ABSTRACT
Background: Post-traumatic stress disorder (PTSD) with dissociative symptoms is now a full-fledged subtype of this disorder. The dissociative subtype is associated with a greater number of psychiatric comorbidities. To date, the impact of dissociation on the efficacy of PTSD treatment remains unclear.
Objective: The aim of this study was to compare the efficacy of a traumatic memory reactivation procedure with the administration of propranolol or a placebo once a week for six consecutive weeks in reducing PTSD and MDE symptoms between PTSD subjects with or without high dissociative symptoms.
Method: For that, we conducted a randomized clinical trial in 66 adults diagnosed with longstanding PTSD and measured the SCID PTSD module, the PTSD Checklist (PCL-S), Beck’s Depression Inventory-II (BDI-II), and the Dissociative Experiences Scale (DES).
Results: Patients with and without high dissociative experience had significant improvement in their PCL-S scores over the 6 treatment sessions, and PCL-S scores continued to decline in all patients during the post-treatment period. However, there was no correlation between the presence/absence of high dissociative experiences and no specific effect of propranolol treatment. We found exactly the same results for MDE symptoms. Interestingly, patients with high dissociative experiences before treatment exhibited very significant improvement in their DES scores after the 6 treatment sessions, and patients maintained this improvement 3 months post-treatment.
Conclusions: The traumatic memory reactivation procedure is an effective way to treat dissociative symptoms in patients with PTSD, and improvement of these dissociative symptoms was associated with a decrease in both PTSD and depression severity.
HIGHLIGHTS
Traumatic memory reactivation procedure is an effective way to treat dissociative symptoms in patients with PTSD.
The improvement of these dissociative symptoms was associated to a decrease of both PTSD and depression severity.
Dissociative symptoms do not seem to mitigate the efficacy of traumatic memory reactivation during the treatment of PTSD.
Antecedentes: El trastorno de estrés postraumático (TEPT) con síntomas disociativos es ahora un subtipo consolidado de este trastorno. El subtipo disociativo está asociado con una gran cantidad de comorbilidades psiquiátricas. Hasta la fecha, el impacto de la disociación en la eficacia del tratamiento del TEPT permanece incierto.
Objetivo: El objetivo de este estudio fue comparar la eficacia del procedimiento de reactivación de la memoria traumática con la administración de propranolol o de un placebo una vez a la semana por seis semanas consecutivas, en la reducción de síntomas de TEPT y de EDM en sujetos con o sin síntomas altamente disociativos.
Método: Para esto, dirigimos un ensayo clínico aleatorizado en 66 adultos diagnosticados con TEPT prolongado y medimos el módulo de TEPT de la SCID, la lista de chequeo para TEPT (PCL-S), el Inventario de depresión de Beck II (BDI-II), y la Escala de Experiencias Disociativas (DES).
Resultados: Los pacientes con o sin experiencias altamente disociativas tuvieron una mejoría significativa en sus puntajes de PCL-S tras las 6 sesiones de tratamiento, y los puntajes de PCL-S continuaron bajando en todos los pacientes durante el periodo de postratamiento. Sin embargo, no hubo correlación entre la presencia/ausencia de experiencias altamente disociativas y el efecto no específico del tratamiento con propranolol. Encontramos exactamente los mismos resultados para síntomas de EDM. Interesantemente, los pacientes con experiencias altamente disociativas antes del tratamiento mostraron una mejoría muy significativa en sus puntajes de DES tras las 6 sesiones de tratamiento, y los pacientes mantuvieron esta mejoría a los 3 meses postratamiento.
Conclusiones: El procedimiento de reactivación de la memoria traumática es una manera efectiva de tratar los síntomas disociativos en pacientes con TEPT, y la mejoría de estos síntomas disociativos fue asociada con una disminución en la severidad tanto de la depresión como del TEPT.
背景:伴解离症状的创伤后应激障碍 (PTSD) 现在是这种疾病的一个成熟亚型。解离亚型与更多的精神合并症相关。迄今为止,解离对 PTSD 治疗效果的影响仍不清楚。
目的:本研究旨在比较创伤性记忆再激活程序与连续六周每周一次心得安或安慰剂在减少有或无高解离症状的 PTSD 被试之间 PTSD 和 MDE 症状的疗效。
方法:为此,我们对 66 名被诊断为长期 PTSD 的成年患者进行了一项随机临床试验,测量了 SCID PTSD 模块、PTSD 检查表 (PCL-S)、贝克抑郁量表-II (BDI-II) 和解离经历量表(DES)。
结果:有和无高解离经历的患者在 6 个治疗期间的 PCL-S 评分均有显著改善,并且在治疗后期间所有患者的 PCL-S 评分均持续下降。然而,高解离经历的存在/不存在与心得安治疗无特定效果之间没有相关性。我们发现 MDE 症状的结果完全相同。有趣的是,治疗前具有高解离经历的患者在 6 次治疗后表现出非常显著的 DES 评分改善,并且患者在治疗后 3个月仍保持这种改善。
结论:创伤记忆再激活程序是治疗 PTSD 患者解离症状的有效方法,这些解离症状的改善与 PTSD 和抑郁严重程度的降低有关。
1. Introduction
Dissociation is defined as an abnormal integration of consciousness, memory, identity, body representation, emotion, perception, motor control, and behaviour (Diagnostic and Statistical Manual of Mental Disorders Citation2013). This phenomenon encompasses a wide range of subjective experiences, some relatively common, such as daydreaming, and some related to more severe mental states, such as not remembering autobiographic memories (Bernstein & Putnam, Citation1986). Historically, Charcot and Janet linked dissociation and trauma in the late nineteenth century (Yrondi et al., Citation2019), and it is now known that post-traumatic stress disorder (PTSD) is among the psychiatric disorders that cause the most dissociative symptoms (Lyssenko et al., Citation2018).
This link was tightened in the last version of the DSM with the addition of the ‘with dissociative symptoms’ subtype of PTSD, which was justified based on different neural and psychophysiological responses to the recall of traumatic memories (van Huijstee & Vermetten, Citation2018). Some studies have reported a high frequency of this subtype, up to 80% when systematically searched (Hill et al., Citation2020). Moreover, patients with the dissociative symptom subtype of PTSD have more severe PTSD symptoms (intrusion, avoidance, and arousal) (Haagen et al., Citation2018). The dissociative subtype is also associated with a greater number of comorbidities, such as substance use and depressive and anxiety disorders (Kim et al., Citation2019; Tsai et al., Citation2015). Moreover, previous studies have highlighted the positive correlation between the severity of depressive symptoms and dissociation (Bob et al., Citation2010). In addition, it is well know that patients with both PTSD and major depressive disorder experience more frequent and higher dissociative symptoms (Bedard-Gilligan et al., Citation2015; Contractor et al., Citation2015; Salloum et al., Citation2018). It remains unclear to date whether dissociation negatively influences the treatment of PTSD. The question is still being debated in the literature, even though previous data have demonstrated that trauma-focused (Zoet et al., Citation2018) and cognitive processing therapy (Resick et al., Citation2012) were effective in diminishing PTSD and dissociative symptoms. On the other hand, narrative storytelling (NST) has shown short-term efficacy in the treatment of the dissociative subtype of PTSD. The improvement did not last over time since, at 40 weeks, NST was not associated with an affective and interpersonal regulation procedure (Cloitre et al., Citation2012).
For PTSD treatment, the beta-blocking compound, propranolol, has been shown to interfere with memory reconsolidation, suggesting its potential use as a pharmacological treatment in conditions involving increased memory intrusions such as PTSD. The noradrenergic system is critical in modulating memory processes, and β-noradrenergic receptor stimulation has been found to facilitate emotional memory reconsolidation. Moreover, a hyper-noradrenergic state is implicated in the pathophysiology of PTSD.
In a new therapeutic procedure (Brunet et al., Citation2018; Roullet et al., Citation2021), PTSD patients required to actively recalled their traumatic event under the influence of propranolol once a week for up to 6 weeks. In a previous study (Roullet et al., Citation2021), we showed that this traumatic memory reactivation, whether it was associated with a placebo or propranolol, was an effective treatment of PTSD. Moreover, despite the lack of differences between the propranolol and placebo groups at the end of the procedure, during follow-up at three months, patients in the propranolol group maintained the improvement more significantly than those in the placebo group. However, we do not know the potential impact of dissociative symptoms. Thus, the aim of this ancillary study was to compare the efficacy of traumatic memory reactivation over PTSD and depressive and dissociative symptoms between a highly dissociated group of patients and a lower one.
2. Methods
Details of the procedure and the main results for this clinical trial are presented elsewhere (Roullet et al., Citation2021).
2.1. Subjects and study design
Participants were enrolled from January 2013 to October 2017 from three different university hospitals (Toulouse, Lille, Tours) in France. All participants were outpatients recruited from specialized trauma clinics (Psychotrauma regional centre). To be included, adults aged 18–65 years needed to have a primary diagnosis of PTSD according to the DSM-IV criteria (Frances et al., Citation2000) with the Structured Clinical Interview for DSM (SCID) (First et al., Citation2007) and suffering from PTSD for at least three consecutive months with a PCL-S score ≥ 45 at the first session (W1). The exclusion criteria were: contraindication to propranolol (hypotension, higher than a first-degree heart block, bronchial asthma etc.); medication recommended or suggested for PTSD treatment; psychotherapy; basal systolic blood pressure < 100 mm Hg; basal heart rate < 50 bpm; psychotic or bipolar disorders; traumatic brain injury; current substance or alcohol dependence; acute suicidal ideation; pregnancy and breast-feeding.
Participants received detailed information about the study and gave their written informed consent to participate. All procedures were reviewed and approved by institutional review boards associated with the lead research team and each treatment site. Following inclusion, participants were assigned by randomized complete block to either the ‘traumatic memory reactivation + propranolol’ group, hereafter referred to as the propranolol group, or the ‘traumatic memory reactivation + placebo’ group, referred to as the placebo group.
Propranolol or a placebo was administered 90 min before the memory reactivation session. This reactivation was performed in the centre once a week for six consecutive weeks (W1 to W6). For the first session (W1), 90 min after ingesting the propranolol or a placebo, participants wrote a one-page trauma narrative in the present tense, first person singular, focusing on the event’s most disturbing moments. This task took up to 30 min. The therapist asked the patient to add some emotional details, if possible. Prior to the second session, a ‘traumatic script’ was prepared. In subsequent treatment sessions (W2 to W6), 90 min after receiving the medication, participants read their trauma script. Participants did not receive any additional intervention. The post-treatment effect was assessed one week (W7) and three months (W18) after the end of the procedure (for details of the procedure, see Roullet et al., Citation2021).
2.2. Assessment
PTSD diagnosis was assessed according to the DSM-IV criteria (Frances et al., Citation2000) with the Structured Clinical Interview for DSM (SCID) (First et al., Citation2007), MDE, panic disorder, social phobia, obsessive-compulsive disorder (OCD), alcohol dependence/abuse, psychotic symptoms, and general anxiety disorder (GAD) were assessed according to the DSM-IV criteria (Frances et al., Citation2000) with the Mini-International Neuropsychiatric Interview (M.I.N.I.5.0.0) (Lecrubier et al., Citation1997). The SCID PTSD module was performed before treatment and one week and three months post treatment. The severity of PTSD and depressive symptoms were assessed with the PTSD Checklist–Specific (PCL-S) total score (Blanchard et al., Citation1996) and the Beck’s Depression Inventory (BDI-II) total score (Beck et al., Citation1996), respectively. Dissociative experiences were assessed with the Dissociative Experiences Scale (DES) (Bernstein & Putnam, Citation1986), and we used the cut-off of 30 to define patients without (DES < 30) or with (DES ≥ 30) high dissociative experiences (Carlson et al., Citation1993; Simeon et al., Citation1998). PCL, DES and BDI scales were performed before treatment, during each treatment sessions and one week and three months post treatment. The instructions were modified for PTSD, dissociative and depressive symptoms to inquire about ‘current’ symptoms.
2.3. Statistical analysis
Sociodemographic and clinical characteristics were presented using means and standard deviations for continuous variables and frequency distributions for categorical variables. For comparisons between groups, we used chi-square tests for categorical variables and t-tests for continuous variables. Linear regression models (enter method) were applied to test the association between the dependent variable (intensity of depressive symptoms: BDI) and the independent variables: dissociation experience (DES) and the intensity of post-traumatic symptoms (PCL). Linear regression models were adjusted based on age and gender. To analyze the evolution of the DES, PCL-S, and BDI scores during the different sessions, we used a repeated factor Anova.
As indicated in the introduction, in the original experiment (Roullet et al., Citation2021), PTSD patients significantly improved their PCL-S scores after the 6 treatment sessions, but PCL-S scores decreased to a similar extent in patients treated with propranolol and a placebo. For this reason and as there was no difference in the DES scores in these two groups of patients, we decided not to consider this factor in the analyses.
3. Results
3.1. Sociodemographic and clinical characteristic
Sixty-six participants were assessed, but three of them did not respond correctly to the DES and thus were excluded from the analysis. The mean age was 39.2 years old (95% CI: 35.7–42.1). Thirty-nine (61.9%) participants were female.
The kind of traumatic experiences that caused the PTSD was not different in the two group of patients (p = .147). We can note that, for sexual trauma, seven patients (7/12) had this trauma during childhood, two patients (2/5) in the ‘without high dissociative experience’ group and five patients (5/7) in the ‘with high dissociative experience’ group.
Before the first treatment session, the mean PCL, BDI, and DES scores were 63.8 (95% CI: 61.8–66.4), 30.6 (95% CI: 27.9–34.1), and 25.3 (95% CI: 21.4–29.5), respectively (). Before the first treatment session, high dissociative experiences (DES score ≥ 30) were recorded in 38.1% (24/63) of participants.
Table 1. Demographic and clinical characteristics.
We did not measure any difference in the sociodemographic characteristics between participants with or without high dissociative experiences. However, participants with high dissociative experiences had higher PCL-S and BDI scores before the beginning of the treatment procedure than participants without high dissociative experiences (PCL-S p = .006; BDI p < .001). This group of participants also had a higher rate of MDE (p = .003).
We must note that in our study, only 14.3% (9/63) of the participants dropped out at the end of the treatment procedure [without high dissociative experience 15.4% (6/39); with high dissociative experience 12.5% (3/24)] and that, for the follow-up 3 months after treatment (W18), 77.8% (49/63) of the participants were still participating in the study [without high dissociative experience 76.9% (30/39); with high dissociative experience 79.2% (19/24)]. No major adverse event occurred during our study (especially no hospitalization nor suicide attempt). None of the subjects had a significant increase of their depressive symptoms per protocol. A transient minor increase of their posttraumatic and dissociative symptoms (concerning respectively two and three non-overlapping subjects) was noted at V7 but went back to clinically insignificant levels at V9 (maximum DES increase at V9 = 7.5; maximum PCL-S2 increase at V9 = 3).
The SCID-Post-treatment PTSD diagnosis decreased in both groups with no significant intergroup differences (p = .346) at W7. Almost two-thirds of the patients were in remission one week post-treatment: 69.7% in the ‘without high dissociative experience’ group and 57.1% in the ‘with high dissociative experience’ group. At 3 months post-treatment, the rates of SCID PTSD diagnoses were low (14.3% in the ‘without high dissociative experience’ group and 25% in the ‘with high dissociative experience’ group) and there was no significant difference between the two groups (p = .375). However, these low rates are partly biased because some patients were withdrawn from the study after session 7 for another treatment.
3.2. Comparison of PCL-S scores in PTSD patients with or without high dissociative experiences before treatment
Anova for repeated measures reveals that, for all participants, the PCL-S scores decreased significantly over the 6 treatment sessions (A, W1–W7) [F(6,318) = 45.37; p < .001]. However, we did not find any effect related to the presence/absence of a high dissociative experiences [F(1.53) = 3.63; p = .062], nor any interaction between this factor and the sessions [F(6,318) = 0.87; p = .515]. We only found significant differences for the PCL-S score between the groups of PTSD participants with or without high dissociative experiences during the first two sessions and in the fifth session (W1: p < .01; W2 and W5: p < .05), but there was no difference in this score one week or three months after treatment. Thus, participants with and without high dissociative experiences had significant improvement in their PCL-S scores over the 6 treatments sessions.
Figure 1. Change over the treatment period in PTSD patient with or without high dissociative experiences before treatment in the (A) PCL-S score, (B) BDI score, and (C) DES score. Mean (± SEM). *p < .05, **p < .01, ***p < .001 between groups of patients with the presence (≥ 30) or absence (< 30) of high dissociative experiences.
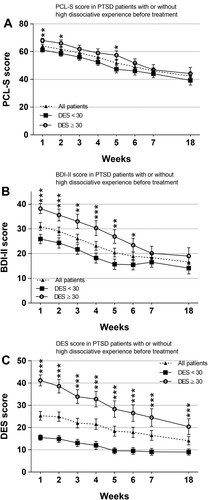
During the post-treatment period (W7–W18), PCL-S scores continued to decline in all participants [F(1.45) = 4.38; p = .042], but there was no effect link to the presence/absence of high dissociative experiences [F(1.45) = 0.85; p = .362] and no interaction between this factor and the sessions [F(1.45) = 0.03; p = .858].
3.3. Comparison of BDI-II scores in PTSD patients with or without high dissociative experiences before treatment
As we have shown that the reactivation procedure with or without propranolol was effective on the PCL-S scores but also on the BDI-scores (Roullet et al., Citation2021), it seemed important to us to investigate the effect of the dissociation level on this anxiety score.
For all participants, BDI-II scores decreased significantly over the 6 treatment sessions (B, W1–W7) [F(6,318) = 39.97; p < .001]. We found a significant effect related to the presence/absence of high dissociative experiences [F(1,53) = 10.3; p = .002] and a significant interaction between this level of dissociation severity and weeks [F(6,318) = 3.88; p < .001]. Thus, the severity of dissociative experiences has a very significant impact on the BDI-II scores, and we found significant differences between the two groups over the first six treatment sessions. However, this difference was no longer present one week and three months after treatment.
During the post-treatment period (W7–W18), Anova revealed that in all participants, BDI-II scores did not change significantly [F(1.46) = 0.85; p = .359] and there was no effect link to the presence/absence of high dissociative experiences [F(1.46) = 1.67; p = .202] and no interaction between this factor and the sessions [F(1.46) = 0.03; p = .870].
3.4. Evolution of DES scores in PTSD patients with or without high dissociative experiences before treatment
It can be noted that, on all participants (C), the DES scores decreased significantly during the sessions [F(6,312) = 31.65; p < .001] and that this decrease was more significant in the group with high dissociative experiences [F(6,312) = 5.55; p < .001]. Although the difference in DES scores between participants with or without high dissociative experiences decreased at each session, this difference remained significant at all sessions, including the 3 months post-treatment session.
During the post-treatment period (W7-W18), an overall decrease in DES scores was found [F(1,47) = 4.19 p = .046]. There was an effect link to the presence/absence of high dissociative experiences [F(1.47) = 13.80; p < .001] but no interaction between this factor and the sessions [F(1.47) = 3.02 p = .089]. We should note that before the first treatment session, high dissociative experiences were recorded in 38.1% (24/63) of participants, but after six treatment sessions, this level dropped dramatically to 11.1% (6/54) at W7 and to 10.2% (5/49) at W18.
3.5. Association between severity of dissociative experiences and severity of depressive symptoms and PTSD symptoms
Before treatment, in a model adjusted for age and gender, we found a significant positive association between dissociative experiences severity (DES W1) and depressive symptom severity (BDI W1) [β = 0.447; p = .002] but not with PTSD symptom severity (PCL-S W1) [β = 0.246; p = .082].
This time, one week after treatment, we found a significant positive association between dissociative experience severity (DES W7) and PTSD symptom severity (PCL-S W7) [β = 0.473; p = .006] but not with depressive symptom severity (BDI W7) [β = 0.119; p = .473]. We found the same results three months post-treatment, i.e. a significant positive association between dissociative experience severity (DES W18) and PTSD symptom severity (PCL-S W18) [β = 0.418; p = .045] but not with depressive symptom severity (BDI W18) [β = 0.270; p = .188].
We found a very significant association between dissociative experience severity before treatment (DES W1) and PTSD symptom severity one week after treatment (PCL-S W7) [β = 0.303; p = .028] and depressive symptom severity (BDI W7) [β = 0.383; p = .005]. This predictive association of dissociative experience severity before treatment (DES W1) with PCL and BDI scores was found again three months after treatment [PCL-S W18: β = 0.306; p = .042; BDI W18: β = 0.310; p = .037]. However, no significant association was found between dissociative symptoms severity before treatment (DES W1) and the evolution of PTSD and depressive symptoms severity during treatment (W7–W1). During the 18 weeks of the study (W18–W1), there was no association focusing on PTSD symptoms nevertheless, an association was found for depressive symptoms (BDI score) [BDI: W18–W1: β = 0.318; p = .043].
4. Discussion
In our study, traumatic memory reactivation led to a global decrease of PTSD, depressive, and dissociative symptoms in patients with PTSD diagnosis independently of the adjunction of propranolol or a placebo. Interestingly, at the end of treatment, the number of participants that met the criteria necessary to be considered highly dissociated (e.g. DES > 30) dropped from 38.1% (24/63) to 11.1% (6/54) on all subjects. In addition, in these highly dissociated participants, we observed a very significant decrease in the DES score of 14 points at the end of treatment and of 19.7 points 3 months post-treatment. Interestingly, there was no more statistically significant difference of the intensity of dissociation between the two groups one week and three months after the treatment. More important, the decrease of dissociative symptoms seems to go along with both depressive and post-traumatic ones.
Even if PTSD hugely overlaps with both anxiety and depressive-related disorders with some of its symptoms being present in both conditions (i.e. anhedonia, sleep disturbance), it also integrates in its diagnostic criteria dissociative symptoms that are far less commons among the nosography. Even if dissociation is considered by some authors as a physiological defense mechanism and an attempt to gain a psychological distance from the traumatic event (Dalenberg & Carlson, Citation2012), some authors alleged that peritraumatic dissociation is one for the best predictors of PTSD and its intensity (Ozer et al., Citation2003) even though this remains debated (Lensvelt-Mulders et al., Citation2008). By considering it as a coping strategy, previous authors theorized that dissociation might mitigate the effects of trauma-focused treatments, because of its interference with the habituation process (Foa & Kozak, Citation1986). Even now, therapists often consider these dissociative symptoms as a contraindication for exposure-based treatments in PTSD, or at least believe that they would lead to poorer results (Becker et al., Citation2004). However, recent studies found no evidence for an attenuating effect of dissociation on psychotherapy outcomes in PTSD (Hoeboer et al., Citation2020) and concluded that patients with PTSD and high dissociation could benefit of trauma-focused therapies, which often decrease significantly both posttraumatic and dissociative symptoms (Atchley & Bedford, Citation2021). Nevertheless, even though some psychotherapeutic approaches have shown encouraging results, their overall methodological flaws constrain their generalizability (Brand et al., Citation2009). Our results are in lines with the most recent reviews and add one more building block to the management of patients suffering from PTSD with associated dissociative symptoms. They suggest that dissociation might not be an active coping strategy as previous authors described it, but a reaction to the traumatic event that is encoded with other features (such as emotions, behavioural response) that finally becomes a core component of the traumatic memory. This might explain the larger improvement in highly dissociate patient-subgroups in some studies (Brand et al., Citation2019). Trauma-focus interventions are known to act on the phenomenological features of traumatic memories in patients with PTSD (Bisson et al., Citation2019); these data make us hypothesize that dissociation might be one of them.
Despite all this growing body of literature, our study failed to show a correlation between the initial severity of the dissociative symptoms and the overall improvement of both posttraumatic and depressive symptoms even though there was a significant correlation between DES and BDI-II at W18.
In our study, subjects in the higher dissociation group had greater depressive and post-traumatic symptoms than those in the lower dissociation group, which is consistent with the literature. Despite this, we observed an overall reduction in BDI-II and PCL-S scores over time, a change that was even more marked in the high dissociation group. We believe this suggests that even with higher severity, traumatic memory reactivation procedures might be a promising therapeutic option. Finally, with an overall reduction in traumatic symptoms and a 12.7% patient drop rate during follow-up, our results not only showed the efficacy of traumatic memory reactivation over dissociative symptoms but also demonstrated that this procedure seems to be safe and acceptable for patients.
Nevertheless, our study suffers from certain flaws. First, it was not specifically designed to assess the efficacy of traumatic memory reactivation procedures on traumatic dissociative symptoms and thus, these results should be considered as preliminary and require replication in future controlled experiments. Previous reports also reported a link between exposure to childhood trauma and the occurrence of PTSD and dissociative symptoms throughout the lifetime (Dorahy et al., Citation2015; Evren et al., Citation2011). This might be a confounding factor that future studies need to control for.
5. Conclusion
This study suggests that traumatic memory reactivation procedures are an effective way to treat dissociative symptoms in patients with PTSD. Moreover, the improvement of these dissociative symptoms was associated with a decrease in both PTSD and depression severity. Interestingly, we observed a very low drop rate concerning the patients included, which suggests a high acceptability of this treatment. Future studies with a specific controlled design are needed to confirm these promising results for patients who suffer from PTSD with the dissociative subtype.
Author contributions
Profs. Roullet and Birmes had full access to all study data and assume responsibility for the integrity and accuracy of the data analysis. Study concept and design (Roullet, Thalamas, Birmes), Statistical analysis (Roullet, Yrondi, Thalamas, Birmes), article compilation (Roullet, Birmes, Yrondi, Taïb), critical revision of the article for key intellectual content: All authors. Final approval of the version to be published: all authors.
Ethics statement
Participants received detailed information about the study and gave their written informed consent to participate. All procedures were reviewed and approved by institutional review boards (ClinicalTrials.gov identifier: NCT01713556).
Supplemental Material
Download MS Word (15.2 KB)Supplemental Material
Download TIFF Image (1.1 MB)Supplemental Material
Download TIFF Image (377.5 KB)Acknowledgement
The authors would like to thank the CIC of Toulouse University Hospital and all the patients who participated in this trial.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Atchley, R., & Bedford, C. (2021). Dissociative symptoms in posttraumatic stress disorder: A systematic review. Journal of Trauma & Dissociation, 22(1), 69–88. https://doi.org/10.1080/15299732.2020.1760410
- Beck, A. T., Steer, R. A., & Brown, G. K. (1996). BDI-II, Beck depression inventory: Manual. Psychological Corporation.
- Becker, C. B., Zayfert, C., & Anderson, E. (2004). A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy, 42(3), 277–292. https://doi.org/10.1016/S0005-7967(03)00138-4
- Bedard-Gilligan, M., Duax Jakob, J. M., Doane, L. S., Jaeger, J., Eftekhari, A., Feeny, N., & Zoellner, L. A. (2015). An investigation of depression, trauma history, and symptom severity in individuals enrolled in a treatment trial for chronic PTSD. Journal of Clinical Psychology, 71(7), 725–740. https://doi.org/10.1002/jclp.22163
- Bernstein, E. M., & Putnam, F. W. (1986). Development, reliability, and validity of a dissociation scale. The Journal of Nervous and Mental Disease, 174(12), 727–735. https://doi.org/10.1097/00005053-198612000-00004
- Bisson, J. I., Berliner, L., Cloitre, M., Forbes, D., Jensen, T. K., Lewis, C., Monson, C. M., Olff, M., Pilling, S., Riggs, D. S., Roberts, N. P., & Shapiro, F. (2019). The international society for traumatic stress studies new guidelines for the prevention and treatment of posttraumatic stress disorder: Methodology and development process. Journal of Traumatic Stress, 32(4), 475–483. https://doi.org/10.1002/jts.22421
- Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., & Forneris, C. A. (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. https://doi.org/10.1016/0005-7967(96)00033-2
- Bob, P., Raboch, J., Maes, M., Susta, M., Pavlat, J., Jasova, D., Benakova, H., & Zima, T. (2010). Depression, traumatic stress and interleukin-6. Journal of Affective Disorders, 120(1-3), 231–234. https://doi.org/10.1016/j.jad.2009.03.017
- Brand, B. L., Classen, C. C., McNary, S. W., & Zaveri, P. (2009). A review of dissociative disorders treatment studies. Journal of Nervous & Mental Disease, 197(9), 646–654. https://doi.org/10.1097/NMD.0b013e3181b3afaa
- Brand, B. L., Schielke, H. J., Putnam, K. T., Putnam, F. W., Loewenstein, R. J., Myrick, A., Jepsen, E. K. K., Langeland, W., Steele, K., Classen, C. C., & Lanius, R. A. (2019). An online educational program for individuals with dissociative disorders and their clinicians: 1-year and 2-year follow-up. Journal of Traumatic Stress, 32(1), 156–166. https://doi.org/10.1002/jts.22370
- Brunet, A., Saumier, D., Liu, A., Streiner, D. L., Tremblay, J., & Pitman, R. K. (2018). Reduction of PTSD symptoms with pre-reactivation propranolol therapy: A randomized controlled trial. American Journal of Psychiatry, 175(5), 427–433. https://doi.org/10.1176/appi.ajp.2017.17050481
- Carlson, E. B., Putnam, F. W., Ross, C. A., Torem, M., Coons, P., Dill, D. L., Loewenstein, R. J., & Braun, B. G. (1993). Validity of the dissociative experiences scale in screening for multiple personality disorder: A multicenter study. American Journal of Psychiatry, 150(7), 1030–1036. https://doi.org/10.1176/ajp.150.7.1030
- Cloitre, M., Petkova, E., Wang, J., & Lu Lassell, F. (2012). An examination of the influence of a sequential treatment on the course and impact of dissociation among women with PTSD related to childhood abuse. Depression and Anxiety, 29(8), 709–717. https://doi.org/10.1002/da.21920
- Contractor, A. A., Elhai, J. D., Fine, T. H., Tamburrino, M. B., Cohen, G., Shirley, E., Chan, P. K., Liberzon, I., Galea, S., & Calabrese, J. R. (2015). Latent profile analyses of posttraumatic stress disorder, depression and generalized anxiety disorder symptoms in trauma-exposed soldiers. Journal of Psychiatric Research, 68, 19–26. https://doi.org/10.1016/j.jpsychires.2015.05.014
- Dalenberg, C., & Carlson, E. B. (2012). Dissociation in posttraumatic stress disorder part II: How theoretical models fit the empirical evidence and recommendations for modifying the diagnostic criteria for PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 551–559.
- Diagnostic and Statistical Manual of Mental Disorders. (2013). 5th ed. Amer Psychiatric Pub Incorporated.
- Dorahy, M. J., Middleton, W., Seager, L., McGurrin, P., Williams, M., & Chambers, R. (2015). Dissociation, shame, complex PTSD, child maltreatment and intimate relationship self-concept in dissociative disorder, chronic PTSD and mixed psychiatric groups. Journal of Affective Disorders, 172, 195–203. https://doi.org/10.1016/j.jad.2014.10.008
- Evren, C., Sar, V., Dalbudak, E., Cetin, R., Durkaya, M., Evren, B., & Celik, S. (2011). Lifetime PTSD and quality of life among alcohol-dependent men: Impact of childhood emotional abuse and dissociation. Psychiatry Research, 186(1), 85–90. https://doi.org/10.1016/j.psychres.2010.07.004
- First, M. B., Williams, J. B. W., Spitzer, R. L., & Gibbon, M. (2007). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Clinical Trials Version (SCID-CT). Biometrics Research; New York State Psychiatric Institute.
- Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. https://doi.org/10.1037/0033-2909.99.1.20
- Frances, A., Pincus, H. A., & First, M. B. (2000). American Psychiatric Association DSM-IV-TR. Fourth edition.
- Haagen, J. F. G., van Rijn, A., Knipscheer, J. W., van der Aa, N., & Kleber, R. J. (2018). The dissociative post-traumatic stress disorder (PTSD) subtype: A treatment outcome cohort study in veterans with PTSD. British Journal of Clinical Psychology, 57(2), 203–222. https://doi.org/10.1111/bjc.12169
- Hill, S. B., Wolff, J. D., Bigony, C. E., Winternitz, S. R., Ressler, K. J., Kaufman, M. L., & Lebois, L. A. M. (2020). Dissociative subtype of posttraumatic stress disorder in women in partial and residential levels of psychiatric care. Journal of Trauma & Dissociation, 21(3), 305–318. https://doi.org/10.1080/15299732.2019.1678214
- Hoeboer, C. M., Kleine, R. A. D., Molendijk, M. L., Schoorl, M., Oprel, D. C., Mouthaan, J., Van der Does, W., & Van Minnen, A. (2020). Impact of dissociation on the effectiveness of psychotherapy for post-traumatic stress disorder: Meta-analysis. BJPsych Open, 6(3), https://doi.org/10.1192/bjo.2020.30
- Kim, D., Kim, D., Lee, H., Cho, Y., Min, J. Y., & Kim, S. H. (2019). Prevalence and clinical correlates of dissociative subtype of posttraumatic stress disorder at an outpatient trauma clinic in South Korea. European Journal of Psychotraumatology, 10(1), 1657372. https://doi.org/10.1080/20008198.2019.1657372
- Lecrubier, Y., Sheehan, D., Weiller, E., Amorim, P., Bonora, I., Harnett Sheehan, K., Janavs, J., & Dunbar, G. C. (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: reliability and validity according to the CIDI. European Psychiatry, 12(5), 224–231. https://doi.org/10.1016/S0924-9338(97)83296-8
- Lensvelt-Mulders, G., van der Hart, O., van Ochten, J. M., van Son, M. J. M., Steele, K., & Breeman, L. (2008). Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis. Clinical Psychology Review, 28(7), 1138–1151. https://doi.org/10.1016/j.cpr.2008.03.006
- Lyssenko, L., Schmahl, C., Bockhacker, L., Vonderlin, R., Bohus, M., & Kleindienst, N. (2018). Dissociation in psychiatric disorders: A meta-analysis of studies using the dissociative experiences scale. American Journal of Psychiatry, 175(1), 37–46. https://doi.org/10.1176/appi.ajp.2017.17010025
- Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. https://doi.org/10.1037/0033-2909.129.1.52
- Resick, P. A., Suvak, M. K., Johnides, B. D., Mitchell, K. S., & Iverson, K. M. (2012). The impact of dissociation on PTSD treatment with cognitive processing therapy. Depression and Anxiety, 29(8), 718–730. https://doi.org/10.1002/da.21938
- Roullet, P., Vaiva, G., Véry, E., Bourcier, A., Yrondi, A., Dupuch, L., Lamy, P., Thalamas, C., Jasse, L., El Hage, W., & Birmes, P. (2021). Traumatic memory reactivation with or without propranolol for PTSD and comorbid MD symptoms: A randomised clinical trial. Neuropsychopharmacology, 46(9), 1643–1649. https://doi.org/10.1038/s41386-021-00984-w
- Salloum, A., Johnco, C., Smyth, K. M., Murphy, T. K., & Storch, E. A. (2018). Co-occurring posttraumatic stress disorder and depression among young children. Child Psychiatry & Human Development, 49(3), 452–459. https://doi.org/10.1007/s10578-017-0764-6
- Simeon, D., Guralnik, O., Gross, S., Stein, D. J., Schmeidler, J., & Hollander, E. (1998). The detection and measurement of depersonalization disorder. The Journal of Nervous & Mental Disease, 186(9), 536–542. https://doi.org/10.1097/00005053-199809000-00004
- Tsai, J., Armour, C., Southwick, S. M., & Pietrzak, R. H. (2015). Dissociative subtype of DSM-5 posttraumatic stress disorder in U.S. Veterans. Journal of Psychiatric Research, 66-67, 67–74. https://doi.org/10.1016/j.jpsychires.2015.04.017
- van Huijstee, J., & Vermetten, E. (2018). The dissociative subtype of post-traumatic stress disorder: Research update on clinical and neurobiological features. Current Topics in Behavioral Neurosciences, 38, 229–248. https://doi.org/10.1007/7854_2017_33
- Yrondi, A., Taib, S., Dupuch, L., Schmitt, L., Very, E., & Birmes, P. (2019). Traumatic hystero-neurasthenia in Professor Charcot’s Leçons du Mardi. Journal of Nervous & Mental Disease, 207(9), 799–804. https://doi.org/10.1097/NMD.0000000000001093
- Zoet, H. A., Wagenmans, A., van Minnen, A., & de Jongh, A. (2018). Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology, 9(1), 1468707. https://doi.org/10.1080/20008198.2018.1468707
