ABSTRACT
Background: Exposure to earthquakes can cause adverse effects on the mental health of survivors, including an increased risk of PTSD.
Objective: This systematic review aims to analyse the previous secondary studies to identify the risk factors for PTSD from children to elderly earthquake survivors. In addition, it aims to consider the complexity of the joint effects of the individual, relational, and contextual risk factors, to also detect the most at-risk families.
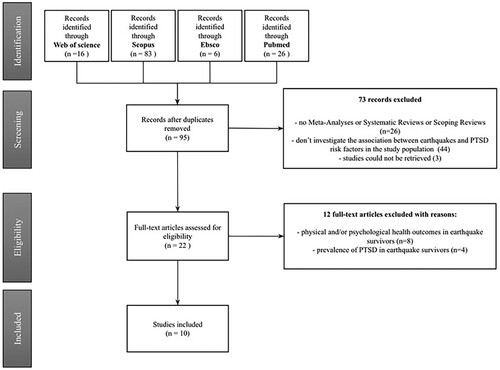
Method: After reviewing and screening studies from the literature search through PubMed, Web of Science, Scopus, and EBSCO under the guidance of PRISMA guidelines, ten eligible secondary studies were identified that examine the risk factors for PTSD in individuals (from children to elderly) affected by worldwide earthquakes.
Results: The analysis of the included studies allowed the identification of a series of socio-demographic, pre-traumatic, peri-traumatic, and post-traumatic PTSD risk factors in children, adolescents, youth, adults, and elderly survivors. The results represent the complexity of the joint effects of these risk factors at individual, relational, and contextual levels.
Conclusions: The consideration of the PTSD risk factors highlights the importance of individual characteristics and the type of experiences and exposure in the period before, during, and after the earthquake. This knowledge could allow the early identification of at-risk individuals of different ages and families and the implementation of intervention programmes.
HIGHLIGHTS
This is the first systematic review to identify PTSD risk factors from children to elderly earthquake survivors using secondary studies.
Considering the complexity of the joint effects at individual, relational, and contextual levels, several socio-demographic, pre-traumatic, peri-traumatic, and post-traumatic risk factors for PTSD were identified in the age groups considered. Moreover, the consideration of these factors could help the identification of at-risk families.
The identification of risk factors for PTSD across the lifespan could provide helpful knowledge for prevention and intervention programmes.
Antecedentes: La exposición a terremotos puede causar efectos adversos en la salud mental de los sobrevivientes, incluyendo un mayor riesgo de Trastorno de Estrés Postraumático (TEPT).
Objetivo: Esta revisión sistemática tiene como objetivo analizar los estudios secundarios previos para identificar los factores de riesgo de TEPT en sobrevivientes de un terremoto, desde niños hasta ancianos. Además, pretende considerar la complejidad de los efectos conjuntos de los factores de riesgo individuales, relacionales y contextuales, para detectar también a las familias en mayor riesgo.
Método: Después de revisar y seleccionar estudios de la búsqueda bibliográfica a través de PubMed, Web of Science, Scopus y EBSCO, bajo la guía de las pautas PRISMA, se identificaron diez estudios secundarios elegibles que examinan los factores de riesgo para TEPT en individuos afectados por terremotos en todo el mundo (desde niños hasta ancianos).
Resultados: El análisis de los estudios incluidos permitió identificar una serie de factores de riesgo de TEPT sociodemográficos, pretraumáticos, peritraumáticos y postraumáticos en niños, adolescentes, jóvenes, adultos y ancianos sobrevivientes. Los resultados representan la complejidad de los efectos conjuntos de estos factores de riesgo a nivel individual, relacional y contextual.
Conclusiones: La consideración de los factores de riesgo para TEPT resalta la importancia de las características individuales y el tipo de experiencias y exposición en el período previo, durante y después del terremoto. Este conocimiento podría permitir la identificación temprana de personas en riesgo de diferentes edades y familias, y la implementación de programas de intervención.
PALABRAS CLAVE:
1. Introduction
1.1. PTSD and other psychological consequences of earthquakes
Earthquakes could cause a significant impact on communities in terms of high economic losses, structural damages, affected people, deaths (CRED, Citation2023; Yaghmaei, Citation2020), and possible survivors’ adverse psychological outcomes (e.g., Cénat et al., Citation2020). More specifically, previous research indicated a wide range of adverse psychological consequences. These include sleep difficulties, distress, depression, suicidal ideations, anxiety, post-traumatic stress disorder (PTSD), and increased alcohol consumption (see reviews of Cénat et al., Citation2020; Dai et al., Citation2016; Kušević et al., Citation2021). PTSD is one of the most prevalent psychological disorders among disaster survivors (Hong & Efferth, Citation2016). The prevalence rates of post-earthquake PTSD range from 2.5% to 60% in children and adolescents and from 4% to 67% in adults (Tang et al., Citation2017). PTSD is characterised by the appearance of specific symptomatology following direct exposure (experiencing a traumatic event firsthand or witnessing a traumatic event occur to others) or indirect exposure (learning of an event that happened to close ones or experiencing repeated or extreme exposure to adverse details of the event) to traumatic events) (APA, Citation2013, Citation2022). More specifically, the diagnostic criteria include four symptom clusters in the DSM-5/5-TR (intrusive symptoms, avoidance, negative cognition and mood, alterations of arousal states) (APA, Citation2013, Citation2022) and three symptom clusters in the ICD-11 (re-experiencing, avoidance, persistent sense of threat, WHO, Citation2018).
1.2. PTSD risk factors in earthquake survivors
Considering the remarkable presence and variability in the range of post-disaster PTSD rates among earthquake survivors, many studies focused on the understanding of the risk factors of PTSD symptom onset. Risk factors are those characteristics, variables, or hazards that precede or increase the likelihood of developing a disorder (Tortella-Feliu et al., Citation2019). Some studies (Sayed et al., Citation2015; Tortella-Feliu et al., Citation2019; Trickey et al., Citation2012) classified the PTSD risk variables into four descriptive categories: (1) socio-demographic factors (e.g., gender); (2) pre-trauma factors (before the traumatic experience; e.g., prior mental ill-health); (3) peritraumatic factors (during or in the immediate aftermath of the traumatic experience; e.g., trauma severity); and (4) post-trauma factors (in the period after traumatic experiences, e.g., low social support).
1.3. The present study
In the literature, the availability of secondary studies (reviews, systematic reviews, and meta-analyses) is noteworthy to summarise the empirical results about the role of some risk factors in predicting PTSD onset. However, some of these significant secondary studies showed some limitations. More specifically, some focus mainly only on specific age groups (e.g., Gordon-Hollingsworth et al., Citation2015, which detected PTSD risk factors in only children/adolescents), while others did not deepen the impact of the risk factors identified (e.g., Aker, Citation2006), and still others considered only a few most significant risk factors in different age groups (e.g., Tang et al., Citation2017). To our knowledge, a paucity of secondary studies examined and deepened the impact of PTSD risk factors in survivors of different ages simultaneously. Moreover, these studies did not identify the individual, relational, and contextual risk factors that could allow the identification of at-risk families. To overcome this limitation, the present systematic review aims to analyse previous secondary studies to identify the individual, relational, and contextual PTSD risk factors for survivors of different ages, that could help the identification of at-risk individuals and families.
2. Method
2.1. Search strategy
This systematic review was conducted in March 2023 under the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Page et al., Citation2021) to identify secondary studies (systematic reviews and meta-analyses) published from 2003 to 2023 that examine or report PTSD risk factors in children, adolescents, youth, adults and elderly affected by the earthquakes. The electronic databases of Web of Science, Scopus, Pubmed, and EBSCO (to locate studies in APA PsycArticles and APA PsycINFO) were used for an advanced search using the keywords (‘Meta-analysis’ or ‘Systematic review’) AND (‘PTSD’ or ‘Post-traumatic stress disorder’) AND (‘Earthquake’ or ‘Seismic events’).
2.2. Eligibility criteria and quality assessment
Studies eligible for this systematic review had to fulfil specific inclusion criteria described in . Specifically, included studies had to be meta-analyses, systematic reviews, or scoping reviews that examined or reported PTSD risk factors in children, adolescents, youth, adults, or elderly earthquake survivors. PTSD can be defined in any edition of the International Classification of Diseases (ICD) manual or the Diagnostic and Statistical Manual of Mental Disorders (DSM) and assessed using validated interviews or questionnaires. In addition, studies could come from any Country and be published from 2003 to 2023.
Taking as reference the indications of Kitchenham et al. (Citation2022) and the JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses (2017), we assessed the quality of the selected secondary studies of the present review. Specifically, we considered the following criteria: the review questions, the explicit description of the period covered by the search, the clear indication of the rules of inclusion/exclusion of the studies, the description of the quality/validity of the included studies; the precise description of the search strategy, the description of the resources used for the search, the presence of two or more reviewers. Based on these listed criteria, we can outline that most of the secondary studies of the present review are appropriate.
3. Results
3.1. Systematic search results
This search produced 131 articles. Of these identified articles, 36 records were eliminated as duplicates, 73 records were excluded after their abstract evaluation, and 22 full-text articles were assessed for eligibility. Regarding these 22 papers, 12 were excluded based on the appraisal of the full text, and ten were included for the analysis in this review. We excluded 12 full-text articles because these did not specifically investigate the association between earthquakes and PTSD risk factors in the study population. Their focus was on physical and/or psychological health outcomes in earthquake survivors and the prevalence of PTSD in earthquake survivors. The flow diagram (), created according to the PRISMA 2020 statement (Page et al., Citation2021), describes the steps for the study selection process and related exclusion criteria, which are better explained in .
Table 1. Inclusion and exclusion criteria.
3.2. Characteristics of included studies
The ten included secondary studies examined PTSD risk factors in children, adolescents, youth, adults, and elderly victims of earthquakes. These secondary studies were three scoping reviews (Aker, Citation2006; Farooqui et al., Citation2017; KalantarMotamedi et al., Citation2012), three systematic reviews (Alipour & Ahmadi, Citation2020; Hong & Efferth, Citation2016; Liang et al., Citation2019), two systematic reviews and meta-analyses (Cénat et al., Citation2020; Dai et al., Citation2016), and two meta-analyses (Gordon-Hollingsworth et al., Citation2015; Tang et al., Citation2017). These studies came from Europe, America, and Asia and considered different earthquakes, including Wenchuan, Marmara, and Haiti. Considering these ten secondary studies, we examined the cited primary studies that analysed the PTSD risk factors in earthquake survivors. A total of 109 primary studies were extracted from the 10 included secondary studies, of which 46 primary studies were about children, adolescents, and youth (the age ranged from 2 years to university students), 59 were about adults (community-based studies without a specific age range), and finally, three specifically were about elderly (the age ranged from 60 to >81 years). The analysis of each PTSD risk factor is shown in .
Table 2. PTDS risk factor in children, adolescents, and youth earthquake survivors.
Table 3. PTDS risk factor in adult earthquake survivors (community studies).
Table 4. PTDS risk factor in the elderly earthquake survivors.
3.3. Results and classification of PTSD risk factors
The analysis of the included studies allowed the identification of a series of PTSD risk factors in children, adolescents, youth, adults, and the elderly (see for the complete list of PTSD risk factors and the references). These risk factors range across individual, relational, and contextual levels, considering the four categories of PTSD risk factors in terms of socio-demographic, pre-traumatic, peri-traumatic, and post-traumatic risk factors.
3.4. Socio-demographic risk factors
Several socio-demographic risk factors could expose survivors to the risk of PTSD after earthquakes. The following subsections describe some of those PTSD risk factors identified in earthquake survivors across the lifespan (see ).
3.4.1. Female gender
Female gender is a significant PTSD risk factor (Hong & Efferth, Citation2016; Tang et al., Citation2017). Studies outlined the genetic, biological, psychosocial, and cultural factors that may be involved in explaining the gender differences in terms of women's more sensitivities to stress hormones, perceived threats, less effective coping strategies, greater propensity to interpret disasters more negatively, and increased stress due to their traditional role in society than men (Korol et al., Citation1999; Tang et al., Citation2017; Zhou et al., Citation2013).
3.4.2. Older age
Some studies (Hong & Efferth, Citation2016; Tang et al., Citation2017) suggested that older age could be a PTSD risk factor. For example, adolescents who could cognitively understand the event and its negative consequences could have adverse predictions for the future, increasing their stress and psychological maladjustment (Liu et al., Citation2010; Tang et al., Citation2017). Older adults could experience high stress related to careers, family burdens, and elderly relatives (Guo et al., Citation2015), while the elderly could face multiple sets of difficulties regarding health and mobility problems, inadequate financial resources, lack of personal transportation, and small social networks (Chen et al., Citation2012).
3.4.3. Low educational level and economic difficulties
Low educational level and economic difficulties (e.g., low socio-economic status, no/low income, and unemployment) could be significant PTSD risk factors (Hong & Efferth, Citation2016; Tang et al., Citation2017), because they could be associated with poorer coping skills, social status, social networks, and health behaviour (Chen et al., Citation2012; Tang et al., Citation2017).
3.4.4. Marital status
In the elderly, being widowed is identified as a PTSD risk factor (Chen et al., Citation2012). Conversely, for adults, findings about marital status are conflicting (Kun et al., Citation2013; Wang et al., Citation2011). Indeed, marriage could be a double-edged sword because married people could be overly worried about the damage to family members and possessions. Conversely, unmarried/divorced/widowed people could be more vulnerable due to a lack of emotional support (Guo et al., Citation2017). In addition, people who have lost a spouse could have suffered more mental stress and feelings of helplessness (Chen et al., Citation2012).
3.4.5. Having siblings
Some studies indicated that having siblings could be a PTSD risk factor in children and adolescents. This is because the recovery process in multi-child families may be hindered by less parental care and support and by the eventual presence of more injuries in family members (Zhang et al., Citation2012). In addition, one study suggested that compared to children with siblings, only children could possess some positive personality traits, such as extroversion, optimism, and gregariousness (Fan et al., Citation2015).
3.4.6. Nuclear family
Studies showed how living in a nuclear family could be a PTSD risk factor due to the presence of less significant social support than in joint family contexts (three generations or more) (Jin & Wang, Citation2014; Naeem et al., Citation2011).
3.5. Pre-trauma PTSD risk factors
Studies showed several pre-trauma risk factors concerning personal and loved ones’ backgrounds. The following subsections describe the PTSD risk factors identified in earthquake survivors across the lifespan (see ).
3.5.1. Personal and loved ones history of mental ill-health
Personal and loved ones’ histories of mental ill-health are identified as PTSD risk factors (Aker, Citation2006; Gökçen et al., Citation2013). Mental health allows individuals to have fulfilled lives, develop and manage relations, study, work, follow interests, and decide about education, employment, housing, etc. Conversely, mental ill-health can adversely affect these abilities and decisions, causing reduced functioning at the personal, family, relational, and social levels. In addition, a loved one's history of mental ill-health could make individuals more vulnerable due to the significant caregiving burden provided (Cerdá et al., Citation2013).
3.5.2. Previous trauma
Experience of previous trauma is a PTSD risk factor (Gordon-Hollingsworth et al., Citation2015; Tang et al., Citation2017). According to the sensitivity perspective, individuals traumatised in the face of subsequent adversity are more likely to suffer greater vulnerability and psychological distress than individuals without a history of trauma. These individuals could undergo reactivation following further exposure to stressors, especially if there is a similarity to the initial trauma (Başoğlu et al., Citation2004; Solomon, Citation1993; Solomon et al., Citation2021; Ying et al., Citation2013).
3.5.3. Neuroticism
One study (Chen et al., Citation2017) showed that, in the presence of high neuroticism in children, the risk of suffering a co-occurrence of PTSD and depressive symptoms was 40 times higher. This is because the overlapping aspect of neuroticism and arousal symptoms could contribute to its effect on the increased risk of PTSD.
3.5.4. Locus of control
Chance locus of control and powerful others locus of control were found to be the two risk factors for the severity of PTSD symptoms in adolescents because the belief that the outcomes of events were controlled by chance or powerful others led survivors to think they could not do anything, such as seeking help or believe social supports useless (Zhang et al., Citation2011).
3.5.5. Negative coping
Studies evidenced that negative/maladaptive coping (e.g., denial, behavioural disengagement, self-blame) could be a PTSD risk factor, in contrast to the protective effects of positive/adaptive coping (e.g., positive restructuring, active coping, and seeking emotional support). This is because positive coping, in contrast to negative coping, increases the likelihood of resistance and allows the adaptation to stress (Cofini et al., Citation2015; Fan et al., Citation2015).
3.6. Peri-trauma PTSD risk factors
Several experiences of objective (direct and indirect) and subjective exposure during or immediately after the earthquakes are identified as peri-trauma risk factors for PTSD. The following subsections describe some of those PTSD risk factors identified in earthquake survivors across the lifespan (see ).
3.6.1. Being buried/trapped or injured during the earthquake
The direct experience of being buried/trapped and injured is a significant PTSD risk factor due to the high level of experienced fear, pain, and mortal danger. Moreover, the stress and rehabilitation accompanying injury and the consequences of the injuries, in terms of amputation and disability, could reduce the quality of life (Hong & Efferth, Citation2016; Tang et al., Citation2017).
3.6.2. Witnessing earthquake-related traumatic and stressful events
Direct witnessing of severe traumatic and stressful scenes during the earthquake is a PTSD risk factor (Hong & Efferth, Citation2016). These experiences could lead to more intense fear reactions and perceived life threats (Boztaş et al., Citation2019) and adversely affect cognitive and emotional functioning (Fan et al., Citation2015). In addition, for children and adolescents, parents are role models for dealing with stress; thus, witnessing parents experiencing extreme reactions could increase children's feelings of insecurity, fear, helplessness, and anxiety (Ekşi et al., Citation2007).
3.6.3. Bereavement or injury of a loved one
Bereavement and injury of loved ones are significant PTSD risk factors (Hong & Efferth, Citation2016). Loved one loss removes part of the support resources from close relationships at a time of intense need, compounding the psychological stress (Tang et al., Citation2017). In addition, the loss/injury of a loved one could impact the affective attachment system of survivors with significant consequences for their well-being (Fan et al., Citation2015).
3.6.4. Subjective experiences
Subjective experiences or ‘peritraumatic reactions’ include thoughts and feelings experienced by the individual during the traumatic event (Massazza et al., Citation2021). The subjective responses of fear, fear for the safety of loved ones, helplessness, and horror are peritraumatic distress reactions that make the recovery from trauma difficult (Tang et al., Citation2017; Thomas et al., Citation2012; Vahidniya et al., Citation2023; Ying et al., Citation2013). Moreover, studies showed that the symptoms of dissociation and hyper-arousal contributed to the prediction of PTSD symptoms six months after the earthquake, suggesting that such initial symptoms could tend to persist over time (Priebe et al., Citation2009).
3.7. Post-trauma PTSD risk factors
Regarding the post-earthquake period, several objective (earthquake consequences) and subjective (post-earthquake symptoms or perceptions or personal responses) risk factors for PTSD were detected. The following subsections describe some of those PTSD risk factors identified in earthquake survivors across the lifespan (see ).
3.7.1. Material losses and houses damaged or destroyed
The destruction/damage of houses and possessions are significant PTSD risk factors (Hong & Efferth, Citation2016). These factors could act as intense and life-threatening stressors, and they also could aggravate the secondary adversities (e.g., relocation, resettlement, change in care-taking, change in family finances, medical and rehabilitative treatment for personal injuries and disabilities). In addition, for children, severe loss of family possessions could increase the negative effect of fearfulness, anxiety, worry, and upset about the family's future (Chen et al., Citation2007; Zhang et al., Citation2011).
3.7.2. Participation in rescue work
Participation in rescue work is a PTSD risk factor identified in adults (Aker, Citation2006). This participation could expose them to stressful situations, feelings of anxiety and helplessness, desperation, self-blame, and guilt resulting from the impossibility of saving people or loved ones.
3.7.3. Low social support
Low social support is a PTSD risk factor (Gordon-Hollingsworth et al., Citation2015; Hong & Efferth, Citation2016), probably due to feelings of isolation and loneliness, which could make it difficult to cope with the trauma (Vahidniya et al., Citation2023). Therefore, adequate social support could act as a buffer that heightens tolerance to stressful life events and facilitates increased feelings of safety and strength, consequently enhancing positive coping mechanisms, promoting and protecting psychological well-being, and improving overall adaptations (Gordon-Hollingsworth et al., Citation2015; Mesidor & Sly, Citation2019). In the specific case of children and adolescents, low social support may depend on the absence of parents or difficulties in parents in their role as supportive parents (Cadichon et al., Citation2017).
3.7.4. Post-earthquake adverse life events and traumatic events
Individuals who experience other traumatic events after an earthquake could be more sensitive to the effect of the experience (Fan et al., Citation2015; Guo et al., Citation2017). The additive effect of post-earthquake adverse life events could aggravate post-disaster stress reactions by increasing daily hassles and strains and affecting recovery from the earthquake (Fan et al., Citation2015).
3.7.5. Post-traumatic cognition
Post-traumatic cognition emerged as a PTSD risk factor (Ma et al., Citation2011). Maladaptive cognitive styles seem to be relevant for emotional regulation problems and the onset of PTSD (Ehlers et al., Citation2003). Social support could reduce the impact of earthquakes by influencing post-traumatic cognition. However, in individuals with extremely negative cognition, social support could have little effect on PTSD (Ma et al., Citation2011).
4. Discussion
To our knowledge, this is the first systematic review aimed at analyzing the previous secondary studies regarding the PTSD risk factors in earthquake survivors of different ages. Our analysis identified several socio-demographic, pre-traumatic, peri-traumatic, and post-traumatic risk factors for PTSD, from children to the elderly (see ), considering the complexity of the joint risk factors on an individual, relational, and contextual level.
PTSD is one of the adverse psychological consequences for earthquake survivors (Kušević et al., Citation2021). Since PTSD symptomatology not only causes clinically significant distress but also impairment in social, occupational, or other significant areas of functioning (APA, Citation2022), it becomes essential to prevent its onset in vulnerable survivors and subsequent risk of chronicity. In this direction, the PTSD risk factors could be helpful to understand the possible variables involved in PTSD risk trajectories that make individuals and families more vulnerable to PTSD.
Specifically, socio-demographic and pre-traumatic risk factors highlight how several pre-existing characteristics and backgrounds could expose survivors at-risk of PTSD. For instance, the female gender could be at higher risk of PTSD due to genetic, biological, psychosocial, and cultural factors (Korol et al., Citation1999; Tang et al., Citation2017; Zhou et al., Citation2013). In addition, having a low level of education and economic difficulties could expose one to greater vulnerability to PTSD as it is associated with poorer social status, social networks, health behaviours, and coping skills (Chen et al., Citation2012; Tang et al., Citation2017). Furthermore, having negative/maladaptive coping could counteract resilience and adaptation to stress (Cofini et al., Citation2015; Fan et al., Citation2015). Moreover, having previous trauma could increase vulnerability, psychological distress, and reactivation following exposure to stressors, especially if there is a similarity with the initial trauma (Başoğlu et al., Citation2004; Ying et al., Citation2013).
In addition, peritraumatic risk factors outline the significant role of exposure and subjective experiences during earthquakes in PTSD survivors’ vulnerability. For instance, being buried/trapped and injured could cause high exposure to danger, stress, fear, pain, and the possible consequences of injuries in terms of amputation and disability (Hong & Efferth, Citation2016; Tang et al., Citation2017). In addition, direct witnessing of severe traumatic and stressful scenes could provoke more intense fear reactions and life-threatening perceptions and negatively affect cognitive and emotional functioning (Boztaş et al., Citation2019; Fan et al., Citation2015; Hong & Efferth, Citation2016). In addition, subjective experiences could also make recovery from trauma difficult (Tang et al., Citation2017; Thomas et al., Citation2012; Vahidniya et al., Citation2023; Ying et al., Citation2013).
Similarly, post-traumatic risk factors underline the significance of the variables of the post-earthquake period on PTSD risk vulnerability. For instance, the destruction/damage of houses and possessions could act as intense and life-threatening stressors. Also, it could aggravate secondary adversities (e.g., relocation, change in family finances) (Hong & Efferth, Citation2016). Furthermore, the additive effect of other traumatic events after the earthquake might lead individuals to be more sensitive, leading to aggravated stress and tension reactions that impair recovery (Fan et al., Citation2015; Guo et al., Citation2017).
An important aspect of this systematic review is to emphasize the multifactorial nature associated with the risk of PTSD in earthquake survivors, considering the complexity of joint PTSD risk factors linked not only to individual and contextual aspects but also to relational ones related to the family system and other interpersonal relationships. The relational perspective on PTSD risk factors could provide interesting future lines of research insights into the role of family and interpersonal relationships in the vulnerability, onset, and maintenance of PTSD in earthquake survivors. For instance, married people seem to be more at PTSD risk due to increased concern about damage to family members and property, while unmarried/divorced/widowed people could suffer from a lack of emotional support (Guo et al., Citation2017; Tang et al., Citation2017). In addition, having a loved one with a history of mental ill-health seems to make survivors more vulnerable to PTSD due to the significant burden of care. Similarly, adults could experience high stress related to family burdens and elderly relatives’ care (Guo et al., Citation2015). Moreover, a loved one loss could affect part of the support resources from close relationships (Tang et al., Citation2017) and, together with the injury of loved ones, could impact the affective attachment system of survivors (Fan et al., Citation2015). As for low social support, it could cause feelings of isolation and loneliness, which could make it difficult to cope with the trauma (Vahidniya et al., Citation2023). Moreover, living in a nuclear family could be associated with less significant social support than in joint family contexts (Jin & Wang, Citation2014; Naeem et al., Citation2011). However, the recovery process in multi-child families could be compromised by reduced parental care and support to children and the possible presence of more injured family members (Zhang et al., Citation2012). Furthermore, witnessing parents’ extreme reactions (such as crying, fainting, or panic) could increase feelings of insecurity, fear, helplessness, and anxiety in children, as parents are role models in dealing with stress (Ekşi et al., Citation2007). Indeed, children's incomplete cognitive and emotional development makes them particularly vulnerable to influences on parents’ emotion regulation, stress responses, and coping strategies (La Greca & Prinstein, Citation2002; Ozturk et al., Citation2023). In addition, severe loss of family possessions could increase children's fearfulness, anxiety, worry, and upset about the family's future (Chen et al., Citation2007; Zhang et al., Citation2011).
Therefore, studying PTSD risk factors could be a useful strategy in the psychological operational context in response to earthquakes. Specifically, these factors could help in secondary prevention (preventing disease progression through the early identification of cases at risk) and in tertiary prevention (preventing and decreasing disease severity/complications) (Lowe et al., Citation2015). Indeed, early knowledge of these risk factors could provide a more complex view of the etiology and the underlying mechanisms of the vulnerability to PTSD symptoms (Georgescu & Nedelcea, Citation2023). Consequently, it could promote preventive strategies for the early identification of vulnerable or high-risk individuals and families in the acute phase post-earthquake, which could lead to early diagnosis and/or implementation of support and intervention programmes. Therefore, such strategies could positively contribute to reducing the onset and duration of PTSD, preventing its chronicity and severity in survivors of earthquakes (Tang et al., Citation2017; Wafa et al., Citation2019) and even other natural phenomena. Indeed, the literature showed that some of the PTSD risk factors reported in the present systematic review were also identified in other studies related to different types of natural phenomena, such as floods (Shabani et al., Citation2024), tornadoes (Lee & First, Citation2022), and tsunamis (Pyari et al., Citation2012). For instance, common PTSD factors with earthquake survivors are female gender, economic difficulties, unemployment, low education level, previous trauma, history of mental ill-health, personal and family injury, loss of a loved one, property damage, and limited access to health services. The findings of the present review may, therefore, be useful in future studies to improve the understanding of PTSD vulnerability after large-scale events.
4.1. Limitation and future perspectives
The present study has some limitations. The primary studies extracted reported significant heterogeneity due to differences in sampling, variety of worldwide earthquakes and impacts and effects on the earthquake-affected population, design, measurement for PTSD, and statistical analysis. Therefore, these limitations may have influenced the findings. In addition, some risk factors have only been studied and reported in one or a few studies and should, therefore, be further investigated in other empirical studies. Moreover, the present review emphasized the importance of considering the complexity of joint PTSD risk factors linked not only to individual and contextual aspects but also to relational ones related to the family system and other interpersonal relationships. To date, the potential role of risk factors related to family relationships and dynamics (such as family functioning, marital relationship, co-parenting, and parent–child relationship) is still limited. Future research could better explore the potential impact of the quality of family relationships on the onset and chronicity of PTSD and mental health problems in earthquake victims.
5. Conclusion
The systematic review deepened the knowledge of PTSD risk factors in earthquake survivors of different ages, considering the complexity of the joint effects at the individual, relational, and contextual levels. Identifying risk factors for PTSD across the lifespan could provide helpful knowledge for prevention and intervention programmes for vulnerable survivors.
Acknowledgments
We wish to express our thanks to the MEDEA project co-founded by the EU (CUP:H87G22000140006) for funding this systematic review.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
As this article is a systematic review, data sharing is not applicable because no new data were created or analysed in this study.
Additional information
Funding
References
- Aker, A. T. (2006). 1999 marmara Depremleri: EpidemiyolojikBulgularveToplumRuhSağliğiUygulamalariUzerine Bir GözdenGeçirme [1999 Marmara earthquakes: A review of epidemiologic findings and community mental health policies]. Turk psikiyatridergisi = Turkish Journal of Psychiatry, 17(3), 204–212.
- Alipour, F., & Ahmadi, S. (2020). Social support and Posttraumatic Stress Disorder (PTSD) in earthquake survivors: A systematic review. Social Work in Mental Health, 1–14. doi:10.1080/15332985.2020.1795045.
- American Psychiatric Association. (2013). Manuale diagnostico e statistico dei disturbi mentali, Quinta edizione (DSM-5). Trad. it. Raffaello Cortina, Minano 2014.
- American Psychiatric Association (Ed.). (2022). Diagnostic and statistical manual of mental disorders: DSM-5-TR (Fifth edition, text revision). American Psychiatric Association Publishing.
- Başoğlu, M., Kiliç, C., Salcioğlu, E., & Livanou, M. (2004). Prevalence of posttraumatic stress disorder and comorbid depression in earthquake survivors in Turkey: An epidemiological study. Journal of Traumatic Stress, 17(2), 133–141. https://doi.org/10.1023/B:JOTS.0000022619.31615.e8
- Boztaş, M. H., Aker, A. T., Münir, K., Çelik, F., Aydın, A., Karasu, U., & Mutlu, E. A. (2019). Post traumatic stress disorder among adults in the aftermath of 2011 Van-Ercis earth-quake in Turkey. KlinikPsikiyatriDergisi-Turkish Journal of Clinical Psychiatry, 22, 380–388. https://doi.org/10.5505/kpd.2019.62534.
- Cadichon, J. M., Lignier, B., Cénat, J. M., & Derivois, D. (2017). Symptoms of PTSD among adolescents and young adult survivors six years after the 2010 Haiti earthquake. Journal of Loss and Trauma, 22(8), 646–659. https://doi.org/10.1080/15325024.2017.1360585
- Cénat, J. M., McIntee, S. E., & Blais-Rochette, C. (2020). Symptoms of posttraumatic stress disorder, depression, anxiety and other mental health problems following the 2010 earthquake in Haiti: A systematic review and meta-analysis. Journal of Affective Disorders, 273, 55–85. https://doi.org/10.1016/j.jad.2020.04.046
- Cerdá, M., Paczkowski, M., Galea, S., Nemethy, K., Péan, C., & Desvarieux, M. (2013). Psychopathology in the aftermath of the Haiti earthquake: A population-based study of posttraumatic stress disorder and major depression. Depression and Anxiety, 30(5), 413–424. https://doi.org/10.1002/da.22007
- Chen, C. H., Tan, H. K., Liao, L. R., Chen, H. H., Chan, C. C., Cheng, J. J., Chen, C. Y., Wang, T. N., & Lu, M. L. (2007). Long-term psychological outcome of 1999 Taiwan earthquake survivors: A survey of a high-risk sample with property damage. Comprehensive Psychiatry, 48(3), 269–275. https://doi.org/10.1016/j.comppsych.2006.12.003
- Chen, G., Shen, H., & Chen, G. (2012). A cross-sectional study on posttraumatic stress disorder among elderly Qiang citizens 3 years after the Wenchuan earthquake in China. The Canadian Journal of Psychiatry, 57(9), 547–553. https://doi.org/10.1177/070674371205700905
- Chen, X., Xu, J., Li, B., Li, N., Guo, W., Ran, M. S., Zhang, J., Yang, Y., & Hu, J. (2017). The role of personality and subjective exposure experiences in posttraumatic stress disorder and depression symptoms among children following Wenchuan earthquake. Scientific Reports, 7(1), 17223. https://doi.org/10.1038/s41598-017-17440-9
- Cofini, V., Carbonelli, A., Cecilia, M. R., Binkin, N., & di Orio, F. (2015). Post traumatic stress disorder and coping in a sample of adult survivors of the Italian earthquake. Psychiatry Research, 229(1-2), 353–358. https://doi.org/10.1016/j.psychres.2015.06.041
- CRED. (2023). 2022 Disasters in numbers.
- Dai, W., Chen, L., Lai, Z., Li, Y., Wang, J., & Liu, A. (2016). The incidence of post-traumatic stress disorder among survivors after earthquakes: A systematic review and meta-analysis. BMC Psychiatry, 16(1), 188. https://doi.org/10.1186/s12888-016-0891-9
- Ehlers, A., Mayou, R. A., & Bryant, B. (2003). Cognitive predictors of posttraumatic stress disorder in children: Results of a prospective longitudinal study. Behaviour Research and Therapy, 41(1), 1–10. https://doi.org/10.1016/S0005-7967(01)00126-7
- Ekşi, A., Braun, K. L., Ertem-Vehid, H., Peykerli, G., Saydam, R., Toparlak, D., & Alyanak, B. (2007). Risk factors for the development of PTSD and depression among child and adolescent victims following a 7.4 magnitude earthquake. International Journal of Psychiatry in Clinical Practice, 11(3), 190–199. https://doi.org/10.1080/13651500601017548
- Fan, F., Long, K., Zhou, Y., Zheng, Y., & Liu, X. (2015). Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychological Medicine, 45(13), 2885–2896. https://doi.org/10.1017/S0033291715000884
- Farooqui, M., Quadri, S. A., Suriya, S. S., Khan, M. A., Ovais, M., Sohail, Z., Shoaib, S., Tohid, H., & Hassan, M. (2017). Posttraumatic stress disorder: A serious post-earthquake complication. Trends in Psychiatry and Psychotherapy, 39(2), 135–143. https://doi.org/10.1590/2237-6089-2016-0029
- Georgescu, T., & Nedelcea, C. (2023). Pretrauma risk factors and posttraumatic stress disorder symptoms following subsequent exposure: Multilevel and univariate meta-analytical approaches. Clinical Psychology & Psychotherapy 31 (1). Advance online publication. https://doi.org/10.1002/cpp.2912.
- Gökçen, C., Sahingöz, M., & Annagür, B. B. (2013). Does a non-destructive earthquake cause posttraumatic stress disorder? A cross-sectional study. European Child & Adolescent Psychiatry, 22(5), 295–299. https://doi.org/10.1007/s00787-012-0348-8
- Gordon-Hollingsworth, A. T., Yao, N., Chen, H., Qian, M., & Chen, S. (2015). Understanding the impact of natural disasters on psychological outcomes in youth from Mainland China: A meta-analysis of risk and protective factors for post-traumatic stress disorder symptoms. Journal of Child & Adolescent Trauma, 11(2), 205–226. https://doi.org/10.1007/s40653-015-0051-2
- Guo, J., He, H., Qu, Z., Wang, X., & Liu, C. (2017). Post-traumatic stress disorder and depression among adult survivors 8 years after the 2008 Wenchuan earthquake in China. Journal of Affective Disorders, 210, 27–34. https://doi.org/10.1016/j.jad.2016.12.009
- Guo, J., Wang, X., Yuan, J., Zhang, W., Tian, D., & Qu, Z. (2015). The symptoms of posttraumatic stress disorder and depression among adult earthquake survivors in China. Journal of Nervous & Mental Disease, 203(6), 469–472. https://doi.org/10.1097/NMD.0000000000000310
- Hong, C., & Efferth, T. (2016). Systematic review on post-traumatic stress disorder among survivors of the Wenchuan earthquake. Trauma, Violence, & Abuse, 17(5), 542–561. https://doi.org/10.1177/1524838015585313
- Jin, Y., & Wang, G. (2014). Individual risk factors for PTSD in adolescents from the 2010 earthquake in Yushu: The predictor effect of rumination. Journal of Psychiatry, 17. https://doi.org/10.4172/2378-5756.1000144
- KalantarMotamedi, M. H., Sagafinia, M., Ebrahimi, A., Shams, E., & KalantarMotamedi, M. (2012). Major earthquakes of the past decade (2000-2010): a comparative review of various aspects of management. Trauma Monthly, 17(1), 219–229. https://doi.org/10.5812/traumamon.4519
- Kitchenham, B., Madeyski, L., & Budgen, D. (2022). SEGRESS: Software engineering guidelines for reporting secondary studies. IEEE Transactions on Software Engineering, 49(3), 1273–1298. https://doi.org/10.1109/TSE.2022.3174092
- Korol, M., Green, B. L., & Gleser, G. C. (1999). Children’s responses to a nuclear waste disaster: PTSD symptoms and outcome prediction. Journal of the American Academy of Child & Adolescent Psychiatry, 38(4), 368–375. https://doi.org/10.1097/00004583-199904000-00008
- Kun, P., Tong, X., Liu, Y., Pei, X., & Luo, H. (2013). What are the determinants of post-traumatic stress disorder: Age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health, 127(7), 644–652. https://doi.org/10.1016/j.puhe.2013.04.018
- Kušević, Z., Krstanović, K., & Kroflin, K. (2021). Some psychological, gastrointestinal and cardiovascular consequences of earthquakes. PsychiatriaDanubina, u tisku.
- La Greca, A. M., & Prinstein, M. J. (2002). Hurricanes and earthquakes. In A. M. La Greca, W. K. Silverman, E. M. Vernberg, & M. C. Roberts (Eds.), Helping children cope with disasters and terrorism (pp. 107–138). American Psychological Association. https://doi.org/10.1037/10454-005
- Lee, S., & First, J. M. (2022). Mental health impacts of tornadoes: A systematic review. International Journal of Environmental Research and Public Health, 19(21), 13747. https://doi.org/10.3390/ijerph192113747
- Liang, Y., Cheng, J., Ruzek, J. I., & Liu, Z. (2019). Posttraumatic stress disorder following the 2008 Wenchuan earthquake: A 10-year systematic review among highly exposed populations in China. Journal of Affective Disorders, 243, 327–339. https://doi.org/10.1016/j.jad.2018.09.047
- Liu, W. M., Fan, F., Zheng, Y. H., & Cui, M. M. (2010). Postramatic stress symptoms and related factors among adolescents in Dujiangyan district 6 months after the earthquake. Chinese Mental Health Journal, 24(9), 647–651.
- Lowe, S. R., Blachman-Forshay, J., & Koenen, K. C. (2015). Trauma as a public health issue: Epidemiology of trauma and trauma-related disorders. In U. Schnyder & M. Cloitre (Eds.), Evidence based treatments for trauma-related psychological disorders: A practical guide for clinicians (pp. 11–40). Springer International Publishing/Springer Nature. https://doi.org/10.1007/978-3-319-07109-1_2
- Ma, X., Liu, X., Hu, X., Qiu, C., Wang, Y., Huang, Y., Wang, Q., Zhang, W., & Li, T. (2011). Risk indicators for post-traumatic stress disorder in adolescents exposed to the 5.12 Wenchuan earthquake in China. Psychiatry Research, 189(3), 385–391. https://doi.org/10.1016/j.psychres.2010.12.016
- Massazza, A., Brewin, C. R., & Joffe, H. (2021). Feelings, thoughts, and behaviors during disaster. Qualitative Health Research, 31(2), 323–337. https://doi.org/10.1177/1049732320968791
- Mesidor, J. K., & Sly, K. F. (2019). Religious coping, general coping strategies, perceived social support, PTSD symptoms, resilience, and posttraumatic growth among survivors of the 2010 earthquake in Haiti. Mental Health, Religion & Culture, 22(2), 130–143. https://doi.org/10.1080/13674676.2019.1580254
- Naeem, F., Ayub, M., Masood, K., Gul, H., Khalid, M., Farrukh, A., Shaheen, A., Waheed, W., & Chaudhry, H. R. (2011). Prevalence and psychosocial risk factors of PTSD: 18months after Kashmir earthquake in Pakistan. Journal of Affective Disorders, 130(1-2), 268–274. https://doi.org/10.1016/j.jad.2010.10.035
- Ozturk, E., Akis, A. D., Derin, G., & Erdogan, B. (2023). Social trauma and disaster psychology: The impact of earthquakes on children’s mental health from the perspective of dissoanalysis theory and modern psychotraumatology. Novel Forensic Research, 2(3), 57–70. https://doi.org/10.5455/NOFOR.2023.07.010
- Page, M. J., Moher, D., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hrobjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … McKenzie, J. E. (2021). PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. bmj, 372, n160. https://doi.org/10.1136/bmj.n160
- Priebe, S., Grappasonni, I., Mari, M., Dewey, M., Petrelli, F., & Costa, A. (2009). Posttraumatic stress disorder six months after an earthquake: Findings from a community sample in a rural region in Italy. Social Psychiatry and Psychiatric Epidemiology, 44(5), 393–397. https://doi.org/10.1007/s00127-008-0441-y
- Pyari, T. T., Kutty, R. V., & Sarma, P. S. (2012). Risk factors of post-traumatic stress disorder in tsunami survivors of Kanyakumari District, Tamil Nadu, India. Indian Journal of Psychiatry, 54(1), 48–53. https://doi.org/10.4103/0019-5545.94645
- Sayed, S., Iacoviello, B. M., & Charney, D. S. (2015). Risk factors for the development of psychopathology following trauma. Current Psychiatry Reports, 17(8), 612. https://doi.org/10.1007/s11920-015-0612-y
- Shabani, A., Rasoulian, M., Naserbakht, M., Hakim Shooshtari, M., Hajebi, A., Tiyuri, A., & Motevalian, S. A. (2024). Prevalence and determinants of post-traumatic stress disorder five months after the 2019 huge flooding in Iran. BMC Public Health, 24(1), 346. https://doi.org/10.1186/s12889-024-17861-y
- Solomon, Z. (1993). Combat stress reaction: The enduring toll of war. Plenum Press.
- Solomon, Z., Mikulincer, M., Ohry, A., & Ginzburg, K. (2021). Prior trauma, PTSD long-term trajectories, and risk for PTSD during the COVID-19 pandemic: A 29-year longitudinal study. Journal of Psychiatric Research, 141, 140–145. https://doi.org/10.1016/j.jpsychires.2021.06.031
- Tang, B., Deng, Q., Glik, D., Dong, J., & Zhang, L. (2017). A meta-analysis of risk factors for post-traumatic stress disorder (PTSD) in adults and children after earthquakes. International Journal of Environmental Research and Public Health, 14(12), 1537. https://doi.org/10.3390/ijerph14121537
- Thomas, É, Saumier, D., & Brunet, A. (2012). Peritraumatic distress and the course of posttraumatic stress disorder symptoms: A meta-analysis. The Canadian Journal of Psychiatry, 57(2), 122–129. https://doi.org/10.1177/070674371205700209
- Tortella-Feliu, M., Fullana, M. A., Pérez-Vigil, A., Torres, X., Chamorro, J., Littarelli, S. A., Solanes, A., Ramella-Cravaro, V., Vilar, A., González-Parra, J. A., Andero, R., Reichenberg, A., Mataix-Cols, D., Vieta, E., Fusar-Poli, P., Ioannidis, J. P. A., Stein, M. B., Radua, J., & Fernández de la Cruz, L. (2019). Risk factors for posttraumatic stress disorder: An umbrella review of systematic reviews and meta-analyses. Neuroscience & Biobehavioral Reviews, 107, 154–165. https://doi.org/10.1016/j.neubiorev.2019.09.013
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. https://doi.org/10.1016/j.cpr.2011.12.001
- Vahidniya, N., Javadzadeh, H. R., & Mahmoodi, S. (2023). Trauma characteristics and risk factors of posttraumatic stress disorder in children and adolescents. Trauma Monthly, 28(4), 882–889.
- Wafa, M. H., Viprey, M., Magaud, L., Haesebaert, J., Leaune, E., Poulet, E., Bied, C., & Schott, A. M. (2019). Identification of biopSychoSocial factors predictive of post-traUmatic stress disorder in patients admitted to the Emergency department after a trauma (ISSUE): protocol for a multicenter prospective study. BMC Psychiatry, 19(1), 163. https://doi.org/10.1186/s12888-019-2154-z
- Wang, B., Ni, C., Chen, J., Liu, X., Wang, A., Shao, Z., Xiao, D., Cheng, H., Jiang, J., & Yan, Y. (2011). Posttraumatic stress disorder 1 month after 2008 earthquake in China: Wenchuan earthquake survey. Psychiatry Research, 187(3), 392–396. https://doi.org/10.1016/j.psychres.2009.07.001
- World Health Organization. (2018). ICD-11 for mortality and morbidity statistics.
- Yaghmaei, N. (Eds.). (2020). Human cost of disasters: An overview of the last 20 years, 2000-2019. UN Office for Disaster Risk Reduction.
- Ying, L. H., Wu, X. C., Lin, C. D., & Chen, C. (2013). Prevalence and predictors of posttraumatic stress disorder and depressive symptoms among child survivors 1 year following the wenchuan earthquake in China. European Child & Adolescent Psychiatry, 22(9), 567–575. https://doi.org/10.1007/s00787-013-0400-3
- Zhang, W., Jiang, X., Ho, K. W., & Wu, D. (2011). The presence of post-traumatic stress disorder symptoms in adolescents three months after an 8·0 magnitude earthquake in Southwest China. Journal of Clinical Nursing, 20(21-22), 3057–3069. https://doi.org/10.1111/j.1365-2702.2011.03825.x
- Zhang, Z., Ran, M. S., Li, Y. H., Ou, G. J., Gong, R. R., Li, R. H., Fan, M., Jiang, Z., & Fang, D. Z. (2012). Prevalence of post-traumatic stress disorder among adolescents after the Wenchuan earthquake in China. Psychological Medicine, 42(8), 1687–1693. https://doi.org/10.1017/S0033291711002844
- Zhou, X., Kang, L., Sun, X., Song, H., Mao, W., Huang, X., Zhang, Y., & Li, J. (2013). Prevalence and risk factors of post-traumatic stress disorder among adult survivors six months after the Wenchuan earthquake. Comprehensive Psychiatry, 54(5), 493–499. https://doi.org/10.1016/j.comppsych.2012.12.010