ABSTRACT
Background: Refugees and asylum seekers (ASRs) are frequently exposed to loss in addition to a variety of other stressors and often display high levels of various psychological symptoms.
Objective: The study aimed to primarily determine clusters of prolonged grief disorder (PGD), posttraumatic stress disorder (PTSD), and depression symptoms in bereaved ASRs and secondly identify predictors of cluster membership. Sociodemographic – and flight-related variables were investigated in exploratory analyses.
Method: ASRs in Germany (N = 92) with interpersonal loss exposure, i.e. at least one missing or deceased relative or friend, were assessed with interview-based questionnaires for PGD, PTSD, and depressive symptoms. We used k-means cluster analysis to distinguish symptom profiles and logistic regression analyses to identify predictors of cluster membership.
Results: We found a three-cluster-solution. The PGD-cluster (30%) was characterised predominantly by PGD symptoms, while the PGD/PTSD-cluster (32%) had high PGD and PTSD and moderate depressive symptoms. The resilient cluster (38%) showed low symptoms overall. insecure residence status predicted membership in the PGD and PGD/PTSD clusters relative to the resilient cluster, whilst higher attachment anxiety predicted membership in the PGD/PTSD cluster relative to the other clusters. Explorative analysis revealed duration of stay as a significant predictor.
Conclusion: Findings can extend the current knowledge about different symptom profiles among bereaved ASRs in Europe. Insights to attachment – and migration-related variables distinguishing between these profiles offer starting points for interventions.
HIGHLIGHTS
Bereaved asylum seekers and refugees in Germany can be grouped into three symptom clusters: (1) predominantly prolonged grief, (2) high prolonged grief, high posttraumatic stress, and moderate depressive symptoms, and (3) low symptom load.
Attachment – and migration-related variables (i.e. residence status, duration of stay, and attachment anxiety) distinguish between cluster membership.
Results highlight the importance of attending to profiles and not only single categories of symptoms and attachment features in bereaved asylum seekers and refugees.
Antecedentes: Los refugiados y solicitantes de asilo (ASRs) están frecuentemente expuestos a la pérdida, además de una variedad de otros factores estresantes, y a menudo muestran altos niveles de diversos síntomas psicológicos.
Objetivo: El estudio tiene como objetivo principal determinar los grupos de síntomas del trastorno de duelo prolongado (PGD por sus siglas en ingles), trastorno de estrés postraumático (TEPT) y depresión en ASRs en duelo, y secundariamente identificar los predictores de pertenencia a cada grupo. Las variables sociodemográficas y relacionadas con el vuelo fueron investigadas en análisis exploratorios.
Método: Se evaluaron a los ASRs en Alemania (N = 92) con exposición a la pérdida interpersonal, es decir, al menos un familiar o amigo desaparecido o fallecido, mediante cuestionarios basados en entrevistas para los síntomas de PGD, TEPT y depresión. Utilizamos análisis de agrupamiento k-media para distinguir perfiles de síntomas y análisis de regresión logística para identificar predictores de la pertenencia a los grupos.
Resultados: Encontramos una solución de tres grupos. El grupo de PGD (30%) se caracterizó predominantemente por síntomas de PGD, mientras que el grupo de PGD/TEPT (32%) tenía altos síntomas de PGD y TEPT y síntomas depresivos moderados. El grupo resiliente (38%) mostró bajos síntomas en general. El estado de residencia insegura predijo la pertenencia a los grupos de PGD y PGD/TEPT en comparación con el grupo resiliente, mientras que un mayor apego ansioso predijo la pertenencia al grupo de PGD/TEPT en comparación con los otros grupos. El análisis exploratorio reveló que la duración de la permanencia fue un predictor significativo.
Conclusión: Los hallazgos pueden ampliar el conocimiento actual sobre los diferentes perfiles de síntomas entre los ASRs en duelo en Europa. Los conocimientos sobre las variables relacionadas con el apego y la migración que se distinguen entre estos perfiles ofrecen puntos de partida para intervenciones.
1. Introduction
Around 117.2 million refugees are expected worldwide in 2023, and Germany is among the top four receiving countries (UNHCR, Citation2023). The distressing events asylum seekers and refugees (ASRs) face before, during, and after migration have various negative impacts on mental health (e.g. Steel et al., Citation2002). ASRs are often exposed to potentially traumatic events and loss (e.g. Nickerson et al., Citation2014) and are at increased risk for developing symptoms of post-traumatic stress disorder (PTSD), prolonged grief disorder (PGD), and depression, with pooled prevalence rates ranging from 30% to over 50% (Blackmore et al., Citation2020; Lechner-Meichsner et al., Citation2024).
PGD has recently been added as a new diagnosis to the ICD-11 (WHO, Citation2018) and DSM-5-TR (APA, Citation2022) and is characterised by yearning or persistent preoccupation coupled with additional symptoms that persist to an impairing degree for more than six (ICD-11) or 12 months (DSM-5-TR) after the loss. Despite certain similarities (e.g. intrusions), PGD differs from PTSD and depression, for example regarding specific cognitive beliefs (Boelen et al., Citation2016) and neurological activation patterns (Bryant et al., Citation2021). Nonetheless, PGD, PTSD, and depressive symptoms can develop interconnectedly (Boelen et al., Citation2010; Heeke, Kampisiou, et al., Citation2017; Karatzias et al., Citation2022). In a network analysis (Karatzias et al., Citation2022), symptoms of these disorders showed significant co-occurrence, with up to 61% of variance explained by adjacent symptoms. In light of the close association and comorbidity of these conditions, it seems worth investigating if subgroups with specific symptom constellations exist.
Prior studies have focused on understanding when and how symptoms of these disorders co-occur using latent class analysis (LCA). A systematic review of LCA studies in bereaved community samples and conflict-affected and displaced persons (Heeke et al., Citation2023) pointed towards three classes: a resilient class characterised by low symptoms, a class primarily displaying PGD symptoms, and a combined class with both PGD and PTSD symptoms. Depressive symptoms occurred in the PGD/PTSD class in some studies, while other studies did not find any differences in terms of depressive symptoms between classes (Heeke et al., Citation2023).
This pattern of LCA results has also been found in studies with ASRs samples, although the number of these studies is limited (Heeke et al., Citation2023). In a sample of traumatised ASRs undergoing psychological treatment in the Netherlands, three classes were identified based on moderate (10%), severe (43%), very severe (46%) PTSD, depression, anxiety, and somatic symptoms (Jongedijk et al., Citation2020). Nickerson et al. (Citation2014) found four classes among Mandaean adult ASRs in Australia: resilient (43%), PGD (16%), PTSD (25%), and combined PGD/PTSD (16%). Tay et al. (Citation2015) also identified these four classes in ASRs to Papua New Guinea, and Jann et al. (Citation2024) found the same solution in Iraqi internally displaced persons. None of these studies have investigated profiles based on PGD, PTSD and depressive symptoms simultaneously.
Previous research has identified several predictors of specific symptom profiles in ASR samples. For ASRs, pre- and post-migration stressors are essential predictors of mental health problems (Knipscheer et al., Citation2015; Lechner-Meichsner et al., Citation2024). Residential status seems to be an especially important determinant of mental health (e.g. Nickerson et al., Citation2019), while attachment style (Maccallum & Bryant, Citation2013) and potentially traumatic events (Arnetz et al., Citation2013; Knipscheer et al., Citation2015) play an important role for PDG, PTSD and depressive symptoms. To also account for protecting effects that might mitigate stress, we were interested in perceived social support.
ASRs face specific post-migration stressors in host countries, which have an impact on symptom levels (e.g. Lechner-Meichsner et al., Citation2024). An uncertain residence status, such as prolonged asylum proceedings, has been repeatedly linked to elevated PTSD (Borho et al., Citation2020; Georgiadou et al., Citation2018) and depressive symptoms (Hajak et al., Citation2021) in ASR samples. Regarding bereaved ASRs, the current study used data from a previously published study that linked an uncertain residence to higher levels of PGD and PTSD symptoms in bereaved ASRs in Germany (Comtesse & Rosner, Citation2019). Like in many other Western countries, waiting periods for asylum decisions are lengthy in Germany and only temporary permits are granted (BAMF, Citation2018). However, the possible influence of residence status has not been included in any LCA on bereaved individuals before.
Bereaved ASRs have to cope not only with general reactive distress to negative life events, but also with separation stress specific to the loss of an attachment figure (O'Connor, Citation2012). It is therefore important to also consider the role of attachment as an additional factor when studying psychological symptoms in bereaved ASRs. Attachment style has a prominent modulation role in models of the development of PGD (e.g. Maccallum & Bryant, Citation2013). Previous research has consistently linked attachment anxiety with concurrent symptoms of PGD, although results were less consistent for attachment avoidance (Russ et al., Citation2022). A longitudinal study has not found relationships between prolonged grief symptoms and attachment over time when controlling for baseline symptoms (Janshen et al., Citation2024). For PTSD symptoms, research has also identified associations with insecure attachment in ASRs (e.g. Liddell et al., Citation2021; Morina et al., Citation2016). In a LCA in bereaved adults with PGD and comorbid depression diagnoses, attachment styles differentiated between classes, with high anxious attachment predicting the PGD/depression class and avoidant attachment predicting the depression class (Maccallum & Bryant, Citation2018). However, in how far these associations extend to bereaved ASRs has not been studied before.
Besides, the cumulative effect of potentially traumatic events is presumed to increase reactive distress levels. It heightened the risk of PTSD and depressive symptoms in several regression-based studies (e.g. Arnetz et al., Citation2013; Knipscheer et al., Citation2015), while associations with PGD symptoms among ASRs were inconsistent (e.g. Bryant et al., Citation2020). Results regarding the influence of potentially traumatic events on class membership in bereaved and traumatised samples are also inconsistent (Heeke, Kampisiou, et al., Citation2017; Nickerson et al., Citation2014).
Lastly, predictors of class membership might also have a protective function such as social support. Yet, only two LCAs have investigated this (Heeke, Stammel, et al., Citation2017; Nickerson et al., Citation2014). In internally displaced conflict survivors in Columbia, less social support was perceived by members of a combined PGD/PTSD compared to a resilient class (Heeke, Stammel, et al., Citation2017). Similarly, in Mandaean ASRs to Australia, loss of culture and support predicted PTSD/PGD and PTSD but not PGD-only class membership (Nickerson et al., Citation2014). Some cross-sectional and longitudinal regression-based studies with different refugee samples have shown associations between social support and PTSD and depressive symptoms (e.g. LeMaster et al., Citation2018; Sierau et al., Citation2019), while others did not (e.g. Green et al., Citation2021). Also, more PGD symptoms were associated with less social support in ASRs to Germany who also form the sample for the current study (Comtesse et al., Citation2022) and in Cambodian conflict survivors (Heeke, Stammel, et al., Citation2017). However, the relevance of social support for class membership has not been investigated in bereaved ASRs before.
The present study aimed at identifying symptom profiles of PGD, PTSD, and depression in bereaved ASRs to Germany. To the best of our knowledge, this is the first investigation of such profiles in a refugee sample in Europe. The specific goals were twofold: First, we sought to identify symptom profiles of PGD, PTSD, and depressive symptoms using k-means cluster analysis. Based on the evidence reviewed above, we expected a resilient cluster with low symptoms, a cluster with predominantly PGD symptoms, and a cluster with high-symptom severity across all domains. Second, we aimed at determining predictors of cluster membership. We hypothesised that a higher number of potentially traumatic events, insecure residence status, and higher attachment insecurity would predict membership in clusters of PGD and high symptoms, while greater perceived social support would predict membership in a low-symptom or more resilient cluster.
2. Method
2.1. Procedure and sample
The study is a secondary analysis of data collected from ASRs living in Bavaria, Germany, between December 2017 and July 2018 (Comtesse & Rosner, Citation2019). The study was approved by the IRB of the Catholic University Eichstaett-Ingolstadt (approval number 2017/09) and detailed information on recruitment and data collection have been published elsewhere (see Comtesse & Rosner, Citation2019). In brief, recruitment was conducted in one initial reception centre and four decentralised collective accommodations in Bavaria, Germany. Participants were contacted via email distribution lists and posters and through personal conversations with the help of two cultural mediators. Overall, 104 ASRs met criteria for participation (i.e. applied for asylum in Germany, age 18 years or older, and informed consent, no suicidality, acute psychosis, or cognitive deficits). Participants were interviewed with questionnaire-based, interpreter-assisted interviews. Ninety-three participants had experienced the death of a loved one and one participant had to be excluded due to an outlier status (see below). The final sample for the current analysis thus consisted of N = 92 persons.
2.2. Measures
Sociodemographic data included personal and migration-related information (see Comtesse & Rosner, Citation2019; for a more detailed description). For the present study, residence status was dichotomised in secure (i.e. temporary residence permit) and insecure (i.e. rejected application in appeal or application in process).
Exposure to loss was assessed with a questionnaire on the number of deaths or missing persons within the nuclear family (spouse, children, parents, siblings), among other relatives, and close friends.
Exposure to potentially traumatic events across the life span was assessed with the Life Event Checklist (LEC; Weathers et al., Citation2013). A simplified response scheme was used in the present study and participants were asked to indicate whether they have experienced and/or witnessed 17 different events themselves on a dichotomous scale. The sum score for experienced potentially traumatic events was calculated, ranging from 0 to 17.
The 18-item Traumatic Grief Inventory Self-Report (TGI-SR; Boelen & Smid, Citation2017) was used to assess PGD symptom severity. Participants are asked to rate the extent to which they experienced grief symptoms during the past month on a scale ranging from 1 = never to 5 = always. In order to use the same reference point for all mental health measures in this study, we used a scale from 0 to 4 (see also Rosner et al., Citation2022). The TGI-SR sum score had excellent internal consistency (α = .93; Cohen, Citation1988).
Symptoms of PTSD were assessed with the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Weathers et al., Citation2013). The PCL-5 comprises 20 items that are rated on a scale from 0 = not at all to 4 = extremely and had good internal consistency (α = .90).
The 9-item Patient Health Questionnaire Depression Module (PHQ-9; Kroenke et al., Citation2001) was used to measure depressive symptoms. Items assess depressive symptoms during the last two weeks and range from 0 = not at all to 3 = nearly every day. The PHQ-9 had good internal consistency (α = .83).
Attachment security was assessed with the short version of the Experiences in Close Relationships-Revised Questionnaire (ECR-RD8; Ehrenthal et al., Citation2021). The ECR-RD8 uses four items each for the subscales anxiety and avoidance on an adapted Likert scale from 0 = do not agree at all to 4 = do fully agree (Ehrenthal et al., Citation2021). Taking scale length into account, the subscales had acceptable (anxiety: α = .73; avoidance: α = .67;) values for internal consistency in the present study.
We assessed perceived social support with the Duke/UNC Functional Social Support Questionnaire (FSSQ; Broadhead et al., Citation1998), which consists of eight items ranging from 0 to 4. The FSSQ had acceptable internal consistency (α = .78).
2.3. Statistical analysis
All analyses were conducted using R Studio version 4.2.3 (R Core Team, Citation2023). There were 24 incomplete cases with missing values (1% up to 28%) and no case needed to be excluded (Enders, Citation2022). Multiple imputation of missing values was performed using the MissForest package (Stekhoven, Citation2022).
Cluster analysis based on the k-means cluster method from the Stats package (R Core Team, Citation2023) was used to find symptom profiles for PGD, PTSD and depressive symptoms. Because of the present sample size (N = 92), we chose k-means cluster analysis over LCA. K-means cluster analysis tends to work well with samples as small as N = 50 (Dalmaijer et al., Citation2022; Henry et al., Citation2015), especially when the data has well-separated clusters. A sample size of n = 30 participants per expected subgroup is recommended and has been shown to provide adequate power in a simulation study (Dalmaijer, Citation2023; Dalmaijer et al., Citation2022). As we expected three clusters, our sample size was within those recommendations. Also, k-means cluster analysis in contrast to LCA accommodates metric variables without requiring dichotomisation, and thus retains more information on symptom levels. In sum, we favoured k-means cluster analysis for its superior handling of small sample sizes and capacity to incorporate dimensional data, thereby enhancing the analytical information content. However, it should be kept in mind when comparing results that the majority of studies that investigated symptom profiles used LCA.
Outliers were investigated using the single-linkage method (Satari et al., Citation2019). Visual inspection of the dendrograms revealed that one person was clustered at a significant distance from the others and assigned to a cluster of their own in the average linkage procedure. Therefore, this person was classified as an outlier and excluded from the subsequent analyses, leading to N = 92 persons analysed. The optimal number of clusters based on the k-means cluster procedure was determined using the NbClust package with the help of 23 indices (Charrad et al., Citation2014).
Associations of correlates with clusters were tested with multinomial logistic regression analyses. We first examined whether each predictor (i.e. potentially traumatic events, residence status, attachment, social support) was independently associated with cluster membership. In a second step, the predictors were combined in one multinomial logistic regression to control for overlap between the predictor variables. In addition, for exploratory purposes, sociodemographic and flight-related characteristics were compared between clusters using one-way ANOVAs. All tests were performed two-tailed with α = 0.05. We did not account for multiple testing for the explorative analysis as we aimed at hypothesis generation and not hypothesis testing. Using the adjusted p-value would most likely lead to the omission of relevant results because of missing power due to smaller sample size. The complete analytical code can be found in the Open Science Framework (OSF): https://osf.io/wek4b.
3. Results
Participants were on average 30.83 years old and the majority (68.48%) was male (see ). Participants had experienced on average 7.40 different potentially traumatic events (SD = 3.43). About 42% of participants had a temporary residence permit, and about 47% had an insecure residence status. presents the means, standard deviations, and intercorrelations of the socio-demographic data, mental health measures, and predictors.
Table 1. Sociodemographic and flight-related characteristics for the total sample and clusters.
Table 2. Means, standard deviations, correlations and internal consistency.
3.1. Cluster analysis
Nine indices pointed to two and three clusters each, two indices pointed to six and 15 clusters each, and one indice favoured an eight-cluster solution. The two- and three-cluster solution were therefore considered in terms of content and their interpretability. The two-cluster solution separated the sample into a high- and low-symptoms cluster. The three-cluster solution yielded more differentiated clusters. It clearly distinguished between one subgroup with predominantly PGD symptoms (PGD-cluster), a high-symptoms subgroup with a combination of PGD, PTSD and depressive symptoms (PGD/PTSD-cluster), and a low-symptoms cluster (resilient cluster). The resilient cluster in the three-cluster solution had lower values than the low-symptoms cluster in the two-cluster solution. Overall, the three-cluster solution showed superior content relevance, as it differentiated not solely in terms of symptom severity but also in the specific types of symptoms. This is relevant because k-means clustering maximises the distance between clusters, which tends to result in groups with a high and a low level of expression in the variables in case of highly correlated variables (e.g. Kodinariya & Makwana, Citation2013). This is often the case with regard to psychological symptoms and therefore the two-cluster solution was discarded.
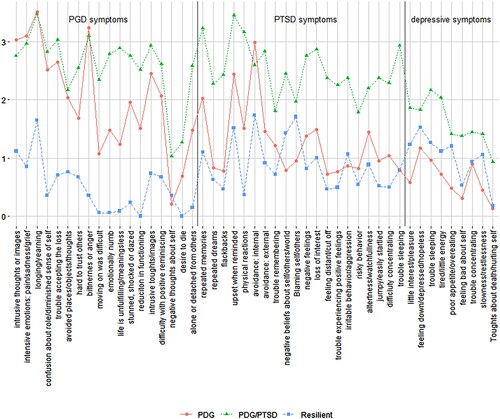
Participants in the PGD-cluster (n = 28; 30.43%) had high PGD symptoms (M = 36.50, SD = 9.11), moderate PTSD symptoms (M = 25.36, SD = 12.45), and low depressive symptoms (M = 5.75, SD = 4.47). The PGD/PTSD-cluster (n = 29; 31.52%) was characterised by high PGD symptoms (M = 46.66, SD = 15.77), high PTSD symptoms (M = 50.51, SD = 11.89), and moderate depressive symptoms (M = 14.48, SD = 6.10). Participants in the resilient cluster (n = 35; 38.04%) had low PGD symptoms (M = 9.17, SD = 8.25), low PTSD symptoms (M = 18.09, SD = 12.20), and low depressive symptoms (M = 8.94, SD = 6.61). displays the mean symptom scores of all items in the three-cluster solution.
Figure 1. Mean symptom scores per cluster.
3.2. Predictors of cluster membership
Results of the single multinomial logistic regressions are presented in . Secure residence status increased the likelihood of being in the resilient cluster compared to the PGD-cluster (OR = 3.57, 95%CI [1.25; 10.19]) and the PGD/PTSD-cluster (OR = 4.44, 95%CI [1.53; 12.88]). There was no significant difference for being in the PGD-cluster compared to the PGD/PTSD-cluster. Attachment anxiety also predicted cluster membership. Higher scores increased the likelihood of being in the PGD/PTSD-cluster relative to the PGD-cluster (OR = 1.50, 95%CI [1.04; 2.18]) and the resilient cluster (OR = 1.46, 95%CI [1.03; 2.06]). There was no difference for the PGD-cluster compared to the resilient cluster. The PGD/PTSD-cluster had the highest attachment anxiety scores (M = 2.29, SD = 1.42), followed by the resilient cluster (M = 1.46, SD = 1.58) and the PGD cluster with slightly lower scores (M = 1.30, SD = 1.34). Attachment avoidance, perceived social support, exposure to potentially traumatic events did not predict cluster membership.
Table 3. Single multinominal logistic regression analyses.
As the duration of stay yielded a significant difference between clusters in the exploratory analysis (see ), the variable was included in the multiple multinomial regression with all predictors (). Residence status remained a significant predictor for membership in the PGD/PTSD-cluster relative to the resilient cluster. The prediction of PGD-cluster membership relative to the resilient cluster membership was no longer significant. Attachment anxiety remained a significant predictor of the PGD/PTSD-cluster relative to the resilient and PGD-cluster. Additionally, duration of stay significantly predicted PGD/PTSD-cluster membership relative to PGD-cluster membership. A longer duration of stay increased the likelihood of being in the PGD/PTSD-cluster relative to the PGD-cluster (OR = 1.04, 95%CI [1.00; 1.09]).
Table 4. Multiple multinominal logistic regression analysis.
3.3. Exploratory analysis
Sociodemographic and flight-related characteristics were compared between clusters (). Tukey post-hoc tests after to the one-way ANOVAs revealed a significant difference in the duration of stay between the PGD- and resilient cluster (diff = 10.54, 95% CI [2.81, 18.27], p = .015), with the resilient cluster having spent more time in Germany.
4. Discussion
The present study focused on identifying symptom profiles of PGD, PTSD and depressive symptoms and their predictors among bereaved ASRs in Germany. K-means cluster analysis revealed a three-cluster-solution: PGD, PGD/PTSD, and resilient. Residence status, attachment anxiety, and duration of stay in Germany were relevant predictors of cluster membership.
These results align with the majority of existing research using LCA in bereaved community and displaced samples that points to three-class solutions with a resilient class with low symptoms, a high symptoms class, and a class predominantly characterised by PGD symptoms (Heeke et al., Citation2023). This combined evidence highlights the centrality of PGD symptoms among bereaved individuals. No cluster with elevated depressive symptoms emerged in the present study, which is also in line with previous LCA studies assessing depressive symptoms in bereaved individuals (Heeke et al., Citation2023). However, some previous studies (see Heeke et al., Citation2023) identified a higher number of classes, possibly due to sample differences (e.g. age, gender ratio) as well as symptom domains assessed. Unlike in previous studies with conflict-affected and ASR samples (Heeke, Stammel, et al., Citation2017; Nickerson et al., Citation2014), PTSD symptoms did not form a separate cluster. The only study with ASRs that also examined PGD and PTSD (Nickerson et al., Citation2014) revealed four classes, with an additional predominant PTSD class. Sample characteristics (e.g. shorter stay in the host country and more heterogeneous sample in the current study) could account for this difference. The resilient cluster in the present study was also larger than the respective classes in some previous studies with non-ASRs samples (Heeke et al., Citation2023), but smaller than in the two studies that focused exclusively on ASRs (Nickerson et al., Citation2014; Tay et al., Citation2015).
Insecure residence status and attachment anxiety appeared as predictors of cluster membership in this study. This aligns with other studies that linked insecure residence status to PTSD symptoms (Borho et al., Citation2020; Georgiadou et al., Citation2018) and depressive symptoms (Hajak et al., Citation2021) and lends further evidence to its detrimental effects. Attachment anxiety predicted PGD/PTSD-cluster membership, relative to both the PGD- and resilient cluster. This underlines its relation to PGD symptoms (Maccallum & Bryant, Citation2013), although it is unclear whether it has a modulating function or changes are solely a concomitant phenomenon of loss. A study on trauma-focused treatment demonstrated a concurrent improvement of PTSD symptoms and attachment avoidance and anxiety, pointing towards a correlation between attachment and stress-related symptoms (Rimane et al., Citation2022). Also, the result aligns with existing cross-sectional research linking insecure attachment, particularly attachment anxiety, to PTSD (e.g. Liddell et al., Citation2021), and PGD symptoms (Russ et al., Citation2022) in bereaved adults. However, due to the cross-sectional character of these studies and the present study, it remains unclear in how far the loss event has a possible impact on attachment styles themselves (e.g. increasing insecurity) and how the relation between attachment styles and PGD and PTSD symptoms develops over time. Future studies could investigate the development of symptoms over time, especially with regard to the interplay of symptoms and duration of stay, service utilisation, and residence status. For example, a systematic review suggested that ASRs use more mental health services, the longer they stay in their host country (Satinsky et al., Citation2019).
Exposure to potentially traumatic events did not emerge as a predictor. This adds to the inconsistent findings regarding the effect of cumulative traumatisation in bereaved samples (e.g. Lacour et al., Citation2020; Nickerson et al., Citation2014). Our results pointed against this association on a descriptive level, which makes it unlikely that the non-significant effect resulted from low power. Further, social support did not emerge as a protective factor, possibly due to sample characteristics such as the (temporary) collective housing conditions and relativity short duration of stay in Germany.
Our findings show that psychological reactions to trauma and bereavement during flight among ASRs to Germany are not uniform, but that there might be specific subgroups. First, the results highlight the co-occurrence of PDG, PTSD, and depressive symptoms in some individuals which is consistent with previous research (Boelen et al., Citation2010; Heeke, Kampisiou, et al., Citation2017; Karatzias et al., Citation2022). Second, a substantial proportion of the sample fell into the PGD only cluster, emphasising the distinction of PGD as a separate diagnostic entity (e.g. Boelen et al., Citation2010). Importantly, one third of the sample belonged to the resilient subgroup, pointing to their capacity to adapt to adversities and the need to identify more protective factors among ASRs (e.g. Safdar et al., Citation2021). The exploratory analyses revealed differences between clusters regarding the duration of stay in Germany and therefore longitudinal analyses are needed to shed light on the trajectories of symptoms over time.
Future analyses of symptom profiles in ASRs should be expanded to include complex PTSD, due to its high prevalence in this group (Lechner-Meichsner et al., Citation2024). Some studies with ASRs samples already investigated PTSD and complex PTSD together (e.g. Hyland et al., Citation2018), but the findings are still ambiguous and none of the previous studies have focused on bereaved ASRs. Regarding clinical practice, our results indicate that it might be favourable to treat bereaved ASRs based on their symptom profile. Future studies could explore a PGD-specific programme, a combined programme to address symptoms of PGD and PTSD and moderate depression (see Eddinger et al., Citation2021), and potentially a third, non-specific and low-threshold programme of preventative nature to support individuals with mild symptoms. Regarding public health implications, the present findings underscore the relevance of residence status on mental health outcomes. Asylum procedures should be sped up to reduce the duration of uncertainties, anxiety, and stress related to the outcome (Walther et al., Citation2020), which might be beneficial overall. While that might be challenging to achieve, as changes on a political level are needed, ASRs should also receive more support during the application process to help them cope with anxiety and uncertainties and avoid unnecessary delays. The connection between poor mental health and material and social disadvantages (Peñuela-O’Brien et al., Citation2023) emphasises the need for a close collaboration between health services and migration facilities.
4.1. Limitations
The study has several limitations. First, the cross-sectional design does not allow to draw causal inferences and we used a secondary correlational analysis, k-means cluster analysis. The selection and interpretation of clusters inevitably contains a certain arbitrariness (e.g. Kodinariya & Makwana, Citation2013). Our analysis of predictors of cluster membership was also limited to a small number of variables. Larger longitudinal studies among refugee samples are needed to unveil temporal relationships between symptoms and their predictors.
Second, the study relied on convenience sampling. The sample is quite representative for the refugee population in Germany at the time of the data collection regarding their countries of origin (see Comtesse & Rosner, Citation2019), but it cannot be ruled out that ASRs self-selected into the study based on their symptom severity. In addition, there was a large heterogeneity with regard to participants’ ethnic backgrounds (e.g. with regard to culture, language, home countries). We cannot rule out influences of cultural variables on our results, but due to the small sample size, we could directly not test for such influences. In addition, although the measures have been used with refugee and non-Western samples before (see Heeke et al., Citation2023 for an overview of instruments), they have not been culturally adapted, which might have led to missing culturally specific aspects of symptom profiles.
Third, data were collected with self-report measures that were administered with semi-structured interpreter-assisted interviews. Though professional interpreters can enhance communication, disclosure, and service equality (e.g. Karliner et al., Citation2007), perceived stigmatisation and social desirability might have influenced responses. Besides, the attachment avoidance subscale exhibited somewhat low internal consistency (Cohen, Citation1988). Results obtained with this subscale should be interpreted as conservative estimates.
Regarding the explorative analysis, the results are no longer significant when accounting for multiple testing and should thus be evaluated carefully.
Finally, although appropriate for the analyses, the sample size was at the lower end of the recommendations which may have influenced the stability of the cluster solution.
5. Conclusion
The present study offers valuable insights into the interplay of PGD, PTSD, and depression symptoms among bereaved ASRs in Germany. The results point to the importance of attending to symptom profiles rather than single categories of diagnoses in ASRs and the attachment features of PGD.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available upon request to the first author.
Additional information
Funding
References
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425787
- Arnetz, J., Rofa, Y., Arnetz, B., Ventimiglia, M., & Jamil, H. (2013). Resilience as a protective factor against the development of psychopathology among refugees. Journal of Nervous & Mental Disease, 201(3), 167–172. https://doi.org/10.1097/NMD.0b013e3182848afe
- Blackmore, R., Boyle, J. A., Fazel, M., Ranasinha, S., Gray, K. M., Fitzgerald, G., Misso, M., & Gibson-Helm, M. (2020). The prevalence of mental illness in refugees and asylum seekers: A systematic review and meta-analysis. PLoS medicine, 17(9), e1003337. https://doi.org/10.1371/journal.pmed.1003337
- Boelen, P. A., Reijntjes, A., Djelantik, A. M. J., & Smid, G. E. (2016). Prolonged grief and depression after unnatural loss: Latent class analyses and cognitive correlates. Psychiatry Research, 240, 358–363. https://doi.org/10.1016/j.psychres.2016.04.012
- Boelen, P. A., & Smid, G. E. (2017). The traumatic grief inventory self-report version (TGI-SR): Introduction and preliminary psychometric evaluation. Journal of Loss and Trauma, 22(3), 196–212. https://doi.org/10.1080/15325024.2017.1284488
- Boelen, P. A., van de Schoot, R., van den Hout, M. A., de Keijser, J., & van den Bout, J. (2010). Prolonged grief disorder, depression, and posttraumatic stress disorder are distinguishable syndromes. Journal of affective disorders, 125(1-3), 374–378. https://doi.org/10.1016/j.jad.2010.01.076
- Borho, A., Viazminsky, A., Morawa, E., Schmitt, G. M., Georgiadou, E., & Erim, Y. (2020). The prevalence and risk factors for mental distress among Syrian refugees in Germany: A register-based follow-up study. BMC Psychiatry, 20(1), 1–13. https://doi.org/10.1186/s12888-020-02746-2
- Broadhead, W. E., Gehlbach, S. H., De Gruy, F. V., & Kaplan, B. H. (1988). The Duke-UNC functional social support questionnaire: Measurement of social support in family medicine patients. Medical care, 709–723. https://doi.org/10.1097/00005650-198807000-00006
- Bryant, R. A., Andrew, E., & Korgaonkar, M. S. (2021). Distinct neural mechanisms of emotional processing in prolonged grief disorder. Psychological Medicine, 51(4), 587–595. https://doi.org/10.1017/S0033291719003507
- Bryant, R. A., Edwards, B., Creamer, M., O'Donnell, M., Forbes, D., Felmingham, K. L., Silove, D., Steel, Z., McFarlane, A. C., van Hooff, M., Nickerson, A., & Hadzi-Pavlovic, D. (2020). A population study of prolonged grief in refugees. Epidemiology and Psychiatric Sciences, 29, e44. https://doi.org/10.1017/S2045796019000386
- Bundesamt für Migration und Flüchtlinge (BAMF). (2018). Das Bundesamt in Zahlen 2018. Asyl, Migration und Integration. https://www.bamf.de/SharedDocs/Anlagen/DE/Statistik/BundesamtinZahlen/bundesamt-in-zahlen-2018.html?nn=284738
- Charrad, M., Ghazzali, N., Boiteau, V., & Niknafs, A. (2014). NbClust: An R Package for determining the relevant number of clusters in a data set. Journal of Statistical Software, 61(6), 1–36. http://www.jstatsoft.org/v61/i06/
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Academic Press.
- Comtesse, H., Lechner-Meichsner, F., Haneveld, J., Vogel, A., & Rosner, R. (2022). Prolonged grief in refugees living in Germany confronted with ambiguous or confirmed loss. Anxiety, Stress, & Coping, 35(3), 259–269. https://doi.org/10.1080/10615806.2021.1967936
- Comtesse, H., & Rosner, R. (2019). Prolonged grief disorder among asylum seekers in Germany: The influence of losses and residence status. European Journal of Psychotraumatology, 10(1), 1591330. https://doi.org/10.1080/20008198.2019.1591330
- Dalmaijer, E. S. (2023). Tutorial: A priori estimation of sample size, effect size, and statistical power for cluster analysis, latent class analysis, and multivariate mixture models. arXiv preprint arXiv:2309.00866.
- Dalmaijer, E. S., Nord, C. L., & Astle, D. E. (2022). Statistical power for cluster analysis. BMC Bioinformatics, 23(1), 1–28. https://doi.org/10.1186/s12859-022-04675-1
- Eddinger, J. R., Hardt, M. M., & Williams, J. L. (2021). Concurrent treatment for PTSD and prolonged grief disorder: Review of outcomes for exposure- and nonexposure-based treatments. OMEGA – Journal of Death and Dying, 83(3), 446–469. https://doi.org/10.1177/0030222819854907
- Ehrenthal, J. C., Zimmermann, J., Brenk-Franz, K., Dinger, U., Schauenburg, H., Brähler, E., & Strauß, B. (2021). Evaluation of a short version of the Experiences in Close Relationships-Revised questionnaire (ECR-RD8): Results from a representative German sample. BMC Psychology, 9(1), 1–11. https://doi.org/10.1186/s40359-021-00637-z
- Enders, C. K. (2022). Applied missing data analysis. Guilford Publications.
- Georgiadou, E., Zbidat, A., Schmitt, G. M., & Erim, Y. (2018). Prevalence of mental distress among Syrian refugees with residence permission in Germany: A registry-based study. Frontiers in psychiatry, 9, 393. https://doi.org/10.3389/fpsyt.2018.00393
- Green, M., King, E., & Fischer, F. (2021). Acculturation, social support and mental health outcomes among Syrian refugees in Germany. Journal of Refugee Studies, 34(2), 2421–2433. https://doi.org/10.1093/jrs/fez095
- Hajak, V. L., Sardana, S., Verdeli, H., & Grimm, S. (2021). A systematic review of factors affecting mental health and well-being of asylum seekers and refugees in Germany. Frontiers in Psychiatry, 12, 643704. https://doi.org/10.3389/fpsyt.2021.643704
- Heeke, C., Franzen, M., Knaevelsrud, C., & Lenferink, L. I. (2023). Latent classes of prolonged grief and other indicators of mental health in bereaved adults: A systematic review. Journal of Affective Disorders Reports, 14, 100654. https://doi.org/10.1016/j.jadr.2023.100654
- Heeke, C., Kampisiou, C., Niemeyer, H., & Knaevelsrud, C. (2017). A systematic review and meta-analysis of correlates of prolonged grief disorder in adults exposed to violent loss. European Journal of Psychotraumatology, 8(sup6), 1583524. https://doi.org/10.1080/20008198.2019.1583524
- Heeke, C., Stammel, N., Heinrich, M., & Knaevelsrud, C. (2017). Conflict-related trauma and bereavement: Exploring differential symptom profiles of prolonged grief and posttraumatic stress disorder. BMC Psychiatry, 17(1), 1–10. https://doi.org/10.1186/s12888-017-1286-2
- Henry, D., Dymnicki, A. B., Mohatt, N., Allen, J., & Kelly, J. G. (2015). Clustering methods with qualitative data: A mixed-methods approach for prevention research with small samples. Prevention Science, 16(7), 1007–1016. https://doi.org/10.1007/s11121-015-0561-z
- Hyland, P., Ceannt, R., Daccache, F., Abou Daher, R., Sleiman, J., Gilmore, B., Byrne, S., Shevlin, M., Murphy, J., & Vallières, F. (2018). Are posttraumatic stress disorder (PTSD) and complex-PTSD distinguishable within a treatment-seeking sample of Syrian refugees living in Lebanon? Global Mental Health, 5, e14. https://doi.org/10.1017/gmh.2018.2
- Jann, P., Neldner, S., Neuner, F., & Mohammed, R. (2024). Complicated grief and posttraumatic stress after loss and separation under terror conditions. Journal of Traumatic Stress, 37(1), 154–165. https://doi.org/10.1002/jts.22990
- Janshen, A., Boelen, P. A., Schut, H. A. W., & Eisma, M. C. (2024). Do insecure attachment styles predict prolonged grief symptoms? Significant null findings. Death Studies, 1–9. https://doi.org/10.1080/07481187.2023.2300063
- Jongedijk, R. A., Eising, D. D., van der Aa, N., Kleber, R. J., & Boelen, P. A. (2020). Severity profiles of posttraumatic stress, depression, anxiety, and somatization symptoms in treatment seeking traumatized refugees. Journal of Affective Disorders, 266, 71–81. https://doi.org/10.1016/j.jad.2020.01.077
- Karatzias, T., Knefel, M., Maercker, A., Cloitre, M., Reed, G., Bryant, R. A., Ben-Ezra, M., Kazlauskas, E., Jowett, S., Shevlin, M., & Hyland, P. (2022). The network structure of ICD-11 disorders specifically associated with stress: Adjustment disorder, prolonged grief disorder, posttraumatic stress disorder, and complex posttraumatic stress disorder. Psychopathology, 226–234. https://doi.org/10.1159/000523825
- Karliner, L. S., Jacobs, E. A., Chen, A. H., & Mutha, S. (2007). Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Services Research, 42(2), 727–754. https://doi.org/10.1111/j.1475-6773.2006.00629.x
- Knipscheer, J. W., Sleijpen, M., Mooren, T., Ter Heide, F. J. J., & van der Aa, N. (2015). Trauma exposure and refugee status as predictors of mental health outcomes in treatment-seeking refugees. BJPsych Bulletin, 39(4), 178–182. https://doi.org/10.1192/pb.bp.114.047951
- Kodinariya, T. M., & Makwana, P. R. (2013). Review on determining number of cluster in k-means clustering. International Journal of Advance Research in Computer Science and Management Studies, 1(6), 90–95.
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- Lacour, O., Morina, N., Spaaij, J., Nickerson, A., Schnyder, U., von Känel, R., Bryant, R. A., & Schick, M. (2020). Prolonged grief disorder among refugees in psychological treatment—association with self-efficacy and emotion regulation. Frontiers in Psychiatry, 11, 526. https://doi.org/10.3389/fpsyt.2020.00526
- Lechner-Meichsner, F., Comtesse, H., & Olk, M. (2024). Prevalence, comorbidities, and factors associated with prolonged grief disorder, posttraumatic stress disorder and complex posttraumatic stress disorder in refugees: A systematic review. Conflict and Health, 18(32). https://doi.org/10.1186/s13031-024-00586-5
- LeMaster, J. W., Broadbridge, C. L., Lumley, M. A., Arnetz, J. E., Arfken, C., Fetters, M. D., Jamil, H., Pole, N., & Arnetz, B. B. (2018). Acculturation and post-migration psychological symptoms among Iraqi refugees: A path analysis. American Journal of Orthopsychiatry, 88(1), 38. https://doi.org/10.1037/ort0000240
- Liddell, B. J., Malhi, G. S., Felmingham, K. L., Den, M. L., Das, P., Outhred, T., Nickerson, A., Askovic, M., Coello, M., Aroche, J., & Bryant, R. A. (2021). Activating the attachment system modulates neural responses to threat in refugees with PTSD. Social Cognitive and Affective Neuroscience, 16(12), 1244–1255. https://doi.org/10.1093/scan/nsab077
- Maccallum, F., & Bryant, R. A. (2013). A cognitive attachment model of prolonged grief: Integrating attachments, memory, and identity. Clinical Psychology Review, 33(6), 713–727. https://doi.org/10.1016/j.cpr.2013.05.001
- Maccallum, F., & Bryant, R. A. (2018). Prolonged grief and attachment security: A latent class analysis. Psychiatry Research, 268, 297–302. https://doi.org/10.1016/j.psychres.2018.07.038
- Morina, N., Schnyder, U., Schick, M., Nickerson, A., & Bryant, R. A. (2016). Attachment style and interpersonal trauma in refugees. Australian & New Zealand Journal of Psychiatry, 50(12), 1161–1168. https://doi.org/10.1177/0004867416631432
- Nickerson, A., Byrow, Y., O’Donnell, M., Mau, V., McMahon, T., Pajak, R., Li, S., Hamilton, A., Minihan, S., Liu, C., Bryant, R. A., Berle, D., & Liddell, B. J. (2019). The association between visa insecurity and mental health, disability and social engagement in refugees living in Australia. European journal of Psychotraumatology, 10(1), 1688129. https://doi.org/10.1080/20008198.2019.1688129
- Nickerson, A., Liddell, B. J., Maccallum, F., Steel, Z., Silove, D., & Bryant, R. A. (2014). Posttraumatic stress disorder and prolonged grief in refugees exposed to trauma and loss. BMC Psychiatry, 14(1), 1–11. https://doi.org/10.1186/1471-244X-14-106
- O'Connor, M.-F. (2012). Immunological and neuroimaging biomarkers of complicated grief. Dialogues in Clinical Neuroscience, 14(2), 141–148. https://doi.org/10.31887/DCNS.2012.14.2/mfoconnor
- Peñuela-O’Brien, E., Wan, M. W., Edge, D., & Berry, K. (2023). Health professionals’ experiences of and attitudes towards mental healthcare for migrants and refugees in Europe: A qualitative systematic review. Transcultural Psychiatry, 60(1), 176–198. https://doi.org/10.1177/13634615211067360
- R Core Team. (2023). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/.
- Rimane, E., Steil, R., Renneberg, B., & Rosner, R. (2022). Does attachment predict the outcome of cognitive processing therapy for posttraumatic stress disorder in adolescent patients with interpersonal traumatization? Psychotherapy Research, 32(5), 611–623. https://doi.org/10.1080/10503307.2021.1977866
- Rosner, R., Hagl, M., Bücheler, L., & Comtesse, H. (2022). Homesickness in asylum seekers: The role of mental health and migration-related factors. Frontiers in Psychiatry, 13, 1034370. https://doi.org/10.3389/fpsyt.2022.1034370
- Russ, V., Stopa, L., Sivyer, K., Hazeldine, J., & Maguire, T. (2022). The relationship between adult attachment and complicated grief: A systematic review. OMEGA – Journal of Death and Dying, 0, 00302228221083110. https://doi.org/10.1177/00302228221083110
- Safdar, S., Ray-Yol, E., Reif, J. A., & Berger, R. (2021). Multidimensional individual difference acculturation (MIDA) model: Syrian refugees’ adaptation into Germany. International Journal of Intercultural Relations, 85, 156–169. https://doi.org/10.1016/j.ijintrel.2021.09.012
- Satari, S. Z., Di, N. F. M., & Zakaria, R. (2019). Single-linkage method to detect multiple outliers with different outlier scenarios in circular regression model. AIP Conference Proceedings, 2059(1), 020003. https://doi.org/10.1063/1.5085946
- Satinsky, E., Fuhr, D. C., Woodward, A., Sondorp, E., & Roberts, B. (2019). Mental health care utilisation and access among refugees and asylum seekers in Europe: A systematic review. Health Policy, 123(9), 851–863. https://doi.org/10.1016/j.healthpol.2019.02.007
- Sierau, S., Schneider, E., Nesterko, Y., & Glaesmer, H. (2019). Alone, but protected? Effects of social support on mental health of unaccompanied refugee minors. European Child & Adolescent Psychiatry, 28(6), 769–780. https://doi.org/10.1007/s00787-018-1246-5
- Steel, Z., Silove, D., Phan, T., & Bauman, A. (2002). Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. The Lancet, 360(9339), 1056–1062. https://doi.org/10.1016/S0140-6736(02)11142-1
- Stekhoven, D. J. (2022). MissForest: Nonparametric missing value imputation using random forest. R Package Version 1.5. https://www.r-project.org, https://github.com/stekhoven/missForest
- Tay, A. K., Rees, S., Chen, J., Kareth, M., & Silove, D. (2015). The coherence and correlates of intermittent explosive disorder amongst West Papuan refugees displaced to Papua New Guinea. Journal of Affective Disorders, 177, 86–94. https://doi.org/10.1016/j.jad.2015.02.009
- United Nations High Commissioner for Refugees (UNHCR). (2023). Global Appeal 2023. Verfügbar unter: https://reporting.unhcr.org/globalappeal2023/pdf
- Walther, L., Fuchs, L. M., Schupp, J., & Von Scheve, C. (2020). Living conditions and the mental health and well-being of refugees: Evidence from a large-scale German survey. Journal of Immigrant and Minority Health, 22(5), 903–913. https://doi.org/10.1007/s10903-019-00968-5
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD. Retrieved June, 2022. https://www.ptsd.va.gov
- World Health Organization. (2018). ICD-11. International classification of diseases 11th revision. The global standard for diagnostic health information.
