?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background: A negative self-concept is characterised by dysfunctional cognitions about the self and has been suggested to be a key factor involved in the development and maintenance of posttraumatic stress disorder (PTSD). In addition, the current definitions of PTSD according to DSM-5 and the new ICD-11 diagnosis of Complex PTSD (CPTSD) include aspects of negative self-concept in their diagnostic criteria.
Objective: The aim of this meta-analysis was to synthesise the currently available evidence on the effects of psychological interventions for PTSD on negative self-concept.
Methods: PubMed, PsychINFO, PSYNDEX, PTSDpubs and Cochrane Library were searched for randomised controlled trials (RCTs) of psychological treatments for PTSD symptoms in adults, published up to February 2021. A systematic review and meta-analysis were conducted, with risk of bias assessed by the Cochrane Risk of Bias Assessment Tool.
Results: A total of 25 RCTs (N = 2585) were included in the meta-analysis. Results showed that psychological interventions significantly improve a negative self-concept with a moderate to large controlled effect size (k = 30, g = 0.67, 95% CI [0.31, 1.02], p < .001) at post-treatment. Heterogeneity between studies was large but could not be accounted for by moderators included in the current analysis, i.e. different types of interventions (e.g. with vs. without a cognitive restructuring component, trauma-focused vs. not).
Conclusions: Current treatments for PTSD are effective in reducing a negative self-concept. However, more research is needed to identify moderators of this effect and identify interventions that are most effective for reducing negative self-concept.
HIGHLIGHTS
Posttraumatic stress disorder is related to a negative self-concept.
In this meta-analysis, we found that existing treatments for posttraumatic stress disorder reduce a negative self-concept.
Future research is needed to identify interventions that are most effective in reducing a negative self-concept.
Antecedentes: El autoconcepto negativo se caracteriza por cogniciones disfuncionales sobre uno mismo y se ha sugerido que es un factor clave involucrado en el desarrollo y mantención del trastorno de estrés postraumático (TEPT). Además, la definición actual de TEPT según el DSM-5 y el nuevo diagnóstico de TEPT complejo (TEPTC) de la CIE-11 incluyen aspectos del autoconcepto negativo en sus criterios diagnósticos.
Objetivo: El objetivo de este meta-análisis fue sintetizar la evidencia actualmente disponible sobre los efectos de las intervenciones psicológicas para el TEPT sobre el autoconcepto negativo.
Métodos: Se realizaron búsquedas en PubMed, PsychINFO, PSYNDEX, PTSDpubs y Cochrane Library de ensayos controlados aleatorizados (ECA) de tratamientos psicológicos para los síntomas de TEPT en adultos, publicados hasta febrero de 2021. Se realizó una revisión sistemática y un meta-análisis, con riesgo de sesgo evaluado por la Herramienta Cochrane de Evaluación del Riesgo de Sesgo.
Resultados: Se incluyeron un total de 25 ECA (N = 2585) en el meta-análisis. Los resultados mostraron que las intervenciones psicológicas mejoran significativamente el autoconcepto negativo con un tamaño del efecto controlado de moderado a grande (k = 30, g = 0,67, IC del 95% [0,31, 1,02], p < 0,001) después del tratamiento. La heterogeneidad entre los estudios fue grande, pero los moderadores incluidos en el análisis actual no pudieron explicarla, es decir, diferentes tipos de intervenciones (p. ej., presencia vs. ausencia de un componente de reestructuración cognitiva, centrada en el trauma vs. no centrada en el trauma).
Conclusiones: Los tratamientos actuales para el TEPT son efectivos para reducir el autoconcepto negativo. Sin embargo, se necesita de más investigaciones para identificar moderadores de este efecto e identificar intervenciones que sean más efectivas para reducir el autoconcepto negativo.
背景:负性自我概念的特征是对自我的认知功能失调,并被认为是创伤后应激障碍 (PTSD) 发展和维持的关键因素。此外,当前根据 DSM-5 对 PTSD 的定义和新的 ICD-11 复杂性 PTSD 诊断 (CPTSD) 在其诊断标准中纳入了负性自我概念方面。
目的:本元分析旨在综合当前 PTSD 心理干预对负性自我概念影响的可用证据。
方法: 搜索了PubMed、PsychINFO、PSYNDEX、PTSDpubs 和 Cochrane Library 截至 2021 年 2 月发表的成人 PTSD 症状心理治疗的随机对照试验 (RCT)。进行了系统综述和元分析,使用 Cochrane 偏倚风险评估工具评估偏倚风险评估。
结果:元分析共纳入了 25 项 RCT(N = 2585)。结果表明,心理干预在治疗后显著改善了负性自我概念,具有中到大的控制效应量(k = 30, g = 0.67, 95% CI [0.31, 1.02], p < .001)。研究之间异质性很大,但当前分析中包含的调节因素无法解释,即不同类型的干预措施(例如,有无认知重组成分、聚焦创伤与非聚焦创伤)。
结论:当前对 PTSD 的治疗可有效减少负性自我概念。然而,需要更多的研究来确定这种影响的调节因素,并确定对减少负性自我概念最有效的干预措施。
PALABRAS CLAVE:
1. Introduction
The self-concept can be regarded as a cognitive representation of one's own person (Harter, Citation1999). Closely related to the self-concept are the cognition-dependent self-related emotions of guilt and shame. While shame is triggered by the negative evaluation of one's own person, guilt follows the negative evaluation of one's own action (Lewis, Citation1971; Tracy & Robins, Citation2004). Consequently, a negative self-concept is defined by the presence of dysfunctional cognitions about the self, which includes guilt- and shame-related cognitions.
There are strong associations between a negative self-concept and posttraumatic stress disorder (PTSD). For example, the DSM-5 (American Psychiatric Association, Citation2013) lists dysfunctional cognitions about the self as well as shame and guilt among the PTSD symptom criteria. In the ICD-11, the newly introduced diagnosis of complex PTSD (CPTSD) includes a negative self-concept (beliefs about oneself as diminished, defeated, or worthless, accompanied by constant feelings of shame, guilt, or failure in relation to the traumatic event) as part of the disturbance in self-organisation criteria (World Health Organisation, Citation2019). Furthermore, theoretical models of PTSD posit that dysfunctional trauma-related cognitions, especially those related to a negative self-concept, are a key factor involved in the development and maintenance of the disorder (Ehlers & Clark, Citation2000; Foa & Rothbaum, Citation1998). There is extensive evidence supporting this view (Engelbrecht & Jobson, Citation2020; LoSavio et al., Citation2017), e.g, trauma-related negative cognitions about the self predicting PTSD following trauma over and above other known risk factors (Beierl et al., Citation2020; Ehring et al., Citation2008; Hansen et al., Citation2014).
As a negative self-concept plays a crucial role in the diagnosis, development, and maintenance of PTSD and CPTSD, treatment for these disorders should include interventions that are effective in reducing a negative self-concept. The extent to which psychological interventions for PTSD also reduce a negative self-concept has been examined in one systematic review (Brown et al., Citation2019) and four meta-analyses to date (Coventry et al., Citation2020; Diehle et al., Citation2014; Karatzias et al., Citation2019; Melton et al., Citation2019). Results uniformly show that current evidence-based treatments for PTSD reduce a negative self-concept. However, it is yet unclear whether treatment approaches systematically differ regarding their effects on this variable. There is preliminary evidence that trauma-focused interventions may reduce a negative self-concept more effectively than non-trauma-focused ones (Diehle et al., Citation2014). Importantly, however, trauma-focused interventions differ regarding the degree to which a negative self-concept is explicitly addressed, e.g. via cognitive restructuring. From both a theoretical as well as clinical perspective, it appears relevant to test whether interventions directly targeting a negative self-concept are superior to those that do not. Interestingly, results from two earlier meta-analyses addressing this issue did not find support for this (Diehle et al., Citation2014; Karatzias et al., Citation2019). However, these earlier analyses have limitations, including the lack of distinguishing between cognitive interventions in general vs. those targeting a negative self-concept, the focus on rather broad categories to classify treatments, and a low number of included studies examining the effects on negative self-concept (K < 10) in all meta-analyses (Coventry et al., Citation2020; Diehle et al., Citation2014; Karatzias et al., Citation2019; Melton et al., Citation2019).
The current meta-analysis aimed to replicate and extend these earlier findings. First, we hypothesised that the efficacy of psychological interventions on a negative self-concept is larger compared with control groups (waitlist, no contact control group, psychological placebo, or TAU; Hypothesis 1). Second, we hypothesised that therapies with formal cognitive restructuring have a greater effect on the negative self-concept than therapies without formal cognitive restructuring (Hypothesis 2). Third, we hypothesised that therapies with the formal restructuring of explicitly self-related cognitions have a greater effect on the negative self-concept than therapies with formal restructuring of cognitions that are not specifically self-related (Hypothesis 3). To examine further systematic differences between intervention types, we additionally examined whether the effect on a negative self-concept differed between trauma-focused and non-trauma-focused interventions, as well as between different types of therapy.
2. Methods
2.1. Protocol registration
The protocol of the present meta-analysis was registered in the PROSPERO database on May 14, 2021 (CRD42021255038).
2.2. Primary outcome
Primary outcome was the standardised mean difference of negative self-concept scores between the intervention and control group at post-treatment. Note that this was different from the primary outcome of the original studies included (see eligibility criteria below).
2.3. Eligibility criteria
In order to be included in the meta-analysis, all studies had to meet the following criteria:
Randomised controlled trial (RCT) with at least one active psychological intervention being compared to at least one control group and/or another active psychological interventionFootnote1;
Primary intervention target: Reduction of PTSD symptoms;
Primary outcome: Severity of PTSD symptoms assessed with a validated instrument at least pre- and post-treatmentFootnote2;
(Secondary) outcome measures included a measure of negative self-concept assessed with a validated instrument capturing cognitions about the self (including cognitions of guilt and shame) at least at post-treatment;
≥18 years old or separate data from the subsample ≥ 18y available;
At least 10 participants per condition;
Published in a peer-reviewed journal (no language restrictions);
No diagnosed developmental disability, intellectual disability, or neurodegenerative disorder.
2.4. Literature search and study selection
Appropriate studies were identified through systematic literature searches of PubMed, PsychINFO, PSYNDEX, PTSDpubs, and Cochrane Library databases. The following search terms were combined:
(PTSD OR posttraumatic stress disorder OR PTBS OR Posttraumatische Belastungsstörung) AND ([treatment trial OR randomized controlled trial OR clinical trial] OR [indexed by a thesaurus term as clinical trial]).
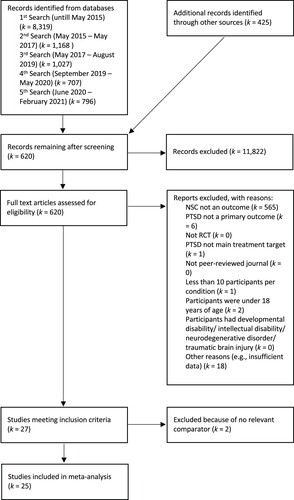
The selection of studies is depicted in the PRISMA flowchart (see ). In the first step, all articles were selected based on title and abstract. In the second step, the remaining articles were further selected based on reviewing the full text. The literature searches and all steps of the study selection were performed by two independent raters. Discrepancies were discussed and resolved by consensus.
2.5. Data extraction
Data were coded for study participants, the intervention and control group and the negative self-concept instrument (see ) by two independent raters, with discrepancies being resolved by consensus.
Table 1. Study characteristics coded.
2.6. Risk of bias
The Cochrane Risk of Bias Assessment Tool (Higgins et al., Citation2011) was used to assess the risk of bias within the studies. In addition, researcher allegiance was assessed as an important risk of bias, as this is not integrated in the Cochrane Risk of Bias Assessment Tool (Cuijpers, Citation2016).
2.7. Statistical analyses
2.7.1. Effect size calculation
Hedges’ g was used for the primary outcome of this meta-analysis (post-intervention standardised mean difference of negative self-concept scores) and was calculated with a confidence interval of 95% using the R software package esc (Lüdecke, Citation2019). Positive effect sizes (corresponding to cases in which the intervention group had a better averaged negative self-concept value at post-treatment than the control group) were additionally converted into the number needed to treat. Negative effect sizes (corresponding to cases where the control group had a better averaged negative self-concept value at post-treatment than the intervention group) were converted to the number needed to harm. The R software package dmetar (Harrer et al., Citation2019), which determines the number needed to treat, or the number needed to harm according to Kraemer and Kupfer (Citation2006), was used for the calculation.
When M or SD at post-treatment of the respective groups were not reported in the original articles, Hedges’ g was calculated from other available data (Cohen's d, p-, t-, or F-value) using the R software package dmetar (Harrer et al., Citation2019). If these were also not reported, the authors of the respective study were contacted by email. If there was no response, the study was excluded.
In the case of multiple negative self-concept instruments, one was selected for effect size calculation according to an a-priori hierarchy with preference for the most frequently used instrument as well as for structured clinician-administered interviews.
If there were three or more intervention arms, the control group sample size was divided by the number of intervention arms, allowing each intervention arm to be used for the analysis, avoiding double counting and thus overestimation of effect sizes (Higgins et al., Citation2019). If a cross-over design was used, only outcome data from the first randomisation period were used.
All statistical analyses were calculated using the R software package meta (Balduzzi et al., Citation2019). As heterogeneity between included studies was assumed, a random-effects model was applied. Subgroup analyses (moderator and sensitivity analyses) were performed with a mixed-effects model.
2.7.2. Effects of psychological interventions on negative self-concept
To test Hypothesis 1, the pooled effect size of psychological interventions on negative self-concept was determined. In order to find out whether the effect differed according to the type of control group, two additional meta-analyses were calculated, one with exclusively inactive control groups (waiting list or no contact control) and one with exclusively active control groups (psychological placebo or treatment-as-usual [TAU]). The pooled effect sizes were interpreted according to Cohen’s guidelines for controlled effect sizes (small = 0.20, moderate = 0.50, large = 0.80; Cohen, Citation2013).
2.7.3. Effects of interventions to restructure dysfunctional cognitions on negative self-concept
Hypotheses 2 and 3 were tested using moderator analyses, comparing therapies containing vs. not containing interventions to restructure dysfunctional cognitions (Hypothesis 2), and therapies that did vs. did not explicitly focus on self-related cognitions (Hypothesis 3).
2.7.4. Effects of types of therapy and trauma-focused interventions on negative self-concept
Additional moderator analyses were conducted to determine whether the effect of psychological interventions on negative self-concept was dependent on the type of therapy (cognitive [behavior] therapy [CT/CBT], exposure alone, Eye Movement Desensitisation and Reprocessing [EMDR], and other types of therapy), and trauma-focused versus non-trauma-focused interventions, respectively.
2.7.5. Statistical heterogeneity
To assess heterogeneity, the Q-test was performed; in addition, I2 was also calculated (25%: low, 50%: moderate, 75% high heterogeneity; Higgins et al., Citation2003). To find possible reasons for the heterogeneity, a leave-one-out analysis was performed, and the meta-analysis was again calculated excluding influential cases (outliers that may bias the pooled effect and its heterogeneity). To identify outliers, an outlier analysis was first performed. To identify studies with comparatively high influence on the effect and its heterogeneity, a leave-one-out analysis was then performed. Furthermore, a sensitivity analysis was conducted on the type of negative self-concept instrument used.
2.7.6. Publication bias
Publication bias was first tested by visual inspection of the funnel plots, followed by the Egger's test. Duval and Tweedie's trim and fill method was used to obtain a corrected estimate of the pooled effect size (Duval & Tweedie, Citation2000).
3. Results
3.1. Included studies
Detailed results for the study search and selection are shown in the PRISMA flowchart (see ). 27 studies met eligibility criteria. 25 of these studies compared a psychological intervention with a control group (waitlist, no contact control group, psychological placebo, or TAU); the other two studies compared a psychological intervention that included restructuring dysfunctional cognitions to another psychological intervention without cognitive restructuring. The latter studies had originally been included as we had planned to analyze Hypotheses 2 and 3 in two ways: first, using moderator analyses including all studies, and second, exclusively focusing on studies with direct comparisons of interventions with vs. without restructuring dysfunctional cognitions. However, the second type of analyses could not be performed due to the insufficiently small number of studies using such a design (k = 2). As these two studies were not suitable to be used for the remaining analyses (requiring the comparison of an intervention with a control group, not another bona fide treatment), they were excluded from the analyses. Our meta-analysis thus finally included k = 25 studies.
3.2. Study characteristics
Among the 30 intervention arms included in the analysis, 15 arms included interventions to restructure dysfunctional cognitions, with nine of the 15 arms explicitly focusing on dysfunctional cognitions about the self (see Supplementary Material, Table A, for an overview of study characteristics). Fourteen arms used CT/CBT, six used exposure alone, one used EMDR, and nine used other types of therapy (e.g. counselling). Twenty arms included trauma-focused interventions. Nineteen arms used inactive control groups (waiting list or no contact control group), and 11 arms used active control groups (psychological placebo or TAU). N = 2,585 participants were randomised and used for analyses (56% female; age: M = 40.49; SD = 11.04). Negative self-concept was assessed in different ways, namely as trauma-related cognitions about the self (9 studies; e.g. Self subscale of the Posttraumatic Cognitions Inventory, PTCI), non-trauma-related cognitions about the self (11 studies; e.g. Rosenberg's Self-Esteem Scale, RSE), guilt cognitions (11 studies; e.g. Trauma-Related Guilt Inventory, TRGI).
3.3. Hypothesis 1: effects of psychological interventions on negative self-concept
In the comparison of intervention to control groups, controlled effects ranged from medium to large (k = 30, g = 0.67, 95% CI [0.31, 1.02], p < .001). Results support Hypothesis 1 and show that psychological interventions significantly improved a negative self-concept compared with control groups at post-treatment (see also forest plot in ).
Figure 2. Forest plot of between-group effect sizes (post-treatment). Notes. SMD refers to the comparison between the intervention and control groups at post-treatment; measure used is Hedges’ g; positive values refer to cases where the intervention group had a better averaged NSC value than the control group at post-treatment. NNT
= Number Needed to Treat (NNT with negative sign refers to Number Needed to Harm, NNH). CPT = Cognitive Processing Therapy. PE = Prolonged Exposure.
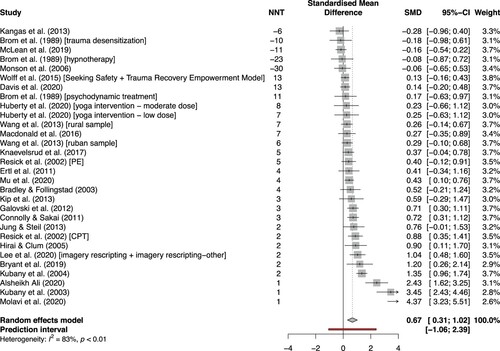
Comparing interventions with inactive control groups again showed a medium to large effect (k = 19, g = 0.68, 95% CI [0.28, 1.09], p = .002), whereas the effect was no longer significant when comparing with active control groups (k = 11, g = 0.65, 95% CI [−0.15, 1.45], p = .102; for details, see ).
Table 2. Results of meta-analyses.
3.4. Hypotheses 2 and 3: effects of interventions to restructure dysfunctional cognitions on negative self-concept
The difference between interventions to restructure dysfunctional cognitions vs. those without interventions to restructure dysfunctional cognitions was not significant (k = 30, Q = 1.74, p = .187). Similarly, effects of therapies explicitly targeting self-related cognitions did not significantly differ from those not explicitly targeting self-related cognitions (k = 15, Q = 0.23, p = .634; for details on both moderator analyses, see ).
3.5. Exploratory moderator analyses
In an exploratory moderator analysis, type of therapy (CT/CBT; exposure alone; other types of therapy) did not significantly moderate effects of treatment on negative self-concept (k = 30, Q = 2.34, p = .51). Similarly, no significant difference was found between trauma-focused vs. non-trauma-focused interventions on negative self-concept (k = 30, Q = 0.47, p = .50; for details see Supplementary Material, Table B).
3.6. Statistical heterogeneity
The effect sizes of the included studies differed significantly from each other (k = 30, Q = 167.87, p < .001). Heterogeneity of effect sizes was estimated to be = 0.68, 95% CI [0.43, 1.67] with an I2 = 82.70%, 95% CI [76.20%, 87.40%], indicating large heterogeneity (Higgins et al., Citation2003). The prediction interval ranged from g = −1.06 to 2.39, so negative intervention effects cannot be ruled out for future studies. Several analyses were performed to further examine sources of heterogeneity (see ). The outlier analysis identified four studies (Alsheikh Ali, Citation2020; Kubany et al., Citation2003; McLean et al., Citation2019; Molavi et al., Citation2020), and leave-one-out analyses identified three studies that emerged as most influential in terms of both pooled effect size and heterogeneity (Alsheikh Ali, Citation2020; Kubany et al., Citation2003; Molavi et al., Citation2020). Since all three studies were previously identified as outliers, it can be assumed that these studies are influential cases. Removing the influential cases from the meta-analysis lowered the overall heterogeneity but kept it in a moderate to high range (k = 27, I2 = 60.60%, 95% CI [14.00%, 74.10%]). The effect size decreased from g = 0.67 to g = 0.42, 95% CI [0.25, 0.58], p < .001. In a sensitivity analysis, no significant difference between types of negative self-concept instruments was found (k = 30, Q = 2.66, p = .264).
3.7. Publication bias
Egger's test was significant, indicating publication bias (k = 30, intercept (B0) = 2.5, 95% CI [0.27, 4.73], p = .037). Visual inspection of the funnel plot revealed an asymmetric distribution of effect sizes as a function of SE (see Figure A in the Supplementary Material). However, the reason for the asymmetry was not studies with large effect sizes and simultaneously high SE (small-study effect), but studies with negative effect sizes and simultaneously low SE, which did not indicate a publication bias. Similarly, when applying the trim and fill method the effect size did not change (g = 0.67, 95% CI [0.31, 1.02], p < .001). Nevertheless, it can be assumed that the effect of psychological interventions on negative self-concept was overestimated due to publication bias, as the high heterogeneity observed (I2 = 82.70%) makes the trim-and-fill test less robust (Peters et al., Citation2006).
3.8. Risk of bias
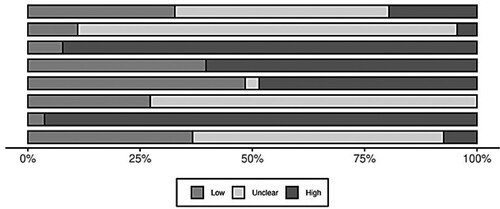
Results of the risk of bias assessment of all included studies (k = 25) is provided in the Supplementary Material (Table C). An overview of the weighted risk of bias across all studies is provided in . About one third of all studies used appropriate methods to generate a randomisation sequence (k = 8; 32%), but group assignment was kept secret in only few studies (k = 3; 12%). In almost half of the studies, it was not reported which methods were used to generate a randomisation sequence (k = 12, 48%) and in almost all studies there was no info on allocation concealment (k = 21, 84%). The risk of performance bias was estimated to be high in almost all studies (k = 23, 92%) because blinding of study personnel and participants during treatment was mostly absent, as inevitable in RCTs evaluating psychological interventions. The risk of detection bias was considered high in more than half of all studies (k = 15; 60%) although almost all studies used a self-report to measure negative self-concept symptoms. The risk of attrition bias was estimated to be high in almost half of the studies (k = 12, 48%) because a complete case analysis rather than an intention-to-treat analysis was performed. The risk of reporting bias was unclear in almost all studies (k = 18; 72%) because the study protocol was not preregistered and therefore could not be matched with outcome reports. Researcher allegiance risk was estimated to be high in almost all studies (k = 24; 96%). No other potential causes of bias were evident in approximately one-third of the studies (k = 9; 36%), but assessment was complicated by the often nontransparent reporting.
Figure 3. Weighted risk of bias of all studies (k = 25) assessed according to the Cochrane Risk of Bias Assessment Tool (Higgins et al., Citation2011).
4. Discussion
The aim of this meta-analysis was to replicate and extend earlier findings on the effects of psychological treatment for PTSD on negative self-concept, specifically to identify systematic differences between different types of interventions.
Hypothesis 1 was confirmed as psychological interventions significantly improved a negative self-concept compared with control groups at post-treatment. The moderate to large effect size is comparable to previous meta-analyses on effects of psychological interventions on a negative self-concept, although the type of control group and the types of therapy analyzed partly differed from the earlier meta-analysis (Coventry et al., Citation2020; Diehle et al., Citation2014; Karatzias et al., Citation2019; Melton et al., Citation2019). The number needed to treat, or the number needed to harm showed a range from −30 to 13. The negative estimated values (number needed to harm) was due to five studies where the intervention group had worse negative self-concept values compared to the control group at post-treatment, suggesting a negative impact of the intervention on the self-concept. Number needed to treat estimates from a previous meta-analysis on the efficacy of CBT interventions and exposure alone on the disturbance of self-organisation symptom clusters of CPTSD had been much more precise and ranged between 2 and 7 (Karatzias & Cloitre, Citation2019).
The wide interval of the number needed to treat estimates is partly due to the large heterogeneity of the effect sizes, which parallels previous meta-analyses (Coventry et al., Citation2020; Diehle et al., Citation2014; Melton et al., Citation2019). To further address this heterogeneity, two additional hypotheses were tested. In contrast to the hypotheses, neither presence vs. absence of formal restructuring of dysfunctional cognitions nor presence vs. absence of interventions targeting cognitions about the self-showed significant effects on change in negative self-concept. Similarly, neither type of therapy nor trauma focus were found to moderate effects in additional analyses, partially contradicting the results of a previous meta-analysis where trauma-focus had a significant effect (Diehle et al., Citation2014). In sum, although current evidence-based interventions for PTSD are clearly effective in reducing a negative self-concept, the current meta-analysis does not suggest that there are systematic differences between different types of treatments regarding their effect on a negative self-concept. Different explanations for this finding are conceivable. First, the average effect sizes for treatments including cognitive restructuring vs. not including this intervention component showed large numerical differences (g = 0.91 vs. g = 0.45). However, as there was also large heterogeneity within the respective categories this difference was not statistically significant. As the number of studies available for inclusion in the meta-analysis was only modest, the statistical power for this analysis was probably too low. Second, however, the large heterogeneity within the categories suggests that the mere fact of an intervention targeting cognitions (or the negative self-concept, respectively) may not be the key factor leading to a large effect of this treatment on negative self-concept. Instead, additional factors may be responsible that are yet poorly understood. Possible additional moderators to be investigated in future research may include the fact whether hot (i.e. emotionally laden) or cold (i.e. purely verbal or semantic) cognitions are targeted and/or the dose and timing of cognitive restructuring. In addition, whereas some treatments interweave cognitive interventions with interventions targeting the trauma memory (e.g. Ehlers and Clark’s cognitive therapy; Ehlers et al., Citation2005) others deliver cognitive restructuring as a separate intervention.
Additional analyses exploring possible sources of heterogeneity of findings did not find an effect of different types of negative self-concept instruments used. However, the type of control group was a significant moderator with significant effects of the intervention on a negative self-concept only being found in studies using inactive control groups, but not those with active control groups. This pattern was also evident in a previous meta-analysis (Karatzias et al., Citation2019), and may suggest that rather non-specific factors are responsible for the effects of PTSD treatment on a negative self-concept (Karatzias et al., Citation2019). However, it is important to note that there was at least moderate to high heterogeneity within subgroups in all moderator analyses, suggesting that the lack of moderation could also be due to low statistical power.
The present meta-analysis has a number of limitations. First, the studies overall showed high risk of bias. This particularly affected the domains of researcher allegiance, performance, and detection, so that a bias of the pooled effect can be assumed. In addition, the lack of differences between different types of treatment on a negative self-concept found in the current study may be due to limited statistical power and should therefore be interpreted with caution. In addition, the very low number of studies directly comparing psychological interventions with vs. without restructuring of a negative self-concept prevented us from investigating possible differences between these approaches when used within a randomised design. Another limitation is the relatively narrow definition of negative self-concept, which limits the findings to the effect of psychological interventions on dysfunctional cognitions about the self, guilt and shame cognitions. However, the construct can also be defined more broadly, including affective components of guilt and shame (see e.g. the ICD-11 definition of CPTSD, World Health Organisation, Citation2019). Finally, no follow-up data on negative self-concept measures were evaluated.
Despite the limitations mentioned above, the meta-analysis was able to show that psychological interventions can effectively improve a negative self-concept directly after the intervention. Thus, psychological interventions should be considered in the treatment of disturbance of self-organisation symptomatology of CPTBS. However, the large heterogeneity between studies suggests that not all evidence-based interventions reduced a negative self-concept to the same degree. Which factors determine a strong vs. moderate or weak effect of a particular intervention on a negative self-concept is still poorly understood. As a negative self-concept is not only included in current diagnostic criteria for (C)PTSD but also considered to play a causal role in the maintenance of the disorder, future research should systematically address this question.
Based on the current meta-analysis, a number of recommendations for future research in this area can be drawn. First, the negative self-concept should be more systematically included as a secondary outcome variable in RCTs examining psychological treatments for PTSD in order to provide a larger and more representative evidence based for this research question. Second, RCTs directly comparing different interventions regarding their effects on a negative self-concept are needed, e.g. comparing intervention with vs. without cognitive restructuring with vs. without trauma-focused interventions, or with different types of delivering cognitive interventions (e.g. targeting hot vs. cold cognitions; cognitive restructuring as separate elements vs. interwoven with imagery-based interventions). In addition, it would be of interest to study more closely when and how a negative self-concept changes within a given treatment approach. Finally, a more differentiated conceptualisation and assessment of a negative self-concept in PTSD and CPTSD is needed, including affective components.
Supplemental Material
Download MS Word (146.5 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Notes
1 When comparing an active psychological intervention with another active psychological intervention, only one of the two intervention arms was allowed to include the restructuring of dysfunctional cognitions.
2 Note that PTSD severity was not used as an outcome in this meta-analysis, but the eligibility criterion was used to ensure that only treatments for PTSD were included.
References
- Alsheikh Ali, A. S. S. (2020). Efficiency of intervention counseling program on the enhanced psychological well-being and reduced post-traumatic stress disorder symptoms Among Syrian women refugee survivors. Clinical Practice and Epidemiology in Mental Health, 16(Suppl-1), 134–141. https://doi.org/10.2174/1745017902016010134
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596.
- Balduzzi, S., Rücker, G., & Schwarzer, G. (2019). How to perform a meta-analysis with R: A practical tutorial. Evidence-Based Mental Health, 22(4), 153–160. https://doi.org/10.1136/ebmental-2019-300117
- Beierl, E. T., Böllinghaus, I., Clark, D. M., Glucksman, E., & Ehlers, A. (2020). Cognitive paths from trauma to posttraumatic stress disorder: A prospective study of ehlers and clark's model in survivors of assaults or road traffic collisions. Psychological Medicine, 50(13), 2172–2181. https://doi.org/10.1017/S0033291719002253
- Bradley, R. G., & Follingstad, D. R. (2003). Group therapy for incarcerated women who experienced interpersonal violence: A pilot study. Journal of Traumatic Stress, 16(4), 337–340. https://doi.org/10.1023/A:1024409817437
- Brom, D., Kleber, R. J., & Defares, P. B. (1989). Brief psychotherapy for posttraumatic stress disorders. Journal of Consulting and Clinical Psychology, 57(5), 607–612. https://doi.org/10.1037//0022-006x.57.5.607
- Brown, L. A., Belli, G. M., Asnaani, A., & Foa, E. B. (2019). A review of the role of negative cognitions about oneself, others, and the world in the treatment of PTSD. Cognitive Therapy and Research, 43(1), 143–173. https://doi.org/10.1007/s10608-018-9938-1
- Bryant, R. A., Kenny, L., Rawson, N., Cahill, C., Joscelyne, A., Garber, B., Tockar, J., Dawson, K., & Nickerson, A. (2019). Efficacy of exposure-based cognitive behaviour therapy for post-traumatic stress disorder in emergency service personnel: A randomised clinical trial. Psychological Medicine, 49(9), 1565–1573. https://doi.org/10.1017/S0033291718002234
- Cohen, J. (2013). Statistical Power Analysis for the Behavioral Sciences. Academic press.
- Connolly, S., & Sakai, C. (2011). Brief trauma intervention with Rwandan genocide-survivors using thought field therapy. International Journal of Emergency Mental Health, 13(3), 161–172.
- Coventry, P. A., Meader, N., Melton, H., Temple, M., Dale, H., Wright, K., Cloitre, M., Karatzias, T., Bisson, J., & Roberts, N. P. (2020). Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: Systematic review and component network meta-analysis. PLoS Medicine, 17(8), e1003262. https://doi.org/10.1371/journal.pmed.1003262
- Cuijpers, P. (2016). Meta-analyses in Mental Health Research. A Practical Guide. Uitgeverij.
- Davis, L. W., Schmid, A. A., Daggy, J. K., Yang, Z., O'Connor, C. E., Schalk, N., Do, A.-N. L., Maric, D., Lazarick, D., & Knock, H. (2020). Symptoms improve after a yoga program designed for PTSD in a randomized controlled trial with veterans and civilians. Psychological Trauma: Theory, Research, Practice, and Policy, 12(8), 904–991. https://doi.org/10.1037/tra0000564
- Diehle, J., Schmitt, K., Daams, J. G., Boer, F., & Lindauer, R. J. (2014). Effects of psychotherapy on trauma-related cognitions in posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 27(3), 257–264. https://doi.org/10.1002/jts.21924
- Duval, S., & Tweedie, R. (2000). Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. https://doi.org/10.1111/j.0006-341x.2000.00455.x
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. https://doi.org/10.1016/s0005-7967(99)00123-0
- Ehlers, A., Clark, D. M., Hackmann, A., McManus, F., & Fennell, M. (2005). Cognitive therapy for post-traumatic stress disorder: Development and evaluation. Behaviour Research and Therapy, 43(4), 413–431. https://doi.org/10.1016/j.brat.2004.03.006
- Ehring, T., Ehlers, A., & Glucksman, E. (2008). Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. Journal of Consulting and Clinical Psychology, 76(2), 219–230. https://doi.org/10.1037/0022-006x.76.2.219
- Engelbrecht, A., & Jobson, L. (2020). Self-concept, post-traumatic self-appraisals and post-traumatic psychological adjustment: What are the relationships? Behavioural and Cognitive Psychotherapy, 48(4), 463–480. https://doi.org/10.1017/s1352465820000156
- Ertl, V., Pfeiffer, A., Schauer, E., Elbert, T., & Neuner, F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: A randomized controlled trial. JAMA, 306(5), 503–512. https://doi.org/10.1001/jama.2011.1060
- Foa, E. B., & Rothbaum, B. O. (1998). Treating the Trauma of Rape: Cognitive-Behavioral Therapy for PTSD. Guilford Press.
- Galovski, T. E., Blain, L. M., Mott, J. M., Elwood, L., & Houle, T. (2012). Manualized therapy for PTSD: Flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology, 80(6), 968–981. https://doi.org/10.1037/a0030600
- Hansen, M., Armour, C., Wittmann, L., Elklit, A., & Shevlin, M. (2014). Is there a common pathway to developing ASD and PTSD symptoms? Journal of Anxiety Disorders, 28(8), 865–872. https://doi.org/10.1016/j.janxdis.2014.09.019
- Harrer, M., Cuijpers, P., Furukawa, T. A., & Ebert, D. D. (2019). dmetar: Companion R Package For The Guide ‘Doing Meta-Analysis in R’. R package version 0.0.9000. http://dmetar.protectlab.org/.
- Harter, S. (1999). The Construction of the Self: A Developmental Perspective. Guilford Press.
- Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., Savovic, J., Schulz, K. F., Weeks, L., & Sterne, J. A. (2011). The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ, 343(oct18 2), d5928. https://doi.org/10.1136/bmj.d5928
- Higgins, J. P., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. (2019). Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons.
- Higgins, J. P., Tompson, S., Deeks, J., & Altman, D. (2003). A meta-analysis on the effectiveness of smart-learning. BMJ, 327(1), 557–560. https://doi.org/10.13000/JFMSE.2014.26.1.148
- Hirai, M., & Clum, G. A. (2005). An internet-based self-change program for traumatic event related fear, distress, and maladaptive coping. Journal of Traumatic Stress, 18(6), 631–636. https://doi.org/10.1002/jts.20071
- Huberty, J., Sullivan, M., Green, J., Kurka, J., Leiferman, J., Gold, K., & Cacciatore, J. (2020). Online yoga to reduce post traumatic stress in women who have experienced stillbirth: A randomized control feasibility trial. BMC Complementary Medicine and Therapies, 20(1), 1–19. https://doi.org/10.1186/s12906-020-02926-3
- Jung, K., & Steil, R. (2013). A randomized controlled trial on cognitive restructuring and imagery modification to reduce the feeling of being contaminated in adult survivors of childhood sexual abuse suffering from posttraumatic stress disorder. Psychotherapy and Psychosomatics, 82(4), 213–220. https://doi.org/10.1159/000348450
- Kangas, M., Milross, C., Taylor, A., & Bryant, R. A. (2013). A pilot randomized controlled trial of a brief early intervention for reducing posttraumatic stress disorder, anxiety and depressive symptoms in newly diagnosed head and neck cancer patients. Psycho-Oncology, 22(7), 1665–1673. https://doi.org/10.1002/pon.3208
- Karatzias, T., & Cloitre, M. (2019). Treating adults with complex posttraumatic stress disorder using a modular approach to treatment: Rationale, evidence, and directions for future research. Journal of Traumatic Stress, 32(6), 870–876. https://doi.org/10.1002/jts.22457
- Karatzias, T., Murphy, P., Cloitre, M., Bisson, J., Roberts, N., Shevlin, M., Hyland, P., Maercker, A., Ben-Ezra, M., & Coventry, P. (2019). Psychological interventions for ICD-11 complex PTSD symptoms: Systematic review and meta-analysis. Psychological Medicine, 49(11), 1761–1775. https://doi.org/10.1017/S0033291719000436
- Kip, K. E., Rosenzweig, L., Hernandez, D. F., Shuman, A., Sullivan, K. L., Long, C. J., Taylor, J., McGhee, S., Girling, S. A., & Wittenberg, T. (2013). Randomized controlled trial of accelerated resolution therapy (ART) for symptoms of combat-related post-traumatic stress disorder (PTSD). Military Medicine, 178(12), 1298–1309. https://doi.org/10.7205/MILMED-D-13-00298
- Knaevelsrud, C., Böttche, M., Pietrzak, R. H., Freyberger, H. J., & Kuwert, P. (2017). Efficacy and feasibility of a therapist-guided internet-based intervention for older persons with childhood traumatization: A randomized controlled trial. The American Journal of Geriatric Psychiatry, 25(8), 878–888. https://doi.org/10.1016/j.jagp.2017.02.024
- Kraemer, H. C., & Kupfer, D. J. (2006). Size of treatment effects and their importance to clinical research and practice. Biological Psychiatry, 59(11), 990–996. https://doi.org/10.1016/j.biopsych.2005.09.014
- Kubany, E. S., Hill, E. E., & Owens, J. A. (2003). Cognitive trauma therapy for battered women with PTSD: Preliminary findings. Journal of Traumatic Stress, 16(1), 81–91. https://doi.org/10.1023/A:1022019629803
- Kubany, E. S., Hill, E. E., Owens, J. A., Iannce-Spencer, C., McCaig, M. A., Tremayne, K. J., & Williams, P. L. (2004). Cognitive trauma therapy for battered women with PTSD (CTT-BW). Journal of Consulting and Clinical Psychology, 72(1), 3–18. https://doi.org/10.1037/0022-006X.72.1.3
- Lee, D. J., Schnitzlein, C. W., Wolf, J. P., Vythilingam, M., Rasmusson, A. M., & Hoge, C. W. (2016). Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: Systemic review and meta-analyses to determine first-line treatments. Depression and Anxiety, 33(9), 792–806. https://doi.org/10.1002/da.22511
- Lewis, H. B. (1971). Shame and guilt in neurosis. Psychoanalytic Review, 58(3), 419–438.
- LoSavio, S. T., Dillon, K. H., & Resick, P. A. (2017). Cognitive factors in the development, maintenance, and treatment of post-traumatic stress disorder. Current Opinion in Psychology, 14, 18–22. https://doi.org/10.1016/j.copsyc.2016.09.006
- Lüdecke, D. (2019). esc: Effect Size Computation for Meta Analysis (Version 0.5.1). https://doi.org/10.5281/zenodo.1249218.
- Macdonald, A., Pukay-Martin, N. D., Wagner, A. C., Fredman, S. J., & Monson, C. M. (2016). Cognitive–behavioral conjoint therapy for PTSD improves various PTSD symptoms and trauma-related cognitions: Results from a randomized controlled trial. Journal of Family Psychology, 30(1), 157–162. https://doi.org/10.1037/fam0000177
- McLean, C. P., Zandberg, L., Brown, L., Zang, Y., Benhamou, K., Dondanville, K. A., Yarvis, J. S., Litz, B. T., Mintz, J., & Young-McCaughan, S. s. (2019). Guilt in the treatment of posttraumatic stress disorder among active duty military personnel. Journal of Traumatic Stress, 32(4), 616–624. https://doi.org/10.1002/jts.22416
- Melton, H. A., Meader, N., Dale, H., Wright, K., Jones-Diette, J. S., Temple, M., Shah, I., Lovell, K., McMillan, D., & Churchill, R. C. (2019). Interventions for Complex Traumatic Events (INCiTE): systematic review and research prioritisation exercise. Health Technology Assessment, 24, 43. https://doi.org/10.3310/hta24430
- Molavi, P., Pourabdol, S., & Azarkolah, A. (2020). The effectiveness of acceptance and commitment therapy on posttraumatic cognitions and psychological inflexibility among students with trauma exposure. Archives of Trauma Research, 9(2), 69–74. https://doi.org/10.1016/j.beth.2010.08.009
- Monson, C. M., Schnurr, P. P., Resick, P. A., Friedman, M. J., Young-Xu, Y., & Stevens, S. P. (2006). Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74(5), 898–907. https://doi.org/10.1037/0022-006X.74.5.898
- Mu, W., Narine, K., Farris, S., Lieblich, S., Zang, Y., Bredemeier, K., Brown, L., & Foa, E. (2020). Trauma-related cognitions predict treatment response in smokers with PTSD: Evidence from cross-lagged panel analyses. Addictive Behaviors, 108, 106376. https://doi.org/10.1016/j.addbeh.2020.106376
- Peters, J. L., Sutton, A. J., Jones, D. R., Abrams, K. R., & Rushton, L. (2006). Comparison of two methods to detect publication bias in meta-analysis. JAMA, 295(6), 676–680. https://doi.org/10.1001/jama.295.6.676
- Resick, P. A., Nishith, P., Weaver, T. L., Astin, M. C., & Feuer, C. A. (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70(4), 867–879. https://doi.org/10.1037//0022-006x.70.4.867
- Schäfer, I., Gast, U., Hofmann, A., Knaevelsrud, C., Lampe, A., Liebermann, P., Lotzin, A., Maercker, A., Rosner, R., & Wöller, W. (2019). S3-Leitlinie Posttraumatische Belastungsstörung. Springer. https://doi.org/10.1007/978-3-662-59783-5.
- Shapiro, F. (2017). Eye movement desensitization and reprocessing (EMDR) therapy. Guilford.
- Tracy, J. L., & Robins, R. W. (2004). Putting the self into self-conscious emotions: A theoretical model. Psychological Inquiry, 15(2), 103–125. https://doi.org/10.1207/s15327965pli1502_01
- Wang, Z., Wang, J., & Maercker, A. (2013). Chinese My trauma recovery, a Web-based intervention for traumatized persons in two parallel samples: Randomized controlled trial. Journal of Medical Internet Research, 15(9), e213. https://doi.org/10.2196/jmir.2690
- Wolff, N., Huening, J., Shi, J., Frueh, B. C., Hoover, D. R., & McHugo, G. (2015). Implementation and effectiveness of integrated trauma and addiction treatment for incarcerated men. Journal of Anxiety Disorders, 30, 66–80. https://doi.org/10.1016/j.janxdis.2014.10.009
- World Health Organisation. (2019). International statistical classification of diseases and related health problems (11 ed.). https://icd.who.int/.