ABSTRACT
Background: Domestic violence (DV) is a widespread yet commonly underdetected problem with severe impact on physical and mental health. To date, only limited information is available on prevalence and detection-rates of victims of DV in hospital settings.
Objective: The aim of this study was (a) to assess the prevalence and impact of DV on physical and mental health as well as risk-factors associated with it, (b) to determine how many patients had been asked directly about DV in the hospital and (c) to investigate patients’ preferences about being asked about DV in a hospital setting.
Methods: Adult inpatients and outpatients at seven somatic departments at the University Hospital Innsbruck (Austria) were included consecutively in this ad-hoc, cross-sectional paper-and-pencil questionnaire-based study. In total, n = 2,031 patients were assessed regarding their experiences with DV. They also reported on whether they had been asked about DV at the hospital and whether they would mind being asked about it. To evaluate the impact of DV on patients’ self-reported physical and mental health, odds ratios were calculated using binary logistic regression.
Results: DV was reported by 17.4% of patients, with 4.0% indicating current DV exposure. Lifetime DV exposure was associated with a significant risk for both physical and mental health-problems. Only 4.8% of patients with DV exposure had ever been asked about it by hospital staff. While patients with a history of DV were more open to being asked about DV than patients without DV (78.2% vs. 72.9%), overall acceptance was still high (74%).
Conclusion: DV is a frequently overlooked problem with detrimental effects on physical and mental health. While high acceptance of DV assessment was found, only a small proportion of affected patients had indeed been assessed for DV. Screening for DV in hospitals may thus increase the number of identified patients.
HIGHLIGHTS
• Domestic violence (DV) is a major health concern in healthcare facilities.• DV remains an underdetected issue in the context of hospitals.• Only 4.8% of patients who experienced DV had been asked about DV at the hospital.• Most patients do not mind being asked about DV in a hospital setting.• Acceptance of DV screening was higher among patients with a history of DV.• Screening for DV and specific training for healthcare professionals may improve the detection rate of DV.
Antecedentes: La violencia doméstica es un problema extendido, pero poco detectado, que tiene un impacto severo sobre la salud física y mental. A la fecha, únicamente se encuentra disponible información limitada sobre la prevalencia y tasas de detección de víctimas de violencia doméstica en entornos hospitalarios.
Objetivo: El propósito de este estudio fue de a) determinar la prevalencia y el impacto de la violencia doméstica sobre la salud física y mental, además de los factores de riesgo a ella asociadas, b) determinar a cuántos pacientes se les ha preguntado directamente en el hospital sobre la violencia doméstica, y c) investigar las preferencias de los pacientes sobre el hecho de preguntarles respecto a la violencia doméstica en un entorno hospitalario.
Métodos: Se incluyeron pacientes hospitalizados y ambulatorios de siete departamentos somáticos de la Universidad de Innsbruck (Austria) en este estudio ad-hoc, transversal y basado en un cuestionario resuelto a mano. Se evaluó un total de n = 2031 pacientes respecto a sus experiencias en torno a la violencia doméstica. También reportaron si se les preguntó respecto a la violencia doméstica en el hospital, y si les importaba que se les pregunte sobre ello. Para evaluar el impacto de la violencia doméstica sobre su estado autoreportado de salud física y mental, se calculó la proporción de probabilidades mediante regresión logística binaria.
Resultados: La violencia doméstica fue reportada por el 17,4% de los pacientes, con un 4,0% reportando violencia doméstica en curso. La prevalencia de vida de exposición a la violencia doméstica se asoció con un riesgo significativo de problemas de salud tanto físicos como mentales. El personal del hospital preguntó sobre violencia doméstica solo a un 4,8% de pacientes con exposición a ella. Pese a que los pacientes con antecedente de violencia doméstica eran más abiertos a que se les pregunte sobre ella que los pacientes sin antecedente de violencia doméstica (78,2% contra 72,9%), la aceptación general era aún alta (74%).
Conclusión: La violencia doméstica es un problema con frecuencia ignorado que presenta consecuencias nocivas sobre la salud física y mental. A pesar de que se encontró una alta aceptación para la evaluación de la violencia doméstica, solo a una pequeña proporción de pacientes en efecto se les evaluó respecto la violencia doméstica. Por tanto, un tamizaje sobre violencia doméstica en hospitales podría incrementar el número de pacientes identificados.
背景:家庭暴力(DV)是一个广泛存在但却普遍欠缺检测的问题,会对身心健康造成严重影响。迄今为止,医院中DV受害者的患病率和检出率仅有有限的信息可用。
目的:本研究的目的是:(a)评估DV的流行率、对身心健康的影响以及与之相关的风险因素,(b)确定医院中有多少患者被直接问及了DV相关信息以及(c)调查患者对于在医院中被问及DV的偏好。
方法:奥地利因斯布鲁克大学医院的七个躯体科的成年住院病人和门诊病人被依次纳入这项特定的基于纸笔问卷的横断面研究。总共评估了2031名病人的DV经历。他们还报告了是否曾在医院被问及DV以及是否介意被问到这个问题。为估计DV对病人自评身心健康的影响,采用二元逻辑回归计算了优势比。
结果:17.4%的病人报告经历过DV,4.0%表示目前正在处于DV暴露。终身DV暴露与躯体和精神健康问题的风险均有显著相关。仅有4.8%的DV暴露病人被医院工作人员问及相关信息。虽然有DV史的病人比没有经历过DV的病人更乐于接纳被问及DV(78.2%对72.9%),总体接受度仍然很高(74%)。
结论:DV是一个会对身心健康产生不利影响却经常被忽略的问题。虽然发现了对于DV评估的高度接纳度,但只有一小部分受到DV影响的病人真正地进行了评估。因此,在医院筛查DV也许能够提高确诊病人的数量。
1. Background
Violence within close personal relationships is a common experience worldwide and has severe detrimental effects on physical and psychological health (Campbell, Citation2002; World Health Organization, Citation2013). The terms ‘domestic violence’ (DV) and ‘intimate partner violence’ (IPV) are not clearly separated within scholarly literature and are often used interchangeably [e.g. Campbell (Citation2002); Watts and Zimmerman (Citation2002)]. By definition, IPV focuses on a more narrow field of interpersonal aggressions (i.e. within an intimate partnership) and may thus be considered one major part of the broader concept of DV. DV refers to physical violence and various forms of psychological abuse between adults in a domestic setting, including violence by intimate partners but also by in-laws, parents, children or other household members (WHO, Citation2012). Abusers aim to gain power and control over other individuals and are aware that their behaviour is against the partners’ consent and may be harmful to the abused person (Brzank, Citation2009; Winstok, Citation2016). The lifetime prevalence of IPV among women is estimated to be 30% worldwide, 19–25% in Europe and 21% in North America (Devries et al., Citation2013; FRA, Citation2014; World Health Organization, Citation2013). In a recent population-based study in Austria, 30% of the female cohort reported a lifetime prevalence of physical violence, 40% had experienced psychological violence and 30% sexual violence. Men reported a prevalence of 28% for physical violence, 31% for psychological and 6% for sexual violence (Austrian Institute for Family Studies, Citation2011).
While DV can occur among all socioeconomic, religious and cultural groups (WHO, Citation2012), several ‘risk factors’ for DV victimization have been identified, including gender, socioeconomic status, age and experiences of childhood maltreatment (especially pronounced for polyvictimization, i.e. ≥ 4 types of childhood trauma (Finkelhor, Ormrod, & Turner, Citation2007; Hughes et al., Citation2017)) (Alhabib, Nur, & Jones, Citation2010; Kimber, Adham, Gill, McTavish, & MacMillan, Citation2018; Riedl et al., Citation2019; Rozmann & Ariel, Citation2018). The consequences of violence on patients’ health are manifold; negative consequences are frequently observed even long after the violence has ended (Campbell, Citation2002). Chronic distress through repeated experiences of DV increases the risk for several distress-related symptoms, such as chronic pain, gastrointestinal and cardiovascular symptoms and gynaecological and obstetric problems (Campbell, Citation2002; Riedl et al., Citation2019). Long-term physical health consequences of DV victimization are often strongly associated with long-term mental health consequences (Shen & Kusunoki, Citation2019). Mental health issues may include trauma and stressor-related disorders, eating disorders, insomnia, anxiety disorders, depression and suicidal tendencies as well as addictive disorders (Campbell, Citation2002; Halim et al., Citation2017; Sarkar, Citation2008; Sugg, Citation2015).
A large-scale European study has shown that the majority (~60%) of women affected by DV committed by their current partner look for help in the health system, mostly in hospitals (FRA, Citation2014). An Australian study found that while 85% of those affected by DV look for help in the health system at least five times a year, only 10% of them are actually asked about their experiences of violence (Hegarty et al., Citation2010). Apart from inadequate time resources, physicians often point to feelings of insecurity in regard to this topic and fear of negative emotional reactions as barriers to asking their patients about DV (Sprague et al., Citation2012). Nevertheless, there is evidence that DV screening is feasible and well accepted during routine examinations in general hospitals, especially when conducted in a sensitive, non-judgemental way (Mork, Andersen, & Taket, Citation2014; Phelan, Citation2007; Stockl et al., Citation2013). However, only limited evidence is available, and existing studies have mainly focused on women in specific hospital settings (e.g. antenatal care) (Mork et al., Citation2014). The identification of victims of DV is therefore an important task for healthcare institutions. Yet research indicates that DV remains largely undetected among hospital patients (Brzank & Blattner, Citation2010; Kothari & Rhodes, Citation2006).
The aims of this study were (a) to assess the prevalence of DV in a large mixed sample of hospital patients and to identify risk factors for current DV, (b) to investigate the influence of lifetime DV on patients’ mental and physical health, (c) to find out how many patients had been asked at the hospital about DV and (d) to evaluate patients’ attitudes and preferences about being asked in a hospital context about DV.
2. Methods
2.1. Sample and procedure
This study is a secondary subanalysis of a patient sample collected in a project dealing with the ‘Influence of Violence on the Physical and Psychological Health of Patients in a Hospital Setting’ [for more details, see also Riedl et al. (Citation2019)]. In that cross-sectional observational study, inpatients and outpatients from seven departments at the University Hospital of Innsbruck (Otolaryngology, Trauma Surgery, Neurosurgery, Neurology, Gynaecology, Internal Medicine, Radiology) were included between October 2015 and March 2017. For a period of three months (per department), patients were approached by research associates (trained undergraduate psychology students and medical students) in waiting areas at the hospital. After receiving detailed information about the design and aims of the study, patients were asked to sign an informed consent form and to complete a paper-and-pencil questionnaire in private – wherever possible, in a separate part of the waiting area. Research associates were available to patients for any questions and to assure privacy. All patients received a contact address for professional psychological support free of charge. The study design was approved by the ethics committee of the Medical University of Innsbruck (AN2015-0175 351/4.18).
2.2. Measures
Sociodemographic data included age, gender, family status, living arrangements and education level. Patients were asked about the reason for their hospital visit (open text field) and how many times they had been admitted to the hospital as an inpatient or outpatient during the preceding five years (options: 0–3 times; 4–7 times; 8–10 times; 10–15 times; >15 times).
Additional items included whether patients had been asked about experiences of domestic violence in the hospital (yes/no), followed by a checklist of who had approached them (physicians, nurses, social workers, other). Patients were also asked whether they considered it important to be asked about experiences of violence (yes/no) and who they would want to be asked by (open text field allowing multiple answers).
2.3. Hurt-Insult-Threaten-Scream-Scale (HITS)
DV levels were evaluated using an adapted German version of the Hurt-Insult-Threaten-Scream (HITS) scale (Sherin, Sinacore, Li, Zitter, & Shakil, Citation1998), which consists of four items asking whether the participant was ever (1) screamed at or insulted, (2) threatened, (3) cursed at, talked down to or (4) physically hurt by a partner. The items were answered on a five-point scale: ‘never’ (1), ‘rarely’ (2), ‘sometimes’ (3), ‘fairly often’ (4) and ‘frequently’ (5). The score range was from 4 to 20 points, with higher scores indicating more frequent DV. In accordance with Miszkurka et al. (Miszkurka, Steensma, & Phillips, Citation2016), we chose a weighted cut-off: if patients reported physical violence (item 4) at least ‘rarely’ or psychological violence (items 1–3) at least ‘sometimes’, we considered them DV cases. As many patients also suffer from violence committed by other people living in the same household (e.g. father, mother, sibling, brother-in-law), the HITS instructions were adapted to read ‘your partner or other persons living in the same household’. Furthermore, patients were asked about the time frame of the abuse, i.e. ‘during the last two years’, ‘two to three years ago’, ‘three to five years ago’ and ‘six or more years ago’, with multiple answers possible. In our sample, good internal consistency for the HITS total score (α = .83) was found.
2.3.1. Maltreatment and Abuse Chronology of Exposure Scale (MACE)
Childhood victimization was assessed with the German version of the Maltreatment and Abuse Chronology of Exposure Scale (MACE) [KERF; Isele et al. (Citation2014); Teicher and Parigger (Citation2015)]. It consists of 75 items that retrospectively gauge the severity of exposure to different types of maltreatment, including physical and emotional neglect and abuse, peer-abuse, sexual abuse, and witnessing intrafamilial violence, with specific cut-off values for each scale (Isele et al., Citation2014). In accordance with previous study methodology, patients with values exceeding the cut-offs in four or more categories were considered polyvictimized [see also Riedl et al. (Citation2019)]. The MACE has good test-retest reliability and validity (Isele et al., Citation2014; Teicher & Parigger, Citation2015). The internal consistency of the MACE total score was α = .91 in our sample.
2.3.2. Health checklist (German Pain Questionnaire)
We used a comprehensive self-report list of diseases derived from the German Pain Questionnaire (Association GP, Citation2015) to retrospectively assess lifetime prevalence of disease as rated by patients. The health checklist covered eleven major physical disease clusters (cancer; cardiovascular diseases; neurological disorders; gastrointestinal diseases; metabolic diseases; musculoskeletal disorders; urogenital diseases; respiratory diseases; skin diseases; chronic pain; gynaecological diseases). For each category, examples of diseases and conditions were given. Patients were asked (yes/no) whether they suffered from each disease cluster and rated associated impairment on a four-point scale from ‘not at all’ (0) to ‘strongly’ (4).
2.3.3. Essener Trauma Inventory (ETI)
To assess trauma-related symptoms, the Essener Trauma Inventory (ETI) was used. The ETI allows the classification of posttraumatic disorders and consists of a trauma checklist (18 dichotomous items) and an assessment of trauma-related symptoms within the preceding month (23 items rated on a four-point Likert scale), followed by five items assessing functional impairment. Based on the trauma-related symptoms, a total score (range: 0 to 69) is calculated, with higher values indicating more trauma-related distress. Values >16 on the ETI total score indicate a clinically relevant level of trauma-related symptoms. Good internal consistency and validity have been reported for the total score (Tagay et al., Citation2007; Tagay & Senf, Citation2014). In our sample, good internal consistency (α = .95) was found.
2.3.4. Brief Symptom Inventory (BSI-18)
Psychological distress was assessed with the Brief Symptom Inventory (BSI-18) (Franke et al., Citation2017), consisting of 18 items rated on a four-point Likert scale (from ‘not at all’ to ‘very often’). Three subscale scores (depression, anxiety, somatization) and a global score can be computed to measure global psychological distress. In this study, only the depression and anxiety scales were used as the BSI-18’s somatization items show a significant overlap with symptoms strongly associated with several physical diseases. Good reliability and validity for the subscales and total score have been reported (Franke et al., Citation2017; Spitzer et al., Citation2011). In our sample, good internal consistency was found for the BSI total score (α = .89) as well as for the anxiety (α = .80) and depression (α = .85) subscales.
2.4. Statistical procedures
Analyses were limited to individuals with complete data relating to DV, age and sex. Group differences were analysed using chi-square tests for nominal data, Man-Whitney U tests for ordinal data, and independent sample t-tests, analysis of variance (ANOVA) and Pearson correlation coefficients for continuous data. The size of the group difference in the ANOVAs was evaluated using partial η2. Effect sizes of η2 = 0.01 were considered small, η2 = 0.06 medium and η2 = 0.14 large (Ellis, Citation2010).
To investigate factors influencing the odds for current DV, binary logistic regression analyses (backward elimination method, likelihood-ratio test) were calculated. Predictors included sociodemographic variables (age, sex, education level, relationship status, number of children, living environment, disability and history of childhood vicitimization) and hospital-related variables (inpatient vs. outpatient, frequency of visits as an inpatient or outpatient over the preceding five years). The same set of variables and the dichotomous variable DV were used to determine which parameters predicted whether patients had actually been asked about DV at the hospital. Odds ratios (OR) are presented with 95% confidence intervals.
The association between lifetime DV, childhood victimization and current psychological symptoms or number of physical symptoms was investigated through calculation of univariate ANOVAS. An interaction term of childhood polyvictimization (i.e. ≥ 4 types of childhood trauma) * DV timeframe was entered as an independent variable, with age and gender as covariates and the ETI total score and BSI depression and anxiety values as dependent variables. To allow sufficiently large and balanced subgroups, the timeframes for DV were pooled into three groups (i.e. ‘current’, ‘two to five years ago’, ‘six or more years ago’). P-values < .05 (two-sided) were considered statistically significant. All statistical analyses were performed with IBM SPSS (v22.0).
3. Results
3.1. Sociodemographic data
Of all the patients approached (n = 2629), 84.2% (n = 2214) were willing to participate in the study. The primary reasons for non-participation were lack of interest, not having enough time or finding the questionnaire too long. For some patients, the topic of the study was too personal. Individuals with missing data relating to DV, age or sex (n = 183) were excluded from the analyses, resulting in a final sample of n = 2031 patients with complete data sets.
The mean age of the total sample was 43.1 years, and 54.1% were female. Most of the patients were married or in a long-term relationship, more than half were living with their partner and/or children, and about 52% were parents. Approximately half of the patients had higher education or a university degree. Most patients in our sample were being treated as outpatients (85.9%) at the time. For details, see .
Table 1. Sociodemographic data for patients with and without DV.
3.2. Prevalence of DV and risk factors for DV
Mean HITS value for the sample was 5.1 (SD: 2.2; range: 4 to 20). Lifetime prevalence of DV in the total sample was 17.4% (n = 353), of which 30% (n = 106) reported physical and psychological violence, 49% exclusively psychological violence (n = 175) and 21% exclusively physical violence (n = 73). With respect to violence committed by intimate partners (IPV), no statistically significant gender difference was found (women: 35.1%; men: 28.1%; χ2 = 1.89; p = .20).
Prevalence of current DV (i.e. within the preceding two years) was 4.0% (n = 82). Another 7.7% (n = 156) reported DV within the preceding two to five years and 6.6% (n = 134) six or more years earlier. No significant difference in lifetime DV was found between women and men (18.8% vs. 15.7%; p = .06). A substantial proportion (44.2%) of patients with DV reported having children.
The most frequently cited perpetrators of DV were intimate partners (32.3%), (step-)fathers (29.4%) and mothers (23.3%). Other frequently named perpetrators were siblings (13.3%) and the patient’s own children (6.9%). Most patients (72.6%) named one single offender, while the remaining 27.4% indicated having been abused by multiple offenders.
Logistic regression analysis showed that patients with a history of childhood polyvictimization were twice as likely (OR: 2.04, 95% CI 1.21–3.42, p = .007) to experience DV currently. Other predictors for current DV included physical disability (OR: 4.0; 95% CI 1.91–8.49; p < .001), being treated as an outpatient (OR: 4.62; 95% CI 1.42–15.15; p = .011) and those with a higher number of children living in the same household (OR: 1.22; 95% CI 1.03–1.44; p = .011). No significant association was found with age, sex, relationship status, frequency of hospital visits, patients’ living environment or level of education (all p > .20).
3.3. Clinical aspects
3.3.1. Physical health
The majority of patients (75.2%) reported one type of the diseases assessed, with 4.3% reporting six or more and 0.9% all eleven disease types. The highest prevalence was found for chronic pain (25.0%), followed by respiratory diseases (16.0%), musculoskeletal disorders (15.9%) and neurological disorders (15.5%). Overall, 14.4% of patients reported being strongly impaired by at least one physical disease, 19.5% at least quite impaired, 23.0% at least a little impaired, and 43.1% did not feel at all impaired by any of their diseases. For details see .
Patients with DV reported significantly higher numbers of physical diseases (t = 4.13, p < .001) and a significantly higher subjective impairment by the respective disease (t = 4.33, p < .001). Additionally, logistic regression analyses showed that patients with DV had a significantly higher risk for chronic pain, gastrointestinal disorders, metabolic diseases, musculoskeletal disorders, gynaecological disorders, respiratory diseases, urogenital disorders, skin diseases and cardiovascular diseases. No significant effects were found for cancer and neurological disorders. For details, see .
Table 2. Clinical data for patients with and without DV.
Table 3. Odds ratios for patients with DV (compared to patients without DV) for physical and mental health.
3.3.2. Mental health
DV was associated with a 3.7-times increased likelihood of suffering from clinically relevant PTSD symptoms as well as a 2.9-times and a 2.4-times increased risk for depression and anxiety, respectively.
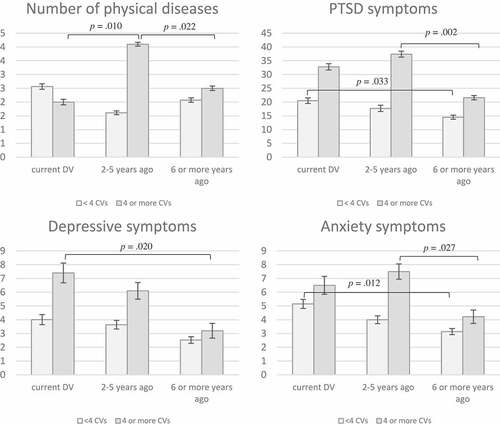
We found a significant interaction between childhood victimization and the trajectories of the number of reported physical diseases (F = 4.04, p < .002, η2 = .08), trauma-related symptoms (F = 8.88, p < .001, η2 = .19), anxiety (F = 4.02, p = .002, η2 = .09) and depression (F = 3.39, p = .006, η2 = .07) over time:
Patients without childhood polyvictimization reported slightly lower values of trauma-related symptoms, anxiety and depression with time since DV. While post-hoc analysis showed no significant differences between the three groups for depression or number of physical diseases (p > .05), mean trauma-related (p = .033) and anxiety symptoms (p = .012) were significantly higher in patients with current DV than in patients with DV six or more years earlier. No other significant group differences were found (p > .05).
For patients with a history of childhood polyvictimization, on the other hand, a significantly higher number of physical diseases was observed in patients two to five years after DV. Additionally, trauma-related symptoms and anxiety increased, even up to five years after DV, and only decreased in the group of patients with DV six or more years earlier, while for depression, a steady decrease with increasing time since DV was found. Post-hoc testing showed a significant difference between patients with DV two to five years earlier and patients with DV six or more years earlier for trauma-related (p = .002) and anxiety (p = .027) symptoms, while for depressive symptoms, a significant difference was found between current DV and DV six or more years earlier (p = .020). As to the reported number of physical diseases, a significantly higher number was observed two to five years after DV, both compared to current DV (p = .010) and to DV six or more years earlier (p = .022). See also .
3.4. Asking patients about experiences of DV
3.4.1. Clinical reality
Across all patients, a total of 4.4% (n = 87) reported having been asked about DV in a hospital setting. Most of the patients asked about DV had been approached by a physician (38.3%) and/or a nurse (22.8%). With regard to current DV, the number of identified victims was particularly low: Only 4.8% of patients (n = 4 out of 82) who reported current DV had been approached by a healthcare professional (see ). Patients with lower levels of education (OR: 1.40; 95% CI 1.10–1.85; p = .008) and patients from urban living environments (OR: 1.87; 95% CI 1.11–3.15) had significantly higher odds of having been asked about DV. No significant association was found for history of childhood victimization, experiences of DV or other sociodemographic parameters. A comparable percentage of men and women had been asked about DV (4.1% vs. 4.6%; p = .62).
3.4.2. Patients’ preferences
When asked whether they found it important to be asked about DV in the context of a hospital visit, most patients (73.9%, n = 1,500) gave affirmative answers. Patients with a history of DV found it significantly more important than patients without DV (78.2% vs. 72.9%, p = .010). Overall, women were more positive about being asked about DV than men (81.9% vs. 70.0%, p < .001). No significant differences were found for education level (U = 286,898,00, p = .443) or age (t = 0.53, p = .596).
A total of 633 patients (31.1%) responded to the question of who they would prefer to be asked about DV by: Most reported that they would prefer to be approached by physicians (67.9%, n = 430), followed by nurses (17.0%, n = 108), psychologists (9.1%, n = 58) and social workers (5.2%, n = 33). An additional 5% had no preference, and 4.1% preferred a confidant. About 10% preferred a female healthcare professional, regardless of her profession.
4. Discussion
The results of the present study show that with a lifetime prevalence of 17.4%, DV is a highly relevant phenomenon among hospital patients. Patients exposed to DV reported significantly worse physical and mental health. Experiences of childhood abuse, having a disability and having a higher number of children were identified as risk factors for current DV. Only a small proportion of affected patients (~5%) had been asked about DV, while the general acceptance of DV assessment was high.
The prevalence rates of current DV in our sample are in line with the results of Brzank, Hellbernd, Maschewsky-Schneider, and Kallischnigg (Citation2005), who reported a prevalence rate of 4.6% for current intimate partner violence (IPV) in a female emergency room patient sample. When compared to epidemiological studies, the lifetime prevalence of 17.4% for psychological or physical DV was significantly lower than previously reported for Europe (women: ~19–25%) (Devries et al., Citation2013; FRA, Citation2014; World Health Organization, Citation2013), which suggests underreporting of DV in our study. Additionally, most prevalence studies have primarily focused on women, while the evidence for male victims of DV is still comparably scarce (Godbout et al., Citation2019). Interestingly, in contrast to previous studies (Kimber et al., Citation2018), we found no significant gender differences for self-reported DV. Recent research has indicated that the extent and directionality of violence among the genders may vary according to the type of relationship. Moreover, due to social stigma prevalence rates among men may be underestimated due to asymmetrical reporting (Rozmann & Ariel, Citation2018). In our sample, men were more reluctant to being asked about DV, which points to an enduring social taboo or stigma. Overstreet and Quinn (Citation2013) have described various types of stigma (i.e. internalized stigmata, such as self-blame, anticipated stigmata and cultural stigmata) that may hamper DV reporting. It is encouraging, however, that in our sample as many men as women had been asked about experiences of DV.
We identified specific risk factors for DV in our sample: Patients with disabilities were significantly more at risk of becoming victims of DV, which is also in line with current epidemiological research (Dammeyer & Chapman, Citation2018). Nearly half of patients reporting DV were parents. We may thus assume that in many of those cases, children witness the violence between parents. This is quite alarming as childhood exposure to DV is significantly associated with perpetration (intergenerational transmission of family violence) and DV victimization in adulthood (Kimber et al., Citation2018; Nikulina, Gelin, & Zwilling, Citation2017), which was further supported by our data showing that childhood abuse was a significant risk factor for DV (Kimber et al., Citation2018; Riedl et al., Citation2019).
Experiences of DV were associated with a significantly higher risk for a broad range of physical diseases, including chronic pain, gastrointestinal disorders and gynaecological diseases. This is in accordance with literature closely linking DV to long-lasting health issues, especially chronic pain and gynaecological symptoms (Campbell, Citation2002; Dillon, Hussain, Loxton, & Rahman, Citation2013). Additionally, we observed a significantly increased risk for patients with DV exposure to develop clinically relevant psychological symptoms, with odds ratios ranging from 2.4 for anxiety to 3.7 for the development of PTSD. Thus, this study replicated previous findings linking DV exposure to an increase in trauma-related symptoms, depression and anxiety (Chandan et al., Citation2019; Shen & Kusunoki, Citation2019).
Despite the serious consequences of DV on physical and mental health, affected patients in our sample had been largely underdetected, which is in accordance with previous studies (Daoud et al., Citation2019; Hegarty et al., Citation2010): Only 4.8% of patients with experiences of DV had previously been identified and approached by healthcare professionals or psychosocial staff in the hospital. The results also indicate that the clear majority (~74%) of patients – especially those who were actually affected by DV – want to be approached. Interestingly, patients with lower levels of formal education were significantly more likely to be asked about DV in our sample than patients with higher levels of education, although there was no significant difference in the prevalence of DV between these groups. This may be attributable to the widespread preconception that DV is a greater problem among lower socioeconomic classes or to the fact that healthcare professionals may be more confident to ask patients with lower education levels about DV. In line with previous research (Austrian Institute for Family Studies, Citation2011; FRA, Citation2014), our results indicate that DV is not a problem of a specific socioeconomic class but can be found across all groups in society.
In our study, increased levels of psychological distress and trauma-related symptoms were present not only in patients with current experiences of DV but also in patients who had experienced DV years earlier. This effect was especially pronounced in patients with a history of childhood abuse, which is in accordance with a recent review by Galatzer-Levy et al. (Galatzer-Levy, Huang, & Bonanno, Citation2018). Our results indicate that it is necessary to implement screening procedures in hospitals, focusing not only on current DV but also on the perspective of lifetime violence and childhood maltreatment experienced by patients.
Acceptance of DV assessment was rather good in our sample, especially among patients with DV. This result is in line with several scholars whose findings show that the majority of women at healthcare facilities believe that health professionals should routinely screen for abuse (Caralis & Musialowski, Citation1997; Richardson et al., Citation2002). This indicates that the frequently articulated fear of healthcare professionals of overstepping a boundary when asking patients about DV may be unfounded (Sprague et al., Citation2012). It appears that the underdetection of DV may, in fact, be due to insecurity and defence mechanisms on the part of healthcare professionals or to social stigma (Overstreet & Quinn, Citation2013). To prevent long-term detrimental effects of DV on physical and mental health, early identification of and professional help for patients with DV is a crucial task for healthcare professionals.
Several strengths and limitations of this investigation may be pointed out. One of its strengths is its large sample size: Patients with a wide range of symptoms were taken from various departments, thus yielding a broad and mixed patient sample. To our knowledge, this is the first study to assess patients’ preferences for being asked about DV, the first to assess the clinical reality of dealing with this problem and the first to link results with data on strongly influential factors, such as childhood victimization.
As to limitations of this study, one was the patient-rated assessment of physical health and disease, which is a subjective measure. However, as this approach assesses subjective impairment due to disease, it provides a picture of the health problems that are most important to the individual patient. Moreover, since a cross-sectional, non-interventional study design was applied, no conclusive statements on causality can be made.
Data was collected from patients in the waiting areas of the participating departments, usually with other patients present. Several strategies were applied to guarantee best possible privacy and confidentiality (see methods for details). Yet we cannot rule out the possibility that, due to concerns about privacy, some patients either did not participate or downplayed their experiences. Finally, although we offered translated versions of the questionnaire in the languages of the major immigrant groups in Tyrol, the proportion of immigrants in our sample was small. Aside from the language barrier, sociocultural factors may also have played a role. Future studies should try to include greater cultural diversity in the research team to facilitate better inclusion of non-native speakers.
5. Conclusion
This study is in line with previous research and provides evidence of the detrimental effect of chronic distress on physical and mental health. Our findings strongly suggest that early identification of patients with experiences of DV is crucial so that appropriate psychosocial support can be offered. Although a clear majority of patients did not mind being asked about experiences of DV, only very few actually had been asked. Thus, improvements in staff training appear to be necessary so that healthcare professionals can better identify victims of violence at an early stage and offer them professional help. In order to prevent the continuing cycle of chronic distress, psychological and physical disease, it is essential to sensitize healthcare professionals to better identify patients with DV experience.
Acknowledgments
We thank Emil Chamson for the proofreading and language editing of our manuscript.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Alhabib, S., Nur, U., & Jones, R. (2010). Domestic violence against women: Systematic review of prevalence studies. Journal of Family Violence, 25(4), 369–11.
- Association GP. (2015) German pain questionnaire. Retrieved from https://www.dgss.org/deutscher-schmerzfragebogen/
- Austrian Institute for Family Studies. (2011). Violence in the family and the closer social environment. The Austrian prevalence study of violence towards men and women. Vienna: Author.
- Brzank, P. (2009). (Domestic) violence against women: socioeconomic consequences and societal costs. Introduction and overview. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 52(3), 330–338.
- Brzank, P., & Blattner, B. (2010). Screening for intimate partner violence against women. International discussion, considerations for Germany. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 53(2), 221–232.
- Brzank, P., Hellbernd, H., Maschewsky-Schneider, U., & Kallischnigg, G. (2005). Domestic violence against women and health care demands. Results of a female emergency department patient survey. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 48(3), 337–345.
- Campbell, J. C. (2002). Health consequences of intimate partner violence. Lancet (London, England), 359(9314), 1331–1336.
- Caralis, P. V., & Musialowski, R. (1997). Women’s experiences with domestic violence and their attitudes and expectations regarding medical care of abuse victims. Southern Medical Journal, 90(11), 1075–1080.
- Chandan, J. S., Thomas, T., Bradbury-Jones, C., Russell, R., Bandyopadhyay, S., Nirantharakumar, K., & Taylor, J. (2019). Female survivors of intimate partner violence and risk of depression, anxiety and serious mental illness. The British Journal of Psychiatry: The Journal of Mental Science, 1–6. doi:10.1192/bjp.2019.124
- Dammeyer, J., & Chapman, M. (2018). A national survey on violence and discrimination among people with disabilities. BMC Public Health, 18(1), 355.
- Daoud, N., Berger-Polsky, A., Sergienko, R., O’Campo, P., Leff, R., & Shoham-Vardi, I. (2019). Screening and receiving information for intimate partner violence in healthcare settings: a cross-sectional study of Arab and Jewish women of childbearing age in Israel. BMJ Open, 9(2), e022996.
- Devries, K. M., Mak, J. Y., Garcia-Moreno, C., Petzold, M., Child, J. C., Falder, G., … Watts, C. H. (2013). Global health. The global prevalence of intimate partner violence against women. Science (New York, NY), 340(6140), 1527–1528.
- Dillon, G., Hussain, R., Loxton, D., & Rahman, S. (2013). Mental and Physical health and intimate partner violence against women: A review of the literature. International Journal of Family Medicine, 2013, 313909.
- Ellis, P. D. (2010). The essential guide to effect sizes: Statistical power, meta-analysis, and the interpretation of research results. Cambridge: Cambridge University Press.
- Finkelhor, D., Ormrod, R. K., & Turner, H. A. (2007). Poly-victimization: a neglected component in child victimization. Child Abuse & Neglect, 31(1), 7–26.
- FRA. (2014). Violence against women: A European survey. Vienna: European Union Agency for Fundamental Rights.
- Franke, G. H., Jaeger, S., Glaesmer, H., Barkmann, C., Petrowski, K., & Braehler, E. (2017). Psychometric analysis of the brief symptom inventory 18 (BSI-18) in a representative German sample. BMC Medical Research Methodology, 17(1), 14.
- Galatzer-Levy, I. R., Huang, S. H., & Bonanno, G. A. (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55.
- Godbout, N., Vaillancourt-Morel, M. P., Bigras, N., Briere, J., Hebert, M., Runtz, M., & Sabourin, S. (2019). Intimate partner violence in male survivors of child maltreatment: A meta-analysis. Trauma, Violence & Abuse, 20(1), 99–113.
- Halim, N., Beard, J., Mesic, A., Patel, A., Henderson, D., & Hibberd, P. (2017). Intimate partner violence during pregnancy and perinatal mental disorders in low and lower middle income countries: A systematic review of literature, 1990–2017. Clinical Psychology Review. doi:10.1016/j.cpr.2017.11.004
- Hegarty, K. L., Gunn, J. M., O’Doherty, L. J., Taft, A., Chondros, P., Feder, G., … Brown, S. (2010). Women’s evaluation of abuse and violence care in general practice: a cluster randomised controlled trial (weave). BMC Public Health, 10, 2.
- Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., … Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2(8), e356–e366.
- Isele, D., Teicher, M. H., Ruf-Leuschner, M., Elbert, T., Kolassa, I.-T., Schury, K., & Schauer, M. (2014). KERF—An instrument for measuring adverse childhood experiences: Construction and psychometric evaluation of the German MACE (maltreatment and abuse chronology of exposure) scale. Zeitschrift für Klinische Psychologie und Psychotherapie: Forschung und Praxis, 43(2), 121–130.
- Kimber, M., Adham, S., Gill, S., McTavish, J., & MacMillan, H. L. (2018). The association between child exposure to intimate partner violence (IPV) and perpetration of IPV in adulthood-A systematic review. Child Abuse & Neglect, 76, 273–286.
- Kothari, C. L., & Rhodes, K. V. (2006). Missed opportunities: emergency department visits by police-identified victims of intimate partner violence. Annals of Emergency Medicine, 47(2), 190–199.
- Miszkurka, M., Steensma, C., & Phillips, S. P. (2016). Correlates of partner and family violence among older Canadians: a life-course approach. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice, 36(3), 45–53.
- Mork, T., Andersen, P. T., & Taket, A. (2014). Barriers among Danish women and general practitioners to raising the issue of intimate partner violence in general practice: a qualitative study. BMC Women’s Health, 14, 74.
- Nikulina, V., Gelin, M., & Zwilling, A. (2017). Is there a cumulative association between adverse childhood experiences and intimate partner violence in emerging adulthood? Journal of Interpersonal Violence, 886260517741626. doi:10.1177/0886260517741626
- Overstreet, N. M., & Quinn, D. M. (2013). The intimate partner violence stigmatization model and barriers to help-seeking. Basic and Applied Social Psychology, 35(1), 109–122.
- Phelan, M. B. (2007). Screening for intimate partner violence in medical settings. Trauma, Violence & Abuse, 8(2), 199–213.
- Richardson, J., Coid, J., Petruckevitch, A., Chung, W. S., Moorey, S., & Feder, G. (2002). Identifying domestic violence: cross sectional study in primary care. BMJ (Clinical Research Ed), 324(7332), 274.
- Riedl, D., Beck, T., Exenberger, S., Daniels, J., Dejaco, D., Unterberger, I., & Lampe, A. (2019). Violence from childhood to adulthood: The influence of child victimization and domestic violence on physical health in later life. Journal of Psychosomatic Research, 116, 68–74.
- Rozmann, N., & Ariel, B. (2018). The extent and gender directionality of intimate partner violence in different relationship types: A systematic review and meta-analysis. Partner Abuse, 9(4), 335–361.
- Sarkar, N. N. (2008). The impact of intimate partner violence on women’s reproductive health and pregnancy outcome. Journal of Obstetrics and Gynaecology: the Journal of the Institute of Obstetrics and Gynaecology, 28(3), 266–271.
- Shen, S., & Kusunoki, Y. (2019). Intimate partner violence and psychological distress among emerging adult women: A bidirectional relationship. Journal of Women’s Health, 2002. doi:10.1089/jwh.2018.7405
- Sherin, K. M., Sinacore, J. M., Li, X. Q., Zitter, R. E., & Shakil, A. (1998). HITS: a short domestic violence screening tool for use in a family practice setting. Family Medicine, 30(7), 508–512.
- Spitzer, C., Hammer, S., Lowe, B., Grabe, H. J., Barnow, S., Rose, M., … Franke, G. H. (2011). The short version of the brief symptom inventory (BSI −18): preliminary psychometric properties of the German translation. Fortschritte der Neurologie-Psychiatrie, 79(9), 517–523.
- Sprague, S., Madden, K., Simunovic, N., Godin, K., Pham, N. K., Bhandari, M., & Goslings, J. C. (2012). Barriers to screening for intimate partner violence. Women & Health, 52(6), 587–605.
- Stockl, H., Hertlein, L., Himsl, I., Ditsch, N., Blume, C., Hasbargen, U., … Stockl, D. (2013). Acceptance of routine or case-based inquiry for intimate partner violence: a mixed method study. BMC Pregnancy and Childbirth, 13, 77.
- Sugg, N. (2015). Intimate partner violence: prevalence, health consequences, and intervention. The Medical Clinics of North America, 99(3), 629–649.
- Tagay, S., Erim, Y., Stoelk, B., Möllering, A., Mewes, R., & Senf, W. (2007). The essen trauma-inventory (ETI) – A screening instrument of identification of traumatic events and posttraumatic disorders. ZPPM, 1, 75–89.
- Tagay, S., & Senf, W. (2014). The essen trauma-inventory (ETI) - Manual. Göttingen: Hogrefe.
- Teicher, M. H., & Parigger, A. (2015). The ‘maltreatment and abuse chronology of exposure’ (MACE) scale for the retrospective assessment of abuse and neglect during development. PloS One, 10(2), e0117423–e0117423.
- Watts, C., & Zimmerman, C. (2002). Violence against women: Global scope and magnitude. Lancet (London, England), 359(9313), 1232–1237.
- WHO. (2012). Understanding and addressing violence against women - Intimate partner violence. World Health Organization. Retrieved from http://www.who.int/reproductivehealth/publications/violence/en/index.html
- Winstok, Z. (2016). A new definition of partner violence. Aggression and Violent Behavior, 28, 95–102.
- World Health Organization. (2013). Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: WHO.