longitudinal studies were characterized by a high risk of bias and low methodological quality (with the exception of the study by Johnson and Johnston (Citation2021)). Moreover, specific grief scores for women after previous miscarriages versus stillbirths were only available in the study by Gozuyesil et al. (Citation2022). Lastly, the validity of the study findings is clearly restricted due to a marked selection bias. It has to be assumed that underrepresentation of women especially affected by previous miscarriages or stillbirths (who avoid grief inventories as stressing reminds them of their pregnancy loss) was accompanied by underrepresentation of women least affected by previous miscarriages or stillbirths (who are not motivated to participate in a study addressing the psychological consequences of a pregnancy loss (Farren et al., Citation2018)). This suggestion is supported by the fact that the majority of studies recruited women with previous miscarriages or stillbirths in hospitals with a rather low response rate (Conway & Russell, Citation2000). In this context, it must be emphasized that those who did not participate may have chosen not to participate for a range of reasons and be more or less affected by their pregnancy loss than participants.
Since the heterogeneity of the included studies (regarding study design, demographic variables, characteristics of the pregnancy, instruments for the assessment of grief and measurement times) was too large it was impossible to conduct a meta-analysis regarding grief in women with previous miscarriages or stillbirths.
5.3. Strengths and methodological limitations of the systematic review
One strength of this review is the fact that frequencies of severe grief scores and mean scores in corresponding inventories have both been considered. Moreover, both cross-sectional studies and prospective longitudinal studies have been included.
Within this review, only descriptive summaries of study findings have been possible in view of the large heterogeneity in measurement times. However, this heterogeneity can also be considered to be advantageous because it facilitates different perspectives of grief after miscarriages or stillbirths.
Regarding the prevalence of complicated grief, no valid data were available in the context of the included studies.
Moreover, several studies had to be excluded since both women with previous miscarriages or stillbirths and women with experiences of perinatal death had been considered with their grief scores not being reported separately.
6. Conclusions
According to this systematic review, more prospective longitudinal studies are needed to delineate the course of grief in women with previous miscarriages or stillbirths. Future studies should specifically address complicated grief in these women.
In addition, future studies should have larger sample sizes and recruit women with previous miscarriages or stillbirths not only in hospitals, but also in other settings (e.g. self-help groups and online forums). These studies should also consider subgroup analyses. In this context, women with recurrent pregnancy loss, women with miscarriages versus stillbirths and women with termination of pregnancy for medical reasons are of special interest.
Lastly, it would be very important to conduct more studies allowing the comparison of women with previous miscarriages or stillbirths on the one hand and women with other loss experiences on the other.
Further research is necessary to estimate the proportions of women with adequate coping of grief and women who will develop prolonged grief disorder, depression or other mental-health problems. This knowledge will allow definition of strategies for prevention and treatment of prolonged grief disorders in this special population.
Supplemental Material
Download MS Word (48.4 KB)Acknowledgements
We would like to thank Ann-Christine Weiderer (A.-C.W.) and Vanessa Lemke (V.L.) for their contributions to the selection of included studies and the assessment of their risk of bias. Parts of this manuscript were prepared within the context of Lisa-Madeleine Edeler’s Master Thesis at the Institute of Psychology, Universität der Bundeswehr München, Neubiberg, Germany.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data presented in this systematic review can be found in the included studies (Black et al., Citation2021; Burgoine et al., Citation2005; Conway & Russell, Citation2000; Das et al., Citation2021; De Montigny et al., Citation2017; Gozuyesil et al., Citation2022; Güçlü et al., Citation2021; Hanschmidt et al., Citation2018; Johnson & Johnston, Citation2021; Keefe-Cooperman, Citation2005; Kersting et al., Citation2005; Köneş & Yildiz, Citation2021; Krosch & Shakespeare-Finch, Citation2017; Kulathilaka et al., Citation2016; Lafarge et al., Citation2017; Nazaré et al., Citation2012; Rich Citation2000; Scheidt et al., Citation2012; Serrano & Lima, Citation2006; Séjourné et al., Citation2016; Volgsten et al., Citation2018).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
- Bellieni, C. V., & Buonocore, G. (2013). Abortion and subsequent mental health: Review of the literature. Psychiatry and Clinical Neurosciences, 67(5), 301–310. https://doi.org/10.1111/pcn.12067
- Beutel, M., Will, H., Völkl, K., von Rad, M., & Weiner, H. (1995). Erfassung von Trauer am Beispiel des Verlustes einer Schwangerschaft: Entwicklung und erste Ergebnisse zur Validität der Münchner Trauerskala [Assessment of grief exemplified pregnancy loss: Development and initial results on the validity of the Munich Grief Scale]. Psychotherapie, Psychosomatik, Medizinische Psychologie, 45(9–10), 295–302.
- Black, J., Belicki, K., McCann, A., & Piro, R. (2021). Dreaming of the deceased after miscarriage: A pilot study. Dreaming, 31(3), 229–243. https://doi.org/10.1037/drm0000177
- Brier, N. (2008). Grief following miscarriage: A comprehensive review of the literature. Journal of Women's Health, 17(3), 451–464. https://doi.org/10.1089/jwh.2007.0505
- Burden, C., Bradley, S., Storey, C., Ellis, A., Heazell, A. E., Downe, S., Cacciatore, J., & Siassakos, D.. (2016). From grief, guilt pain and stigma to hope and pride - a systematic review and meta-analysis of mixed-method research of the psychosocial impact of stillbirth. BMC Pregnancy and Childbirth, 16(9), 1–12. https://doi.org/10.1186/s12884-016-0800-8
- Burgoine, G. A., van Kirk, S. D., Romm, J., Edelman, A. B., Jacobson, S. L., & Jensen, J. T. (2005). Comparison of perinatal grief after dilation and evacuation or labor induction in second trimester terminations for fetal anomalies. American Journal of Obstetrics and Gynecology, 192(6), 1928–1932. https://doi.org/10.1016/j.ajog.2005.02.064
- Conway, K., & Russell, G. (2000). Couples’ grief and experience of support in the aftermath of miscarriage. British Journal of Medical Psychology, 73(4), 531–545. https://doi.org/10.1348/000711200160714
- Cook, B., & Phillips, S. G. (1995). Verlust und Trauer Bedeutung – Umgang – Bewältigung. Ullstein Mosby.
- Das, M. K., Arora, N. K., Gaikwad, H., Chellani, H., Debata, P., Rasaily, R., Meena, K. R., Kaur, G., Malik, P., Joshi, S., & Kumari, M. (2021). Grief reaction and psychosocial impacts of child death and stillbirth on bereaved North Indian parents: A qualitative study. PLoS One, 16(1), e0240270. https://doi.org/10.1371/journal.pone.0240270
- De Montigny, F., Verdon, C., Meunier, S., & Dubeau, D. (2017). Women's persistent depressive and perinatal grief symptoms following a miscarriage: The role of childlessness and satisfaction with healthcare services. Archives of Women's Mental Health, 20(5), 655–662. https://doi.org/10.1007/s00737-017-0742-9
- Farren, J., Mitchell-Jones, N., Verbakel, J. Y., Timmerman, D., Jalmbrant, M., & Bourne, T. (2018). The psychological impact of early pregnancy loss. Human Reproduction Update, 24(6), 731–749. https://doi.org/10.1093/humupd/dmy025
- Gozuyesil, E., Manav, A. I., Yesilot, S. B., & Sucu, M. (2022). Grief and ruminative thought after perinatal loss among Turkish women: One-year cohort study. Sao Paulo Medical Journal, 140(2), 188–198. https://doi.org/10.1590/1516-3180.2021.0148.R1.09062021
- Güçlü, O., Şenormanci, G., Tüten, A., Gök, K., & Şenormanci, Ö. (2021). Perinatal grief and related factors after termination of pregnancy for fetal anomaly: One-year follow-up study. Noro Psikiyatr Ars, 58(3), 221–227. https://doi.org/10.29399/npa.25110
- Hanschmidt, F., Treml, J., Klingner, J., Stepan, H., & Kersting, A. (2018). Stigma in the context of pregnancy termination after diagnosis of fetal anomaly: Associations with grief, trauma, and depression. Archives of Women's Mental Health, 21(4), 391–399. https://doi.org/10.1007/s00737-017-0807-9
- Heazell, A. E. P., Siassakos, D., Blencowe, H., Burden, C., Bhutta, Z. A., Cacciatore, J., Dang, N., Das, J., Flenady, V., Gold, K. J., Mensah, O. K., Millum, J., Nuzum, D., O’Donoghue, K., Redshaw, M., Rizvi, A., Roberts, T., Toyin Saraki, H. E., Storey, C., … Downe, S. (2016). Lancet ending preventable stillbirths series study group, lancet ending preventable stillbirths investigator group. Stillbirths: Economic and psychosocial consequences. The Lancet, 387(10018), 604–616. https://doi.org/10.1016/S0140-6736(15)00836-3
- Jauniaux, E. R. M., & Simpson, J. L. (2021). Chapter 33: Pregnancy loss. In M. B. Landon, H. L. Galan, E. R. M. Jauniaux, D. A. Driscoll, V. Berghella, W. A. Grobman, S. J. Kilpatrick, & A. G. Cahill (Eds.), Gabbe’s obstetrics: Normal and problem pregnancies (8th ed., pp. 615–633). Elsevier.
- Johnson, M. P., & Johnston, R. L. (2021). The psychological implications of a subsequent pregnancy outcome in couples with a history of miscarriage. Journal of Reproductive and Infant Psychology, 39(1), 16–29. https://doi.org/10.1080/02646838.2020.1792427
- Keefe-Cooperman, K. (2005). A comparison of grief as related to miscarriage and termination for fetal abnormality. OMEGA - Journal of Death and Dying, 50(4), 281–300. https://doi.org/10.2190/QFDW-LGEY-CYLM-N4LW
- Kersting, A., Dorsch, M., Kreulich, C., Reutemann, M., Ohrmann, P., Baez, E., & Arolt, V. (2005). Trauma and grief 2-7 years after termination of pregnancy because of fetal anomalies - a pilot study. Journal of Psychosomatic Obstetrics & Gynecology, 26(1), 9–14. https://doi.org/10.1080/01443610400022967
- Kolte, A. M., Bernardi, L. A., Christiansen, O. B., Quenby, S., Farquharson, R. G., & Goddijn, M. (2015). Stephenson MD on behalf of the ESHRE special interest group, early pregnancy. terminology for pregnancy loss prior to viability: A consensus statement from the ESHRE early pregnancy special interest group. Human Reproduction, 30(3), 495–498. https://doi.org/10.1093/humrep/deu299
- Köneş, MÖ, & Yildiz, H. (2021). The level of grief in women with pregnancy loss: A prospective evaluation of the first three months of perinatal loss. Journal of Psychosomatic Obstetrics & Gynecology, 42(4), 346–355. https://doi.org/10.1080/0167482X.2020.1759543
- Krosch, D. J., & Shakespeare-Finch, J. (2017). Grief, traumatic stress, and posttraumatic growth in women who have experienced pregnancy loss. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 425–433. https://doi.org/10.1037/tra0000183
- Kulathilaka, S., Hanwella, R., & de Silva, V. A. (2016). Depressive disorder and grief following spontaneous abortion. BMC Psychiatry, 16(1), 1–6. https://doi.org/10.1186/s12888-016-0812-y
- Lafarge, C., Mitchell, K., & Fox, P. (2017). Posttraumatic growth following pregnancy termination for fetal abnormality: The predictive role of coping strategies and perinatal grief. Anxiety, Stress, & Coping, 30(5), 536–550. https://doi.org/10.1080/10615806.2016.1278433
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, P. R. I. S. M. A. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Open Medicine, 3(3), e123–e130.
- Murphy, F. A., Lipp, A., & Powles, D. L. (2012). Follow-up for improving psychological well being for women after a miscarriage. Cochrane Database of Systematic Reviews, 3(3), 1–39. https://doi.org/10.1002/14651858.CD008679.pub2
- Nazaré, B., Fonseca, A., & Canavarro, M. C. (2012). Grief following termination of pregnancy for fetal abnormality: Does marital intimacy foster short-term couple congruence? Journal of Reproductive and Infant Psychology, 30(2), 168–179. https://doi.org/10.1080/02646838.2012.693154
- Nikcevic, A. V., Snijders, R., Nicolaides, K. H., & Kupek, E. (1999). Some psychometric properties of the texas grief inventory adjusted for miscarriage. British Journal of Medical Psychology, 72(2), 171–178. https://doi.org/10.1348/000711299159925
- Potvin, L., Lasker, J., & Toedter, L. (1989). Measuring grief: A short version of the perinatal grief scale. Journal of Psychopathology and Behavioral Assessment, 11(1), 29–45. https://doi.org/10.1007/BF00962697
- Prigerson, H. G., & Jacobs, S. C. (2001). Traumatic grief as a distinct disorder: A rationale, consensus criteria and a preliminary empirical test. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. A. W. Schut (Eds.), Handbook of bereavement research: Consequences, coping and care (pp. 613–646). American Psychological Association. https://doi.org/10.1037/10436-026
- Prigerson, H. G., Maciejewski, P. K., Reynolds, C. F. R., Bierhals, A. J., Newsom, J. T., Fasiczka, A., Frank, E., Doman, J., Miller, M. (1995). Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research, 59(1-2), 65–79. https://doi.org/10.1016/0165-1781(95)02757-2
- Quenby, S., Gallos, I. D., Dhillon-Smith, R. K., Podesek, M., Stephenson, M. D., Fisher, J., Brosens, J. J., Brewin, J., Ramhorst, R., Lucas, E. S, McCoy, R. C, Anderson, R., Daher, S., Regan, L., Al-Memar, M., Bourne, T., MacIntyre, D. A, Rai, R., Christiansen, O. B, … , Coomarasamy, A.. (2021). Miscarriage matters: The epidemiological, physical, psychological, and economic costs of early pregnancy loss. The Lancet, 397(10285), 1658–1667. https://doi.org/10.1016/S0140-6736(21)00682-6
- Rich, D. (2000). The impact of postpregnancy loss services on grief outcome: Integrating research and practice in the design of perinatal bereavement programs. Illness, Crisis & Loss, 8(3), 244–264. https://doi.org/10.1177/105413730000800303
- Rowlands, I., & Lee, C. (2010). Adjustment after miscarriage: Predicting positive mental health trajectories among young Australian women. Psychology, Health & Medicine, 15(1), 34–49. https://doi.org/10.1080/13548500903440239
- Scheidt, C. E., Hasenburg, A., Kunze, M., Waller, E., Pfeifer, R., Zimmermann, P., Hartmann, A., & Waller, N. (2012). Are individual differences of attachment predicting bereavement outcome after perinatal loss? A prospective cohort study. Journal of Psychosomatic Research, 73(5), 375–382. https://doi.org/10.1016/j.jpsychores.2012.08.017
- Serrano, F., & Lima, M. L. (2006). Recurrent miscarriage: Psychological and relational consequences for couples. Psychol Psychother-T, 79(4), 585–594. https://doi.org/10.1348/147608306(96992)
- Séjourné, N., Fagny, J., Got, F., Lacroix, P., Pauchet, C., & Combalbert, L. (2016). Internet forums following a miscarriage: A place for women in particular pain? Journal of Reproductive and Infant Psychology, 34(1), 28–34. https://doi.org/10.1080/02646838.2015.1079601
- Volgsten, H., Jansson, C., Svanberg, A. S., Darj, E., & Stavreus-Evers, A. (2018). Longitudinal study of emotional experiences, grief and depressive symptoms in women and men after miscarriage. Midwifery, 64, 23–28. https://doi.org/10.1016/j.midw.2018.05.003
- Wells, G. A., Shea, B., O'Connell, D., Peterson, J., Welch, V., Losos, M., & Tugwell, P. (2021) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf
- Wool, C. (2011). Systematic review of the literature: Parental outcomes after diagnosis of fetal anomaly. Advances in Neonatal Care, 11(3), 182–192. https://doi.org/10.1097/ANC.0b013e31821bd92d
- World Health Organization. (2021). International classification of diseases for mortality and morbidity statistics (11th Revision). https://icd.who.int/browse11/l-m/en