ABSTRACT
Background: Co-occurrence of posttraumatic stress disorder (PTSD) in psychosis (estimated as 12%) raises personal suffering and societal costs. Health–economic studies on PTSD treatments in patients with a diagnosis of a psychotic disorder have not yet been conducted, but are needed for guideline development and implementation. This study aims to analyse the cost-effectiveness of guideline PTSD therapies in patients with a psychotic disorder.
Methods: This health–economic evaluation alongside a randomized controlled trial included 155 patients with a psychotic disorder in care as usual (CAU), with comorbid PTSD. Participants received eye movement desensitization and reprocessing (EMDR) (n = 55), prolonged exposure (PE) (n = 53) or waiting list (WL) (n = 47) with masked assessments at baseline (T0) and at the two-month (post-treatment, T2) and six-month follow-up (T6). Costs were calculated using the TiC-P interview for assessing healthcare consumption and productivity losses. Incremental cost-effectiveness ratios and economic acceptability were calculated for quality-adjusted life years (EQ-5D-3L-based QALYs) and PTSD ‘Loss of diagnosis’ (LoD, CAPS).
Results: Compared to WL, costs were lower in EMDR (-€1410) and PE (-€501) per patient per six months. In addition, EMDR (robust SE 0.024, t = 2.14, p = .035) and PE (robust SE 0.024, t = 2.14, p = .035) yielded a 0.052 and 0.051 incremental QALY gain, respectively, as well as 26% greater probability for LoD following EMDR (robust SE = 0.096, z = 2.66, p = .008) and 22% following PE (robust SE 0.098, z = 2.28, p = .023). Acceptability curves indicate high probabilities of PTSD treatments being the better economic choice. Sensitivity analyses corroborated these outcomes.
Conclusion: Adding PTSD treatment to CAU for individuals with psychosis and PTSD seem to yield better health and less PTSD at lower costs, which argues for implementation.
HIGHLIGHTS
• This is the first randomized study (N = 155) to examine cost-effectiveness of trauma focused therapy (TFT) in psychotic patients.• Exposure and EMDR yielded less PTSD, better health and lower costs than a PTSD waiting list.• TFT in psychosis is a candidate for clinical guidelines.
Antecedentes: La comorbilidad de TEPT en la psicosis (estimada en 12%) aumenta el sufrimiento personal y los costos para la sociedad. No se han realizado aún estudios de economía de la salud de los tratamientos de TEPT en pacientes con diagnóstico de un trastorno psicótico, pero son necesarios para el desarrollo e implementación de guías. Este estudio apunta a analizar la costo-efectividad de las terapias para TEPT con guías clínicas en pacientes con un trastorno psicótico.
Métodos: Esta evaluación de economía de la salud asociada a un estudio randomizado controlado incluyó a 155 pacientes con un trastorno psicótico en cuidado habitual (CAU), con TEPT comórbido.
Los pacientes recibieron terapia de reprocesamiento por movimientos oculares (EMDR, n=55), exposición prolongada (PE, n=53) o lista de espera (WL, n=47) con evaluaciones ciegas basal (T0), a los 2 meses (post-tratamiento, T2) y a los 6 meses de seguimiento (T6). Los costos fueron calculados usando la entrevista TiC-P para evaluar el consumo en los sistemas de salud y pérdidas de productividad. Las tasas incrementales de costo-efectividad y acepabilidad económica fueron calculadas por Años de Vida ajustados por calidad (QALY basado en EQ-5D-3L) y pérdida de diagnóstico de TEPT (LoD, CAPS)
Resultados: En comparación a lista de espera, los costos fueron menores en EMDR (-€1410) y PE (-€501) por paciente por cada 6 meses. Además, EMDR (SE robusta 0.024, t=2.14, p=0.035) y PE (SE robusta 0.024, t=2.14, p=0.035) produjeron una ganancia incremental en QALY de 0.05 y una probabilidad 26% mayor de LoD luego de EMDR (SE robusta 0.096, z=2.66, p=0.008) y 22% luego de PE (SE robusta 0.098, z=2.28, p=0.023). Las curvas de aceptabilidad indican altas probabilidades de que los tratamientos para TEPT sean la mejor alternativa económica. Los análisis de sensibilidad corroboraron estos resultados.
Conclusion: El agregar tratamiento para TEPT a los cuidados habituales en pacientes con psicosis y TEPT parece producir mejor salud y menos TEPT a menor costo, lo que aboga por su implementación.
背景:PTSD在精神病症中的共病率(估计为12%)会增加个人痛苦和社会成本。尚未对PTSD治疗在精神病症的患者中展开健康-经济研究(health–economic studies),但这些研究是治疗指南制定和实施所必需的。本研究旨在分析精神失常(psychotic disorder)患者的PTSD治疗指南的成本-效益。
方法:这项健康-经济评估与一项随机对照试验一起进行,包括155名接受普通护理(CAU)的共病PTSD的精神失常患者。被试接受了眼动脱敏和再处理疗法(EMDR,n= 55),延长暴露疗法(PE,n= 53)或进入等待名单(WL,n= 47),并在基线期(T0)和2个月(治疗后,T2)和6个月(T6)的随访进行了隐蔽评估(masked assessments)。使用TiC-P访谈评估医疗保健消耗和生产力损失。根据质量调整生命时间(quality-adjusted life years,基于EQ-5D-3L的QALYs)和PTSD’去诊断’(LoD,CAPS)计算增量成本效益比和经济可接受性。
结果:与WL相比,每位患者的EMDR( −1410欧元)和PE( −501欧元)每六个月治疗成本较低。此外,EMDR(robust SE 0.024,t = 2.14,p = .035)和PE(robust SE 0.024,t = 2.14,p = .035)产生0.05增量的QALY增益,EMDR后的LoD概率增加26%(robust SE = 0.096,z = 2.66,p = .008)和PE后增加22%(robust SE 0.098,z = 2.28,p = .023)。可接受性曲线表明 PTSD治疗的高概率是更经济的选择。敏感性分析证实了这些结果。
结论:在同时患有精神病症和创伤后应激障碍的个体的CAU加入PTSD治疗似乎可以以更低的成本得到更好的健康和更少的 PTSD,从而有助于实践运用。
Until now, no study has assessed the cost-effectiveness of trauma-focused treatment (TFT) in patients with a psychotic disorder. This is probably related to existing controversies as to whether or not to offer TFT to this target group, e.g. for a comorbid posttraumatic stress disorder (PTSD). On the one hand, manuals (Foa, Hembree, & Rothbaum, Citation2007), guidelines (Cloitre, Courtois, & Ford et al., Citation2012), clinicians (Becker, Zayfert, & Anderson, Citation2004; Frueh, Cusack, Grubaugh, Sauvageot, & Wells, Citation2006; Meyer, Farrell, Kemp, Blakey, & Deacon, Citation2014; Salyers, Evans, Bond, & Meyer, Citation2004; van Minnen, Hendriks, & Olff, Citation2010) and researchers (Ronconi, Shiner, & Watts, Citation2014) generally apply exclusion or a stabilization programme instead of offering TFT for psychotic individuals. On the other hand, there is no evidence to suggest that TFT would be unsafe and detrimental for individuals with comorbid problems such as psychosis (Brand, McEnery, Rossell, Bendall, & Thomas, Citation2017; van Minnen et al., Citation2010). On the contrary, evidence suggests that first-line TFT, more specifically prolonged exposure (PE) and eye movement desensitization and reprocessing (EMDR) therapy, might be as effective in patients with a psychotic disorder as in other patient groups (Brand et al., Citation2017; De Jongh et al., Citation2016). This controversy affects many people. It is estimated that in Europe about 600,000 and in the USA a quarter of a million adults need treatment for both a psychotic disorder and a comorbid PTSD (Achim et al., Citation2011). Yet, given the practice of exclusion, very few individuals will have received TFT. Resolving the PTSD treatment controversy is not only important for patients, but also for their families and the larger community because, worldwide, psychosis (Murray et al., Citation2012; Neil, Carr, Mihalopoulos, Mackinnon, & Morgan, Citation2014b; Reininghaus et al., Citation2015) and PTSD (Beard, Weisberg, & Keller, Citation2010; Issakidis, Sanderson, Corry, Andrews, & Lapsley, Citation2004) are among the most personally disabling and economically costly disorders. The joint impact of both disorders worsens the course of the disease and further increases costs (Lysaker & LaRocco, Citation2008; Seow et al., Citation2016). The need to address costs and effects of PTSD treatment in psychosis is reported as one of the NICE 2014 key priorities for implementation in recent clinical guidelines, sparking the awareness and assessment of trauma and PTSD in psychosis (NICE, Citation2014). The 2017 APA PTSD guideline (APA, Citation2017) and the 2013 WHO Guidelines for the Management of Conditions Specifically Related to Stress (WHO, Citation2013) state the importance of cost-effectiveness studies to expand the evidence base for future guideline recommendations. Guideline panels and financiers need cost-effectiveness examinations in order to be able to decide on the application, dissemination and implementation of TFT for individuals with psychotic disorders. Importantly, no economic data are currently available on this topic.
Cognitive behavioural therapy (CBT) has favourable economic evaluations for anxiety disorders (Issakidis et al., Citation2004; Mihalopoulos, Baxter, Whiteford, & Vos, Citation2014) and PTSD (Mihalopoulos et al., Citation2015), but was not examined in psychotic PTSD populations. A study among US veterans (N = 60) showed that PE for PTSD led to a significant and strong reduction in symptomatology and PE reduced health service utilization by (on average) US$194 per person (Tuerk et al., Citation2013). A randomized controlled trial in a non-psychotic traumatized population (N = 103) showed PE to be cost-effective relative to sertraline, saving US$262 per individual and yielding a 0.056 incremental gain in quality-adjusted life years (QALY) (Le, Doctor, Zoellner, & Feeny, Citation2014). PE was considered to be the preferable treatment option. Although EMDR is a recommended treatment for the effects of exposure to traumatic events, it has not yet produced a cost-effectiveness study in any patient group.
The present study conducts a cost-effectiveness analysis alongside a randomized clinical trial. In that trial we challenged the no-TFT paradigm in psychosis by demonstrating that TFT for PTSD primarily reduced PTSD (van Den Berg et al., Citation2015b) and secondarily also paranoid thinking (de Bont et al., Citation2016), depression (in PE) (de Bont et al., Citation2016) and re-victimization risk (van Den Berg et al., Citation2015a). Additionally, TFT fostered remission from schizophrenia and had no detrimental effect on voice hearing and social functioning (de Bont et al., Citation2016). The present health–economic analysis addresses the question as to whether PTSD treatment in patients with a psychotic disorder is economically affordable and perhaps even cost-saving. The study assesses costs and effects in 155 patients in care as usual (CAU) for psychosis, comparing a PTSD waiting list (WL) to add-on first-line PTSD treatments, i.e. EMDR therapy and PE therapy.
1. Methods
1.1. Participants and procedures
Full details of the study are reported elsewhere (de Bont et al., Citation2013; van Den Berg et al., Citation2015b). In brief, the study was designed as a randomized controlled trial in three parallel groups (EMDR, PE, WL) measuring costs and effects at baseline (T0), at the two-month (post-treatment, T2) and six-month follow-up (T6). Only the experimental conditions (EMDR and PE) had a longer-term follow-up, conducted at 12 months post-baseline, including measurements of both effects and costs, in order to assess the development (the robustness) of both outcomes over time.
Participants were recruited from 13 mental health services in the Netherlands. Eligible were adults (18–65 years) in care for psychotic disorders or mood disorders with psychotic features as confirmed by the Mini-International Neuropsychiatric Interview Plus (MINI Plus) (Sheehan et al., Citation1998) and suffering from co-morbid PTSD as established with the Clinician Administered PTSD Scale (CAPS) (Blake et al., Citation1995). Exclusion criteria were (i) language or attendance problems, (ii) seclusion, (iii) staying in a closed ward, (iv) high suicidality (MINI-Plus ‘high’ suicidality + last suicide attempt < six months + BDI-II-score ≥ 35), (v) mood and/or antipsychotic medication changes two months prior to study start, and (vi) IQ < 70. All eligible participants received a study description and 155 individuals gave written consent to participate. The CONSORT flow chart is available online (Supplemental Figure 1). The independent randomization bureau of the Parnassia Psychiatric Institute randomized participants using www.randomizer.org, yielding N = 47 participants in WL, N = 55 in EMDR and N = 53 in PE. Assessors masked for the participants’ randomization status carried out the measurements. The trial (de Bont et al., Citation2013) was designed in accordance with CONSORT guidelines, registered at isrctn.com (ISRCTN79584912) and approved by the Medical Ethics committee of the VU University Medical Center.
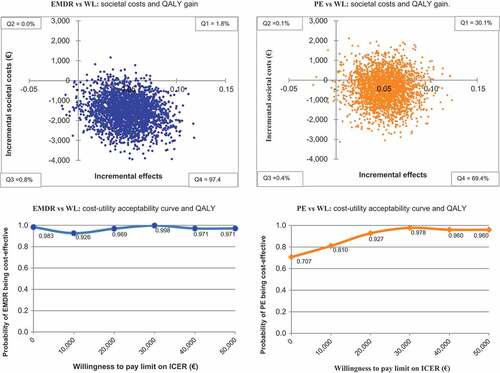
Figure 1. Cost-utility of QALY gain in main analysis (EM) after bootstrapping (n = 2500) comparing EMDR and PE to WL: ICUR planes and acceptability curves.
1.2. Interventions
All 155 participants received standard care from Multidisciplinary Assertive Community Treatment teams, consisting of pharmaceutical intervention, psychological treatment, casework, nursing and/or coaching (e.g. individual placement and support). Trauma-focused interventions were not allowed in CAU. As fully described elsewhere (de Bont et al., Citation2013; van Den Berg et al., Citation2015b), the waiting list patients obtained information on PTSD from their therapists. After six months they could choose the PTSD treatment they desired. Patients in the experimental conditions received eight weekly sessions of EMDR or PE therapy, yielding good to excellent adherence and therapist competence. EMDR was provided in 90-minute sessions conducted according to the standard 8-phase EMDR protocol using the Dutch translation. Eye movements were applied to tax patients’ working memory. EMDR therapy did not contain homework assignments. PE consisted of 90-minute imaginal exposure sessions in which the patient recounted the most disturbing traumatic memories. Between the sessions, patients listened daily to the audio-recording of the weekly sessions and completed exposure in vivo assignments, during which fearful trauma-related situations were approached.
1.3. Measures
The health outcome was QALY based on the EuroQol (EQ-5D-3L) self-report (König, Roick, & Angermeyer, Citation2007) which measured health-related quality of life in five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The five dimensions have three scoring levels (no problem, some problem, severe problem) describing 243 health states. The preference for each health state is expressed in utilities. A utility is anchored at 1 (perfect health) and 0 (death). We based utilities on a survey in the Netherlands (Lamers, Stalmeier, McDonnell, Krabbe, & van Busschbach, Citation2005) and used the so-called ‘Dutch tariff’. Utilities were obtained at baseline (T0), post-treatment (T2) and at six months (T6). Changes in utilities over time were converted to QALYs with the area under the curve method (Matthews, Altman, Campbell, & Royston, Citation1990). The EQ-5D has good reliability and validity (König et al., Citation2007).
The clinical outcome was ’loss of PTSD diagnosis’ (LoD), measured with the Clinician-Administered PTSD Scale (CAPS-IV). The CAPS (Blake et al., Citation1995) demonstrates excellent reliability, validity and sensitivity (Weathers, Keane, & Davidson, Citation2001). The CAPS is considered to be the gold standard for diagnosing DSM-IV-TR (APA, Citation2000) PTSD presence (y/n) and symptom severity (0–136). Following PTSD benchmark guidelines (Schnurr & Lunney, Citation2016), we defined LoD as no longer fulfilling the criteria of a CAPS-PTSD diagnosis and a CAPS severity score < 45. LoD was measured at six-months follow-up in all conditions, and at 12-months follow-up only in the PE and EMDR conditions.
1.4. Costs
Costs were assessed using the Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness, TiC-P (Hakkaart-van Roijen, Citation2002) developed by Trimbos institute and the Institute for Medical Technology Assessment (MTA). The TiC-P interview asks individuals for ‘health care units’ (see ), i.e. the number of contacts with healthcare providers (e.g. ‘family doctor/GP’) and for productivity losses stemming from absenteeism and/or presenteeism, i.e. being less productive while at work or at home.
Table 1. Baseline characteristics of the intention-to-treat sample for the three conditions with costs under expectation maximization imputation (N = 155).
Healthcare costs (including intervention costs of the add-on experimental treatments) were calculated by multiplying health care units by the standard full economic unit cost price in 2014 Euro (Supplementary Table 1). Medication costs were calculated by multiplying the official Dutch costs of Daily Defined Dosages (DDD) (http://www.medicijnkosten.nl) by the number of prescription days, plus €6.00 for the pharmacist’s dispensing costs.
Costs of productivity losses. Productivity losses stemming from absenteeism and presenteeism were calculated according to the human capital approach (Rice & Cooper, Citation1967) using standard hourly productivity costs (Hakkaart-van Rooijen, Tan, & Bouwmans, Citation2010). The cost accumulation from baseline to six months was assessed with the area under the curve method (Matthews et al., Citation1990).
Societal costs are the sum of healthcare costs and productivity losses: the total amount that is imposed upon society to pay as a consequence of the disorder.
The TiC-P is a reliable and valid alternative for collecting data on care consumption and productivity losses (Bouwmans et al., Citation2013). Costs were measured in Euro (€) for the reference year 2014.
1.5. Analysis
The cost-effectiveness analyses were conducted in accordance with the CONSORT (http://www.consort-statement.org/) and CHEERS (Husereau et al., Citation2013) guidelines. The aim of the cost-utility study (CUA) is to obtain incremental cost-utility ratios (ICURs) of costs per QALY gained. The aim of the cost-effectiveness study (CEA) is to obtain cost-effectiveness ratios (ICERs) of costs per lost PTSD diagnosis (LoD). Missing values of LoD, QALYs and costs at follow-up were imputed using the expectation maximization (EM) algorithm as implemented in SPSS 22.0. In a linear probability model, the incremental effects on QALY health gains and LoD clinical improvement were examined using robust standard errors based on the first-order Taylor-series linearization method.
An ICER (or ICUR) summarizes cost-effectiveness of a healthcare intervention. ICERs are calculated as (C1 − C0)/(E1 − E0) where C1 and E1 are the cost and effect in an experimental condition (i.e. EMDR or PE) and C0 and E0 are the cost and effect in the control condition (WL). In Stata14.2 resampling procedures (bootstrapping) generated 2500 ICERs, with incremental costs and incremental effects under a seemingly unrelated regression equations (SURE) model adjusted for possibly confounding baseline differences between the conditions. The simulated ICERs were depicted as a scatter over a cost-effectiveness plane: the intersection (zero) represents WL, the vertical axis represents the incremental costs of the treatment condition compared to WL and the horizontal axis represents the incremental effects of the treatment compared to WL. When most ICERs fall in the top left quadrant of the plane (Q2), depicting less effect at higher costs of the treatment compared to WL, then the treatment is considered ‘inferior’ to WL and is consequentially rejected from a cost-effectiveness perspective. When most simulated ICERs fall into the lower right quadrant (Q4), i.e. more health effect and lower costs, the intervention (EMDR or PE) is said to show ‘dominance’ over the control intervention (no treatment, WL). Obviously this outcome is the best possible from an economic perspective: the dominant treatment is considered to be the preferred option over the no treatment alternative. The bottom-left quadrant (Q3) implies health loss but for concomitantly lower cost. For decision-making purposes we need to take an additional step when the ICERs fall into the upper right-hand quadrant (Q1) where better health is obtained at additional costs. Then we need to address the question about the willingness to pay (WTP) for an additional unit of effect. We used a WTP ceiling of €50,000 for gaining one extra QALY.
1.6. Sensitivity analysis
To assess the robustness of the main analysis we carried out three sensitivity analyses. In the first two we switched from EM imputation (used in the main analysis) to last observation carried forward (LOCF) and to regression imputation (REG) as alternatives. The third re-analysis excluded the costs of admissions to psychiatric hospitals from the EM imputed dataset, as these were considered to be influential outlier costs (i.e. only a few patients generated high hospitals costs). Non-parametric paired samples Wilcoxon testing was used to assess longer-term consolidation of costs in PE and EMDR at 12-month follow-up.
2. Results
2.1. Sample
presents the baseline characteristics of the intention-to-treat sample (N = 155). Regarding current symptoms at baseline, 61.9% of the participants had active delusions, 40.0% had active hallucinations, 55.5% had current core symptoms of schizophrenia, 60.6% reported suicide attempts in the past and 45.2% had a current medium to high suicidal risk (de Bont et al., Citation2016). At baseline, there were no clinically or economically relevant differences between the conditions. Treatment dropout (EMDR 20%, PE 24.5%, p = .57) and dropout from our main assessment at six-months follow-up (EMDR 22%, PE 15%, WL 15%, p = .56) also showed no significant differences between the conditions.
2.2. Costs
The cost and effect outcomes of the main analysis are presented in ; note that the societal and healthcare perspectives are included, and the productivity perspective can be deduced from this. Compared to costs in the WL condition, healthcare costs (i.e. costs of CAU plus the add-on experimental intervention) were reduced by €1410 per patient in the EMDR condition and by €501 per patient in the PE condition. In other words, the experimental conditions (EMDR and PE) were associated with lower costs, even when offering EMDR or PE entails additional healthcare costs of their own. Compared to costs in the WL condition, the total societal costs (i.e. healthcare costs plus costs stemming from productivity losses) were reduced by €1574 in the EMDR condition and by €422 in the PE condition.
Table 2. Results of main analysis and sensitivity analyses.
2.3. Effects
The main analysis showed that EMDR gained 0.052 more QALYs compared with WL: this is a significant difference (robust SE = 0.025, t = 2.09, p = .039). Similarly, PE gained 0.051 more QALYs compared with WL (robust SE 0.024, t = 2.14, p = .035). In the EMDR condition, 26% more patients fulfilled the criteria of LoD than in the WL condition (incremental LoD = 0.256, robust SE = 0.096, z = 2.66, p = .008). Similarly, PE yielded an incremental effect of 22% (incremental LoD = 0.223, robust SE 0.098, z = 2.28, p = .023).
2.4. Cost-utility analysis
2.4.1. Healthcare perspective
From the healthcare perspective, the ICUR of EMDR was associated with a cost reduction of €26,924 per QALY gained and in PE a reduction of €9741, i.e. both PTSD treatment conditions are ‘dominant’ over WL (i.e. comparatively, they yielded reduced healthcare costs while QALYs were gained).
2.4.2. Societal perspective
When adopting the societal perspective, compared to WL, both EMDR and PE yielded lower costs while gaining QALYs. The ICUR of EMDR is -€30,061 and the ICUR in PE is -€8209. Therefore, both PTSD treatment conditions seem to be the better choice, i.e. ‘dominant’ over WL (i.e. better health outcomes for lower costs). shows 2500 bootstrapped ICERs in a scatterplot: for EMDR 97.4% and for PE 69.4% of the ICERs fall into the ‘dominant’ quadrant (Q4). This implies a high PE to very high EMDR probability that the treatments are dominant over WL. also shows the acceptability curves that depict the probability that EMDR and PE are deemed cost-effective relative to WL at varying willingness-to-pay ceilings for gaining one QALY. The curves show that, if there is no willingness to pay at all, EMDR still has a 98% probability and PE about a 70% probability of being more cost-effective than WL.
2.5. Cost-effectiveness analysis
2.5.1. Healthcare perspective
Comparison of WL and the experimental conditions shows that the ICER of EMDR is -€5497 per LoD and that of PE is -€2245, signifying that both experimental conditions are associated with better clinical outcomes and lower healthcare costs.
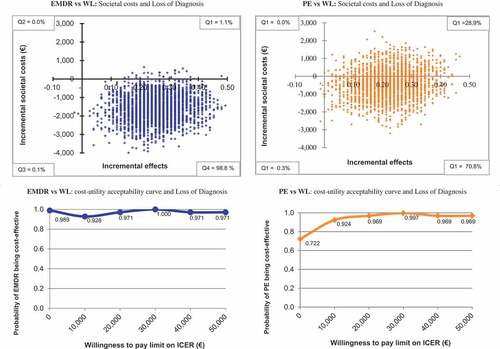
2.5.2. Societal perspective
The ICER of EMDR is -€6138 and for PE is -€1892, signifying lower costs for society while gaining one additional LoD. presents the cost-effectiveness graphs of LoD from the societal perspective. The scatter of the 2500 simulated ICERs shows that 98.8 and 70.8% of the ICERs fall in the dominant quadrant for EMDR and PE, respectively. When there is no willingness to pay for a LoD, EMDR still has a 99% probability and PE a 72% probability of being cost-effective.
Figure 2. Cost-effectiveness of PTSD loss of diagnosisa in main analysis (EM) after bootstrapping (n = 2500) comparing EMDR and PE to WL: ICER planes and acceptability curves.
2.6. Sensitivity analyses
As shown in , all three sensitivity checks corroborated that EMDR and PE are dominant over WL in terms of their cost-utility and cost-effectiveness. The results of LOCF and REG imputed analyses are comparable to the main analysis, which was based on EM imputation. An important finding is that one of the sensitivity analyses, i.e. ‘EM analysis without psychiatric hospital costs’, showed smaller cost reductions than the other three analyses, all of which included hospital costs (main analysis, LOCF and REG analysis). This finding indicates that a sizeable proportion of the relatively lower costs in EMDR and PE originates from fewer days in psychiatric hospitals.
2.7. Longer-term follow-up in EMDR and PE
Nonparametric paired samples Wilcoxon tests showed a significant decrease between the follow-up at six months and the extended follow-up at 12 months in healthcare costs (z = −4.99, p < .001) and production loss (z = −2.250, p = .024) in EMDR, whereas in PE the healthcare costs (z = −5.794, p < .001) decreased and productivity losses (z = −0.907, p = .364) remained the same over time. Apparently, cost reductions in the experimental conditions did not decay but were sustained or even increased over time.
2.8. Implementation costs
Up to now we have examined the so-called ‘steady-state costs’ in our health economic evaluation, i.e. the operating cost of offering CAU plus EMDR and PE interventions. This was done to the exclusion of the initial investment cost of about (i) €2800 for eight days of EMDR and PE training, and (ii) an additional €1100 for 10 sessions of supervision plus €1100 for 10 sessions of inter-vision. The sum total of these one-off costs is €5000 per therapist. Assuming that a trained and supervised therapist treats 10 patients in the first implementation year, then the per-patient costs would average at 5000/10 = €500; in the present study, these are costs recouped within six months by offering PTSD treatment. Therefore, the implementation costs can be seen as a good return on investment. Obviously, the per-patient costs of the implementation decrease after the initial phase, although some costs for supervision and/or inter-vision might continue.
3. Discussion
3.1. Main findings
This study evaluated the cost-effectiveness of EMDR and PE therapy for treating PTSD in patients with a psychotic disorder compared to CAU for these patients while in WL for PTSD treatment. Costs and effects were measured at six-months follow-up. Convincing evidence was obtained that both EMDR and PE are likely to reduce costs and yield better outcomes with regard to health gains expressed in QALYs and PTSD ‘Loss of diagnosis’. Three sensitivity analyses confirmed the robustness of the main findings. One sensitivity analysis provided an indication that, to some extent, lower costs in PTSD treatment originated from fewer days of hospital admission. A longer-term (12-month) assessment of costs in the treatment conditions showed that cost reductions were sustained or even increased.
3.2. Strengths and limitations
3.2.1. Strengths
To our knowledge, this is the first study to evaluate the cost-effectiveness of guideline trauma-focused treatment protocols for PTSD in psychotic psychiatric patients. Additionally, this study is the first to examine the cost-effectiveness of EMDR therapy in any patient group. The training and implementation of the treatments we studies is considered feasible in clinical practice, since EMDR and PE protocols are widely used and easily accessible. Dropout was low and comparable to PTSD studies in other patient groups (Hembree et al., Citation2003).
3.2.2. Limitations
A six-month follow-up is too short to draw final conclusions, as differences in costs and effects between the conditions might change over time. However, we found favourable developments in the costs at the extended 12-month follow-up concomitant with previously reported beneficial effects at 12-month follow-up on PTSD, depression, paranoid-referential thinking and remission from schizophrenia (van Den Berg et al., Citation2018) and a strongly reduced re-victimization risk (van Den Berg et al., Citation2015a). This suggests that cost reductions could increase further over time. Another limitation is that the economic evaluation relied on participants’ self-report regarding healthcare usage and changes in productivity; however, a validation study found a satisfactory to nearly perfect agreement between patient-reported data and data provided by health services (Bouwmans et al., Citation2013). Third, the imputation of missing endpoints using the EM algorithm might have added to outcome uncertainty; however, all of our sensitivity analyses replicated the results of the main analysis. Finally, the generalizability of our results is limited due to differences in healthcare systems across settings and countries. We recommend replication in different mental healthcare settings.
4. Conclusions
The present results suggest that in individuals with psychotic disorders and PTSD add-on EMDR and PE for PTSD reduce costs and yield better quality of life (more QALY gains) and clinical effects (more loss of diagnosis) than standard treatment for psychosis alone. At every level of society’s willingness to pay for a unit health gain (one loss of diagnosis, one QALY gained), adding PTSD treatment is the preferred option. The current findings challenge the ‘no trauma-focused treatment’ paradigm for psychotic individuals. Adjustment of clinical treatment guidelines and implementation decisions seem warranted. With about one in eight patients with a psychotic disorder having PTSD, implementing PTSD treatment might yield considerable personal and economic benefits in this relatively costly sector within mental health care.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Supplemental Material
Download Zip (5.6 MB)Acknowledgments
The authors wish to thank all participating patients, healthcare providers, the research team and mental health organizations. Special thanks go to Marion Bruns, BSc, and Daniëlle Tilburgs, MSc, Parnassia Psychiatric Institute, for managing logistics and filing of the data collection.
Disclosure statement
M.v.d.G. and D.v.d.B. receive income for published books on psychotic disorders and for the training of postdoctoral professionals in the treatment of psychotic disorders. A.d.J. receives income for published books on EMDR therapy and for the training of postdoctoral professionals in this method. A.v.M. receives income for published books and book chapters on PTSD and for the training of postdoctoral professionals in prolonged exposure. C.d.R. receives income for the training of postdoctoral professionals in EMDR therapy.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Achim, A. M. , Maziade, M. , Raymond, E. , Olivier, D. , Merette, C. , & Roy, M.-A. (2011). How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophrenia Bulletin , 37, 811–12.
- APA ed. (2000). Diagnostic and statistical manual of mental disorders . Washington, DC: American Psychiatric Association.
- APA . (2017). Clinical practice Guideline for the Treatment of PTSD. Retrieved from http://www.apa.org/ptsd-guideline/ptsd.pdf
- Beard, C. , Weisberg, R. B. , & Keller, M. B. (2010). Health-related quality of life across the anxiety disorders: Findings from a sample of primary care patients. Journal of Anxiety Disorders , 24, 559–564.
- Becker, C. B. , Zayfert, C. , & Anderson, E. (2004). A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy , 42, 277–292.
- Blake, D. D. , Weathers, F. W. , Nagy, L. M. , Kaloupek, D. G. , Gusman, F. D. , Charney, D. S. , & Keane, T. M. (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress , 8, 75–90.
- Bouwmans, C. , De Jong, K. , Timman, R. , Zijlstra-Vlasveld, M. , Van der Feltz-Cornelis, C. , Tan, S. S. , & Hakkaart-van Roijen, L. (2013). Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Services Research , 13, 217.
- Brand, R. M. , McEnery, C. , Rossell, S. , Bendall, S. , & Thomas, N. (2017). Do trauma-focussed psychological interventions have an effect on psychotic symptoms? A systematic review and meta-analysis. Schizophrenia Research , 195, 13–22.
- Cloitre, M. , Courtois, C. A. , Ford, J. D. , Green, B. L. , Alexander, P., Briere, J., … Van der Hart, O. (2012). The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults. Retrieved from https://www.istss.org/ISTSS_Main/media/Documents/ISTSS-Expert-Concesnsus-Guidelines-for-Complex-PTSD-Updated-060315.pdf
- de Bont, P. , van Den Berg, D. P. , van der Vleugel, B. M. , de Roos, C. , de Jongh, A. , van der Gaag, M. , & van Minnen, A. (2016). Prolonged exposure and EMDR for PTSD v. a PTSD waiting-list condition: Effects on symptoms of psychosis, depression and social functioning in patients with chronic psychotic disorders. Psychological Medicine , 46, 2411–2421.
- de Bont, P. A. , van Den Berg, D. P. , van der Vleugel, B. M. , de Roos, C. , Mulder, C. L. , Becker, E. S. , … van Minnen, A. (2013). A multi-site single blind clinical study to compare the effects of prolonged exposure, eye movement desensitization and reprocessing and waiting list on patients with a current diagnosis of psychosis and co morbid post traumatic stress disorder: Study protocol for the randomized controlled trial Treating Trauma in Psychosis. Trials , 14, 151.
- De Jongh, A. , Resick, P. A. , Zoellner, L. A. , van Minnen, A. , Lee, C. W. , Monson, C. M. , … Bicanic, I. A. E. (2016). A critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety , 33, 359–369.
- Foa, E. B. , Hembree, E. A. , & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide . New York, NY: Oxford University Press; US.
- Frueh, B. C. , Cusack, K. J. , Grubaugh, A. L. , Sauvageot, J. A. , & Wells, C. (2006). Clinicians’ perspectives on cognitive-behavioral treatment for PTSD among persons with severe mental illness. Psychiatric Services , 57, 1027–1031.
- Hakkaart-van Roijen, L. (2002). Handleiding Trimbos/iMTA questionnaire for costs associated with psychiatric illness (Tic-P) . Rotterdam, The Netherlands: Institute for Medical Technology Assessment. Retrieved from http://hdl.handle.net/1765/1337
- Hakkaart-van Rooijen, L. , Tan, S. S. , & Bouwmans, C. A. M. (2010). Handleiding voor kostenonderzoek. Methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg (in Dutch). Rotterdam, The Netherlands: Institute for Medical Technology Assessment, Erasmus University.
- Hembree, E. A. , Foa, E. B. , Dorfan, N. M. , Street, G. P. , Kowalski, J. , & Tu, X. (2003). Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress , 16, 555–562.
- Husereau, D. , Drummond, M. , Petrou, S. , Carswell, C. , Moher, D. , Greenberg, D. , … Force, C. T. (2013). Consolidated health economic evaluation reporting standards (CHEERS) statement. Value Health , 16, e1–e5.
- Issakidis, C. , Sanderson, K. , Corry, J. , Andrews, G. , & Lapsley, H. (2004). Modelling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychological Medicine , 34, 19–35.
- König, -H.-H. , Roick, C. , & Angermeyer, M. C. (2007). Validity of the EQ-5D in assessing and valuing health status in patients with schizophrenic, schizotypal or delusional disorders. European Psychiatry , 22, 177–187.
- Lamers, L. M. , Stalmeier, P. F. M. , McDonnell, J. , Krabbe, P. F. M. , & van Busschbach, J. J. (2005). Kwaliteit van leven meten in economische evaluaties: Het Nederlands EQ-5D-tarief [Measuring the quality of life in cost-utility analyses: The Dutch EQ-5D tariff]. Nederlands Tijdschrift voor Geneeskunde Ned Tijdschr Geneeskd , 149, 1574–1578.
- Le, Q. , Doctor, J. , Zoellner, L. , & Feeny, N. (2014). Cost-effectiveness of prolonged exposure therapy versus pharmacotherapy and treatment choice in posttraumatic stress disorder (the Optimizing PTSD Treatment Trial): A doubly randomized preference trial. The Journal of Clinical Psychiatry , 75, 222–230.
- Lysaker, P. , & LaRocco, V. (2008). The prevalence and correlates of trauma-related symptoms in schizophrenia spectrum disorder. Comprehensive Psychiatry , 49, 330–334.
- Matthews, J. , Altman, D. G. , Campbell, M. , & Royston, P. (1990). Analysis of serial measurements in medical research. Bmj , 300, 230–235.
- Meyer, J. M. , Farrell, N. R. , Kemp, J. J. , Blakey, S. M. , & Deacon, B. J. (2014). Why do clinicians exclude anxious clients from exposure therapy? Behaviour Research and Therapy , 54, 49–53.
- Mihalopoulos, C. , Baxter, A. J. , Whiteford, H. , & Vos, T. (2014). The Cost-effectiveness of Treatments for Anxiety Disorders. In P. Emmelkamp & T. Ehring (Eds.), The Wiley Handbook of Anxiety Disorders . Chichester, UK: John Wiley & Sons, Ltd.
- Mihalopoulos, C. , Magnus, A. , Lal, A. , Dell, L. , Forbes, D. , & Phelps, A. (2015). Is implementation of the 2013 Australian treatment guidelines for posttraumatic stress disorder cost-effective compared to current practice? A cost-utility analysis using QALYs and DALYs. Australian & New Zealand Journal of Psychiatry, 49(4), 360–376. https://doi.org/10.1177/0004867414553948
- Murray, C. , Vos, T. , Lozano, R. , Naghavi, M. , Flaxman, A. , Michaud, C. , … Edmond, K. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet , 380, 2197–2223.
- Neil, A. , Carr, V. , Mihalopoulos, C. , Mackinnon, A. , & Morgan, V. (2014b). Costs of psychosis in 2010: Findings from the second Australian National Survey of Psychosis. Australian and New Zealand Journal of Psychiatry , 48, 169–182.
- NICE . (2014, February). Psychosis and schizophrenia in adults: Key priorities for implementation. Retrieved from https://www.nice.org.uk/guidance/cg178/chapter/Key-priorities-for-implementation
- Reininghaus, U. , Dutta, R. , Dazzan, P. , Doody, G. A. , Fearon, P. , Lappin, J. , … Jones, P. B. (2015). Mortality in schizophrenia and other psychoses: A 10-year follow-up of the ӔSOP first-episode cohort. Schizophrenia Bulletin , 41, 664–673.
- Rice, D. P. , & Cooper, B. S. (1967). The economic value of human life. American Journal of Public Health and the Nations Health , 57, 1954–1966.
- Ronconi, J. M. , Shiner, B. , & Watts, B. V. (2014). Inclusion and exclusion criteria in randomized controlled trials of psychotherapy for PTSD. Journal of Psychiatric Practice , 20, 25–37.
- Salyers, M. P. , Evans, L. J. , Bond, G. R. , & Meyer, P. S. (2004). Barriers to assessment and treatment of posttraumatic stress disorder and other trauma-related problems in people with severe mental illness: Clinician perspectives. Community Mental Health Journal , 40, 17–31.
- Schnurr, P. P. , & Lunney, C. A. (2016). Symptom benchmarks of improved quality of life in PTSD. Depression and Anxiety , 33, 247–255.
- Seow, L. S. E. , Ong, C. , Mahesh, M. V. , Sagayadevan, V. , Shafie, S. , Chong, S. A. , & Subramaniam, M. (2016). A systematic review on comorbid post-traumatic stress disorder in schizophrenia. Schizophrenia Research , 176, 441–451.
- Sheehan, D. , Lecrubier, Y. , Sheehan, K. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry , 59, 22–33.
- Tuerk, P. W. , Wangelin, B. , Rauch, S. A. , Dismuke, C. E. , Yoder, M. , Myrick, H. , … Acierno, R. (2013). Health service utilization before and after evidence-based treatment for PTSD. Psychological Services , 10, 401.
- van Den Berg, D. , de Bont, P. , van der Vleugel, B. , de Roos, C. , de Jongh, A. , van Minnen, A. , & van der Gaag, M. (2015a, Published online: 24 November 2015). Trauma-focused treatment in PTSD patients with psychosis: Symptom exacerbation, adverse events, and revictimization. Schizophrenia Bulletin , 42, 693–702.
- van Den Berg, D. , de Bont, P. A. J. M. , van der Vleugel, B. M. , de Roos, C. , de Jongh, A. , Van Minnen, A. , & van der Gaag, M. (2015b). Prolonged exposure vs eye movement desensitization and reprocessing vs waiting list for posttraumatic stress disorder in patients with a psychotic disorder: A randomized clinical trial. JAMA Psychiatry , 72, 259–267.
- van Den Berg, D. , de Bont, P. A. J. M. , van der Vleugel, B. M. , de Roos, C. , de Jongh, A. , van Minnen, A. , & van der Gaag, M. (2018). Long-term outcomes of trauma-focused treatment in psychosis. The British Journal of Psychiatry , 1–3.
- van Minnen, A. , Hendriks, L. , & Olff, M. (2010). When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behaviour Research and Therapy , 48, 312–320.
- Weathers, F. W. , Keane, T. M. , & Davidson, J. R. (2001). Clinician-administered PTSD scale: A review of the first ten years of research. Depression & Anxiety , 13, 132–156.
- WHO . (2013). Guidelines for the management of conditions specifically related to stress. Retrieved from http://www.who.int/mental_health/emergencies/stress_guidelines/en/
