ABSTRACT
Background: Elevated prevalences of post-traumatic stress disorder (PTSD) and major depression (MD) have been reported in populations exposed to war. However, no global estimates of war survivors suffering from PTSD and/or MD in absolute numbers have been reported.
Objective: We made the first attempt to estimate in absolute numbers how many adult war survivors globally may suffer PTSD and/or MD, which should inform local and global mental health programmes.
Method: Drawing on the Uppsala Conflict Database, we reviewed all countries that suffered at least one war within their own territory between 1989 and 2015 (time span chosen on availability of geo-referenced data and population estimates). We then conducted a meta-analysis of current randomized epidemiological surveys on prevalence of PTSD and/or MD among war survivors. Finally, we extrapolated our results from the meta-analysis on the global population of adult war survivors by means of using general population data from the United Nations.
Results: We estimate that about 1.45 billion individuals worldwide have experienced war between 1989 and 2015 and were still alive in 2015, including one billion adults. On the basis of our meta-analysis, we estimate that about 354 million adult war survivors suffer from PTSD and/or MD. Of these, about 117 million suffer from comorbid PTSD and MD.
Conclusions: Based on the slim available evidence base, the global number of adult war survivors suffering PTSD and/or MD is vast. Most war survivors live in low-to-middle income countries with limited means to handle the enormous mental health burden. Since representative high quality data is lacking from most of these countries, our results contain a large margin of uncertainty and should be interpreted with caution.
HIGHLIGHTS
• We estimate that 1.45 billion people worldwide have experienced war between 1989 and 2015.• We estimate that 354 million adult war survivors globally suffer from PTSD and/or MD.• We estimate that 117 million adult war survivors globally suffer from a comorbidity of PTSD+MD.• Most war survivors live in low-to-middle income countries with limited means to handle the associated mental health burden.
Antecedentes: Se han reportado elevadas prevalencias de Trastorno de Estrés Postraumático (TEPT) y Depresión Mayor (DM) en poblaciones expuestas a la guerra. Sin embargo, no se han reportado estimaciones globales en números absoultos de los sobrevivientes a la guerra que padecen de TEPT y/o DM.
Objetivo: Realizamos el primer intento de estimar en números absolutos cuántos adultos sobrevivientes a la guerra globalmente sufren de TEPT y/o DM, lo que debería informar a los programas locales y globales de salud mental.
Método: Usando la Base de Datos de conflictos de Uppsala, revisamos todos los países que experimentaron al menos una guerra en su territorio entre 1989 y 2015 (intervalo de tiempo elegido según la disponibilidad de datos y estimaciones de población georeferenciados). Luego llevamos a cabo un meta-análisis de encuestas epidemiológicas randomizadas actuales sobre la prevalencia de TEPT y/o DM entre los sobrevivientes a la guerra. Finalmente, extrapolamos nuestros resultados del meta-análisis a la población global de adultos sobrevivientes a la guerra utilizando datos de población general de las Naciones Unidas.
Resultados: Estimamos que alrededor de 1.45 billones de individuos alrededor del mundo han experimentado la guerra entre 1989 y 2015 y continuaban con vida en 2015, incluyendo 1 billón de adultos. En base a nuestro meta-análisis, estimamos que alrededor de 354 millones de adultos sobrevivientes a la guerra padecen de TEPT y/o DM. De ellos, alrededor de 117 millones padecen de TEPT y DM comórbidos.
Conclusiones: Basado en la escasa evidencia disponible, el número global de adultos sobrevivientes a la guerra que padece de TEPT y/o DM es vasto. La mayoría de los sobrevivientes a la guerra viven en países de ingresos bajos a medios con limitados medios para manejar la enorme carga de salud mental. Dado que no se cuenta con datos representativos de alta calidad para la mayoría de estos países, nuestros resultados contienen un amplio margen de incertidumbre y deberían ser interpretados con precaución.
背景:已发现战争暴露的人群中创伤后应激障碍(PTSD)和重度抑郁症(MD)的患病率升高。但是,没有对遭受PTSD和/或MD的战争幸存者的全球数量进行估计。
目标:我们首次尝试估算全球可能患有PTSD和/或MD的成年战争幸存者的绝对数量,可以为当地和全球心理健康计划提供信息。
方法:借鉴乌普萨拉冲突(Uppsala Conflict)数据库,我们综述了1989年至2015年期间(时间跨度根据地理参考数据和人口估计数据的可用性)在其领土内至少遭受过一次战争的所有国家。然后,我们对战争幸存者中PTSD和/或MD患病率的随机流行病学调查进行了元分析。最后,我们通过使用联合国的一般人口数据,基于元分析结果,对成人战争幸存者的全球人口的进行推断。
结果:我们估计全球约有14.5亿人在1989年至2015年期间经历过战争,并且在2015年仍然活着,其中包括10亿成年人。根据我们的元分析,我们估计约有3.54亿成年战争幸存者患有
结论:基于有限的可用证据,全球患有PTSD和/或MD的成年战争幸存者的数量是巨大的。大多数战争幸存者生活在中低收入国家,应对巨大的心理健康负担的途径有限。由于大多数这些国家缺乏具有代表性的高质量数据,因此我们的结果存在很大的不确定性,应谨慎解释。
1. Introduction
Posttraumatic stress disorder (PTSD) and major depression (MD) are among the leading contributors to the global disease burden according to the global burden of disease report 2010 (Whiteford, Ferrari, Degenhardt, Feigin, & Vos, Citation2015). According to numerous predictions, MD will be the leading contributor to the global disease burden by 2020 (Mathers & Loncar, Citation2006; Murray & Lopez, Citation1996). PTSD also leads to a substantial functional impairment due to mental and physical dysfunctions and can follow a chronic course if untreated (Kessler et al., Citation2009; Morina, Wicherts, Lobbrecht, & Priebe, Citation2014; Nemeroff et al., Citation2006). Accordingly, PTSD and MD need to be addressed as a public health priority (Collins et al., Citation2011). Since the end of the Cold War in 1989, more than half of the countries in the world have been affected by armed conflicts (Marshall & Cole, Citation2009). PTSD and MD are the most prevalent mental disorders in war-affected communities, and significantly more prevalent than in communities with no recent history of conflict (Priebe et al., Citation2010). A meta-analysis from 2009 indicated that about 30% of individuals exposed to mass conflict and displacement suffer from PTSD and/or MD (Steel et al., Citation2009). However, this meta-analysis relied mostly on surveys conducted with subgroups of survivors of organized violence, such as survivors of torture or refugees. Hence, no conclusions about the prevalence of PTSD and MD in the general population in countries with a recent history of war can be made. Recently, we reported a meta-analysis on prevalences of PTSD and MD in adult civilian war survivors who live in war-afflicted regions. Similar to the results of Steel et al. (Citation2009), we found a prevalence of 26% for PTSD (k = 30 studies) and 27% for MD (k = 18 studies; Morina, Stam, Pollet, & Priebe, Citation2018). In the current paper, we extend this earlier work by estimating the global prevalence of PTSD and MD in adult survivors of war in absolute numbers. To the best of our knowledge, this is the first attempt to do so.
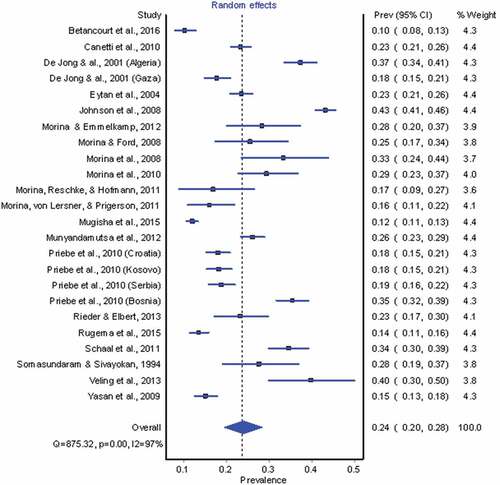
Figure 1. Forest plot depicting meta-analytic results of all representative surveys assessing PTSD in countries with a history of war between 1989 and 2015.
This approach should prove useful in better evaluating the current burden of PTSD and MD in war-ridden regions. Hence, this article aims at giving a global estimate of the absolute number of adult war survivors who suffer from PTSD and/or MD.
2. Materials and methods
2.1. Definition of war regions
To operationalize war and war regions, we utilized data from the Uppsala Conflict Data Program (UCDP) from the Department of Peace and Conflict Research of the Uppsala University in Sweden (Pettersson & Wallensteen, Citation2015; UCDP, Citation2018). The UCDP is a free access database on fatality statistics, geo-referenced event data, armed actor(s) and descriptions of conflict for all armed conflicts since 1946 until the previous calendar year. Data is collected globally, vigorously, comparable across cases and countries and updated annually. The year 1989 was chosen as a starting year, as the UCDP offers geo-referenced data on armed conflicts from 1989 onwards. Geo-referenced data is essential for the present review, as it makes prevalence estimates of war-related PTSD, MD or PTSD+MD more precise. The geo-referenced data of the UCDP helped us to identify how widespread each war was and, therefore, allowed for a more precise estimate of how many people had been affected by each war. In line with the UCDP, the following definition of war was utilized for the present review: ‘Armed conflict in which at least one actor is the government of a state, resulting in at least 1000 battle-related deaths in one calendar year’.
2.2. Reference estimates for extrapolation
The aims and methods of the previously published meta-analysis, on which the present work is based, were registered with the PROSPERO database (CRD42016032720, https://www.crd.york.ac.uk/prospero/). A more detailed description of methodology of the original meta-analysis can also be found in Morina et al. (Citation2018). We reviewed available epidemiological research on prevalences of PTSD and MD in adult civilian survivors of war who stayed in war-afflicted regions by means of a systematic research and meta-analysis. We located relevant epidemiological studies conducted in war-effected countries in Medline, PsycINFO and PILOTS (PILOTS is managed by the USA National Center for PTSD). The search was conducted in September 2017 in titles, abstracts and key concepts using terms relating to PTSD, major depression, general mental health and war survivors. Studies meeting the following criteria were selected for the meta-analysis: (a) a sample size of at least 50 participants who were living in the area of former conflict at the time the survey was conducted; (b) participants had experienced war-related events within 25 years prior to conducting the survey; (c) at least 80% of the participants were older than 18 years; and (d) PTSD and/or MD was measured with a structured psychiatric interview based on the Diagnostic and Statistical Manuals of Mental Disorders or International Classification of Diseases criteria for these conditions (American Psychiatric Association [APA], Citation1980, 1994, 2013; World Health Organization [WHO], Citation1992). Surveys were excluded if the studied population were not representative of the general population (e.g. subgroup of participants who had all received mental health interventions or subgroups like combatants in armed forces or refugees). For the same reason, surveys carried out with Israeli samples were excluded as they usually involved a small group of the population who were exposed to specific terrorist attacks. If a publication reported on more than one sample because the study was carried out in more than one country or with different groups of war survivors, the samples were treated as distinct. For the purpose of the current publication, we added an additional inclusion criterion to the meta-analysis conducted by Morina et al. (Citation2018), namely that surveys had to utilize a random sampling procedure from the general population to allow for an extrapolation on general populations. We conducted random effects meta-analyses to generate pooled prevalence estimates for depression and PTSD using MetaXL version 2.0 (EpiGear, QLD, Australia).
2.3. Population estimates
National population estimates relied on United Nations data for the year 2015 conducted by the Population Division of the Department of Economic and Social Affairs (DESA) of the United Nations Secretariat (UN, Citation2018). As stated above, geo-referenced data of the UCDP was utilized to analyse whether a respective war was spread out across an entire country or took place only in a certain region of a country (e.g. province). When a war was clearly regional rather than national, regional population estimates were taken from Wikipedia instead of DESA as the latter does not offer regional population estimates. Research indicates that Wikipedia is a reliable source in this respect (Anthony, Smith, & Williamson, Citation2009). Finally, regional population estimates taken from Wikipedia were multiplied with the percentage of individuals equal and above the age of 18, as given by the UN (Citation2018). This last step was necessary, as the Wikipedia estimates do not include age groups whereas DESA estimates do. Our time span was limited to the year of 2015 as UN population estimates including the necessary age ranges (i.e. 0–17 and 18+) were only available for the year 2015. In line with our original aim, we first report the total population size, number of adults and number of people estimated to suffer from PTSD and/or MD for all countries listed by the UCDP as countries with a recent or ongoing history of war.
3. Results
3.1. Prevalences of MD and PTSD
Two raters independently rated the quality of the included trials. This was done by developing a scale tailored to the particular requirements for the current review following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines and based on previous literature (Sanderson, Tatt, & Higgins, Citation2007; Von Elm et al., Citation2007, Citation2014). As all but one study (Alhasnawi et al., Citation2009) reported point prevalences, only studies reporting point prevalences were entered. Overall, 24 and 15 epidemiological surveys met inclusion criteria that measured PTSD and MD, respectively. Taken together, 14,718 war survivors from 14 countries/regions (including Palestine) from three continents were assessed in epidemiological surveys focusing on PTSD and 9272 war survivors from eight countries and three continents were assessed in epidemiological surveys focusing on MD. In the surveys assessing PTSD, participation rate (i.e. study participants/potential participants) was higher than 70% in 83.3% of the samples. With regards to MD, participation rate was higher than 70% in 73.3% of the samples. All but two surveys reported that the interviewers were trained in assessing PTSD and/or MD. All instruments used to diagnose PTSD and/or MD had originally been developed in English and subsequently translated into the language of study participants. However, none of the authors reported the psychometric properties of the translated instruments used to assess PTSD and/or MD. The most frequently used diagnostic interview for both PTSD and MD was the MINI International Neuropsychiatric Interview (Sheehan et al., Citation1998). A basic description of the included surveys is provided in and prevalences for all included surveys are depicted in the forest plots for PTSD and MD (see and ). Utilizing a random effects model, we found that 23.81% of adult war survivors met diagnostic criteria for PTSD (95% CI, 19.54–28.35%) and 23.37% for MD (95% CI, 19.68–27.27%). Of these, 48.99% met criteria for comorbid PTSD and MD (95% CI, 30.29–67.83%). We utilized these percentages as a meta-analytically informed reference for the planned extrapolation.
Table 1. Characteristics of included studies in the meta-analysis.
3.2. Extrapolated prevalence estimates of global war survivors suffering MD and/or PTSD in absolute numbers
Global estimates of absolute numbers of war survivors with PTSD, MD or PTSD+MD per war-country/region are depicted in . In three countries, wars were clearly regional rather than statewide. These took place in India (five regions), the Russian Federation (one region) and Ukraine (five regions). In the case of India, war took place in the five provinces of Kashmir, Punjab, Nagaland, Assam and Manipur. The population size is distributed as follows: Punjab = 27,743,338; Nagaland = 1,980,602; Kashmir = 12,541,302; Assam = 31,169,272; Manipur = 2,721,756. Nationally, 66% of Indians were 18 years old or above in 2015. Based on this proportion, we estimated that 50,263,138 inhabitants in the given five war regions were adult war survivors in 2015. In Ukraine, warfare took place in five provinces of Eastern Ukraine, namely Donetsk (4,403,178 inhabitants), Kharkiv (2,742,180 inhabitants), Luhansk (2,272,676 inhabitants), Zaporizhia (1,791,668 inhabitants) and Dnipropetrovsk (3,320,299 inhabitants). Based on the national proportion of 82.2% adults, we estimated that 11,943,661 adult war survivors lived in the given five regions in 2015. In the Russian Federation, war took place in Chechnya with a population of 1,395,678. Based on the national proportion of 79.9% adults, we estimated 1,115,147 adult war survivors living in Chechnya in 2015. Since no population estimates were available for Kosovo in the UN database, we also took this population estimate from Wikipedia with 1,920,079 inhabitants in total and 1,555,264 adults (i.e. 81%). Overall, wars took place in the territory of 47 countries between 1989 and 2015. presents a world map with all countries or regions marked that have a war history during these 26 years. Presented data and estimations for countries in which at least one of the included surveys were conducted are presented with bold font whereas normal font indicates that no survey was available.
Table 2. Prevalence estimates of PTSD and MD in absolute numbers for countries/regions with a recent or ongoing history of war (between 1989 and 2015).
For the reference year 2015, we estimate that globally 1,471,401,246 individuals were still alive who experienced war between 1989 and 2015. Of this global population estimate of war survivors, 1,017,887,545 (i.e. about 70%) were adults and the remaining 432,146,933 children and adolescents in 2015. These about 1.45 billion living estimated war survivors in 2015 represented about 19.6% of the whole world population. In other words, we estimate that a little less than one in five individuals on the planet in 2015 experienced war between 1989 and 2015. Similarly, the estimated approximately one billion adult war survivors represented about 20% of the global adult population, and the approximately 0.4 billion children about 18.9% of the global population of children and adolescents. Based on the meta-analytically informed overall prevalence of 23.81% for PTSD (95% CI, 19.54–28.35%) and 23.37% for MD (95% CI, 19.68–27.27%), about 242 million adult war survivors residing in (post-)war regions are estimated to suffer from PTSD (95% CI, 198,895,226–288,571,119) and about another 238 million adult survivors of war from MD (95% CI, 200,320,269–277,577,934). Based on the reported comorbidity rate of 48.99% (95% CI, 30.29–67.83%), about 117 million war survivors are estimated to suffer from both conditions (95% CI, 72,053,949–161,354,221), leaving about 126 million people suffering from PTSD exclusively and another approximately 121 million people suffering from MD exclusively. Accordingly, about 354 million adult war survivors are estimated to suffer from PTSD and/or MD.
4. Discussion/conclusion
From the approximate five billion adults worldwide in 2015, we estimate that about one billion, or about one in five, were residing in a country or region that has been directly affected by war between 1989 and 2015. Our findings suggest that 354 million adult war survivors suffer from PTSD and/or MD and, of these, about 117 million suffer from both conditions.
4.1. Comparison with the literature
Our findings are in line with the meta-analysis conducted by Steel et al. (Citation2009) who reported that about 30% of populations exposed to mass conflict and displacement suffer from PTSD and/or MD. Steel et al. (Citation2009) based their results on surveys conducted with selected populations that had undergone specific war events (e.g. torture) and most of the included samples were refugees. These results cannot directly inform estimates of mental disorders in the general population in post-war regions. Hence, the studies included in our meta-analysis are likely to better capture prevalences for whole regions with a recent war history.
4.2. Strengths and limitation
To our knowledge, this is the first publication to provide estimates of absolute numbers of war survivors with PTSD and/or MD. For this purpose, we included only surveys that applied a randomized procedure to collect data in the general population and a valid psychiatric interview to diagnose the disorders in question. However, our paper has several limitations. First, the number of the available surveys that met our inclusion criteria was rather limited. Our estimates involving 1 billion adults living in (post-)conflict regions are based on only 24 surveys assessing PTSD that included 14,718 participants from 14 countries/regions (including Palestine) and 15 surveys assessing MD that included 9272 participants from eight countries. Overall, we were able to include random samples from 14 countries/regions only (lines in bold font in ). The reader will notice that only 13 lines are presented in bolt font in . This concerns the fact that Palestinians reside in several regions across several countries and hence could not be categorized. The overall slim evidence base in this field of research reminds us that our findings must be interpreted with caution until more research has been conducted.
Another major limitation of the present review concerns variability in trauma exposure on a country as well as subpopulation level. We relied on the definition of the UCDP to define war but, naturally, war is not a categorical phenomenon as the definition may imply. The duration of war as well as the intensity (e.g. number of casualties, committed war crimes, etc.) may vary considerably across countries. However, our analysis could not account for such country-based differences. Also, on a subpopulation level, different individuals may have been exposed to different war-related events. We have tried to adjust for this problem by dividing into nationwide/widespread wars and local/regional wars. However, this categorical approach can again be criticized for lacking specificity. Nevertheless, we would like to emphasize that our meta-analysis was based on surveys that utilized a random sampling procedure and were conducted in the general population. By definition, this included individuals with different levels of exposure to war-related events. Accordingly, such surveys offered mean prevalences of PTSD and depression in the general population. Furthermore, we report mean prevalences of PTSD and depression across countries and results yielded narrow confidence intervals for both PTSD and MD (i.e. 95% CI of 19.54–28.35% and 19.68–27.27%, respectively). The narrow confidence intervals point towards a similarly high prevalence across the included samples/countries despite the lack in adjusting for variability in conflict length and intensity on a country and subpopulation level. Another limitation is that samples from Kosovo and Rwanda are overrepresented in the available literature. This is crucial as the prevalences from war survivors from these countries may skew the results of the meta-analysis. A further issue to consider is that all instruments had been translated from English into the spoken language of the participants. While they possess good psychometric properties in English, none of the included surveys reported psychometric cross-validation of the translated instruments. As such, the missing psychometric validation presents a main methodological limitation in this field of research.
While PTSD is trauma-related per definition, MD is not necessarily. MD is the most prevalent mental disorder across countries (Ferrari et al., Citation2013). As such, the high MD prevalence reported in this paper may or may not be directly associated with exposure to and consequences of war events. While exposure to war-related events and the consequences of these events can play a causal role in the aetiology of MD, other influential variables (i.e. other pre-war and post-war stressors) may also lead to the development and maintenance of depression.
Crucially, we were not able to control for the frequency and duration of exposure to other types of trauma. Neither can we expect that frequency and duration of non-war-related trauma types are equally distributed across countries around the world. Hence, we cannot preclude the hypothesis that other trauma types may be more prevalent in countries with a recent or ongoing history of war, compared to countries without recent history of conflict, and that the increased prevalence may boil down to the exposure to different trauma types rather than the postulated war-related traumas (i.e. third variable problem). Kessler et al. (Citation2017) concluded from their analysis of the WHO World Mental Health Surveys that the most common trauma-exposures globally are witnessing or discovering death or serious injury (35.7% of respondents) followed by traumas involving accidents (34.3% of respondents), unexpected death of a loved one (31.4% of respondents), physical violence (22.9% of respondents), intimate partner sexual violence (14% of respondents), war trauma (13.1% of respondents) and ‘other’ traumas (8.4% of respondents). As such, literature suggests that war-related traumas, globally speaking, are a rather uncommon trauma type compared to the other trauma types that people may experience. However, it should be noted that conclusions by Kessler et al. were mainly limited to data from countries without a war history between 1989 and 2015. In fact, they included data from only three of the countries that the UCDP lists as countries with a war history between 1989 and 2015, namely Colombia, Nigeria and Peru. They also reported data from Ukraine, which, however, were collected in 2002 (i.e. before the recent war had started). Hence, it remains speculative whether the pooled data analysed by Kessler et al. and their conclusions based on these data are representative for countries with a recent history of war.
Furthermore, the definition of trauma type is crucial. In their article, Kessler et al. subdivided war trauma into the following categories: combat experience, purposefully injured/killed someone, saw atrocities, being a relief worker or peacekeeper, being a civilian in war zone, being a civilian in a region of terror, and being forcefully displaced (i.e. a refugee). Arguably, this list is not exhaustive and lines between the trauma types are blurred. For instance, rape is categorized as a subcategory of ‘intimate partner or sexual violence’ in Kessler et al.’s analyses. However, war atrocities such as mass rapes show that rape in a war context may be conceptualized as war-related trauma rather than ‘intimate partner or sexual violence’ (see Kuwert et al., Citation2010; Silove, Citation1999).
Kessler et al. (Citation2017) also report that war-trauma is associated with a higher risk of developing PTSD (3.5%) compared to, for instance, physical violence (2.8%) or accidents (2%), but associated with less risk compared to intimate partner or sexual violence (11.4%) or unexpected death of a loved one (5.4%). These data in particular suggest the possibility that the increased prevalence rates reported in the present analysis are not simply due to war-related traumas, but to other forms of traumatization, such as intimate interpersonal traumas. Again, the lacking data from countries with a recent war history in their analyses do not allow for a generalization and hence this statement remains speculative.
We would also like to stress that, apart from the degree of exposure and differences in exposure levels, the cultural and socioeconomic profile of a country relates to the risk of developing trauma-related mental health disorders and thus to country-level prevalence rates. For instance, Burri and Maercker (Citation2014) noted that, apart from country-specific trauma rates during World War II as a significant predictor of country-level PTSD prevalence, the cultural value orientation of ‘stimulation’, which they conceptualized as a cultural orientation towards modern values, as opposed to traditional values, was related to higher country-level PTSD prevalences. Since their results are specific to European countries in the aftermath of World War II, we cannot simply translate these findings to different cultural- and war-contexts of the countries included in our analysis. Yet their findings indicate that, next to trauma exposure, culture-specific factors may also explain differences in prevalence rates. As we did not account for cultural differences, this should be regarded as another limitation of the present analysis.
On this note, Dückers, Alisic, and Brewin (Citation2016) verified the positive relation between trauma exposure and country-level PTSD prevalence. However, paradoxically they also found a negative relationship between a country’s overall cultural and socioeconomic vulnerability to adversity and a country’s PTSD prevalence. Trauma exposure and the country’s cultural and socioeconomic vulnerability, together with the interaction between the two, explained about 75% of the variance in country-level PTSD prevalence. The population samples included in our study did not allow us to corroborate these results. It should be pointed out that, similar to Kessler et al. (Citation2017), Dückers et al. (Citation2016) included data mainly from middle-to-upper and high income countries and only data from six of the 47 countries with a war history between 1989 and 2015 (i.e. Nigeria, Israel, Colombia, Iraq, Lebanon and Ukraine). Again, the included data might not be representative for low-to-middle income countries (LMICs) with a recent war history and therefore conclusions from their study may not apply globally. The included surveys in our review did not enable us to control for the cultural and socioeconomic profile of a country and the relation to PTSD prevalence and persistence.
Furthermore, the included surveys did not systematically report prevalences by gender, which is another limitation in the current analysis. However, this was reported by Priebe et al. (Citation2010) in relation to the five countries of former Yugoslavia that were surveyed in their project. The findings of this study revealed that women had higher prevalences of both PTSD and depression in four of the surveyed countries, whereas the sample from Croatia did not report any significant gender difference. Similarly, the included studies did not systematically report on the relationship between age and prevalences of PTSD and depression. Again, this was mentioned in the publication by Priebe et al. (Citation2010) who reported that older age (i.e. defined as being older than 40 years old) was associated with higher prevalences of both PTSD and depression on all of the five surveyed countries.
4.3. Implications and conclusions
PTSD and MD in war-afflicted societies have to be prioritized as a serious global health issue. To improve estimates of mental disorders, and perhaps more importantly to assess factors associated with the maintenance of and recovery from mental disorders, randomized surveys conducted in post-war societies applying empirically validated measurements are required. Furthermore, longitudinal research is crucial to better capture the course of mental disorders, which might fluctuate over time. This notion directly relates to the extent of accuracy of our findings. Theoretically, one can expect rates of PTSD and MD to decline over time in populations with no current open conflict. However, research indicates that PTSD, if left untreated, has a rather chronic course (Morina et al., Citation2014). This notion is supported by the fact that 10 of the included samples were assessed at least 10 years after the respective war ended and the prevalences of PTSD and/or MD were still high (see ). Kessler et al. (Citation2017) report that war-related trauma is associated with a slower speed of PTSD-remission compared to other trauma types such as intimate partner violence, sexual violence or accidents in the first six years after traumatization, with war-related trauma victims being the subgroup with the least PTSD-remissions by far (see in their article). However, at about six years after traumatization, Kessler et al. report a steep increase in PTSD-remission rates resulting in better remission rates compared to physical violence, intimate partner or sexual violence, and other traumas. After about 10 years, about 90% of those initially with war-trauma-related PTSD did not meet criteria for this condition anymore. However, one limitation regarding the study by Kessler et al. is that we cannot conclude whether remission from PTSD at a certain point translates into recovery from this disorder. This conclusion might only result from longitudinal surveys with repeated measurements for a long period of time. As mentioned before, we have included 10 epidemiological surveys that were assessed at least 10 years after war exposure and yet these surveys report PTSD and MD prevalences way above 10%. One reason for this difference in figures could be different data sources. Again, Kessler et al. mainly included data from middle-to-upper and high-income countries and were only able to include data from three countries with a recent war history in their analyses. As such, their PTSD-remission curve may not apply to the war-afflicted LMICs context. There is a lack of research on the course of PTSD or depression among war survivors living in LMICs. However, a follow-up study by Priebe et al. (Citation2013) indicates that there might be a fluctuating course of PTSD symptoms over time. In this study, about a third of 522 war survivors who had initially reported PTSD did not meet criteria for this disorder a year later. One implication is therefore that our averaged prevalence of PTSD might possibly decline over time. Besides the mentioned research implications, the findings call for more clinical efforts to develop feasible interventions in LMICs-contexts to address the large number of survivors of mass violence who are in need of mental health services (Morina, Malek, Nickerson, & Bryant, Citation2017).
Figure 2. Forest plot depicting meta-analytic results of all representative surveys assessing MD in countries with a history of war between 1989 and 2015.
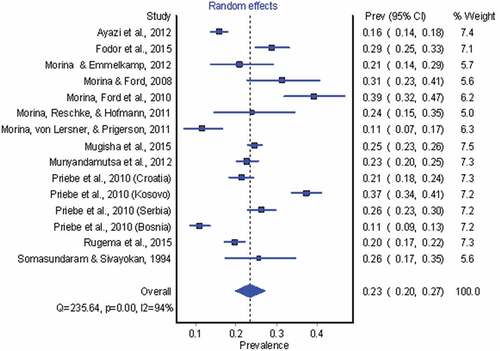
Figure 3. World map with countries and regions marked which have a history of at least one war between 1989 and 2015.

Based on the slim available evidence base, it is estimated that globally about 354 million adult survivors of war suffer from PTSD and/or MD, of which about 117 million are estimated to suffer from comorbid PTSD and MD. More randomized surveys with longitudinal assessments of mental health conditions in general population samples utilizing (cross-)validated measures are necessary to evaluate the accuracy of the estimates reported here. Most countries with a recent or ongoing history of war are LMICs with limited resources to handle the vast PTSD and MD burden at hand. We would like to encourage the development of feasible solutions for treatment purposes as well as international collaborations for war prevention.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Alhasnawi, S., Sadik, S., Rasheed, M., Baban, A., Al-Alak, M. M., Othman, A. Y., … Murthy, S. (2009). The prevalence and correlates of DSM-IV disorders in the Iraq Mental Health Survey (IMHS). World Psychiatry, 8(2), 97–12.
- Anthony, D., Smith, S. W., & Williamson, T. (2009). Reputation and reliability in collective goods: The case of the online encyclopedia Wikipedia. Rationality and Society, 21(3), 283–306.
- APA. (1980, 1994, 2013). Diagnostic and statistical manual of mental disorders III-5. Washington, DC: American Psychiatric Association.
- Ayazi, T., Lien, L., Eide, A. H., Ruom, M. M., & Hauff, E. (2012). What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? A cross-sectional community study in South Sudan. BioMed Central Psychiatry, 12(1), e175.
- Betancourt, T. S., Brennan, R. T., Vinck, P., VanderWeele, T. J., Spencer-Walters, D., Jeong, J., … Pham P. (2016). Associations between mental health and ebola-related health behaviors: A regionally representative cross-sectional survey in post-conflict Sierra Leone. Public Library of Science Medicine, 13(8), e1002073.
- Burri, A., & Maercker, A. (2014). Differences in prevalence rates of PTSD in various European countries explained by war exposure, other trauma and cultural value orientation. BioMed Central Research Notes, 7(1), e407.
- Canetti, D., Galea, S., Hall, B. J., Johnson, R. J., Palmieri, P. A., & Hobfoll, S. E. (2010). Exposure to prolonged socio-political conflict and the risk of PTSD and depression among Palestinians. Psychiatry, 73(3), 219–231.
- Collins, P. Y., Patel, V., Joestl, S. S., March, D., Insel, T. R., & Daar, A. S. (2011). Grand challenges in global mental health. Nature, 475(7354), 27–30.
- De Jong, J. T., Komproe, I. H., Van Ommeren, M., El Masri, M., Araya, M., Khaled, N., … Somasundaram, D. (2001). Lifetime events and posttraumatic stress disorder in 4 postconflict settings. Journal of the American Medical Association, 286(5), 555–562.
- Dückers, M. L., Alisic, E., & Brewin, C. R. (2016). A vulnerability paradox in the cross-national prevalence of post-traumatic stress disorder. The British Journal of Psychiatry, 209(4), 300–305.
- Eytan, A., Gex-Fabry, M., Toscani, L., Deroo, L., Loutan, L., & Bovier, P. A. (2004). Determinants of postconflict symptoms in Albanian Kosovars. The Journal of Nervous and Mental Disease, 192(10), 664–671. doi: 00005053-200410000-00004
- Ferrari, A. J., Somerville, A. J., Baxter, A. J., Norman, R., Patten, S. B., Vos, T., & Whiteford, H. A. (2013). Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychological Medicine, 43(3), 471–481.
- Fodor, K. E., Pozen, J., Ntaganira, J., Sezibera, V., & Neugebauer, R. (2015). The factor structure of posttraumatic stress disorder symptoms among Rwandans exposed to the 1994 genocide: A confirmatory factor analytic study using the PCL-C. Journal of Anxiety Disorders, 32, 8–16.
- Johnson, K., Asher, J., Rosborough, S., Raja, A., Panjabi, R., Beadling, C., & Lawry, L. (2008). Association of combatant status and sexual violence with health and mental health outcomes in postconflict Liberia. Journal of the American Medical Association, 300(6), 676–690.
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Florescu, S. (2017). Trauma and PTSD in the WHO World Mental Health surveys. European Journal of Psychotraumatology, 8, 1–16.
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Chatterji, S., Lee, S., Ormel, J., … Wang, P. S. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiology and Psychiatric Sciences, 18(1), 23–33.
- Kuwert, P., Klauer, T., Eichhorn, S., Grundke, E., Dudeck, M., Schomerus, G., & Freyberger, H. J. (2010). Trauma and current posttraumatic stress symptoms in elderly German women who experienced wartime rapes in 1945. The Journal of Nervous and Mental Disease, 198(6), 450–451.
- Marshall, M. G., & Cole, B. R. (2009). Global report 2009: Conflict, governance, and state fragility. Vienna: Center for Systemic Peace.
- Mathers, C. D., & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. Public Library of Science Medicine, 3(11), e442.
- Morina, N., & Emmelkamp, P. M. (2012). Mental health outcomes of widowed and married mothers after war. British Journal of Psychiatry, 200(2), 158–159.
- Morina, N., & Ford, J. D. (2008). Complex sequelae of psychological trauma among Kosovar civilian war victims. International Journal of Social, 54(5), 425–436.
- Morina, N., Ford, J. D., Risch, A. K., Morina, B., & Stangier, U. (2010). Somatic distress among Kosovar civilian war survivors: Relationship to trauma exposure and the mediating role of experiential avoidance. Social Psychiatry and Psychiatric Epidemiology, 45(12), 1167–1177.
- Morina, N., Malek, M., Nickerson, A., & Bryant, R. A. (2017). Meta-analysis of interventions for posttraumatic stress disorder and depression in adult survivors of mass violence in low- and middle-income countries. Depression and Anxiety, 34(8), 679–691.
- Morina, N., Reschke, K., & Hofmann, S. G. (2011). Long-term outcomes of war-related death of family members in Kosovar civilian war survivors. Death Studies, 35(4), 365–372.
- Morina, N., Stam, K., Pollet, T. V., & Priebe, S. (2018). Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. Journal of Affective Disorders, 239, 328–338.
- Morina, N., Stangier, U., & Risch, A. K. (2008). Experiential avoidance in civilian war survivors with current versus recovered posttraumatic stress disorder: A pilot study. Behaviour Change, 25(1), 15–22.
- Morina, N., Von Lersner, U., & Prigerson, H. G. (2011). War and bereavement: Consequences for mental and physical distress. Public Library of Science One, 6(7), e22140.
- Morina, N., Wicherts, J. M., Lobbrecht, J., & Priebe, S. (2014). Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clinical Psychology Review, 34(3), 249–255.
- Mugisha, J., Muyinda, H., Malamba, S., & Kinyanda, E. (2015). Major depressive disorder seven years after the conflict in northern Uganda: Burden, risk factors and impact on outcomes (The Wayo-Nero Study). BioMed Central Psychiatry, 15(1), e48.
- Munyandamutsa, N., Nkubamugisha, P. M., Gex-Fabry, M., & Eytan, A. (2012). Mental and physical health in Rwanda 14 years after the genocide. Social Psychiatry and Psychiatric Epidemiology, 47(11), 1753–1761.
- Murray, C. J., & Lopez, A. D. (1996). The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Boston: Harvard School of Public Health.
- Nemeroff, C. B., Bremner, J. D., Foa, E. B., Mayberg, H. S., North, C. S., & Stein, M. B. (2006). Posttraumatic stress disorder: A state-of-the-science review. Journal of Psychiatric Research, 40(1), 1–21.
- Pettersson, T., & Wallensteen, P. (2015). Armed conflicts, 1946–2014. Journal of Peace Research, 52(4), 536–550.
- Priebe, S., Bogic, M., Ajdukovic, D., Franciskovic, T., Galeazzi, G. M., Kucukalic, A., … Schützwohl, M. (2010). Mental disorders following war in the Balkans: A study in 5 countries. Archives of General Psychiatry, 67(5), 518–528.
- Priebe, S., Gavrilovic, J., Bremner, S., Ajdukovic, D., Franciskovic, T., Neri, G., … Schützwohl, M. (2013). Course of post-traumatic stress disorder following war in the Balkans: 1-year follow-up study. Psychological Medicine, 43(9), 1837–1847.
- Rieder, H., & Elbert, T. (2013). Rwanda–Lasting imprints of a genocide: Trauma, mental health and psychosocial conditions in survivors, former prisoners and their children. Conflict and Health, 7(1), e6.
- Rugema, L., Mogren, I., Ntaganira, J., & Krantz, G. (2015). Traumatic episodes and mental health effects in young men and women in Rwanda, 17 years after the genocide. British Medical Journal Open, 5(6), e006778.
- Sanderson, S., Tatt, I. D., & Higgins, J. (2007). Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: A systematic review and annotated bibliography. International Journal of Epidemiology, 36(3), 666–676.
- Schaal, S., Dusingizemungu, J. P., Jacob, N., & Elbert, T. (2011). Rates of trauma spectrum disorders and risks of posttraumatic stress disorder in a sample of orphaned and widowed genocide survivors. European Journal of Psychotraumatology, 2(1), e6343.
- Sheehan, D., Lecrubier, Y., Sheehan, K., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59, 22–33; quiz 34–57.
- Silove, D. (1999). The psychosocial effects of torture, mass human rights violations, and refugee trauma: Toward an integrated conceptual framework. The Journal of Nervous and Mental Disease, 187(4), 200–207.
- Somasundaram, D. J., & Sivayokan, S. (1994). War trauma in a civilian population. British Journal of Psychiatry, 165(4), 524–527.
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & Van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. Journal of the American Medical Association, 302(5), 537–549.
- UCDP. (2018). UCDP conflict encyclopedia. Uppsala: Uppsala University.
- UN. (2018, October 31). Population statistics. Retrieved from https://population.un.org/wpp/Download/Standard/Population/
- Veling, W., Hall, B. J., & Joosse, P. (2013). The association between posttraumatic stress symptoms and functional impairment during ongoing conflict in the Democratic Republic of Congo. Journal of Anxiety Disorders, 27(2), 225–230.
- Von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., Vandenbroucke, J. P., & Strobe Initiative. (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Public Library of Science Medicine, 4(10), e296.
- Von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., Vandenbroucke, J. P., & Strobe Initiative. (2014). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. International Journal of Surgery, 12(12), 1495–1499.
- Whiteford, H. A., Ferrari, A. J., Degenhardt, L., Feigin, V., & Vos, T. (2015). The global burden of mental, neurological and substance use disorders: An analysis from the global burden of disease study 2010. Public Library of Science One, 10(2), e0116820.
- WHO. (1992). International classification of diseases (Vol. 10). Geneva: World Health Organization.
- Yasan, A., Saka, G., Ozkan, M., & Ertem, M. (2009). Trauma type, gender, and risk of PTSD in a region within an area of conflict. Journal of Traumatic Stress, 22(6), 663–666.
