ABSTRACT
Background: Complex posttraumatic stress disorder (CPTSD) has recently been added to the ICD-11 diagnostic system for classification of diseases. The new disorder adds three symptom clusters to posttraumatic stress disorder (PTSD) related to disturbances in self-organization (affect dysregulation, negative self-concept, and disturbances in relationships). Little is known whether recommended evidence-based treatments for PTSD in youth are helpful for youth with CPTSD.
Objectives: This study examined whether Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT) is useful in reducing PTSD and CPTSD in traumatized youth.
Methods: Youth (n = 73, 89.0% girls, M age = 15.4 SD = 1.8) referred to one of 23 Norwegian child and adolescent mental health clinics that fulfilled the criteria for PTSD or CPTSD according to ICD-11 and received TF-CBT were included in the study. Assessments were conducted pre-treatment, and every fifth session. Linear mixed effects models were run to investigate whether youth with CPTSD and PTSD responded differently to TF-CBT.
Results: Among the 73 youth, 61.6% (n = 45) fulfilled criteria for CPTSD and 38.4% (n = 28) fulfilled criteria for PTSD. There were no differences in sex, age, birth country, trauma type, number of trauma types or treatment length across groups. Youth with CPTSD had a steeper decline in PTSD and CPTSD compared to youth with PTSD. The groups reported similar levels of PTSD and CPTSD post-treatment. The percentage of youth who dropped out of treatment was not different across groups. Further, the groups did not differ significantly in number of received treatment sessions.
Conclusions: This is the first study to examine whether TF-CBT is helpful for youth who have CPTSD using a validated instrument for measuring CPTSD. The results suggest that TF-CBT may be useful for treating CPTSD in youth. These are promising findings that should be replicated in studies with larger sample sizes.
HIGHLIGHTS
TF-CBT is a recommended treatment for youth with PTSD.
The ICD-11 introduced a new sibling disorder for Complex PTSD (CPTSD), but no studies have examined whether TF-CBT may be helpful for youth with CPTSD using a validated instrument.
The results show that youth with CPTSD respond well to TF-CBT.
Antecedentes: El trastorno de estrés postraumático complejo (TEPT-C) ha sido agregado recientemente al sistema de diagnóstico para la clasificación de enfermedades CIE-11. El nuevo trastorno agrega tres grupos de síntomas al trastorno de estrés postraumático (TEPT), relacionados con alteraciones en la autoorganización (desregulación afectiva, autoconcepto negativo y alteraciones en las relaciones). Poco se sabe acerca de si los tratamientos basados en evidencia recomendados para el TEPT en jóvenes son útiles para los jóvenes con TEPT-C.
Objetivos: Este estudio examinó si la Terapia Cognitiva Conductual Centrada en el Trauma (TF-CBT en sus siglas en inglés) es útil para reducir el TEPT y el TEPT-C en jóvenes traumatizados.
Método: Se incluyó en el estudio a jóvenes derivados a una de las 23 clínicas noruegas de salud mental para niños y adolescentes, que cumplían con los criterios para TEPT o TEPT-C según el CIE-11 y recibieron TF-CBT (n = 73, 89% niñas, Medad = 15,4, DE = 1,8). Se realizaron evaluaciones antes del tratamiento y cada cinco sesiones. Se ejecutaron modelos de efectos mixtos lineales para investigar si los jóvenes con TEPT-C y TEPT respondían de manera diferente a la TF-CBT.
Resultados: Entre los 73 jóvenes, el 61,6% (n = 45) cumplió con los criterios de TEPT-C y el 38,4% (n = 28) cumplió con los criterios de TEPT. No hubo diferencias en sexo, edad, país de nacimiento, tipo de trauma, número de tipos de trauma o duración del tratamiento entre los grupos. Los jóvenes con TEPT-C tuvieron una disminución más pronunciada en TEPT y TEPT-C en comparación con los jóvenes con TEPT. Los grupos reportaron niveles similares de TEPT y TEPT-C después del tratamiento. El porcentaje de jóvenes que abandonaron el tratamiento no difirió entre los grupos. Además, los grupos no difirieron significativamente en el número de sesiones de tratamiento recibidas.
Conclusiones: Éste es el primer estudio que examina si la TF-CBT es útil para los jóvenes que tienen TEPT-C mediante un instrumento validado para medir el TEPT. Los resultados sugieren que la TF-CBT puede ser útil para tratar el TEPT-C en jóvenes. Estos son hallazgos prometedores que deberían replicarse en estudios con tamaños muestrales más grandes.
摘要
背景:复杂性创伤后应激障碍 (CPTSD) 最近已被添加到用于疾病分类的 ICD-11 诊断系统中。这种新疾病在创伤后应激障碍 (PTSD)中增加了三个自我组织障碍相关的症状簇(情感失调、消极自我概念和人际关系障碍)。对于青少年 PTSD 的推荐循证治疗对于患有 CPTSD 的青少年是否有帮助尚不清楚。
目的:本研究考查了聚焦创伤的认知行为疗法 (TF-CBT) 是否有助于减少受创伤青少年的 PTSD 和 CPTSD。
方法:研究纳入了被转诊至 23 家挪威儿童和青少年心理健康诊所之一的符合 ICD-11 PTSD 或 CPTSD 标准并接受了 TF-CBT的青少年(n = 73,89.0 % 女孩,平均年龄 = 15.4,标准差 = 1.8)。评估在治疗前进行,每五个疗程进行一次。采用线性混合效应模型以考查患有 CPTSD 和 PTSD 的青少年对 TF-CBT 的反应是否不同。
结果:在 73 名青少年中,61.6%(n = 45)符合 CPTSD 标准,38.4%(n = 28)符合 PTSD 标准。性别、年龄、出生国家、创伤类型、创伤类型数量或治疗时间方面没有组间差异。与患有 PTSD 的青少年相比,患有 CPTSD 的青少年的 PTSD 和 CPTSD 下降幅度更大。这些组别报告了治疗后相似水平的 PTSD 和 CPTSD。退出治疗青少年的百分比无组间差异。此外,各组在接受治疗的次数上没有显著差异。
结论:这是第一项使用经过验证的 CPTSD 测量工具考查 TF-CBT 对于患有 CPTSD 的青少年是否有帮助的研究。结果表明,TF-CBT 可能对治疗青少年 CPTSD 有用。这些有希望的发现应该在更大样本量的研究中重复。
PALABRAS CLAVE:
1. Introduction
Complex posttraumatic stress disorder (CPTSD) has recently been included in the 11th revision of the International Classification of Diseases (World Health Organization, Citation2018) as a sibling disorder to posttraumatic stress disorder (PTSD). The addition of CPTSD to the diagnostic classifications has prompted a debate about the suitability of existing evidence-based treatments for persons who have developed CPTSD after trauma (Cloitre, Citation2015; De Jongh et al., Citation2016; Maercker et al., Citation2022). Separating CPTSD from PTSD has also led to an expectation that CPTSD is more difficult to treat (Lehrner & Yehuda, Citation2020). Although this may make sense clinically, this claim has not been substantiated empirically. The International Society of Traumatic Stress Studies (ISTSS) released its third revision of treatment guidelines in 2018 and concluded that the lack of studies on CPTSD both in the adult and child domain make treatment recommendations premature (ISTSS Guidelines Position Paper on Complex PTSD in Adults, Citation2019; ISTSS Guidelines Position Paper on Complex PTSD in Children and Adolescents, Citation2019). In this paper, we examine whether Trauma-Focused Cognitive-Behavioral Therapy (TF-CBT), a recommended treatment model for treating PTSD in youth (ISTSS, Citation2018), also is helpful for treating CPTSD.
In ICD-11, PTSD and CPTSD are defined as two distinct conditions under the category of ‘Disorders specifically associated with stress’. A diagnosis of PTSD requires at least one symptom within each of the three PTSD symptom clusters, which includes re-experiencing the traumatic experience in the present, deliberate avoidance, and a current sense of threat. CPTSD includes these three symptom clusters in addition to symptoms within three additional clusters that reflect disturbances in self-organization (DSO). These comprise affect dysregulation, negative self-concept, and disturbances in relationships. Importantly, the diagnosis is made based on symptom profile and does not require other types of trauma exposure distinct from PTSD (Brewin, Citation2020).
Given that CPTSD is a new disorder, there are to date no studies assessing predictors for CPTSD in youth clinical samples and no studies examining the effectiveness of treating CPTSD in youth using the new ICD-11 criteria with a validated instrument. Pending validated instruments, scholars have however used proxy instruments to measure CPTSD. A typical approach is to select items based on face validity using questions that are closely representative of the suggested DSO symptoms (see Cloitre et al., Citation2013 for a description). Using this strategy studies have shown that interpersonal trauma as well as multiple victimization predicts CPTSD (Eilers et al., Citation2021; Sachser et al., Citation2017).
Four studies have to date examined treatments effects for CPTSD in youth using proxy instruments. Eilers et al. (Citation2021) examined the use of a developmentally adapted youth model of Cognitive Processing Therapy (D-CPT) for CPTSD and found that both the CPTSD and the non-CPTSD groups showed significant symptom reductions. The CPTSD group reported however higher symptom severity both before and after treatment (Eilers et al., Citation2021). Similar results have been found in treatment studies for youth receiving TF-CBT (Hébert & Amedée, Citation2020; Ross et al., Citation2021; Sachser et al., Citation2017), suggesting that treatment length may need to be extended or the dosage of the individual components altered for youth with CPTSD. However, the findings are not consistent and Hébert and Amedée (Citation2020) found in their study of sexually abused children larger effect sizes for children classified as having CPTSD. Since youth with CPTSD struggle with disturbances in maintaining and forming interpersonal relationships, feelings of negative self-worth and affect regulation, one may assume that treatment attrition would be particularly high for this group of youth. Also, it has been suggested that treatment length should be extended relative to treating PTSD (Cloitre, Citation2020). However, studies examining dropout and treatment length are, to date, lacking, and treatment recommendations for youth with CPTSD are pending new studies (Jensen et al., Citation2020; Maercker et al., Citation2022).
In sum, to move the field forward there is a need for treatment studies that examine clinical samples with different trauma exposures using measurements developed to measure PTSD and CPTSD for children and adolescents (Cloitre et al., Citation2021; Maercker et al., Citation2022). In this paper, we address this gap by examining what characterizes youth who have developed CPTSD and whether TF-CBT is helpful for treating CPTSD. We also compare treatment length and dropout rates between the groups. Since TF-CBT is currently being used and implemented in several countries throughout the world, it is particularly valuable to know more about its effects on CPTSD.
The research questions are:
What characterizes youth in treatment who have CPTSD compared to youth who have PTSD?
We explore potential differences in trauma exposure (i.e. type of trauma and number of different types of trauma exposures), sex, and age. We hypothesize that CPTSD is associated with interpersonal trauma and multiple traumas. Due to lack of studies on clinical samples of youth with CPTSD we have no predefined hypotheses regarding associations between sex, age and CPTSD.
(2) Do youth with CPTSD and PTSD respond differently to TF-CBT?
Based on the literature we hypothesize that youth with CPTSD and PTSD report a significant reduction in symptoms from pre- to post-treatment, but that the youth with PTSD have a steeper recovery slope.
(3) Do youth with CPTSD receive more treatment sessions than youth with PTSD?
Based on suggestions from the developers of TF-CBT that youth with complex trauma may need more sessions than given in standard TF-CBT, we hypothesize that youth with CPTSD will receive significantly more sessions than the youth with PTSD.
(4) Is there a higher drop-out rate for youth presenting with CPTSD than for youth with PTSD?
We hypothesize that, due to the disturbances in self-organisation associated with CPTSD, the drop-out rate will be significantly higher than in the PTSD group.
2. Methods
2.1. Procedures
This is a naturalistic observational study of a clinical sample of youth who were referred to one of 23 Norwegian child and adolescent mental health clinics during 2018–2020.
All therapists in the participating clinics were trained in trauma and screening of posttraumatic stress symptoms (PTSS). Routine screening procedures for trauma and PTSS were implemented so that all newly referred youth were screened by a therapist during one of the first meetings at the clinic. When found eligible for TF-CBT, the patient and her or his caregiver(s) were asked by the therapist to take part in the study and informed consent was given. A group of trained TF-CBT therapists (N = 74) recruited youth to the study, which averages to approximately 2.3 youth per therapist. All data, including the consent form, were securely transferred to the University of Oslo Services for Sensitive Data for storage. The study was approved by the Norwegian Regional Committee for Medical and Health Research Ethics, and the Norwegian Centre for Research Data.
2.2. Participants and study design
Among the referred patients, 173 youth were eligible for receiving TF-CBT and agreed to participate in the study according to the following criteria: exposure to at least one potentially traumatic event, age between 6 and 18 years, and PTSS of clinically significance, defined as a score of ≥15 on CATS-2 (Child and Adolescent Trauma Screen-2; Sachser et al., Citation2022). Among these, 73 fulfilled criteria for either PTSD or CPTSD and were included in the study sample (89.0% girls M age = 15.4, SD = 1.8). Therapists were asked to collect data from their patients every fifth session, and in this study, we use data from pre-treatment (T1), session 5 (T2), session 10 (T3), session 15 (T4) and post-treatment (T5).
2.3. Measurement instruments
Exposure to potentially traumatic events, posttraumatic stress disorder and complex posttraumatic disorder were measured by the Child and Adolescent Trauma Screen 2 (CATS-2) (Sachser et al., Citation2022). CATS-2 measures PTSD according to both DSM-5 and ICD-11, as well as CPTSD according to ICD-11. Since the screening for PTSS in the clinics is part of an overall assessment for treatment needs and treatment planning, the CATS-2 was administered by a clinician. This allowed the clinician to ask further follow-up questions to the youth to ensure valid responses. Potentially traumatizing events are first assessed using a 15-item structured checklist following the definitions of traumatic events in the DSM-5 and ICD-11 and include natural disasters, serious accidents, experiencing or witnessing violence at home or in the community, sexual abuse (off- and online), serious bullying – saying scaring things (off- and online), traumatic loss, stressful or scary medical procedures and war. Participants can indicate whether they had experienced the event by checking ‘yes’ or ‘no’. Those respondents who have experienced at least one such event are then assessed for symptoms experienced the last four weeks using 25 PTSS items rated on a 4-point Likert scale with the following anchors: 0 = ‘Never’, 1 = ‘Sometimes’, 2 = ‘Often’, 3 = ‘Almost Always’. The 25 items map directly onto the diagnostic criteria for PTSD in DSM-5 and ICD-11 PTSD and CPTSD. The CATS-2 has demonstrated good internal consistency and construct validity. In this study, Cronbach’s alpha was .64 for ICD-11 PTSD (6 items), .82 for ICD-11 CPTSD (12 items), and .79 for the six DSO items of CPTSD. According to the ICD-11 criteria, CPTSD requires fulfilling criteria for PTSD as well as DSO symptoms. We used the algorithms for probable PTSD and CPTSD according to the ICD-11 criteria to identify youth with probable PTSD (without CPTSD) and youth with probable CPTSD. In the remaining text, we use the terms PTSD and CPTSD to refer to probable PTSD and CPTSD diagnoses.
2.4. Intervention
TF-CBT is a phase-based trauma treatment for children and adolescents who experience posttraumatic stress following trauma exposure. It consists of three phases. The first skills building phase consists of: psychoeducation, learning stress reduction skills, affect modulation and cognitive coping. The next phase consists of trauma processing and includes creating a trauma narrative and altering maladaptive cognitions. The last phase is a consolidation phase where skills are reinforced. An integrative part of TF-CBT is the parallel work with caregivers to support the therapy and build caregiver skills (Cohen et al., Citation2016). The components are used flexibly and tailored to the individual needs of the youth and family. Typically, the length of the treatment is 12–16 sessions. However, since youth with complex trauma often have regulation and relational problems, the authors have argued that more time may be allocated to the skills building phase, and the total treatment length often needs to be extended, sometimes up to a total of 30 sessions (see Cohen et al., Citation2012).
2.5. Dropout, fidelity and missing data
Dropout was defined by the therapist and was conceptualized as not receiving the full TF-CBT protocol according to the therapist judgement. This means that therapists recorded drop-out in cases where the youth stopped attending the therapy sessions when this was not agreed upon. Some youths were also offered other treatments after a re-assessment, and these are also included as dropouts. Based on this the therapists reported that of the 73 youth, 24.7% (n = 18) dropped out of treatment. Of these, 27.8% (n = 5) of the youth were offered other treatment methods, 11.1% (n = 2) moved, and 22.2% (n = 4) did not wish to continue treatment. For the remaining 38.9% (n = 7) we do not have information on reasons for dropping out. Logistic regressions show that the odds of dropping out of treatment were not related to pre-treatment levels of PTSD (p = .596), pre-treatment levels of CPTSD (p = 0.750), sex (p = .981), or age (p = .836).
Of the 55 remaining youth, 83.6% (n = 46) received TF-CBT with sufficient fidelity as assessed by a TF-CBT certified supervisor using a modified version of the TF-CBT Brief Practice Fidelity Checklist (TF-CBT, Citation2022). A total of 16.4% (n = 9) youths did not receive TF-CBT with fidelity. The percentage of youths who received TF-CBT with fidelity was not different in youth with CPTSD as compared to youth with PTSD (p = .321). Of these 55 participants, 30 provided data post-treatment whereas data from the remaining 25 patients were missing. Logistic regressions indicate that among these 55, the odds of missing data were not related to pre-treatment levels of PTSD (p = .442), pre-treatment levels of CPTSD (p = .881), sex (p = .536), or age (p = .131).
Of our intent-to-treatment sample of 73 participants at post-treatment (T1), the number who provided data at each of the following four time points were: T2: n = 19, T3: n = 15, T4: n = 5, and T5, n = 30. We compared levels of symptoms of PTSD and CPTSD at each time point between the participants who provided data at post-treatment (n = 30) and those who did not (n = 43) and found no significant differences at T1, T2 or T3 (due to missing data this was not possible to examine in T4 or T5; see Tables S1 and S2 and Figures S1 and S2 in the supplemental materials). In summary, we did not find evidence of systematic differences in the most relevant observed variables between participants who dropped out of TF-CBT or not, or between participants who provided post-treatment data or not. This could imply that missing data is completely at random (MCAR), however we choose to be more conservative and assume that data are missing at random (MAR).
2.6. Analyses
To assess the characteristics of youth with CPTSD compared to youth with PTSD, we conducted descriptive statistics with t-tests and chi-square tests. To investigate whether youth with CPTSD and PTSD responded differently to TF-CBT, we used linear mixed effects models. Linear mixed effects modelling was chosen as the main analytic strategy due to its ability to include both fixed and random effects and because it uses maximum likelihood to handle missing data. This approach assumes data are missing at random (MAR), and all observed information is used to produce the maximum likelihood estimation of parameters. Maximum likelihood is one of the recommended ways to handle missing data (Schafer & Graham, Citation2002).
In order to test differences in continuous scores in our intent to treat sample (n = 73), we conducted three linear mixed effects models, with levels of PTSS, CPTSD, and disturbance in self-organization (DSO) as outcomes. We added random effects of participants and therapists. We also did a sensitivity analysis using data only from a subsample with the participants who provided data at post-treatment (n = 30). Differences in dropout and number of sessions across groups were examined with chi-square tests and ANOVA tests. We used IBM SPSS Statistics and R with the package nmle (Pinheiro & Bates, Citation2000).
3. Results
3.1. Characteristics of youth with CPTSD compared to youth with PTSD
Among the 73 youth fulfilling the criteria for either PTSD or CPTSD according to ICD-11, 61.6% (n = 45) fulfilled criteria for CPTSD and 38.4% (n = 28) fulfilled criteria for PTSD provides an overview of baseline demographics of the total sample, participants with subclinical symptoms of PTSS, participants with PTSD, and participants with CPTSD. No significant differences between youth with CPTSD, and youth with PTSD were found in sex, age, birth country (Norway vs other), trauma type or number of trauma types.
Table 1. Sample characteristics (n = 73).
3.2. Treatment response in youth with CPTSD compared to youth with PTSD
As expected, pre-treatment levels of PTSS were higher in youth with CPTSD than in youth with PTSD (difference = 2.82, p = .002) (, ). The slopes indicate significant decreases in PTSS over time in youth with PTSD (estimate = –1.42, p < .001) and CPTSD (estimate = −2.09, p < .001). Thus, between each of the time points (T1-T5), the PTSS level decreased with on average 1.42 for those with PTSD and 2.09 for those with CPTSD. The difference between these two slopes was significant (difference = −0.66, p = .015), indicating that the change was greater for youth with CPTSD than youth with PTSD.
Figure 1. Levels of posttraumatic stress symptoms (PTSS) in youth with CPTSD compared to youth with PTSD over the course of TF-CBT, measured pre-treatment, session 5, session 10, session 15 and post-treatment.
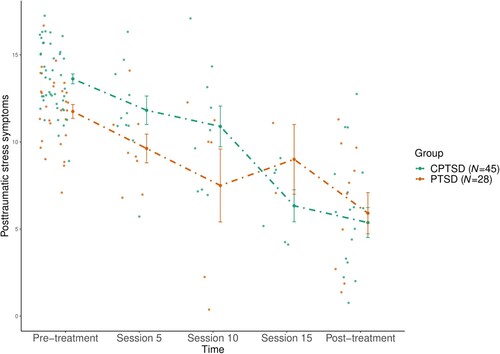
Table 2. Associations between CPTSD (vs PTSD) and change in symptoms of posttraumatic stress and complex posttraumatic stress from pre-treatment to post-treatment (T1–T5) in the intent to treat sample (n = 73)Table Footnotea.
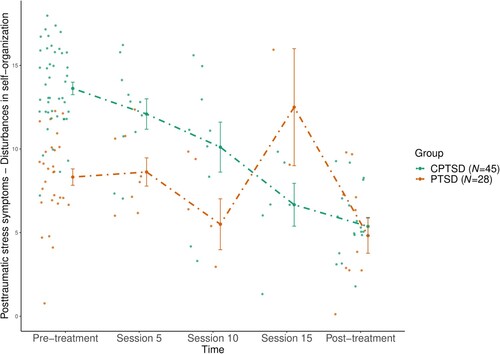
Similar findings were revealed when examining changes in levels of CPTSS (, ) and levels of DSO (, ). Compared to youth with PTSD, youth with CPTSD had higher levels of CPSS at pre-treatment (difference = 9.24, p < .001), and a steeper decrease in CPSS from pre- to post-treatment (estimate = −2.28, p < .001 vs estimate = −4.16, p < .001, difference = −1.87, p < .001). Similarly, youth with CPTSD reported higher pre-treatment levels of DSO than youth with PTSD (difference = 6.43, p < .001), and a steeper decrease in DSO from pre- to post-treatment (difference = −1.22, p < .001). Our sensitivity analysis using data from the subsample of participants providing post-treatment data provided similar results (see Table S3 in the Supplementary materials).
Figure 2. Levels of complex posttraumatic stress symptoms (CPTSS) in youth with CPTSD compared to youth with PTSD over the course of TF-CBT, measured pre-treatment, session 5, session 10, session 15 and post-treatment.
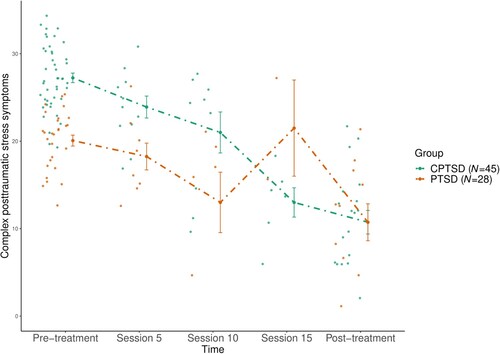
Figure 3. Levels of disturbances in self-organization (DSO) in youth with CPTSD compared to youth with PTSD over the course of TF-CBT, measured pre-treatment, session 5, session 10, session 15 and post-treatment.
Among youth who provided post-treatment data (n = 30), all with pre-treatment diagnosis of CPTSD (n = 19) lost their CPTSD diagnosis at post-treatment, and three (15.8%) had PTSD. All with pre-treatment diagnosis of PTSD (n = 11) lost their diagnosis at post-treatment.
3.3. Dropout and number of sessions for youth with CPTSD as compared to in youth with PTSD
The percentage of youth with CPTSD who dropped out of treatment (20.0%, n = 9) was not significantly different from the percentage of youth with PTSD who dropped out of treatment (32.1%, n = 9, p = .242). Youth with CPTSD received on average 17.5 sessions of TF-CBT (including caregiver sessions), which was not significantly different from the number of sessions received by youth with PTSD (17.2 sessions, p = .902). The mean number of sessions the dropout group completed was 9.13 (SD 5.40).
4. Discussion
In this study, we set out to examine pre-treatment characteristics, treatment response, treatment length, and dropout rates in youth with CPTSD compared to youth with PTSD where both groups received TF-CBT. The results showed no differences in sex, age, birth country, trauma type, number of trauma types or treatment length across groups. Compared to youth with PTSD, youth with CPTSD had a steeper decline in both PTSS and CPTSS over the course of TF-CBT and they also had a steeper decrease in DSO from pre- to post-treatment. The CPTSD group did not receive more treatment sessions and the percentage of youth who dropped out of treatment was not different across groups. At post-treatment, the groups reported similar levels of PTSS and CPTSS.
It was somewhat surprising that we did not find any significant differences in pre-treatment characteristics between youth with PTSD and CPTSD. Studies have found that the prevalence of PTSD in youth varies by trauma type, with higher rates occurring after interpersonal trauma both in community samples (Alisic et al., Citation2014), and in clinical samples (Birkeland et al., Citation2022). Multiple and prolonged trauma in childhood has also been associated with symptom complexity (Cloitre et al., Citation2009; Dierkhising et al., Citation2019; Trickey et al., Citation2012). Nonetheless the ICD workgroup, recognizing that studies have also shown that symptom trajectories are idiosyncratic (Cloitre et al., Citation2013), did not limit the CPTSD stressor identifier to interpersonal and prolonged trauma but mentions it as a potential risk factor (Brewin, Citation2020). Our study lends support to this conclusion and shows that type of trauma exposure in itself may not be the crucial factor in determining complexity in responses for youth.
The finding that youth with CPTSD had a more rapid improvement of symptoms and that the difference in post-treatment PTSS scores was non-significant is promising. It was also promising that the decline in DSO symptoms was comparable and that all CPTSD youth lost their probable diagnosis albeit three still fulfilled the criteria for PTSD diagnosis. It is positive that an evidenced-based practice such as TF-CBT shows such encouraging results. If other evidence-based practices also show similar results in future studies this means that clinicians may not need to learn many new methods but can build on their existing expertise to also help youth with CPTSD.
Consistent with Judith Herman’s early work (Citation1992) related to the treatment of complex trauma, it has been suggested that treatment for adults who have experienced interpersonal trauma should be given in a phase-based approach where the first phase includes symptom management and skill building before the second phase of trauma processing and exposure (see Cloitre et al., Citation2013; Karatzias & Cloitre, Citation2019). Since TF-CBT is a phase-based treatment for PTSD in children and adolescents, it may not be so surprising that youth with CPTSD showed improvement. It may also be that TF-CBT is particularly helpful since the model focuses on improving interpersonal relationships and cognitive distortions, as well as including parents in the treatment to enhance personal relationships. The findings are also consistent with the findings reported by Sachser et al. (Citation2017), where both youth with PTSD and CPTSD improved with large effect sizes after receiving TF-CBT, although many in their study still had elevated symptoms post-treatment. Other studies have also shown TF-CBT to be helpful for youth with a range of experiences typically defined as complex, such as violence and sexual abuse (Cohen et al., Citation2005; Cohen et al., Citation2010; Cohen et al., Citation2011; Goldbeck et al., Citation2016; Jensen et al., Citation2014). In fact, the TF-CBT treatment protocol was originally developed for youth who had experienced sexual abuse (Cohen et al., Citation2016).
It was more surprising that the treatment length was not significantly longer for the youth with CPTSD compared to youth with PTSD. In TF-CBT for PTSD the recommended treatment length is 12–15 sessions, and the therapist typically spends about one-third of the time equally on the three phases (skill building, trauma narration and processing, integration and consolidation). For complex trauma, the developers have proposed that the length of the therapy may be extended to 25–30 sessions as these youth may need longer time on the skill building activities and that half of the sessions are devoted to skill building and half of the time on the two remaining phases (Cohen et al., Citation2012; Cohen et al., Citation2017) Although our study was not specifically designed to test this, the findings do suggest that additional sessions are not always necessary. Further studies should however seek to examine both the sequencing of components and treatment dose.
Because youth with CPTSD struggle with relational issues such as trusting others and having negative self-appraisals, which may lead to negative foresight and lack of hope for the future, we had anticipated that there would be a higher dropout from treatment in the CPTSD group. Although it is concerning that 20.0% with CPTSD did drop out of treatment, this percentage was similar to the dropout from the PTSD group (32.1%). It may be that the initial components in TF-CBT where psychoeducation about trauma and its effects and cognitive appraisals are addressed, helped to alleviate shame and self-blame and keep them in treatment. Also, previous studies have shown that youth receiving TF-CBT score high on alliance and that this is an important predictor for treatment retention (Ormhaug et al., Citation2014; Ormhaug & Jensen, Citation2018). However, the sample size for the dropout analysis was low and further studies are needed to establish whether there are higher risks for treatment termination among youth with CPTSD.
This is the first study to examine the effect of an evidenced-based treatment for traumatized youth with CPTSD with a validated measure. The participants were recruited from regular (non-trauma specialist) mental health outpatient clinics and had experienced a wide range of traumas strengthening the external validity of the findings. However, the results must be interpreted with some caution. This is a naturalistic observational study, and the findings need to be supplemented with a randomized controlled study to test the differential effect of TF-CBT on CPTSD compared to other interventions. The sample size was small and there was missing data that may have affected the results. It may be that therapists in the study selectively omitted reporting on cases with less promising results. We have however examined predictors of dropout and missing data, examined differences between participants who provided post-treatment data, as well as conducted sensitivity analyses that all indicated that this is not very probable. The greater amount of change in youth with CPTSD compared to PTSD could also be due to their higher PTSS and DSO baseline scores which provided a greater potential range of change than for the PTSD youth. On the other hand, studies have shown that more severe and impairing psychopathology scores pre-treatment is associated with less favourable outcomes (Compton et al., Citation2014), so the finding that the improvement slope was higher in the CPTSD group is very encouraging. Although the dropout rate was comparable to other studies and the dropout rate was lower in the CPTSD group, we do not know whether those that dropped out were different in other respects. And finally, the study needs to be replicated with a larger sample size and although a validated measure was used to measure CPTSD, self-reporting should be supplemented with clinician-rated diagnosis. There are to date no such instruments for CPTSD.
5. Conclusion
At present, most research on youth treatment for CPTSD focuses on post hoc analyses using items extracted from several self-report measures and clinical interviews, and they are therefore best regarded as approximations. In this study, we were able to test whether TF-CBT can be helpful for youth with CPTSD using a validated measure. In conclusion, youth with CPTSD experienced a significant decline in symptoms, did not seem to need an extended number of sessions, and did not drop out more than youth with PTSD. Importantly the youth experienced a significant decline in DSO symptoms. This is good news for clinicians and youth, because it indicates that TF-CBT can be implemented and offered for this group of youth as well. Still, many do drop out and some do not respond to treatment. Hence more studies are needed to disentangle the relative importance, temporal order, and dosage of the components in TF-CBT for CPTSD. Also, the finding that pre-treatment factors such as trauma type and multi-traumatization does not seem to impede on treatment results is encouraging, and clinicians should pay attention to the severity of symptoms rather than to exposure per se.
Supplemental Material
Download MS Word (30.2 KB)Acknowledgements
We wish to thank the TF-CBT implementation team at the Norwegian Center for Violence and Traumatic Stress Studies, participating clinics, therapists and families for contributing data to this paper.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
According to European law (GDPR), data containing potentially identifying or sensitive patient information are restricted. Our data involving clinical participants are therefore not freely available. Data may be made available upon reasonable request.
Additional information
Funding
References
- Alisic, E., Zalta, A. K., van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., & Smid, G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. The British Journal of Psychiatry, 204(5), 335–340.
- Birkeland, M. S., Skar, A.-M. S., & Jensen, T. K. (2022). Understanding the relationships between trauma type and individual posttraumatic stress symptoms: A cross-sectional study of a clinical sample of children and adolescents. Journal of Child Psychol Psychiatry. https://doi.org/10.1111/jcpp.13602
- Brewin, C. R. (2020). Complex post-traumatic stress disorder: A new diagnosis in ICD-11. BJPsych Advances, 26(3), 145–152. https://doi.org/10.1192/bja.2019.48
- Cloitre, M. (2015). The ‘one size fits all’ approach to trauma treatment: Should we be satisfied? European Journal of Psychotraumatology, 6(1), Article 27344. https://doi.org/10.3402/ejpt.v6.27344
- Cloitre, M. (2020). ICD-11 complex post-traumatic stress disorder: Simplifying diagnosis in trauma populations. The British Journal of Psychiatry, 216(3), 129–131. https://doi.org/10.1192/bjp.2020.43
- Cloitre, M., Brewin, C. R., Kazlauskas, E., Lueger-Schuster, B., Karatzias, T., Hyland, P., & Shevlin, M. (2021). Commentary: The need for research on PTSD in children and adolescents – a commentary on Elliot et al. (2020). Journal of Child Psychology and Psychiatry, 62(3), 277–279. https://doi.org/10.1111/jcpp.13361
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. European Journal of Psychotraumatology, 4(1), 20706. https://doi.org/10.3402/ejpt.v4i0.20706
- Cloitre, M., Stolbach, B. C., Herman, J. L., Kolk, B. V. D., Pynoos, R., Wang, J., & Petkova, E. (2009). A developmental approach to complex PTSD: Childhood and adult cumulative trauma as predictors of symptom complexity. Journal of Traumatic Stress, 22(5), 399–408. https://doi.org/10.1002/jts.20444
- Cohen, J. A., Berliner, L., & Mannarino, A. P. (2010). Trauma focused CBT for children with co-occurring trauma and behavior problems. Child Abuse & Neglect, 34(4), 215–224. https://doi.org/10.1016/j.chiabu.2009.12.003
- Cohen, J. A., Deblinger, E., & Mannarino, A. P. (2005). Trauma-focused cognitive-behavioral therapy for sexually abused children. American Psychological Association.
- Cohen, J. A., Deblinger, E., & Mannarino, A. P. (2016). Trauma-Focused Cognitive Behavioral Therapy for children and families. Psychotherapy Research, 28, (1), 47–57. https://doi.org/10.1080/10503307.2016.1208375
- Cohen, J. A., Mannarino, A. P., & Deblinger, E. (2017). Treating trauma and traumatic grief in children and adolescents (2nd ed.). The Guilford Press.
- Cohen, J. A., Mannarino, A. P., & Iyengar, S. (2011). Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics Adolescent Medicine, 165(1), 16–21. https://doi.org/10.1001/archpediatrics.2010.247. http://archpedi.ama-assn.org/cgi/content/abstract/165/1/16
- Cohen, J. A., Mannarino, A. P., Kliethermes, M., & Murray, L. A. (2012). Trauma-focused CBT for youth with complex trauma. Child Abuse & Neglect, 36(6), 528–541. https://doi.org/10.1016/j.chiabu.2012.03.007
- Compton, S. N., Peris, T. S., Almirall, D., Birmaher, B., Sherrill, J., Kendall, P. C., March, J. S., Gosch, E. A., Ginsburg, G. S., Rynn, M. A., Piacentini, J. C., McCracken, J. T., Keeton, C. P., Suveg, C. M., Aschenbrand, S. G., Sakolsky, D., Iyengar, S., Walkup, J. T., & Albano, A. M. (2014). Predictors and moderators of treatment response in childhood anxiety disorders: Results from the CAMS trial. Journal of Consulting and Clinical Psychology, 82(2), 212–224. https://doi.org/10.1037/a0035458
- De Jongh, A., Resick, P. A., Zoellner, L. A., Van Minnen, A., Lee, C. W., Monson, C. M., Foa, E. B., Wheeler, K., Broeke, E. T., Feeny, N., & Rauch, S. A. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33(5), 359–369. https://doi.org/10.1002/da.22469
- Dierkhising, C. B., Ford, J. D., Branson, C., Grasso, D. J., & Lee, R. (2019). Developmental timing of polyvictimization: Continuity, change, and association with adverse outcomes in adolescence. Child Abuse and Neglect, 87, 40–50. https://doi.org/10.1016/j.chiabu.2018.07.022
- Eilers, R., Rimane, E., Vogel, A., Renneberg, B., Steil, R., & Rosner, R. (2021). Response of young patients with probable ICD-11 complex PTSD to treatment with developmentally adapted cognitive processing therapy. European Journal of Psychotraumatology, 12(1), Article 1929024. https://doi.org/10.1080/20008198.2021.1929024
- Goldbeck, L., Muche, R., Sachser, C., Tutus, D., & Rosner, R. (2016). Effectiveness of Trauma-Focused Cognitive Behavioral Therapy for children and adolescents: A randomized controlled trial in eight German mental health clinics. Psychotherapy and Psychosomatics, 85(3), 159–170. https://doi.org/10.1159/000442824
- Herman, J. L. (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5(3), 377–391. https://doi.org/10.1002/jts.2490050305
- Hébert, M., & Amedée, L. M. (2020). Latent class analysis of post-traumatic stress symptoms and complex PTSD in child victims of sexual abuse and their response to Trauma-Focused Cognitive Behavioural Therapy. European Journal of Psychotraumatology, 11(1), Article 1807171. https://doi.org/10.1080/20008198.2020.1807171
- International Society for Traumatic Stress Studies. (2018). New ISTSS prevention and treatment guidelines. www.istss.org/treating-trauma/new-istss-prevention-and-treatment-guidelines.aspx
- ISTSS Guidelines Position Paper on Complex PTSD in Adults. (2019). www.istss.org/getattachemen/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_CPTSD-Position-Paper-(Adults)_FNL.pdf.aspx
- ISTSS Guidelines Position Paper on Complex PTSD in Children and Adolescents. (2019). www.istss.org/getattachemen/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_CPTSD-Position-Paper-(Children-and-Adolescents)_FNL.pdf.aspx
- Jensen, T. K., Cohen, J., Jaycox, L., & Rosner, R. (2020). Treatment of PTSD and complex PTSD. In D. Forbes, J. I. Bisson, C. M. Monson, & L. Berliner (Eds.), Effective treatments for PTSD. Practice guidelines from the International Society for Traumatic Stress Studies (3rd ed., pp. 385–413). The Guilford Press.
- Jensen, T. K., Holt, T., Ormhaug, S. M., Egeland, K., Granly, L., Hoaas, L. C., Hukkelberg, S. S., Indregard, T., Stormyren, S. D., & Wentzel-Larsen, T. (2014). A randomized effectiveness study comparing Trauma-Focused Cognitive Behavioral Therapy with therapy as usual for youth. Journal of Clinical Child & Adolescent Psychology, 43(3), 356–369. https://doi.org/10.1080/15374416.2013.822307
- Karatzias, T., & Cloitre, M. (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. https://doi.org/10.1002/jts.22457
- Lehrner, A., & Yehuda, R. (2020). PTSD diagnoses and treatments: Closing the gap between ICD-11 and DSM-5. BJPsych Advances, 26(3), 153–155. https://doi.org/10.1192/bja.2020.10
- Maercker, A., Cloitre, M., Bachem, R., Schlumpf, Y. R., Khoury, B., Hitchcock, C., & Bohus, M. (2022). Complex post-traumatic stress disorder. The Lancet, 400(10345), 60-72. https://doi.org/10.1016/S0140-6736(22)00821-2
- Ormhaug, S. M., & Jensen, T. K. (2018). Investigating treatment characteristics and first-session relationship variables as predictors of dropout in the treatment of traumatized youth. Psychotherapy Research, 28(2), 235–249. https://doi.org/10.1080/10503307.2016.1189617
- Ormhaug, S. M., Jensen, T. K., Wentzel-Larsen, T., & Shirk, S. R. (2014). The therapeutic alliance in treatment of traumatized youths: Relation to outcome in a randomized clinical trial. Journal of Consulting and Clinical Psychology, 82(1), 52–64. https://doi.org/10.1037/a0033884
- Pinheiro, J., & Bates, D. (2000). Mixed effects models in S and S-Plus. New York: Springer-Verlag.
- Ross, S. L., Sharma-Patel, K., Brown, E. J., Huntt, J. S., & Chaplin, W. F. (2021). Complex trauma and trauma-focused cognitive-behavioral therapy: How do trauma chronicity and PTSD presentation affect treatment outcome? Child Abuse and Neglect, 111, Article 104734. https://doi.org/10.1016/j.chiabu.2020.104734
- Sachser, C., Berliner, L., Risch, E., Rosner, R., Birkeland, M. S., Eilers, R., Hafstad, R. S., Pfeiffer, E., Plener, P. L., & Jensen, T. K. (2022). The child and adolescent trauma screen 2 (CATS-2) – validation of an instrument to measure DSM-5 and ICD-11 PTSD and complex PTSD in children and adolescents. European Journal of Psychotraumatology, 13(2), Article 2105580. https://doi.org/10.1080/20008066.2022.2105580
- Sachser, C., Keller, F., & Goldbeck, L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to Trauma-Focused Cognitive Behavioral Therapy. Journal of Child Psychology and Psychiatry, 58(2), 160–168. https://doi.org/10.1111/jcpp.12640
- Schafer, J. L., & Graham, J. W. (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. https://doi.org/10.1037/1082-989X.7.2.147
- TF-CBT Brief Practice Fidelity Checklist. (2022). https://tfcbt.org/tf-cbt-brief-practice-fidelity-checklist/
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychological Review, 32(2). https://doi.org/10.1016/j.cpr.2011.12.001
- World Health Organization. (2018). International statistical classification of diseases and related health problems (11th review). https://www.who.int/classifications/icd/en
