ABSTRACT
Background: People forced to leave their homes, such as refugees and internally displaced persons, are exposed to various stressors during their forced displacement, putting them at risk for mental disorders.
Objective: To summarize evidence on the efficacy of psychosocial interventions aiming to promote mental health and/or to prevent mental symptoms by fostering transdiagnostic skills in forcibly displaced persons of all ages.
Method: Four databases and reference lists were searched for randomized controlled trials on interventions in this population on 11 March 2022. Thirty-six studies were eligible, 32 studies (comprising 5299 participants) were included in random-effects multilevel meta-analyses examining the effects of interventions on mental symptoms and positive mental health (e.g. wellbeing) as well as moderators to account for heterogeneity. OSF Preregistration-ID: 10.17605/OSF.IO/XPMU3
Results: Our search resulted in 32 eligible studies, with 10 reporting on children/adolescents and 27 on adult populations. There was no evidence for favourable intervention effects in children/adolescents, with 44.4% of the effect sizes pointing to potentially negative effects yet remaining non-significant. For adult populations, our meta-analyses showed a close-to-significant favourable effect for mental symptoms, M(SMD) = 0.33, 95% CI [–0.03, 0.69], which was significant when analyses were limited to high-quality studies and larger for clinical compared to non-clinical populations. No effects emerged for positive mental health. Heterogeneity was considerable and could not be explained by various moderators (e.g. type of control, duration, setting, theoretical basis). Certainty of evidence was very low across all outcomes limiting the generalizability of our findings.
Conclusion: The present review provides at most weak evidence for an effect favouring transdiagnostic psychosocial interventions over control conditions for adult populations but not for children and adolescents. Future research should combine the imperative of humanitarian aid in face of major crises with studying the diverse needs of forcibly displaced persons to improve and tailor future interventions.
HIGHLIGHTS
This review is the first to examine the efficacy of transdiagnostic interventions for mental health promotion and prevention of mental disorders in forcibly displaced persons of all ages.
Overall, we found no favourable effect of transdiagnostic interventions in both children/adolescents and adults. Excluding studies at high risk of bias, there was weak evidence for a small favourable effect in adults, but not in children and adolescents. Thus, so far, there is weak evidence for transdiagnostic interventions in forcibly displaced persons.
Research efforts need to match care needs: While most people live and need care in low-income countries, the majority of research has been conducted in high-income countries.
Antecedentes: Las personas obligadas a abandonar sus hogares, como los refugiados y personas desplazadas internamente, están expuestas a diversos factores estresantes durante sus desplazamientos forzados, lo que los pone en riesgo de sufrir trastornos mentales.
Objetivo: Resumir la evidencia sobre la eficacia de intervenciones psicosociales orientadas a promover la salud mental y/o prevenir síntomas mentales mediante el fomento de estrategias transdiagnósticas en personas desplazadas a la fuerza de todas las edades.
Método: Se realizaron búsquedas en cuatro bases de datos y listas de referencia en busca de ensayos controlados aleatorizados sobre intervenciones en esta población el 11 de marzo del 2022. Treinta y seis estudios fueron elegibles, 32 estudios (que comprenden 5.299 participantes) se incluyeron en el metanálisis multinivel de efectos aleatorios que examinó los efectos de las intervenciones sobre síntomas mentales y de salud mental positiva (ej. Bienestar) así como moderadores que den cuenta de la heterogeneidad. DI-de registro previo de OSF: 10.17605/OSF.IO/XPMU3
Resultados: Nuestra búsqueda resultó en 32 estudios elegibles, con 10 que reportaban sobre niños/adolescentes y 27 en poblaciones adultas. No hubo evidencia de efectos favorables de la intervención en niños/adolescentes, con un 44.4% de los tamaños de efecto apuntando a efectos potencialmente negativos pero que no fueron significativos. Para las poblaciones adultas, nuestro metanálisis mostró un efecto favorable cercano a significativo para los síntomas mentales, M(SMD)=0.33, IC 95% [–0.03, 0.69], que fue significativo cuando los análisis se limitaron a estudios de alta calidad y más grandes para poblaciones clínicas en comparación con no clínicas. No surgieron efectos para salud mental positiva. La heterogeneidad fue considerable y no pudo ser explicada por varios moderadores (ej., tipo de control, duración, ambiente, base teórica). La certeza de la evidencia fue muy baja en todos los resultados lo cual limita la generalización de nuestros hallazgos.
Conclusiones: La presente revisión provee, como máximo, pruebas débiles de un efecto que favorece las intervenciones psicosociales transdiagnósticas sobre las condiciones de control para poblaciones adultas pero no para adolescentes y niños. La investigación futura debería combinar el imperativo de ayuda humanitaria frente a las grandes crisis con el estudio de las diversas necesidades de las personas desplazadas a la fuerza para mejorar y adaptar las intervenciones futuras.
背景:被迫离开家园的人,如难民和国内流离失所者,在被迫流离失所期间会面临各种应激源,使他们面临精神障碍的风险。
目的:总结旨在通过发展跨诊断技能来促进所有年龄段被迫流离失所者心理健康和/或预防精神症状的社会心理干预效果的证据。
方法: 在 2022 年 3 月 11 日搜索了四个数据库和参考列表,以查找在此群体中干预措施的随机对照试验。36 项研究符合条件,32 项研究(包括 5,299 名参与者)被纳入随机效应多水平元分析,以考查对精神症状和积极心理健康(例如幸福感)的干预以及解释异质性的调节因素。 OSF 预注册号:10.17605/OSF.IO/XPMU3
结果:我们的检索产生了 32 项符合条件的研究,其中 10 项针对儿童/青少年,27 项针对成年人。 没有证据表明干预效果在儿童/青少年更有利,44.4% 的效应量指向有潜在负面作用但仍然不显著。 对于成年人群,我们的元分析显示对精神症状有接近显著的有利影响,M(SMD) = 0.33, 95% CI [–0.03, 0.69],当分析仅限于高质量时显著且在临床群体比非临床人群效应更大。 对积极心理健康没有影响。 异质性相当大,无法被各种调节因素(例如,控制类型、持续时间、设置、理论基础)解释。 所有结果的证据质量都非常低,限制了我们研究结果的可推广性。
结论:本综述至多为支持跨诊断心理社会干预对成年人的效果优于控制条件的影响但对儿童和青少年则不然提供了微弱的证据。 未来的研究应该将面对重大危机时人道主义援助的必要性与研究被迫流离失所者的不同需求结合起来,以改进和精确调整未来的干预措施。
1. Introduction
The invasion of Ukraine is among the most devastating humanitarian crises of recent history. As of 31 January 2023, about 8 million people have left Ukraine and more than 7 million have been internally displaced since the beginning of the Russian military offensive (United Nations High Commissioner for Refugees, Citation2022b). This adds to a global situation where many wars and armed conflicts (e.g. in Afghanistan, Ethiopia, Iran, Yemen) force people to leave their homes (United Nations High Commissioner for Refugees, Citation2022a, Citation2023). Several reviews have pointed to serious mental health effects of exposure to armed conflicts (Bendavid et al., Citation2021; Leon et al., Citation2022; Bryant et al., Citation2022b; Steel et al., Citation2009). Soldiers but also war- and conflict-affected civilians are at increased risk for mental health problems, including posttraumatic stress disorder (PTSD), anxiety and depressive disorders (Blackmore et al., Citation2020; Charlson et al., Citation2019; Morina et al., Citation2018).
In 2022, the global number of forcibly displaced persons has been pushed over 100 million, of which 42% are children and adolescents (United Nations High Commissioner for Refugees, Citation2021, Citation2022c). Forcibly displaced persons (also referred to as involuntarily displaced persons) are exposed to several macro-stressors including the circumstances forcing people to leave their homes (e.g. armed conflicts), travel- and transit-related events (e.g. life-threatening events, physical harm), post-arrival stressors (e.g. uncertain asylum status), and integration/settlement-related problems (e.g. unemployment; [Sonne Citation2018]). As stressor exposure is among the leading causes for the onset and persistence of mental disorders (Zorn et al., Citation2017), the World Health Organization (WHO) presented a global action plan on the health of refugees which puts mental health as priority (World Health Organization, Citation2019).
A recent Cochrane umbrella review (Uphoff et al., Citation2019) provided an overview on mental health interventions for forcibly displaced persons differentiating between mental health promotion, prevention and treatment of common mental disorders. Mental health promotion is in most cases universal (i.e. it targets the general population), but it may also address high-risk groups like forcibly displaced persons. Primary outcomes of health-promoting interventions are often indicators of positive mental health rather than symptom measures, as health-promoting interventions aim at lowering the risk of mental disorders (Tol, Citation2015). Prevention of mental disorders or symptoms can be understood as specific, population- and/or individual-based interventions aiming to minimize the burden of disease. Prevention can either be primary, that is, interventions aim at avoiding that a disease manifests, or secondary, that is, interventions aim at the early detection and management of diseases (World Health Organization, Citation2022b). In contrast to mental health promotion, which focuses on general mental health, prevention may also include symptom-specific strategies. These interventions can be differentiated from the treatment of common mental disorders, which aims at reducing symptoms of specific disorders after their manifestation. These may include cognitive behavioural therapies (CBTs; e.g. trauma-focused; [Ehlers, Citation2013]) or culturally sensitive CBT (Hinton et al., Citation2012), or other forms of psychotherapy (Shapiro, Citation2012). While several reviews examined the effects of psychotherapy in forcibly displaced persons in different age groups (Morina & Sterr, Citation2019; Thompson et al., Citation2018), so far, only one review targeted community-based prevention measures for forcibly displaced children and adolescents in high-income countries (Soltan et al., Citation2020, Citation2022), without finding evidence for favourable intervention effects on mental symptoms. However, quantitative summaries were limited to at most two studies per outcome, and the overall certainty of evidence was very low to low. Another review (Turrini et al., Citation2019) stated to examine psychosocial interventions in asylum seekers and refugees, finding evidence for beneficial effects on mental symptoms. However, as in many other reviews (Nocon et al., Citation2017; Tribe et al., Citation2014), this evidence synthesis largely considered treatments of specific, manifest mental disorders, limiting conclusions about interventions to promote mental health or to prevent mental health issues. Thus, no review is available for health-promoting interventions or prevention measures in adult populations (Turrini et al., Citation2019).
Delivering mental health interventions to forcibly displaced persons is challenging. Standard treatments that are effectively delivered in Western societies might not be as effective in this population (Uphoff et al., Citation2019). First, high rates of comorbidity (Bogic et al., Citation2015; McMahon, Citation2014) may decrease intervention effects. Second, the generalizability of findings from research with forcibly displaced persons is limited as most studies on mental health interventions are conducted in high-income countries, while most people live and need care in low-income countries (United Nations High Commissioner for Refugees, Citation2022b; Wainberg et al., Citation2017). Third, even in countries with national health services, mental health care use by forcibly displaced persons is low due to different barriers (e.g. language, stigma; [Satinsky et al., Citation2019]).
Reduced effectiveness of standard treatments, low contact coverage of specialized mental healthcare professionals and limited resources in low-income countries have resulted in an increasing interest in transdiagnostic interventions (Dawson et al., Citation2015). Those interventions go beyond single diagnostic categories by addressing shared common aetiological and maintenance processes of mental health problems as well as cognitive, affective, behavioural, and interpersonal features of mental disorders, that is, they assume a general latent psychopathological factor (Fusar-Poli et al., Citation2019). Processes targeted by transdiagnostic interventions are, for instance, emotion regulation (Cludius et al., Citation2020), rumination (Hsu et al., Citation2015), repetitive negative thinking (Drost et al., Citation2014), or psychological (in)flexibility (Paulus et al., Citation2016).
Recently, different transdiagnostic treatments for common mental disorders have been proposed for forcibly displaced persons (Dawson et al., Citation2015; Murray et al., Citation2014). Given the aim of mental health promotion to foster general mental health and wellbeing and the goal of prevention measures to avoid the onset and/or chronification of mental symptoms and disorders, transdiagnostic approaches are of major relevance in this field (O’Bryan et al., Citation2021). This notion is supported by a rapidly increasing number of organizations developing transdiagnostic programmes for forcibly displaced persons (Ager et al., Citation2011; Dawson et al., Citation2015; De Graaff et al., Citation2020; World Health Organization, Citation2022a) (see for common intervention components).
Table 1. Common components of transdiagnostic psychosocial interventions.
Given the challenging circumstances under which mental health promotion and prevention in forcibly displaced persons needs to be delivered, intervention intensity is also a matter of debate (Rawlinson et al., Citation2020). Low-intensity interventions need less resources by using self-help materials, having six hours or less contact time, and being delivered by practitioners or trained supporters (Shafran et al., Citation2021). Reviews found low-intensity interventions to be effective in reducing mental symptoms (Bower et al., Citation2013; Hazell et al., Citation2016). Thus, especially low-intensity transdiagnostic interventions may have the potential to improve mental health care in forcibly displaced persons by targeting a broad range of symptoms, in low-resource settings and at lower costs than standard interventions (Dawson et al., Citation2015). At the same time, concerns were raised whether those low-intensity interventions are sufficient to meet the complex demands of this population due to rigid time schedules and their reliance on internal resources (Knefel et al., Citation2022).
So far, despite the enormous need for mental health promotion and prevention in forcibly displaced persons and the increasing interest in transdiagnostic interventions, a systematic review examining the effect of interventions targeting transdiagnostic factors is missing. The present study aimed at addressing this gap by providing an evidence synthesis on both low- and high-intensity transdiagnostic psychosocial interventions to promote mental health and/or to prevent mental symptoms in children/adolescents and adults affected by forced displacement. In contrast to previous reviews, our aim was to map potential multidimensional effects of transdiagnostic interventions by examining multiple outcomes including mental symptoms and positive mental health. Moreover, we aimed at examining moderators influencing their efficacy.
2. Methods
This systematic review adheres to standards outlined by the Cochrane Collaboration (Higgins et al., Citation2022) and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; [Page et al., Citation2021]). Differences between the preregistration of this review (preregistration-ID: 10.17605/OSF.IO/XPMU3) and the final review are presented as Supplementary Material (SM1). Most importantly, the review type evolved from a rapid to a systematic review and analyses were performed separately for children/adolescents and adult samples.
2.1. Search strategy
The search strategy was developed based on previous systematic reviews (Uphoff et al., Citation2019). Four databases were searched from inception of each database to 11 March 2022, including the Cochrane Central Register of Controlled Trials (CENTRAL), Ovid PsycINFO, and Embase (including Embase Core, Medline, and PubMed).
The strategy comprised three clusters of search terms that were searched in title, abstract and keywords: terms related to (i) forcibly displaced persons, (ii) interventions, and (iii) mental health outcomes. Within clusters, terms were combined with the Boolean operator OR, while clusters were combined using AND. For PsycINFO and Embase, common filters for randomized controlled trials were used (Glanville et al., Citation2019; National Health and Medical Research Council, Citation2013). If available, we used Medical Subject Heading (MeSH) and Emtree (for Embase). Search strategies are presented in SM2. Moreover, reference lists of included studies and related systematic reviews were screened for eligible studies.
2.2. Selection criteria
Eligible studies were published (cluster) randomized controlled trials ([c]RCTs). Participants were forcibly displaced persons based on the definitions provided by the UNHCR (United Nations High Commissioner for Refugees, Citation2016), including refugees, asylum seekers and internally displaced persons (see SM3). Samples were included irrespective of the geographical location of the triggering conflict, their age and physical/mental health status. Interventions were eligible if they aimed at promoting mental health, preventing mental symptoms and/or providing psychosocial support. Interventions were considered to be transdiagnostic when they explicitly targeted transdiagnostic factors (e.g. emotion regulation, rumination) or stated to promote general mental health or prevent mental symptoms. We included interventions that were described as based on psychotherapy (e.g. CBT), but excluded interventions solely consisting of disorder-specific psychotherapy or pharmacological treatments. All comparators were eligible. To be eligible for quantitative synthesis, studies were required to report on at least one primary mental health outcome at post-intervention assessment, including psychological distress, depressive, anxiety and PTSD symptoms or positive mental health.
2.3. Study selection
Following de-duplication, titles/abstracts were screened by two reviewers independently using Rayyan (Ouzzani et al., Citation2016). Interrater reliability (kappa = .57) was moderate at title/abstract level (Landis & Koch, Citation1977). At full-text level, eligibility was also double-screened, resulting in substantial interrater reliability (kappa = .63). At both stages of screening, disagreements were resolved through discussion or by consulting a third reviewer.
2.4. Data extraction
A customized data extraction sheet was developed for this review. Data were extracted by one reviewer and checked by a second reviewer. Any disagreements were resolved through discussion or consultation of a third reviewer.
2.5. Quality appraisal
2.5.1 Risk of bias
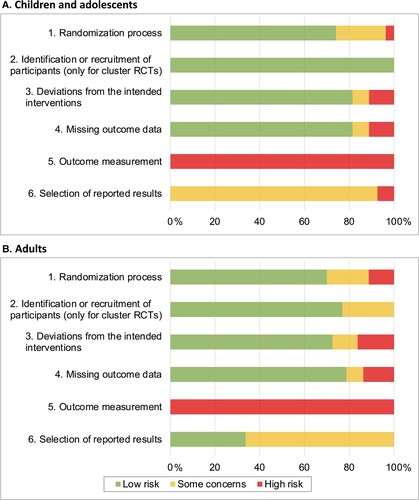
Two team members independently assessed the risk of bias of included studies using the Cochrane risk-of-bias tool for randomized trials (RoB2; [Sterne et al., Citation2019]). We assessed the following bias domains: (i) randomization process, (ii) deviations from the intended interventions, (iii) missing outcome data, (iv) outcome measurement, and (v) selection of reported results. For cRCTs, we additionally assessed risk of bias due to identification/recruitment of participants. In addition to bias ratings per domain, the overall bias at study and outcome level was assessed. Judgments could be ‘low’ or ‘high’ risk of bias or express ‘some concerns’ (Sterne et al., Citation2019). All disagreements were resolved through discussion or by consulting a third reviewer.
2.5.2 Publication bias
We examined a potential publication bias using visual inspections of contour-enhanced funnel plots (Peters et al., Citation2008) as well as statistically by approximating Begg and Mazumdar rank correlation test (Begg & Mazumdar, Citation1994), which are available for multilevel models by including sampling error as moderator to the main analyses. In case the sampling error would significantly predict effect sizes, this can be interpreted as indicative of a publication bias.
2.6. Data synthesis
Included studies were summarized narratively and in tabular form. Pairwise meta-analyses were performed for primary outcomes if more than two studies were available, and if these were sufficiently homogeneous in terms of interventions (i.e. length, design, providers, theoretical basis, etc.) and outcomes (i.e. examining mental symptoms or positive mental health). For studies with multiple intervention arms, it was determined which group was relevant for this review. However, in none of these multi-arm studies, more than one intervention group was eligible for inclusion in our review.Footnote1 In meta-analyses, we combined active and passive control groups. However, potential differences between passive and active controls were examined by means of subgroup analyses. In case data needed for effect size calculation was missing or unclear, study authors were contacted.
Meta-analyses were performed in R version 4.2.2 (R Core Team, Citation2021) using the package metafor (Viechtbauer, Citation2010). All analyses used random-effects models and maximum likelihood estimations. Due to differential clinical implications, we performed pairwise meta-analyses for children/adolescents and adult populations separately. Standardized mean differences (SMDs, Hedges’ g) at post-intervention assessment were used as effect size and their 95% confidence intervals (CIs) as indicator of their significance. SMDs were calculated based on means and standard deviations (SDs), with positive SMDs indicating favourable intervention effects for all outcomes. We additionally calculated 95% prediction intervals (PIs; i.e. an estimate of the interval in which 95% of future observations will fall) to account for uncertainty of meta-analytical findings (Deeks et al., Citation2022). Effect sizes of cRCTs were corrected for clustering effects (Higgins et al., Citation2022). As no cRCTs reported corrected standard errors, we used the formula 1 + (M – 1)•ICC to estimate the design effect, with M being the average cluster size and ICC the intra-cluster correlation coefficient (Higgins et al., Citation2022). As no ICC from cRCTs was available, we used ICC = .05 as a mild conservative estimate for primary analyses, and ICC = .10, a more conservative estimate, for sensitivity analyses.
Our main analyses aimed at answering the question of whether there is an effect of transdiagnostic psychosocial interventions on overall mental symptoms. For this purpose, we used a multilevel approach nesting effect sizes of symptom measures within studies and outcome types (Assink & Wibbelink, Citation2016). Thereby, our model allowed for correlations of effect sizes coming from the same study as well as for correlations of effect sizes that came from different studies but assessed the same outcome (see SM4 for exemplary R code). Additional analyses aimed at answering the question of whether there is an effect of transdiagnostic psychosocial interventions on specific symptom types and positive mental health. For this purpose, we used traditional meta-analyses for all primary outcomes in the subgroups of children/adolescents and adults.
Statistical heterogeneity was assessed using Cochran’s Q statistic (Cochran, Citation1954), with a significant Q test indicating the presence of heterogeneity. To assess the amount of heterogeneity, we used the I2 statistic (range: 0–100%; ≥ 50% indicates substantial heterogeneity; [Deeks et al., Citation2022]). As part of the multilevel approach, we differentiated between heterogeneity related to between-study and between-outcome differences (Assink & Wibbelink, Citation2016).
Due to substantial between-study heterogeneity, we performed several moderator analyses in the subgroups of children/adolescents and adults based on the meta-analytical approach used for primary analyses. Analyses were limited to the higher-level outcome categories of mental symptoms and positive mental health as the larger number of effect estimates available for these analyses resulted in higher statistical power and reduced the number of statistical tests (i.e. type-I error inflation). We used subgroup analyses for categorical variables (e.g. intervention settings) when at least three effect sizes per subgroup were available and meta-regression for omnibus moderation test and continuous moderators (e.g. intervention duration), with a significant QM statistic indicating the presence of a moderator effect. Moderator analyses were performed for control conditions (passive vs. active), sample typeFootnote2 (clinical vs. non-clinical), intervention intensity (low- vs. high-intensity; [Shafran et al., Citation2021]), intervention setting (individual vs. group), intervention location (low/lower-middle-income vs. upper-middle/high-income following the World Bank Atlas classification; [World Bank, Citation2022]), intervention providers (lays/non-professionals vs. professionals), theoretical basis (CBT vs. others), intervention duration and publication year. In case of children/adolescents, we also compared effect estimates from interventions targeting children/adolescents versus parents, caregivers, or families.
Sensitivity analyses for mental symptoms and positive mental health were performed based on the risk of bias assessment (for domains with relevant between-study variation), ICC estimates for cRCTs, and study designs. The certainty of evidence for primary outcomes at post-intervention was assessed in duplicate for both age groups using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE; [Schünemann et al., Citation2022]).
3. Results
3.1. Search outcomes
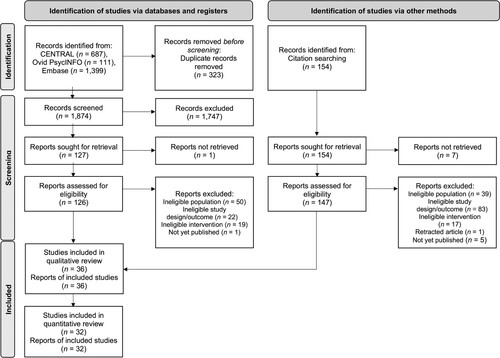
Databases yielded 2197 records, and 323 duplicates were removed. Of 1874 records screened at title/abstract level, 127 were assessed at full-text level. Moreover, 154 records were identified by citation searching of which 147 were assessed at full-text level. Taken together, this resulted in 36 eligible studies for the qualitative review and 32 eligible studies (from 32 records) for the quantitative synthesis (see ). Of these 32 studies, 10 studies reported outcomes for children and adolescents and 27 for adults, with five studies reporting data for both age groups.
3.2. Study characteristics
The characteristics of 36 included studies published between 2001 and 2022 are presented in . The studies were performed in various countries, including Germany, Jordan (five studies each), Lebanon, the United States, Uganda (three studies each), Austria, Tanzania, and Turkey (two studies each). Transdiagnostic interventions included the WHO interventions Problem Management Plus (PM+; 5 studies) and Self-Help Plus (SH+; 3 studies) in adult samples, as well as Early Adolescent Skills for Emotions (EASE; 2 studies), and Teaching Recovery Techniques (TRT, 2 studies) for children/adolescents. Other interventions were only examined in single studies.
Table 2. Characteristics of the included studies.
Most studies reported on refugees and/or asylum seekers (children/adolescents: 60%; adults: 89.7%), while fewer studies included internally displaced persons (children/adolescents: 26.6%; 6.9%) and had mixed samples (children/adolescents: 13.3%; adults: 3.4%). In both age groups, most studies were designed as RCTs (children/adolescents: 66.7%; adults: 82.8%), while cRCTs were less common (children/adolescents: 33.3%; adults: 17.2%).
The 36 studies comprised 14,133 observations from 5299 forcibly displaced persons in total (children/adolescents: 1427; adults: 3872). The mean age of was 13.00 years [SD 3.16] for children/adolescents and 34.10 years [SD 5.32] for adult samples. On average, 42.5% [SD 22.2] of the child/adolescent samples were female, while 58.2% [SD 26.3] of the adult samples self-identified as women. The most common triggers for displacement were wars (children/adolescents: 66.7%; adults: 58.6%), while mixed events (children/adolescents: 20.0%; adults: 20.7%) and armed conflicts (children/adolescents: 13.3%; adults: 20.7%) were less common. Interventions for children/adolescents had a mean duration of 8 weeks (range: 0.5–20 weeks) and were comparable long for adults (9 weeks; range: 1–52 weeks). Interventions were delivered in host/resettlement countries (children/adolescents: 46.7%; adults: 79.3%) or in refugee camps (children/adolescents: 53.3%; adults: 17.2%), with only one intervention for adults being delivered in the home country (3.4%). When classifying interventions according to components presented in , the vast majority of studies combined different components (children/adolescents: 93.3%; adults: 96.6%). Across both age groups, the most frequently used components were psychoeducation (children/adolescents: 73.3%; adults: 75.9%), problem management (children/adolescents: 53.3%; adults: 58.6%), and relaxation (children/adolescents: 53.3%; adults: 48.3%). Active (mostly enhanced care as usual; children/adolescents: 53.3%; adults: 40.0%) and passive control conditions (mostly wait-list controls; children/adolescents: 53.3%; adults: 60.0%) were almost equally common.
3.3. Quality appraisal
3.3.1 Risk of bias
Overall, there was a moderate to high risk of bias (see and SM5). Main flaws across the included studies and outcomes were found for outcome measurement due to reliance on self-report measures in non-blinded interventions (100.0% some concerns or high-risk ratings in both age groups), selective reporting (children/adolescents: 100%, adults: 66.3%), randomization (children/adolescents: 25.9%; adults: 30.0%), deviations from interventions (children/adolescents: 25.2%; adults: 27.5%), and missing outcome data (children/adolescents: 18.5%; adults: 21.3%).
3.3.2 Publication bias
Meta-regression models provided no clear evidence for an association of standard errors and effect size estimates (children/adolescents: QM[19] = 2.34, p = .142; adults: QM[57] = 1.17, p = .283). However, visual inspections of contour-enhanced funnel plots suggested the presence of a publication bias for the analyses on adult samples (see SM6). Effect sizes were more likely to fall into the right significant border area of the funnel plot, while a comparable number of studies balancing these findings on the left side was missing.
3.4. Quantitative findings
3.4.1 Pairwise meta-analyses – main analyses
Children and adolescents. Thirteen studies (comprising 27 effect sizes across four outcomes from 2776 observations of 1427 participants) were included in the meta-analyses on children and adolescents. Across all mental symptom categories, we found no evidence for an effect favouring transdiagnostic psychosocial interventions, M(SMD) = 0.08, 95% CI [−0.21, 0.36], p = .562, with moderate heterogeneity, Q(21) = 75.31, p < .001, I2 = 69.9% (see and ). The majority of heterogeneity derived from between-study differences (49.5%), while between-outcome differences accounted for 20.4%. To note, nine of 22 effect sizes (40.9%) pointed to potentially negative intervention effects, however, these effects remained non-significant across all studies. Moreover, for none of the single symptom categories, there was evidence for an effect favouring psychosocial interventions, M(SMDs)–0.22–0.19, ps ≥ .271. Also for positive mental health, there was no evidence for an effect favouring transdiagnostic psychosocial interventions, M(SMD)=−0.03, 95% CI [–0.26, 0.20], p = .823, with moderate heterogeneity in this analysis, Q(4) = 5.93, p = .205 and I2 = 39.1%. For this outcome, three out of five effect sizes (60.0%) were numerically negative. However, again, none of the primary study effects was significant. Overall certainty of evidence was very low for all analyses in this age group (see SM7).
Figure 3. Forest plots of the multilevel meta-analyses on mental symptoms and the traditional meta-analysis on positive mental health in child/adolescent samples. Positive effect estimates indicate an effect favoring transdiagnostic psychosocial interventions over control conditions. CI: confidence interval; df: degree of freedom; I2: heterogeneity index in percentage (range: 0–100%); Q: Cochran's Q statistic with p value.
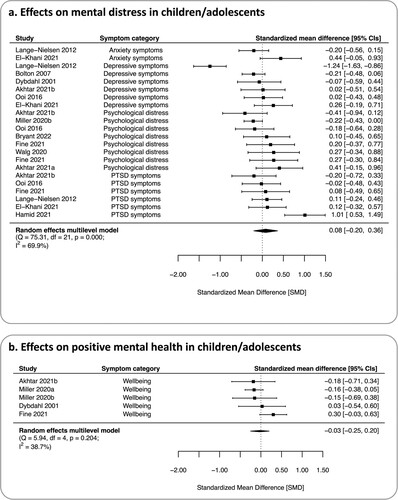
Table 3. Results of main analyses (multilevel and traditional meta-analyses) for primary outcomes comparing transdiagnostic psychosocial interventions with control conditions.
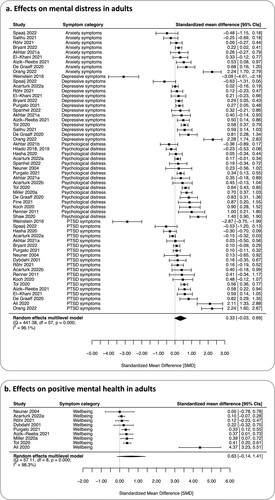
Adults. Twenty-six studies (comprising 67 effect sizes across four outcomes from 11,357 observations of 3872 participants) were included in the meta-analyses on adult samples (see ). Across all mental symptom categories, we found no evidence for an effect favouring transdiagnostic psychosocial interventions, M(SMD) = 0.33, 95% CI [–0.03, 0.69], p = .072, with considerable heterogeneity, Q(57) = 441.38, p < .001, I2 = 96.1%, of which the majority was accounted for by between-study differences (95.3%), while between-outcome differences were of minor importance (0.8%). Examining single symptom categories, we found evidence for a small to moderate effect in favour of transdiagnostic psychosocial interventions for psychological distress, M(SMD) = 0.44, 95% CI [0.22, 0.67], p < .001, again with substantial heterogeneity, Q(15) = 67.35, p < .001, I2 = 82.0%. For other symptom categories and positive mental health, there was no evidence for an effect favouring transdiagnostic psychosocial interventions, M(SMDs) 0.22–0.63, ps ≥ .111. Overall certainty of evidence was very low for all analyses on adult samples (see SM7).
Figure 4. Forest plots of the multilevel meta-analyses on mental symptoms and the traditional meta-analysis on positive mental health in adult samples. Positive effect estimates indicate an effect favoring transdiagnostic psychosocial interventions over control conditions. CI: confidence interval; df: degree of freedom; I2: heterogeneity index in percentage (range: 0–100%); Q: Cochran's Q statistic with p value.
3.4.2 Moderators
Moderator analyses were performed for mental symptoms and positive mental health in both age groups (see ).
Table 4. Results of moderator analyses on categorial and continuous variables.
Control condition. We did not find evidence for a moderator effect of the type of control condition (passive vs. active control) on mental symptoms and positive mental health, ps ≥ .203.
Clinical vs. non-clinical samples. There was no evidence for a moderation by sample type in children and adolescents, while effects on mental symptoms in adults were larger and significant in clinical compared to non-clinical samples, QM(1,55) = 8.08, p = .006.
Intervention intensity. While the small number of studies did not allow for an analysis of intervention intensity in children/adolescents, the analyses in adult samples provided no evidence for differences between low- and high-intensity interventions, ps ≥ .152.
Intervention setting. In adult samples, there was no evidence for a moderation by intervention setting (individual vs. group), p = .229.
Intervention location. When we compared effects for interventions delivered in low/lower middle-income countries with those delivered in upper-middle/high-income countries, we found no moderation, ps ≥ .542.
Intervention providers. When comparing interventions delivered by professionals with those delivered by lays or non-professionals, we found no moderation, ps ≥ .295.
Target group. For children and adolescents, we examined whether interventions solely targeting children/adolescents differed from interventions delivered to parents, caregivers or families. However, we found no moderator effect for mental symptoms, p = .282.
Intervention duration. Analyses examining intervention duration as moderator yielded no evidence for a moderator effect, ps ≥ .068.
Theoretical basis. When we compared interventions grounded in CBT with those relying on other concepts (e.g. creative play; [Bolton et al., Citation2007]), we found no moderator effects in adults, p = .376.
Improvement over time. Meta-regressions examining publication year as moderator did not provide evidence for changes of efficacy over time, ps ≥ .250.
3.4.3 Sensitivity analyses
Risk of bias. We re-estimated our primary analyses on mental symptoms excluding effect estimates at risk of different bias domains (i.e. some concerns or high risk; see SM8). For children and adolescents, our results on mental symptoms and positive mental health remained unchanged. All re-estimations provided no evidence for an effect favouring transdiagnostic psychosocial interventions, M(SMDs) 0.08–0.15, ps ≥ .276 For adult populations, sensitivity analyses provided a more positive view on transdiagnostic psychosocial interventions. All analyses on mental symptoms correcting for single bias domains provided evidence for a small to moderate favourable intervention effect, M(SMDs) 0.21–0.50, ps ≤ .047. For positive mental health, excluding effect estimates at risk for bias caused by randomization and selective reporting yielded small favourable effects of transdiagnostic psychosocial interventions, ps < .001.
Impact of cRCTs. We re-estimated our meta-analyses on primary outcomes using a more conservative estimate of ICC for cRCTs (ICC = .10; see SM9). For both age groups, our results remained unchanged. Also, when we excluded cRCTs from our analyses, our results remained the same.
4. Discussion
The present review was the first to provide an evidence synthesis on the efficacy of transdiagnostic psychosocial interventions to promote mental health and/or to prevent mental symptoms in forcibly displaced persons. Our analyses revealed substantial age-related differences: While there was no evidence for beneficial effects in children and adolescents, there was some (at least close-to-significance) evidence favouring transdiagnostic psychosocial interventions over control conditions in adults. Except for larger intervention effects in clinical compared to non-clinical adult samples, various moderator analyses could not account for residual between-study differences. Moreover, sensitivity analyses pointed to a relevant impact of risk of bias. When removing effect estimates of studies at risk for bias from our analyses, all analyses on mental symptoms in adult samples provided evidence favouring interventions over control conditions. Thus, insufficient study quality may have resulted in an underestimation of intervention effects in adult samples, while studies at high risk of bias did not account for our results in child and adolescent samples.
The finding that there is no evidence for the efficacy of transdiagnostic psychosocial interventions in children and adolescents, with overall 44.4% of the effect sizes even pointing to potentially negative effects, is alarming. Children and adolescents make up for almost half of the population of forcibly displaced persons and are exposed to numerous hardships of forced displacement in a crucial phase of their physical, emotional, social and cognitive development (Scharpf et al., Citation2021; United Nations High Commissioner for Refugees, Citation2021). Thereby, they are at particular risk for the onset and persistence of mental disorders (Fazel et al., Citation2012), making mental health promotion and prevention of mental symptoms a priority in this age group (World Health Organization, Citation2018). Our findings tie in with a recent meta-analysis on the efficacy of psychotherapies for PTSD and depression in forcibly displaced children and adolescents finding no evidence for an effect favouring psychotherapies over control conditions (Morina & Sterr, Citation2019) and another review finding symptom reductions only for one out of three programmes (Alzaghoul et al., Citation2022). These results raise the question of what may account for these null effects. In general, research on child and adolescent populations was rare and often associated with low study quality, which may also reflect that research is difficult to conduct due to cultural differences in the perception and presentation of mental symptoms as well as in the conceptualization and stigmatization of mental illness (Frounfelker et al., Citation2020; Kananian et al., Citation2020). Moreover, levels of importance placed on the value of research are likely to differ between cultures (Frounfelker et al., Citation2020). These difficulties may impact on the design and delivery of interventions, which both have to be critically evaluated for cultural appropriateness (Betancourt et al., Citation2020; Hodes & Vostanis, Citation2019). Difficulties specific to intervention delivery and adherence in children and adolescents (e.g. ethical concerns when assigning children to control conditions; [Gearing et al., Citation2012]) may add to these general challenges in the work with forcibly displaced persons (Silove et al., Citation2017). Furthermore, the low study quality may also reflect that research has not been a priority in this population. Interventions may be tailored to meet urgent demands in forcibly displaced children/adolescents (e.g. adjusting to a new educational system) that could not be captured appropriately by standard outcome measures. Our finding of more heterogeneous responses across different outcomes supports the idea of larger between-outcome heterogeneity in children/adolescents compared to adults. This in line with previous studies on the multidimensionality of responses to stress in children (Infurna & Luthar, Citation2018; Martinez-Torteya et al., Citation2017), which may also apply to intervention effects in stressor-exposed populations. Therefore, previous reviews on psychosocial interventions for children and adolescents called for multi-outcome research and the inclusion of positive mental health outcomes (e.g. wellbeing and resilience; [Frounfelker et al., Citation2020; Uphoff et al., Citation2019]). For the first time, the current review included these outcomes, however, without finding evidence for favourable effects. The only study providing evidence for a favourable effect of transdiagnostic interventions in children and adolescents assessed PTSD symptoms as single outcome (Hamid et al., Citation2021), finding a mix of information on dental/oral health and psychosocial support to have a large favourable effect. In this study, psychosocial support included trauma healing, information on (not further specified) ‘friendly behavior’ and positive visions of the future. However, as other studies using similar interventions provided no evidence for favourable effects (e.g. Ooi et al., Citation2016), differences in intervention components may not (fully) account for the differential efficacy. Another reason for the null effects obtained by our meta-analyses may lie in our findings being limited to post-intervention assessments instead of trajectories of mental health. Intervention effects may become more visible over longer periods (Frounfelker et al., Citation2020). However, the small number of studies including follow-up periods in our analyses point to even smaller intervention effects over time (El-Khani et al., Citation2021).
Overall, our findings may partly be accounted for by specific challenges in delivering interventions to children and adolescents after displacement. Due to the very low certainty of evidence across all outcomes, we have very little confidence in the effect estimate provided by our analyses and the true effect is likely to be substantially different (Schünemann et al., Citation2022). Thus, the small body of evidence does not allow to answer the question of whether interventions in this age group have favourable effects, have no effect, or may even have negative effects. However, in none of the included studies, numerically negative effects were significant, thus, negative effect sizes might also reflect variation around a ‘true’ null effect or a decrease of stigma and/or an increase in awareness of mental symptoms after the intervention as observed previously for other interventions (Ertl et al., Citation2011; Im et al., Citation2018). However, the question remains open why this effect should occur (more pronounced) at younger ages. Unfortunately, we were unable to perform several moderator analyses for children/adolescents as no or only one study was available per subgroup. Thus, based on our findings we cannot answer the question of what makes these interventions ineffective. However, the weak evidence – in line with previous reviews (Alzaghoul et al., Citation2022; Soltan et al., Citation2020; Soltan et al., Citation2022; Morina & Sterr, Citation2019) – points to the urgent need to critically evaluate and improve interventions for young forcibly displaced persons and to rigorously test their efficacy and (their likely questionable) cost-effectiveness. In case, a more solid evidence base provides support for the finding that existing interventions have no favourable effects for children/adolescents, care providers need to respond with adapting existing programmes or develop new evidence-based prevention programmes. However, so far, our findings cannot be used for such impactful decisions.
Findings in the adult sample were more promising by at least providing evidence for a small to moderate effect of transdiagnostic psychosocial interventions on overall mental symptoms and positive mental health after the exclusion of effect estimates at high risk of bias. However, these findings also must be interpreted with caution. While we found evidence for an effect favouring psychosocial interventions on overall mental symptoms in our sensitivity analyses, this effect seems to arise mainly from intervention effects on psychological distress, whereas we found no evidence for the efficacy in reducing single symptom categories. At the same time, the greater efficacy for overall psychological distress may also provide evidence for the truly transdiagnostic nature of the interventions. Moreover, we found larger favourable effects for clinical compared to non-clinical populations. This may reflect that intervention effects can only unfold if participants experience a certain level of distress and interventions may not be useful for stressor-exposed populations not (yet) experiencing elevated levels of distress. The finding may also point to some studies underestimating intervention effects due to floor effects (i.e. already low symptoms cannot be further reduced), but may also show that secondary prevention might be more important in this population. Besides this finding, the large amount of heterogeneity could not be accounted for by other moderators like intervention intensity. This may be attributed to the heterogeneity of interventions ranging from (unstructured) supportive counselling (Neuner et al., Citation2004) to interventions specifically addressing coping with trauma (El-Khani et al., Citation2021). Moreover, moderator effects may also be more complex and interdependent. For instance, we could not test whether high-intensity interventions were more effective in low- or high-income countries as the number of studies was too small for such analyses. Future reviews based on more primary studies may shed light on interactions of moderators. Also, overall low study quality reflected in a heightened risk of bias in different domains may cause unsystematic variance.
Looking at the studies with large effect estimates in adult samples, that is, focusing on studies that may report on particular auspicious interventions, six studies emerged (Ali, Citation2020; de Graaff et al., Citation2020; Koch et al., Citation2020; Orang et al., Citation2022; Renner et al., Citation2011; Shaw et al., Citation2021). In a study with moderate risk of bias, de Graaff et al. (Citation2020) compared the efficacy of peer-provided problem management plus (PM+) combined with care as usual (CAU) to CAU only, finding PM + (Dawson et al., Citation2015), a combination of stress management, problem management, behavioural activation and strengthening of social support, to reduce mental symptoms. Moreover, Koch et al. (Citation2020) examined the efficacy of a transdiagnostic intervention to enhance emotion regulation finding a large effect on psychological distress. Both interventions clearly address transdiagnostic factors, however, with PM + addressing a broad set of factors and the emotion regulation training focusing on a single factor. The remaining four studies with large effect sizes in adult samples were associated with at least ‘some concerns’ for risk of bias in three out of five domains (Ali, Citation2020; Orang et al., Citation2022; Renner et al., Citation2011; Shaw et al., Citation2021). Thus, so far, no clear picture of effective interventions can be drawn.
Overall, there is little research on mental health promotion and prevention of mental symptoms in forcibly displaced persons compared to research on similar interventions in other populations at lower risk for mental disorders (Conley et al., Citation2015; Galante et al., Citation2021). Moreover, the present review again showed that a major shortcoming of previous research is the focus on interventions delivered in upper-middle to high-income countries (Nosè et al., Citation2017; Soltan et al., Citation2022; Uphoff et al., Citation2019). In case of our quantitative synthesis, 70 of 94 effect sizes (74.5%) came from upper-middle- or high-income countries, which stands in strong contrast to the fact that 82% of forcibly displaced persons live and need care in low-income and developing countries (United Nations High Commissioner for Refugees, Citation2022b; Wainberg et al., Citation2017). Our moderator analysis did not point to relevant differences between the efficacy of interventions delivered in upper-middle-/high-income and low-/lower-middle-income countries, but our review does not allow for strong conclusions on interventions delivered in the latter countries. It is likely that the location of intervention delivery matters (Soltan et al., Citation2022), yet the current state of research does not allow for a more nuanced picture. Future studies need to overcome this mismatch between care needs and research efforts.
4.1. Limitations
For this review, we searched four databases, thus, we cannot exclude that we missed relevant studies. To make up for the relatively small number of databases, we performed extensive citation searching of related (umbrella) systematic reviews and included studies, resulting in another two relevant studies. Moreover, we made some minor changes from the preregistration of this systematic review that are detailed in SM1. In line with recommendations of the Cochrane collaboration (Cuijpers et al., Citation2017; Higgins et al., Citation2022), we refrained from analysing pre-to-post changes within our quantitative summary, as we could not obtain data on pre-to-post value correlations. In such cases, analyses of pre-to-post changes may yield misleading results and ‘correct’ unsuccessful randomization processes, as seen in some of the included studies (Weinstein et al., Citation2016). Thus, our findings may diverge from those of the study authors who mostly based their conclusions on pre-to-post changes or between-group comparisons of pre-to-post changes. Moreover, we were not able to perform a (component) network meta-analysis. Such an analysis would be valuable to compare different interventions with each other and rank intervention components according to their efficacy. In case of our review, the method was not applicable as requirements for network meta-analyses (Salanti, Citation2012) were not met (i.e. there were non-random differences in effect modifiers like symptom severity between comparisons). Future meta-analyses based on more comparable studies may make use of network meta-analysis to shed light on the relative efficacy of intervention components.
Moreover, some of the included studies also aimed at targeting other outcomes than mental symptoms and positive mental health (e.g. reducing pain; [Hasha et al., Citation2020]), enhancing emotion regulation capacities (Koch et al., Citation2020), improving sleep quality (Röhr et al., Citation2020), promoting oral health (Hamid et al., Citation2021) or need satisfaction (Weinstein et al., Citation2016). These outcomes were not part of the current review. Thus, our results only allow for conclusions on mental health, but should not be misinterpreted as overall evaluation of the included interventions as these may be effective in addressing other outcomes.
A major issue of included studies was the imprecise definition of interventions and study samples. In many cases, it remained unclear whether interventions aimed at mental health promotion, prevention or even treatment of mental disorders. For the purpose of the current review, we followed intervention aims as defined by study authors and excluded studies that specifically focused on the treatment of mental disorders. However, in some cases, this may result in inconsistent in- and exclusion of interventions. The most accurate distinction would base on sample characteristics (Tol, Citation2015), yet, mental health states were only insufficiently assessed in most studies.
Another limitation is the large heterogeneity of samples included in the present review. Assuming that being displaced from Ukraine due to the Russian military offensive is similar to a displacement from Syria as consequence of civil war is highly oversimplifying. At the same time, even two persons forced to leave the same country may have entirely different life experiences, may be exposed to different stressors, and may therefore have different requirements to transdiagnostic psychosocial interventions. So far, the amount of research does not allow for research questions on single conflict settings or subpopulations. However, such research is needed to tailor interventions to diverse needs at individual but also cultural level.
Overall, study quality was low, and risk of bias was high across all analyses. This may also reflect the challenges of conducting high-quality research under circumstances that may not allow for rigid research protocols. Methodological shortcomings of these studies are understandable, but at the same time impede establishment of a solid evidence base (Frounfelker et al., Citation2020).
4.2. What can we learn for current and future crises?
The current systematic review does not allow for a strong recommendation in favour of any transdiagnostic psychosocial intervention. However, we may learn from its findings for interventions in face of future crises.
First, our findings show that there is an urgent need for action in the field of transdiagnostic psychosocial interventions for children and adolescents. There is no evidence for the efficacy of existing interventions, suggesting revisiting those with at least small to medium favourable effects (Hamid et al., Citation2021) and exploring reasons for the lack of efficacy for other interventions. These interventions may fail to meet the complex demands of children and adolescents after forcibly displacement by being insufficiently adapted to children/adolescents’ life experiences, provided at the wrong time (i.e. before established safety) or in unfavourable settings (e.g. refugee camps), or may be ineffective as most of them only target individuals but not their caregivers and families (Frounfelker et al., Citation2020). Embedding transdiagnostic interventions in broader concepts addressing multilevel problems of forcibly displaced children and adolescents (e.g. making friends, participating in school) after establishing basic human rights may have a greater potential to improve mental health or to prevent mental symptoms. Current and future crises should be used to understand children and adolescents’ needs after forced displacement in greater depth and to actively involve them in intervention design, delivery, and evaluation.
Second, in adult populations, there is a strong need for high-quality research allowing to examine intervention components. For the current review, we were not able to make use of network meta-analyses to examine the efficacy of single components. However, as most interventions are multi-component training programmes, it is essential to disentangle their efficacy to combine most efficient components into one programme. For such studies, it would also be essential to provide detailed information on delivered interventions (van Agteren et al., Citation2021; Michie et al., Citation2013). A more detailed description of intervention characteristics may also allow to identify circumstances that account for the surprising (in)efficacy of the same intervention in similar contexts (De Graaff et al., Citation2020; Spaaij et al., Citation2022).
Third, interventions and samples included in this review were heterogeneous. This may also point to the fact that a deeper understanding of effect modifiers for single interventions is needed. Recently registered traditional (Schäfer et al., Citation2022) and individual-participant data (IPD; [de Graaff et al., Citation2022]) meta-analysis projects on the WHO programmes PM + and Step-by-Step may point into this direction. However, such projects are also urgently needed for interventions delivered to children and adolescents like EASE (Brown et al., Citation2019; Dawson et al., Citation2019). The combination of traditional and IPD analyses may allow to identify study- and participant-level moderators of specific interventions.
Fourth, future research may put larger efforts into the state-of-the-art assessment of positive mental health (Chmitorz et al., Citation2018; Kalisch et al., Citation2021). Deviating from our initial plan, we were unable to perform a meta-analysis on resilience due to an insufficient number of studies reporting on this outcome. Especially when examining interventions to promote mental health, outcomes beyond mental symptoms may be more eligible to capture intervention effects.
5. Conclusion
The present review was the first to summarize evidence on the efficacy of both low- and high-intensity transdiagnostic psychosocial interventions for forcibly displaced persons in different age groups. Our analyses provided weak evidence for an effect favouring transdiagnostic psychosocial interventions over control conditions for adult but not for child and adolescent populations. Substantial between-study heterogeneity could not be explained by moderators except for larger favorable effects in clinical compared to non-clinical samples in adults. The findings of the current review point to an urgent need of improving transdiagnostic psychosocial interventions for children and adolescents and to identify efficient training components in adult populations. Current and future crises require firm humanitarian aid and may also provide an opportunity to examine needs in diverse populations of forcibly displaced persons in greater depth to tailor future interventions.
Authors contributions
SKS: conceptualization, methodology, formal analysis, data curation, writing (original draft), visualization, project administration; AMK: conceptualization, methodology, data curation, writing (original draft), project administration; SL: conceptualization, data curation, writing (review & editing), project administration; JB: data curation, writing (review & editing); MS: data curation, writing (review & editing); JSW: conceptualization, methodology, data curation, writing (review & editing); KL: conceptualization, methodology, resources, writing (review & editing), supervision.
Supplemental Material
Download MS Word (420.8 KB)Acknowledgements
We acknowledge the assistance of Carolina Pank, Javen Schneider-Rothhaar and Kirsten Stewens in preparing this systematic review. Moreover, we thank all authors of primary studies who provided additional information on their studies.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Data are available upon reasonable request from the corresponding author.
Additional information
Funding
Notes
1 Multi-arm studies (e.g. [50]) included in this review compared disorders-specific psychotherapy with unspecific health promotion or psychosocial support programs (as relevant to this review) and no-intervention controls. In these cases, we only included the latter two groups, while the disorder-specific psychotherapy was not considered.
2 Clinical samples were those that on average exceeded the cut-off criteria in at least one standard mental health measure at baseline assessment (e.g. Patient Health Questionnaire 9 [74]) or were explicitly recruited for high mental burden.
References
- *Acarturk, C., Uygun, E., Ilkkursun, Z., Carswell, K., Tedeschi, F., Batu, M., Eskici, S., Kurt, G., Anttila, M., Au, T., Baumgartner, J., Churchill, R., Cuijpers, P., Becker, T., Koesters, M., Lantta, T., Nosè, M., Ostuzzi, G., Popa, M., … Purgato, M. (2022a). Effectiveness of a WHO self-help psychological intervention for preventing mental disorders among Syrian refugees in Turkey: A randomized controlled trial. World Psychiatry, 21, 88–95. https://doi.org/10.1002/wps.20939
- *Acarturk, C., Uygun, E., Ilkkursun, Z., Yurtbakan, T., Kurt, G., Adam-Troian, J., Senay, I., Bryant, R., Cuijpers, P., Kiselev, N., McDaid, D., Morina, N., Nisanci, Z., Park, A. L., Sijbrandij, M., Ventevogel, P., & Fuhr, D. C.. (2022b). Group problem management plus (PM+) to decrease psychological distress among Syrian refugees in Turkey: A pilot randomised controlled trial. BMC Psychiatry, 22. https://doi.org/10.1186/s12888-021-03645-w
- Ager, A., Akesson, B., Stark, L., Flouri, E., Okot, B., McCollister, F., & Boothby, N. (2011). The impact of the school-based psychosocial structured activities (PSSA) program on conflict-affected children in northern Uganda. Journal of Child Psychology and Psychiatry, 52, 1124–33. https://doi.org/10.1111/j.1469-7610.2011.02407.x
- *Aizik-Reebs, A., Yuval, K., Hadash, Y., Gebreyohans, G. S., & Bernstein, A. (2021). Mindfulness-based trauma recovery for refugees (MBTR-R): randomized waitlist-control evidence of efficacy and safety. Clinical Psychological Science, 9, 1164–84. https://doi.org/10.1177/2167702621998641
- *Akhtar, A., Giardinelli, L., Bawaneh, A., Awwad, M., Al-Hayek, H., Whitney, C., Jordans Mark, J. D., Sijbrandij, M., Cuijpers, P., Dawson, K., Bryant, R. (2021a). Feasibility trial of a scalable transdiagnostic group psychological intervention for Syrians residing in a refugee camp. European Journal of Psychotraumatology, 12, 1932295. https://doi.org/10.1080/20008198.2021.1932295
- *Akhtar, A., Malik, A., Ghatasheh, M., Aqel Ibrahim, S., Habashneh, R., Dawson Katie, S., Watts, S., Jordans Mark, J. D., Brown, F., Sijbrandij, M., Cuijpers, P., & Bryant, R. (2021b). Feasibility trial of a brief scalable psychological intervention for Syrian refugee adolescents in Jordan. European Journal of Psychotraumatology, 12, 1901408. https://doi.org/10.1080/20008198.2021.1901408
- Aldao A, Gee DG, De Los Reyes A, & Seager, I. Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Development and Psychopathology 2016;28:927–46. https://doi.org/10.1017/S0954579416000638
- Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217–37. https://doi.org/10.1016/j.cpr.2009.11.004
- *Ali, A. (2020). Efficiency of intervention counseling program on the enhanced psychological well-being and reduced post-traumatic stress disorder symptoms among Syrian women refugee survivors. Clinical Practice & Epidemiology in Mental Health, 16, 134–41. https://doi.org/10.2174/1745017902016010134
- Alzaghoul, A. F., McKinlay, A. R., & Archer, M. (2022). Post-traumatic stress disorder interventions for children and adolescents affected by war in low- and middle-income countries in the Middle East: Systematic review. BJPsych Open, 8, e153. https://doi.org/10.1192/bjo.2022.552
- Assink, M., & Wibbelink, C. J. (2016). Fitting three-level meta-analytic models in R: A step-by-step tutorial. The Quantitative Methods for Psychology, 12, 154–74. https://doi.org/10.20982/tqmp.12.3.p154
- Begg, C. B., & Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 1088–101. https://doi.org/10.2307/2533446
- Bendavid, E., Boerma, T., Akseer, N., Langer, A., Malembaka Espoir, B., Okiro Emelda, A., Wise Paul, H., Heft-Neal, S., Black Robert, E., Bhutta Zulfiqar, A., Bhutta, Z., Black, R., Blanchet, K., Boerma, T., Gaffey, M., Langer, A., Spiegel, P., Waldman, R., & Wise, P. (2021). The effects of armed conflict on the health of women and children. The Lancet, 397, 522–32. https://doi.org/10.1016/S0140-6736(21)00131-8
- *Betancourt, T. S., Berent, J. M., Freeman, J., Frounfelker Rochelle, L., Brennan Robert, T., Abdi, S., Maalim, A., Abdi, A., Mishra, T., Gautam, B., Creswell John, W., & Beardslee William, R. (2020). Family-based mental health promotion for Somali bantu and bhutanese refugees: Feasibility and acceptability trial. Journal of Adolescent Health, 66, 336–44. https://doi.org/10.1016/j.jadohealth.2019.08.023
- Blackmore, R., Boyle, J. A., Fazel, M., Ranasinha, S., Gray Kylie, M., Fitzgerald, G., Misso, M., & Gibson-Helm, M. (2020). The prevalence of mental illness in refugees and asylum seekers: A systematic review and meta-analysis. PLOS Medicine, 17, e1003337. https://doi.org/10.1371/journal.pmed.1003337
- Bogic, M., Njoku, A., & Priebe, S. (2015). Long-term mental health of war-refugees: A systematic literature review. BMC International Health and Human Rights, 15, 29. https://doi.org/10.1186/s12914-015-0064-9
- *Bolton, P., Bass, J., Betancourt, T., Speelman, L., Onyango, G., Clougherty, K. F., Neugebauer, R., Murray, L., & Verdeli, H. (2007). Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA, 298(5), 519–527. https://doi.org/10.1001/jama.298.5.519
- Bower, P., Kontopantelis, E., Sutton, A., Kendrick, T., Richards, D. A., Gilbody, S., Knowles, S., Cuijpers, P., Andersson, G., Christensen, H., Meyer, B., Huibers, M., Smit, F., van Straten, A., Warmerdam, L., Barkham, M., Bilich, L., Lovell, K., Liu, & E. T.-H.. (2013). Influence of initial severity of depression on effectiveness of low intensity interventions: Meta-analysis of individual patient data. BMJ, 346, f540. https://doi.org/10.1136/bmj.f540
- Brown, F. L., Steen, F., Taha, K., Aoun, M., Bryant, R., Jordans Mark, J. D., Malik, A., van Ommeren, M., Abualhaija, A., Aqel Ibrahim, S., Ghatasheh, M., Habashneh, R., Sijbrandij, M., El Chammay, R., Watts, S., & Akhtar, A. (2019). Early adolescent skills for emotions (EASE) intervention for the treatment of psychological distress in adolescents: Study protocol for randomised controlled trials in Lebanon and Jordan. Trials, 20, 545. https://doi.org/10.1186/s13063-019-3654-3
- *Bryant, R. A., Bawaneh, A., Awwad, M., Al-Hayek, H., Giardinelli, L., Whitney, C., Jordans Mark, J. D., Cuijpers, P., Sijbrandij, M., Ventevogel, P., Dawson, K., & Akhtar, A. (2022a). Effectiveness of a brief group behavioral intervention for common mental disorders in Syrian refugees in Jordan: A randomized controlled trial. PLOS Medicine, 19, e1003949. https://doi.org/10.1371/journal.pmed.1003949
- Bryant, R. A., Schnurr, P. P., & Pedlar, D. (2022b). Addressing the mental health needs of civilian combatants in Ukraine. The Lancet Psychiatry, 9, 346–7. https://doi.org/10.1016/S2215-0366(22)00097-9
- Carlsson, J., & Sonne, C. (2018). Mental health, pre-migratory trauma and post-migratory stressors among adult refugees. In N. Morina, & A. Nickerson (Eds.), Mental Health of Refugee and Conflict-Affected Populations: Theory, Research and Clinical Practice (pp. 15–35). Springer International Publishing. https://doi.org/10.1007/978-3-319-97046-2_2
- Charlson, F., van Ommeren, M., Flaxman, A., Cornett, J., Whiteford, H., & Saxena, S. (2019). New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. The Lancet, 394, 240–8. https://doi.org/10.1016/S0140-6736(19)30934-1
- Chmitorz, A., Kunzler, A., Helmreich, I., Tüscher, O., Kalisch, R., Kubiak, T., Wessa, M., & Lieb, K.. (2018). Intervention studies to foster resilience - A systematic review and proposal for a resilience framework in future intervention studies. Clinical Psychology Review, 59, 78–100. https://doi.org/10.1016/j.cpr.2017.11.002
- Cludius, B., Mennin, D., & Ehring, T. (2020). Emotion regulation as a transdiagnostic process. Emotion, 20, 37–42. https://doi.org/10.1037/emo0000646
- Cochran, W. G. (1954). Some methods for strengthening the common χ2 tests. Biometrics, 10, 417–51. https://doi.org/10.2307/3001616
- Conley, C. S., Durlak, J. A., & Kirsch, A. C. (2015). A meta-analysis of universal mental health prevention programs for higher education students. Prevention Science, 16, 487–507. https://doi.org/10.1007/s11121-015-0543-1
- Creswell, J. D. (2017). Mindfulness interventions. Annual Review of Psychology, 68, 491–516. https://doi.org/10.1146/annurev-psych-042716-051139
- Cuijpers, P., Weitz, E., Cristea, I. A., & Twisk J. (2017). Pre-post effect sizes should be avoided in meta-analyses. Epidemiology and Psychiatric Sciences, 26, 364–8. https://doi.org/10.1017/S2045796016000809
- Dawson, K. S., Bryant, R. A., Harper, M., Kuowei Tay, A., Rahman, A., Schafer, A., & van Ommeren, M. (2015). Problem Management Plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World psychiatry : official journal of the World Psychiatric Association (WPA), 14(3), 354–357. https://doi.org/10.1002/wps.20255
- Dawson, K. S., Watts, S., Carswell, K., Shehadeh Melissa, H., Jordans Mark, J.D., Bryant Richard, A., Miller Kenneth, E., Malik, A., Brown Felicity, L., Servili, C., & van Ommeren, M. (2019). Improving access to evidence-based interventions for young adolescents: Early adolescent skills for emotions (EASE). World Psychiatry, 18, 105. https://doi.org/10.1002/wps.20594
- *de Graaff, A., Cuijpers, P., McDaid, D., Park, A., Woodward, A., Bryant, R. A., Fuhr, D. C., Kieft, B., Minkenberg, E., & Sijbrandij, M.. (2020). Peer-provided problem management plus (PM+) for adult Syrian refugees: A pilot randomised controlled trial on effectiveness and cost-effectiveness. Epidemiology and Psychiatric Sciences, https://doi.org/10.1017/S2045796020000724
- de Graaff, A. M., Cuijpers, P., Acarturk, C., Akhtar, A., Alkneme, M. S., Aoun, M., Awwad, M., Bawaneh, A. Y., Brown, F. L., Bryant, R., Burchert, S., Carswell, K., Drogendijk, A., Engels, M., Fuhr, D. C., Hansen, P., van 't Hof, E., Giardinelli, L., Hemmo, M., Hessling, J. M., … STRENGTHS consortium (2022). Scalable psychological interventions for Syrian refugees in Europe and the Middle East: STRENGTHS study protocol for a prospective individual participant data meta-analysis. BMJ open, 12, e058101. https://doi.org/10.1136/bmjopen-2021-058101
- Deeks, J. J., Higgins, J. P. T., Altman, D. G. (2022). Chapter 10: Analysing data and undertaking meta-analyses. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, M.J. Page, & V.A. Welch (Eds.), Cochrane Handbook for Systematic Reviews of Interventions (pp. 241-84). www.training.cochrane.org/handbook.
- Drost, J., van der Does, W., van Hemert, A. M., Penninx Brenda, W.J.H., & Spinhoven, P. (2014). Repetitive negative thinking as a transdiagnostic factor in depression and anxiety: A conceptual replication. Behaviour Research and Therapy, 63, 177–83. https://doi.org/10.1016/j.brat.2014.06.004
- Dybdahl, R. (2001). Children and Mothers in War: An Outcome Study of a Psychosocial Intervention Program. Child Development, 72, 1214–1230. https://doi.org/10.1111/1467-8624.00343
- Ehlers, A. (2013). Trauma-focused cognitive behavior therapy for posttraumatic stress disorder and acute stress disorder. In G. Simos, & S. G. Hofmann (Eds.), CBT for Anxiety Disorders: A Practitioner Book (pp. 161–89). Wiley Blackwell. https://doi.org/10.1002/9781118330043.ch7
- Ekhtiari H, Rezapour T, Aupperle RL, & Paulus Martin, P. Chapter 10 - neuroscience-informed psychoeducation for addiction medicine: A neurocognitive perspective. In: Calvey T, Daniels WMU, eds. Progress in Brain Research. Elsevier 2017. 239–64. https://doi.org/10.1016/bs.pbr.2017.08.013
- *El-Khani, A., Cartwright, K., Maalouf, W., Haar, K., Zehra, N., Çokamay-Yılmaz, G., & Calam, R. (2021). Enhancing teaching recovery techniques (TRT) with parenting skills: Rct of trt + parenting with trauma-affected Syrian refugees in Lebanon utilising remote training with implications for insecure contexts and COVID-19. International Journal of Environmental Research and Public Health, 8652. https://doi.org/10.3390/ijerph18168652
- Ertl, V., Pfeiffer, A., Schauer, E., Elbert, T., & Neuner, F. (2011). Community-Implemented trauma therapy for former child soldiers in northern Uganda. JAMA, 306, 503–12. https://doi.org/10.1001/jama.2011.1060
- Fazel, M., Reed, R. V., Panter-Brick, C., & Stein, A. (2012). Mental health of displaced and refugee children resettled in high-income countries: Risk and protective factors. The Lancet, 379, 266–82. https://doi.org/10.1016/S0140-6736(11)60051-2
- *Fine, S., Malik, A., Guimond, M., Nemiro, A., Temu, G., Likindikoki, S., Annan, J., & Tol Wietse, A. (2021). Improving mental health in low-resource settings: A feasibility randomized controlled trial of a transdiagnostic psychological intervention among Burundian refugee adolescents and their caregivers. Behaviour Research and Therapy, 145, 103944. https://doi.org/10.1016/j.brat.2021.103944
- Frounfelker, R. L., Miconi, D., Farrar, J., Brooks Mohamad, A., Rousseau, C., & Betancourt Theresa, S. (2020). Mental health of refugee children and youth: Epidemiology, interventions, and future directions. Annual Review of Public Health, 41, 159–76. https://doi.org/10.1146/annurev-publhealth-040119-094230
- Fusar-Poli, P., Solmi, M., Brondino, N., Davies, C., Chae, C., Politi, P., Borgwardt, S., Lawrie Stephen, M., Parnas, J., & McGuire, P. (2019). Transdiagnostic psychiatry: A systematic review. World Psychiatry, 18, 192–207. https://doi.org/10.1002/wps.20631
- Galante, J., Friedrich, C., Dawson, A. F., Modrego-Alarcón, M., Gebbing, P., Delgado-Suárez, I., Gupta, R., Dean, L., Dalgleish, T., White, I. R., & Jones, P. B. (2021). Mindfulness-based programmes for mental health promotion in adults in nonclinical settings: A systematic review and meta-analysis of randomised controlled trials. PLOS Medicine, 18, e1003481. https://doi.org/10.1371/journal.pmed.1003481
- Gearing, R. E., Schwalbe, C. S., & Short, K. D. (2012). Adolescent adherence to psychosocial treatment: Mental health clinicians’ perspectives on barriers and promoters. Psychotherapy Research, 22, 317–26. https://doi.org/10.1080/10503307.2011.653996
- Glanville, J., Foxlee, R., Wisniewski, S., Noel-Storr, A., Edwards, M., & Dooley, G. (2019). Translating the cochrane EMBASE RCT filter from the ovid interface to embase.com: A case study. Health Information & Libraries Journal, 36, 264–77. https://doi.org/10.1111/hir.12269
- *Goodkind, J., Bybee, D., Hess, J., Amer, S., Ndayisenga, M., Greene, R. N., Choe, R., Isakson, B., Baca, B., & Pannah, M. (2020). Randomized controlled trial of a multilevel intervention to address social determinants of refugee mental health. American Journal of Community Psychology, 65, 272–289. https://doi.org/10.1002/ajcp.12418
- *Greene, M., Likindikoki, S., Rees, S., Bonz, A., Kaysen, D., Misinzo, L., Njau, T., Kiluwa, S., Turner, R., Ventevogel, P., Mbwambo Jessie, K. K., & Tol, W. A.. (2021). Evaluation of an integrated intervention to reduce psychological distress and intimate partner violence in refugees: Results from the nguvu cluster randomized feasibility trial. PloS one, 16, e0252982. https://doi.org/10.1371/journal.pone.0252982
- *Hamid, S., Dashash, M., & Latifeh, Y. (2021). A short-term approach for promoting oral health of internally displaced children with PTSD: The key is improving mental health—results from a quasi-randomized trial. BMC Oral Health, 21, 58. https://doi.org/10.1186/s12903-020-01385-z
- *Hasha, W., Igland, J., Fadnes, L. T., Kumar, B., Haj-Younes, J., Strømme Elisabeth, M., Norstein Eirin, Z., Vårdal, R., & Diaz, E. (2020). The effect of physiotherapy group intervention in reducing pain disorders and mental health symptoms among Syrian refugees: A randomized controlled trial. International Journal of Environmental Research and Public Health, 17, 9468–15. https://doi.org/10.3390/ijerph17249468
- Hazell, C. M., Hayward, M., Cavanagh, K., & Strauss, C. (2016). A systematic review and meta-analysis of low intensity CBT for psychosis. Clinical Psychology Review, 45, 183–92. https://doi.org/10.1016/j.cpr.2016.03.004
- Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. (2022). Cochrane Handbook for Systematic Reviews of Interventions version 6.3. 2022. www.training.cochrane.org/handbook.
- *Hilado, A., Leow, C., & Yinmei, Y. (2019). Understanding immigration trauma and the potential of home visiting among immigrant and refugee families. Zero to Three, 39, 44–53.
- Hinton, D. E., Rivera, E. I., Hofmann, S. G., Barlow David, H., & Otto Michael, W. (2012). Adapting CBT for traumatized refugees and ethnic minority patients: Examples from culturally adapted CBT (CA-CBT). Transcultural Psychiatry, 49, 340–65. https://doi.org/10.1177/1363461512441595
- Hodes, M., & Vostanis, P. (2019). Practitioner review: Mental health problems of refugee children and adolescents and their management. Journal of Child Psychology and Psychiatry, 60, 716–31. https://doi.org/10.1111/jcpp.13002
- Hsu, K. J., Beard, C., Rifkin, L., Dillon Daniel, G., Pizzagalli Diego, A., & Björgvinsson, T. (2015). Transdiagnostic mechanisms in depression and anxiety: The role of rumination and attentional control. Journal of Affective Disorders, 188, 22–7. https://doi.org/10.1016/j.jad.2015.08.008
- Im, H., Jettner, J. F., Warsame, A. H., Isse Maimuna, M., Khoury, D., & Ross Avina, I. (2018). Trauma-Informed psychoeducation for Somali refugee youth in urban Kenya: Effects on PTSD and psychosocial outcomes. Journal of Child & Adolescent Trauma, 11, 431–41. https://doi.org/10.1007/s40653-017-0200-x
- Infurna, F. J., & Luthar, S. S. (2018). Re-evaluating the notion that resilience is commonplace: A review and distillation of directions for future research, practice, and policy. Clinical Psychology Review, 65, 43–56. https://doi.org/10.1016/j.cpr.2018.07.003
- Kalisch, R., Köber, G., Binder, H., Ahrens Kira, F., Basten, U., Chmitorz, A., Choi Karmel, W., Fiebach, C. J., Goldbach, N., Neumann Rebecca, J., Kampa, M., Kollmann, B., Lieb, K., Plichta Michael, M., Reif, A., Schick, A., Sebastian, A., Walter, H., Wessa, M., Yuen Kenneth, S. L., Tüscher, O., & Engen, H. (2021). The frequent stressor and mental health monitoring-paradigm: A proposal for the operationalization and measurement of resilience and the identification of resilience processes in longitudinal observational studies. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.710493
- Kananian, S., Soltani, Y., Hinton, D., & Stangier, U. (2020). Culturally adapted cognitive behavioral therapy plus problem management (CA-CBT+) With Afghan refugees: A randomized controlled pilot study. Journal of Traumatic Stress, 33, 928–938. https://doi.org/10.1002/jts.22615
- Kanter, J. W., Manos, R. C., Bowe, W. M., Baruch David, E., Busch, A. M., & Rusch Laura, C. (2010). What is behavioral activation?A review of the empirical literature. Clinical Psychology Review, 30, 608–20. https://doi.org/10.1016/j.cpr.2010.04.001
- Knefel, M., Kantor, V., Weindl, D., Schiess-Jokanovic, J., Nicholson Andrew, A., Verginer, L., Schäfer, I., & Lueger-Schuster, B. (2022). Mental health professionals’ perspective on a brief transdiagnostic psychological intervention for Afghan asylum seekers and refugees. European Journal of Psychotraumatology, 13, 2068913. https://doi.org/10.1080/20008198.2022.2068913
- *Koch, T., Ehring, T., & Liedl, A. (2020). Effectiveness of a transdiagnostic group intervention to enhance emotion regulation in young Afghan refugees: A pilot randomized controlled study. Behaviour Research and Therapy, 103689. https://doi.org/10.1016/j.brat.2020.103689
- Kroenke, K., Spitzer, R. L., Williams, J. B. W., & Löwe, B. (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry, 32, 345–59. https://doi.org/10.1016/j.genhosppsych.2010.03.006
- Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 159–74. https://doi.org/10.2307/2529310
- *Lange-Nielsen, I. I., Kolltveit, S., Thabet, A. A. M., Dyregrov, A., Pallesen, S., Johnsen Tom, B., & Laberg Jon, C. (2012). Short-term effects of a writing intervention among adolescents in gaza. Journal of Loss and Trauma, 17, 403–22. https://doi.org/10.1080/15325024.2011.650128
- Leon, D. A., Jdanov, D., Gerry, C. J., Grigoriev, P., Jasilionis, D., McKee, M., Meslé, F., Penina, O., Twigg, J., Vallin, J., & Vågerö, D. (2022). The Russian invasion of Ukraine and its public health consequences. The Lancet Regional Health - Europe, 100358. https://doi.org/10.1016/j.lanepe.2022.100358
- Marchette, L. K., & Weisz, J. R. (2017). Practitioner review: Empirical evolution of youth psychotherapy toward transdiagnostic approaches. Journal of Child Psychology and Psychiatry, 58, 970–84. https://doi.org/10.1111/jcpp.12747
- Martin, P., Murray, L. K., Darnell, D., & Dorsey, S. (2018). Transdiagnostic treatment approaches for greater public health impact: Implementing principles of evidence-based mental health interventions. Clinical Psychology: Science and Practice, 25, e12270. https://doi.org/10.1111/cpsp.12270
- Martinez-Torteya, C., Miller-Graff, L. E., Howell, K. H., & Figge, C. (2017). Profiles of adaptation Among child victims of suspected maltreatment. Journal of Clinical Child & Adolescent Psychology, 46, 840–7. https://doi.org/10.1080/15374416.2015.1072822
- McCallie, M. S., Blum, C. M., & Hood, C. J. (2006). Progressive muscle relaxation. Journal of Human Behavior in the Social Environment, 13, 51–66. https://doi.org/10.1300/J137v13n03_04
- McMahon, F. J. (2014). Prediction of treatment outcomes in psychiatry—where do we stand? Dialogues in Clinical Neuroscience, 16, 455–64. https://doi.org/10.31887/DCNS.2014.16.4/fmcmahon
- Meichenbaum, D. (2017). Stress inoculation training: A preventative and treatment approach. In D. Meichenbaum (Ed.), The Evolution of Cognitive Behavior Therapy (pp. 101–24). Routledge.
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine, 46(1), 81–95. https://doi.org/10.1007/s12160-013-9486-6
- Miller, K. E., Koppenol-Gonzalez, G. V., Jawad, A., Steen, F., Sassine, M., & Jordans, M. J. D. (2020). A randomised controlled trial of the I-Deal life skills intervention with Syrian refugee adolescents in Northern Lebanon. Intervention, 18, 119–28. https://doi.org/10.4103/INTV.INTV_4_20
- *Miller, K. E., Koppenol-Gonzalez, G. V., Arnous, M., Tossyeh, F., Chen, A., Nahas N., & Jordans Mark, J.D. (2020b). Supporting Syrian families displaced by armed conflict: A pilot randomized controlled trial of the caregiver support intervention. Child Abuse & Neglect, 104512. https://doi.org/10.1016/j.chiabu.2020.104512
- Morina, N., Akhtar, A., Barth, J., & Schnyder, U. (2018). Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Frontiers in Psychiatry, 9. https://doi.org/10.3389/fpsyt.2018.00433
- Morina, N., & Sterr, T. N. (2019). Lack of evidence for the efficacy of psychotherapies for PTSD and depression in child and adolescent refugees. World Psychiatry, 18, 107. https://doi.org/10.1002/wps.20596
- Murray, L. K., Dorsey, S., Haroz, E., & Lee, C. (2014). A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cognitive and Behavioral Practice, 21, 111–23. https://doi.org/10.1016/j.cbpra.2013.06.005
- National Health and Medical Research Council (NHMRC). (2013). Clinical practice guideline for the management of borderline personality disorder. https://www.nhmrc.gov.au/file/18549/download?token = c1vvkxtR.
- *Neuner, F., Schauer, M., Klaschik, C., & Elbert, T. (2004). A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology, 72, 579–587. https://doi.org/10.1037/0022-006X.72.4.579
- Nocon, A., Eberle-Sejari, R., Unterhitzenberger, J., & Rosner, R. (2017). The effectiveness of psychosocial interventions in war-traumatized refugee and internally displaced minors: Systematic review and meta-analysis. European Journal of Psychotraumatology, 8, 1388709. https://doi.org/10.1080/20008198.2017.1388709
- Nosè, M., Ballette, F., Bighelli, I., Turrini, G., Purgato, M., Tol, W., Priebe, S., & Barbui, C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. PloS one, 12(2), e0171030. https://doi.org/10.1371/journal.pone.0171030
- O’Bryan, E. M., Kraemer, K. M., & McLeish, A. C. (2021). Using transdiagnostic mechanistic targets to advance prevention science. Clinical Psychology: Science and Practice, 28, 338–40. https://doi.org/10.1037/cps0000044
- *Ooi, C. S., Rooney, R. M., Roberts, C., & Chatzisarantis, N. (2016). The efficacy of a group cognitive behavioral therapy for war-affected young migrants living in Australia: A cluster randomized controlled trial. Frontiers in Psychology, 7. https://doi.org/10.3389/fpsyg.2016.01641
- *Orang, T. M., Missmahl, I., Thoele, A.-M., Alensise, L., Brenner, A., Gardisi, M., Peter, H., & Kluge, U. (2022). New directions in the mental health care of migrants, including refugees—A randomized controlled trial investigating the efficacy of value-based counselling. Clinical Psychology & Psychotherapy, https://doi.org/10.1002/cpp.2728
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—a web and mobile app for systematic reviews. Systematic Reviews, 5, 210. https://doi.org/10.1186/s13643-016-0384-4
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann Tammy, C., Mulrow Cynthia, D., Shamseer, L., Tetzlaff Jennifer, M., Akl Elie, A., Brennan Sue, E., Chou, R., Glanville, J., Grimshaw Jeremy, M., Hróbjartsson, A., Lalu Manoj, M., Li, T., Loder Elizabeth, W., Mayo-Wilson, E., McDonald, S … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
- Paulus, D. J., Vanwoerden, S., Norton, P. J., & Sharp, C. (2016). From neuroticism to anxiety: Examining unique contributions of three transdiagnostic vulnerability factors. Personality and Individual Differences, 94, 38–43. https://doi.org/10.1016/j.paid.2016.01.012
- Peters, J. L., Sutton, A. J., Jones, D. R., Abrams Keith, R., & Rushton, L. (2008). Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology, 61, 991–6. https://doi.org/10.1016/j.jclinepi.2007.11.010
- Purgato, M., Carswell, K., Tedeschi, F., Acarturk, C., Anttila, M., Au, T., Bajbouj, M., Baumgartner, J., Biondi, M., Churchill, R., Cuijpers, P., Koesters, M., Gastaldon, C., Ilkkursun, Z., Lantta, T., Nosè, M., Ostuzzi, G., Papola, D., Popa, M., Roselli, V., … Barbui, C. (2021). Effectiveness of Self-Help Plus in preventing mental disorders in refugees and asylum Seekers in Western Europe: A multinational randomized controlled trial. Psychotherapy and psychosomatics, 90(6), 403–414. https://doi.org/10.1159/000517504
- R Core Team. (2021). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. https://www.R-project.org/.
- Rawlinson, R., Aslam, R. W., Burnside, G., Chiumento, A., Eriksson-Lee, M., Humphreys, A., Khan, N., Lawrence, D., McCluskey, R., Mackinnon, A., Orton, L., Rahman, A., Roberts, E., Rosala-Hallas, A., Edwards, R. T., Uwamaliya, P., White, R. G., Winrow, E., & Dowrick, C. (2020). Lay-therapist-delivered, low-intensity, psychosocial intervention for refugees and asylum seekers (PROSPER): protocol for a pilot randomised controlled trial. Trials, 21. https://doi.org/10.1186/s13063-020-04310-5
- *Renner, W., Bänninger-Huber, E., & Peltzer, K. (2011). Culture-Sensitive and resource oriented peer (CROP)-groups as a community based intervention for trauma survivors: A randomized controlled pilot study with refugees and asylum seekers from Chechnya. Australas J Disaster Trauma Stud, 2011, 1–13.
- *Röhr, S., Jung, F., Pabst, A., Grochtdreis, T., Dams, J., Nagl, M., Renner, A., Hoffmann, R., König, H-H, Kersting, A., & Riedel-Heller, S G. (2021). A self-help App for Syrian refugees with posttraumatic stress (sanadak): randomized controlled trial. JMIR MHealth and UHealth, 9, e24807. https://doi.org/10.2196/24807
- Röhr, S., Jung, F. U., Renner, A., Plexnies, A., Hoffmann, R., Dams, J., Grochtdreis, T., König, H-H, Kersting, A., & Riedel-Heller, S. G. (2020). Recruitment and baseline characteristics of participants in the “sanadak” trial: A self-help app for Syrian refugees with post-traumatic stress. International Journal of Environmental Research and Public Health, 17, 7578–16. https://doi.org/10.3390/ijerph17207578
- Salanti, G. (2012). Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: Many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Synth Methods, 3, 80–97. https://doi.org/10.1002/jrsm.1037
- *Salihu, D., Wong, E., & Kwan, R. (2021). Effects of an African circle dance programme on internally displaced persons with depressive symptoms: A quasi-experimental study. International Journal of Environmental Research and Public Health, 843. https://doi.org/10.3390/ijerph18020843
- Satinsky, E., Fuhr, D. C., Woodward, A., Sondorp, E., & Roberts, B. (2019). Mental health care utilisation and access among refugees and asylum seekers in Europe: A systematic review. Health Policy, 123, 851–63. https://doi.org/10.1016/j.healthpol.2019.02.007
- Schäfer, S. K., Thomas, L. M., & Lieb, K. (2022). Problem Management Plus (PM+): Protocol of a systematic review. https://osf.io/y4 ( 8b.
- Scharpf, F., Kaltenbach, E., Nickerson, A., & Hecker, T. (2021). A systematic review of socio-ecological factors contributing to risk and protection of the mental health of refugee children and adolescents. Clinical Psychology Review, 83, 101930. https://doi.org/10.1016/j.cpr.2020.101930
- *Scheiber, B., Greinz, G., Hillebrand, J. B., Wilhelm, F. H., & Blechert, J. (2019). Resilienztraining für unbegleitete minderjährige flüchtlinge. Kindheit und Entwicklung, 28, 173–81. https://doi.org/10.1026/0942-5403/a000287
- Schünemann, H. J., Higgins, J. P. T., Vist, G. E., Glasziou, P., Akl, E. A., Skoetz, N., Guyatt, G. H. (2022). Chapter 14: Completing ‘summary of findings’ tables and grading the certainty of the evidence. In J. P. T. Higgins, J. Thomas, J. Chandler, M. Cumpston, T. Li, T. M. J. Page, & V.A. Welch (Eds.), Cochrane Handbook for Systematic Reviews of Interventions (pp. 375–402). www.training.cochrane.org/handbook
- Shafran, R., Myles-Hooton, P., Bennett, S., & Öst, L-M.. (2021). The concept and definition of low intensity cognitive behaviour therapy. Behaviour Research and Therapy, 138, 103803. https://doi.org/10.1016/j.brat.2021.103803
- Shapiro, E. (2012). EMDR and early psychological intervention following trauma. European Review of Applied Psychology, 62, 241–51. https://doi.org/10.1016/j.erap.2012.09.003
- *Shaw, S., Ward, K., Pillai, V., Ali, L. M., & Karim, H. (2021). A randomized clinical trial testing a parenting intervention among Afghan and rohingya refugees in Malaysia. Family Process, 60, 788–805. https://doi.org/10.1111/famp.12592
- Silove, D., Ventevogel, P., & Rees, S. (2017). The contemporary refugee crisis: An overview of mental health challenges. World Psychiatry, 16, 130–9. https://doi.org/10.1002/wps.20438
- Soltan, F., Cristofalo, D., Marshall, D., Purgato, M., Taddese, H., Vanderbloemen, L., Barbui, C., & Uphoff, E. (2022). Community-based interventions for improving mental health in refugee children and adolescents in high-income countries. Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.CD013657.pub2
- Soltan, F., Uphoff, E., Newson, R., Purgato, M., Taddese, H., Barbui, C., & Vanderbloemen, L. (2020). Community-based interventions for improving mental health in refugee children and adolescents in high-income countries. Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.CD013657
- *Spaaij, J., Kiselev, N., Berger, C., Bryant, R. A., Cuijpers, P., de Graaff, A. M., Fuhr, D. C., Hemmo, M., McDaid, D., Moergeli, H., Park, A. L., Pfaltz, M. C., Schick, M., Schnyder, U., Wenger, A., Sijbrandij, M., & Morina, N. (2022). Feasibility and acceptability of Problem Management Plus (PM+) among Syrian refugees and asylum seekers in Switzerland: a mixed-method pilot randomized controlled trial. European journal of psychotraumatology, 13(1), 2002027. https://doi.org/10.1080/20008198.2021.2002027
- *Spanhel, K., Hovestadt, E., Lehr, D., Spiegelhalder, K., Baumeister, H., Bengel, J., & Sander, L. B. (2022). Engaging refugees with a culturally adapted digital intervention to improve sleep: A randomized controlled pilot trial. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.832196
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Ommeren, M. (2009). Association of torture and other potentially traumatic events With mental health outcomes Among populations exposed to mass conflict and displacement. JAMA, 302, 537–49. https://doi.org/10.1001/jama.2009.1132
- Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, ., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., … Higgins, J. P. T. Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. https://doi.org/10.1136/bmj.l4898
- Thompson, C. T., Vidgen, A., & Roberts, N. P. (2018). Psychological interventions for post-traumatic stress disorder in refugees and asylum seekers: A systematic review and meta-analysis. Clinical Psychology Review, 63, 66–79. https://doi.org/10.1016/j.cpr.2018.06.006
- *Tol, W. A., Leku, M. R., Lakin, D. P., Carswell, K., Augustinavicius, J., Adaku, A., Au, T. M., Brown, F. L., Bryant, R. A., Garcia-Moreno, C., Musci, R. J., Ventevogel, P., White, R. G, & van Ommeren, M. (2020). Guided self-help to reduce psychological distress in south Sudanese female refugees in Uganda: A cluster randomised trial. The Lancet Global Health, 8, e254–63. https://doi.org/10.1016/S2214-109X(19)30504-2
- Tol, W. A. (2015). Stemming the tide: Promoting mental health and preventing mental disorders in low- and middle-income countries. Global Mental Health, 2, e11. https://doi.org/10.1017/gmh.2015.9
- Tribe, R., Weerasinghe, D., & Parameswaran, S. (2014). Increasing mental health capacity in a post-conflict country through effective professional volunteer partnerships: A series of case studies with government agencies, local NGOs and the diaspora community. International Review of Psychiatry, 26, 558–65. https://doi.org/10.3109/09540261.2014.918025
- Turrini, G., Purgato, M., Acarturk, C., Anttila, M., Au, T., Ballette, F., Bird, M., Carswell, K., Churchill, R., Cuijpers, P., Hall, J., Hansen, L. J., Kösters, M., Lantta, T., Nosè, M., Ostuzzi, G., Sijbrandij, M., Tedeschi, F., Valimaki, M., Wancata, J., White, R., van Ommeren, M., & Barbui C. (2019). Efficacy and acceptability of psychosocial interventions in asylum seekers and refugees: Systematic review and meta-analysis. Epidemiology and Psychiatric Sciences, 28, 376–88. https://doi.org/10.1017/S2045796019000027
- United Nations High Commissioner for Refugees. (2021). UNHCR’s Refugee Population Statistics Database. https://www.unhcr.org/refugee-statistics/.
- United Nations High Commissioner for Refugees. (2022a). Global Trends Report 2021. https://www.unhcr.org/62a9d1494/global-trends-report-2021.
- United Nations High Commissioner for Refugees. (2022b). Ukraine Refugee Situation - UNHCR data portal. https://data2.unhcr.org/.
- United Nations High Commissioner for Refugees. (2022c). Ukraine, other conflicts push forcibly displaced total over 100 million for first time. https://www.unhcr.org/ua/en/45221-ukraine-other-conflicts-push-forcibly-displaced-total-over-100-million-for-first-time.html.
- United Nations High Commissioner for Refugees. (2023). A Moment of Truth for Global Displacement. https://www.unhcr.org/spotlight/2023/01/2023-a-moment-of-truth-for-global-displacement/.
- United Nations High Commissioner for Refugees. (2016). ‘Refugees’ and ‘migrants’ frequently asked questions (FAQs). http://www.refworld.org/docid/56e81c0d4.html.
- Uphoff, E., Purgato, M., Churchill, R., & Barbui, C. (2019). An overview of systematic reviews on mental health promotion, prevention, and treatment of common mental disorders for refugees, asylum seekers, and internally displaced persons. Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.CD013458
- van Agteren, J., Iasiello, M., Ali, K., Fassnacht, D. B., Furber, G., Woodyatt, L., Howard, A., & Kyrios, M. (2021). Using the intervention mapping approach to develop a mental health intervention: A case study on improving the reporting standards for developing psychological interventions. Frontiers in psychology, 12, 648678. https://doi.org/10.3389/fpsyg.2021.648678
- Viechtbauer, W. (2010). Conducting meta-analyses inRwith themetaforPackage. Journal of Statistical Software, 36, 1–48. https://doi.org/10.18637/jss.v036.i03
- Wainberg, M. L., Scorza, P., Shultz, J. M., Helpman, L., Mootz, J. J., Johnson, K. A., Neria, Y., Bradford, J. E., Oquendo, M. A., & Arbuckle, M. R. (2017). Challenges and opportunities in global mental health: A research-to-practice perspective. Current Psychiatry Reports, 19, 28. https://doi.org/10.1007/s11920-017-0780-z
- *Walg, M., Angern, J. S., Michalak, J., & Hapfelmeier, G. (2020). Wirksamkeit des stabilisierungstrainings für jugendliche flüchtlinge mit traumafolgestörungen: Eine randomisierte kontrollgruppenstudie. Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie, 48, 369–79. https://doi.org/10.1024/1422-4917/a000749
- *Weinstein, N., Khabbaz, F., & Legate, N. (2016). Enhancing need satisfaction to reduce psychological distress in Syrian refugees. Journal of Consulting and Clinical Psychology, 84, 645–650. https://doi.org/10.1037/ccp0000095
- World Bank. (2022). World Bank Country and lending groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed 2 Jun 2022).
- World Health Organization. (2018). Health of refugee and migrant children: Technical guidance. https://apps.who.int/iris/handle/10665/342285.
- World Health Organization. 2019. Promoting the health of refugees and migrants. Draft global action plan 2019–2023. 72nd World health assembly 2019.
- World Health Organization. (2022a). Problem Management Plus (PM+): Individual psychological help for adults impaired by distress in communities exposed to adversity. https://www.who.int/publications/i/item/WHO-MSD-MER-16.2.
- World Health Organization. (2022b). Health promotion and disease prevention through population-based interventions, including action to address social determinants and health inequity. http://www.emro.who.int/about-who/public-health-functions/health-promotion-disease-prevention.html.
- Zorn, J. V., Schür, R. R., Boks, M. P., Boks, M. P., Kahn, R. S., Joëls, M., & Vinkers, C. H. (2017). Cortisol stress reactivity across psychiatric disorders: A systematic review and meta-analysis. Psychoneuroendocrinology, 77, 25–36. https://doi.org/10.1016/j.psyneuen.2016.11.036