ABSTRACT
Background:
Post-traumatic stress symptoms (PTSS) are often experienced by children and family members after pediatric traumatic medical events (PTMEs). Assessing families’ psychosocial risk factors is a crucial part of trauma-informed practice as it helps identify risk for PTSS in the aftermath of PTME.
Objectives:
Using the Psychosocial Assessment Tool 2.0 (PAT2.0), this study describes the psychosocial risk of families following PTMEs in two ways: 1. Describing the psychosocial risk defined by the PAT2.0 based on three-tiered risk levels; 2. Using latent profile analysis (LPA); identifying psychosocial risk profiles and examining how child- and injury-related factors can affect profile membership.
Methods:
Caregivers of 374 children following PTMEs admitted to a pediatric rehabilitation department in Israel completed the PAT2.0. Total PAT2.0 score and the seven PAT2.0 subscales (family structure/resources, social support, child problems, sibling problems, family problems, caregiver stress reactions, and family beliefs) were included in the first analysis. Mean PAT2.0 scores of three risk categories (universal, targeted, clinical) were calculated; LPA, which allows for cross-sectional latent variable mixture models to identify heterogeneity within a population, and multinomial logistic regressions using six out of the seven PAT2.0 subscales, were used to determine distinct profile differences and predictors of profile membership.
Results:
The three-tiered risk levels revealed were relatively high, as compared to levels in families of children with other clinical diagnoses. LPA yielded a three-profile solution: low family risk (63.53%); high caregiver stress, above-average levels of family risk (22.5%); and sibling problems, above-average levels of family risk (13.94%). Ethnicity and type of injury predicted group membership.
Conclusion:
Families of children following PTMEs are at increased psychosocial risk. A clinically useful approach to identifying and preventing PTSS may be to evaluate specific domain patterns rather than just the total PAT2.0 risk level alone, based on the PAT2.0 subscales.
HIGHLIGHTS
Families of children in pediatric rehabilitation are prone to significant psychosocial risk following traumatic medical events.
Using latent profile analysis of PAT2.0 psychosocial risk domains in pediatric rehabilitation identified specific patterns of risk factors.
Screening for all families of children hospitalised following pediatric medical events may enable the facilitation of early interventions and appropriate allocation of medical support resources to those in greatest need.
Antecedentes: Síntomas de estrés postraumático (SEPT) a menudo son experimentados por los niños y miembros de la familia después de eventos médicos pediátricos traumáticos (PTME, por sus siglas en inglés). La evaluación de los factores de riesgo psicosocial de las familias es una parte crucial de la práctica informada sobre el trauma, ya que ayuda a identificar el riesgo de SEPT después de PTME.
Objetivos: Usando la Herramienta de Evaluación Psicosocial 2.0 (PAT2.0), este estudio describe el riesgo psicosocial de las familias luego de un PTME de dos maneras: 1. Describiendo el riesgo psicosocial definido por la PAT2.0 basado en niveles de riesgo en tres niveles; 2. Usando un análisis de perfiles latentes (LPA, por sus siglas en inglés); identificar perfiles de riesgo psicosocial y examinar cómo los factores relacionados con los niños y las lesiones pueden afectar la pertenencia al perfil.
Métodos: Los cuidadores de 374 niños después de un PTME admitidos en un departamento de rehabilitación pediátrica en Israel completaron el PAT2.0. En el primer análisis se incluyeron la puntuación total de PAT2.0 y las siete subescalas de PAT2.0 (estructura/recursos familiares, apoyo social, problemas de los niños, problemas de hermanos, problemas familiares, reacciones de estrés del cuidador y creencias familiares). Se calcularon las puntuaciones medias de PAT2.0 de tres categorías de riesgo (universal, específico, clínico); se usaron LPA, que permite crear modelos transversales de una mezcla de las variables latentes para identificar la heterogeneidad dentro de una población, y regresiones logísticas multinomiales usando seis de las siete subescalas PAT2.0, para determinar distintas diferencias de perfil y predictores de membresía al perfil.
Resultados: Los tres niveles de riesgo revelados fueron relativamente altos, en comparación con los niveles en familias de niños con otros diagnósticos clínicos. LPA arrojó una solución de tres perfiles: bajo riesgo familiar (63,53%); alto estrés del cuidador, niveles de riesgo familiar superiores a la media (22,5%); y problemas entre hermanos, niveles de riesgo familiar superiores a la media (13,94%). La pertenencia étnica y el tipo de lesión pronosticaron la pertenencia al grupo.
Conclusión: Las familias de niños que presentan PTME tienen un mayor riesgo psicosocial. Un enfoque clínicamente útil para identificar y prevenir el TEPT puede ser evaluar patrones de dominio específicos en lugar de solo el nivel de riesgo total de PAT2.0, basado en las subescalas de PAT2.0.
背景:儿童和家人在儿科创伤性医疗事件 (PTME) 后经常经历创伤后应激症状 (PTSS)。评估家庭的心理社会风险因素是创伤知情实践的重要组成部分,因为它有助于识别 PTME 后发生 PTSS 的风险。
目的:本研究使用心理社会评估工具 2.0(PAT2.0),从两个方面描述PTME 后家庭的心理社会风险: 1. 根据基于三层风险水平的PAT2.0 定义的心理社会风险描述; 2.使用潜在剖面分析(LPA);识别心理社会风险剖面并考查儿童和伤害相关因素如何影响剖面所属。
方法:以色列一家儿科康复科收治的 374 名 PTME 患儿的照顾者完成了 PAT2.0。 PAT2.0 总分和 7 个 PAT2.0 分量表(家庭结构/资源、社会支持、儿童问题、兄弟姐妹问题、家庭问题、照顾者应激反应和家庭信念)被纳入了首次分析中。计算了三个风险类别的PAT2.0 平均得分(通用、靶向、临床); LPA 允许横截面潜在变量混合模型识别群体内的异质性,并使用七个 PAT2.0 分量表中的六个进行多项逻辑回归,用于确定不同剖面差异和剖面所属的预测因素。
结果:与具有其他临床诊断的儿童家庭的水平相比,显示的三层风险水平相对较高。 LPA 产生了一个三剖面的结果:低家庭风险(63.53%);照顾者高应激、平均水平以上家庭风险(22.5%);和有兄弟姐妹问题、平均水平以上家庭风险(13.94%)。种族和伤害类型预测了组别所属。
结论:PTME后儿童家庭的社会心理风险增加。基于 PAT2.0 分量表,识别和预防 PTSS 的临床有用方法可能是评估特定领域模式,而不仅仅是单独的总 PAT2.0 风险水平。
1. Introduction
Pediatric injuries and illnesses have a significant impact on children, adolescents, and families worldwide (Kullgren & Carter, Citation2020). In Israel, approximately 200,000 children visit emergency rooms annually (Nir et al., Citation2017), with 20,600 children hospitalised as a consequence of unintentional injury. These injuries/illnesses are often associated with prolonged hospitalisation, impaired physical functioning, and significant psychosocial distress for both child and family (McCarthy, Hearps, et al., Citation2016). In some cases, children and youth following pediatric traumatic medical events (PTMEs) are admitted to a pediatric rehabilitation centre to further assist recovery (Jones et al., Citation2018). Given the high levels of emotional distress, providers and families in pediatric healthcare settings can benefit from trauma-informed care which may help prevent or reduce the risk of further traumatic responses (Marsac et al., Citation2016). Pediatric care has increasingly promoted in recent years family-centred approaches that highlight the importance of the family for the child’s health and well-being by routinely assessing the family and providing family-level support so that all members are met in terms of their needs (Christofferson et al., Citation2020).
Studies conducted among various pediatric populations have identified a variety of negative effects experienced by families and children following PTMEs (Price et al., Citation2015). Such effects include increased financial burden on the family, lack of social support, parents’ mental-health problems, reduced family relationship quality, and reduced sibling well-being (Kazak, Schneider, et al., Citation2015). Furthermore, these effects may increase the risk of pediatric medical traumatic stress (PMTS). Symptoms of PMTS include hyperarousal, avoidance, and re-experiencing events that occurred as a result of a serious disease or medical intervention that threatened the child's health and entailed intrusive, painful, and frightening medical care for the child (National Child Traumatic Stress Network, Citation2020).
Previous studies conducted in pediatric rehabilitation settings have indicated that approximately 20% of mothers report significant emotional distress (Silberg et al., Citation2016). Additionally, 21% of mothers and 27% of children following PTMEs have self-reported significant levels of PMTS (Sadeh et al., Citation2020), interacting with other psychosocial risk factors, which may in turn increase child's risk of developing PTSS (Sadeh et al., Citation2020).
2. The pediatric psychosocial preventative health model (PPPHM)
Screening families for psychosocial risk and stress symptoms is considered a necessary factor for the development of early and effective prevention programmes (Kazak, Abrams, et al., Citation2015). The Pediatric Psychosocial Preventative Health Model (PPPHM) outlines three dimensions meant to distinguish between degrees of risk for maladaptation associated with pediatric medical conditions (Kazak, Schneider, et al., Citation2015). This model suggests that screening should involve all families entering the pediatric healthcare system, not just those thought to be at elevated risk.
Based on the PPPHM, the Psychosocial Assessment Tool 2.0 (PAT2.0) was developed (Pai et al., Citation2008). The PAT2.0 is a family-centred screening tool used to measure psychosocial risk in pediatric settings; has been widely used in the US (Kazak et al., Citation2019), Australia (McCarthy, Hearps, et al., Citation2016), Canada (Barrera et al., Citation2014), and the Netherlands (Sint Nicolaas et al., Citation2016); and is suitable for families from different races, ethnicities, and socioeconomic status (SES) (Kazak et al., Citation2018). It assesses seven dimensions affecting a family’s functioning and health, such as problems among multiple family members or difficulties in social domains (Pai et al., Citation2008), as well as a total psychosocial risk score. The total score is a sum of the subscales, with three tiers of risk – universal, targeted, and clinical. Universal risk forms the bottom tier and represents the largest group of families (50–60%); this group has the lowest psychosocial risk and most favourable outcome and ability to adjust to the child’s health condition. Targeted risk forms the middle tier and represents approximately 25–33% of families; this group has identifiable challenges and psychosocial risks. At the top of the pyramid are families at clinical risk; this group comprises the smallest group (≤ 15%), has more serious or chronic psychosocial challenges, and consists of families with increased risk for severe or escalating difficulties. To the best of our knowledge, a systematic screening for psychosocial risk in families in Israel and more specifically in families whose child has been admitted to pediatric rehabilitation following PTMEs has not been conducted. Thus, the first aim of the current study was to describe levels of psychosocial risk among families of children following PTMEs admitted to pediatric rehabilitation, according to the PAT2.0 three-tiered model of risk (i.e. universal, targeted, clinical).
Studies have found that PAT2.0 screening increases the amount of care provided and that such care is in line with the PPPHM tiers both in the US (Kazak et al., Citation2011) and the Netherlands (Schepers et al., Citation2017). However, McCarthy, Wakefield, et al. (Citation2016) found that PAT2.0 screening does not necessarily lead to services that match families’ needs, and other recent studies have indicated that categorisation into three risk groups may not accurately demonstrate the full extent of heterogeneity of within-group problems experienced in particular domains (e.g. child or siblings problems, financial burden, emotional distress) (Muscara et al., Citation2017; Sharkey et al., Citation2020). Thus, although the PAT2.0 is a multi-dimensional screener with the potential of providing more information about various domains of psychosocial risk, existing studies examining psychosocial risk in pediatric populations have predominantly used a cumulative frequency score (i.e. summing the subscale scores to create a total PAT2.0 score with the three-tiered model of risk) (Kazak et al., Citation2018) potentially limiting the multidimensional, qualitative-based conceptualisation of family psychosocial risk (Spurk et al., Citation2020).
Thus, it is often not clear what drives overall risk; diverse symptomatic manifestation may not be captured; and substantial information may be lost (Kotov et al., Citation2017). Using an approach that allows the study of relationships among individual difficulties and family factors, and illustrates the dynamic nature of the interaction between components, can be useful for improving our understanding of the characteristics of the problems and the domains central to the development of psychosocial difficulties (Colliva et al., Citation2020). For example, according to a recent study, epilepsy and asthma both have the same overall PAT score, but different domains have different interrelationships with each other that influence the risk for other domains (Colliva et al., Citation2020).
Our second aim was to identify latent patterns of psychosocial risk experienced by families of children in pediatric rehabilitation following PTMEs, by examining associations across the different PAT2.0 sub-domains. An increasingly accepted method for studying complex multidimensional phenomena, such as family psychosocial risk, is latent profile analysis (LPA). LPA is a cross-sectional latent variable mixture modelling approach which aims to find heterogeneity within a given population (Petersen et al., Citation2019). The LPA approach uses multiple aspects of individual/family functioning that can be studied holistically by finding common types, called profiles (Petersen et al., Citation2019). Each individual/family is probabilistically assigned to a specific profile, according to both level of similarity to other members in the profile and level of dissimilarity from those in other profiles.
Therefore, to better understand the psychosocial context surrounding children, we conceptualised psychosocial risk as a set of interdependent domains and explored the hypothesis that different profiles of needs and risks are associated with different demographic and illness factors. Examining the factors that may be universally related to adjustment outcomes and those that may be culture- or diagnosis-dependent could enhance our understanding of specific risk and protective factors following PTMEs (Sharkey et al., Citation2020). Studies have indicated that due to social structures that drive oppression and racism, ethnic minorities such as the Israeli-Arab population, may have an increased risk of developing PTSS following PTMEs (Hussien et al., Citation2021; Randall, Citation1996). These may be related to disparities in access to economic and social resources, perceptions of discrimination, or due to culturally-specific attitudes and beliefs that mediate coping with a traumatic event (Wolmer et al., Citation2014).
Furthermore, due to the relatively wide range of medical conditions and etiologies among children admitted to pediatric rehabilitation, recovery pathways also differ widely (Kullgren & Carter, Citation2020). Child’s gender and age at time of PTME may also contribute to family’s psychosocial risk (Price et al., Citation2015). Research shows that parents of female-gender and younger-aged children are more likely to be at risk for parental PTSS following various types of trauma (Cox et al., Citation2008) and following accidental trauma specifically (Trickey et al., Citation2012). Thus, examining specific profile predictors, such as ethnicity, etiology, illness/injury phase, age, and gender as predictors of profile membership could be particularly important for the development of person- and family-centred interventions.
3. The current study
Our first aim was to categorise psychosocial risk based on the classification of the overall PAT2.0 total risk score into the previously established three levels of risk (i.e. universal, targeted, clinical). We hypothesised that due to the unique circumstances (prolonged rehabilitation, possible chronicity of the child’s healthcare needs, and long-term implications for child and family) of families and children admitted to pediatric rehabilitation following PTMEs, the distribution of PAT2.0 scores would lean toward the increased risk categories (i.e. targeted and clinical) as compared to those reported in the literature (Kazak et al., Citation2018). Our second aim was to identify latent profiles of psychosocial risk using LPA, based on the six sub-domains measured by the PAT2.0. The literature suggests that various factors may be associated with PTSS risk (Marsac et al., Citation2014); however to the best of our knowledge, only one study employed latent analysis using PAT2.0 subscales (Sharkey et al., Citation2020). Thus, the current study used exploratory analysis to reveal specific psychosocial risk profiles associated with PTSS risk, above the PAT2.0 general risk categories. We expected to observe several distinct latent risk profiles, with related elevations in different domains. Lastly, as LPA has the potential to develop and expand theoretical thinking regarding the existence of different configurations of profiles in variables relevant to health and children, including their predictors (Spurk et al., Citation2020), our third aim was to examine, in an exploratory fashion, whether the following – ethnicity, type of etiology, illness/injury phase, child's age, gender – were sensitive predictors of risk profiles.
4. Methods
4.1. Participants
We used a cross-sectional retrospective design extracted from the medical records of 374 children (221 males), 0–18 years of age (M = 9.11, SD = 5.42), who were admitted to a pediatric rehabilitation department between 2011 and 2019 (see for a detailed description of the demographic and injury/illness characteristics of study participants).
Table 1. Demographics and injury/illness characteristics.
Inclusion criteria were: (1) child hospitalised in the pediatric rehabilitation department between 2011 and 2019, (2) parents’ agreement to complete the department’s screening procedure, and (3) sufficient mastery of the native language to complete the questionnaires. Potential participants were excluded if their injuries were due to family violence or suspected child abuse.
Among the 537 children who were eligible to be included in the analyses, N = 120 families declined to participate, and N = 43 families could not complete the questionnaires due to lack of sufficient proficiency in their native language. Between those who provided data to be included in the analyses, M(374) = 9.11, SD = 5.42, and those who did not provide such data, M(163) = 9.02 SD = 11.11, there were no significant differences in child’s age, t(496) = 1.535, p = .25, gender, χ2(1) = 2.689, p = .12, or etiology type χ2(42) = 49.47, p = .20.
4.2. Procedure
As part of the pediatric rehabilitation department’s admissions process, each family was asked by their psychologist/social worker to complete the questionnaires regarding their current situation in order to screen for the family’s psychosocial factors. All study procedures were approved by the Institutional Review Board at The Sheba Medical Center.
4.3. Measures
Child- and injury-related factors were abstracted from electronic health records, including ethnicity categories, type of etiology, illness/injury phase, age, and gender.
4.3.1. Psychosocial assessment tool 2.0
The PAT2.0 (Pai et al., Citation2008) comprises seven subscales including family structure and resources (8 items; e.g. financial difficulties); social support (4 items; e.g. provision of emotional/financial support); child problems (16 items; e.g. being distracted); sibling problems (16 items; e.g. school or learning difficulties); family problems (15 items; e.g. marital difficulties, separation); parent stress reactions (3 items; e.g. arousal and avoidance); and family beliefs (10 items; e.g. the ability to make good treatment decisions). The seven subscales are calculated by dividing the number of item responses indicative of risk by the total number of items in the respective domain, yielding a subscale score ranging from 0.0–1.0, with higher scores indicating higher psychosocial risk, for each subscale. Total score is a sum of 7 subscales (each subscale is a sum of endorsed risk items on that subscale) from 0 to 7, mapping onto the three tiers of the PPPHM (Kazak, Citation2006). In a study by Kazak et al. (Citation2018) the PAT2.0 subscales showed good internal consistency using the Kuder–Richardson 20 coefficient (child problems were KR20 > 0.80, and family structure/resources, social support, and family problems were adequate, ranging from 0.59 to 0.64). The PAT2.0 has shown excellent convergent validity in a range of pediatric conditions (Guerra-Peña & Steinley, Citation2016; McCarthy, Hearps, et al., Citation2016; Sint Nicolaas et al., Citation2016). In this study, internal reliability was good for the PAT2.0 total score (α = 0.703). The PAT2.0 questionnaire has been translated into 13 languages, including Hebrew: the version that was used in this study.
4.4. Statistical analysis
An initial descriptive analysis was conducted, and mean scores for those who provided data were compared with those who did not (using Pearson correlations and chi-square). According to our first goal, we calculated the prevalence of psychosocial risk for every PAT2.0 risk category (universal, targeted, clinical) as a percentage of all participating families (). A one-sample t-test was conducted to compare our mean level with those of other samples that also measured psychosocial risk among caregivers of specific pediatric populations using the total PAT2.0 score. Furthermore, descriptive analyses identified unacceptable skewness due to floor effect (3.56; >2) in the social support domain across the entire sample, resulting in the removal of the social support domain from our second analysis. LPA studies have shown that a great challenge is identifying the true or meaningful profiles rather than the ‘spurious’ profiles (Spurk et al., Citation2020). One of the reasons for detecting spurious profiles in LPA can be caused by non-normally distributed data (skewed data) (Spurk et al., Citation2020) related to a floor/ceiling effect. When data is non-normally distributed, fit indices tend to favour models with more latent profiles than those used to simulate them, potentially creating spurious profiles in LPA (Guerra-Peña & Steinley, Citation2016). As a solution to this problem, formulating a preliminary test that takes account of higher-order moments (e.g. skewness and krtosis) of the observed data is recommended (Muthén, Citation2003), as was done in this study.
Table 2. Descriptive statistics of the PAT2.0Table Footnotea.
To achieve our second aim, we used Mplus version 7.4 to conduct LPA based on the observed response patterns across the remaining six domains of PAT2.0. To interpret which indicators are above and below the sample means clearly, we used the z-standardized mean scale scores. Five sequential latent profile models were identified. Relative model fit and accuracy of classification were examined using three fit statistics (Nylund et al., Citation2007; van de Schoot et al., Citation2017): (1) The Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC), with lower AIC and BIC values indicating better fit; (2) The Vuong-Lo-Mendell-Rubin (VLMR) Adjusted Likelihood Ratio Test, and the Lo-Mendell-Rubin Adjusted Likelihood Ratio Test (LMR) where P-values <.05 were assumed to indicate that the larger profile solution was a better model fit; and (3) Entropy values closer to 1 indicating better class separation and values, with .80 being considered acceptable.
After identifying the optimal latent profile solution, the three-step approach was conducted to test our third aim: demographic- and event-related predictors associated with membership in the profiles (Asparouhov & Muthén, Citation2014). This approach employed a classification-error corrected multinomial logistic regression to test differences between classes in demographic variables; child’s gender (1 = boys, 2 = girls), age (in years), ethnicity (1 = Jewish, 2 = Arab), illness etiology (i.e. acquired brain injury/ABI, spinal cord, orthopedic, other) and illness/injury phase. Information about the illness/injury phase was grouped into two categories based on previous research (Marsac et al., Citation2014; Rolland, Citation2005). The first category concerned the crisis phase (i.e. one-month post-illness/injury); the second category comprised the chronic or adaptation phase (i.e. families within the first year up to 4 years after the initial illness/injury phase).
5. Results
5.1. Bivariate analyses
5.1.1. Levels of PAT2.0 total score and PAT2.0 sub-domains in the sample
The whole sample had a mean PAT2.0 total score of 1.17 (SD = 0.77; i.e. targeted risk). Domain mean scores ranged from 0.00 to 1.00, with the highest risk level in the family beliefs domain. Descriptive statistics for the PAT2.0 domain scores are presented in . Out of the 374 families, 46.5% (n = 174; M = 0.53; 95% CI [0.49, 0.57]) corresponded with the universal risk category; 39% (n = 146; M = 1.42; 95% CI [1.37, 1.47]) with the targeted risk category; and 14.4% (n = 54; M = 2.58; 95% CI [2.46, 2.72]) with the clinical risk category. A one-sample t-test comparing PAT2.0 scores in our sample (M = 1.177, SD = 0.771) with previous studies revealed that our sample had significantly higher levels of psychosocial risk compared to specific clinical pediatric samples, such as pediatric cystic fibrosis (M = 1.00, SD = 0.77, N = 374) (Filigno et al., Citation2019) or pediatric cancer (M = 1.021, SD = 0.700, N = 396) (Kazak et al., Citation2020). However, the total risk score in our sample was relatively similar to that of children with medical complexities (CMC) (M = 1.170, SD = 0.740, N = 136) (Verma et al., Citation2020).
5.1.2. Latent profile analysis
Overall, based on fit statistics and parsimony of the class solution, a three-profile LPA model of psychosocial risk profiles provided the most theoretically interpretable and adequate fit to the data ( shows the fit indices for the latent profile models, one to five profiles). According to the VLMR and LMR, the two-profile and three-profile solution had an optimal fit to the data and meaningful profile sizes. All entropy values were acceptable, with the two- and five-profile models having the highest values. However, in the five-profile solution, the sample sizes of some of the profiles were too small (<1%), and the LMR value was non-significant.
Table 3. Fit statistics for PAT2.0 domains latent profile analysis.
Additionally, although the four- and five-profiles had decreasing AIC and BIC values suggesting solutions with more profiles, the LMR and VLMR indicated that the improvement compared to the three- and four-profile (accordingly) was not statistically significant. Between the two-and-three-profiles, the three-profile solution was selected as the best fitting model as it had the lower BIC and AIC for the three-class solution compared to the two-class solution, which is considered the preferred fit index to rely on according to an expert panel (van de Schoot et al., Citation2017).
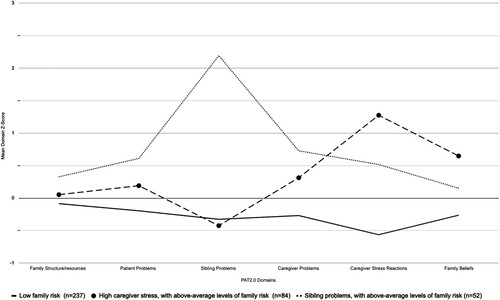
The largest latent profile, labelled low family risk (n = 238, 63.53%), showed low average risk across all domains of PAT2.0 (Bs < −0.085). A smaller latent profile, labelled high caregiver stress, with above-average levels of family risk (n = 84, 22.5%), demonstrated moderate risk, above-average, across all psychosocial domains (Bs > 0.10), with particularly high risk, on average, in the caregiver stress reaction domain, B = 1.275, 95% CI [1.16, 1.39], and family belief domain, B = 0.648, 95% CI [0.53, 0.76]. The third profile, labelled sibling problems, with above-average levels of family risk (n = 52, 13.94%), demonstrated elevated risk, on average, across all psychosocial domains (Bs > 0.152) with particularly high risk, on average, in the sibling problems domain, B = 2.193, 95% CI [2.074, 2.312]. See for a graphical representation of group risk across domains.
5.1.3. Predictors of profile membership
In , comparisons between classes in terms of demographic- and illness-related variables are summarised. Predictors of profile membership were examined via the three-step approach procedure (Asparouhov & Muthén, Citation2014). Correlates of profile membership included in the analysis comprised gender (1 = boys, 2 = girls), child’s age (0–18), ethnicity (1 = Israeli-Jewish, 2 = Israeli-Arab), illness/injury etiology (i.e. ABI, spinal cord, orthopedic, other), and illness/injury phase (i.e. crisis or chronic/adaptation). Ethnicity predicted membership in the sibling problems, above-average levels of family risk (profile 3), with Israeli-Arab ethnicity (vs. Israeli-Jewish ethnicity) related to the likelihood of being a member of the sibling problems, above-average levels of family risk (profile 3), compared to the low family risk (profile 1). Ethnicity did not predict membership in any other group, relative to the high caregiver stress, above-average levels of family risk (profile 2), or low family risk (profile 1).
Table 4. Univariate associations with class membership.
Etiology predicted membership in the high caregiver stress, above-average levels of family risk (profile 2), with ABI associated with higher odds of being in the high caregiver stress, above-average levels of family risk (profile 2), compared to the sibling problems, above-average levels of family risk (profile 3). Other etiologies did not predict membership in any other group, relative to sibling problems, above-average levels of family risk (profile 3), or high caregiver stress, above-average levels of family risk (profile 2). Child’s age, gender or illness/injury phase did not predict group membership relative to sibling problems, above-average levels of family risk (profile 3), or high caregiver stress, above-average levels of family risk (profile 2).
6. Discussion
The present study aimed to assess psychosocial risk and identify unique risk and protective factors of families admitted to pediatric rehabilitation following PTMEs. Our findings show that families of children in pediatric rehabilitation are prone to significant psychosocial risk, demonstrated by an average PAT2.0 score of 1.17 and a distribution of PAT2.0 scores of 46.5% universal vs. 39% targeted and 14.4% clinical. Previous research shows that, in generally, two-thirds of families in multiple samples fall within the universal range, about one-third fall within the targeted range, and 11% or less fall within the clinical range (Kazak et al., Citation2015; Law et al., Citation2019). Results suggest that there was a higher proportion of families in the targeted (39%) and clinical (14.4%) ranges in our sample compared to samples in previous studies (Filigno et al., Citation2019; Kazak et al., Citation2020). This difference can be attributed to the relatively high heterogeneity of etiologies in our sample, as compared to those found in more homogeneous samples (Filigno et al., Citation2019; Kazak et al., Citation2020). Furthermore, our results are in accordance with a recent study (Verma et al., Citation2020) among families of children with medical complexities (CMC). In the CMC sample, similar frequencies of families in the higher-risk categories (45% universal vs. 44% targeted and 11% clinical) were found. The authors suggested that the high proportion could have been attributable to the intense stressors among the CMC population, including prolonged hospitalisation, uncertainty of life expectancy, and time spent by caregivers advocating for resources (Verma et al., Citation2020). These stressors are also common among families with children hospitalised in pediatric rehabilitation departments post-TME and may partly explain the presence of high-risk families in our sample (Kaufman & Lahey, Citation2020). Other studies that found similar frequencies of families in the higher-risk categories suggest that socioeconomic considerations in these samples are important to recognise (Kazak et al., Citation2018; Reader et al., Citation2020). Specifically in terms of pediatric rehabilitation, these findings reinforce the need to examine the unique risk profiles that characterise families following PTMEs via the use of a complementary profile analysis method, such as LPA.
Our second aim was to identify latent profiles of psychosocial risk using LPA, based on the sub-domains measured by the PAT2.0. LPA resulted in a three-profile solution. Low family risk (profile 1) (63.53%) was defined by generally low levels of risk across all PAT2.0 domains. High caregiver stress, above-average levels of family risk (profile 2) (22.5%), showed a high probability of caregiver’s stress reactions – which diverged substantially from the third group (12.7%, 5.17%, respectively) – and negative family beliefs (6.48%, 1.5%, respectively). Sibling problems, above-average levels of family risk (profile 3) (13.94%), depicted an overall high probability of reports of all domains with a characterising feature of sibling problems. This tendency toward divergence might support a multidimensional, qualitative-based conceptualisation of psychosocial risk patterns among families of children admitted to pediatric settings (Spurk et al., Citation2020).
Parents’ stress reactions post-PTME and parents’ beliefs (also known as cognitive appraisals/perceptions) regarding their child’s recovery are known to be interrelated (Schilpzand et al., Citation2018). Parents who are more symptomatic and overwhelmed tend to perceive their child’s PTME as more severe and/or as posing significant limitations on the child’s and family’s current and future functioning (Salvador et al., Citation2015). Compared to other psychosocial risk domains, both factors (i.e. parental stress and parental beliefs) are seen to be more event-related appraisals. As such, examining demographic and PTME variables that might predict membership in the high caregiver stress, above-average levels of family risk (profile 2), could further enhance our understanding of this group’s specific risk factors.
Sibling problems, above-average levels of family risk (profile 3) (13.94%), was differentiated by relatively high levels of risk in four out of six PAT2.0 domains (i.e. family’s structure/resources, parental problems, and child’s problems), with a specific increased risk pattern defined by an elevated score in the sibling problems domain. Our findings bolster findings from previous studies indicating that siblings’ distress may have an adverse impact on the whole family (Gill, Citation2020). Research in the field suggests that siblings’ emotional challenges might contribute to increased family stress and conflict (Velleman et al., Citation2016). When their unique needs are not adequately addressed, siblings may be at risk for adverse developmental and psychological outcomes (Gill, Citation2020), contributing to the elevated risk among families in the sibling problems, above-average levels of family risk.
Sharkey et al. (Citation2020) suggested that families in any of the three risk groups could experience an escalation of risk due to the change in one domain and the established links between the different domains. For example, research shows that siblings who receive emotional and social support display improved behaviour, emotional well-being, and illness knowledge, resulting in better family functioning and greater patient and family satisfaction (Besier et al., Citation2010). These results align with research in the pediatric field that emphasises the importance of evaluating the relationship between risk factors in various domains of the family in order to target specific sources of psychosocial risk (Christofferson et al., Citation2020; Muscara et al., Citation2017; Sadeh et al., Citation2020; Sharkey et al., Citation2020). Incorporating trauma-informed and family-centred care requires recognition that these events can be traumatic for all members of the family (Christofferson et al., Citation2020).
As for our third aim, several characteristics were identified as predictors of group membership. The present findings indicate that families affected by PTMEs experience different cross-cultural patterns of psychosocial risk. Israeli-Arab ethnicity (vs. Israeli-Jewish ethnicity) was related to elevated risk of being a member of sibling problems, above-average levels of family risk (profile 3) – compared to low family risk (profile 1) – which was characterised by relatively high levels of risk in four out of six domains. These findings may be understood in light of previous findings indicating that Israeli-Arab citizens often have lower SES, and that schools have lower budgets and fewer available resources (Hobfoll et al., Citation2007). When further resources are threatened, minority groups who are already discriminated against might be exposed to an increased risk for psychological distress. In addition, perceived discrimination may prevent individuals from seeking support and using social resources that are perceived to be available only to the majority group (Wolmer et al., Citation2014). Acknowledging the health disparities faced by ethnicity groups worldwide (Kazak et al., Citation2020) and in Israel in particular (Hussien et al., Citation2021) is in line with the recent Sustainable Development Goals identified by the United Nations for a better future for all (Daelmans et al., Citation2017). Health services tailored to cultural values and needs may help bridge the gap between families and the pediatric healthcare system (Williams et al., Citation2014).
Among the other risk factors, etiology predicted membership in high caregiver stress, above-average levels of family risk (profile 2), with ABI being associated with higher odds of being in that group compared to sibling problems, above-average levels of family risk (profile 3). High caregiver stress, above-average levels of family risk (profile 2), was characterised by high levels of caregiver stress reactions and negative family beliefs. In our sample, a relatively high percentage of children were diagnosed with an ABI (56.7%). Thus, our findings may be understood in light of the wide range of cognitive and neuro-behavioural impairments associated with ABIs (Renaud et al., Citation2020), which may add additional burden compared to other etiologies (Brown et al., Citation2013).
The current study had several limitations. The first limitation of this study was that no follow-up or comparison data were collected, which made it impossible to determine whether the risk profiles presently identified are associated with later psychosocial distress. Second, because of the removal of social support from all analyses due to high levels of skewness, the relationship between social support difficulties and risk was not established. We suggest that future studies should examine confirmatory factor analysis in a larger sample to determine whether all subscales represent themselves as theoretically hypothesised (Sint Nicolaas et al., Citation2016). Furthermore, due to the important impact of sibling’s and parent’s distress on the entire family, additional information regarding the family (e.g. how many of the families included siblings, history of prior traumatic experiences, whether more than one family member have been injured, whether the caregiver witnessed or been part of the accident) is needed.
Clinical implications
The current study provides greater information on the applicability of the PAT2.0 and its use across different cultures and within various medical settings. This study is aligned with global collaboration aims for traumatic stress (Olff et al., Citation2020) supporting the global effort to evaluate cross-cultural differences in trauma-related outcomes. By examining family’s psychosocial risk as a multidimensional phenomenon, with unique and qualitatively differentiated profiles, our findings have important implications regarding enhancing the need for tailored assessments and interventions for children and families post-TMEs. For example, our second profile suggests that families who display more difficulties regarding stress reactions also display difficulties in their personal beliefs about their child’s TMEs, with ABIs being associated with higher odds of being in that group. These families may face many difficulties due to their embedded emotional reactions following the diagnosis of their child; therefore, interventions in support of resolution (i.e. coming to terms) with a child’s diagnosis could be a central aspect of parenting such children. Parents having unresolved concerns related with grief or despair may continue to be overwhelmed or show displaced anger, potentially putting these families at an even higher risk over the years (Yehene et al., Citation2021).
Together with other more traditional approaches, LPA may provide a new approach for exploring and understanding the impact of pediatric severe and chronic conditions on the needs of families (Colliva et al., Citation2020). In light of these findings, we should try to develop and implement interventions that directly target the most significant domains, while expecting improvements in the other domains as well. Additionally, the current findings point to the importance of family-centred and trauma-informed design and delivery of pediatric care. It is essential for providers to understand and identify the impact of trauma symptoms on child, parents, and siblings (Christofferson et al., Citation2020).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Due to the nature of this research, participants of this study did not agree to have their data shared publicly; supporting data are therefore not available.
References
- Asparouhov, T., & Muthén, B. (2014). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 329–341. https://doi.org/10.1080/10705511.2014.915181
- Barrera, M., Hancock, K., Rokeach, A., Cataudella, D., Atenafu, E., Johnston, D., Punnett, A., Nathan, P. C., Bartels, U., Silva, M., Cassidy, M., Jansen, P., Shama, W., & Greenberg, C. (2014). External validity and reliability of the psychosocial assessment tool (PAT) among Canadian parents of children newly diagnosed with cancer. Pediatric Blood & Cancer, 61(1), 165–170. https://doi.org/10.1002/pbc.24774
- Besier, T., Hölling, H., Schlack, R., West, C., & Goldbeck, L. (2010). Impact of a family-oriented rehabilitation programme on behavioural and emotional problems in healthy siblings of chronically ill children. Child: Care, Health and Development, 36(5), 686–695. https://doi.org/10.1111/j.1365-2214.2010.01085.x
- Brown, F. L., Whittingham, K., Sofronoff, K., & Boyd, R. N. (2013). Parenting a child with a traumatic brain injury: Experiences of parents and health professionals. Brain Injury, 27(13-14), 1570–1582. https://doi.org/10.3109/02699052.2013.841996
- Christofferson, J. L., Okonak, K., Kazak, A. E., Pierce, J., Kelly, C., Schifano, E., Sciolla, J., Deatrick, J. A., & Alderfer, M. A. (2020). Family consequences of potentially traumatic pediatric medical events: Implications for trauma-informed care. Journal of Family Psychology, 34(2), 237–246. https://doi.org/10.1037/fam0000597
- Colliva, C., Cellini, M., Dalla Porta, F., Ferrari, M., Bergamini, B. M., Guerra, A., Di Giuseppe, S., Pinto, A., Capasso, R., Caprino, D., Ferrari, M., Benatti, C., Tascedda, F., & Blom, J. M. C. (2020). Psychosocial assessment of families caring for a child with acute lymphoblastic leukemia, epilepsy or asthma: Psychosocial risk as network of interacting symptoms. PLoS One, 15(3), 1–27. https://doi.org/10.1371/journal.pone.0230194
- Cox, C. M., Kenardy, J. A., & Hendrikz, J. K. (2008). A meta-analysis of risk factors that predict psychopathology following accidental trauma. Journal for Specialists in Pediatric Nursing, 13(2), 98–110. https://doi.org/10.1111/j.1744-6155.2008.00141.x
- Daelmans, B., Darmstadt, G. L., Lombardi, J., Black, M. M., Britto, P. R., Lye, S., Dua, T., Bhutta, Z. A., & Richter, L. M. (2017). Early childhood development: The foundation of sustainable development. The Lancet, 389(10064), 9–11. https://doi.org/10.1016/S0140-6736(16)31659-2
- Filigno, S. S., Miller, J., Moore, S., Peugh, J., Weiland, J., Backstrom, J., & Borschuk, A. (2019). Assessing psychosocial risk in pediatric cystic fibrosis. Pediatric Pulmonology, 54(9), 1391–1397. https://doi.org/10.1002/ppul.24414
- Gill, M. A. (2020). Making space for siblings in family- centered care. Pediatric Nursing, 46(1), 48–51. https://search.proquest.com/scholarly-journals/making-space-siblings-family-centered-care/docview/2355333589/se-2?accountid=14483.
- Guerra-Peña, K., & Steinley, D. (2016). Extracting spurious latent classes in growth mixture modeling with nonnormal errors. Educational and Psychological Measurement, 76(6), 933–953. https://doi.org/10.1177/0013164416633735
- Hobfoll, S. E., Canetti-Nisim, D., Johnson, R. J., Palmieri, P. A., Varley, J. D., & Galea, S. (2007). The association of exposure, risk, and resiliency factors with PTSD among Jews and Arabs exposed to repeated acts of terrorism in Israel. Journal of Traumatic Stress, 20(3), 251–262. https://doi.org/10.1002/jts.20223
- Hussien, S., Sadeh, Y., Dekel, R., Shadmi, E., Brezner, A., Landa, J., & Silbreg, T. (2021). Using a biopsychosocial approach to examine differences in post-traumatic stress symptoms among Arab and Jewish Israeli mothers following a child’s traumatic medical event. International Journal for Equity in Health, 20(1), 1–12. https://doi.org/10.21203/rs.3.rs-134926/v1
- Jones, S., Davis, N., & Tyson, S. F. (2018). A scoping review of the needs of children and other family members after a child’s traumatic injury. Clinical Rehabilitation, 32(4), 501–511. https://doi.org/10.1177/0269215517736672
- Kaufman, J. N., & Lahey, S. (2020). Pediatric rehabilitation psychology. In M. C. Roberts (Eds.), Clinical handbook of psychological consultation in pediatric medical settings (pp. 251–262). Springer.
- Kazak, A. E. (2006). Pediatric psychosocial preventative health model (PPPHM): research, practice, and collaboration in pediatric family systems medicine. Families, Systems, & Health, 24(4), 381–395. https://doi.org/10.1037/1091-7527.24.4.381
- Kazak, A. E., Abrams, A. N., Banks, J., Christofferson, J., DiDonato, S., Grootenhuis, M. A., Kabour, M., Madan-Swain, A., Patel, S. K., Zadeh, S., & Kupst, M. J. (2015a). Psychosocial assessment as a standard of care in pediatric cancer. Pediatric Blood & Cancer, 62(5), s426–s459. https://doi.org/10.1002/pbc.25730
- Kazak, A. E., Barakat, L. P., Hwang, W. T., Ditaranto, S., Biros, D., Beele, D., Kersun, L., Hocking, M. C., & Reilly, A. (2011). Association of psychosocial risk screening in pediatric cancer with psychosocial services provided. Psycho-oncology, 20(7), 715–723. https://doi.org/10.1002/pon.1972
- Kazak, A. E., Chen, F. F., Hwang, W.-T., Askins, M. A., Vega, G., Kolb, E. A., Reilly, A., & Barakat, L. P. (2020a). Stability and change in family psychosocial risk over 6 months in pediatric cancer and its association with medical and psychosocial healthcare utilization. Pediatric Blood & Cancer, 67(2), 4–11. https://doi.org/10.1002/pbc.28051
- Kazak, A. E., Christofferson, J., Richards, H. G., Rivero-Conil, S., & Sandler, E. (2019). Implementing screening with the psychosocial assessment tool (PAT) in clinical oncology practice. Clinical Practice in Pediatric Psychology, 7(2), 140–150. https://doi.org/10.1037/cpp0000246
- Kazak, A. E., Deatrick, J. A., Scialla, M. A., Sandler, E., Madden, R. E., & Barakat, L. P. (2020b). Implementation of family psychosocial risk assessment in pediatric cancer with the psychosocial assessment tool (PAT): study protocol for a cluster-randomized comparative effectiveness trial. Implementation Science, 15(1), 1–13. https://doi.org/10.1186/s13012-020-01023-w
- Kazak, A. E., Hwang, W.-T., Chen, F. F., Askins, M. A., Carlson, O., Argueta-Ortiz, F., & Barakat, L. P. (2018a). Screening for family psychosocial risk in pediatric cancer: Validation of the psychosocial assessment tool (PAT) version 3. Journal of Pediatric Psychology, 43(7), 737–748. https://doi.org/10.1093/jpepsy/jsy012
- Kazak, A. E., Hwang, W.-T., Chen, F. F., Askins, M. A., Carlson, O., Argueta-Ortiz, F., Vega, G., & Barakat, L. P. (2018b). Validation of the Spanish version of the psychosocial assessment tool (PAT) in pediatric cancer. Journal of Pediatric Psychology, 43(10), 1104–1113. https://doi.org/10.1093/jpepsy/jsy046
- Kazak, A. E., Schneider, S., Didonato, S., & Pai, A. L. H. (2015b). Family psychosocial risk screening guided by the pediatric psychosocial preventative health model (PPPHM) using the psychosocial assessment tool (PAT). Acta Oncologica, 54(5), 574–580. https://doi.org/10.3109/0284186X.2014.995774
- Kotov, R., Krueger, R. F., Watson, D., Achenbach, T. M., Althoff, R. R., Bagby, R. M., Brown, T. A., Carpenter, W. T., Caspi, A., Clark, L. A., Eaton, N. R., Forbes, M. K., Forbush, K. T., Goldberg, D., Hasin, D., Hyman, S. E., Ivanova, M. Y., Lynam, D. R., Markon, K., … Zimmerman, M. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. https://doi.org/10.1037/abn0000258
- Kullgren, K. A., & Carter, B. D. (2020). Introduction to the clinical handbook of psychological consultation in pediatric medical settings. In B. D. Carter & K. A. Kullgren (Eds.), Clinical Handbook of Psychological Consultation in Pediatric Medical Settings (pp. 3–9). Springer. https://doi.org/10.1007/978-3-030-35598-2_1
- Law, E. F., Powers, S. W., Blume, H., & Palermo, T. M. (2019). Screening family and psychosocial risk in pediatric migraine and tension-type headache: Validation of the psychosocial assessment tool (PAT). Headache: The Journal of Head and Face Pain, 59(9), 1516–1529. https://doi.org/10.1111/head.13599
- Marsac, M. L., Kassam-Adams, N., Delahanty, D. L., Widaman, K. F., & Barakat, L. P. (2014). Posttraumatic stress following acute medical trauma in children: A proposed model of bio-psycho-social processes during the peri-trauma period. Clinical Child and Family Psychology Review, 17(4), 399–411. https://doi.org/10.1007/s10567-014-0174-2
- Marsac, M. L., Kassam-Adams, N., Hildenbrand, A. K., Nicholls, E., Winston, F. K., Leff, S. S., & Fein, J. (2016). Implementing a trauma-informed approach in pediatric health care networks. JAMA Pediatrics, 170(1), 70–77. https://doi.org/10.1001/jamapediatrics.2015.2206
- McCarthy, M. C., Hearps, S. J. C., Muscara, F., Anderson, V. A., Burke, K., Hearps, S. J., & Kazak, A. E. (2016a). Family psychosocial risk screening in infants and older children in the acute pediatric hospital setting using the psychosocial assessment tool. Journal of Pediatric Psychology, 41(7), 820–829. https://doi.org/10.1093/jpepsy/jsw055
- McCarthy, M. C., Wakefield, C. E., DeGraves, S., Bowden, M., Eyles, D., & Williams, L. K. (2016). Feasibility of clinical psychosocial screening in pediatric oncology: Implementing the PAT2.0. Journal of Psychosocial Oncology, 34(5), 363–375. https://doi.org/10.1080/07347332.2016.1210273
- Muscara, F., McCarthy, M. C., Thompson, E. J., Heaney, C.-M., Hearps, S. J. C., Rayner, M., Burke, K., Nicholson, J. M., & Anderson, V. A. (2017). Psychosocial, demographic, and illness-related factors associated with acute traumatic stress responses in parents of children with a serious illness or injury. Journal of Traumatic Stress, 30(3), 237–244. https://doi.org/10.1002/jts.22193
- Muthén, B. (2003). Statistical and substantive checking in growth mixture modeling: Comment on Bauer and Curran (2003). Psychological Methods, 8(3), 369–377. https://doi.org/10.1037/1082-989X.8.3.369
- National Child Traumatic Stress Network. (2020). Medical trauma. https://www.nctsn.org/what-is-child-trauma/tra uma-types/medical-trauma
- Nir, N., Ophir, Y., Weiss, O., & Levi, S. (2017). Child Injuries in Israel: ‘Beterem’ National Report 2017 (Publication No. 1100). Petach Tikva: ‘Beterem’- Safe Kids Israel.
- Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. https://doi.org/10.1080/10705510701575396
- Olff, M., Bakker, A., Frewen, P., Aakvaag, H., Ajdukovic, D., Brewer, D., Elmore Borbon, D. L., Cloitre, M., Hyland, P., Kassam-Adams, N., & Knefel, M. (2020). Screening for consequences of trauma–an update on the global collaboration on traumatic stress. European Journal of Psychotraumatology, 11(1), 1752504.
- Pai, A. L. H., Patino-Fernandez, A., McSherry, M., Beele, D., Alderfer, M. A., Reilly, A. T., Hwang, W.-T., & Kazak, A. E. (2008). The psychosocial assessment tool (PAT 2.0): Psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. Journal of Pediatric Psychology, 33(1), 50–62. https://doi.org/10.1093/jpepsy/jsm053
- Petersen, K. J., Qualter, P., & Humphrey, N. (2019). The application of latent class analysis for investigating population child mental health: A systematic review. Frontiers in Psychology, 10(MAY), https://doi.org/10.3389/fpsyg.2019.01214
- Price, J., Kassam-Adams, N., Alderfer, M. a., Christofferson, J., & Kazak, A. E. (2015). Systematic review: A reevaluation and update of the integrative (trajectory) model of pediatric medical traumatic stress. Journal of Pediatric Psychology, 1–12. https://doi.org/10.1093/jpepsy/jsv074
- Randall, M. (1996). Children: Ethnic and political violence. Child Development, 67(1), 14–18. https://doi.org/10.7588/worllitetoda.89.5.0034
- Reader, S. K., Keeler, C. N., Chen, F. F., Ruppe, N. M., Rash-Ellis, D. L., Wadman, J. R., Miller, R. E., & Kazak, A. E. (2020). Psychosocial screening in sickle cell disease: Validation of the psychosocial assessment tool. Journal of Pediatric Psychology, 1–11. https://doi.org/10.1093/jpepsy/jsaa002
- Renaud, M. I., Lambregts, S. A. M., van de Port, I. G. L., Catsman-Berrevoets, C. E., & van Heugten, C. M. (2020). Predictors of activities and participation six months after mild traumatic brain injury in children and adolescents. European Journal of Paediatric Neurology, 25, 145–156. https://doi.org/10.1016/j.ejpn.2019.11.008
- Rolland, J. S. (2005). Cancer and the family: An integrative model. Cancer, 104(11 SUPPL.), 2584–2595. https://doi.org/10.1002/cncr.21489
- Sadeh, Y., Dekel, R., Brezner, A., Landa, J., & Silberg, T. (2020). Child and family factors associated with posttraumatic stress responses following a traumatic medical event: The role of medical team support. Journal of Pediatric Psychology, 45(9), 1063–1073. https://doi.org/10.1093/jpepsy/jsaa070
- Salvador, Á, Crespo, C., Martins, A. R., Santos, S., & Canavarro, M. C. (2015). Parents’ perceptions about their child’s illness in pediatric cancer: Links with caregiving burden and quality of life. Journal of Child and Family Studies, 24(4), 1129–1140. https://doi.org/10.1007/s10826-014-9921-8
- Schepers, S. A., Sint Nicolaas, S. M., Maurice-Stam, H., van Dijk-Lokkart, E. M., van den Bergh, E. M. M., de Boer, N., Verhaak, C. M., & Grootenhuis, M. A. (2017). First experience with electronic feedback of the psychosocial assessment tool in pediatric cancer care. Supportive Care in Cancer, 25(10), 3113–3121. https://doi.org/10.1007/s00520-017-3719-3
- Schilpzand, E. J., Conroy, R., Anderson, V., & Alisic, E. (2018). Development and evaluation of the thinking about recovery scale: Measure of parent posttraumatic cognitions following children’s exposure to trauma. Journal of Traumatic Stress, 31(1), 71–78. https://doi.org/10.1002/jts.22258
- Sharkey, C. M., Schepers, S. A., Drake, S., Pai, A. L. H., Mullins, L. L., & Grootenhuis, M. A. (2020). Psychosocial risk profiles among American and Dutch families affected by pediatric cancer. Journal of Pediatric Psychology, 45(4), 463–473. https://doi.org/10.1093/jpepsy/jsaa012
- Silberg, T., Brezner, A., Gal, G., Ahonniska-Assa, J., & Levav, M. (2016). The role of maternal distress in the report of behavioral and emotional problems among children with chronic disabilities. The Israel Journal of Psychiatry and Related Sciences, 53(2), 17–24. https://search.proquest.com/docview/1921108553?accountid=14483
- Sint Nicolaas, S. M., Schepers, S. A., Hoogerbrugge, P. M., Caron, H. N., Kaspers, G. J. L., van den Heuvel-Eibrink, M. M., Grootenhuis, M. A., & Verhaak, C. M. (2016). Screening for psychosocial risk in Dutch families of a child with cancer: Reliability, validity, and usability of the psychosocial assessment tool. Journal of Pediatric Psychology, 41(7), 810–819. https://doi.org/10.1093/jpepsy/jsv119
- Spurk, D., Hirschi, A., Wang, M., Valero, D., & Kauffeld, S. (2020). Latent profile analysis: A review and “how to” guide of its application within vocational behavior research. Journal of Vocational Behavior, 120(May), 103445. https://doi.org/10.1016/j.jvb.2020.103445
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. https://doi.org/10.1016/j.cpr.2011.12.001
- van de Schoot, R., Sijbrandij, M., Winter, S. D., Depaoli, S., & Vermunt, J. K. (2017). The GRoLTS-checklist: Guidelines for reporting on latent trajectory studies. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 451–467. https://doi.org/10.1080/10705511.2016.1247646
- Velleman, S., Collin, S. M., Beasant, L., & Crawley, E. (2016). Psychological wellbeing and quality-of-life among siblings of paediatric CFS/ME patients: A mixed-methods study. Clinical Child Psychology and Psychiatry, 21(4), 618–633. https://doi.org/10.1177/1359104515602373
- Verma, R., Mehdian, Y., Sheth, N., Netten, K., Vinette, J., Edwards, A., Polyviou, J., Orkin, J., & Amin, R. (2020). Screening for caregiver psychosocial risk in children with medical complexity: A cross-sectional study. BMJ Paediatrics Open, 4(1), 1–9. https://doi.org/10.1136/bmjpo-2020-000671
- Williams, M. E., Carson, M. C., Zamora, I., Harley, E. K., & Lakatos, P. P. (2014). Child-Parent psychotherapy in the context of the developmental disability and medical service systems. Pragmatic Case Studies in Psychotherapy, 10(3), 212–226. https://doi.org/10.14713/pcsp.v10i3.1871
- Wolmer, L., Hamiel, D., Slone, F. M., Picker, M., Adiv, T., & Laor, N. (2013). Post-traumatic reaction of Israeli Jewish and Arab children exposed to rocket attacks before and after teacher-delivered intervention. Israel Journal of Psychiatry, 50(3), 165–173.
- Yehene, E., Brezner, A., Ben-Valid, S., Golan, S., Bar-Nadav, O., & Landa, J. (2021). Factors associated with parental grief reaction following pediatric acquired brain injury. Neuropsychological Rehabilitation, 31(1), 105–128. https://doi.org/10.1080/09602011.2019.1668280