ABSTRACT
Background: Posttraumatic stress disorder (PTSD) is prevalent in people with acquired brain injury (ABI). Despite the established efficacy of eye movement desensitization and reprocessing (EMDR) for PTSD in general, evaluation studies on EMDR in ABI patients with PTSD are limited.
Objective: The aim of this study is to explore clinical features, treatment characteristics, feasibility and first indications of efficacy of EMDR in adult ABI patients with PTSD.
Method: This retrospective consecutive case series included ABI patients, who received at least one session of EMDR for PTSD between January 2013 and September 2020. PTSD symptoms were measured using the Impact of Event Scale (IES) pre- and post-treatment. Affective distress was measured using the Subjective Units of Distress (SUD) pre- and post-treatment of the first target.
Results: Sixteen ABI patients (median age 46 years, 50% males), with predominantly moderate or severe TBI (50%) or stroke (25%) were included. Treatment duration was a median of seven sessions. Post-treatment IES scores were significantly lower than pre-treatment scores (p < .001). In 81% of the cases there was an individual statistically and clinically relevant change in IES score. Mean SUD scores of the first target were significantly lower at the end of treatment compared to scores at the start of treatment (p < .001). In 88% of the patients full desensitization to a SUD of 0–1 of the first target was accomplished. Only few adjustments to the standard EMDR protocol were necessary.
Conclusions: Findings suggest that EMDR is a feasible, well tolerated and potentially effective treatment for PTSD in ABI patients. For clinical practice in working with ABI patients, it is advised to consider EMDR as a treatment option.
HIGHLIGHTS
This retrospective consecutive case series (N = 16) explores clinical features, treatment characteristics, feasibility and first indications of efficacy of eye movement desensitization and reprocessing (EMDR) in adult patients with acquired brain injury (ABI) and Posttraumatic stress disorder (PTSD).
The results suggest that EMDR is a feasible and potentially efficacious treatment for PTSD in ABI patients, as patients demonstrated statistically and clinically significant large sized reductions in PTSD-symptoms after EMDR treatment.
For clinical practice in working with ABI patients, we advise to consider EMDR as a treatment option.
Antecedentes: El trastorno de estrés postraumático (TEPT) es prevalente en personas con lesión cerebral adquirida (ABI, por sus siglas en inglés). A pesar de la eficacia establecida de la desensibilización y reprocesamiento por movimientos oculares (EMDR) para el TEPT en general, los estudios de evaluación de EMDR en pacientes con ABI con TEPT son limitados.
Objetivo: El objetivo de este estudio es explorar las características clínicas, las características del tratamiento, la viabilidad y los primeros indicios de eficacia de la EMDR en pacientes adultos con ABI y TEPT.
Método: Esta serie retrospectiva de casos consecutivos incluyó pacientes con ABI, que recibieron al menos una sesión de EMDR para el TEPT entre enero de 2013 y septiembre de 2020. Los síntomas de TEPT se midieron utilizando la Escala de Impacto del Evento (IES) antes y después del tratamiento. La perturbación emocional se midió utilizando las Unidades Subjetivas del Malestar (SUD por sus siglas en inglés) pre y post-tratamiento del primer objetivo.
Resultados: Se incluyeron dieciséis pacientes con ABI (mediana de edad 46 años, 50% varones), con predominio de TBI moderado o grave (50%) o accidente cerebrovascular (25%). La duración media del tratamiento fue de siete sesiones. Las puntuaciones IES posteriores al tratamiento fueron significativamente inferiores a las anteriores (p < 0,001). En el 81% de los casos se produjo un cambio individual estadística y clínicamente relevante en la puntuación IES. Las puntuaciones IES medias del primer objetivo fueron significativamente inferiores al final del tratamiento en comparación con las puntuaciones al inicio del tratamiento (p < 0,001). En el 88% de los pacientes se logró la desensibilización completa a una SUD de 0–1 del primer objetivo. Sólo fueron necesarios unos pocos ajustes en el protocolo EMDR estándar.
Conclusiones: Los hallazgos sugieren que la EMDR es un tratamiento factible, bien tolerado y potencialmente eficaz para el TEPT en pacientes con ABI. Para la práctica clínica en el trabajo con pacientes ABI, se aconseja considerar EMDR como una opción de tratamiento.
背景:创伤后应激障碍 (PTSD) 在后天性脑损伤 (ABI) 患者中普遍存在。尽管眼动脱敏与再加工 (EMDR) 对 PTSD 的总体疗效已得到证实,但对患有 PTSD 的 ABI 患者进行 EMDR 的评估研究仍然有限。
目的:本研究旨在探讨 EMDR 对患有 PTSD 的ABI 成年患者的临床特征、治疗特点、可行性和疗效的首要适应症。
方法:本回顾性连续病例系列纳入了在 2013 年 1 月至 2020 年 9 月期间至少接受过一次针对 PTSD 的 EMD的RABI 患者。治疗前和治疗后使用事件影响量表 (IES) 测量 PTSD 症状。治疗前和治疗后使用主观痛苦单位(SUD)来测量第一个目标的情感痛苦。
结果:纳入了16 名 ABI 患者(中位年龄 46 岁,50% 男性),主要患有中度或重度 TBI (50%) 或中风 (25%)。 治疗持续时间的中位数为七疗程。治疗后 IES 评分显著低于治疗前评分 (p < .001)。 在 81% 的病例中,IES 评分出现了个体统计和临床相关的变化。与治疗开始时的分数相比,第一个目标的平均 SUD 分数在治疗结束时显著较低 (p < .001)。 88% 的患者对第一个目标的 SUD 0–1 完全脱敏。只需要对标准 EMDR 流程进行少量调整。
结论:研究结果表明,EMDR 是治疗 ABI 患者 PTSD 的一种可行、耐受性良好且可能有效的治疗方法。对于 ABI 患者的临床实践,建议考虑 EMDR 作为一种治疗选择。
1. Introduction
Acquired brain injury (ABI) refers to damage to the brain caused by events after birth. Most common causes of ABI are trauma, cerebrovascular incident and hypoxia. Consequences of ABI include long-lasting disorders/problems in cognition, behaviour and emotion (Consortium Cognitieve Revalidatie, Citation2007). There is increased risk of posttraumatic stress disorder (PTSD) in patients with ABI. Prevalence of PTSD is estimated at 16% after traumatic brain injury (TBI) (Van Praag et al., Citation2019) and 23% in the first year after stroke (Edmondson et al., Citation2013).
PTSD can develop after experiencing or witnessing a life-threatening or seriously injuring event and is classified as a trauma-stressor disorder (American Psychiatric Association, Citation2013). PTSD is characterized by four clusters of symptoms: (1) intrusions, (2) avoidance, (3) negative alterations in cognition and mood, and (4) alterations in arousal and reactivity that start after the traumatic event. Symptoms persist for at least one month and cause significant distress or impairment in social, occupational or other important areas of functioning (American Psychiatric Association, Citation2013).
PTSD has shown to be related to decreased health-related quality of life and decreased functional outcome in patients with ABI (Haagsma et al., Citation2015; Stein et al., Citation2018). In addition, the presence of PTSD in ABI patients is associated with lower return to work (Garrelfs et al., Citation2015; Glozier et al., Citation2008; Hedlund et al., Citation2011; Stein et al., Citation2018). As only a minority of people with PTSD spontaneously remits within months after onset (Kessler et al., Citation2017; Morina et al., Citation2014), awareness of the possible presence of PTSD in ABI patients is important, as well is treatment of PTSD.
There is robust support for the efficacy of Eye Movement Desensitization and Reprocessing (EMDR) in treatment of PTSD in adults (Cusack et al., Citation2016; Mavranezouli et al., Citation2020; Wilson et al., Citation2018). EMDR is recommended by several guidelines for treatment of PTSD (Department Of Veterans Affairs, D.o.D., Citation2017; Phelps et al., Citation2022; World Health Organization, Citation2013). EMDR is a standardized, protocolled treatment based on the assumption that distress associated with traumatic events is caused by unprocessed information (Shapiro, Citation2001). During the treatment, the client attends to disturbing material while simultaneously focusing on an external stimulus, i.e. most commonly therapist-directed eye movements, or auditory or tactile stimuli. The distress is reduced during this desensitization process and changes in dysfunctional or negative beliefs occur (de Jongh & ten Broeke, Citation2011a). Currently, most evidence for the explanation of how EMDR works, supports the ‘working memory hypothesis’. This entails that as a consequence of tasks competing for limited working memory capacity when done simultaneously, negative memories become less vivid and less emotional and are stored in this new way (van den Hout & Engelhard, Citation2011). There is also evidence supporting other models to explain the mechanisms of EMDR, such as the orienting response, see Landin-Romero, Moreno-Alcazar (Landin-Romero et al., Citation2018) for a review.
Given the substantial support for the efficacy of EMDR in adults with PTSD, this treatment may also be a suitable treatment for PTSD in ABI, especially since EMDR does not rely heavily on cognitive functions (de Jongh & ten Broeke, Citation2011a), which are often impaired in patients with ABI. There are some encouraging case reports that suggest EMDR is feasible and efficacious in ABI patients with PTSD (de Roos et al., Citation2011; Pagani et al., Citation2018; van Oort & van Zandvoort, Citation2016; Vink et al., Citation2016). However, there are, to the best of our knowledge, no controlled studies on the efficacy and feasibility of EMDR in adult patients with ABI and PTSD.
Given the lack of research into the applicability and efficacy of EMDR as a treatment for PTSD in patients with ABI, we performed an explorative study as an initial evaluation. We retrospectively evaluated clinical features, treatment characteristics, feasibility and first indications of efficacy of EMDR in adult patients with ABI and PTSD in a retrospective case series.
2. Method
2.1. Design and participants
The current study was set up as a retrospective case series. We included patients who were treated at the Multidisciplinary Specialist Center for Brain Injury and Neuropsychiatry of GGZ Oost Brabant, the Netherlands, between January 2013 and September 2020. This centre offers multidisciplinary treatment to patients with psychiatric problems and ABI, combining rehabilitation treatment and mental health care.
Patients were included in the current study if they (1) were diagnosed with PTSD according to the criteria of DSM-IV or DSM-5 by clinical evaluation of a psychiatrist or psychologist; (2) were treated with at least one session of EMDR for PTSD; (3) filled out the Impact of Event Scale (Horowitz et al., Citation1979) prior to and post-EMDR; (4) were > 18 years old. Patients participating in an experimental study on this subject were not included.
All patients provided informed consent. The study was approved by the scientific review board of GGZ Oost Brabant and conducted in accordance with the 1964 Declaration of Helsinki and its later amendments.
2.2. Measurements and procedures
2.2.1. Sociodemographic and clinical information
The following sociodemographic and clinical information was collected from the electronic patient record (EPR): sex, age, in- or outpatient, the ABI (type of and time since ABI), other DSM classifications, PTSD (i.e. the index trauma and time point of traumatic event), EMDR treatment (i.e. therapist, number and frequency of sessions, stimuli used in desensitization, adjustments to standard protocol). Further, total pre-treatment scores on the Outcome Questionnaire-45 (de Jong et al., Citation2007; Lambert et al., Citation2004) were collected from the EPR as a descriptive baseline measure of subjective general mental health. The cut-off for clinical significance (i.e. a score below which is considered normal functioning) was set at 56 (Timman et al., Citation2017). EPRs were checked for adverse advents (e.g. self-harm, suicidal behaviour, necessity for crisis intervention) during the period of treatment with EMDR.
2.2.2. Outcome measures
2.2.2.1. PTSD symptoms
Self-reported symptoms of PTSD were assessed using the Dutch version of the Impact of Event Scale (IES) (Brom & Kleber, Citation1985; Horowitz et al., Citation1979). Patients filled out the IES before starting (T0) and after ending the treatment with EMDR (T1) in the context of evaluation of clinical care: the period between filling out the IES (T0) and start of treatment varied as the IES was used either as a screener for PTSD symptoms (after which EMDR treatment was indicated) or as starting point of already planned EMDR treatment. The IES consists of 15 items on a 4-point scale, total score 0–75 (with higher scores representing more symptoms), regarding the amount of distress that one associates with a specific event (i.e. PTSD symptoms of the two factors intrusion and avoidance) in the past week. The IES has been used to screen for PTSD symptoms in ABI patients (Bruggimann et al., Citation2006; Huenges Wajer et al., Citation2018; Utz et al., Citation2019) and demonstrated adequate psychometric properties (van der Ploeg et al., Citation2004). The cut-off for clinical significance was set at 26 (Rodenburg et al., Citation2009).
2.2.2.2. Affective distress
In every EMDR session Subjective Units of Distress (SUD’s) were recorded as part of the treatment protocol to assess the level of affective distress in relation to an image of the traumatic event. The SUD is rated on a scale ranging from 0 (absence of distress) to 10 (maximum of distress) (Wolpe, Citation1969) and is an ongoing measure throughout the delivery of EMDR. For the purpose of this study, the SUD before starting and after ending treatment of the first trauma target (‘Target 1’, i.e. the most distressing image, see Treatment), was used as a measure of effect of EMDR treatment. Adequate psychometric properties have been reported of SUD scores obtained in the context of EMDR treatment (Kim et al., Citation2008). Full desensitization of a target is operationalized as decline of the SUD to a score of 0–1 (Shapiro, Citation2001).
2.2.3. Treatment
EMDR treatment was delivered by four clinical neuropsychologists, who all completed an EMDR Europe-approved Basic Training program and were experienced in diagnosing and treating patients with ABI. The number of sessions was based on the patient’s individual needs and judgement of the therapist considering the PTSD. EMDR therapy was delivered using the manualized standard EMDR 8-phased protocol, in Dutch (de Jongh & ten Broeke, Citation2011a; Shapiro, Citation2001). Treatment included all eight phases of the EMDR standard protocol, with the only exception being the installation of the safe place or any other form of stabilization. Slight changes in treatment protocol were made by the Dutch EMDR Association during the time frame of the study. See Box 1, Appendix A, for a detailed description of the procedure. Eye movements are the preferred and first stimulus to use, but in case of epilepsy, eye movements are refrained from and other (combinations of) stimuli are used (de Jongh & ten Broeke, Citation2011b). In case horizontal eye movements are complicated (for instance, due to hemianopia or ocular motoric problems), other stimuli are chosen. The ‘index trauma’ is the traumatic event that is currently most distressing and the subject of intrusion symptoms. One or more targets of this event are treated (first) in EMDR.
2.3. Statistical analyses
2.3.1. Sociodemographic, clinical and treatment characteristics
Descriptive analyses (count, percentage, median and range) were performed to describe sociodemographic (i.e. age, sex), clinical (i.e. type of ABI, months since ABI, type of index trauma, timing of index trauma, in- or outpatient, DSM disorders, OQ45 score, adverse events) and treatment characteristics (i.e. therapist, adjustments to standard treatment protocol, total number of sessions, number of sessions to desensitize the first target, stimuli used in desensitization, drop out).
2.3.2. PTSD symptoms
Descriptive analyses were performed on time span between T0-start of treatment and end of treatment-T1, follow-up time (T0-T1 span in weeks; median, range, IQR) and IES group scores at T0 and T1 (median, range and IQR). Comparative analyses for IES group scores at T0 and T1 were performed with Wilcoxon signed-rank test (because the assumptions of normality were not met upon exploration of the data), and effect size r (r = z/√N) (Rosenthal, Citation1991). We respectively considered r = .10 as a small, r = .30 a medium and r = .50 as a large sized effect. We counted the number and percentages of patients scoring impaired (i.e. defined as IES score ≥26) at T0 and T1 to assess the clinical significance of individual PTSD symptoms over time. Individual statistically significant change from T0 to T1 in IES scores was determined by computation of the reliable change index (RCI) for the IES (see Appendix B, Box 2). This RCI value reflects the absolute difference required for an individual change score to be regarded as reliable (i.e. unlikely due to measurement error alone). Change was defined as a RCI value exceeding +/−11.31, representing worsened and improved PTSD symptoms, respectively. The number and percentage of patients reporting improved, stable or worsened symptoms were counted. To examine the relationship between follow-up time (T0-T1 span in weeks) and IES change scores (i.e. T0-T1 difference scores), Spearman’s correlation coefficient was used.
2.3.3. Affective distress
Descriptive (median, range and IQR) and comparative analyses (i.e. using Wilcoxon signed-rank test and r for effect size) were performed for SUD group scores of the start and end of treatment of Target 1. We counted the number and percentage of patients reaching full desensitization to a SUD of 0–1 for Target 1 and described the pattern of change in SUD scores for the individuals not reaching full desensitization. Statistical analyses were performed using the IBM Statistical Package for the Social Sciences (SPSS) version 26.0. Alpha was set at .05.
3. Results
3.1. Participant characteristics
Thirty-four patients with PTSD and ABI were treated with EMDR between January 2013 and September 2020. Eleven patients did not fill out an IES pre- and post-EMDR, four patients participated in an experimental study and were therefore excluded from the current study, three patients did not provide consent for study participation. In total, 16 patients were included in the current study.
presents characteristics of the ABI patients treated with EMDR who completed the IES at T0 and T1. For more than half (n = 5 TBI, n = 2 stroke, n = 2 other ABI) of the patients, the (circumstance surrounding the) ABI was the index trauma, for example the accident or violent assault causing TBI, the experience of having a stroke, or delusions in a confusional state. In three patients, the A criterion for PTSD according to the DSM-5 was, in contrast to criteria B-H, actually not fulfilled, due to the nature of the traumatic events (classified as ‘other’ in ).
Table 1. Sociodemographic and clinical characteristics of ABI patients with PTSD treated with EMDR who completed the IES.
Thirteen percent of the cases (n = 2) experienced the index trauma in their childhood (i.e. prior to sustaining the ABI): both index traumas were single events (sexual abuse and sudden death of a parent).
3.2. Treatment characteristics
All patients were treated by the first author. In most cases, treatment was provided in weekly sessions of a maximum duration of 90 min. Sessions were shortened (with a minimum of 45 min) if, for instance, cognitive dysfunction complicated longer session duration. In one patient therapy during clinical admittance was more frequent and consisted of four sessions a week (on separate days) with therapist rotation of four different psychologists. There were no drop outs of treatment before completion. lists treatment characteristics of the included patients.
Table 2. Treatment characteristics of ABI patients with PTSD treated with EMDR who completed the IES.
The instructions of the standard protocol were comprehensible for the majority of patients. In one patient adjusted instructions, namely simplification of language and presenting instructions in a visual manner, were needed due to aphasia. The Dutch children’s and adolescent’s protocol for EMDR (de Roos et al., Citation2018) was used as a guideline for these adjustments, and instructions were shortened and simplified to the core of the standard protocol. Adjustments were made in the presentation and rating of the SUD and VOC (which are verbal in the standard protocol), because giving marks or understanding the scale proved difficult. The scale was drawn as a continuum with marks and the SUD/VOC was rated by pointing the scale.
In the majority of patients eye movements were used to tax working memory, although in some cases a switch was made to other stimuli because eye movements proved difficult to perform or seemed to elicit somatic complaints like dizziness. In almost half of the patients multiple stimuli at once were used in desensitization to tax working memory load. No adverse events were reported.
3.3. PTSD symptoms
The IES was filled out within a day prior to start of EMDR in nine patients, within two weeks pre-treatment in three patients and respectively in one, two, three and five months pre-treatment in four patients. The IES post-treatment was filled out within two weeks after finishing EMDR in ten patients, within three to four weeks in four patients and within six to seven weeks in two patients. Median follow-up time (span between T0 and T1) was 16 weeks (range 3–54, IQR = 20.75). No other PTSD treatment was administered between respectively T0 and EMDR, and EMDR and T1.
Median IES score at T0 was 42 (range 33–64, IQR = 16.5). Median IES score at T1 was 6 (range 0–47, IQR = 18.75). IES score was significantly lower at T1 versus T0, z = −3.52, p < .001, ES was large with r = .62. There was no significant relationship between follow-up time and IES change score from pre- to post-treatment, rS = .15, p = .57.
At T0, all patients had clinically significant scores on the IES (n = 16). At T1, 81% of the patients (n = 13) scored below the cut-off for clinical significance. displays individual scores set against the IES cut-off for clinical significance.
Figure 1. Individual IES scores of ABI patients with PTSD pre- and post-treatment with EMDR (n = 16).
Note: Plot showing the pre-treatment (X-axis) and post-treatment (Y-axis) individual patient’s Impact of Event Scale (IES) scores. The dashed lines mark the boundaries of reliable change (i.e. +/−11.31). The circle marks the mean group score pre- and post-treatment. Points above the upper boundary of reliable change represent statistically significant deterioration (i.e. reporting more symptoms after treatment as compared to before treatment), triangles within the dashed lines represent no statistically significant improvement over time and squares below the lower boundary of reliable change represent statistically significant improvement (i.e. reporting less symptoms after treatment as compared to before treatment). The dotted lines mark the IES clinical cut-off score of 26, IES scores right of and above these lines are considered clinically significant. Based on Morley and Dowzer (Citation2014).
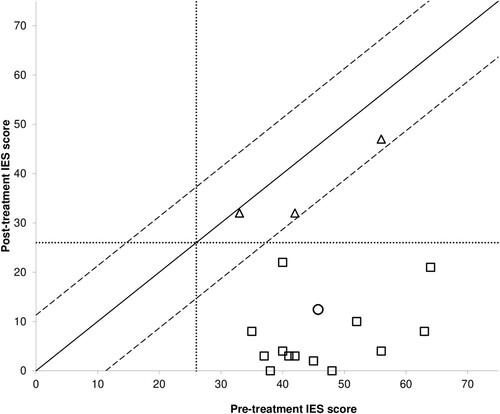
In 81% (n = 13) of the patients there was a statistically significant improvement over time, represented by the IES change score exceeding the RCI value of −11.31 at T1 compared to T0. There were no patients with positive IES change scores, indicating that no individual showed absolute deterioration from pre- to post-treatment. For all individuals who showed a statistically significant improvement in IES score over time, post-treatment IES scores were no longer clinically significant. displays individual change set against the boundaries of reliable change on the IES.
3.4. Affective distress
Median SUD of Target 1 at the start of treatment was 9 (range 7–10, IQR = 2, N = 16). Median SUD of Target 1 at the end of treatment of Target 1 was 0 (range 0–8, IQR = .88, N = 16). SUD scores were significantly lower at the end of treatment of Target 1 versus the start, z = −3.44, p < .001, ES was large with r = .61. In 14 patients (88%), full desensitization to a SUD of 0–1 of Target 1 was accomplished. In the remaining two patients (12%) no full desensitization was accomplished with SUD scores of respectively 2 (starting at 9) and 8 (starting at 8).
4. Discussion
This retrospective case series explored clinical features, treatment characteristics, feasibility and first indications of efficacy of EMDR as a treatment for PTSD in adult ABI patients. All patients included in the current study were, in addition to the diagnosis PTSD, diagnosed with a neurocognitive disorder according to the DSM-classification. Only in one of the patients adjustments of instructions in the standard protocol for EMDR were made. These adjustments were in line with the Dutch children’s protocol for EMDR in which instructions are simplified and presented in a visual manner. No adverse events were reported. There was no exacerbation of PTSD-symptoms measured by the IES. There were significant and large reductions in PTSD-symptoms on a group level, as well as individual statistically and clinically significant reductions in PTSD-symptoms in the majority of patients. This was corroborated by significant reductions in affective distress (SUD) reported by ABI patients in relation to the most disturbing traumatic image during the course of EMDR treatment. Overall, results suggest that EMDR treatment is feasible and seems to be efficacious in reducing PTSD-symptoms in ABI patients.
It has been suggested that symptoms of ABI (e.g. cognitive impairments, problems with emotion regulation, impulse control) and physical problems (e.g. headache or problems with vision or other senses) may limit patients’ ability to engage in or benefit from psychological PTSD treatments (Kennedy et al., Citation2007; Tanev et al., Citation2014). On the other hand, it can be stated that EMDR is a straightforward, relatively short psychotherapy, which does not rely heavily on cognitive functions, and painful memories do not have to be extensively discussed (de Jongh & ten Broeke, Citation2011a). This is one of the first studies demonstrating that EMDR treatment indeed is feasible as well as promising with regard to its efficacy in patients with ABI, cognitive disorder and PTSD. Although no controlled studies are available on the efficacy and feasibility of EMDR in patients with ABI and PTSD, controlled studies are available of EMDR on PTSD symptoms in other patient groups with comorbid disorders, like severe psychotic disorder (van den Berg et al., Citation2015), autism (Lobregt-van Buuren et al., Citation2019) and intellectual disability (Karatzias et al., Citation2019; Mevissen et al., Citation2017). In those studies, EMDR was also shown to be feasible, acceptable, and effective (van den Berg et al., Citation2015) or potentially effective (Karatzias et al., Citation2019; Lobregt-van Buuren et al., Citation2019; Mevissen et al., Citation2017).
This study has some limitations that need to be noted. The most important limitation is the lack of an experimental design which facilitates the exclusion of threats to the validity of our findings (e.g. regression to mean, lack of control group, selection bias etc.). For instance, the time point at which the IES was administered varied significantly. Although we found no relationship between the change in IES-scores and the time span between pre- and post-EMDR IES, and no other PTSD-treatment was offered between pre- and post-IES, we cannot rule out any effects from non-PTSD-specific treatments (e.g. cognitive rehabilitation). However, the significant reduction in affective distress, measured during the EMDR sessions, suggests that EMDR is producing a treatment effect.
Secondly, we established PTSD classification by clinical diagnosis and solely used self-report instruments to establish PTSD symptoms post-treatment, whilst taking a structured clinical diagnostic interview is considered the gold standard in diagnosing PTSD in general. In addition, the diagnostic interview appears to distinguish symptoms of psychopathology better from symptoms of ABI than self-report questionnaires, and is less affected by ABI-related problems such as memory deficits (Cnossen et al., Citation2017). Future research should therefore incorporate structured clinical diagnostic interviews, such as the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) (Weathers et al., Citation2018), to diagnose PTSD and to serve as a primary outcome measure.
Third, as the study is an initial, clinically based evaluation, we included patients with various kinds of index traumas, for instance the ABI itself, childhood trauma and sexual assault and with various kinds of ABI. We did not assess whether any of our patients met the criteria of the International Statistical Classification of Diseases and Related Health Problems, 11th revision (ICD-11), diagnosis of complex PTSD (Maercker et al., Citation2022), which was being proposed at the time of the study. It is still unclear whether complex PTSD requires a different treatment approach than described in the existing international treatment guidelines for PTSD, namely with extra preparatory, stabilizing interventions (Cloitre et al., Citation2010; Maercker et al., Citation2022). We could not examine this in our study. However, results of recent randomized controlled trials suggest a different treatment approach may not be required (Oprel et al., Citation2021; van Vliet et al., Citation2021).
Further, we did not include performance-based measures of cognition, i.e. from neuropsychological tests. Studies of psychotherapy of PTSD showed that more proficient pre-treatment performance on standardized neuropsychological measures of memory was associated with better treatment response (Haaland et al., Citation2016; Nijdam et al., Citation2015; Scott et al., Citation2017). Research is needed to examine to what extent pre-treatment cognitive performance moderates treatment effect in patients with ABI and what the minimum level of cognitive function is to engage in EMDR. Also, psychological treatments for PTSD have been shown to improve memory functioning (Susanty et al., Citation2022). It would be interesting to include pre- and post-treatment measures of cognitive performance in studies on psychotherapy for PTSD in patients with ABI, to learn more on the relative contribution of PTSD to cognitive disorders in this group.
A final limitation is that the participants included in our study may not be fully representative of ABI patients in general, as our population had more comorbid psychiatric disorders than the ABI-population in general (Mitchell et al., Citation2017; Whelan-Goodinson et al., Citation2009). However, although the patients in our study had comorbid psychiatric and/or cognitive disorders, results nevertheless suggest EMDR treatment is feasible and potentially effective. Therefore, we presume that EMDR treatment is feasible and potentially effective in ABI patients with PTSD and less psychiatric comorbidity. Future randomized controlled research should now address the subject.
In conclusion, the results of this evaluative retrospective case series suggest that EMDR is a feasible and potentially efficacious treatment for PTSD in ABI patients. The study included a diversity of ABI patients, mostly with moderate or severe TBI or stroke, with comorbid psychiatric and/or cognitive disorders. Treatment was well tolerated, relatively short and few adjustments to the standard protocol for EMDR were required. For clinical practice in working with ABI patients, we advise to consider EMDR as a treatment option. In case adjustments to the standard EMDR protocol are necessary because of cognitive disorder or aphasia, the children’s EMDR protocol and presenting instructions in a visual way may be helpful.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research supporting data is not available.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed). American Psychiatric Publishing.
- Brom, D., & Kleber, R. J. (1985). De schok verwerkings lijst. Nederlands Tijdschrift Voor de Psychologie, 40, 164–168.
- Bruggimann, L., Annoni, J. M., Staub, F., von Steinbuchel, N., Van der Linden, M., & Bogousslavsky, J. (2006). Chronic posttraumatic stress symptoms after nonsevere stroke. Neurology, 66(4), 513–516. https://doi.org/10.1212/01.wnl.0000194210.98757.49
- Cloitre, M., Stovall-McClough, K. C., Nooner, K., Zorbas, P., Cherry, S., Jackson, C. L., Gan, W., & Petkova, E. (2010). Treatment for PTSD related to childhood abuse: A randomized controlled trial. American Journal of Psychiatry, 167(8), 915–924. https://doi.org/10.1176/appi.ajp.2010.09081247
- Cnossen, M. C., Scholten, A. C., Lingsma, H. F., Synnot, A., Haagsma, J., Steyerberg, P. E., & Polinder, S. (2017). Predictors of major depression and posttraumatic stress disorder following traumatic brain injury: A systematic review and meta-analysis. Journal of Neuropsychiatry Clinical Neuroscience, 29(3), 206–224. https://doi.org/10.1176/appi.neuropsych.16090165
- Consortium Cognitieve Revalidatie. (2007). Richtlijn cognitieve revalidatie niet-aangeboren hersenletsel. https://www.kennispleingehandicaptensector.nl/tips-tools/tools/richtlijn-cognitieve-revalidatie-nah
- Cusack, K., Jonas, D. E., Forneris, C. A., Wines, C., Sonis, J., Middleton, J. C., Feltner, C., Brownley, K. A., Olmsted, K. R., Greenblatt, A., Weil, A., & Gaynes, B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. https://doi.org/10.1016/j.cpr.2015.10.003
- de Jong, K., Nugter, M. A., Polak, M. G., Wagenborg, J. E. A., Spinhoven, P., & Heiser, W. J. (2007). The outcome questionnaire (OQ-45) in a Dutch population: A cross-cultural validation. Clinical Psychology & Psychotherapy, 14(4), 288–301. https://doi.org/10.1002/cpp.529
- de Jongh, A., & ten Broeke, E. (2011a). Handboek EMDR. Een geprotocolleerde behandelmethode voor de gevolgen van psychotrauma. Pearson.
- de Jongh, A., & ten Broeke, E. (2011b). Vraagbaak EMDR: Oplossingen en tips voor EMDR-behandelingen. Pearson.
- de Roos, C., Beer, R., de Jongh, A., & ten Broeke, E. (2018). EMDR protocol voor kinderen en jongeren tot 18 jaar. Vereniging EMDR Nederland.
- de Roos, C., Las, S., & Veenstra, S. (2011). Toepassingen van EMDR bij revalidatie. Nieuwsbrief Sectie Revalidatie NIP. 61(Thema Behandelingen), 7–9.
- Department Of Veterans Affairs, D.o.D. (2017). Clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Department of Veterans Affairs, Department of Defense.
- Edmondson, D., Richardson, S., Fausett, J. K., Falzon, L., Howard, V. J., & Kronish, I. M. (2013). Prevalence of PTSD in survivors of stroke and transient ischemic attack: A meta-analytic review. PLoS One, 8(6), e66435. https://doi.org/10.1371/journal.pone.0066435
- Garrelfs, S. F., Donker-Cools, B. H. P. M., Wind, H., & Frings-Dresen, M. H. W. (2015). Return-to-work in patients with acquired brain injury and psychiatric disorders as a comorbidity: A systematic review. Brain Injury, 29(5), 550–557. https://doi.org/10.3109/02699052.2014.995227
- Glozier, N., Hackett, M. L., Parag, V., & Anderson, C. S. (2008). The influence of psychiatric morbidity on return to paid work after stroke in younger adults. Stroke, 39(5), 1526–1532. https://doi.org/10.1161/STROKEAHA.107.503219
- Haagsma, J. A., Scholten, A. C., Andriessen, T. M. J. C., Vos, P. E., Van Beeck, E. F., & Polinder, S. (2015). Impact of depression and post-traumatic stress disorder on functional outcome and health-related quality of life of patients with mild traumatic brain injury. Journal of Neurotrauma, 32(11), 853–862. https://doi.org/10.1089/neu.2013.3283
- Haaland, K. Y., Sadek, J. R., Keller, J. E., & Castillo, D. T. (2016). Neurocognitive correlates of successful treatment of PTSD in female veterans. Journal of the International Neuropsychological Society, 22(6), 643–651. https://doi.org/10.1017/S1355617716000424
- Hedlund, M., Zetterling, M., Ronne-Engström, E., Carlsson, M., & Ekselius, L. (2011). Depression and post-traumatic stress disorder after aneurysmal subarachnoid haemorrhage in relation to lifetime psychiatric morbidity. British Journal of Neurosurgery, 25(6), 693–700. https://doi.org/10.3109/02688697.2011.578769
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218. https://doi.org/10.1097/00006842-197905000-00004
- Huenges Wajer, I. M. C., Smits, A. R., Rinkel, G. J. E., van Zandvoort, M. J. E., Wijngaards-de Meij, L., & Visser-Meily, J. M. A. (2018). Exploratory study of the course of posttraumatic stress disorder after aneurysmal subarachnoid hemorrhage. General Hospital Psychiatry, 53, 114–118. https://doi.org/10.1016/j.genhosppsych.2018.03.004
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037/0022-006X.59.1.12
- Karatzias, T., Brown, M., Taggart, L., Truesdale, M., Sirisena, C., Walley, R., Mason-Roberts, S., Bradley, A., & Paterson, D. (2019). A mixed-methods, randomized controlled feasibility trial of Eye Movement Desensitization and Reprocessing (EMDR) plus Standard Care (SC) versus SC alone for DSM-5 Posttraumatic Stress Disorder (PTSD) in adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 32(4), 806–818. https://doi.org/10.1111/jar.12570
- Kennedy, J. E., Jaffee, M. S., Leskin, G. A., Stokes, J. W., Leal, F. O., & Fitzpatrick, P. J. (2007). Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. The Journal of Rehabilitation Research and Development, 44(7), 895–920. https://doi.org/10.1682/JRRD.2006.12.0166
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., Degenhardt, L., de Girolamo, G., Dinolova, R. V., Ferry, F., Florescu, S., Gureje, O., Haro, J. M., Huang, Y., Karam, E. G., Kawakami, N., Lee, S., Lepine, J.-P., Levinson, D., … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. https://doi.org/10.1080/20008198.2017.1353383
- Kim, D., Bae, H., & Chon Park, Y. (2008). Validity of the subjective units of disturbance scale in EMDR. Journal of EMDR Practical Research, 1, 57–62. https://doi.org/10.1891/1933-3196.2.1.57
- Lambert, M. J., Morton, J. J., Hatfield, D. R., Harmon, C., Hamilton, S., Shimokawa, K., & Burlingame, G. M. (2004). Administration and scoring manual for the OQ-45.2 (outcome questionnaire) (3rd ed.). American Professional Credentialling Services LLC.
- Landin-Romero, R., Moreno-Alcazar, A., Pagani, M., & Amann, B. L. (2018). How does eye movement desensitization and reprocessing therapy work? A systematic review on suggested mechanisms of action. Frontiers in Psychology, 9, 1395. https://doi.org/10.3389/fpsyg.2018.01395
- Lobregt-van Buuren, E., Sizoo, B., Mevissen, L., & de Jongh, A. (2019). Eye movement desensitization and reprocessing (EMDR) therapy as a feasible and potential effective treatment for adults with autism spectrum disorder (ASD) and a history of adverse events. Journal of Autism and Developmental Disorders, 49(1), 151–164. https://doi.org/10.1007/s10803-018-3687-6
- Logie, R. D. J., & de Jongh, A. (2014). The “Flashforward Procedure”: Confronting the catastrophe. Journal of EMDR Practice and Research, 8(1), 25–32. https://doi.org/10.1891/1933-3196.8.1.25
- Maercker, A., Cloitre, M., Bachem, R., Schlumpf, Y. R., Khoury, B., Hitchcock, C., & Bohus, M. (2022). Complex post-traumatic stress disorder. The Lancet, 400(10345), 60–72. https://doi.org/10.1016/S0140-6736(22)00821-2
- Mavranezouli, I., Megnin-Viggars, O., Daly, C., Dias, S., Welton, N. J., Stockton, S., Bhutani, G., Grey, N., Leach, J., Greenberg, N., Katona, C., El-Leithy, S., & Pilling, S. (2020). Psychological treatments for post-traumatic stress disorder in adults: A network meta-analysis. Psychological Medicine, 50(4), 542–555. https://doi.org/10.1017/S0033291720000070
- Mevissen, L., Didden, R., Korzilius, H., & de Jongh, A. (2017). Eye movement desensitisation and reprocessing therapy for posttraumatic stress disorder in a child and an adolescent with mild to borderline intellectual disability: A multiple baseline across subjects study. Journal of Applied Research Intellectual Disabilities, 34–41. https://doi.org/10.1111/jar.12335
- Mitchell, A. J., Sheth, B., Gill, J., Yadegarfar, M., Stubbs, B., Yadegarfar, M., & Meader, N. (2017). Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. General Hospital Psychiatry, 47, 48–60. https://doi.org/10.1016/j.genhosppsych.2017.04.001
- Morina, N., Wicherts, J. M., Lobbrecht, J., & Priebe, S. (2014). Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clinical Psychology Review, 34(3), 249–255. https://doi.org/10.1016/j.cpr.2014.03.002
- Morley, S., & Dowzer, C. N. (2014). Manual for the Leeds Reliable Change Indicator: Simple Excel(tm) applications for the analysis of individual patient and group data, U.o: Leeds, UK.
- Nijdam, M. J., de Vries, G.-J., Gersons, B. P. R., & Olff, M. (2015). Response to psychotherapy for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 76(08), e1023–e1028. https://doi.org/10.4088/JCP.14m09438
- Oprel, D. A. C., Hoeboer, C. M., Schoorl, M., Kleine, R. A. d., Cloitre, M., Wigard, I. G., van Minnen, A., & van der Does, W. (2021). Effect of prolonged exposure, intensified prolonged exposure and STAIR+prolonged exposure in patients with PTSD related to childhood abuse: A randomized controlled trial. European Journal of Psychotraumatology, 12(1), 1851511. https://doi.org/10.1080/20008198.2020.1851511
- Pagani, M., Castelnuovo, G., Daverio, A., La Porta, P., Monaco, L., Ferrentino, F., Chiaravalloti, A., Fernandez, I., & Di Lorenzo, G. (2018). Metabolic and electrophysiological changes associated to clinical improvement in Two severely traumatized subjects treated with EMDR—A pilot study. Frontiers in Psychology, 9, 475. https://doi.org/10.3389/fpsyg.2018.00475
- Phelps, A. J., Lethbridge, R., Brennan, S., Bryant, R. A., Burns, P., Cooper, J. A., Forbes, D., Gardiner, J., Gee, G., Jones, K., Kenardy, J., Kulkarni, J., McDermott, B., McFarlane, A. C., Newman, L., Varker, T., Worth, C., & Silove, D. (2022). Australian guidelines for the prevention and treatment of posttraumatic stress disorder: Updates in the third edition. Australian & New Zealand Journal of Psychiatry, 56(3), 230–247. https://doi.org/10.1177/00048674211041917
- Rodenburg, R., Benjamin, A., Meijer, A. M., & Jongeneel, R. (2009). Eye movement desensitization and reprocessing in an adolescent with epilepsy and mild intellectual disability. Epilepsy & Behavior, 16(1), 175–180. https://doi.org/10.1016/j.yebeh.2009.07.015
- Rosenthal, R. (1991). Meta-analytic procedures for social research (2nd ed). Sage.
- Scott, J. C., Harb, G., Brownlow, J. A., Greene, J., Gur, R. C., & Ross, R. J. (2017). Verbal memory functioning moderates psychotherapy treatment response for PTSD-related nightmares. Behaviour Research and Therapy, 91, 24–32. https://doi.org/10.1016/j.brat.2017.01.004
- Shapiro, F. (2001). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures (2nd ed.). Guilford Press.
- Stein, L. A., Goldmann, E., Zamzam, A., Luciano, J. M., Messé, S. R., Cucchiara, B. L., Kasner, S. E., & Mullen, M. T. (2018). Association between anxiety, depression, and post-traumatic stress disorder and outcomes after ischemic stroke. Frontiers in Neurology, 9, 890. https://doi.org/10.3389/fneur.2018.00890
- Susanty, E., Sijbrandij, M., van Dijk, W., Srisayekti, W., de Vries, R., & Huizink, A. C. (2022). The effects of psychological interventions on neurocognitive functioning in posttraumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 13(1), 2071527. https://doi.org/10.1080/20008198.2022.2071527
- Tanev, K. S., Pentel, K. Z., Kredlow, M. A., & Charney, M. E. (2014). PTSD and TBI co-morbidity: Scope, clinical presentation and treatment options. Brain Injury, 28(3), 261–270. https://doi.org/10.3109/02699052.2013.873821
- Timman, R., de Jong, K., & de Neve-Enthoven, N. (2017). Cut-off scores and clinical change indices for the Dutch outcome questionnaire (OQ-45) in a large sample of normal and several psychotherapeutic populations. Clinical Psychology & Psychotherapy, 24(1), 72–81. https://doi.org/10.1002/cpp.1979
- Utz, K. S., Kiphuth, I. C., & Schenk, T. (2019). Posttraumatic stress disorder in patients after transient ischemic attack: A one-year follow-up. Journal of Psychosomatic Research, 122, 36–38. https://doi.org/10.1016/j.jpsychores.2019.04.016
- van den Berg, D. P. G., de Bont, P. A. J. M., van der Vleugel, B. M., de Roos, C., de Jongh, A., Van Minnen, A., & van der Gaag, M. (2015). Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder. JAMA Psychiatry, 72(3), 259–267. https://doi.org/10.1001/jamapsychiatry.2014.2637
- van den Hout, M. A., & Engelhard, I. M. (2011). Hoe het komt dat EMDR werkt. Directieve Therapie, 31(1), 5–23. https://doi.org/10.1007/s12433-011-0002-5
- van der Ploeg, E., Mooren, T. T. M., Kleber, R. J., van der Velden, P. G., & Brom, D. (2004). Construct validation of the Dutch version of the impact of event scale. Psychological Assessment, 16(1), 16–26. https://doi.org/10.1037/1040-3590.16.1.16
- van Oort, R., & van Zandvoort, M. (2016). Eye movement desensitization and reprocessing (EMDR) bij niet-aangeboren hersenletsel. Tijdschrift Voor Neuropsychologie, 11(2), 109–119.
- Van Praag, D. L. G., Cnossen, M. C., Polinder, S., Wilson, L., & Maas, A. I. R. (2019). Post-Traumatic stress disorder after civilian traumatic brain injury: A systematic review and meta-analysis of prevalence rates. Journal of Neurotrauma, 36(23), 3220–3232. https://doi.org/10.1089/neu.2018.5759
- van Vliet, N. I., Huntjens, R. J. C., van Dijk, M. K., Bachrach, N., Meewisse, M.-L., & de Jongh, A. (2021). Phase-based treatment versus immediate trauma-focused treatment for post-traumatic stress disorder due to childhood abuse: Randomised clinical trial. BJPsych Open, 7(6), e211. https://doi.org/10.1192/bjo.2021.1057
- Vink, M., Janssen, E., & Zaal, A. (2016). Eye movement desensitization and reprocessing. In P. Smits, R. Ponds, N. Farenhorst, M. Klaver, & R. Verbeek (Eds.), Handboek neuropsychotherapie (pp. 189–211). Amsterdam.
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., Keane, T. M., & Marx, B. P. (2018). The clinician-administered PTSD scale for DSM-5 (CAPS-5): development and initial psychometric evaluation in military veterans. Psychological Assessment, 30(3), 383–395. https://doi.org/10.1037/pas0000486
- Whelan-Goodinson, R., Ponsford, J., Johnston, L., & Grant, F. (2009). Psychiatric disorders following traumatic brain injury. Journal of Head Trauma Rehabilitation, 24(5), 324–332. https://doi.org/10.1097/HTR.0b013e3181a712aa
- Wilson, G., Farrell, D., Barron, I., Hutchins, J., Whybrow, D., & Kiernan, M. D. (2018). The use of eye-movement desensitization reprocessing (EMDR) therapy in treating post-traumatic stress disorder—A systematic narrative review. Frontiers in Psychology, 9, 923. https://doi.org/10.3389/fpsyg.2018.00923
- Wolpe, J. (1969). The practice of behavior therapy. Pergamon.
- World Health Organization. (2013). Guidelines for the management of conditions specifically related to stress. 2013/12/19 ed. Vol. 21, Geneva, Switzerland: World Health Organization.
