ABSTRACT
Background: Network analysis has gained increasing attention as a new framework to study complex associations between symptoms of post-traumatic stress disorder (PTSD). A number of studies have been published to investigate symptom networks on different sets of symptoms in different populations, and the findings have been inconsistent.
Objective: We aimed to extend previous research by testing whether differences in PTSD symptom networks can be found in survivors of type I (single event; sudden and unexpected, high levels of acute threat) vs. type II (repeated and/or protracted; anticipated) trauma (with regard to their index trauma).
Method: Participants were trauma-exposed individuals with elevated levels of PTSD symptomatology, most of whom (94%) were undergoing assessment in preparation for PTSD treatment in several treatment centres in Germany and Switzerland (n = 286 with type I and n = 187 with type II trauma). We estimated Bayesian Gaussian graphical models for each trauma group and explored group differences in the symptom network.
Results: First, for both trauma types, our analyses identified the edges that were repeatedly reported in previous network studies. Second, there was decisive evidence that the two networks were generated from different multivariate normal distributions, i.e. the networks differed on a global level. Third, explorative edge-wise comparisons showed moderate or strong evidence for specific 12 edges. Edges which emerged as especially important in distinguishing the networks were between intrusions and flashbacks, highlighting the stronger positive association in the group of type II trauma survivors compared to type I survivors. Flashbacks showed a similar pattern of results in the associations with detachment and sleep problems (type II > type I).
Conclusion: Our findings suggest that trauma type contributes to the heterogeneity in the symptom network. Future research on PTSD symptom networks should include this variable in the analyses to reduce heterogeneity.
HIGHLIGHTS
The current study aimed to investigate trauma type as a potential moderator of PTSD symptom networks, distinguishing between type I trauma (single event; sudden and unexpected, high level of acute threat) vs. type II trauma (repeated and/or protracted; anticipated) with regard to their index trauma.
Findings suggest that the PTSD symptom network structure differs between type I and type II trauma survivors. Edges which emerged as especially important in distinguishing the networks were between intrusions and flashbacks, highlighting the stronger positive association in the group of type II trauma survivors compared to type I survivors. Flashbacks showed a similar pattern of results in the associations with detachment and sleep problems (type II > type I).
Analysis revealed that trauma type contributes to the heterogeneity in the symptom network and it is important variable to consider in the future research.
Antecedentes: El análisis de redes ha ganado cada vez más atención como un nuevo marco para estudiar asociaciones complejas entre síntomas del Trastorno de Estrés Postraumático (TEPT). Se han publicado una cantidad de estudios para investigar las redes de síntomas en diferentes conjuntos de síntomas en distintas poblaciones, y los hallazgos han sido inconsistentes.
Objetivos: Nuestro objetivo fue ampliar la investigación previa probando si se pueden encontrar diferencias entre las redes de síntomas del TEPT en sobrevivientes de trauma de tipo 1 (evento único; súbito e inesperado, niveles elevados de amenaza aguda) versus los de tipo 2 (eventos repetidos y/o prolongados; anticipados) (con respecto a su trauma índice).
Métodos: Los participantes eran individuos expuestos al trauma con niveles elevados de sintomatología de TEPT, la mayoría de los cuales (94%) se sometían a una evaluación en preparación para el tratamiento del TEPT en varios centros de Alemania y Suiza (n = 286 con tipo 1 y n = 187 con tipo 2 de trauma). Estimamos modelos gráficos Bayesianos Gaussianos para cada tipo de grupo de trauma y exploramos las diferencias entre los grupos en la red de síntomas.
Resultados: En primer lugar, para ambos tipos de trauma, nuestros análisis identificaron los bordes que se reportaron repetidamente en estudios de redes anteriores. En segundo lugar, hubo evidencia decisiva que las dos redes fueron generadas de diferentes distribuciones normales multivariadas, es decir, las redes diferían a nivel global. En tercer lugar, las comparaciones exploratorias de los bordes mostraron una evidencia de moderada a fuerte para 12 bordes específicos. Los bordes que surgieron como especialmente importantes para distinguir las redes fueron las intrusiones y flashbacks, destacando la asociación fuertemente positiva entre los grupos de tipo 2 en comparación con los sobrevivientes de trauma del grupo de tipo 1. Los flashbacks mostraron un patrón similar de resultados en las asociaciones con desapego y problemas de sueño (tipo 2 > tipo 1).
Conclusiones: Nuestros resultados sugieren que el tipo de trauma contribuye a la heterogeneidad en los síntomas de red. La investigación futura sobre las redes de los síntomas de TEPT debería incluir esta variable en los análisis para reducir la heterogeneidad.
背景:网络分析作为研究创伤后应激障碍 (PTSD) 症状之间复杂关联的新框架,受到了越来越多的关注。已经发表了许多考查不同人群中不同症状组的症状网络的研究,结果并不一致。
目的:我们旨在通过检验是否能够发现 I 型(单一事件;突然和意外的、高水平的急性威胁)与 II 型 (重复和/或长期的;预期的) 创伤幸存者 PTSD 症状网络(就其指数创伤)的差异来扩展前人研究。
方法:参与者是PTSD症状水平升高的个体,其中大多数(94%)正在德国和瑞士的几个治疗中心接受评估以准备 PTSD 治疗 (n = 286 为 I 型,n = 187 为II 型创伤)。我们估计了每个创伤组的贝叶斯高斯图模型,并探索了症状网络中的组别差异。
结果:首先,对于这两种创伤类型,我们的分析确定了之前网络研究中反复报告的边。其次,有决定性证据表明这两个网络是由不同的多元正态分布产生的,即网络在全局水平上是不同的。第三,探索性的边比较显示了特定 12 条边的中等或有力证据。在区别网络中特别重要的边出现在闯入和闪回之间,突显出II 型创伤幸存者组相较于 I 型幸存者有更强的正相关。闪回在与分离和睡眠问题(II型> I型)的关联中显示出相似模式的结果。
结论:我们的研究结果表明,创伤类型会导致症状网络异质性。未来对 PTSD 症状网络的研究应该在分析中纳入这个变量以减少异质性。
Posttraumatic stress disorder (PTSD) is a highly prevalent and disabling disorder with onset after trauma experiences. Since its introduction into the classification systems in 1980 (DSM-III: American Psychiatric Association, Citation1980), the exact definition and formulation of the disorder has been subject to considerable debate.
Recently, network analysis has been proposed as a novel approach to conceptualising mental disorders (Borsboom & Cramer, Citation2013). Network analysis is a group of statistical techniques that are used to investigate and visualise the co-occurrence (typically correlation) between the phenomena of interest. The goal is to estimate the conditional dependence structure in the shape of a network diagram, with nodes representing each entity and with edges representing the associations between nodes. In psychopathological research, nodes typically represent individual symptoms of psychological disorders and edges are defined as (partial) correlations between the symptoms. In other words, the network approach informs which symptoms co-occur within a disorder and across disorders, and can therefore help to identify a core set of symptoms and their relationships that best characterises a disorder such as PTSD.
Over the past five years, dozens of studies have been published on PTSD symptom networks in trauma survivors, including e.g patients diagnosed with PTSD (Hoffart et al., Citation2019), adult survivors of childhood abuse (Knefel et al., Citation2016), military (Armour et al., Citation2017), survivors of terror attacks (Birkeland et al., Citation2017), survivors of natural disasters. A recent systematic review (Birkeland et al., Citation2020), as well as a recent meta-analysis (Isvoranu et al., Citation2021) identified edges that emerge robustly regardless of differences in culture, trauma type, and symptom severity (see also Fried et al., Citation2018). These include edges between the symptoms hypervigilant and easily startled; nightmares and intrusive thoughts; internal avoidance and external avoidance; emotional numbing and feeling detached; and feeling detached and loss of interest. In addition, amnesia is often recognised as the most peripheral symptom associated with few other symptoms in a network (Isvoranu et al., Citation2021).
Despite some consistent and robust aspects (e.g. re-experiencing amongst the core PTSD symptoms (Bryant et al., Citation2017; Haag et al., Citation2017)), researchers overall have concluded that there is large between-study heterogeneity in published PTSD symptom networks. Analyses of multiple samples and datasets identified large random effect sizes on the correlational structure of the symptoms (Epskamp et al., Citation2021; Isvoranu et al., Citation2021). This raises the question of whether there are systematic differences in symptom networks between different subgroups of trauma survivors.
The current study focused on trauma type as a potential moderator of characteristics in PTSD symptom networks. It is conceivable that trauma type may be an important moderator, as it has been shown to have a significant impact on symptom severity, associations between symptoms, and prevalence of PTSD (Cloitre et al., Citation2009; Kelley et al., Citation2009) as well as the complexity of the symptom presentation (Cloitre et al., Citation2009, Citation2013). In addition, differences in symptom networks between survivors of different types of traumas were indeed found in two recent studies. In the first study, Benfer et al. (Citation2018) computed PTSD symptom networks in female undergraduate students who had survived three different trauma types (i.e. motor vehicle accident, sexual assault, and sudden accidental or violent death of a loved one). Results showed a significant difference in the global edge strength between sexual assault and motor vehicle accident. In addition, visual inspections of the symptom networks for the different groups suggested that the network for sexual assault was most conceptually similar to PTSD as defined by DSM-5 (i.e. symptoms were most consistently linked to each other in a way that was similar to DSM-5 symptom clusters in this group) (Benfer et al., Citation2018). More recently, Macia et al. (Citation2020) examined symptom networks of veterans with combat vs. non-combat index trauma. Their results showed some variability in the network related to presence and absence of combat experiences. However, no formal statistical tests were conducted on the between-network differences, and the conclusions were merely based on visual inspection of the relative network structure (Macia et al., Citation2020). In addition, the distinction between the different trauma types studied appeared to be somewhat arbitrary and not guided by theoretical ideas regarding differences in trauma type that could be related to differences in symptom presentation. For example, there is considerable evidence showing that sudden and unexpected traumatic events that are characterised by high levels of acute threat (e.g. accidents; single episodes of physical or sexual assault) may lead to different symptom presentations than repeated and/or protracted traumatic events (e.g. sexual and/or physical maltreatment in childhood) (Cloitre et al., Citation2013; Courtois & Ford, Citation2009). Research investigating the sequelae of type I vs. type II trauma has mainly focused on conceptual issues (e.g. whether or not different diagnoses are needed for classic vs. more complex PTSD) (Maercker, Brewin, Bryant, Cloitre, Reed, et al., Citation2013; Resick et al., Citation2012) or the type of symptoms experienced following the different trauma types (Briere et al., Citation2008; Cloitre et al., Citation2009). However, to our knowledge, there has been no investigation about whether trauma type defined in this way is related to the co-occurrence of these symptoms, i.e. the PTSD symptom network structure.
The current study aimed to extend the promising findings on trauma type as a potential moderator for the structure of PTSD symptom networks (Benfer et al., Citation2018; Macia et al., Citation2020) in three ways. First, based on the theoretical and empirical findings, we used specific characteristics of trauma (single event; sudden and unexpected, high levels of acute threat vs. repeated and/or protracted, anticipated traumatic events) to distinguish between type I vs. type II trauma. We decided to use the current categorisation given the empirical findings showing that sudden and unexpected traumatic events that are characterised by high levels of acute threat (e.g. accidents; single episodes of physical or sexual assault) and may lead to different symptom presentations than repeated and/or protracted traumatic events, especially those that are experienced early in life (e.g. sexual and/or physical maltreatment in childhood) (Cloitre et al., Citation2013; Courtois & Ford, Citation2009). Second, we targeted mostly treatment-seeking trauma survivors in order to maximise the clinical relevance of our findings. This is because non-clinical samples, such as a student population, may have a different symptom distribution than a clinical population. Third, rather than relying on visual inspection of symptom networks, we used a particular statistical approach – the Bayesian method (Williams, Citation2021; Williams et al., Citation2020) – to estimate and compare the networks of different trauma types. This method has important practical advantages, such as being computationally more efficient and providing a higher power to detect network differences than the permutation-based test (van Borkulo et al., Citation2017) that has been used in the literature (Benfer et al., Citation2018; Fried et al., Citation2018).
Our analysis had three aims. First, we aimed to test whether edges identified in a relatively robust way in earlier studies would also emerge in the symptom networks in our study, irrespective of trauma type. Second, we hypothesised that the symptom network of type I trauma survivors shows a global difference to the network found in type II trauma survivors, considering all possible edges (i.e. the entire covariance matrices). Third, we explored between-network differences regarding each edge to clarify which edges are characteristic of one of the networks but not the other.
1. Method
1.1. Participants
Three datasets (total N = 586) were combined for the current study. The first dataset was taken from a published study (Krüger-Gottschalk et al., Citation2017) comprising 352 traumatised individuals attending different treatment centers specialised in trauma-related disorders across Germany (a subset of 32 participants were traumatised individuals recruited via newspaper ads; for details on recruitment see Krüger-Gottschalk et al., Citation2017). The second data set included 174 patients attending the Outpatient Treatment centre at LMU Munich. The third data set consisted of 60 patients attending at the Outpatient Centre for Specific Psychotherapy at the Psychiatric University Hospital in Zurich, Switzerland. The same inclusion criteria were used across all datasets: (a) participants had been exposed to at least one traumatic event in their lives, and (b) at least one month had elapsed since the trauma. Only those who met both criteria were invited to the assessments. Further, 113 participants had to be excluded from the final sample as they did not provide sufficient data for analyses (for details see Procedure below). Therefore, the final sample comprised 73 participants, most of whom (94%) were attending a PTSD treatment center undergoing assessment prior taking up PTSD-specific treatment. Participants had not received any interventions at the time of assessment (for detailed sample characteristics, see ).
Table 1. Sample characteristics.
1.2. Measures
The German version of the Life Events Checklist for DSM-5 (LEC-5: Weathers, Blake, et al., Citation2013) was used to measure trauma exposure. This self-report questionnaire assesses exposure to 16 categories of traumatic events and one additional item for any other exceptional stressful event. Participants were first instructed to indicate all applicable events among the categories. They also provided follow-up information concerning the most traumatic event. We grouped participants into type I vs. type II trauma survivors on the basis of the most traumatic event reported (see Procedure section).
The German version of the PTSD Checklist for DSM-5 (PCL-5: Krüger-Gottschalk et al., Citation2017; Weathers, Litz, et al., Citation2013) was used to assess PTSD symptoms. The PCL-5 consists of 20 items corresponding to the DSM-5 criteria for PTSD. Each item was rated for the intensity using a 5-point scale (0 = not at all, 4 = extremely). The PCL-5 has an established cut-off of ≥ 33, indicating clinically significant levels of symptoms (Krüger-Gottschalk et al., Citation2017; Weathers, Blake, et al., Citation2013). The PCL-5 has the following four subscales: Re-experiencing, Avoidance, Changes in mood and cognition, and Hyperarousal (Table S1). Internal consistency for the total PCL-5 score was excellent in the final sample (Cronbach's α = .93). When completing the PCL-5, participants were instructed to refer to the most traumatic event that they reported on the LEC (Weathers, Blake, et al., Citation2013).
1.3. Procedure
On the basis of the most traumatic event reported on the LEC, two independent raters classified participants as type I vs. type II trauma survivors with regard to their index trauma. Raters were provided with definitions of the type I and type II trauma and then rated the events based on the narrative description of the worst event reported by participants, including the following questions related to this event (e.g. how long ago it happened, how many times altogether it happened). Both raters were trained clinicians, and the inter-rater reliability was excellent (Cohen's κ = 0.86). Any disagreements were discussed and resolved by the research team. Whenever available, clinicians who worked with the participants were also asked to rate the trauma type, which was used to verify the ratings provided by independent raters; this was possible for a subsample of n = 234. The rating procedure was organised as follows. First, we found that some participants (n = 57) did not provide a description of the most traumatic events on the LEC, so the data for those participants were not used in the analyses. Second, we checked whether the most traumatic events met the DSM-5 A criterion. The events that did not meet this criterion, or the events that could not be classified as type I or type II trauma, were also excluded from the analyses (n = 19). Third, we excluded the data from participants who reported no symptoms of PTSD (as indicated by a PCL-5 total score of zero) or those who had not filled in the PCL-5 (n = 5). Finally, some participants (n = 32) had to be excluded from the analyses as they did not provide sufficient data on PCL items for the analyses. This was default setting on the BGGM package. The final sample size was 473 participants, comprising 286 type I trauma survivors and 187 type II trauma survivors.
1.4. Statistical analyses
First, we estimated Gaussian graphical models, namely symptom networks, on the reported PTSD symptoms for type I and type II trauma sufferers. Each node in the networks represented one of the 20 PTSD symptoms measured by the PCL-5, and each edge represented a partial correlation between two given symptoms. The networks were estimated using the Bayesian method implemented in the R package, BGGM (Williams & Mulder, Citation2020). This package provides a Gibbs sampler to generate posteriors with the Matrix-F prior distribution as a flexible alternative to (inverse) Wishart priors. For each network, we drew 5000 posterior samples, with which we obtained the posterior means of each partial correlation and their 95% credible intervals (CIs). To determine the conditional (in)dependence (i.e. ‘existence’ of an edge in a network), we used the Bayes factor (BF), indexing the strength of the evidence for the alternative hypothesis (i.e. the partial correlation is not equal to zero) relative to the null hypothesis (i.e. the partial correlation is equal to zero). We set the threshold as BF > 3, which is typically interpreted as good evidence in favour of the alternativeFootnote1 (Kass & Raftery, Citation1995).
Second, we tested the differences in the network between type I and type II trauma survivors. To test the network-wide global differences, we performed a predictive check on the basis of the Jensen-Shannon divergence (JSD), which is known as a symmetric version of Kullback-Leibler divergence (Menéndez et al., Citation1997). In general, this test statistic represents the distance between two distributions. From posterior samples, a predictive distribution of JSD is produced, which serves as a reference to determine the predictive p-value for the observed JSD. The hypothesised group equality (to be rejected) was tested with alpha = 0.05. Put differently, this test identifies whether the covariance matrices of type I and type II trauma survivors are generated from different multivariate normal distributions. As another test statistic, we also computed the sum of squared error for the partial correlation matrices (Williams et al., Citation2020). As one of the most important advantages, this predictive method allows for testing a global (not edge-specific) difference between the networks (Williams, Citation2021). Additionally, a simulation study showed that this method is less sensitive to unequal sample sizes between the compared groups than the permutation-based test (Williams et al., Citation2020).
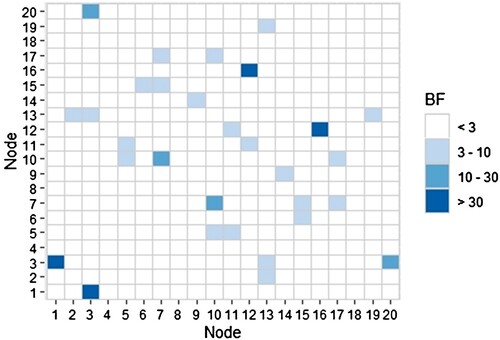
Third, after establishing the global difference, we performed edge-specific comparisons using Bayesian hypothesis testing; here, a BF was defined as the strength of the evidence favouring the alternative hypothesis (H1: the edge is not equal between Type-1 and Type-2 trauma sufferers) over the null hypothesis (H0: the edge is equal between the two groups). The BF can be interpreted as follows: BF > 30 indicates very strong evidence, BF = 10–30 indicates strong evidence, and BF = 3–10 indicates moderate evidence for H1. For each of the network estimations, we identified no convergence issues through visual inspections of the trace plots and auto-correlations, and effective sample sizes of the posterior samples. In reporting the results of the network analyses, we adhered to the reporting standards for psychological network analysesFootnote2 (Burger et al., Citation2020).
2. Results
2.1. Participants’ characteristics
We first tested potential differences in demographics between type I and type II trauma survivors (). Results showed no significant difference in age, t(405.44) = 0.11, d = −0.01, p > .90, but did show a significant difference in the gender distribution, χ2 (1) = 4.33, p < .04, which is consistent with the WHO report that women are more likely to report type II trauma than men (World Health Organisation, Citation2021).
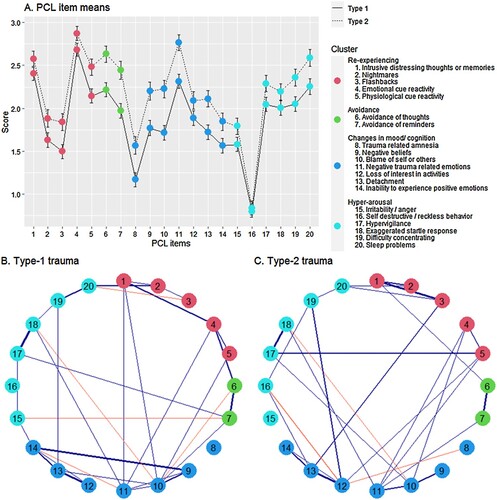
Second, we tested whether groups differed regarding their PCL scores. Type II trauma survivors scored higher on the PCL total score as well as the four subscales than type I trauma survivors (). Within the whole sample, 313 individuals (type I: 173; type II: 140) reported clinically significant levels of PTSD symptoms as indicated by PCL scores above the cut-off of 33 (Krüger-Gottschalk et al., Citation2017). Individual item means (and correlations) can be found in Figure 1A (and in supplementary materials Tables S4 and S5).
Table 2. Means (SDs) of the PCL-5 Scores for type I and type II trauma survivors.
2.2. Network estimation for type I and type II trauma
We estimated separate Bayesian Gaussian graphical models (partial-correlation networks) for type I and type II trauma survivors ((B,C)).
2.3. Testing the global network differences and edge-wise comparisons
In a next step, we tested for differences between the networks for the two groups. As a test of the global network difference, the predictive p-value for the observed JSD rejected the null hypothesis, (JSD = 1.40, p < .01), which means that there were significant differences in the network structure between type I and type II trauma survivors. The sum of the squared error confirmed this global group difference, (SSE = 2.58, p < .01).
In order to better understand differences between the networks, we explored group differences in edge strength and identified 15 edges with BF > 3, favouring the alternative hypothesis that the edge strength differed between the two networks (). illustrates the selected 12 edges for interpretation, which (a) were recognised in either the network of type I or type II survivors (or both) and (b) showed BF > 3 for the network comparisons; the other three edges appeared neither in the network of type I nor type II survivors. The most prominent difference was found for the edge between the symptoms of intrusions and flashbacks, highlighting the stronger positive association in the group of type II trauma survivors compared to type I survivors. Flashbacks showed a similar pattern of results in the associations with detachment and sleep problems (type II > type I). These group differences were identified even after controlling for the gender differences and education levels (see the supplementary material, Table S6). Additionally, we repeated the analysis without the 32 participants who had not been recruited via treatment centers; results were overall unchanged.
Table 3. Bayes Factors (BFs) and Posterior Means and Standard Deviations for Edge-wise Group Differences (BF>3).
3. Discussion
Earlier studies investigating PTSD symptom networks have shown large between-study heterogeneity (Isvoranu et al., Citation2021) suggesting that there may be subgroups of trauma survivors showing systematic differences in symptom network structures. The current study aimed to test whether trauma type is a significant moderator of characteristics in PTSD symptom networks. Both networks showed a strong edge between the items hypervigilance and being easily startled, which has repeatedly been found in previous network studies (Birkeland et al., Citation2020; Fried et al., Citation2018; Isvoranu et al., Citation2021). Furthermore, other edges identified in the earlier literature emerged in both networks: nightmares – intrusive thoughts, internal avoidance – external avoidance, emotional numbing – feeling detached, feeling detached – loss of interest. These edges appear to be robust across different trauma types and other sample characteristics (Birkeland et al., Citation2020; Fried et al., Citation2018; Isvoranu et al., Citation2021) and thus, may be interpreted as common features of PTSD-symptom networks. These robust edges can be interpreted as common features of PTSD symptom networks across different sample populations, including treatment-seeking trauma survivors.
We then tested our hypothesis that there should be significant differences in PTSD symptom networks in survivors of type I vs. type II trauma. In line with our hypothesis, the network comparison test provided strong evidence for a global difference between the networks of the two groups. This global difference endorses the heterogeneity in symptom networks due to the difference in trauma type (Benfer et al., Citation2018; Macia et al., Citation2020). There is consistent earlier evidence showing that type II trauma is related to higher symptom severity (Ehring & Quack, Citation2010), and complexity (Briere et al., Citation2008; Cloitre et al., Citation2009). The current findings additionally suggest that type I vs. type II trauma also leads to differences in the structure or co-occurrence of PTSD symptoms. If replicated, this could suggest that future studies investigating PTSD symptom networks may benefit from paying closer attention to trauma type as a moderator, whereby the distinction between type I and type II trauma appears to be a promising starting point. In addition, there may also be implications for the literature focusing on differences in sequelae of type I vs. type II trauma, suggesting that in addition to focusing on the question of whether the different types of trauma lead to different symptoms and/or diagnoses (see Maercker, Brewin, Bryant, Cloitre, van Ommeren, et al., Citation2013; Resick et al., Citation2012), the structure and inter-relationship of symptoms, as well as their potentially causal links, may be important to consider.
As the literature on symptom network models is still at an early stage, it is yet unclear whether the identification of cross-sectional network models also has clinical implications. However, preliminary evidence suggests that pre-treatment cross-sectional symptom networks predict within-subject relationships between symptoms in the sense of change trajectories (Klipstein et al., Citation2021). Therefore, it appears promising to investigate whether information on differences in symptom network structures between different subgroups of trauma survivors can inform the differential selection of treatment targets.
As symptom networks were found to differ between groups at a global level, we also conducted edge-wise comparisons to explore unique edges for the different trauma groups. The network of type I trauma survivors (but not those with type II trauma) comprised positive associations between the core symptoms of PTSD (e.g. avoidance, cue reactivity) and cognitive and emotional problems (e.g. blame, negative beliefs, lack of positive emotions). On the other hand, the network of type II trauma survivors also showed unique (or stronger) edges compared to those who had experienced type I trauma. For example, flashbacks were closely associated with intrusions, detachment, and sleep problems. Due to the highly exploratory nature of these analyses, these findings should be interpreted with great caution. If replicated in future research, the findings may be indicative of a key role of flashbacks, i.e. re-experiencing with a strong dissociative component in the symptomatology related to type II trauma, with dissociative flashbacks being closely related to a broad network of symptoms. On the other hand, the findings might suggest a particularly strong relationship between core symptoms of PTSD and cognitive and emotional problems in type I trauma survivors. In addition, the findings are in line with differences in coping behaviour between trauma groups, with a link between avoidance and anger in the type I trauma group, and reckless behaviour and loss of interest in activities in the type II group.
Several limitations are noteworthy. First, the total sample was derived by combining different subsamples that had been recruited at different locations and drawn from slightly different populations. Although heterogeneity to this extent is common in the literature, the generalizability of the findings may be in question. Second, information about participants’ history of the psychological and medication treatment could not be collected and reported. Third, the sample size of the current study was around the average of other published network analysis studies on PTSD (Isvoranu et al., Citation2021). However, replication using larger sample sizes nevertheless appears necessary. Fourth, we were specifically interested in the difference between type I and II trauma; therefore, we did not examine differences between more specific types of events (e.g. physical assaults vs. sexual abuse). Although our results support the view that the rather broad distinction between type I and type II trauma is important to explain some of the heterogeneity found in earlier research, it cannot be ruled out that more specific trauma types may account for additional heterogeneity. Future studies are needed to address this issue. Additionally, future research should address other trauma characteristics that could explain differences in the symptom constellation (e.g. accidental vs. interpersonal trauma). Fifth, there are many other pre-, peri- and post-traumatic moderators that should be considered that may also explain some of the differences. Sixth, we used just event index for the trauma type distinction. Future research should consider using additionally Childhood Trauma Questionnaire (CTQ) to obtain additional information about childhood trauma. Furthermore, future research should more closely consider all traumatic experiences experienced by participants rather than focusing on the index trauma only. Lastly, we used only questionnaire self-report data. Observer-rated measures or more objective (behavioural/physiological) variables can be included in the future studies.
Despite the limitations, this study provides important evidence for the hypothesis that trauma type is a relevant moderator that may help account for part of the inconsistent findings in PTSD network literature to date. Given that the shape of network depends on what items (symptoms) are included in the analysis, future research should go beyond the item set defined by DSM-5 and additionally include symptoms indicative of more complex PTSD presentations (e.g. disturbance in emotion regulation, negative self-identity, relationship difficulties) and other trauma-related symptoms as suggested in the study of Haan and colleagues (Haan et al., Citation2020). This will provide a more comprehensive picture of the PTSD symptomatology and variants. Furthermore, widening the focus to symptoms of other psychopathology may help establish the transdiagnostic role of trauma.
Ethical approval
The study was approved by the Ethics Committees of the Institute of Psychology, University of Münster, Germany, as wells as the Department of Psychology, LMU Munich, Germany. All participants provided informed written consent.
Supplemental Material
Download MS Word (151.1 KB)Acknowledgements
The authors would love to thank Hannah Schumm and Nathalie Kammer for assisting with the ratings of trauma type.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data can be shared with other researchers on request. Unfortunately, we did not obtain informed consent from the participants in this study to make their data publicly available. As our local Ethics Committee deems this necessary when making data publicly available, we are unable to post the data in an open repository.
Additional information
Funding
Notes
1 We found that the use of another threshold, i.e., a posterior probability > 0.95 for the alternative hypothesis, led to a network structure similar to the used threshold of BF > 3 (Biel and Friedrich (Citation2018); see also the supplementary materials and Tables S2 and S3). Naturally, a more conservative threshold prunes more edges; e.g., for the network of the Type-1 trauma survivors, the threshold of a posterior probability > 0.99 identified 26 ‘significant’ edges, whereas the threshold of > 0.95 led to 32 edges. A more conservative threshold is, in general, better to control the false discovery rate, but the threshold of 0.99 could be too conservative given that this threshold is known to identify many fewer edges than the standard estimation approach using the regularization with the graphical lasso (Williams, Citation2021).
2 Most of earlier studies on symptom networks in PTSD have reported centrality indices. We therefore also provide centrality indices for the networks computed in this study in the supplementary materials (Figures S2 and S3), as they may be informative to see the relative importance of a node within a network. However, we decided not to interpret the centrality indices here because we see little or no additive value of the indices in the context of network comparison (Bringmann et al., Citation2019). Instead, we explored network differences for each edge. Given that a centrality is e.g., a sum of edge strengths per node, edge-wise comparisons would already suffice to clarify how and where two networks differ.
References
- American Psychiatric Association. (1980). Diagnostic and Statistical Manual of Mental Disorders (3rd ed). American Psychiatric Association.
- Armour, C., Fried, E. I., Deserno, M. K., Tsai, J., & Pietrzak, R. H. (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. Military veterans. Journal of Anxiety Disorders, 45, 49–59. https://doi.org/10.1016/j.janxdis.2016.11.008
- Benfer, N., Bardeen, J. R., Cero, I., Kramer, L. B., Whiteman, S. E., Rogers, T. A., Silverstein, M. W., & Weathers, F. W. [Frank W.]. (2018). Network models of posttraumatic stress symptoms across trauma types. Journal of Anxiety Disorders, 58, 70–77. https://doi.org/10.1016/j.janxdis.2018.07.004
- Biel, A. L., & Friedrich, E. V. C. (2018). Why you should report Bayes factors in your transcranial brain stimulation studies. Frontiers in Psychology, 9, 1125. https://doi.org/10.3389/fpsyg.2018.01125
- Birkeland, M. S., Blix, I., Solberg, Ø., & Heir, T. (2017). Gender differences in posttraumatic stress symptoms after a terrorist attack: A network approach. Frontiers in Psychology, 8, 2091. https://doi.org/10.3389/fpsyg.2017.02091
- Birkeland, M. S., Greene, T., & Spiller, T. R. (2020). The network approach to posttraumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 11(1), 1700614. https://doi.org/10.1080/20008198.2019.1700614
- Borsboom, D., & Cramer, A. O. J. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9(1), 91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
- Briere, J., Kaltman, S., & Green, B. L. (2008). Accumulated childhood trauma and symptom complexity. Journal of Traumatic Stress, 21(2), 223–226. https://doi.org/10.1002/jts.20317
- Bringmann, L. F., Elmer, T., Epskamp, S., Krause, R. W., Schoch, D., Wichers, M., Wigman, J. T. W., & Snippe, E. (2019). What do centrality measures measure in psychological networks? Journal of Abnormal Psychology, 128(8), 892–903. https://doi.org/10.1037/abn0000446
- Bryant, R. A., Creamer, M., O’Donnell, M., Forbes, D., McFarlane, A. C., Silove, D., & Hadzi-Pavlovic, D. (2017). Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: A network analysis. JAMA Psychiatry, 74(2), 135–142. https://doi.org/10.1001/jamapsychiatry.2016.3470
- Burger, J., Isvoranu, A-M, Lunansky, G., Haslbeck, J. M. B., Epskamp, S., Hoekstra, R. H. A., Fried, E. I., Borsboom, D., & Blanken, T. (2020). Reporting standards for psychological network analyses in cross-sectional data. https://doi.org/10.31234/osf.io/4y9nz.
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(1), 20706. https://doi.org/10.3402/ejpt.v4i0.20706
- Cloitre, M., Stolbach, B. C., Herman, J. L., van der Kolk, B., Pynoos, R., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. https://doi.org/10.1002/jts.20444
- Courtois, C. A., & Ford, J. D. (2009). Treating Complex Traumatic Stress Disorders: An Evidence-Based Guide. Guilford Press.
- Ehring, T., & Quack, D. (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41(4), 587–598. https://doi.org/10.1016/j.beth.2010.04.004
- Epskamp, S., Isvoranu, A.-M., & Cheung, M. W.-L. (2021). Meta-analytic Gaussian network aggregation. Psychometrika. Advance online publication, 87(1), 12–46. https://doi.org/10.1007/s11336-021-09764-3
- Fried, E. I., Eidhof, M. B., Palic, S., Costantini, G., Huisman-van Dijk, H. M., Bockting, C. L. H., Engelhard, I., Armour, C., Nielsen, A. B. S., & Karstoft, K-I. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351. https://doi.org/10.1177/2167702617745092
- Haag, C., Robinaugh, D. J., Ehlers, A., & Kleim, B. (2017). Understanding the emergence of chronic posttraumatic stress disorder through acute stress symptom networks. JAMA Psychiatry, 74(6), 649–650. https://doi.org/10.1001/jamapsychiatry.2017.0788
- Haan, A. d., Landolt, M. A., Fried, E. I., Kleinke, K., Alisic, E., Bryant, R., Salmon, K., Chen, S.-H., Liu, S-T, Dalgleish, T., McKinnon, A., Alberici, A., Claxton, J., Diehle, J., Lindauer, R., Roos, C. d., Halligan, S. L., Hiller, R., Kristensen, C. H., … Meiser-Stedman, R. (2020). Dysfunctional posttraumatic cognitions, posttraumatic stress and depression in children and adolescents exposed to trauma: A network analysis. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 61(1), 77–87. https://doi.org/10.1111/jcpp.13101
- Hoffart, A., Langkaas, T. F., Øktedalen, T., & Johnson, S. U. (2019). The temporal dynamics of symptoms during exposure therapies of PTSD: A network approach. European Journal of Psychotraumatology, 10(1), 1618134. https://doi.org/10.1080/20008198.2019.1618134
- Isvoranu, A-M, Epskamp, S., & Cheung, MW-L. (2021). Network models of posttraumatic stress disorder: A meta-analysis. Journal of Abnormal Psychology, 130(8), 841–861. https://doi.org/10.1037/abn0000704
- Kass, R. E., & Raftery, A. E. (1995). Bayes factors. Journal of the American Statistical Association, 90(430), 773–795. https://doi.org/10.1080/01621459.1995.10476572
- Kelley, L. P., Weathers, F. W. [Frank W.], McDevitt-Murphy, M. E., Eakin, D. E., & Flood, A. M. (2009). A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress, 22(3), 227–235. https://doi.org/10.1002/jts.20406
- Klipstein, L. v., Borsboom, D., & Arntz, A. (2021). The exploratory value of cross-sectional partial correlation networks: Predicting relationships between change trajectories in borderline personality disorder. PloS One, 16(7), e0254496. https://doi.org/10.1371/journal.pone.0254496
- Knefel, M., Tran, U. S., & Lueger-Schuster, B. (2016). The association of posttraumatic stress disorder, complex posttraumatic stress disorder, and borderline personality disorder from a network analytical perspective. Journal of Anxiety Disorders, 43, 70–78. https://doi.org/10.1016/j.janxdis.2016.09.002
- Krüger-Gottschalk, A., Knaevelsrud, C., Rau, H., Dyer, A., Schäfer, I., Schellong, J., & Ehring, T. (2017). The German version of the posttraumatic stress disorder checklist for DSM-5 (PCL-5): Psychometric properties and diagnostic utility. BMC Psychiatry, 17(1), 1–9. https://doi.org/10.1186/s12888-017-1541-6
- Macia, K. S., Raines, A. M., Maieritsch, K. P., & Franklin, C. L. (2020). Ptsd networks of veterans with combat versus non-combat types of index trauma. Journal of Affective Disorders, 277, 559–567. https://doi.org/10.1016/j.jad.2020.08.027
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., Reed, G. M., van Ommeren, M., Humayun, A., Jones, L. M., Kagee, A., Llosa, A. E., Rousseau, C., Somasundaram, D. J., Souza, R., Suzuki, Y., Weissbecker, I., Wessely, S. C., First, M. B., & Saxena, S. (2013). Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. The Lancet, 381(9878), 1683–1685. https://doi.org/10.1016/S0140-6736(12)62191-6
- Maercker, A., Brewin, C. R., Bryant, R. A., Cloitre, M., van Ommeren, M., Jones, L. M., Humayan, A., Kagee, A., Llosa, A. E., Rousseau, C., Somasundaram, D. J., Souza, R., Suzuki, Y., Weissbecker, I., Wessely, S. C., First, M. B., & Reed, G. M. (2013). Diagnosis and classification of disorders specifically associated with stress: Proposals for ICD-11. World Psychiatry, 12(3), 198–206. https://doi.org/10.1002/wps.20057
- Menéndez, M. L., Pardo, J. A., Pardo, L., & Pardo, M. C. (1997). The Jensen-Shannon divergence. Journal of the Franklin Institute, 334(2), 307–318. https://doi.org/10.1016/S0016-0032(96)00063-4
- Resick, P. A., Bovin, M. J., Calloway, A. L., Dick, A. M., King, M. W., Mitchell, K. S., Suvak, M. K., Wells, S. Y., Stirman, S. W., & Wolf, E. J. (2012). A critical evaluation of the complex PTSD literature: Implications for DSM-5. Journal of Traumatic Stress, 25(3), 241–251. https://doi.org/10.1002/jts.21699
- van Borkulo, C., van Bork, R., Boschloo, L., Kossakowski, J., Tio, P., Schoevers, R., Borsboom, D., & Waldorp, L. (2017). Comparing network structures on three aspects: A permutation test. https://doi.org/10.13140/RG.2.2.29455.38569.
- Weathers, F. W. [Frank W.], Blake, D., Schnurr, P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). National Center for PTSD. http://www.ptsd.va.gov.
- Weathers, F. W. [Frank W.], Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. (2013). The PTSD checklist for DSM-5 (PCL-5). National Center for PTSD. http://www.ptsd.va.gov.
- Williams, D. (2021). Bayesian estimation for Gaussian graphical models: Structure learning, predictability, and network comparisons. Multivariate Behavioral Research, 56(2), 336–352. https://doi.org/10.1080/00273171.2021.1894412
- Williams, D., & Mulder, J. (2020). BGGM: Bayesian Gaussian graphical models in R. Journal of Open Source Software, 5(51), 2111. https://doi.org/10.21105/joss.02111
- Williams, D., Rast, P., Pericchi, L., & Mulder, J. (2020). Comparing Gaussian graphical models with the posterior predictive distribution and Bayesian model selection. Psychological Methods, 25(5), 653–672. https://doi.org/10.1037/met0000254
- World Health Organization. (2021). ICD-11 coding tool. World Health Organization. https://icd.who.int/ct11/icd11_mms/en/release.