ABSTRACT
Background: When traumatic events and losses intersect in the form of traumatic loss, these events can trigger both posttraumatic stress disorder and pathological grief.
Objective: This systematic review investigates which characteristics differentiate between the development of the respective disorders or are associated with comorbidity.
Method: A systematic literature search using Medline, PubMed, APA PsycInfo and Web of Science yielded 46 studies which met the inclusion criteria. In these studies, PTSD was assessed using 17 and pathological grief using 16 different validated instruments. In the quality assessment, 12 studies were classified as average, 30 as above average, and 4 as excellent. The investigated risk factors were categorized into 19 superordinate clusters and processed using narrative synthesis.
Results: The relationship to the deceased, mental health issues, and religious beliefs seem to be associated specifically with pathological grief symptoms compared to PTSD symptoms. Social support and social emotions emerged as significant correlates and potential risk factors for both PTSD and pathological grief. Included studies had mainly cross-sectional designs.
Conclusions: Differentiating factors between pathological grief and PTSD appear to exist. The results should be considered within the limitations of the heterogeneity of the included studies and the research field. There is a lack of studies (1) using a longitudinal study design, (2) starting data collection early following the traumatic loss, (3) using standardized, up-to-date measurement instruments and (4) including comorbidity in their analyses. Further research is urgently needed for more accurate (acute) screenings, prognoses, and interventions following traumatic loss.
HIGHLIGHTS
When traumatic events and losses intersect in the form of traumatic loss, these events can trigger both posttraumatic stress disorder and pathological grief. This systematic review investigates which characteristics can differentiate between the development of the respective disorders or are associated with comorbidity.
The relationship to the deceased, mental health issues, and religious beliefs seem to be specific characteristics for predicting pathological grief. Social support and social emotions were frequently reported as significant correlates of both PTSD and pathological grief.
The studies to date have been very heterogeneous and mainly cross-sectional. Further research considering both disorders after traumatic loss in longitudinal study designs is urgently indicated for better (acute) screenings, prognoses, and interventions.
Antecedentes: Cuando los eventos traumáticos y las pérdidas se cruzan en forma de pérdida traumática, estos eventos pueden desencadenar tanto un trastorno de estrés postraumático (TEPT) como duelo patológico.
Objetivo: Esta revisión sistemática investiga qué características diferencian entre el desarrollo de los respectivos trastornos o están asociadas con la comorbilidad.
Método: Una búsqueda sistemática de literatura utilizando Medline, PubMed, APA PsycInfo y Web of Science arrojó 46 estudios que cumplían con los criterios de inclusión. En estos estudios, el TEPT se evaluó utilizando 17 instrumentos validados y el duelo patológico utilizando 16 instrumentos diferentes validados. En la evaluación de calidad, 12 estudios fueron clasificados como promedio, 30 como superiores al promedio y 4 como excelentes. Los factores de riesgo investigados fueron categorizados en 19 grupos superordinados y se procesaron mediante síntesis narrativa.
Resultados: La relación con el fallecido, los problemas de salud mental y las creencias religiosas parecen estar específicamente asociados con síntomas de duelo patológico en comparación con los síntomas de TEPT. El apoyo social y las emociones sociales surgieron como correlatos significativos y posibles factores de riesgo tanto para el TEPT como para el duelo patológico. Los estudios incluidos tenían principalmente diseños transversales.
Conclusiones: Parecen existir factores diferenciadores entre el duelo patológico y el TEPT. Los resultados deben considerarse dentro de las limitaciones de la heterogeneidad de los estudios incluidos y del campo de investigación. Hay una falta de estudios que (1) utilicen un diseño de estudio longitudinal, (2) comiencen la recopilación de datos temprano después de la pérdida traumática, (3) usen instrumentos de medición estandarizados y actualizados y (4) que incluyan la comorbilidad en sus análisis. Se necesita urgentemente más investigación para evaluaciones (agudas) más precisas, pronósticos e intervenciones después de una pérdida traumática.
1. Introduction
When Horowitz (Citation1974) wrote his famous publication ‘Stress Response Syndromes’ and thus shaped today’s criteria for posttraumatic stress disorder (PTSD), he had already listed a connection to an intense grief reaction. After decades in which this phenomenon was primarily handled as ‘Complicated Grief’ (CG) in science, grief has now also been included as a mental disorder in the DSM-5 (American Psychiatric Association, Citation2013) as well as in the recently published ICD-11 (World Health Organization, Citation2019). In diagnostic systems, pathological grief is now listed under the names ‘Prolonged Grief Disorder’ (PGD) and ‘Persistent Complex Bereavement Disorder’ (PCBD).
The overlap of trauma and grief becomes evident when considering the initiating event criteria, which share the same characteristics. Boelen et al. (Citation2019) defined such events as traumatic losses in the following manner: ‘Traumatic loss refers to the loss of loved ones in the context of potentially traumatizing circumstances. Examples are losses due to homicide, suicide, accidents, and natural disasters, and losses resulting from war and terror’ (Boelen et al., Citation2019, p. 2). Studies investigating the longitudinal association between PTSD symptoms and complicated grief following traumatic loss have found that the development of both disorders is also closely linked and interacting over time (e.g., Glad et al., Citation2022). Given these overlaps, it is crucial to determine which specific characteristics are associated with the development of the respective disorder, especially with regard to support services following such dramatic circumstances of death.
In this regard, risk factors of PTSD are often divided into pre-, peri- and post-traumatic variables. Of the factors present prior to the trauma event, female gender, low socioeconomic status, previous trauma exposure, and increased psychopathology in the family were found to be most relevant in predicting PTSD (Brewin et al., Citation2000; Carmassi et al., Citation2021; Christiansen & Elklit, Citation2008; Kessler et al., Citation2014; Martin-Soelch & Schnyder, Citation2019; Ozer et al., Citation2003; Tortella-Feliu et al., Citation2019). The type of trauma, the number or accumulation of traumatic experiences, the occurrence of dissociation and the perceived threat to life were identified as peritraumatic characteristics predicting PTSD (Martin-Soelch & Schnyder, Citation2019; Ozer et al., Citation2003; Tortella-Feliu et al., Citation2019; Trickey et al., Citation2012). Importantly, posttraumatic characteristics, most notably social support, generally showed the largest effect sizes compared to the other factors predicting PTSD (Brewin et al., Citation2000; Carmassi et al., Citation2021; Hibberd et al., Citation2010; Kessler et al., Citation2014; Martin-Soelch & Schnyder, Citation2019; Ozer et al., Citation2003; Trickey et al., Citation2012).
In contrast to PTSD, which became a focus of psychological research almost 50 years ago following its inclusion in classification systems, grief research has only recently progressed to this point. Accordingly, reviews and meta-analyses about pathological grief are currently rarer and less comprehensive. However, an overall view of existing studies reveals a pattern that closely resembles PTSD predictors. Among demographic characteristics, young age, female gender, and low socioeconomic status were identified (Neimeyer & Burke, Citation2013). Overlaps also emerged with respect to circumstances of death with violent and sudden deaths being particularly associated with significant grief intensity (Barry et al., Citation2002; Hebert et al., Citation2006; Hibberd et al., Citation2010; Neimeyer & Burke, Citation2013). In addition, grief severity is often associated with the closeness of kinship (e.g., Cleiren et al., Citation1994; Mitchell et al., Citation2004; Neimeyer & Burke, Citation2013) and the emotional attachment to the deceased (Neimeyer & Burke, Citation2013; Sekowski & Prigerson, Citation2022). Parents who lost their child (e.g., Wijngaards-de Meij et al., Citation2008; Zetumer et al., Citation2015) and children who lost their parents (e.g., McKay et al., Citation2021) were identified as groups, particularly, at risk in previous research. Post-event social support has also been identified by many studies as a crucial influencing factor in grief (Burke et al., Citation2010; Hibberd et al., Citation2010; King et al., Citation2006; Reed, Citation1998; Stroebe & Schut, Citation2001; Vanderwerker & Prigerson, Citation2004).
As previous study reviews have nearly exclusively highlighted either trauma or grief in different circumstances, the question remains as to what happens when experiences of loss are not solely traumatic or grief-related losses but coincide in the form of a traumatic loss. For this purpose, this review examined studies that (a) correspond to the operationalization of a traumatic loss according to Boelen et al. (Citation2019), (b) have considered both PTSD and PGD/PCBD/CG in the same population and (c) investigate which factors are associated with the pathogenesis of PTSD only, of PGD/PCBD/CG only, or with comorbidity of both disorders. To the best of our knowledge, this is the first comprehensive systematic review investigating both disorders simultaneously in the context of traumatic loss. The aim of this systematic review is to demonstrate the current state of the research field regarding risk factors and to identify remaining research gaps. Results are particularly useful for future research projects and institutions working with relevant target groups such as psychosocial crisis intervention teams, relief organizations in disaster situations or war zones, as well as clinical psychologists operating in acute settings. Certainty in differentiating between trauma and grief after traumatic loss enables better (acute) screening procedures and early specific prevention or intervention options for PTSD or PGD/PCBD/CG.
2. Methods
This review followed the criteria of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA; Moher et al., Citation2009). The protocol was preregistered in February 2023 in PROSPERO (registration number: CRD42023400667).
2.1. Study inclusion
A study was included if it examined (a) correlates of PGD/PCBD/CG and PTSD using (b) standardized measurement instruments (c) in the aftermath of traumatic loss, within an (d) adult sample (≥18 years). Only English-language literature published (f) in a peer-reviewed journal was considered.
Studies that considered mixed groups of initiating events (e.g., having experienced death vs. disappearance of a loved one) were included in the systematic review only if separate data was available for the respective groups, allowing separate consideration of outcomes relevant to the research question. The search was not limited with regard to the publication date.
Publications were excluded if they investigated (a) prenatal, perinatal, or (b) predictable, natural, as well as disease-related losses, (c) did not report the type of circumstance of death, or (d) looked at nonhuman losses (e.g., loss of a pet/job).
2.2. Literature search strategy
A systematic literature search of the electronic databases Medline, PubMed, Web of Science, and APA PsycInfo was conducted in February 2023. The search was repeated in June 2023 to search for additional studies published in the interim. The following search terms were used: traumatic loss OR suicide OR homicide OR accident OR natural disaster OR death AND PTSD OR post traumatic stress disorder OR posttraumatic stress OR traumatic stress AND grief OR bereavement OR mourning OR PGD OR prolonged grief disorder OR PCBD OR persistent complex bereavement disorder OR CG OR complicated grief OR pathological grief OR traumatic grief OR traumatic bereavement AND predict* OR correlate* OR latent class analysis OR LCA OR regression.
To organize the literature, titles and abstracts of all studies were imported into the literature management program Zotero.
2.3. Study selection and data extraction
First, the titles and abstracts of all studies were independently reviewed by the first two authors for potential eligibility. Subsequently, a full-text screening of the remaining studies was conducted, taking into account the inclusion and exclusion criteria. In case of disagreement about the eligibility of a study, the final decision was made either using a discussion between the first two authors or an evaluation by the third author. The information contained in the publications was extracted using a summary table recording the following aspects: Characteristics of the study (title, authors, year, country of survey), sample (sample size, age, gender), loss-related characteristics (cause of death, time elapsed since loss, relationship with the deceased), measurement instruments (including indication of internal consistency), and prevalences and risk factors for PTSD, PGD/PCBD/CG, and comorbidity.
2.4. Quality assessment
The quality assessment of the reviewed studies was based on a valid tool of the international research organization JBI (Moola et al., Citation2020). Since the inclusion criteria of the studies were narrowly defined, we added the following specific questions for enhanced quality differentiation: ‘Is the sample size adequate?’, ‘Were strategies stated to deal with confounding factors? Specifically covariates?’, ‘Were findings adequately generalized considering sample characteristics?’, ‘Was the study design longitudinal or cross-sectional?’.
Scaling ranged from 0 to 8 points, with 0–1 being classified as ‘poor’, 2–3 as ‘below average’, 4–5 as ‘average’, 6–7 as ‘above average’, and 8 as ‘excellent’. The first and third authors of the study rated the studies independently. Disagreements were discussed among all authors to reach consensus.
3. Results
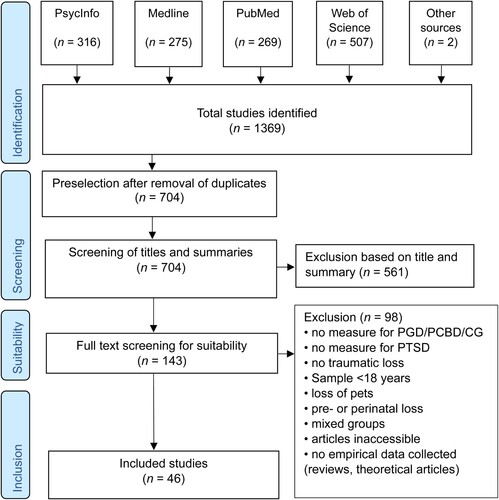
The systematic literature search identified 316 articles in PsycInfo, 275 articles in Medline, 269 articles in PubMed, and 507 articles in Web of Science. Furthermore, two potentially significant publications were added following a manual search. In total, the literature search thus yielded 1369 findings. After duplicates were removed, the titles and abstracts of the remaining 704 articles were reviewed for eligibility, taking into account the inclusion and exclusion criteria. In this process, 561 articles were excluded. The full texts of the remaining 143 potentially eligible studies were reviewed. Finally, 46 studies were identified that met the inclusion criteria for the systematic review. The detailed selection process is shown in .
Figure 1. Selection process flow chart, following the PRISMA guidelines (Moher et al., Citation2009).
3.1. Study characteristics
The considered studies were published in the period from 1998 to 2022. Of the 46 studies included in the review, 40 used a cross-sectional study design, while 6 studies had a longitudinal design. In conducting the literature search, publications from the USA (n = 17), the Netherlands (n = 5), Germany (n = 4), Norway (n = 4), and Cambodia (n = 3) were identified most frequently. It should be noted that these are the survey locations of the studies, which do not always correspond to the countries of origin of the sample. All data extracted from the studies, including study characteristics, sample information, loss-related characteristics, measurement tools used, prevalences and risk factors, are listed in .
Table 1 Maintable.
Sample sizes varied from 32 to 1736 participants. With the exception of seven studies (Cerel et al., Citation2015; Comtesse & Rosner, Citation2019; Djelantik et al., Citation2021; Huh et al., Citation2017; Lubens & Silver, Citation2019; Mitchell & Terhorst, Citation2017; Yehene et al., Citation2022), the majority of participants were female. The average age had a range of 21–62.88 years.
Considering the quality assessment (), 12 studies received an average rating, while 30 studies were rated as above average and four studies as excellent.
Table 2. Quality assessment.
3.2. Loss-related characteristics
The most common cause of death examined in the included studies was war and terror (n = 14), followed by homicide (n = 12), accidents (n = 8), suicide (n = 6) and natural disasters (n = 3). Only three studies (Dyregrov et al., Citation2003; Feigelman & Cerel, Citation2020; Lubens & Silver, Citation2019) examined the consequences of different causes of death.
The average elapsed time since loss ranged from 0.25 to 30 years. In nine studies, data collection was conducted on average within the first year following the loss. The majority of studies (n = 19) collected data within the first five years. In four studies, the loss occurred on average 5–10 years ago, while in 10 studies more than 10 years had passed since the loss. In four studies, the time of loss was not recorded.
Regarding the relationship with the deceased, most studies examined family connections (n = 41), partnership relationships (n = 32) and friendships (n = 17). In individual cases, colleagues (n = 6), acquaintances (n = 3), neighbours (n = 2), flatmates (n = 2), professors (n = 2), teachers (n = 1), strangers (n = 1), commanders (n = 1), military comrades (n = 2), and community members (n = 1) were also considered. Some studies (n = 8) grouped these types of relationships into the category ‘others’.
3.3. Measurement instruments
Grief symptomatology was explored using 16 different validated measures. The Inventory of Complicated Grief (ICG; Prigerson et al., Citation1995) was the most commonly used measure of pathological grief. Including revised (ICG-R; Prigerson & Jacobs, Citation2001) and German-language (ICG-D; Lumbeck et al., Citation2012) versions, it was used in more than half of the studies (n = 23). Furthermore, the Prolonged Grief Scale (PG-13; Prigerson et al., Citation2009) was used in six studies, the Traumatic Grief Inventory Self-Report Version (TGI-SR; Boelen & Smid, Citation2017) in five studies and the Texas Revised Inventory of Grief (TRIG; Faschingbauer et al., Citation1987) in four studies. All other instruments were used in one study each. See Supplementary Files for references of all the measures.
PTSD symptomatology was assessed using 17 different instruments. Different versions of the Posttraumatic Stress Disorder Checklist (PCL; Weathers et al., Citation1993), based on the diagnostic criteria of the DSM-IV, were used in 12 studies. The immediate successor based on the DSM-5, the Posttraumatic Stress Disorder Checklist-5 (PCL-5; Weathers et al., Citation2013), was used in 10 studies. Different versions of the Impact of Events Scale (IES; Horowitz et al., Citation1979; IES-R; Weiss & Marmar, Citation1997; IES-15; Horowitz et al., Citation1979) were used in 11 studies.
3.4. Prevalences
From the total of 46 included studies, 28 studies reported prevalences for PTSD, 27 studies reported prevalences for PGD/PCBD/CG and four studies reported prevalences for a comorbidity of both disorders. Prevalence rates varied considerably: PTSD between 1% and 95%, PGD/PCBD/CG between 0% and 94%, and comorbidity of both disorders between 1% and 53%.
3.5. Potential risk factors
Due to the heterogeneity of the potential risk factors assessed in the included studies, they were grouped into the following categories: age, gender, education, socioeconomic status, relationship to the deceased, time elapsed since loss, number and history of traumatic events, type of exposure, ongoing confrontation with loss, peritraumatic reactions, social emotions, adjustment difficulties, mental health problems, social support, religious beliefs, and other risk factors. The individual variables of the respective studies, which were summarized in the superordinate clusters, can be found in the Supplementary Files. The number of significant risk factors within the categories above, taking into account the number of studies examining them, are shown in . A potential risk factor was considered important if it was significant in the majority of studies analysing it (>50%). Correlates with a significance rate between 40% and 50% were also taken into consideration as correlates of limited relevance. Due to the greater informative value of longitudinal studies with regard to possible risk factors, shows the analysis for longitudinal results separately.
Figure 2. Analysed and significant predictors within the included studies.
Note. Fields with a grey background mean that this predictor was investigated in the study but was not significant. Fields with a coloured dot mean that the predictor was significant for the respective disorder. The percentages were rounded to whole numbers and refer to the proportion of studies in which a correlate was significant among the total number of studies that analysed this correlate.
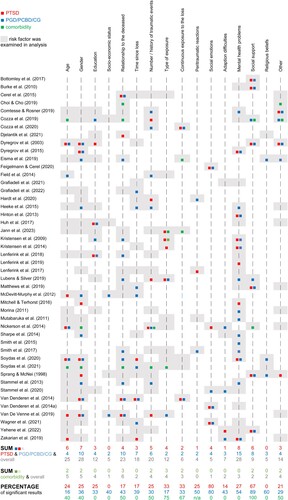
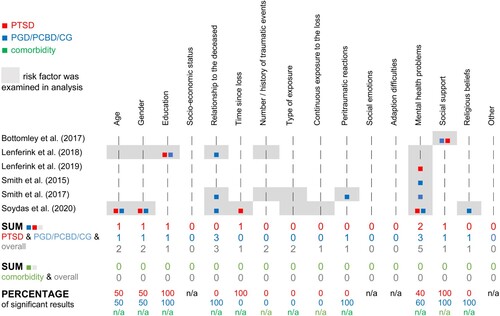
Figure 3. Analysed and significant predictors within the included longitudinal studies.
Note. Fields with a grey background mean that this predictor was investigated in the study but was not significant. Fields with a coloured dot mean that the predictor was significant for the respective disorder. The percentages were rounded to whole numbers and refer to the proportion of studies in which a predictor was significant among the total number of studies that analysed this predictor.
Reviewing the overall results, social emotions were a frequent correlate of PTSD and PGD/PCBD/CG (80%). Both disorders were also often associated with aspects of social support (67% for PTSD and 89% for PGD/PCBD/CG). Regarding PGD/PCBD/CG, religious beliefs (60%) and mental health problems (54%) turned out to be a frequently significant correlate. Other correlates that reached a borderline significance rate in relation to grief were peritraumatic reactions (50%), relationship to the deceased (43%) and adaptation difficulties (43%).
Regarding the longitudinal results only, both disorders were linked to aspects of social support (namely need for and satisfaction with physical assistance; 100%, only one study). PTSD was correlated with time since loss (100%; only one study). PGD/PCBD/CG was consistently associated with relationship to the deceased (100%; three studies), religious beliefs (100%; only one study) and with aspects of mental health in more than half of the corresponding studies (60%). Correlates reaching a borderline significance rate were age and gender for both disorders (50%) as well as mental health problems for PTSD (40%).
Regarding the comorbidity of PTSD and PGD/PCBD/CG, it should be noted that the comorbidity of both disorders was only investigated in eight of the included studies and therefore each of the potential risk factors was only analysed by a few studies. In the two studies that investigated aspects of social support, it turned out that they were a significant correlate of comorbidity (100%). Other frequent correlates were the type of exposure (75%) and continuous exposure (67%). Correlates reaching a borderline significance rate were the relationship to the deceased (50%), the number/history of events (50%), age (40%) and gender (40%).
4. Discussion
This systematic review examined the current state of research on risk factors for PTSD, PGD/PCBD/CG or a comorbidity of both disorders in the context of traumatic loss when both trauma and grief symptomatology are examined within the same sample. A key finding is that research into risk factors is currently at a very early stage. The majority of studies to date used cross-sectional designs, therefore investigating correlates associated with PTSD or grief at the time of survey rather than pathological trajectories in response to risk factors. None of the assessed clusters of potential risk factors were consistently identified as a correlate for the respective disorders across all studies investigating them. This inconsistency in the results is not unexpected given the heterogeneity of the included studies regarding sample characteristics, prevalences and measurement instruments. Nevertheless, some aspects can be identified that have been associated with psychopathological trajectories of PTSD and/or PGD/PCBD/CG by the majority of studies. These aspects will be discussed in the following, keeping in mind that they must be interpreted with caution.
It becomes evident that aspects of social support are related to both disorders, although only examined longitudinally in one study. These findings are in line with previous research revealing low social support as one of the most important predictors of both PTSD (Brewin et al., Citation2000; Ozer et al., Citation2003) and PGD/PCBD/CG (Burke & Neimeyer, Citation2013). However, the reviewed results refer to various operationalizations of social support (e.g., need for support, satisfaction of support, size of support network, …) and results regarding these individual aspects are partly heterogeneous. Research needs to be substantially expanded to allow a more differentiated evaluation of the role of social support. While most of the reviewed studies refer to support by the direct social environment like family members, friends, or neighbours (e.g. Burke et al., Citation2010; Yehene et al., Citation2022), Matthews et al. (Citation2019) also point out the relevance of institutional social support by authorities or support services. They state that timely and adequate communication of information or support with processes and procedures after death can be helpful forms of social support provided by such services. Research should be expanded in this regard to provide support organizations and institutions with informed guidelines on how to offer the best possible social support after a traumatic loss, as they may be particularly needed if the support provided by the individual’s private social support system is not sufficient.
Social emotions like guilt and revengefulness are also quite consistently linked to both PTSD and PGD/PCBD/CG. Given that all studies examining these emotions following traumatic loss were cross-sectional, longitudinal research is urgently needed to determine, whether they are in fact a risk factor predicting psychopathology. In that case, feelings of guilt and revengefulness may be a useful indicator for screening procedures in acute situations to identify people in need of additional support and interventions for PTSD and PGD/PCDB/CG should specifically target these feelings. However, based on the current cross-sectional state of research, feelings of guilt and revengefulness may as well be the consequence of PTSD and PGD/PCBD/CG, with psychopathology making it harder for individuals to adapt to their loss and let go of these feelings.
Regarding PGD/PCBD/CG, religious beliefs seem to be a frequently significant correlate which is in line with previous research reporting a negative association between the importance of religious beliefs or spiritual activities and PGD/PCBD/CG symptomatology (Hawthorne et al., Citation2016; Schaal et al., Citation2010). However, in the reviewed studies higher symptomatology was partially associated with higher religiosity (Eisma et al., Citation2019) and partially with lower religiosity (Sprang & McNeil, Citation1998). These seemingly contradictory results come to light when considering the distinction between negative religious coping (e.g. anger towards God or the faith community, feeling spiritually abandoned, or questioning God’s power) and positive religious coping (e.g. finding consolation in the relationship with God or the faith community, a belief that there is meaning to be found in what happened), which might have different effects on the development of symptoms (Burke et al., Citation2011). Future research should further examine the role of religion and religious coping for different religious groups following traumatic loss.
Another potential risk factor that emerges when considering the longitudinal studies’ results is the relationship to the deceased. All longitudinal studies examining this variable, including the studies rated as excellent in the quality assessment, found an association with PGD/PCBD/CG, but not with PTSD. It therefore appears to be a differentiating factor in the development of both disorders and serves as a specific characteristic for predicting pathological grief. This seems in line with previous studies which have shown an association between PGD/PCBD/CG and the loss of a close relative, particularly one’s own child or partner (e.g., Djelantik et al., Citation2017; Djelantik et al., Citation2020; Heeke et al., Citation2019). However, a similarly frequent connection to PTSD symptoms could have been expected given that the event criterion A in the DSM-IV and V has been broadened to such an extent that learning about the violent death of a close relative can lead to PTSD. There is a body of studies confirming this connection (e.g., Kaltman & Bonanno, Citation2003; Kloep et al., Citation2014). However, these studies did not simultaneously address symptoms of pathological grief. A critical examination of the results of this systematic review raises the question of whether it might be necessary to consider both disorders to adequately assess the predictive importance of the sudden and violent loss of a loved one for the development of PTSD. Otherwise, given the high overlap of symptoms, PGD/PCBD/CG symptoms might be misinterpreted as PTSD symptoms. Further research is required to specifically address this hypothesis and its implications for the event criterion of PTSD.
In view of the longitudinal studies, mental health is also frequently associated with PGD/PCBD/CG. This is in line with previous studies reporting associations of pathological grief symptoms with other psychopathologies such as depression or anxiety (He et al., Citation2014; Schaal et al., Citation2012). Results of longitudinal studies in this review assessing a history of mental health issues prior to a traumatic loss suggest that other mental health issues might not only be of a comorbid nature but also of a predictive nature (Smith et al., Citation2017; Soydas et al., Citation2020).
Regarding the comorbidity of PTSD and PGD/PCBD/CG social support, type of exposure and continuous exposure emerged as potentially relevant correlates. However, very few studies and none of the longitudinal studies included comorbidity in their analyses. Therefore, further research is needed to allow for robust interpretations regarding correlates and potential risk factors of comorbidity.
4.1. Strength and limitations
To the best of our knowledge, this is the first systematic review of the literature investigating potential risk factors for both PTSD and PGD/PCBD/CG in the context of traumatic loss. The theoretical and practical conclusions of the results are based on a research corpus of 46 included studies. Almost three-quarters of these studies were rated as being of above average or excellent quality. The results allow us to draw initial conclusions regarding relevant correlates and possible risk factors of PTSD and PGD/PCBD/CG like social support and social emotions. A great strength of this review is that it provides initial evidence regarding risk factors that differentiate between the development of both disorders, as the relationship to the deceased, religious beliefs and other mental health issues appear to be specifically associated with PGD/PCBD/CG. Additionally, this work impressively shows that the research field is only at the beginning of serious scientific research on the socially and clinically important topic of traumatic loss and associated risk factors.
This conclusion leads to several limitations regarding the included studies. There is considerable variability in terms of the assessed samples, risk factors, applied measurement instruments and reported prevalences. In particular, the heterogeneity of the measurement instruments used to record PTSD and PGD/PCBD/CG may impair the comparability and generalizability of the study results, especially if these instruments do not measure the same construct. For example, the conceptualization of pathological grief has changed considerably in recent years. While the diagnostic criteria for PGD and PCBD show largely similar results in terms of sensitivity, specificity and criterion validity (Boelen et al., Citation2020), the diagnostic criteria for CG deviate considerably from the current diagnostic standards of the DSM-5 and ICD-11 (Maciejewski et al., Citation2016). This heterogeneity and lack of research standards makes it difficult to compare and summarize results and therefore prevents robust, generalizable conclusions. Furthermore, the majority of the included studies were cross-sectional studies, which cannot determine a causal direction of effect. The results discussed before must therefore be cautiously interpreted as initial evidence of potential risk factors that need to be confirmed by further research.
Another limitation is the time of investigation in the reviewed studies. Previous research has pointed out that pathological grief symptoms are highly likely to manifest after a few months and therefore should be addressed at an early stage (Boelen et al., Citation2020; Boelen & Lenferink, Citation2020; Prigerson et al., Citation2009). However, only five of the included studies began within the first year following a traumatic loss and only one conducted the survey approximately within the first month, which reveals a crucial research gap. The question of time is also crucial in terms of symptom progression and interaction. Previous findings clearly suggest that the symptoms of both disorders are related, but it is unclear in which direction. On the one hand, it has been shown that trauma symptoms hinder the processing of a loss (Layne et al., Citation2018; Nakajima et al., Citation2012; Schaal et al., Citation2010) and predict later pathological grief (e.g., Glad et al., Citation2022). On the other hand, grief appears to be a predictive and mediating factor for the development and maintenance of PTSD symptomatology (Djelantik et al., Citation2018; Komischke-Konnerup et al., Citation2023; Lenferink et al., Citation2019; O’Connor et al., Citation2015). In this context, another limiting factor is that only 8 out of the 46 studies accounted for the comorbid development of both disorders.
There are also limitations to be considered regarding the review itself. It was restricted to research published in the English language and in peer-reviewed journals, which on the one hand ensures research quality, but on the other hand, may have led to the exclusion of potentially relevant results. Furthermore, we excluded research regarding prenatal, perinatal, predictable, natural, disease-related and nonhuman losses, although affected individuals may experience these as a form of traumatic loss as well. There are additional hints, that relatives of missing persons experience loss of a traumatic character, with the uncertainty of their whereabouts creating an additional burden (Wayland & Ward, Citation2022). Future research might broaden the inclusion criteria regarding the type of loss to investigate their effect on PTBS and PGD/PCBD/CG symptomatology. In addition, the review includes studies conducted in different cultural contexts, which could not be taken into account in the analysis of the results due to the already very high level of complexity. Furthermore, we did not differentiate between man-made and non-man-made losses. Reviews showed that the prevalence rates are higher following intentional events for both PTSD and PGD (Lobb et al., Citation2010; Santiago et al., Citation2013). In view of the diversity of the recorded risk factors for PTSD and PGD/PCBD/CG, similar risk factors were summarized into broader categories as part of this systematic review to facilitate analyses and interpretation. However, we cannot rule out the possibility that some of these factors, despite their similarity, do not necessarily represent the same construct or facet of a construct.
4.2. Implications for research and practice
This review revealed several research gaps regarding traumatic loss which should be addressed in the future. Overall, there is a lack of studies observing affected individuals immediately following a traumatic loss in order to identify early risk factors for PTSD and PGD/PCBD/CG in the acute phase of intervention. In addition, there are only a limited number of longitudinal studies which repeatedly assess PTSD and PGD/PCBD/CG symptoms to shed light on their development and interplay over time. There is a need for further longitudinal studies which initiate their research immediately after a traumatic loss or even before and examine those affected over a longer period of time. Especially when it comes to the question of which disorder should be treated first, studies that start early and take a longitudinal view are urgently needed. Future projects should also include the comorbidity of PTSD and PGD/PCBD/CG in their analyses given the overlap in symptoms and predictors. In this context, it should be further investigated whether the inclusion of pathological grief symptoms affects results regarding the association between the sudden, violent loss of a loved one and PTSD symptomatology. This may have important implications for the evaluation of event criterion A of the DSM-5, which has been the subject of considerable debate in the past (Friedman, Citation2013). It also remains to be investigated to what extent cultural differences may influence the impact of risk factors.
In order to increase the comparability of future results, both PGD/PCBD/CG and PTSD as well as the risk factors should be assessed using uniform, standardized instruments based on the current diagnostic criteria. The ICG, as the most commonly used instrument for assessing grief is dated and does not correspond to the most recent conceptualizations of Prolonged Grief Disorder in classification systems. Lately, instruments have been developed which correspond to the latest editions of both classification systems (International Prolonged Grief Disorder Scale, IPGDS [Killikelly et al., Citation2020], The Traumatic Grief Inventory-Self Report Plus, TGI-SR+ [Lenferink et al., Citation2022]). Such assessments should be given more consideration in future research projects.
In summary, the following recommendations for future research can be derived from this review: Researchers should focus on (1) longitudinal study designs, (2) starting data collection as early as possible following a traumatic loss, (3) using standardized measuring instruments that meet current criteria of PTSD and PGD, and (4) including comorbidity in their analyses. Instead of assessing various potential risk factors in few studies each as research did to date, future studies should focus on the clusters that emerged as potential risk factors in this review (social support, social emotions, religiosity, relationship to the deceased and mental health) and assess aspects of these clusters in a more systematic way to gain a differentiated and interpretable insight into risk factors following traumatic loss. They may also include aspects that reached borderline significance rates (e.g. peritraumatic reactions and adaptation difficulties) to investigate whether these turn out to be risk factors in high-quality longitudinal studies.
A deeper understanding of the risk factors predicting both psychopathologies will enable the early identification of risk groups and the development of disorder-specific prevention and intervention measures. If the potential risk factors highlighted in this study are confirmed by further research, professionals dealing with people acutely affected by traumatic loss should screen for social support resources, social emotions such as guilt or revenge, a close relationship to the deceased, religious beliefs and other mental health issues to identify individuals in need of further support. Progress in this area of research would enable more efficient and pragmatic approaches to help, particularly for professional occupational groups that frequently deal with traumatic losses (e.g., crisis intervention teams) or for helpers in war/terrorist zones.
4.3. Conclusions
Traumatic losses arguably cause the greatest possible human suffering which can lead to a variety of psychopathologies particularly including PTSD or PGD/PCBD/CG. Researching risk factors in this context therefore is a both societally and clinically important issue. This review shows that social support and social emotions might be risk factors for both PTSD and PGD/PCBD/CG, while the relationship to the deceased, mental health issues, and religious beliefs appear to be associated specifically with pathological grief symptoms and therefore differentiate between the development of both disorders. However, a central conclusion of this review is that research into this issue is still at the very beginning, currently based on a very heterogeneous set of studies as well as a lack of longitudinal research initiating immediately after the occurrence of a traumatic loss event. Therefore, future investigations should address this gap in research using standardized and state-of-the-art measurements to comprehensively explore PGD/PCBD/CG and PTSD symptomatology during the acute phase of loss as well as their development over time in a comparable and generalizable way. In general, extended research in this specific context is needed to identify and specifically care for people in need of long-term help in their darkest hours.
20240602 Supplementary_Clusters_anonymous.docx
Download MS Word (44.7 KB)Acknowledgement
We thank Merle Rehder (M.Sc.) for her valuable assistance, which greatly improved the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data available on request from the authors.
Additional information
Funding
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author.
- Barry, L. C., Kasl, S. V., & Prigerson, H. G. (2002). Psychiatric disorders among bereaved persons: The role of perceived circumstances of death and preparedness for death. The American Journal of Geriatric Psychiatry, 10(4), 447–457. https://doi.org/10.1097/00019442-200207000-00011
- Boelen, P. A., Eisma, M. C., Smid, G. E., & Lenferink, L. I. M. (2020). Prolonged grief disorder in section II of DSM-5: A commentary. European Journal of Psychotraumatology, 11(1), 1771008. https://doi.org/10.1080/20008198.2020.1771008
- Boelen, P. A., & Lenferink, L. I. M. (2020). Symptoms of prolonged grief, posttraumatic stress, and depression in recently bereaved people: Symptom profiles, predictive value, and cognitive behavioural correlates. Social Psychiatry and Psychiatric Epidemiology, 55(6), 765–777. https://doi.org/10.1007/s00127-019-01776-w
- Boelen, P. A., Olff, M., & Smid, G. E. (2019). Traumatic loss: Mental health consequences and implications for treatment and prevention. European Journal of Psychotraumatology, 10(1), 1591331. https://doi.org/10.1080/20008198.2019.1591331
- Boelen, P. A., & Smid, G. E. (2017). The traumatic grief inventory self-report version (TGI-SR): Introduction and preliminary psychometric evaluation. Journal of Loss and Trauma, 22(3), 196–212. https://doi.org/10.1080/15325024.2017.1284488
- Bottomley, J. S., Burke, L. A., & Neimeyer, R. A. (2017). Domains of social support that predict bereavement distress following homicide loss: Assessing need and satisfaction. OMEGA – Journal of Death and Dying, 75(1), 3–25. https://doi.org/10.1177/0030222815612282
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. https://doi.org/10.1037/0022-006X.68.5.748
- Burke, L. A., & Neimeyer, R. A. (2013). Prospective risk factors for complicated grief: A review of the empirical literature. In M. Stroebe, H. Schut, & J. van den Bout (Eds.), Complicated grief: Scientific foundations for health care professionals (pp. 145–161). Routledge/Taylor & Francis Group.
- Burke, L. A., Neimeyer, R. A., & McDevitt-Murphy, M. E. (2010). African American homicide bereavement: Aspects of social support that predict complicated grief, PTSD, and depression. OMEGA – Journal of Death and Dying, 61(1), 1–24. https://doi.org/10.2190/OM.61.1.a
- Burke, L. A., Neimeyer, R. A., McDevitt-Murphy, M. E., Ippolito, M. R., & Roberts, J. M. (2011). Faith in the wake of homicide: Religious coping and bereavement distress in an African American sample. International Journal for the Psychology of Religion, 21(4), 289–307. https://doi.org/10.1080/10508619.2011.607416
- Carmassi, C., Dell’Oste, V., Foghi, C., Bertelloni, C. A., Conti, E., Calderoni, S., Battini, R., & Dell’Osso, L. (2021). Post-traumatic stress reactions in caregivers of children and adolescents/young adults with severe diseases: A systematic review of risk and protective factors. International Journal of Environmental Research and Public Health, 18(1), 189. https://doi.org/10.3390/ijerph18010189
- Cerel, J., van de Venne, J. G., Moore, M. M., Maple, M. J., Flaherty, C., & Brown, M. M. (2015). Veteran exposure to suicide: Prevalence and correlates. Journal of Affective Disorders, 179, 82–87. https://doi.org/10.1016/j.jad.2015.03.017
- Choi, H., & Cho, S.-M. (2020). Posttraumatic stress disorder and complicated grief in bereaved parents of the Sewol Ferry disaster exposed to injustice following the loss. International Journal of Social Psychiatry, 66(2), 163–170. https://doi.org/10.1177/0020764019894607
- Christiansen, D. M., & Elklit, A. (2008). Risk factors predict post-traumatic stress disorder differently in men and women. Annals of General Psychiatry, 7(24). https://doi.org/10.1186/1744-859X-7-24
- Cleiren, M., Diekstra, R. F., Kerkhof, A. J., & van der Wal, J. (1994). Mode of death and kinship in bereavement: Focusing on “who” rather than “how”. Crisis, 15(1), 22–36.
- Comtesse, H., & Rosner, R. (2019). Prolonged grief disorder among asylum seekers in Germany: The influence of losses and residence status. European Journal of Psychotraumatology, 10(1), 1591330. https://doi.org/10.1080/20008198.2019.1591330
- Cozza, S. J., Fisher, J. E., Fetchet, M. A., Chen, S., Zhou, J., Fullerton, C. S., & Ursano, R. J. (2019). Patterns of comorbidity among bereaved family members 14 years after the September 11th, 2001, terrorist attacks. Journal of Traumatic Stress, 32(4), 526–535. https://doi.org/10.1002/jts.22407
- Cozza, S. J., Fisher, J. E., Hefner, K. R., Fetchet, M. A., Chen, S., Zuleta, R. F., Fullerton, C. S., & Ursano, R. J. (2020). Human remains identification, grief, and posttraumatic stress in bereaved family members 14 years after the September 11, 2001, terrorist attacks. Journal of Traumatic Stress, 33(6), 1137–1143. https://doi.org/10.1002/jts.22548
- Djelantik, A. A. A. M. J., Aryani, P., Boelen, P. A., Lesmana, C. B. J., & Kleber, R. J. (2021). Prolonged grief disorder, posttraumatic stress disorder, and depression following traffic accidents among bereaved Balinese family members: Prevalence, latent classes and cultural correlates. Journal of Affective Disorders, 292, 773–781. https://doi.org/10.1016/j.jad.2021.05.085
- Djelantik, A. A. A. M. J., Smid, G. E., Kleber, R. J., & Boelen, P. A. (2017). Symptoms of prolonged grief, post-traumatic stress, and depression after loss in a Dutch community sample: A latent class analysis. Psychiatry Research, 247, 276–281. https://doi.org/10.1016/j.psychres.2016.11.023
- Djelantik, A. A. A. M. J., Smid, G. E., Kleber, R. J., & Boelen, P. A. (2018). Do prolonged grief disorder symptoms predict post-traumatic stress disorder symptoms following bereavement? A cross-lagged analysis. Comprehensive Psychiatry, 80, 65–71. https://doi.org/10.1016/j.comppsych.2017.09.001
- Djelantik, A. A. A. M. J., Smid, G. E., Mroz, A., Kleber, R. J., & Boelen, P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: Systematic review and meta regression analysis. Journal of Affective Disorders, 265, 146–156. https://doi.org/10.1016/j.jad.2020.01.034
- Dyregrov, K., Dyregrov, A., & Kristensen, P. (2015). Traumatic bereavement and terror: The psychosocial impact on parents and siblings 1.5 years after the July 2011 terror killings in Norway. Journal of Loss and Trauma, 20(6), 556–576. https://doi.org/10.1080/15325024.2014.957603
- Dyregrov, K., Nordanger, D., & Dyregrov, A. (2003). Predictors of psychosocial distress after suicide, SIDS and accidents. Death Studies, 27(2), 143–165. https://doi.org/10.1080/07481180302892
- Eisma, M. C., Lenferink, L. I. M., Chow, A. Y. M., Chan, C. L. W., & Li, J. (2019). Complicated grief and post-traumatic stress symptom profiles in bereaved earthquake survivors: A latent class analysis. European Journal of Psychotraumatology, 10(1), 1558707. https://doi.org/10.1080/20008198.2018.1558707
- Faschingbauer, T., Zisook, S., & Devaul, R. (1987). The Texas revised inventory of grief. In S. Zisook (Ed.), Biopsychosocial aspects of bereavement (pp. 111–124). American Psychiatric Press.
- Feigelman, W., & Cerel, J. (2020). Feelings of blameworthiness and their associations with the grieving process in suicide mourning. Frontiers in Psychology, 11, 610. https://doi.org/10.3389/fpsyg.2020.00610
- Field, N. P., Strasser, J., Taing, S., Horiuchi, S., Chhim, S., & Packman, W. (2014). Prolonged grief following the recent death of a daughter among mothers who experienced distal losses during the Khmer Rouge era: Validity of the prolonged grief construct in Cambodia. Psychiatry Research, 219(1), 183–190. https://doi.org/10.1016/j.psychres.2014.05.014
- Friedman, M. J. (2013). Finalizing PTSD in DSM-5: Getting here from there and where to go next. Journal of Traumatic Stress, 26(5), 548–556.https://doi.org/10.1002/jts.21840
- Glad, K. A., Stensland, S., Czajkowski, N. O., Boelen, P. A., & Dyb, G. (2022). The longitudinal association between symptoms of posttraumatic stress and complicated grief: A random intercepts cross-lag analysis. Psychological Trauma: Theory, Research, Practice, and Policy, 14(3), 386–392. https://doi.org/10.1037/tra0001087
- Grafiadeli, R., Glaesmer, H., Hofmann, L., Schäfer, T., & Wagner, B. (2021). Suicide risk after suicide bereavement: The role of loss-related characteristics, mental health, and hopelessness. Journal of Psychiatric Research, 144, 184–189. https://doi.org/10.1016/j.jpsychires.2021.09.056
- Grafiadeli, R., Glaesmer, H., & Wagner, B. (2022). Loss-related characteristics and symptoms of depression, prolonged grief, and posttraumatic stress following suicide bereavement. International Journal of Environmental Research and Public Health, 19(16), 10277. https://doi.org/10.3390/ijerph191610277
- Hardt, M. M., Jobe-Shields, L., & Williams, J. L. (2020). Complications in bereavement following motor vehicle crash fatalities in a sample of young adults. Traumatology, 26(4), 388–395. https://doi.org/10.1037/trm0000271
- Hawthorne, D. M., Youngblut, J. M., & Brooten, D. (2016). Parent spirituality, grief, and mental health at 1 and 3 months after their infant’s/child’s death in an intensive care unit. Journal of Pediatric Nursing, 31(1), 73–80. https://doi.org/10.1016/j.pedn.2015.07.008
- He, L., Tang, S., Yu, W., Xu, W., Xie, Q., & Wang, J. (2014). The prevalence, comorbidity and risks of prolonged grief disorder among bereaved Chinese adults. Psychiatry Research, 219(2), 347–352. https://doi.org/10.1016/j.psychres.2014.05.022
- Hebert, R. S., Dang, Q., & Schulz, R. (2006). Preparedness for the death of a loved one and mental health in bereaved caregivers of patients with dementia: Findings from the REACH study. Journal of Palliative Medicine, 9(3), 683–693. https://doi.org/10.1089/jpm.2006.9.683
- Heeke, C., Kampisiou, C., Niemeyer, H., & Knaevelsrud, C. (2019). A systematic review and meta-analysis of correlates of prolonged grief disorder in adults exposed to violent loss. European Journal of Psychotraumatology, 10(1), 1583524. https://doi.org/10.1080/20008198.2019.1583524
- Heeke, C., Stammel, N., & Knaevelsrud, C. (2015). When hope and grief intersect: Rates and risks of prolonged grief disorder among bereaved individuals and relatives of disappeared persons in Colombia. Journal of Affective Disorders, 173, 59–64. https://doi.org/10.1016/j.jad.2014.10.038
- Hibberd, R., Elwood, L. S., & Galovski, T. E. (2010). Risk and protective factors for posttraumatic stress disorder, prolonged grief, and depression in survivors of the violent death of a loved one. Journal of Loss and Trauma, 15(5), 426–447. https://doi.org/10.1080/15325024.2010.507660
- Hinton, D. E., Nickerson, A., & Bryant, R. A. (2013). Prolonged grief in Cambodian refugees following genocide: Rebirth concerns and avoidance of reminders. Journal of Loss and Trauma, 18(5), 444–460. https://doi.org/10.1080/15325024.2012.714218
- Horowitz, M. (1974). Stress response syndromes. Character style and dynamic psychotherapy. Archives of General Psychiatry, 31(6), 768–781. https://doi.org/10.1001/archpsyc.1974.01760180012002
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of event scale: A measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218. https://doi.org/10.1097/00006842-197905000-00004
- Huh, H. J., Huh, S., Lee, S. H., & Chae, J.-H. (2017). Unresolved bereavement and other mental health problems in parents of the sewol ferry accident after 18 months. Psychiatry Investigation, 14(3), 231. https://doi.org/10.4306/pi.2017.14.3.231
- Jann, P., Neldner, S., Neuner, F., & Mohammed, R. (2024). Complicated grief and posttraumatic stress after loss and separation under terror conditions. Journal of Traumatic Stress, 37(1), 154–165. https://doi.org/10.1002/jts.22990
- Kaltman, S., & Bonanno, G. A. (2003). Trauma and bereavement: Examining the impact of sudden and violent deaths. Journal of Anxiety Disorders, 17(2), 131–147.https://doi.org/10.1016/S0887-6185(02)00184-6
- Kessler, R. C., Rose, S., Koenen, K. C., Karam, E. G., Stang, P. E., Stein, D. J., Heeringa, S. G., Hill, E. D., Liberzon, I., McLaughlin, K. A., McLean, S. A., Pennell, B. E., Petukhova, M., Rosellini, A. J., Ruscio, A. M., Shahly, V., Shalev, A. Y., Silove, D., Zaslavsky, A. M., … Carmen Viana, M. (2014). How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO world mental health surveys. World Psychiatry, 13(3), 265–274. https://doi.org/10.1002/wps.20150
- Killikelly, C., Zhou, N., Merzhvynska, M., Stelzer, E. M., Dotschung, T., Rohner, S., Sun, L. H., & Maercker, A. (2020). Development of the international prolonged grief disorder scale for the ICD-11: Measurement of core symptoms and culture items adapted for Chinese and German-speaking samples. Journal of Affective Disorders, 277, 568–576. https://doi.org/10.1016/j.jad.2020.08.057
- King, D. W., Taft, C., King, L. A., Hammond, C., & Stone, E. (2006). Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology, 36(12), 2980–2992.https://doi.org/10.1111/j.0021-9029.2006.00138.x
- Kloep, M. L., Lancaster, S. L., & Rodriguez, B. F. (2014). Sudden unexpected versus violent death and PTSD symptom development. Journal of Aggression, Maltreatment & Trauma, 23(3), 286–300. https://doi.org/10.1080/10926771.2014.882464
- Komischke-Konnerup, K. B., Vang, M. L., Lundorff, M., Elklit, A., & O’Connor, M. (2023). Do early symptoms of prolonged grief disorder lead to symptoms of posttraumatic stress disorder and depression? A longitudinal register-based study of the two first years of bereavement. Journal of Psychopathology and Clinical Science, 132(8), 996–1006. https://doi.org/10.1037/abn0000859
- Kristensen, P., Weisaeth, L., & Heir, T. (2009). Psychiatric disorders among disaster bereaved: An interview study of individuals directly or not directly exposed to the 2004 tsunami. Depression and Anxiety, 26(12), 1127–1133. https://doi.org/10.1002/da.20625
- Kristensen, P., Weisaeth, L., Hussain, A., & Heir, T. (2015). Prevalence of psychiatric disorders and functional impairment after loss of a family member: A longitudinal study after the 2004 Tsunami. Depression and Anxiety, 32(1), 49–56. https://doi.org/10.1002/da.22269
- Layne, C. M., Kaplow, J. B., Oosterhoff, B., Hill, R. M., & Pynoos, R. S. (2018). The interplay between posttraumatic stress and grief reactions in traumatically bereaved adolescents: When trauma, bereavement, and adolescence converge. Adolescent Psychiatry, 7(4), 266–285. https://doi.org/10.2174/2210676608666180306162544
- Lenferink, L. I. M., de Keijser, J., Smid, G. E., Djelantik, A. A. A. M. J., & Boelen, P. A. (2017). Prolonged grief, depression, and posttraumatic stress in disaster-bereaved individuals: Latent class analysis. European Journal of Psychotraumatology, 8(1), 1298311. https://doi.org/10.1080/20008198.2017.1298311
- Lenferink, L. I. M., Eisma, M. C., Smid, G. E., de Keijser, J., & Boelen, P. A. (2022). Valid measurement of DSM-5 persistent complex bereavement disorder and DSM-5-TR and ICD-11 prolonged grief disorder: The Traumatic Grief Inventory-Self Report Plus (TGI-SR+). Comprehensive Psychiatry, 112, 152281. https://doi.org/10.1016/j.comppsych.2021.152281
- Lenferink, L. I. M., Nickerson, A., de Keijser, J., Smid, G. E., & Boelen, P. A. (2019). Reciprocal associations among symptom levels of disturbed grief, posttraumatic stress, and depression following traumatic loss: A four-wave cross-lagged study. Clinical Psychological Science, 7(6), 1330–1339. https://doi.org/10.1177/2167702619858288
- Lenferink, L. I. M., Nickerson, A., de Keijser, J., Smid, G. E., & Boelen, P. A. (2020). Trajectories of grief, depression, and posttraumatic stress in disaster-bereaved people. Depression and Anxiety, 37(1), 35–44. https://doi.org/10.1002/da.22850
- Lobb, E. A., Kristjanson, L. J., Aoun, S. M., Monterosso, L., Halkett, G. K., & Davies, A. (2010). Predictors of complicated grief: A systematic review of empirical studies. Death Studies, 34(8), 673–698. https://doi.org/10.1080/07481187.2010.496686
- Lubens, P., & Silver, R. C. (2019). U.S. combat veterans’ responses to suicide and combat deaths: A mixed-methods study. Social Science & Medicine, 236, 112341. https://doi.org/10.1016/j.socscimed.2019.05.046
- Lumbeck, G., Brandstaetter, M., & Geissner, E. (2012). Erstvalidierung der deutschen Version des „Inventory of Complicated Grief” (ICG-D). Zeitschrift für Klinische Psychologie und Psychotherapie, 41(4), 243–248.https://doi.org/10.1026/1616-3443/a000172
- Maciejewski, P. K., Maercker, A., Boelen, P. A., & Prigerson, H. G. (2016). ‘Prolonged grief disorder’ and ‘persistent complex bereavement disorder’, but not ‘complicated grief’, are one and the same diagnostic entity: An analysis of data from the Yale Bereavement Study. World Psychiatry: Official Journal of the World Psychiatric Association (WPA), 15(3), 266–275. https://doi.org/10.1002/wps.20348
- Martin-Soelch, C., & Schnyder, U. (2019). Editorial: Resilience and vulnerability factors in response to stress. Frontiers in Psychiatry, 10, 732. https://doi.org/10.3389/fpsyt.2019.00732
- Matthews, L. R., Quinlan, M. G., & Bohle, P. (2019). Posttraumatic stress disorder, depression, and prolonged grief disorder in families bereaved by a traumatic workplace death: The need for satisfactory information and support. Frontiers in Psychiatry, 10, 609. https://doi.org/10.3389/fpsyt.2019.00609
- McDevitt-Murphy, M. E., Neimeyer, R. A., Burke, L. A., Williams, J. L., & Lawson, K. (2012). The toll of traumatic loss in African Americans bereaved by homicide. Psychological Trauma: Theory, Research, Practice, and Policy, 4(3), 303–311. https://doi.org/10.1037/a0024911
- McKay, M. T., Cannon, M., Healy, C., Syer, S., O’Donnell, L., & Clarke, M. C. (2021). A meta-analysis of the relationship between parental death in childhood and subsequent psychiatric disorder. Acta Psychiatrica Scandinavica, 143(6), 472–486. https://doi.org/10.1111/acps.13289
- Mitchell, A. M., Kim, Y., Prigerson, H. G., & Mortimer-Stephens, M. (2004). Complicated grief in survivors of suicide. Crisis, 25(1), 12–18. https://doi.org/10.1027/0227-5910.25.1.12
- Mitchell, A. M., & Terhorst, L. (2017). PTSD symptoms in survivors bereaved by the suicide of a significant other. Journal of the American Psychiatric Nurses Association, 23(1), 61–65. https://doi.org/10.1177/1078390316673716
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed.1000097
- Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., Currie, M., Lisy, K., Qureshi, R., Mattis, P., & Mu, P. (2020). Systematic reviews of etiology and risk. In E. Aromataris, C. Lockwood, K. Porritt, B. Pilla, & Z. Jordan (Eds.), JBI manual for evidence synthesis. JBI. https://doi.org/10.46658/JBIMES-24-06
- Morina, N. (2011). Rumination and avoidance as predictors of prolonged grief, depression, and posttraumatic stress in female widowed survivors of war. Journal of Nervous & Mental Disease, 199(12), 921–927.https://doi.org/10.1097/NMD.0b013e3182392aae
- Mutabaruka, J., Séjourné, N., Bui, E., Birmes, P., & Chabrol, H. (2012). Traumatic grief and traumatic stress in survivors 12 years after the genocide in Rwanda. Stress and Health, 28(4), 289–296. https://doi.org/10.1002/smi.1429
- Nakajima, S., Ito, M., Shirai, A., & Konishi, T. (2012). Complicated grief in those bereaved by violent death: The effects of post-traumatic stress disorder on complicated grief. Dialogues in Clinical Neuroscience, 14(2), 210–214. https://doi.org/10.31887/DCNS.2012.14.2/snakajima
- Neimeyer, R. A., & Burke, L. A. (2013). Complicated grief and the end of life: Risk factors and treatment considerations. In J. L. Werth, Jr. (Ed.), Counseling clients near the end of life: A practical guide for mental health professionals (pp. 205–228). Springer.
- Nickerson, A., Liddell, B. J., Maccallum, F., Steel, Z., Silove, D., & Bryant, R. A. (2014). Posttraumatic stress disorder and prolonged grief in refugees exposed to trauma and loss. BMC Psychiatry, 14, 106. https://doi.org/10.1186/1471-244X-14-106
- O’Connor, M., Nickerson, A., Aderka, I. M., & Bryant, R. A. (2015). The temporal relationship between change in symptoms of prolonged grief and posttraumatic stress following old age spousal bereavement. Depression and Anxiety, 32(5), 335–340. https://doi.org/10.1002/da.22349
- Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. https://doi.org/10.1037/0033-2909.129.1.52
- Prigerson, H. G., Horowitz, M. J., Jacobs, S. C., Parkes, C. M., Aslan, M., Goodkin, K., Raphael, B., Marwit, S. J., Wortman, C., Neimeyer, R. A., Bonanno, G., Block, S. D., Kissane, D., Boelen, P., Maercker, A., Litz, B. T., Johnson, J. G., First, M. B., & Maciejewski, P. K. (2009). Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Medicine, 6(8), e1000121. https://doi.org/10.1371/journal.pmed.1000121
- Prigerson, H. G., & Jacobs, S. C. (2001). Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. Schit (Eds.), Handbook of bereavement research (pp. 613–645). American Psychological Association.
- Prigerson, H. G., Maciejewski, P. K., Reynolds, C. F., III, Bierhals, A. J., Newsom, J. T., Fasiczka, A., Frank, E., Doman, J., & Miller, M. (1995). Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research, 59(1–2), 65–79. https://doi.org/10.1016/0165-1781(95)02757-2
- Reed, M. (1998). Predicting grief symptomatology among the suddenly bereaved. Suicide and Life-Threatening Behavior, 28(3), 285–301.https://doi.org/10.1111/j.1943-278X.1998.tb00858.x
- Santiago, P. N., Ursano, R. J., Gray, C. L., Pynoos, R. S., Spiegel, D., Lewis-Fernandez, R., Friedman, M. J., & Fullerton, C. S. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS One, 8(4), e59236. https://doi.org/10.1371/journal.pone.0059236
- Schaal, S., Dusingizemungu, J.-P., Jacob, N., Neuner, F., & Elbert, T. (2012). Associations between prolonged grief disorder, depression, posttraumatic stress disorder, and anxiety in Rwandan genocide survivors. Death Studies, 36(2), 97–117. https://doi.org/10.1080/07481187.2011.573177
- Schaal, S., Jacob, N., Dusingizemungu, J.-P., & Elbert, T. (2010). Rates and risks for prolonged grief disorder in a sample of orphaned and widowed genocide survivors. BMC Psychiatry, 10(1), Article 55. https://doi.org/10.1186/1471-244X-10-55
- Sekowski, M., & Prigerson, H. G. (2022). Conflicted or close: Which relationships to the deceased are associated with loss-related psychopathology? The British Journal of Clinical Psychology, 61(2), 510–526. https://doi.org/10.1111/bjc.12344
- Sharpe, T. L., Osteen, P., Frey, J. J., & Michalopoulos, L. M. (2014). Coping with grief responses among African American family members of homicide victims. Violence and Victims, 29(2), 332–347.https://doi.org/10.1891/0886-6708.VV-D-12-00083R1
- Smith, A. J., Abeyta, A. A., Hughes, M., & Jones, R. T. (2015). Persistent grief in the aftermath of mass violence: The predictive roles of posttraumatic stress symptoms, self-efficacy, and disrupted worldview. Psychological Trauma: Theory, Research, Practice, and Policy, 7(2), 179–186. https://doi.org/10.1037/tra0000002
- Smith, A. J., Layne, C. M., Coyle, P., Kaplow, J. B., Brymer, M. J., Pynoos, R. S., & Jones, R. T. (2017). Predicting grief reactions one year following a mass university shooting: Evaluating dose-response and contextual predictors. Violence and Victims, 32(6), 1024–1043.https://doi.org/10.1891/0886-6708.VV-D-16-00043
- Soydas, S., Smid, G. E., Goodfellow, B., Wilson, R., & Boelen, P. A. (2020). The UK national homicide therapeutic service: A retrospective naturalistic study among 929 bereaved individuals. Frontiers in Psychiatry, 11, 878. https://doi.org/10.3389/fpsyt.2020.00878
- Soydas, S., Smid, G. E., Lenferink, L. I. M., Djelantik, A. A. M. J., Goodfellow, B., Wilson, R., & Boelen, P. A. (2021). Psychopathology in a treatment-seeking sample of homicidally bereaved individuals: Latent class analysis. Journal of Affective Disorders, 292, 234–241. https://doi.org/10.1016/j.jad.2021.05.026
- Sprang, G., & McNeil, J. (1998). Post-homicide reactions: Grief, mourning and post-traumatic stress disorder following a drunk driving fatality. OMEGA – Journal of Death and Dying, 37(1), 41–58.https://doi.org/10.2190/GCGW-86DC-A30R-286A
- Stammel, N., Heeke, C., Bockers, E., Chhim, S., Taing, S., Wagner, B., & Knaevelsrud, C. (2013). Prolonged grief disorder three decades post loss in survivors of the Khmer Rouge regime in Cambodia. Journal of Affective Disorders, 144(1–2), 87–93. https://doi.org/10.1016/j.jad.2012.05.063
- Stammel, N., Heinzl, L., Heeke, C., Böttche, M., & Knaevelsrud, C. (2020). Association between prolonged grief and attitudes toward reconciliation in bereaved survivors of the Khmer rouge regime in Cambodia. Frontiers in Psychiatry, 11, 644. https://doi.org/10.3389/fpsyt.2020.00644
- Stroebe, W., & Schut, H. (2001). Risk factors in bereavement outcome: A methodological and empirical review. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. Schut (Eds.), Handbook of bereavement research: Consequences, coping, and care (pp. 349–371). American Psychological Association. https://doi.org/10.1037/10436-015
- Tortella-Feliu, M., Fullana, M. A., Pérez-Vigil, A., Torres, X., Chamorro, J., Littarelli, S. A., Solanes, A., Ramella-Cravaro, V., Vilar, A., González-Parra, J. A., Andero, R., Reichenberg, A., Mataix-Cols, D., Vieta, E., Fusar-Poli, P., Ioannidis, J., Stein, M. B., Radua, J., & Fernández de la Cruz, L. (2019). Risk factors for posttraumatic stress disorder: An umbrella review of systematic reviews and meta-analyses. Neuroscience & Biobehavioral Reviews, 107, 154–165. https://doi.org/10.1016/j.neubiorev.2019.09.013
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. https://doi.org/10.1016/j.cpr.2011.12.001
- Van de Venne, J., Cerel, J., Moore, M., & Maple, M. (2020). Sex differences in mental health outcomes of suicide exposure. Archives of Suicide Research, 24(2), 158–185. https://doi.org/10.1080/13811118.2019.1612800
- Van Denderen, M., de Keijser, J., Gerlsma, C., Huisman, M., & Boelen, P. A. (2014). Revenge and psychological adjustment after homicidal loss. Aggressive Behavior, 40(6), 504–511. https://doi.org/10.1002/ab.21543
- Van Denderen, M., de Keijser, J., Huisman, M., & Boelen, P. A. (2016). Prevalence and correlates of self-rated posttraumatic stress disorder and complicated grief in a community-based sample of homicidally bereaved individuals. Journal of Interpersonal Violence, 31(2), 207–227. https://doi.org/10.1177/0886260514555368
- Vanderwerker, L. C., & Prigerson, H. G. (2004). Social support and technological connectedness as protective factors in bereavement. Journal of Loss and Trauma, 9(1), 45–57.https://doi.org/10.1080/15325020490255304
- Wagner, B., Hofmann, L., & Grafiadeli, R. (2021). The relationship between guilt, depression, prolonged grief, and posttraumatic stress symptoms after suicide bereavement. Journal of Clinical Psychology, 77(11), 2545–2558. https://doi.org/10.1002/jclp.23192
- Wayland, S., & Ward, J. (2022). Dreading yet hoping: Traumatic loss impacted by reference DNA sample collection for families of missing people. Frontiers in Psychiatry, 13, 866269. https://doi.org/10.3389/fpsyt.2022.866269
- Weathers, F., Litz, B., Herman, D., Huska, J., & Keane, T. (1993). The PTSD checklist (PCL). Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies.
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5). Instrument National Center for PTSD.
- Weiss, D. S., & Marmar, C. R. (1997). Assessing psychological trauma and PTSD: A practitioner’s handbook (J. P. Wilson & T. M. Keane, Eds.). Guilford Press.
- Wijngaards-de Meij, L., Stroebe, M., Stroebe, W., Schut, H., Van den Bout, J., Van Der Heijden, P. G., & Dijkstra, I. (2008). The impact of circumstances surrounding the death of a child on parents’ grief. Death Studies, 32(3), 237–252. https://doi.org/10.1080/07481180701881263
- World Health Organization. (2019). International statistical classification of diseases and related health problems (11th ed.). WHO. https://icd.who.int/
- Yehene, E., Martin, Y., & Goldzweig, G. (2022). An analysis of factors predicting post-traumatic stress disorder and grief following comrade loss. Omega. Advance online publication. https://doi.org/10.1177/00302228221113616
- Zakarian, R. J., McDevitt-Murphy, M. E., Bellet, B. W., Neimeyer, R. A., & Burke, L. A. (2019). Relations among meaning making, PTSD, and complicated grief following homicide loss. Journal of Loss and Trauma, 24(3), 279–291. https://doi.org/10.1080/15325024.2019.1565111
- Zetumer, S., Young, I., Shear, M. K., Skritskaya, N., Lebowitz, B., Simon, N., Reynolds, C., Mauro, C., & Zisook, S. (2015). The impact of losing a child on the clinical presentation of complicated grief. Journal of Affective Disorders, 170, 15–21.https://doi.org/10.1016/j.jad.2014.08.021
