ABSTRACT
Background: Major Depressive Disorder (MDD) in adolescence has a high prevalence and risk of disability, but current treatments show limited effectiveness and high drop-out and relapse rates. Although the role of distressing experiences that relate to the development and maintenance of MDD has been recognized for decades, the efficacy of a trauma-focused treatment approach for MDD has hardly been studied.
Objective: To determine the effectiveness of eye movement desensitization and reprocessing (EMDR) therapy as a stand-alone intervention in adolescents diagnosed with MDD. We hypothesized that reprocessing core memories related to the onset and maintenance of MDD using EMDR therapy would be associated with a significant decrease in depressive and comorbid symptoms.
Method: We recruited 32 adolescents (12–18 years) fulfilling DSM-IV criteria for mild to moderate-severe MDD from an outpatient youth mental health care unit. Treatment consisted of six weekly 60-min individual sessions. Presence or absence of MDD classification (ADIS-C), symptoms of depression (CDI), symptoms of posttraumatic stress (UCLA), anxiety (SCARED), somatic complaints (CSI), and overall social-emotional functioning (SDQ) were assessed pre and post-treatment and 3 months after treatment.
Results: 60.9% of the adolescents completing treatment no longer met DSM-IV criteria for MDD after treatment anymore, and 69.8% at follow-up. Multilevel analyses demonstrated significant posttreatment reductions of depressive symptoms (CDI: Cohen’s d = 0.72), comorbid posttraumatic stress, anxiety and somatic complaints, while overall social-emotional functioning improved. These gains were maintained at 3-month follow-up (Cohen’s d = 1.11). Severity of posttraumatic stress reactions significantly predicted the posttreatment outcome; however, duration of MDD, number of comorbid disorders, or having a history of emotional abuse, emotional neglect or physical neglect were not predictive for outcome.
Conclusions: This is the first study suggesting that EMDR therapy is associated with a significant reduction of depressive symptoms and comorbid psychiatric problems in adolescents with mild to moderate-severe MDD.
HIGHLIGHTS
• Major Depressive Disorder (MDD) can be treated in adolescents using a trauma focused treatment approach.• EMDR therapy is effective in adolescents with a primary diagnosis of MDD.• Sixty percent no longer fulfilled the MDD diagnosis after 6 sessions of EMDR.• Symptoms of anxiety, post-traumatic stress, somatic complaints also decreased significantly and overall social-emotional functioning improved.
Antecedentes: El Trastorno Depresivo mayor (MDD por sus siglas en inglés) tiene una alta prevalencia y alto riesgo de discapacidad en población adolescente, sin embargo, los tratamientos con los que se cuentan actualmente muestran una efectividad limitada, además de altas tasas de abandono y recaída. Pese a que el rol que juegan las experiencias adversas tanto en el desarrollo como en la mantención del MDD ha sido reconocido por décadas, la eficacia de un tratamiento con enfoque centrado en el trauma para MDD ha sido apenas estudiado.
Objetivo: Determinar la efectividad de la terapia de desensibilización y reprocesamiento por movimientos oculares (EMDR por sus siglas en inglés) como intervención única en adolescentes diagnosticados con MDD. Nuestra hipótesis es que el reprocesamiento de recuerdos esenciales relacionados con el inicio y la mantención del MDD usando terapia EMDR estaría asociado a un descenso significativo en síntomas depresivos y comórbidos.
Método: Reclutamos a 32 adolescentes (de 12 a 18 años) que cumplían los criterios DSM-IV para un MDD leve a moderado-severo de un servicio de salud mental ambulatoria juvenil. El tratamiento consistió en seis sesiones individuales de 60 minutos con frecuencia semanal. Se evaluaron con la presencia o ausencia de la clasificación de MDD (ADIS-C), síntomas depresivos (CDI), síntomas de estrés postraumático (UCLA), síntomas ansiosos (SCARED), quejas somáticas (CSI) y funcionamiento socioemocional global (SDQ) tanto antes de iniciar el tratamiento, post tratamiento y a los tres meses de finalizar el tratamiento.
Resultados: El 60.9% de los adolescentes que completó el tratamiento ya no cumplía los criterios del DSM-IV para MDD una vez finalizada la intervención, y en el seguimiento un 69.8% ya no cumplía los criterios. El análisis de multinivel demostró reducciones significativas de síntomas depresivos post-tratamiento (CDI: d de Cohen=0.72), comorbilidad de estrés postraumático, ansiedad y quejas somáticas, mejorando además el funcionamiento socioemocional global. Esta mejoría fue mantenida al seguimiento de 3 meses (d de Cohen=1.11). La severidad de las reacciones de estrés postraumático predijo significativamente el resultado post tratamiento, aunque la duración del MDD, el número de desórdenes comórbidos o el haber tenido una historia de abuso emocional, negligencia emocional o negligencia física no fueron factores predictores para el resultado.
Conclusiones: este es el 6primer estudio que sugiere que la terapia EMDR está asociada con una reducción significativa de síntomas depresivos y problemas psiquiátricos comórbidos en adolescentes con MDD leve a moderado-severo.
背景:青春期的重度抑郁症(MDD)的患病率和残疾风险很高,但是目前的治疗方法的疗效有限并且有较高的脱落率和复发率。几十年来,对痛苦经历和MDD的发展和维持的关系已经有所认识,但关于创伤中心疗法对MDD的疗效几乎从未得到研究。
目的:检验眼动脱敏和再加工(EMDR)疗法独立干预青少年MDD的有效性。我们假设,使用EMDR对与MDD发病和维持相关的核心记忆进行再加工与抑郁症及其合并症的显著减少相关。
方法:从青年心理卫生门诊招募了32名青少年(12–18岁),均符合DSM-IV标准里轻度至中重度MDD。治疗包括每周一次的60分钟的单独治疗,共六次。在治疗前后和3个月随访时分别评估是否存在MDD分类(ADIS-C),抑郁症状(CDI),创伤后应激障碍(UCLA),焦虑症(SCARED),躯体主诉(CSI)和总体社会情感功能(SDQ)。
结果:完成治疗的青少年中,有60.9%的青少年在治疗后不再符合DSM-IV的MDD标准,随访时达到69.8%。多水平分析表明,治疗后抑郁症状显著减轻(CDI:Cohen’s d = 0.72),并发的创伤后应激症状, 焦虑症和躯体不适也得到减轻,同时总体社会情感功能得到改善。在随访3个月后,这些效果得以维持(Cohen’s d= 1.11)。创伤后应激反应的严重程度显著预测了治疗后的结果。但是,MDD的持续时间,合并症的数量,有情感虐待, 情感忽视或身体忽视的病史不能预测结果。
结论:本研究首次表明,EMDR治疗和青少年轻度至中重度MDD症状及其共病问题的显著减轻有关。
1. Introduction
Major depressive disorder (MDD) is one of the most common psychiatric disorders of childhood and adolescence (Mullen, Citation2018). It has been estimated that 14% to 25% of adolescents experience at least one episode of a depressive disorder before entering adulthood (Ryan, Citation2005). MDD is a leading cause of disability in terms of burden of disease, and poor functioning (Smith, Citation2014; Stikkelbroek, Bodden, Deković, & van Baar, Citation2013). Furthermore, MDD with adolescent onset has been found to be associated with a range of physical health problems and other mental health disorders in adult life (Thapar, Collishaw, Pine, & Thapar, Citation2012; Weersing, Jeffreys, Do, Schwartz, & Bolano, Citation2017) as well as with social problems, legal problems, and elevated suicide risk (Stikkelbroek et al., Citation2013).
There are several treatments for adolescent MDD, with cognitive behavioural therapy (CBT) being recommended as a psychosocial intervention for both mild and moderate to severe forms of MDD (NICE guideline, Citation2019). The efficacy of CBT has been established in several reviews and meta-analyses (Compton et al., Citation2004; Oud et al., Citation2019; Weisz, McCarty, & Valeri, Citation2006) and is known to be the intervention with the largest body of evidence. However, the effectiveness of CBT for this target population has been found to be attenuated when compared to active control conditions, and when applied to clinically complicated samples (Lewis et al., Citation2010; Weersing et al., Citation2017). For example, in a Dutch multicentre study carried out in specialized mental health institutions for depressed adolescents (12–21 years; Stikkelbroek, Citation2016) CBT was not found to be more effective than treatment as usual (TAU). In fact, CBT performed worse on both drop-out (CBT 57% vs TAU 41%) and the number of adverse events during treatment (CBT 3 vs TAU 0). The relative poor efficacy of CBT for adolescent MDD is underlined by a mean effect size of 0.29, as computed in a recent meta-analysis of CBT for adolescent MDD (Weisz et al., Citation2017). Therefore, there is an urgent need to enhance the treatment outcome for depressed adolescents.
Eye movement desensitization and reprocessing (EMDR) therapy (Shapiro, Citation2017) is a recommended treatment for posttraumatic stress disorder (PTSD; ISTSS Guidelines Committee, Citation2018; World Health Organization, Citation2013). It has been found to be capable of processing memories of distressing events (Shapiro, Citation2017). Individuals with MDD frequently report an adolescent onset, often following exposure to distressing experiences (Mandelli, Petrelli, & Serretti, Citation2015; Monroe, Slavich, & Georgiades, Citation2014). Strongest evidence for a relationship between childhood adverse events and the development of MDD has been found for interpersonal experiences, like humiliation and entrapment (Kendler, Hettema, Butera, Gardner, & Prescott, Citation2003), and different forms of abuse, primarily emotional abuse and neglect (Hovens et al., Citation2010; Mandelli et al., Citation2015).
In the past 5 years, several studies have been conducted demonstrating preliminary evidence for the efficacy of EMDR therapy in the treatment of MDD in adults. Promising results were obtained from studies investigating EMDR therapy as an adjacent therapy to CBT (Hofmann et al., Citation2014), to pharmacological treatment (Minelli et al., Citation2019; Ostacoli et al., Citation2018) and to inpatient treatment (Hase et al., Citation2015, Citation2018). Three studies, investigating the efficacy of EMDR as a stand-alone treatment, demonstrated significant reductions of depressive symptoms (Gauhar, Citation2016), even for patients with long-term depression (Wood, Ricketts, & Parry, Citation2018) and treatment-resistant depression (Minelli et al., Citation2019). Treatment of MDD also resulted in significant decreases of trauma symptoms (Gauhar, Citation2016) and anxiety symptoms (Minelli et al., Citation2019), improved social functioning (Minelli et al., Citation2019) and quality of life (Gauhar, Citation2016).
While research involving EMDR treatment for adults with depression is emerging rapidly, research on the effectiveness for adolescents has not followed at the same pace. To our knowledge only one case series (Bae, Kim & Park, Citation2008) has been published, which included two adolescents. Although these adolescents did not report traumatic events in their history, they had experienced loss and rejection in family and peer relationships. EMDR was targeted on these memories involving loss and rejection. Both adolescents displayed a significant decline of depressive symptomatology after three and seven EMDR sessions, respectively. This result was maintained at 2- and 3-month follow-up. Given that distressing or traumatic events have been found to be associated with the onset and maintenance of depressive disorders it is conceivable that adolescent MDD is responsive to EMDR therapy when the memories of these events are targeted and resolved. Therefore, the purpose of the present study was to investigate the effectiveness of EMDR in adolescents (12–18 years) with a primary diagnosis of MDD (DSM-IV; American Psychiatric Association, Citation1994). It was hypothesized that the application of EMDR therapy would be associated with a significant decrease in the severity of depressive symptoms and in the percentage of patients meeting DSM-IV criteria for MDD. Furthermore, we hypothesized that treatment would be associated with a significant decrease in the severity of co-morbid symptoms (i.e., posttraumatic stress symptoms, anxiety, somatic and emotional-behavioural problems). In addition, we examined whether duration of MDD, baseline posttraumatic stress disorder severity, number of comorbid disorders, or having a history of emotional abuse, emotional neglect or physical neglect would significantly predict post-treatment outcome. Moreover, to determine the safety of the intervention for this target group the number of adverse events was recorded.
2. Method
2.1. Participants
Patients were recruited from the regular referrals to the Mental Health Institution (MHI) Rivierduinen Leiden Children and Youth department, an outpatient mental health care unit, between December 2015 and March 2018. Inclusion criteria were: (a) age 12–18 years (b) mild to moderate depressive disorder according to the criteria of the Dutch guidelines (Dutch Multidisciplinary Guideline for Depression in Youth, Citation2009), i.e. five to eight symptoms according to DSM IV (American Psychiatric Association (APA), Citation1994), interference of the condition with a maximum of three out of four life domains (school, social situations, leisure, and home/family) and a Global Assessment of Functioning (GAF) >45 (c) identified memories of at least one distressing or traumatic event related to the depressive symptomatology. Exclusion criteria were: (a) severe suicidal or psychotic symptoms, (b) a suicide attempt or serious non-suicidal self-injury requiring hospitalization in the 3 months prior to intake (c) substance dependence (d) IQ estimated to be ≤80 based on information from the referral letter or diagnostic phase (e) insufficient Dutch language skills.
2.2. Procedure
Patients referred for treatment of depressive symptoms at the participating department were screened for eligibility by the first and third author. After the institutions’ regular intake assessment, adolescents who had depressive symptoms were informed about the study by their clinician. Next, pre-treatment assessment (T0) was administered and a session with the EMDR therapist was planned. This session was aimed at checking the inclusion criterion ‘identified memories of at least one distressing or traumatic event related to the depressive symptomatology’; since no standardized instruments are available to make an inventory of depression-related memories beforehand. Subsequently, remaining in- and exclusion criteria were again checked, and in case of eligibility and willingness to participate, informed consent of both adolescents and their caregivers was obtained. Following EMDR treatment, remaining symptoms and need for further treatment of each adolescent were discussed with participants, parents and the multidisciplinary staff.
Outcomes were measured post-treatment (T1) and 3 months after treatment (follow-up, T2) by a team of eight independent assessors (i.e., trained clinicians and master level students), who were not involved in the treatment. Adverse events, such as suicidal attempts, serious self-injurious behaviour and crisis contacts, were recorded using a checklist by the therapists at the start of each session.
For administration of the ADIS-C, all assessors were trained according to a protocol consisting of observing live and videotaped interviews and completed an exam to prove adequate administration of the interview. Supervision was provided for each assessment and the reports were reviewed and discussed to ensure that administration, scoring and reporting would not drift. Therapists who conducted the EMDR sessions were blind to assessment data.
2.3. Intervention
The Dutch version of the standard EMDR procedure with age-specific adaptations for children and adolescents (De Roos, Beer, de Jongh, & Ten Broeke, Citation2015) was used for the present study. This procedure includes eight phases: history taking, preparation, assessment, desensitization, installation, body scan, closure and re-evaluation (Shapiro, Citation2017). Treatment consisted of six weekly 60-min individual treatment sessions. Memories were placed in a hierarchy based on the Subjective Units of Disturbance (SUD) and were treated subsequently from high to low SUD. Each session was followed by a 10- to 15-min meeting with the adolescent and one or both parents. The content of this meeting was discussed beforehand with the adolescent and could comprise any one of the following elements: (1) an outline of the content of the session (2) parents’ view on the course of symptoms in the week before the session and (3) the need and possibilities for emotional support of the adolescent after the session.
In the present study, EMDR therapy was carried out by a team of seven clinical psychologists. Six of them were registered EMDR Europe Practitioners. All sessions were videotaped and all therapists participated in monthly two-hour supervisions by a certified EMDR Europe Child and Adolescent Consultant (second author). Additional supervision by email or telephone was provided on request. Early completion of treatment (<6 sessions) was assigned in cases where all target memories from the case conceptualization could be retrieved without emotional disturbance (i.e. SUD related to the memory was reduced to zero).
2.4. Assessment instruments
The participants’ demographic characteristics (e.g. living condition, level of education, history of mental health service use) were assessed at baseline. All measurements were administered at all assessments (baseline (T0), post-treatment (T1) and 3-month follow-up (T2), except the Childhood Trauma Questionnaire (CTQ), which was only administered at T0).
The primary outcome measure of this study was the presence of an MDD diagnosis on the Anxiety Disorders Interview Schedule for DSM-IV Child version (ADIS-C). The ADIS-C assesses a wide range of diagnoses according to DSM-IV criteria (American Psychiatric Association, Citation1994; Siebelink & Treffers, Citation2001; Silverman & Albano, Citation1996). The ADIS-C has strong evidence for providing reliable and valid diagnoses and proved to possess adequate sensitivity to clinical change in treatment outcome research (Silverman & Ollendick, Citation2005).
The Dutch version of the Children’s Depression Inventory (CDI; Kovacs, Citation1985; Timbremont, Braet, & Roelofs, Citation2008) was used to assess affective, behavioural and cognitive aspects of depressive symptoms in the past 2 weeks. The CDI includes 27 items dealing with sadness, self-blame, loss of appetite, insomnia, interpersonal relationships, and school adjustment which are scores on a 3-point Likert scale (0–2, total range 0–54). Acceptable levels of internal consistency, validity and test–retest reliability have been established (Kovacs, Citation1985; Roelofs et al., Citation2010). Reliability of the total scale in the current study was acceptable (α = .78).
The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index Adolescent version (UCLA PTSD RI; Steinberg, Brymer, Decker & Pynoos, Citation2004) was used to screen for exposure to traumatic events and to assess PTSD symptoms. The symptom scale consists of 22 items which are scored on a 5-point Likert scale (0–4; total range 0–88) and assesses the frequency of occurrence of PTSD symptoms during the past month. The original list of traumatic events covering medical trauma, natural disasters, community violence and abuse was adapted for the present study by adding four items concerning experiences of loss and separation (death and separation from loved ones) and humiliation (bullying and being isolated/ignored). These experiences, considered as ‘attachment trauma’ (Hofmann et al., Citation2014) have been identified as being connected to the onset of depressive episodes (see, e.g., Bae et al., Citation2008; Kendler et al., Citation2003). Reliability of the UCLA total scale in the current study was excellent (α = .91).
The Dutch version of the Screen for Child Anxiety Related Emotional Disorders (SCARED; Muris, Bodden, Hale, Birmaher, & Mayer, Citation2007; Muris, Merckelbach, Schmidt, & Mayer, Citation1998) was used to assess signs of anxiety disorders in the past 3 months. The SCARED is a 41-item inventory rated on a 3 point Likert-type scale (0 = ’not true’ or ‘hardly ever true’; 1 = ‘somewhat true’ or ‘sometimes true’; 2 = ’very true’ or ‘often true’; total range 0–82). Reliability of the SCARED total scale in the current study was excellent (α = .92).
The Children’s Somatization Inventory (CSI; Garber, Walker, & Zeman, Citation1991; Dutch version: Treffers, Goedhart, & Siebelink, Citation1998) was used to assess the extent and frequency of 35 somatic complaints (e.g. headaches, constipation, dizziness) in children and adolescents in the past 2 weeks. Items are scored on a 5-point Likert scale (0: ‘not at all’, 4 ‘a whole lot’) (total range 0–140). Reliability of CSI total scale in the current study was excellent (α = .93).
The Dutch adolescent version of the Strengths and Difficulties Questionnaire (SDQ; Goedhart, Treffers, & Van Widenfelt, Citation2003; Goodman, Citation1997) was used as a global assessment of psychological problems. The SDQ consists of 25 items which are scored on a 3-point Likert scale ranging from ‘not true’, ‘somewhat true’ or ‘certainly true’ (total range 20–80). In this study, the ‘total difficulties scale’ was used in the analyses. Reliability of the SDQ total scale in the current study was good (α = .80).
The Childhood Trauma Questionnaire (CTQ; Bernstein et al., Citation2003) was used to assess experiences of childhood maltreatment. The CTQ is a self-report list consisting of 28 items which are scored on a 5-point Likert scale. The CTQ has a good criterion validity in both a clinical and a healthy sample (Bernstein et al., Citation2003). The subscales Emotional neglect, Emotional Abuse and Physical Neglect were used in the analyses. Reliability of the CTQ total scale in the current study was excellent (α = .90).
2.4.1. Data analyses
All statistical analyses were performed using IBM SPSS Statistics for Windows (version 24). Descriptive statistics were produced to describe the demographic characteristics and baseline variables of the sample. To investigate the effect of EMDR therapy time contrasts were created (T0-T1, T0-T2) by means of dummy coding. Linear mixed model analyses were used for the main analyses. The mixed model for investigating the general efficacy of the EMDR intervention included a random term for the intercept and fixed terms for time contrasts (T0-T1, T0-T2). The covariance matrix was set to scaled identity. Effect sizes were calculated using Cohen’s d (Cohen, Citation1992), and determined by calculating the mean difference between scores from baseline (T0) to post-treatment (T1) and from baseline (T0) to follow-up (T2), dividing the result by the pooled standard deviation (Cohen, Citation1988). Cohen’s d was calculated for both depressive symptoms and comorbid symptoms.
To identify possible predictors of treatment outcome (depressive symptoms as measured by the CDI), baseline posttraumatic stress symptom severity (UCLA), number of comorbid disorders (ADIS-C) and depression-specific baseline factors (i.e., history of emotional abuse or neglect (CTQ), and duration of the disorder) were entered separately in the linear mixed model analyses. The same time contrasts as described above were used (i.e. T0-T1 and T0-T2). The level of significance was set at a =.05.
3. Results
3.1. Patient flow and sample characteristics
Before referral to our institution, and entering the study, the majority of the patients (n = 23; 72%) received some form of treatment. Based upon the UCLA, 73% of the adolescents had experienced a non-criterion A-event (i.e., bullying/humiliation, being ignored/isolated and bereavement of a loved one) prior to therapy. The characteristics of the study population are presented in . The treatment sample was characterized by a long duration of MDD (M = 72.4 weeks, SD = 74.42, range 18–364 weeks; depressive disorder was present in the family in 59%) and a high number of comorbid disorders (M = 2.39, SD = 1.38; for all but one patient comorbid disorders were classified at T0). These comorbid disorders comprised primarily social phobia, generalized anxiety disorder and dysthymic disorder. From the different forms of childhood trauma, emotional neglect (32% above cut-off), emotional abuse (23% above cut-off) and physical neglect (19% above cut-off) were reported most frequently ().
Table 1. Sample characteristics.
Table 2. Results of linear mixed model analyses.
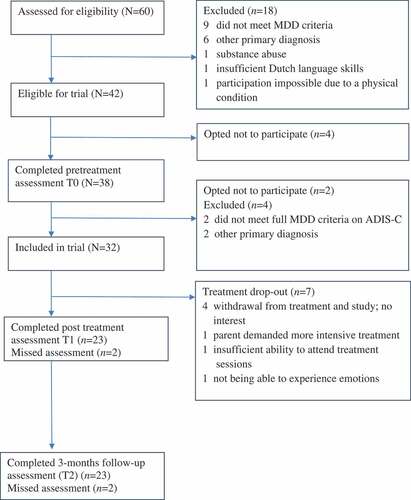
shows the patient flow through the study. In total, 32 patients were included with a mean age of 15.8 years (SD = 1.50). Five (15.6%) were early completers and needed only four (n = 1) or five (n = 4) EMDR sessions. Seven (21.9%) dropped out before the end of treatment; three withdrew from treatment and study because of a lack of interest, one because of spontaneous remission, one because the parent demanded more intensive treatment, one because of insufficient ability to attend treatment sessions and one because the adolescent was not able to experience the emotional load related to the identified depression-related memories (SUD). Independent sample t-tests were performed to compare dropouts with completers on age, gender, baseline severity of MDD symptoms and posttraumatic stress reactions, duration of MDD and number of comorbid disorders at baseline. Therapist factors were excluded because of the low number of patients in each cell of the crosstabs (32 clients were treated by 8 therapists). From all tested variables, only duration of MDD differed significantly between the groups, with dropouts having a shorter duration of depressive symptoms (m = 36.86, SD = 11.60) compared to completers (m = 86.22, SD = 79.84) (t (df = 27.14) = 2.98, p = 0.006).
3.2. Depression
As can be seen from , 14 out of 23 adolescents who completed treatment and T1 assessment (60.9%) no longer fulfilled the criteria of a MDD diagnosis as determined by the ADIS-C after treatment (T1). For the intent to treat group this rate was 43.8% (14 out of 32). The percentage no longer obtaining a MDD diagnosis further increased to 69.8% for completers (16 out of 23) and to 50.0% for the intent to treat group (16 out of 32) at follow-up (T2). shows a significant decrease of depressive symptoms (CDI), with a sharp reduction of symptoms during treatment (T0-T1: Cohen’s d = 0.72) and a further decrease afterwards (T0-T2; Cohen’s d = 1.11).
Table 3. Results of predictor analyses on treatment outcome as measured by level of depressive symptoms (CDI).
Figure 2. Proportion of patients completing treatment meeting DSM-IV criteria for MDD (ADIS-C) at different points in time.
Cohen’s κ was calculated for the inter-rater agreement on the ADIS-C at T1. Half of the interviews (n = 12) were double-scored and κ was calculated at .082.
3.3. Comorbid symptoms
Posttraumatic stress symptoms (UCLA), anxiety symptoms (SCARED), somatic complaints (CSI) and general social-emotional problems (SDQ) showed a significant decrease following EMDR therapy which was maintained at follow-up. For all measures, medium to large effect sizes were found (see ).
3.4. Prediction of post-treatment outcome
Severity of PTSD symptoms significantly predicted treatment outcome as measured by the CDI (p < .01; see ); with higher levels of PTSD symptoms at baseline predicting greater reductions of MDD symptoms during treatment. No other significant predictors of treatment outcome could be identified.
3.5. Adverse events
No adverse events were reported during the study.
4. Discussion
To our knowledge, besides one study on two cases (Bae et al., Citation2008) this is the first outcome study that examined the effectiveness of EMDR therapy in adolescents with a primary diagnosis of MDD. The results demonstrated a significant decrease in depressive symptoms and comorbid posttraumatic stress, anxiety, somatic complaints and overall social-emotional functioning. More than 60% of the adolescents completing treatment no longer fulfilled the criteria of an MDD diagnosis after treatment. The medium to large effect sizes suggested clinically relevant effects that were maintained at 3 months of follow-up.
It is noteworthy that remission of depressive symptoms was achieved after only six one hour sessions. For the completers, most of the MDD related memories that were identified were processed using EMDR therapy. This suggests that the number of six sessions seemed sufficient for most of the adolescents. To this end, there are no similar studies with adolescents to compare our results to, but the present findings are consistent with the case study by Bae et al. (Citation2008), and studies reporting the effect of EMDR therapy as a stand-alone intervention in adult MDD (Gauhar, Citation2016; Minelli et al., Citation2019; Wood et al., Citation2018).
Treatment result in our study seemed to be significantly influenced by baseline severity of posttraumatic stress reactions, meaning that adolescents with high levels of posttraumatic stress reactions demonstrated a larger decrease of depressive symptoms during treatment. None of the remaining predictors (i.e., number of comorbid disorders, duration of MDD and having a history of emotional abuse, emotional or physical neglect) seemed to have influenced treatment outcome. To this end, it could be particularly hopeful that the results suggest that a long duration of MDD and having many comorbid problems (74.2% had two or more comorbid disorders) did not significantly interfere with the effects of EMDR therapy in this population, which is in contrast to what is often observed in studies that used cognitive behavioural therapy (Weersing et al., Citation2017).Yet, these results should, of course, be interpreted with caution, since this is a first small feasibility study with limited power.
The fact that adverse events, such as suicidal attempts, serious self-injurious behaviour and crisis contacts, did not occur suggests that treatment of MDD using a trauma-focused approach is safe. Related to this, the drop-out rate (21.9%) was comparable to drop-out rates obtained in other studies of EMDR therapy as a stand-alone treatment of MDD (e.g. Gauhar, Citation2016: 23%; Minelli et al., Citation2019: 15.4%; Wood et al., Citation2018: 30%). On the other hand, compared to the dropout-rate (57%) of a Dutch CBT study with a comparable population (Stikkelbroek et al., Citation2013) the drop-out rate of the present study can even be considered as low.
This study is a pilot study and has, therefore, several limitations. The most important limitation is that the absence of a waiting list and/or an active control condition so we cannot rule out that the observed improvements were either an artefact of time or due to placebo effects. Secondly, the sample size was small and the follow-up period of 3 months was relatively short. Thirdly, given the wide array of studies showing that this population often suffers from suicidal intentions we wanted to be cautious and excluded individuals with severe depression. Although the results of the present feasibility study do not support the notion that the use of EMDR is unsafe in terms of adverse events, it could be argued that the exclusion of a severe subgroup might make the results less generalizable. Interestingly, however, there are few studies with which we can compare our results on this point. For example, while in the study by Stikkelbroek et al. (Citation2013) with comparable mean CDI total scores, severity of depression was not an exclusion criterion, acute suicide risk was. Besides the obvious limitations of the present study, some strengths should also be noted. An important strength of this study is that it included a representative group of adolescents seen in routine mental health care, in terms of a relatively long duration of depressive symptoms, many comorbid problems, and having received unsuccessful prior treatment or counselling, which makes the results highly generalizable. Another strength is the use of a semi-structured DSM based clinical interview, conducted by trained interviewers. Finally, the therapists used a manualized treatment protocol, session checklists and video-recorded sessions, which were evaluated and discussed during supervision to enhance treatment integrity.
Yet, despite the promising results, most patients still suffered from symptoms of depression after completion of EMDR treatment. More specifically, 39.1% of adolescents who completed treatment still fulfilled the diagnostic criteria of MDD according to ADIS-C; 62.5% scored above CDI cut-off of 16, and 68% of the patients received additional treatment interventions (i.e., CBT, emotion regulation training, parent counselling, family interventions, medication or a combination of these) for the remaining complaints after the study. Further research is needed to determine whether the addition of evidence-based interventions aimed at cognitive restructuring or family interventions may lead to stronger symptom reduction, even lower drop-out, and less after care. More generally, given the heterogeneous nature of MDD, it would be naïve to expect that one single treatment approach, e.g. trauma-focused treatment, would be sufficient to cure all different appearances of MDD. That is, for a certain subgroup of adolescents with MDD treatment using EMDR therapy might be of value as our results suggest, but the treatment of other subgroups, with regard to which (combinations of) interventions are the most successful, requires further investigation.
In conclusion, the results of this study showed that the application of EMDR therapy was safe and associated with a significant reduction of depressive symptoms and comorbid psychiatric problems. Clearly, randomized controlled trials with sufficient statistical power are needed to establish the efficacy of EMDR therapy in adolescents with mild to moderate or severe MDD.
Acknowledgments
We would like to thank all adolescents and their parents, as well as the therapists (Egle Jan Annema, Marjolein van Avesaath, Marieke van der Eijk, Sisca van der Hell, Eva Sabee and Annemariek Sepers). We thank Roselyne Cohen, Annette Cox, Lucie van den Eertwegh, Nynke Jobse, Amal Mahi, Angela van der Meer, Maya Vinnerljung and Sanne van der Zwet for their assistance in collection of the data.
Disclosure statement
Carlijn de Roos and Ad de Jongh receive income from published books about EMDR and for training postdoctoral professionals in EMDR.
References
- American Psychiatric Association (APA). (1994). Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC: American Psychiatric Association.
- Bae, H., Kim, D., & Park, Y. C. (2008). Eye movement desensitization and reprocessing for adolescent depression. Psychiatry Investigation, 5, 60–11.
- Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., … Zule, W. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect, 27(2), 169–190.
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum.
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155.
- Compton, S. N., March, J. S., Brent, D., Albano, A. M., Weersing, V. R., & Curry, J. (2004). Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: An evidence-based medicine review. Journal of the American Academy of Child & Adolescent Psychiatry, 43(8), 930–959.
- De Roos, C., Beer, R., de Jongh, A., & Ten Broeke, E. (2015). EMDR protocol voor kinderen en jongeren tot 18 jaar [EMDR protocol for children and adolescents under 18 years]. Dutch Multidisciplinary Guideline for Depression in Youth. Utrecht: Trimbos-instituut.
- Dutch Multidisciplinary Guideline for Depression in Youth. (2009). The Netherlands, Utrecht: Trimbos Instituut.
- Garber, J., Walker, L. S., & Zeman, J. (1991). Somatization symptoms in a community sample of children and adolescents: Further validation of the children’s somatization inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology, 3(4), 588.
- Gauhar, Y. W. M. (2016). The efficacy of EMDR in the treatment of depression. Journal of EMDR Practice and Research, 10(2), 59–69.
- Goedhart, A., Treffers, F., & Van Widenfelt, B. (2003). Vragen naar psychische problemen bij kinderen en adolescenten [Measuring psychological problems in children and adolescents]: Strengths and Difficulties Questionnaire (SDQ). Maandblad Geestelijke Volksgezondheid, 58, 1018–1035.
- Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586.
- Hase, M., Balmaceda, M., Hase, A., Lehnung, M., Tumani, V., Huchzermeier, C., & Hofman, A. (2015). Eye movement desensitization and reprocessing (EMDR) therapy in the treatment of depression: A matched pairs study in an inpatient setting. Brain and Behavior, 5(6), e00342.
- Hase, M., Plagge, J., Hase, A., Braas, R., Ostacoli, L., Hofmann, A., & Huchzermeier, C. (2018). Eye movement desensitization and reprocessing versus treatment as usual in the treatment of depression: A randomized-controlled trial. Frontiers in Psychology, 9, 1384.
- Hofmann, A., Hilgers, A., Lehnung, M., Liebermann, P., Ostacoli, L., Schneider, W., & Hase, M. (2014). Eye movement desensitization and reprocessing as an adjunctive treatment of unipolar depression: A controlled study. Journal of EMDR Practice and Research, 8(3), 103–112.
- Hovens, J. G., Wiersma, J. E., Giltay, E. J., Van Oppen, P., Spinhoven, P., Penninx, B. W., & Zitman, F. G. (2010). Childhood life events and childhood trauma in adult patients with depressive, anxiety and comorbid disorders vs. controls. Acta Psychiatrica Scandinavica, 122(1), 66–74.
- International Society for Traumatic Stress Studies (ISTSS). (2018). ISTSS PTSD prevention and treatment guidelines: Methodology and recommendations. Retrieved from http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- Kendler, K. S., Hettema, J. M., Butera, F., Gardner, C. O., & Prescott, C. A. (2003). Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Archives of General Psychiatry, 60(8), 789–796.
- Kovacs, M. (1985). The children’s depression inventory (CDI). Psychopharmacology Bulletin, 21, 995–998.
- Lewis, C. C., Simons, A. D., Nguyen, L. J., Murakami, J. L., Reid, M. W., Silva, S. G., & March, J. S. (2010). Impact of childhood trauma on treatment outcome in the treatment for adolescents with depression study (TADS). Journal of the American Academy of Child and Adolescent Psychiatry, 49(2), 132–140.
- Mandelli, L., Petrelli, C., & Serretti, A. (2015). The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. European Psychiatry, 30(6), 665–680.
- Minelli, A., Zampieri, E., Sacco, C., Bazzanella, R., Mezzetti, N., Tessari, E., … Bortolomasi, M. (2019). Clinical efficacy of trauma-focused psychotherapies in treatment-resistant depression (TRD) in-patients: A randomized, controlled pilot-study. Psychiatry Research, 273, 567–574.
- Monroe, S. M., Slavich, G. M., & Georgiades, K. (2014). The social environment and depression: The roles of life stress. In H. Gotlieb & C. Hammen (Eds.), Handbook of depression (3rd ed., pp. 296–314). New York: The Guilford Press.
- Mullen, S. (2018). Major depressive disorder in children and adolescents. Mental Health Clinician, 8(6), 275–283.
- Muris, P., Bodden, D., Hale, W., Birmaher, B., & Mayer, B. (2007). SCARED-NL: Vragenlijst over angst en bang-zijn bij kinderen en adolescenten. Handleiding bij de gereviseerde Nederlandse versie van de Screen for Child Anxiety Related Emotional Disorders. [Questionnaire about fear and anxiety. Manual of the Dutch version of the SCARED]. Amsterdam: Boom test uitgevers.
- Muris, P., Merckelbach, H., Schmidt, H., & Mayer, B. (1998). The revised version of the Screen for Child Anxiety Related Emotional Disorders (SCARED-R): Factor structure in normal children. Personality and Individual Differences, 26(1), 99–112.
- National Institute for Health and Care Excellence. (2019). Depression in children and young people: Identification and management. Retrieved from: https://www.nice.org.uk/guidance/ng134/documents/draft-guideline
- Ostacoli, L., Carletto, S., Cavallo, M., Baldomir-Gago, P., Di Lorenzo, G., Fernandez, I., … Oliva, F. (2018). Comparison of eye movement desensitization reprocessing and cognitive behavioral therapy as adjunctive treatments for recurrent depression: The European Depression EMDR Network (EDEN) randomized controlled trial. Frontiers in Psychology, 9, 74.
- Oud, M., de Winter, L., Vermeulen-Smit, E., Bodden, D., Nauta, M., Stone, L., … Engels, R. (2019). Effectiveness of CBT for children and adolescents with depression: A systematic review and meta-regression analysis. European Psychiatry, 57, 33–45.
- Roelofs, J., Braet, C., Rood, L., Timbremont, B., Van Vlierberghe, L., Goossens, L., & van Breukelen, G. (2010). Norms and screening utility of the Dutch version of the children’s depression inventory in clinical and nonclinical youths. Psychological Assessment, 22(4), 866.
- Ryan, N. D. (2005). Treatment of depression in children and adolescents. The Lancet, 366(9489), 933–940.
- Shapiro, F. (2017). Eye movement desensitization and reprocessing (EMDR) therapy: Basic principles, protocols, and procedures (3rd ed.). New York: Guilford Publications.
- Siebelink, B. M., & Treffers, A., Ph. D. (2001). Nederlandse bewerking van anxiety disorders interview schedule for DSM-IV child version [Dutch Translation of the Anxiety Disorders Interview Schedule for DSM-IV Child Version]. The Netherlands, Lisse: Swets & Zeitlinger.
- Silverman, W. K., & Albano, A. M. (1996). Anxiety disorders interview schedule for DSM-IV child version, child interview schedule. San Antonio: The Psychological Corporation.
- Silverman, W. K., & Ollendick, T. H. (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 380–411.
- Smith, K. (2014). Mental health: A world of depression. Nature News, 515(7526), 180.
- Steinberg, A. M., Brymer, M. J., Decker, K. B., & Pynoos, R. S. (2004). The university of California at Los Angeles Posttraumatic Stress Disorder Reaction Index. Current Psychiatry Reports, 6, 96–100
- Stikkelbroek, Y., Bodden, D. H., Deković, M., & van Baar, A. L. (2013). Effectiveness and cost effectiveness of cognitive behavioral therapy (CBT) in clinically depressed adolescents: Individual CBT versus treatment as usual (TAU). BMC Psychiatry, 13(1), 314.
- Stikkelbroek, Y. A. J. (2016). Turning depression inside out: Life events, cognitive emotion regulation and treatment in adolescents (Doctoral dissertation). Utrecht University, The Netherlands.
- Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067.
- Timbremont, B., Braet, C., & Roelofs, J. (2008). Handleiding children’s depression inventory (herziene versie) [Manual of the children’s depression inventory, revised version]. The Netherlands, Amsterdam: Pearson Assessment and Information B.V.
- Treffers, D. A., Ph, Goedhart, A. W., & Siebelink, B. M. (1998). Resultaten van de Nederlandse vertaling van de children’s somatization inventory. Emotionele Stoornissen en Somatoforme Stoornissen bij kinderen en adolescenten: De stand van zaken. [Results of the Dutch Translating of the Children’s Somatization Inventory. Emotional and somatoform disorders in children and adolescents: State of the art] (pp. 37–52). The Netherlands, Leiden: Boerhaave Commissie voor Postacademisch Onderwijs in de Geneeskunde.
- Weersing, V. R., Jeffreys, M., Do, M. C. T., Schwartz, K. T., & Bolano, C. (2017). Evidence base update of psychosocial treatments for child and adolescent depression. Journal of Clinical Child & Adolescent Psychology, 46(1), 11–43.
- Weisz, J. R., Kuppens, S., Ng, M. Y., Eckshtain, D., Ugueto, A. M., Vaughn-Coaxum, R., … Weersing, V. R. (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. American Psychologist, 72(2), 79.
- Weisz, J. R., McCarty, C. A., & Valeri, S. M. (2006). Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin, 132(1), 132.
- Wood, E., Ricketts, T., & Parry, G. (2018). EMDR as a treatment for long-term depression: A feasibility study. Psychology and Psychotherapy: Theory, Research and Practice, 91(1), 63–78.
- World Health Organization. (2013). Guidelines for the management of conditions that are specifically related to stress. World Health Organization.