ABSTRACT
Background:
Developmental Trauma Disorder (DTD) is a proposed childhood psychiatric diagnosis for psychopathological and developmental sequela of victimization and attachment trauma extending beyond posttraumatic stress disorder (PTSD).
Objective:
To determine whether a sub-group of trauma-impacted children is characterized by symptoms of DTD that extend beyond, or co-occur with, the symptoms of PTSD.
Method:
Person-centred Latent Class Analyses (LCA) were done with data from 507 children (ages 7–18 years, (M = 12.11, SD = 2/92); 49% female) referred to the study by mental health or paediatric clinicians.
Results:
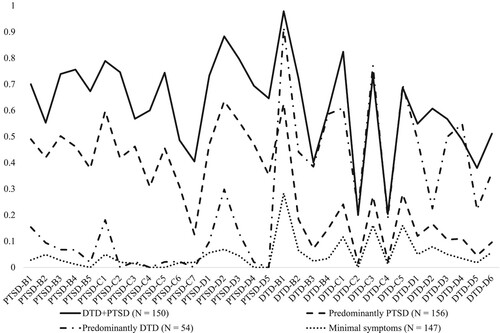
A four class solution was optimal (LMR = 398.264, p < .001; Entropy = .93): (1) combined DTD + PTSD (n = 150); (2) predominant DTD (n = 156); (3) predominant PTSD (n = 54); (4) minimal symptoms (n = 147). Consistent with prior research, the DTD + PTSD class was most likely to have experienced traumatic emotional abuse and neglect (X2(3) = 16.916 and 28.016, respectively, p < .001), and had the most psychiatric comorbidity (F(3, 502) = 3.204, p < .05). Predominant DTD class members were most likely to meet criteria for Oppositional Defiant Disorder (ODD) (X2(3) = 84.66, p < .001).
Conclusion:
Symptoms of DTD may occur with, or separately from, PTSD symptoms. Children with high DTD|+PTSD symptoms had extensive psychiatric comorbidity, while those with high DTD symptoms and minimal PTSD symptoms were highly likely to meet criteria for ODD. In clinical and research assessment and treatment of children with complex psychiatric comorbidity or disruptive behaviour problems, symptoms of DTD should be considered, both along with, and in the absence of, PTSD symptoms.
HIGHLIGHTS
Assessing Developmental Trauma Disorder (DTD) enables clinicians to identify trauma-impacted children who have particularly complex symptoms that exacerbate the psychiatric comorbidity related to PTSD and that extend beyond PTSD to include externalizing problems.
Antecedentes: El trastorno traumático del desarrollo (DTD en su sigla en inglés) es un diagnóstico psiquiátrico infantil propuesto para las secuelas psicopatológicas y del desarrollo de la victimización y el trauma del apego que se extiende más allá del trastorno de estrés postraumático (TEPT).
Objetivo: Determinar si un subgrupo de niños afectados por un trauma se caracteriza por síntomas de DTD que se extienden más allá o coexiste con los síntomas del trastorno de estrés postraumático (TEPT).
Método: Se realizaron análisis de clase latente (LCA en su sigla en inglés) centrados en la persona con datos de 507 niños (de 7 a 18 años de edad, (M = 12.11, DS = 2/92); 49% mujeres) remitidos al estudio por médicos pediátricos o de salud mental.
Resultados: Una solución de cuatro clases fue óptima (LMR = 398.264, p < .001; Entropía = .93): (1) combinado DTD + TEPT (n = 150); (2) DTD predominante (n = 156); (3) TEPT predominante (n = 54); (4) síntomas mínimos (n = 147). De acuerdo con investigaciones previas, la clase DTD + TEPT tenía más probabilidades de haber experimentado abuso emocional traumático y negligencia (X2(3) = 16.916 y 28.016, respectivamente, p < .001), y tenía la mayor comorbilidad psiquiátrica (F(3, 502) = 3.204, p < .05). Los miembros de la clase DTD predominante tenían más probabilidades de cumplir los criterios para el trastorno oposicionista desafiante (ODD en su sigla en inglés) (X2(3) = 84.66, p < .001).
Conclusión: Los síntomas de DTD pueden ocurrir con, o por separado de, los síntomas de TEPT. Los niños con síntomas de DTD + TEPT altos tenían una comorbilidad psiquiátrica extensa, mientras que aquellos con síntomas de DTD altos y síntomas mínimos de TEPT tenían muchas probabilidades de cumplir con los criterios para ODD. En la evaluación y tratamiento clínico y de investigación de niños con comorbilidad psiquiátrica compleja o problemas de comportamiento disruptivo, se deben considerar los síntomas de DTD, tanto junto con, como en ausencia de, síntomas de TEPT.
背景:发育性创伤障碍 (DTD) 是一种倡议的儿童精神病学诊断,用于治疗超出创伤后应激障碍 (PTSD) 受害程度和依恋创伤的精神病和发育后遗症。
目的:确定一个受创伤影响的儿童亚组是否具有超出创伤后应激障碍 (PTSD) 症状或与之并发的 DTD 症状。
方法:对 507 名转诊到心理健康或儿科医生的儿童(年龄 7-18 岁,(平均年龄 = 12.11,标准差 = 2/92);49% 女性)的数据进行了以人分类的潜在类别分析 (LCA)。
结果:四类解决方案是最佳的(LMR = 398.264,p < .001;熵 = .93):(1)DTD + PTSD 组合(n = 150); (2) 主要 DTD (n = 156); (3) 主要的 PTSD (n = 54); (4) 轻微症状 (n = 147)。与先前研究一致,DTD + PTSD 类最有可能经历过创伤性情绪虐待和忽视(分别地,X2(3) = 16.916 和 28.016,p < .001),并且有最多的精神并发症(F(3, 502) = 3.204, p < .05)。主要的 DTD 类人群最有可能符合对立违抗障碍 (ODD) 的标准 (X2(3) = 84.66, p < .001)。
结论:DTD 症状可能与 PTSD 症状同时出现,或与 PTSD 症状分开出现。高 DTD|+PTSD 症状的儿童具有广泛的精神并发症,而高 DTD 症状和少 PTSD 症状的儿童很可能符合 ODD 标准。在对患有复杂精神并发症或破坏性行为问题的儿童进行临床和研究评估和治疗时,无论是否存在 PTSD 症状,都应考虑 DTD 的症状。
Children who have experienced traumatic victimization (e.g. abuse, assault, exploitation, witnessing potentially life-threatening violence) and disruption in attachment bonding with primary caregivers (e.g. severe neglect or caregiver impairment, prolonged separation or loss) are at risk for internalizing and externalizing psychopathology that includes but extends beyond, posttraumatic stress disorder (PTSD) (Bremness & Polzin, Citation2014; Ford et al., Citation2018; Hansen et al., Citation2015; Khamis, Citation2019; Lyons-Ruth & Brumariu, Citation2020; Ma & Li, Citation2014; McLaughlin et al., Citation2014; Murphy et al., Citation2016; Schneider, Citation2020; Seay, Citation2020; Sierau et al., Citation2020; Spinazzola et al., Citation2018; Stolbach et al., Citation2013; van der Kolk et al., Citation2019; Villalta et al., Citation2018; Yoon, Citation2017; Yoon et al., Citation2017; Zhang et al., Citation2019). The complex biopsychosocial sequela of attachment and victimization trauma also overlap with but are not fully represented by many other child psychiatric disorders (Aldao et al., Citation2016; Beauchaine & Cicchetti, Citation2019; Conway et al., Citation2018; Heleniak et al., Citation2016; McLaughlin et al., Citation2020; Wade et al., Citation2020; Weissman et al., Citation2019; Weissman et al., Citation2020). Although PTSD often is comorbid with other child psychiatric disorders, many of these children do not meet criteria for PTSD (e.g. 14% in the DTD field trial studies; Ford et al., Citation2021; van der Kolk et al., Citation2019). Additionally, other children who are diagnosed with PTSD but have complex symptoms that extend beyond PTSD's classic symptoms may require adaptations to evidence-based PTSD treatments (Ford & Courtois, Citation2013).
To address this challenge, a complex PTSD (CPTSD) diagnosis was developed, validated for adults (Redican et al., Citation2021; Rod & & Schmidt, Citation2021), and included in the International Classification of Diseases, 11th Revision. Although CPTSD also has been validated with samples of children (Haselgruber et al., Citation2020a, Citation2020b; Tian et al., Citation2021), the ICD-11 CPTSD formulation is limited to emotion dysregulation, interpersonal detachment and low self-worth. Several other symptom domains (e.g. somatic, dissociation, externalizing/ disruptive behaviour) and aspects of relational and identified dysregulation (i.e. respectively, insecure/ disorganized attachment or relational enmeshment, and self-perception as irreparably damaged) warrant consideration for inclusion in a complex PTSD diagnosis for children based on research evidence that they often are a sequela of childhood victimization trauma (D'Andrea et al., Citation2012). Developmental Trauma Disorder (DTD) was designed as a clinical syndrome complementary with but extending beyond the original and ICD-11 PTSD formulation, including the full range of symptom domains identified in research on victimization and attachment trauma in childhood.
Two surveys of clinicians (DePierro et al., Citation2019; Ford et al., Citation2013) and two field trial studies have demonstrated DTD's construct, convergent and discriminant validity. In the field trial studies, a structured interview for DTD was validated, and three-factor analytically derived sets of symptoms have been identified and replicated (Ford et al., Citation2018; Ford et al., Citation2022). The first DTD domain is affective/somatic dysregulation (Criterion B), based on research and theory demonstrating that maladaptive emotion processing and emotion dysregulation constitute a link between childhood adversity and psychopathology (Aldao et al., Citation2016; Beauchaine & Cicchetti, Citation2019; Conway et al., Citation2018; Heleniak et al., Citation2016; McLaughlin et al., Citation2020; Weissman et al., Citation2019). Somatic dysregulation was included due to evidence that children often express distress indirectly through somatic complaints and somatoform symptoms (Agnafors et al., Citation2019). The second DTD domain, cognitive/behavioural dysregulation (Criterion C), includes symptoms referencing attentional preoccupation with or avoidance of awareness of threat (McLaughlin et al., Citation2020; Weissman et al., Citation2020) and behavioural disinhibition/dyscontrol associated with impaired executive functions and effortful control (Beauchaine & Cicchetti, Citation2019; Hankin et al., Citation2017; Huang-Pollock et al., Citation2017; Santens et al., Citation2020; Snyder et al., Citation2019; Wade et al., Citation2020). The third DTD domain, self and interpersonal dysregulation (Criterion D), includes extreme self-devaluation and self-ideal discrepancy (Mason et al., Citation2019; Schweizer et al., Citation2020), reactive aggressive and betrayal-based modes of relational engagement and social information processing (McLaughlin et al., Citation2020; Schweizer et al., Citation2020), and disorganized attachment, impaired empathy and relational enmeshment (Foxhall et al., Citation2019; Snyder et al., Citation2019).
In the field trial studies, DTD and PTSD were shown to frequently co-occur but to have unique as well as shared traumatic antecedents and comorbidities. DTD and PTSD both were associated with polyvictimization, but, unlike PTSD, DTD was consistently associated with victimization trauma (i.e. emotional abuse, family violence) and attachment trauma (i.e. separation from caregiver; caregiver impairment) and not with non-interpersonal trauma or sexual trauma (Spinazzola et al., Citation2018, Citation2021). DTD also was associated with a more complex pattern of psychiatric comorbidity than PTSD, including both internalizing (e.g. separation anxiety, panic) and externalizing (e.g. attention deficit hyperactivity disorder, oppositional defiant disorder) disorders (Ford et al., Citation2021; van der Kolk et al., Citation2019). Although DTD and PTSD often were present in combination, each syndrome occurred separately from the other in 15–20% of the field trial sample (Ford et al., Citation2018; Ford et al., Citation2022).
Despite the differences between DTD and PTSD in traumatic antecedents and psychiatric comorbidities, their frequent co-occurrence raises the question of whether DTD is fundamentally distinguishable from PTSD. DTD symptoms might be only a set of associated features of PTSD, as was true in the DSM-IV (van der Kolk et al., Citation2005). Alternately, DTD symptoms might simply be variants of the expanded set of core PTSD symptoms in the DSM-5 version of PTSD, because that expanded formulation includes symptoms from the domains of dysregulation represented in DTD (i.e. emotion dysregulation, somatization, dissociation, attention bias toward threat, behavioural dysregulation, altered self-perceptions, and problems in relationships). If DTD is largely a derivative or extension of PTSD, it is possible that cases in which DTD is identified and the criteria for PTSD are not met might be children with significant PTSD symptoms that simply narrowly fail to meet the threshold for a PTSD diagnosis. Thus, it is important to determine empirically whether DTD symptoms are best classified as secondary or associated features of PTSD, or as a distinct clinical syndrome.
One approach to evaluate DTD's distinguishability from PTSD, or lack thereof, is to find whether, in addition to a sub-group of children who have extensive symptoms only of PTSD (i.e. predominant PTSD), or of both PTSD and DTD (i.e. comorbid PTSD and DTD), there also is a distinct sub-group with prominent symptoms of DTD but minimal or limited symptoms of PTSD (i.e. predominant DTD). Person-centred research using latent class analysis has been used to empirically demonstrate the existence of sub-groups distinguished by the ICD-11 CPTSD Disturbances of Self-Organization (DSO) symptoms and relatively few classic PTSD symptoms, as well as other sub-groups that have substantial PTSD symptoms and minimal DSO symptoms, as well as combined PTSD/CPTSD sub-groups – both with adults (Cloitre et al., Citation2013; Cloitre et al., Citation2019; Hyland et al., Citation2020; Karatzias, Cloitre, et al., Citation2017; Karatzias, Shevlin, et al., Citation2017; Knefel & Lueger-Schuster, Citation2013) and with children (Haselgruber et al., Citation2020b; Perkonigg et al., Citation2016). If DTD has a similar relationship to PTSD as DSO has to PTSD in ICD-11 CPTSD, a sub-group with high levels of both DTD and PTSD symptoms (i.e. a DTD + PTSD class) should be identifiable apart from sub-groups in which only DTD or PTSD symptoms are predominant.
This study was designed to determine whether distinct sub-groups of children with predominant DTD, predominant PTSD, and combined PTSD + DTD symptom profiles can be identified, and if so, whether these sub-groups differ in their patterns of traumatic antecedents and internalizing and externalizing disorder comorbidity, or in their gender or racial/ethnic composition. We hypothesized that those distinct classes would be found and that the DTD-only and combined DTD + PTSD classes would be more strongly associated than a PTSD-only class (or a low DTD/PTSD symptoms class) with past victimization and attachment trauma and current externalizing disorder comorbidity in pair-wise comparisons. Based on item response theory analyses from the original and replication phase of this DTD field trial, which showed invariance in DTD symptoms across gender and race/ethnicity (Ford et al., Citation2018, Citation2022), we also hypothesized that the identified classes would not differ on gender or racial/ethnic composition.
2. Method
2.1. Participants
A convenience sample of families of 507 children and adolescents (M age = 12.11, SD = 2.92; 57% children ages 12 years or younger; 43% adolescents ages 13–18), including 244 female and 260 male participants (three did not report their gender) was recruited from 8 sites located in four geographical regions in the United States (Northeast, Mid-Atlantic, South and Midwest) through referrals from mental health, social, work and paediatric providers in those communities who offered all child/adolescent patients and their parent/guardian a written or oral introduction to the study during recruitment periods between September 2011 to August 2013 (Phase 1) and October 2014 to November 2016 (Phase 2). Inclusion criteria included the child's age 7–18 years old and the parent/guardian's and child's willingness to provide, respectively, consent or assent. There were no exclusion criteria for trauma history, treatment status/history, or current psychiatric symptoms or diagnoses. Participants’ ethnic/racial backgrounds were: 256 (50.5%) White, 101 (19.5%) Black or African American, 65 (12.8%) Hispanic, 11 (2.2%) Asian, 49 (9.5%) Biracial, and 13 (2.8%) other or unspecified.
Most participating children/adolescents were either in outpatient psychiatric (N = 347, 68.5%) or residential mental health (N = 113, 22.5%) treatment. Recruitment was done by providing staff in a variety of both public and private and public mental health and paediatric programs with oral and written descriptions of the study and asking them to invite parent/guardians of their child and adolescent clients/patients to participate. The families served by these programs represented the full range of socioeconomic status levels and racial and ethnic sub-groups consistent with each participating site.
2.2. Measures
Developmental Trauma Disorder Semi-Structured Interview (DTD-SI). DTD-SI items were initially designed by experts from the National Child Traumatic Stress Network. After iterative review/revisions, DTD-SI version 10.0 was used in the first phase of this study with N = 236 participants (Ford et al., Citation2018) and version 10.6 was used in the second phase with N = 271 participants (37). The DTD symptoms were identical in both versions of the DTD-SI. Version 10.0 allowed for both threshold and sub-threshold ratings, with either score counted as the symptom was present (12). Version 10.6 scored DTD symptoms only as present or absent, based on the symptom occurring with either evident distress or detachment (37). Fifteen DTD symptoms were scored (Present = 1, Absent = 0) representing three proposed DTD criteria: B (four emotion/somatic dysregulation symptoms), C (five attentional or behavioural dysregulation symptoms) and D (six interpersonal or self- dysregulation symptoms). Each symptom was assessed with a descriptive statement followed by optional probe questions. Three Criterion B symptoms, two Criterion C symptoms and two Criterion D symptoms were identified as optimal for a diagnosis of DTD (Ford et al., Citation2018, Citation2022). Inter-rater agreement across raters for a random sub-sample of interviews across all DTD-SI items was 87-100% (M = 93.0% agreement on child interviews: 93.5% agreement on parent/guardian interviews).
Traumatic Experiences Screening Instrument (TESI). This semi-structured interview assesses eight types of non-interpersonal trauma (accident, illness, death/loss) and 13 types of interpersonal victimization trauma (witness or direct exposure to violence or maltreatment). TESI items have shown evidence of retest reliability over a 2–4 month period (Kappa [K] = .50–.70) and criterion and predictive validity in psychiatric and paediatric samples (Daviss, Mooney, et al., Citation2000; Daviss, Racusin, et al., Citation2000). Binary variables were calculated for the child's lifetime history of trauma exposure to represent any occurrence of (1) non-interpersonal trauma (i.e. accident, illness, or disaster; A2 TESI1.1–1.5), (2) Traumatic loss (TESI_1_5h = 1 or TESI_1_6J = 1), (3) Physical abuse/assault trauma (TESI_2.1j = 1 or TESI_2.2j = 1 or TESI_2.3j = 1 or TESI_2.4j), (4) Witnessing traumatic family violence (TESI_3.1k = 1 or TESI_3.2z = 1), (5) Sexual trauma (TESI_5.1j = 1 or TESI_5.2j = 1), (6) Witnessing traumatic community violence (TESI_4.1k = 1 or TESI_4.2k = 1), (7) Traumatic separation from primary caregiver (TESI_1_7n = 1), (8) Traumatic impairment of primary caregiver (TESI_1.8h = 1 or TESI_1.9r = 1 or TESI_3.3j = 1). The TESI also assesses: (9) Emotional abuse (TESI_6.1hj = 1); (10) neglect (TESI_6.2k = 1), and (11) polyvictimization (i.e. 5 or more types of interpersonal trauma/adversity, #3–10 above). Inter-rater agreement for a random sub-sample of interviews on TESI composite scores was 88–100% (M = 97% agreement for both child and parent/guardian interviews).
Kiddie Schedule for Affective Disorders and Schizophrenia, Present/ Lifetime Version (KSADS/PL). This semi-structured interview assesses DSM-IV child psychiatric disorders with child and parent versions (Kaufman et al., Citation1996). PTSD symptoms were assessed with a module that assessed 17 symptoms (Present = 1, Absent = 0) in 3 symptom clusters: re-experiencing (5 items), avoidance (7 items) and arousal (5 items). Inter-rater agreement for a random sub-sample of interviews on K-SADS PTSD items was 81–100% (M = 85% and 89% agreement for child and parent/guardian interviews, respectively). Other child psychiatric disorders were scored as probable vs. absent with KSADS screening items. Inter-rater agreement across raters for other K-SADS diagnosis screens was 78–98% (M = 88% and 89% agreement for child and parent/guardian interviews, respectively).
2.3. Procedure
All study procedures were conducted following a protocol approved by the Institutional Review Board of the University of Connecticut Health Center (IE-11-096-2), with informed consent obtained by a parent/legal guardian and assent obtained from participating children.
Interviews were conducted with 245 parent-child dyads, 238 parents alone and alone with 24 adolescents. All parents who participated were aware of their child's trauma history and current symptoms. When children were interviewed with a parent, the child version of the interview (TESI, DTD, K-SADS) was used and parents were asked whether they agreed with the child's response or if they had a different answer than their child. Present (past 30 days) diagnoses were used for both DTD and PTSD. Symptoms were considered to be present and traumatic events were considered to have occurred if endorsed by either the parent or child (or both). To reduce the chance of bias leading to spurious correlations between DTD symptoms and either psychiatric symptoms (including PTSD) or trauma/adversity history, the K-SADS and TESI were administered prior to the DTD-SI in all cases.
Interviewers (N = 25) viewed simulated demonstration interviews conducted by expert assessors, then independently rated videotaped interviews until they achieved >80% agreement on trauma history, PTSD symptoms and psychiatric screening variables with expert ratings. They then conducted videotaped role-play interviews with >90% agreement with an independent expert's review required. Interviewers subsequently had their first two study interview tapes reviewed by an independent expert with >80% agreement on the primary interview variables required before conducting further interviews. Approximately every fifth interview conducted by all interviewers was randomly selected for independent re-rating on the DTD-SI, TESI and K-SADS: 73 interviews with a parent or guardian alone, and 36 with a child alone or with an adult.
2.4. Statistical analyses
Descriptive statistics were conducted in IBM SPSS v. 26. A latent class analysis (LCA) was performed to determine the number of heterogeneous groups with homogeneity within each group based on 20 symptoms of PTSD and 15 symptoms of DTD. LCA estimates the posterior probabilities of class membership or size of the class (Nylund et al., Citation2007). Better fitting models are reflected by significant p values for the Bootstrap Likelihood Ratio Test (BLRT) and Lo–Mendell–Rubins likelihood ratio test (LMR), and lower values on the Akaike Information Criteria (AIC), the Bayesian Information Criteria (BIC), and the sample size adjusted BIC (Adjusted BIC) and higher entropy values (i.e. closer to 1). The LCA analysis was done with Mplus 8.4 software employing maximum likelihood estimation with robust standard errors (MLR). To avoid solutions based on local maxima, 500 random sets of starting values were used in the initial stage and 100 optimizations were used in the final stage of convergence. Missing values were minimal in the range of .2% to 1.2% and full information maximum likelihood (FIML) was used to estimate the parameters using all available information.
Latent class membership was exported into the SPSS software and treated as an observed categorical variable. To examine differences across the classes on race, gender, trauma types, and psychiatric diagnoses, chi-square difference testing was conducted. The standardized residuals were calculated for each class, with values ≥ +2 indicating that the observed cell frequency or number of participants endorsing the trauma type or diagnoses, or their race and gender was greater than the expected frequency, and values ≤–2 indicating the number of participants endorsing a specific study variable was less than the expected frequency. Next, differences across the latent classes on exposure to the total number of types of interpersonal trauma, total number of K-SADS diagnoses and DSM-IV-TR PTSD cluster scores were calculated using ANOVA, and pairwise comparisons were conducted. Bonferroni correction for multiple statistical tests was applied to reduce the risk for Type I error.
3. Results
On average child participants had experienced almost 4 types of traumatic stressors or adversity (M = 3.89, SD = 2.34, Range = 0–10). Most had experienced non-interpersonal trauma (i.e. traumatic accident, illness or disaster 74%) and 48.5% had had traumatic losses. Physical abuse/assault (52.7%) was the most often experienced interpersonal trauma, followed by family violence (38.5%), sexual trauma (20.7%) and community violence (17.6%). Other adversities included caregiver separation (45.0%) or impairment (41.6%), emotional abuse (19.9%) and neglect (18.7%). Polyvictimization (exposure to five or more types of traumatic stressors or adversity) had occurred for 13.6% of the child participants.
Nearly one in five child participants met criteria for DTD and PTSD (n = 90; 18%), one in seven met criteria for DTD but not PTSD (n = 72; 14%) and one in six met criteria for PTSD but not DTD (n = 86; 17.0%). Regarding psychiatric morbidity, most participating children (n = 438; 86%) screened positive for at least one internalizing disorder (i.e. depression, bipolar disorder, panic disorder, social anxiety disorder generalized anxiety disorder or obsessive-compulsive disorder) and 346 (68%) screening positive for at least one externalizing disorder (i.e. either conduct disorder, ADHD or oppositional defiant disorder) (see ).
Table 1. Probable DSM-IV psychiatric disorders, and symptoms of PTSD and DTD.
3.1. Latent classes based on DTD and PTSD symptoms
A series of LCA models with one to six-class solutions were estimated. A four-class solution was found to be optimal based on several goodness-of-fit indices () and meaningfulness of the classes. The BLRT was significant for all the latent class solutions but the LMR likelihood ratio test favoured a four-class solution and an entropy of .93 was acceptable and suggested a clear delineation of classes. The average posterior probability for most likely latent class membership ranged from .936 to .974 for the four-class solution, which suggests good class determination (60). The three information criteria – AIC, BIC, sample size adjusted BIC – continued to decrease with each added class. Notably, the decrease or change in information criteria was small. When we inspected visually for an elbow or point of diminishing returns in model fit, the four-class solution appeared to be the optimal and meaningful solution. For instance, although the BIC of the five-class solution was lower than that of the four-class solution, the difference between the classes was not strong (i.e. ΔBIC = 3.792) (60). The five-class solution merely bifurcated the DTD + PTSD class found in the four-class solution, as per probabilities of symptoms (higher vs. moderate). A six-class solution was tested and found to marginally reduce BIC (ΔBIC = 11.671), but the additional class was uninterpretable because it resembled the predominantly PTSD class from the four-class solution albeit with lower probabilities and moderate probability of affect dysregulation symptoms (i.e. PTSD D1/D2, DTD B1). Thus a four-class solution was selected as the optimal fit to the data.
Table 2. Fit indices for the latent class models with one to six classes.
The endorsement probabilities across the four latent classes are presented in . Based on the probabilities of endorsement of PTSD and DTD symptoms, the four latent classes were labelled. Class 1 (n = 150; 70 male; 70 White; 36 Black) was labelled ‘DTD + PTSD’ as it had the highest probability of symptoms of both DTD and PTSD symptoms. Class 2 (n = 156; 78 male; 89 White; 21 Black) was labelled ‘Predominantly PTSD’ (pPTSD), as its members had high probabilities of PTSD symptoms (albeit lower than for the DTD + PTSD class), and low-to-moderate probabilities of DTD symptoms. Class 3 (n = 54; 39 male; 31 White; 12 Black) was labelled ‘Predominantly DTD’ (pDTD) as its members had a very low probability of any PTSD symptoms and high probabilities of DTD symptoms comparable to those of the DTD + PTSD class. With relatively low probabilities of symptoms of both DTD and PTSD, Class 4 (n = 147; 74 male; 66 White; 32 Black) was termed as ‘Minimal symptoms.’
3.2. Latent class differences across gender, race, and trauma types
Examination of the chi-square differences and standardized residuals () indicated that males were over-represented in the pDTD class. No differences were found in distributions of race (white vs. non-white; black vs. non-black; Hispanic vs. non-Hispanic) in the four latent classes. With regard to trauma types (), exposure to traumatic emotional abuse and traumatic neglect were over-represented in the DTD + PTSD class based on standardized residuals. Based on the pairwise comparisons, the DTD + PTSD class had a higher mean number of types of past trauma than the minimal symptoms class, but did not differ from the pDTD or pPTSD classes on cumulative trauma exposure.
Table 3. Distribution of gender and race across the four latent classes.
Table 4. Distribution of trauma/adversity types across the four latent classes.
3.3. Psychiatric diagnoses across the latent classes
When examining the associations between the four classes with diagnoses of DTD and PTSD and the psychiatric disorders screened by the K-SADS (), the DTD + PTSD class had the most evidence of comorbidity (considering all K-SADS diagnoses except PTSD). PTSD diagnoses also were over-represented in the DTD + PTSD class and under-represented in the pDTD class, consistent with the view that DTD is not simply a derivative or extension of PTSD. DTD occurred most often in the DTD + PTSD and pDTD classes, but not with sufficient frequency to locate the DTD diagnosis in those classes with statistical significance.
Table 5. Latent class differences and comparisons across child psychiatric disorders.
Pairwise comparison of the average of the number of diagnoses other than DTD indicated the DTD + PTSD class had the highest mean score compared to the other latent classes, and the pPTSD and p DTD classes were higher than the minimal symptoms class. In the DTD + PTSD class, participants with at least one internalizing disorder as well as each of the three individual externalizing disorders (attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder) were over-represented, with one exception: oppositional defiant disorder was over-represented in the pDTD class. PTSD was under-represented in the pDTD class as hypothesized. PTSD and each internalizing disorder with one exception (obsessive-compulsive disorder) were over-represented in the DTD + PTSD class (i.e. depression, bipolar disorder, psychosis, panic disorder, separation anxiety disorder, phobia and generalized anxiety disorder). No psychiatric disorder was under- or over-represented in the pPTSD class.
The DTD + PTSD class also had the most symptoms on average in each PTSD symptom cluster, followed by the pPTSD class (see ). Consistent with the latent class profiles, the pDTD and minimal symptom classes had the lowest endorsement of PTSD symptoms in each of the PTSD symptom clusters and overall.
Table 6. Latent class differences on PTSD symptom count scores.
4. Discussion
As hypothesized, distinct sub-groups of children were identified based on profiles of DTD and PTSD symptoms, including a combined DTD + PTSD class and classes characterized predominantly by DTD (pDTD) or PTSD (pPTSD) symptoms. Also as hypothesized, members of the DTD + PTSD class had the highest likelihood of having experienced victimization (i.e. emotional abuse) and attachment disruption (i.e. neglect). Contrary to hypotheses, there was no difference between the pDTD and pPTSD classes on any traumatic or adversity antecedents. Thus the proposed antecedents of DTD (i.e. both victimization and attachment disruption) may apply primarily when DTD occurs in combination with PTSD. This is an interesting parallel to the structure proposed for CPTSD, in which the complex traumatic stress symptoms (i.e. DSO) must be accompanied by PTSD symptoms to qualify for a diagnosis of CPTSD (Cloitre et al., Citation2013; Hyland et al., Citation2020).
Also as hypothesized, DTD + PTSD class members had the greatest extent of comorbidity across both internalizing and externalizing disorders, with on average more than five comorbid psychiatric disorders other than PTSD, reflecting an extremely heavy burden of comorbidity. This particularly high amount of comorbidity (including severe emotional disturbance such as bipolar and psychotic disorders) is noteworthy given that the overall sample was comprised of high-risk children, most of whom were in mental health treatment, had extensive trauma histories, and had multiple comorbidities (i.e. even the minimal symptoms class had on average three comorbid psychiatric disorders). Contrary to hypotheses, the pDTD class did not have more extensive comorbidity overall than the pPTSD class. However, study hypotheses were supported by the finding that the pDTD class had more extensive comorbidity than the minimal symptoms class, and that a key externalizing disorder (oppositional defiant disorder; ODD) was over-represented in the pDTD class. Thus the comorbidity findings indicate that, parallel to the structure of CPTSD, a combination of DTD and PTSD symptoms is associated with the greatest degree of psychiatric comorbidity. In addition, the finding that DTD symptoms co-occur with ODD (and PTSD symptoms do not) suggest that DTD's behavioural dysregulation symptoms may be important to fully account for the impact of victimization and disrupted attachment,
As hypothesized, the classes did not differ with respect to gender or race and ethnicity. This result, along with prior findings showing that DTD items were comparably informative across gender and race/ethnicity (Ford et al., Citation2018; Ford et al., Citation2022), indicates that children with DTD symptoms do not differ from other children who also are receiving mental health treatment in the distribution of gender or race/ethnicity. Implications of study findings for the assessment and treatment of trauma-related psychopathology, and for further research, now will be discussed.
The existence of distinct pPTSD and pDTD classes suggests that the classes do not simply represent a hierarchy of levels of severity of PTSD. This is consistent with findings from studies showing that distinct sub-groups of adults can be identified with PTSD symptoms alone, DSO symptoms alone, or a combination of PTSD and DSO symptoms, in adults (Brewin et al., Citation2017) and adolescents (Kazlauskas et al., Citation2020). If only the DTD + PTSD, pPTSD, and minimal symptoms classes are considered, there could be a severity continuum from highest to lowest PTSD severity, similar to findings from a study with adults (Wolf et al., Citation2015)and three studies assessing CPTSD with children in foster care (Haselgruber et al., Citation2020b), receiving trauma-focused cognitive behaviour therapy (Sachser et al., Citation2017), or exposed to mass violence (Crum et al., Citation2018). However, the presence of a pDTD class indicates that there is more than just PTSD severity to consider when assessing posttraumatic symptomatology in children.
Thus, there may be a distinct group of trauma-impacted children who do not display significant PTSD symptoms but who could be identified with an assessment of DTD symptoms. One possible explanation is that these may be children who have experienced a combination of chronic severe deprivation and threat (McLaughlin et al., Citation2014, Citation2020) and subsequently suffer from a sense of diffuse distress that does not include PTSD's classic intrusive re-experiencing or avoidance symptom but instead manifests as multi-domain dysregulation. This parallels the findings of a distinct DSO sub-group in CPTSD research with trauma-exposed adults (Bottche et al., Citation2018; Brewin et al., Citation2017). Assessing DTD symptoms may enable clinicians and researchers to identify trauma-impacted children who would otherwise not receive evidence-based trauma-focused treatment due to not meeting the criteria for PTSD. Assessment of DSM-5 PTSD, which was not done in this study because only the DSM-IV version was available when the study was designed, should be done in future studies to determine whether DTD symptoms can identify a distinct sub-group separately from children who meet the more extensive PTSD symptom set in DSM-5. For example, PTSD in the DSM-5 adds several negative alterations in cognition and mood symptoms similar to the emotion dysregulation symptoms in DTD (and in ICD-11 DSO), as well as self-harm and aggression symptoms similar to some of DTD's behavioural dysregulation symptoms.
The over-representation of ODD in the pDTD class suggests that some children who have a negative prognosis for psychiatric treatment and potentially severe lifelong sociolegal problems as a result of this disorder (Bonham et al., Citation2021; McKinney et al., Citation2021; Mikolajewski et al., Citation2017; Ollendick et al., Citation2018) may be impaired by trauma-related distress and reactions. In the DTD field trial study, ODD was uniquely associated with DTD and not with PTSD (Ford et al., Citation2021). Thus, DTD may capture symptoms associated with oppositional-defiance (e.g. risk taking, betrayal-based schemas, difficulty initiating or sustaining goal-directed behaviour, attachment disorganization, impaired psychological boundaries and impaired empathy) that would not be attributed to trauma if PTSD symptoms appear mild or absent. However, oppositional-defiant youths often have clinically significant trauma-related symptoms that are unassessed and untreated (Ford et al., Citation1999; Ford et al., Citation2000).
Youth with externalizing behaviour problems also often are considered refractory to psychological interventions and destined to be on an antisocial trajectory as a result of personality traits described as callous and unemotional (CU) (Widom et al., Citation2020). However, exposure to maltreatment has been shown to constitute a risk factor for CU (Widom et al., Citation2020) and there is evidence that adolescents may acquire what appears to be CU when they are experiencing post-traumatic emotional numbing (Kerig et al., Citation2012). Thus, although PTSD and ODD have been found to often occur comorbidly (Ford et al., Citation2000), DTD may provide a means of identifying and targeting trauma-focused treatment for youths who have conduct problems but do not meet the criteria for a PTSD diagnosis. Study findings thus point to a need for trauma-focused clinical and research assessment including not only PTSD but also DTD symptoms, with youth who present with ODD-related disruptive behaviour problems.
While the current findings parallel those of studies investigating the relationship of ICD-11 CPTSD and its DSO features with classic PTSD, it is important to note that DTD is not simply a childhood version of CPTSD. Two of the three criterion domains of DTD are similar to the DSO criterion domains, with both formulations including an emotion dysregulation criterion domain and criteria that focus on trauma-related alterations in interpersonal functioning and sense of self. However, CPTSD separates the relational and self-concept symptoms in two criterion domains while DTD combines them in a single criterion set based on the strong linkage between attachment security and self-esteem (Pinto et al., Citation2015) and self-regulation (Pallini et al., Citation2018) in childhood and adolescence. DTD also includes somatic dysregulation along with emotion dysregulation in a criterion domain reflecting the somatic manifestations of traumatic stress adaptations in childhood (Espejo-Siles et al., Citation2020) – which can extend into adulthood (Kuhar & Zager Kocjan, Citation2021). Although not included in CPTSD, dissociation is represented in DTD's emotion/somatic dysregulation domain in light of the evidence of a confluence of abuse and disorganized attachment with emotion dysregulation and dissociation in childhood (Hebert et al., Citation2020) and adolescence (Henschel et al., Citation2019). DTD also includes symptoms are related to externalizing behaviour problems which are not included in CPTSD/DSO. Therefore, research is needed in which CPTSD and DTD are simultaneously assessed, to determine whether DTD and DSO symptoms (a) identify similar or different sub-groups of trauma-impacted children and (b) have similar or different patterns of trauma history and psychiatric comorbidity.
Study findings also suggest that an adaptation of evidence-based screeners for PTSD (e.g. Lang & Connell, Citation2018) including DTD symptoms would be worth investigating. Such a screen could enable children's mental health providers to identify children who would benefit from trauma-focused treatment but do not screen positive for PTSD (i.e. the pDTD class). Such screening could also identify children with severe symptoms of both DTD and PTSD (i.e. the DTD + PTSD class), who might benefit from DTD-related adaptations to evidence-based PTSD treatments (Ford & Courtois, Citation2013; Hodgdon, Spinazzola, et al., Citation2018).
This study had limitations that should be considered when interpreting the results. A convenience sample was enrolled, although participants were drawn from intensive outpatient and residential mental health treatment programs in several geographic regions in the USA and had extensive psychiatric morbidity and trauma histories consistent with sub-populations in child mental health treatment (Basu et al., Citation2020; Ford et al., Citation1999). Trauma/adversity history was assessed with the well-validated and widely used TESI semi-structured interview measure, but may be subject to retrospective bias (Widom, Citation2019) and may have false negatives when based only on either child and parent reports but not both (Hungerford et al., Citation2010; Stover et al., Citation2010). Precise data on the age of onset, chronicity and other trauma exposure variables associated with youth outcomes (Hodgdon, Liebman, et al., Citation2018; Hodgdon, Spinazzola, et al., Citation2018) could not be reported, although in all cases the identified traumas had occurred prior to the current (past month) time frame used to assess symptoms. Both symptoms and trauma/adversity exposure may have been under-reported by children due to reluctance to disclose in a caregiver's presence or due to caregivers’ lack of knowledge of events or of the internal state of the child. PTSD was assessed based on the DSM-IV criteria because the K-SADS for DSM-5 was not yet available. Disrupted attachment was assessed indirectly based on neglect and caregiver separation and impairment rather than by direct assessment of child-caregiver attachment bonding.
Additionally, the use of latent classes as an observed variable to assess differences across trauma types and diagnoses assumes class membership is deterministic when in actuality each individual has a probability of being a member in each class rather than a certain membership in one class. Analyses were initially done to identify class membership on a probabilistic basis using a 3-step procedure, but the models did not converge. Results of those alternative analyses therefore are not reported (but are available from the second author).
In conclusion, study findings indicate that distinct sub-groups of children in mental health treatment can be identified empirically when the symptoms of both DTD and PTSD are assessed. Children with the most extensive psychiatric comorbidity tended to have symptoms of DTD as well as PTSD, both of which should be addressed with trauma-focused treatment in addition to other evidence-based treatment for their typically substantial load of psychiatric comorbidities. Other children were identified with low levels of PTSD symptoms but high levels of DTD symptoms – and often carrying an ODD diagnosis; this sub-group may represent an important unrecognized cohort of children who could benefit from trauma-focused treatment in addition to evidence-based behaviour management and mental health intervention. Further research on the aetiology, diagnostic utility, clinical epidemiology and course, and response to trauma-focused and other evidence-based mental health treatments of DTD also clearly is warranted.
Author contributions
Julian Ford and Joseph Spinazzola designed the original project and conducted data collection, all authors designed the study data analyses, Ruby Charak and Mark Shevlin conducted data analysis, Julian Ford wrote the manuscript, Thanos Karatzias provided consultation on CPTSD research, and all authors reviewed, edited, and approved the manuscript.
Acknowledgements
The study was funded by the Lookout Foundation, Joseph Spinazzola, Ph.D., and Julian Ford, Ph.D., Principal Investigators. No organizational or individual funder had any role in the conduct or publication of this study. The authors gratefully acknowledge the contributions of the National Child Traumatic Stress Network Developmental Trauma Disorder Work Group, co-led by Robert Pynoos, M.D. (UCLA Department of Psychiatry) and Bessel van der Kolk, M.D., to the conceptual framework and initial item development of the Developmental Trauma Disorder Semi-structured Interview (DTD-SI), and the field site coordinators and interviewers who accomplished the data collection for this study.
Disclosure statement
Julian Ford was a consultant to Advanced Trauma Solutions Professionals Inc. (the licensed distributor of the TARGET© intervention copyrighted by the University of Connecticut) in the past 2 years. No other author reports any conflict of interest.
Data availability statement
Per the conditions of Human Subjects Research (IRB) approval, encrypted study data are available upon request from the first author, [email protected].
References
- Agnafors, S., Norman Kjellstrom, A., Torgerson, J., & Rusner, M. (2019). Somatic comorbidity in children and adolescents with psychiatric disorders. European Child & Adolescent Psychiatry, 28(11), 1517–1525. https://doi.org/10.1007/s00787-019-01313-9
- Aldao, A., Gee, D. G., De Los Reyes, A., & Seager, I. (2016). Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Development and Psychopathology, 28(4pt1), 927–946. https://doi.org/10.1017/S0954579416000638
- Basu, A., Farkas, D. K., Jiang, T., Koenen, K. C., Lash, T. L., Sorensen, H. T., & Gradus, J. L. (2020). Incident psychiatric comorbidity following stress disorder diagnoses in Danish school-aged children: Prospective population-based study. The British Journal of Psychiatry, 217(1), 377–382. https://doi.org/10.1192/bjp.2019.247
- Beauchaine, T. P., & Cicchetti, D. (2019). Emotion dysregulation and emerging psychopathology: A transdiagnostic, transdisciplinary perspective. Development and Psychopathology, 31(3), 799–804. https://doi.org/10.1017/S0954579419000671
- Bonham, M. D., Shanley, D. C., Waters, A. M., & Elvin, O. M. (2021). Inhibitory control deficits in children with oppositional defiant disorder and conduct disorder compared to attention deficit/hyperactivity disorder: A systematic review and meta-analysis. Research on Child and Adolescent Psychopathology, 49(1), 39–62. https://doi.org/10.1007/s10802-020-00713-9
- Bottche, M., Ehring, T., Kruger-Gottschalk, A., Rau, H., Schafer, I., Schellong, J., Dyer, A., & Knaevelsrud, C. (2018). Testing the ICD-11 proposal for complex PTSD in trauma-exposed adults: factor structure and symptom profiles. European Journal of Psychotraumatology, 9(1), 1512264. https://doi.org/10.1080/20008198.2018.1512264
- Bremness, A., & Polzin, W. (2014). Commentary: Developmental trauma disorder: A missed opportunity in DSM V. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 23(2), 142–145. http://www.ncbi.nlm.nih.gov/pubmed/24872830.
- Brewin, C. R., Cloitre, M., Hyland, P., Shevlin, M., Maercker, A., Bryant, R. A., Humayun, A., Jones, L. M., Kagee, A., Rousseau, C., Somasundaram, D., Suzuki, Y., Wessely, S., van Ommeren, M., & Reed, G. M. (2017). A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clinical Psychology Review, 58, 1–15. https://doi.org/10.1016/j.cpr.2017.09.001
- Cloitre, M., Garvert, D. W., Brewin, C. R., Bryant, R. A., & Maercker, A. (2013). Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology, 4(1), 20706. https://doi.org/10.3402/ejpt.v4i0.20706
- Cloitre, M., Hyland, P., Bisson, J. I., Brewin, C. R., Roberts, N. P., Karatzias, T., & Shevlin, M. (2019). ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder in the United States: A population-based study. Journal of Traumatic Stress, 32(6), 833–842. https://doi.org/10.1002/jts.22454
- Conway, C. C., Raposa, E. B., Hammen, C., & Brennan, P. A. (2018). Transdiagnostic pathways from early social stress to psychopathology: A 20-year prospective study. Journal of Child Psychology and Psychiatry, 59(8), 855–862. https://doi.org/10.1111/jcpp.12862
- Crum, K. I., Cornacchio, D., Coxe, S., Green, J. G., & Comer, J. S. (2018). A latent profile analysis of co-occurring youth posttraumatic stress and conduct problems following community trauma. Journal of Child and Family Studies, 27(11), 3638–3649. https://doi.org/10.1007/s10826-018-1205-2
- D'Andrea, W., Ford, J. D., Stolbach, B., Spinazzola, J., & van der Kolk, B. A. (2012). Understanding interpersonal trauma in children: Why we need a developmentally appropriate trauma diagnosis. American Journal of Orthopsychiatry, 82(2), 187–200. https://doi.org/10.1111/j.1939-0025.2012.01154.x
- Daviss, W. B., Mooney, D., Racusin, R., Ford, J. D., Fleischer, A., & McHugo, G. J. (2000). Predicting posttraumatic stress after hospitalization for pediatric injury. Journal of the American Academy of Child & Adolescent Psychiatry, 39(5), 576–583. https://doi.org/10.1097/00004583-200005000-00011
- Daviss, W. B., Racusin, R., Fleischer, A., Mooney, D., Ford, J. D., & McHugo, G. J. (2000). Acute stress disorder symptomatology during hospitalization for pediatric injury. Journal of the American Academy of Child & Adolescent Psychiatry, 39(5), 569–575. https://doi.org/10.1097/00004583-200005000-00010
- DePierro, J., D'Andrea, W., Spinazzola, J., Stafford, E., van Der Kolk, B., Saxe, G., Stolbach, B., McKernan, S., & Ford, J. D. (2022). Beyond PTSD: Client presentations of developmental trauma disorder from a national survey of clinicians. Psychological Trauma: Theory, Research, Practice, and Policy, 14(7), 1167–1174. https://doi.org/10.1037/tra0000532
- Espejo-Siles, R., Zych, I., & Llorent, V. J. (2020). Empathy, social and emotional competencies, bullying perpetration and victimization as longitudinal predictors of somatic symptoms in adolescence. Journal of Affective Disorders, 271, 145–151. https://doi.org/10.1016/j.jad.2020.03.071
- Ford, J. D., & Courtois, C. A. (2013). Treating complex traumatic stress disorders in children and adolescents: Scientific foundations and therapeutic models. Guilford.
- Ford, J. D., Grasso, D., Greene, C., Levine, J., Spinazzola, J., & van der Kolk, B. (2013). Clinical significance of a proposed developmental trauma disorder diagnosis. The Journal of Clinical Psychiatry, 74(8), 841–849. https://doi.org/10.4088/JCP.12m08030
- Ford, J. D., Racusin, R., Daviss, W. B., Ellis, C. G., Thomas, J., Rogers, K., Reiser, J., Schiffman, J., & Sengupta, A. (1999). Trauma exposure among children with oppositional defiant disorder and attention deficit-hyperactivity disorder. Journal of Consulting and Clinical Psychology, 67(5), 786–789. http://www.ncbi.nlm.nih.gov/pubmed/10535245. doi:10.1037/0022-006X.67.5.786
- Ford, J. D., Racusin, R., Ellis, C. G., Daviss, W. B., Reiser, J., Fleischer, A., & Thomas, J. (2000). Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment, 5(3), 205–217. http://www.ncbi.nlm.nih.gov/pubmed/11232267. doi:10.1177/1077559500005003001
- Ford, J. D., Spinazzola, J., & van der Kolk, B. (2021). Psychiatric comorbidity of developmental trauma disorder and posttraumatic stress disorder: findings from the DTD field trial replication (DTDFT-R). European Journal of Psychotraumatology, 12(1), 1929028. https://doi.org/10.1080/20008198.2021.1929028
- Ford, J. D., Spinazzola, J., van der Kolk, B., & Chan, G. (2022). Toward an empirically based developmental trauma disorder diagnosis and semi-structured interview for children: The DTD field trial replication. Acta Psychiatrica Scandinavica, 145(6), 628–639. https://doi.org/10.1111/acps.13424
- Ford, J. D., Spinazzola, J., van der Kolk, B., & Grasso, D. (2018). Toward an empirically-based developmental trauma disorder diagnosis for children: Factor structure, item characteristics, reliability, and validity of the developmental trauma disorder semi-structured interview (DTD-SI). Journal of Clinical Psychiatry, 79(5), e1–e9. https://doi.org/10.4088/JCP.17m11675
- Foxhall, M., Hamilton-Giachritsis, C., & Button, K. (2019). The link between rejection sensitivity and borderline personality disorder: A systematic review and meta-analysis. British Journal of Clinical Psychology, 58(3), 289–326. https://doi.org/10.1111/bjc.12216
- Hankin, B. L., Davis, E. P., Snyder, H., Young, J. F., Glynn, L. M., & Sandman, C. A. (2017). Temperament factors and dimensional, latent bifactor models of child psychopathology: Transdiagnostic and specific associations in two youth samples. Psychiatry Research, 252, 139–146. https://doi.org/10.1016/j.psychres.2017.02.061
- Hansen, M., Hyland, P., Armour, C., Shevlin, M., & Elklit, A. (2015). Less is more? Assessing the validity of the ICD-11 model of PTSD across multiple trauma samples. European Journal of Psychotraumatology, 6, 28766. https://doi.org/10.3402/ejpt.v6.28766
- Haselgruber, A., Solva, K., & Lueger-Schuster, B. (2020a). Symptom structure of ICD-11 complex posttraumatic stress disorder (CPTSD) in trauma-exposed foster children: Examining the International Trauma Questionnaire - Child and Adolescent Version (ITQ-CA). European Journal of Psychotraumatology, 11(1), 1818974. https://doi.org/10.1080/20008198.2020.1818974
- Haselgruber, A., Solva, K., & Lueger-Schuster, B. (2020b). Validation of ICD-11 PTSD and complex PTSD in foster children using the International Trauma Questionnaire. Acta Psychiatrica Scandinavica, 141(1), 60–73. https://doi.org/10.1111/acps.13100
- Hebert, M., Langevin, R., & Charest, F. (2020). Disorganized attachment and emotion dysregulation as mediators of the association between sexual abuse and dissociation in preschoolers. Journal of Affective Disorders, 267, 220–228. https://doi.org/10.1016/j.jad.2020.02.032
- Heleniak, C., Jenness, J. L., Stoep, A. V., McCauley, E., & McLaughlin, K. A. (2016). Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research, 40(3), 394–415. https://doi.org/10.1007/s10608-015-9735-z
- Henschel, S., Doba, K., & Nandrino, J. L. (2019). Emotion regulation processes and psychoform and somatoform dissociation in adolescents and young adults with cumulative maltreatment. Journal of Trauma & Dissociation, 20(2), 197–211. https://doi.org/10.1080/15299732.2018.1502714
- Hodgdon, H. B., Liebman, R., Martin, L., Suvak, M., Beserra, K., Rosenblum, W., & Spinazzola, J. (2018). The effects of trauma type and executive dysfunction on symptom expression of polyvictimized youth in residential care. Journal of Traumatic Stress, 31(2), 255–264. https://doi.org/10.1002/jts.22267
- Hodgdon, H. B., Spinazzola, J., Briggs, E. C., Liang, L. J., Steinberg, A. M., & Layne, C. M. (2018). Maltreatment type, exposure characteristics, and mental health outcomes among clinic referred trauma-exposed youth. Child Abuse & Neglect, 82, 12–22. https://doi.org/10.1016/j.chiabu.2018.05.021
- Huang-Pollock, C., Shapiro, Z., Galloway-Long, H., & Weigard, A. (2017). Is poor working memory a transdiagnostic risk factor for psychopathology? Journal of Abnormal Child Psychology, 45(8), 1477–1490. https://doi.org/10.1007/s10802-016-0219-8
- Hungerford, A., Ogle, R. L., & Clements, C. M. (2010). Children's exposure to intimate partner violence: Relations between parent-child concordance and children's adjustment. Violence and Victims, 25(2), 185–201. https://doi.org/10.1891/0886-6708.25.2.185
- Hyland, P., Karatzias, T., Shevlin, M., Cloitre, M., & Ben-Ezra, M. (2020). A longitudinal study of ICD-11 PTSD and complex PTSD in the general population of Israel. Psychiatry Research, 286, 112871. https://doi.org/10.1016/j.psychres.2020.112871
- Karatzias, T., Cloitre, M., Maercker, A., Kazlauskas, E., Shevlin, M., Hyland, P., Bisson, J. I., Roberts, N. P., & Brewin, C. R. (2017). PTSD and Complex PTSD: ICD-11 updates on concept and measurement in the UK, USA, Germany and Lithuania. European Journal of Psychotraumatology, 8(sup7), 1418103. https://doi.org/10.1080/20008198.2017.1418103
- Karatzias, T., Shevlin, M., Fyvie, C., Hyland, P., Efthymiadou, E., Wilson, D., Roberts, N., Bisson, J. I., Brewin, C. R., & Cloitre, M. (2017). Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ). Journal of Affective Disorders, 207, 181–187. https://doi.org/10.1016/j.jad.2016.09.032
- Kaufman, J., Birmaher, B., Brent, D., Rao, U., & Ryan, N. (1996). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of Clinical Child and Adolescent Psychology, 36(7), 980–988. doi:10.1097/00004583-199707000-00021
- Kazlauskas, E., Zelviene, P., Daniunaite, I., Hyland, P., Kvedaraite, M., Shevlin, M., & Cloitre, M. (2020). The structure of ICD-11 PTSD and Complex PTSD in adolescents exposed to potentially traumatic experiences. Journal of Affective Disorders, 265, 169–174. https://doi.org/10.1016/j.jad.2020.01.061
- Kerig, P. K., Bennett, D. C., Thompson, M., & Becker, S. P. (2012). “Nothing really matters”: Emotional numbing as a link between trauma exposure and callousness in delinquent youth. Journal of Traumatic Stress, 25(3), 272–279. https://doi.org/10.1002/jts.21700
- Khamis, V. (2019). Posttraumatic stress disorder and emotion dysregulation among Syrian refugee children and adolescents resettled in Lebanon and Jordan. Child Abuse & Neglect, 89, 29–39. https://doi.org/10.1016/j.chiabu.2018.12.013
- Knefel, M., & Lueger-Schuster, B. (2013). An evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse. European Journal of Psychotraumatology, 4(1), 22608. https://doi.org/10.3402/ejpt.v4i0.22608
- Kuhar, M., & Zager Kocjan, G. (2021). Adverse childhood experiences and somatic symptoms in adulthood: A moderated mediation effects of disturbed self-organization and resilient coping. Psychological Trauma: Theory, Research, Practice, and Policy, https://doi.org/10.1037/tra0001040
- Lang, J. M., & Connell, C. M. (2018). The child trauma screen: A follow-up validation. Journal of Traumatic Stress, 31(4), 540–548. https://doi.org/10.1002/jts.22310
- Lyons-Ruth, K., & Brumariu, L. E. (2021). Emerging child competencies and personality pathology: Toward a developmental cascade model of BPD. Current Opinion in Psychology, 37, 32–38. https://doi.org/10.1016/j.copsyc.2020.07.004
- Ma, E. Y., & Li, F. W. (2014). Developmental trauma and its correlates: A study of Chinese children with repeated familial physical and sexual abuse in Hong Kong. Journal of Traumatic Stress, 27(4), 454–460. https://doi.org/10.1002/jts.21944
- Mason, T. B., Smith, K. E., Engwall, A., Lass, A., Mead, M., Sorby, M., Bjorlie, K., Strauman, T. J., & Wonderlich, S. (2019). Self-discrepancy theory as a transdiagnostic framework: A meta-analysis of self-discrepancy and psychopathology. Psychological Bulletin, 145(4), 372–389. https://doi.org/10.1037/bul0000186
- McKinney, C., Stearns, M., & Szkody, E. (2021). Maltreatment and affective and behavioral problems in emerging adults with and without oppositional defiant disorder symptoms: mediation by parent-child relationship quality. Journal of Interpersonal Violence, 36(5–6), 2612–2632. https://doi.org/10.1177/0886260518760014
- McLaughlin, K. A., Colich, N. L., Rodman, A. M., & Weissman, D. G. (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1), 96. https://doi.org/10.1186/s12916-020-01561-6
- McLaughlin, K. A., Sheridan, M. A., & Lambert, H. K. (2014). Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neuroscience & Biobehavioral Reviews, 47, 578–591. https://doi.org/10.1016/j.neubiorev.2014.10.012
- Mikolajewski, A. J., Taylor, J., & Iacono, W. G. (2017). Oppositional defiant disorder dimensions: genetic influences and risk for later psychopathology. Journal of Child Psychology and Psychiatry, 58(6), 702–710. https://doi.org/10.1111/jcpp.12683
- Murphy, S., Elklit, A., Dokkedahl, S., & Shevlin, M. (2016). Testing the validity of the proposed ICD-11 PTSD and complex PTSD criteria using a sample from Northern Uganda. European Journal of Psychotraumatology, 7(1), 32678. https://doi.org/10.3402/ejpt.v7.32678
- Nestgaard Rod, A., & Schmidt, C. (2021). Complex PTSD: what is the clinical utility of the diagnosis? European Journal of Psychotraumatology, 12(1), 2002028. https://doi.org/10.1080/20008198.2021.2002028
- Nylund, K., Asparouhov, T., & Muthen, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. doi:10.1080/10705510701575396
- Ollendick, T. H., Booker, J. A., Ryan, S., & Greene, R. W. (2018). Testing multiple conceptualizations of oppositional defiant disorder in youth. Journal of Clinical Child & Adolescent Psychology, 47(4), 620–633. https://doi.org/10.1080/15374416.2017.1286594
- Pallini, S., Chirumbolo, A., Morelli, M., Baiocco, R., Laghi, F., & Eisenberg, N. (2018). The relation of attachment security status to effortful self-regulation: A meta-analysis. Psychological Bulletin, 144(5), 501–531. https://doi.org/10.1037/bul0000134
- Perkonigg, A., Hofler, M., Cloitre, M., Wittchen, H. U., Trautmann, S., & Maercker, A. (2016). Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. European Archives of Psychiatry and Clinical Neuroscience, 266(4), 317–328. https://doi.org/10.1007/s00406-015-0639-4
- Pinto, A., Verissimo, M., Gatinho, A., Santos, A. J., & Vaughn, B. E. (2015). Direct and indirect relations between parent-child attachments, peer acceptance, and self-esteem for preschool children. Attachment & Human Development, 17(6), 586–598. https://doi.org/10.1080/14616734.2015.1093009
- Redican, E., Nolan, E., Hyland, P., Cloitre, M., McBride, O., Karatzias, T., Murphy, J., & Shevlin, M. (2021). A systematic literature review of factor analytic and mixture models of ICD-11 PTSD and CPTSD using the International Trauma Questionnaire. Journal of Anxiety Disorders, 79, 102381. https://doi.org/10.1016/j.janxdis.2021.102381
- Sachser, C., Keller, F., & Goldbeck, L. (2017). Complex PTSD as proposed for ICD-11: Validation of a new disorder in children and adolescents and their response to trauma-focused cognitive behavioral therapy. Journal of Child Psychology and Psychiatry, 58(2), 160–168. https://doi.org/10.1111/jcpp.12640
- Santens, E., Claes, L., Dierckx, E., & Dom, G. (2020). Effortful control – A transdiagnostic dimension underlying internalizing and externalizing psychopathology. Neuropsychobiology, 79(4–5), 255–269. https://doi.org/10.1159/000506134
- Schneider, S. (2020). Associations between childhood exposure to community violence, child maltreatment and school outcomes. Child Abuse & Neglect, 104, 104473. https://doi.org/10.1016/j.chiabu.2020.104473
- Schweizer, T. H., Snyder, H. R., Young, J. F., & Hankin, B. L. (2020). The breadth and potency of transdiagnostic cognitive risks for psychopathology in youth. Journal of Consulting and Clinical Psychology, 88(3), 196–211. https://doi.org/10.1037/ccp0000470
- Seay, K. D. (2020). Pathways from parental substance use to child internalizing and externalizing behaviors in a child protective services sample. Child Maltreatment, 25(4), 446–456. https://doi.org/10.1177/1077559520913638
- Sierau, S., Warmingham, J., White, L. O., Klein, A. M., & von Klitzing, K. (2020). Childhood emotional and conduct problems in childhood and adolescence differentially associated with intergenerational maltreatment continuity and parental internalizing symptoms. Research on Child and Adolescent Psychopathology, 48(1), 29–42. https://doi.org/10.1007/s10802-019-00575-w
- Snyder, H. R., Friedman, N. P., & Hankin, B. L. (2019). Transdiagnostic mechanisms of psychopathology in youth: Executive functions, dependent stress, and rumination. Cognitive Therapy and Research, 43(5), 834–851. https://doi.org/10.1007/s10608-019-10016-z
- Spinazzola, J., van der Kolk, B., & Ford, J. D. (2018). When nowhere is safe: Interpersonal trauma and attachment adversity as antecedents of posttraumatic stress disorder and developmental trauma disorder. Journal of Traumatic Stress, 31(5), 631–642. https://doi.org/10.1002/jts.22320
- Spinazzola, J., van der Kolk, B., & Ford, J. D. (2021). Developmental trauma disorder: A legacy of attachment trauma in victimized children. Journal of Traumatic Stress, 34(4), 711–720. https://doi.org/10.1002/jts.22697
- Stolbach, B. C., Minshew, R., Rompala, V., Dominguez, R. Z., Gazibara, T., & Finke, R. (2013). Complex trauma exposure and symptoms in urban traumatized children: a preliminary test of proposed criteria for developmental trauma disorder. Journal of Traumatic Stress, 26(4), 483–491. https://doi.org/10.1002/jts.21826
- Stover, C. S., Hahn, H., Im, J. J., & Berkowitz, S. (2010). Agreement of parent and child reports of trauma exposure and symptoms in the early aftermath of a traumatic event. Psychological Trauma: Theory, Research, Practice, and Policy, 2(3), 159–168. https://doi.org/10.1037/a0019156
- Tian, Y., Li, W., Wu, X., & Cheng, X. (2022). Complex PTSD in Chinese adolescents exposed to childhood trauma: A latent profile analysis. Journal of Interpersonal Violence, 37(21–22). https://doi.org/10.1177/08862605211050111
- van der Kolk, B., Ford, J. D., & Spinazzola, J. (2019). Comorbidity of developmental trauma disorder (DTD) and post-traumatic stress disorder: findings from the DTD field trial. European Journal of Psychotraumatology, 10(1), 1562841. https://doi.org/10.1080/20008198.2018.1562841
- van der Kolk, B. A., Roth, S., Pelcovitz, D., Sunday, S., & Spinazzola, J. (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress, 18(5), 389–399. https://doi.org/10.1002/jts.20047
- Villalta, L., Smith, P., Hickin, N., & Stringaris, A. (2018). Emotion regulation difficulties in traumatized youth: A meta-analysis and conceptual review. European Child & Adolescent Psychiatry, 27(4), 527–544. https://doi.org/10.1007/s00787-018-1105-4
- Wade, M., Zeanah, C. H., Fox, N. A., & Nelson, C. A. (2020). Global deficits in executive functioning are transdiagnostic mediators between severe childhood neglect and psychopathology in adolescence. Psychological Medicine, 50(10), 1687–1694. https://doi.org/10.1017/S0033291719001764
- Weissman, D. G., Bitran, D., Miller, A. B., Schaefer, J. D., Sheridan, M. A., & McLaughlin, K. A. (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 31(3), 899–915. https://doi.org/10.1017/S0954579419000348
- Weissman, D. G., Jenness, J. L., Colich, N. L., Miller, A. B., Sambrook, K. A., Sheridan, M. A., & McLaughlin, K. A. (2020). Altered neural processing of threat-related information in children and adolescents exposed to violence: A transdiagnostic mechanism contributing to the emergence of psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1274–1284. https://doi.org/10.1016/j.jaac.2019.08.471
- Widom, C. S. (2019). Are retrospective self-reports accurate representations or existential recollections? JAMA Psychiatry, 76(6), 567–568. https://doi.org/10.1001/jamapsychiatry.2018.4599
- Widom, C. S., Miller, D., Li, X., Gordon, D., & Brzustowicz, L. (2020). Childhood maltreatment, serotonin transporter gene, and risk for callous and unemotional traits: A prospective investigation. Psychiatry Research, 291, 113271. https://doi.org/10.1016/j.psychres.2020.113271
- Wolf, E. J., Miller, M. W., Kilpatrick, D., Resnick, H. S., Badour, C. L., Marx, B. P., Keane, T. M., Rosen, R. C., & Friedman, M. J. (2015). ICD-11 complex PTSD in US national and veteran samples: Prevalence and structural associations with PTSD. Clinical Psychological Science, 3(2), 215–229. https://doi.org/10.1177/2167702614545480
- Yoon, S. (2017). Child maltreatment characteristics as predictors of heterogeneity in internalizing symptom trajectories among children in the child welfare system. Child Abuse & Neglect, 72, 247–257. https://doi.org/10.1016/j.chiabu.2017.08.022
- Yoon, S., Kobulsky, J. M., Yoon, D., & Kim, W. (2017). Developmental pathways from child maltreatment to adolescent substance use: The roles of posttraumatic stress symptoms and mother–child relationships. Children and Youth Services Review, 82, 271–279. https://doi.org/10.1016/j.childyouth.2017.09.035
- Zhang, Y., Zhang, J., & Ding, C. (2019). Investigating the association between parental absence and developmental trauma disorder symptoms. Journal of Traumatic Stress, 32(5), 733–741. https://doi.org/10.1002/jts.22446