ABSTRACT
Background: Post-traumatic stress disorder (PTSD) is a common and debilitating disorder which has a significant impact on the lives of sufferers. A number of early psychological interventions have been developed to try to prevent chronic difficulties.
Objective: The objective of this study was to establish the current evidence for the effectiveness of multiple session early psychological interventions aimed at preventing or treating traumatic stress symptoms beginning within three months of trauma exposure.
Methods: Randomized controlled trials of early multiple session psychological interventions aimed at preventing or reducing traumatic stress symptoms of individuals exposed to a traumatic event, fulfiling trauma criteria for an ICD or DSM diagnosis of PTSD were identified through a search of the Cochrane Common Mental Disorders Group Clinical Trials Registers database, the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, PsycINFO and PILOTS. Two authors independently extracted study details and data and completed risk of bias assessments. Analyses were undertaken using Review Manager software. Quality of findings were rated according to ‘Grades of Recommendation, Assessment, Development, and Evaluation’ (GRADE) and appraised for clinical importance.
Results: Sixty-one studies evaluating a variety of interventions were identified. For individuals exposed to a trauma who were not pre-screened for traumatic stress symptoms there were no clinically important differences between any intervention and usual care. For individuals reporting traumatic stress symptoms we found clinically important evidence of benefits for trauma-focused cognitive-behavioural therapy (CBT-T), cognitive therapy without exposure and eye movement desensitization and reprocessing (EMDR). Differences were greatest for those diagnosed with acute stress disorder (ASD) and PTSD.
Conclusions: There is evidence for the effectiveness of several early psychological interventions for individuals with traumatic stress symptoms following trauma exposure, especially for those meeting the diagnostic threshold for ASD or PTSD. Evidence is strongest for trauma-focused CBT.
HIGHLIGHTS
• We found no clinically important evidence for the benefit of early intervention offered to all individuals exposed to a traumatic event, regardless of symptomatology.• There was evidence of a clinically important effect for trauma-focused CBT (CBT-T), brief EMDR and cognitive therapy without exposure.• Evidence was strongest for CBT-T.
Antecedentes: El Trastorno de Estrés Postraumático (TEPT) es un trastorno frecuente y debilitante que tiene un impacto significativo en las vidas de los que lo padecen. Se han desarrollado una serie de intervenciones psicológicas tempranas para tratar de prevenir dificultades crónicas.
Objetivo: El objetivo de este estudio fue establecer la evidencia actual para la eficacia de intervenciones psicológicas tempranas con múltiples sesiones con el objetivo de prevenir o tratar síntomas de estrés traumático que comenzaron en los tres meses posteriores a la exposición al trauma.
Métodos: Se realizó una búsqueda bibliográfica basada en la base de datos de Cochrane de Estudios Clínicos de Trastornos Mentales Frecuentes, en el registro de ensayos controlados de Cochrane, MEDLINE, Embase, PsycINFO y PILOTS, para identificar ensayos controlados randomizados de intervenciones psicológicas tempranas de múltiples sesiones que tenían el objetivo de prevenir o reducir síntomas de estrés traumático en individuos expuestos a un evento traumático, y que cumplían los criterios de TEPT según la CIE o el DSM. Dos autores independientes extrajeron los detalles e información del estudio y completaron una evaluación de riesgo de sesgo. Se llevaron a cabo análisis usando el software Review Manager. La calidad de los hallazgos fue puntuada según los ‘Grados de Recomendación, Valoración, Desarrollo y Evaluación’ (GRADE pos sus siglas en inglés) y evaluada por su importancia clínica.
Resultados: Se identificaron sesenta y un estudios que evaluaban una variedad de intervenciones. Para aquellos individuos que estuvieron expuestos a un trauma que no tuvieron una pre-evaluación de síntomas de estrés traumático no hubo una diferencia clínica importante entre cualquier intervención y cuidado usual. Para los individuos que reportaron síntomas de estrés traumático encontramos evidencia clínicamente significativa de los beneficios de la terapia cognitiva focalizada en el trauma (CBT-T por sus siglas en inglés), terapia cognitiva sin exposición y desensibilización y reprocesamiento a través de movimientos oculares (EMDR por sus siglas en inglés). Las diferencias fueron mayores para aquellos diagnosticados con trastornos de estrés agudo (ASD por sus siglas en inglés) y TEPT.
Conclusiones: Existe evidencia para la eficacia de varias intervenciones psicológicas tempranas para individuos con síntomas de estrés traumático posterior a la exposición a un trauma, especialmente para aquellos que cumplen con los criterios para un diagnóstico completo de ASD o TEPT. La evidencia es más fuerte para la CBT-T.
背景:创伤后应激障碍(PTSD)是一种常见的, 使人衰弱的疾病,对患者的生活有重大影响。为预防发展为慢性疾病,已经开发出许多早期心理干预措施。
目标:本研究的目的是为旨在预防或治疗创伤暴露三个月内开始出现的创伤应激症状的多阶段早期心理干预的有效性建立现有证据。
方法:通过搜索Cochrane常见精神障碍小组临床试验注册数据库, Cochrane 临床对照试验数据库, MEDLINE, Embase, PsycINFO 和 PILOTS,确定了早期多阶段心理干预的随机对照试验。这些干预旨在预防或减轻遭受创伤事件且符合 ICD 或 DSM 诊断 PTSD 的创伤标准的个体的创伤应激症状。两位作者分别独自提取了研究细节和数据,并完成了误差风险评估。使用 Review Manager 软件进行分析。根据‘推荐分级的评估, 制定与评价’(GRADE)对结果的质量进行评级并评估其临床重要性。
结果:确定了评估多种干预措施的61项研究。对于有创伤暴露但未预先筛查创伤应激症状的个体,任何干预措施和日常护理间均无重要的临床差异。对于报告有创伤应激症状者,我们发现聚焦创伤的认知行为疗法(CBT-T), 无暴露认知疗法以及眼动脱敏与再加工(EMDR)效益的重要临床证据。在被诊断为急性应激障碍(ASD)和 PTSD 的患者中差异最大。
结论:有证据表明了对于创伤暴露后患有创伤应激症状者,特别是那些达到 ASD 或 PTSD 诊断阈值的个体,几种早期心理干预的有效性。对于聚焦创伤的 CBT 证据最充分。
1. Introduction
Numerous studies demonstrate that a range of traumatic experiences can cause psychological difficulties to those exposed (Berger et al., Citation2012, Brunet, Monson, Liu, & Fikretoglu, Citation2015; Dworkin, Menon, Bystrynski, & Allen, Citation2017; Lowe & Galea, Citation2017; Neria, Nandi, & Galea, Citation2008). For many, these difficulties are short lived or subclinical, and diminish over time without the need for medical or psychological intervention (Giummarra, Lennox, Dali, Costa, & Gabbe, Citation2018; McNally, Bryant, & Ehlers, Citation2003). However, psychological difficulties may develop and persist for some of those exposed. These difficulties include acute stress disorder (ASD) and post-traumatic stress disorder (PTSD). Around a third of individuals with PTSD at 4–6 weeks post trauma exposure remit by 3 months (Santiago et al., Citation2013); whilst for around another third of individuals symptoms become chronic and unremitting (Kessler, Sonnega, Bromet, Hughes, & Nelson, Citation1995; Santiago et al., Citation2013). Estimated life-time prevalence rates of PTSD have been found to vary from 1.3% to 8.8% (Atwoli, Stein, Koenen, & McLaughlin, Citation2015). Rates of PTSD also vary according to trauma type, with an estimated mean conditional risk following any trauma exposure of 4.0%, with much higher rates for some types of interpersonal trauma (Kessler et al., Citation2017) which tend not to show the same pattern of symptom reduction (Santiago et al., Citation2013). PTSD symptoms can have a considerable impact on the life trajectory of those exposed to trauma and their families (McFarlane, Citation2010; Shalev et al., Citation2019). Typically, symptoms affect social, occupational and interpersonal functioning, and physical health. PTSD is frequently associated with comorbidity and unhealthy coping mechanism, which can become chronic and entrenched over time (Shalev et al., Citation2019). PTSD has a significant economic burden (Ferry et al., Citation2015; Greenberg et al., Citation1999).
As the effects of trauma exposure and the development of conditions such as PTSD have become better understood, there have been increasing efforts to develop psychological and pharmacological interventions that might prevent the onset of disorder or ameliorate early symptoms (Kearns, Ressler, Zatzick, & Rothbaum, Citation2012; McNally et al., Citation2003). For a time, Psychological Debriefing (also known as Critical Incident Stress Debriefing) was a widely used form of early intervention. However, its use has declined as evidence challenging its efficacy has emerged (Bastos, Furuta, Small, McKenzie‐McHarg, & Bick, Citation2015; Rose, Bisson, Churchill, & Wessely, Citation2002). Over the past 20 years or so, a range of other approaches, mainly based on established cognitive behavioural therapy (CBT) for PTSD, have emerged (Kearns et al., Citation2012). More recently some groups have started to evaluate telephone-based approaches and approaches based on new technology in order to increase accessibility to potentially effective interventions.
In 2009 we published a systematic review and meta-analysis of randomized controlled trials (RCTs) of psychological interventions aimed at preventing or treating PTSD within three months of a traumatic event (Roberts, Kitchiner, Kenardy, & Bisson, Citation2009). This review included 25 studies. We found no evidence to support the use of preventative interventions offered to individuals irrespective of whether they were symptomatic or not. However, we did find evidence to support the use of trauma focused cognitive behavioural therapy (CBT-T) in studies targeting individuals with early traumatic stress symptoms. Effects were strongest for treatment of acute stress disorder and posttraumatic stress disorder. A subsequent review conducted by the US Agency for Health Care Research and Quality (AHRQ) identified a smaller pool of 19 studies but reported similar findings (Forneris et al., Citation2013). A review focusing specifically on individuals who suffered traumatic injury which included 26 mostly randomised controlled trials (RCTs) also found support for cognitive behavioural interventions, alongside small but significant effects for collaborative care based approaches (Giummarra et al., Citation2018). Neither of these reviews made a distinction between preventative interventions aimed at all individuals exposed and studies focusing specifically on individuals who were symptomatic. Since our previous review (Roberts et al., Citation2009), a range of new early interventions have been developed and evaluated, including brief EMDR, new technology based approaches and interventions aimed at those who have experienced serious illnesses. In light of new developments in the field, the purpose of this paper is to provide an update of our previous review of all available early intervention studies aiming to prevent or treat traumatic stress symptoms following exposure to an event fulfilling trauma criteria for an ICD or DSM diagnosis of PTSD. The review was undertaken as a part of the process for the International Society for Traumatic Stress Studies (ISTSS) Treatment Guidelines (Bisson et al., Citation2019).
2. Method
2.1. Data sources
Following on from the previous search, we undertook a systematic computerized literature search of the Cochrane Common Mental Disorders Group clinical trials registers databases for studies published from January 2008 to May 2016 using the search terms PTSD or posttrauma* or post-trauma* or ‘post trauma*’ or ‘combat disorder*’ or ‘stress disorder*’. These databases are collated and updated on a weekly basis from MEDLINE, EMBASE and PsycINFO. A further search was undertaken in March 2018. We chose not to exclude any potential study based on date of publication, at any time point. Searches were undertaken as part of a search process to support development of new PTSD treatment guidelines for the ISTSS (Bisson et al., Citation2019). See Appendix 1 (online supplement) for details of the search terms and parameters. We checked the reference lists of studies identified in the search, related review articles and management guidelines. We contacted authors of unpublished studies that had completed recruitment when there was a registered protocol available on a trial register, such as Clinical Trials. We posted a list of identified studies on the website of the International Society for Traumatic Stress website and asked the membership to identify studies that we might have missed.
2.2. Study selection
Study selection followed the procedure in our previous review (Roberts et al., Citation2009). Study abstracts were read independently by two of the reviewers to determine if they potentially met the inclusion criteria. The full manuscript of all studies that either reviewer felt potentially met the criteria were obtained and read independently by two reviewers. To be included, a study had to be an RCT that considered one or more defined psychological intervention or treatment aimed at preventing or reducing traumatic stress symptoms in adults following events that appeared to fulfill criteria for a traumatic event according to DSM or ICD PTSD diagnostic descriptions (excluding single session preventative interventions), in comparison with a placebo, other control (e.g. usual care or waiting list control) or alternative psychological treatment condition. All studies had to have been completed and analysed by October 2018 with an available study manuscript. Presence or absence of symptoms, sample size, publication status and language of publication were not used to determine whether a study should be included. The review considered studies involving adults aged 18 and over only. In cases where there were a combination of adults and adolescents, at least 80% of the sample had to be 18 or over.
2.3. Data extraction
A data extraction sheet was designed to capture data which was then entered into Review Management 5 (RevMan-5.3) software (Review Manager [RevMan], Citation2014). Information extracted included demographic details of participants, inclusion and exclusion criteria, details of the traumatic event, the randomization process, the interventions used, drop-out rates and outcome data. Study quality was assessed with the Cochrane Collaboration’s tool for assessing risk of bias (Higgins et al., Citation2011) using the domains: sequence generation, allocation concealment (selection bias), blinding of assessors (detection bias), incomplete outcome data (attrition bias), selective outcome reporting, and other sources of bias. Data were extracted and quality assessed by two reviewers independently. Any disagreements were discussed with a third reviewer and a consensus achieved.
2.4. Data synthesis
In line with our previous review (Roberts et al., Citation2009) we separated trials into three separate groups:
Studies that have offered intervention beginning within three months to any individual exposed to a traumatic event irrespective of their symptoms with the aim of preventing PTSD.
Interventions begun within three months with the aim of preventing PTSD or ongoing distress in individuals with traumatic stress symptoms.
Interventions begun within three months with the aim of treating ASD or PTSD in individuals who already met diagnosis.
In our previous review we combined data from all studies evaluating interventions aimed at any individual exposed to a traumatic event irrespective of their symptoms in one meta-analysis (Roberts et al., Citation2009). In contrast, in this review we only combined data from studies of similar interventions for all the above groupings. We previously identified several studies evaluating CBT-T for individuals with traumatic stress symptoms. We considered undertaking evaluation of CBT-T studies by specific intervention but we took the view that there were insufficient studies following a specific model to make this approach meaningful at this time. As previously, CBT-T was defined as any intervention that focused on the trauma using written, imaginal or in-vivo exposure therapy with or without cognitive therapy and other cognitive behavioural techniques.
Our primary outcome was PTSD symptom severity as this is the outcome most widely reported in the traumatic stress literature (Bisson, Roberts, Andrew, Cooper, & Lewis, Citation2013). When an individual study reported both a clinician-administered and a self-report measure, primacy was given to outcomes using the clinician-administered measure. PTSD diagnosis was our other outcome of interest. We undertook analyses with follow-up data where this was available. Time points were decided a priori as post-treatment, three to six months post-trauma, seven to 12 months post-trauma, one to two years post-trauma, and two years and beyond, based on our knowledge of commonly used follow-up points used in previous early intervention studies.
Data were analysed for summary effects using the Review Manager 5.3 program (RevMan, Citation2014). All continuous outcomes were analysed using standard mean differences (SMD), in order to compare effects across analyses. SMD assumes that all scales are measuring the same underlying symptom or condition. Relative risk was calculated for diagnostic status. 95% confidence intervals were calculated for all outcomes. Available case analysis and intent to treat analysis with imputation using the last observation carried forward method were performed when enough information was available. In cases where there was inadequate information within the paper to perform these analyses further information was requested from the lead author.
Heterogeneity between studies was assessed by considering the I2 and chi2 test of heterogeneity. This statistic measures the percentage of variation that is not due to chance (Fletcher, Citation2007). An I2 of less than 30% was taken to indicate mild heterogeneity and a fixed effects model was used. When the I2 was greater or equal to 30% a random-effects model was used. A visual inspection of the forest plots was used as a test of robustness of these findings. We decided a priori that if a minimum of 10 studies were available in a meta-analysis, we would prepare funnel plots and examine them for signs of asymmetry. Where asymmetry was indicated, we planned to consider other possible reasons for this. We assessed the quality of evidence using the ‘Grades of Recommendation, Assessment, Development, and Evaluation’ (GRADE) approach (Guyatt, Oxman, Schünemann, Tugwell, & Knottnerus, Citation2011, Guyatt et al., Citation2013; Langendam et al., Citation2013) using five factors: limitations in study design and implementation of available studies, indirectness of evidence, unexplained heterogeneity or inconsistency of results, imprecision of effect estimates, and potential publication bias. The quality of evidence for each comparison was graded according to our confidence that the estimate of effect would remain unchanged as a result of further research. A high rating indicates that further research is very unlikely to change our confidence in the estimate of effect; a moderate rating indicates that research is likely to have an important impact on the confidence in the estimate of effect and may change the estimate; low quality indicates that further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate; very low quality indicates that the estimate of effect is very uncertain. Finally, we rated findings in terms of clinical importance. We used a definition of clinical importance, which was developed by the ISTSS Treatment Guidelines Committee and approved by the ISTSS Board and membership (Bisson et al., Citation2019), building on previous work by the National Institute of Health and Care Excellence (National Collaborating Centre for Mental Health, Citation2005). To be rated clinically important, an early intervention had to demonstrate an effect size of >0.5 for continuous outcomes for wait list control comparisons, >0.4 for placebo control comparisons and >0.2 for active treatment control comparisons. For relative risk outcomes an effect of <0.8 was required. When only one study, evaluating a specific intervention, was available its findings could not be judged as clinically important, unless the sample size was large (>300 participants). Non-inferiority RCT evidence alone was not sufficient to recommend an intervention as clinically important.
Following the procedure undertaken previously (Roberts et al., Citation2009), to determine the impact of quality on outcome we decided that we that we would undertake a sensitivity analysis for allocation concealment. Inadequate allocation concealment has been found to have influence the degree of effect in research trials and is thought to be one of the more important features of risk of bias (Hewitt, Hahn, Torgerson, Watson, & Bland, Citation2005). We therefore decided that we would investigate whether there was any indication of differential treatment effects through a sensitivity analysis to see if there was a change in the magnitude of effect and confidence intervals, excluding studies rated to have a high or unclear risk of bias for allocation concealment.
3. Results
Figure one displays the results of the systematic searches. In addition to the 25 studies and two long-term outcome studies included in the previous review, 6704 additional titles and abstracts were identified as a result of the search process and 204 papers were reviewed in detail by two of the authors independently to establish if they met the specified inclusion criteria. Thirty-six new studies were found to meet the inclusion criteria along with one paper reporting long term follow-up data for one of the newly identified studies, giving a total of 61 studies plus three long-term follow-up studies. Twenty seven of the 61 studies evaluated preventative interventions, aimed at anyone exposed to the relevant traumatic event; the other 34 studies evaluated early treatment interventions in individuals with early traumatic stress symptoms; of these 14 were studies where participants met diagnosis for ASD or PTSD. Fifty-nine studies were reported in English, one was in French (Andre, Lelord, Legeron, Reignier, & Delattre, Citation1997) and one in Persian (Taghizadeh, Jafarbegloo, Arbabi, & Faghihzadeh, Citation2008). A flow diagram of the systematic review can be seen in . The characteristics of all studies identified in this search and the previous review are described in , with inclusion and exclusion criteria in Table S1 (see online supplement).
Table 1. Description of included studies.
3.1. Synthesis of results
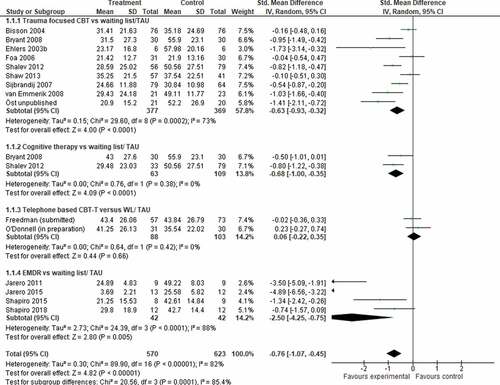
The outcomes for individual studies are shown in . The post intervention and follow-up results of the meta-analyses for comparisons that included more than one study are shown in with examples of Forest plots in and . The outcomes reported are severity of PTSD and rates of PTSD.
Table 2. Summary of meta-analysis of results for interventions.
Figure 2. Forest plot of PTSD severity, post treatment for studies offering intervention to individuals involved in a traumatic event irrespective of their symptoms.
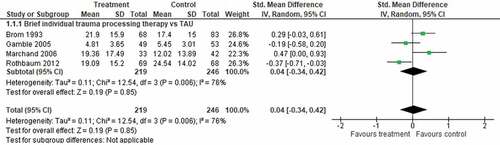
Figure 3. Forest plot of PTSD severity, post treatment for studies of interventions begun within three months with the aim of preventing PTSD or ongoing distress in individuals with traumatic stress symptoms.
3.1.1. Studies offering intervention to individuals involved in a traumatic event irrespective of their symptoms
Twenty-seven studies (Als et al., Citation2015; Biggs et al., Citation2016; Borghini et al., Citation2014; Brom et al., Citation1993; Brunet et al., Citation2013; Cox et al., Citation2018; Curtis et al., Citation2016; Gamble, Citation2010; Gamble et al., Citation2005; Gidron et al., Citation2001, Citation2007; Holmes et al., Citation2007; Irvine et al., Citation2011; Jensen et al., Citation2016; Jones et al., Citation2010; Kazak et al., Citation2005; Lindwall et al., Citation2014; Marchand et al., Citation2006; Mouthaan et al., Citation2013; Rothbaum et al., Citation2012; Ryding et al., Citation1998, Citation2004; Wang et al., Citation2015; Wijesinghe et al., Citation2015; Zatzick et al., Citation2001) evaluated brief psychosocial interventions aimed at preventing PTSD in individuals exposed to a specific traumatic event. All started within one month of the trauma. Seven studies (Brom et al., Citation1993; Gamble et al., Citation2005; Gidron et al., Citation2001, Citation2007; Marchand et al., Citation2006; Rothbaum et al., Citation2012; Ryding et al., Citation1998) used an approach which we grouped as ‘brief individual trauma processing’. These studies evaluated a number of brief therapies that were theoretically diverse but shared similar core treatment components. These included: psychoeducation and therapist directed reliving of the index trauma to promote elaboration of the trauma memory and help to contextualize or reframe aspects of the experience. We found no statistical difference between brief individual trauma processing approaches and usual care or a supportive listening control intervention at any time point (see ). We did find evidence to support the use of brief CBT based dyadic therapy over treatment as usual, at 3 months (Brunet et al., Citation2013; Kazak et al., Citation2005) but this effect was not judged clinically important. A single study showed a significant difference in PTSD severity for self-guided internet-based intervention over treatment as usual (Mouthaan et al., Citation2013) at 1 month (N = 300; SMD −0.38 CI −0.61 to −0.15; GRADE low) and 3–6 months post trauma (N = 300; SMD −0.27 CI −0.50 to −0.04; GRADE low) but not at 7–12 months (N = 300 SMD 0.00 CI −0.23 to 0.23; GRADE low). These effects were not judged clinically important. One single study showed no significant difference for intensive care diaries over delayed access to intensive care diaries at 3–6 months but did show a significant difference for PTSD diagnosis (N = 322; RR 0.38 CI 0.17 to 0.82; GRADE low). Another single study evaluating telephone-based CBT following cardioverter defibrillator transplant (Irvine et al., Citation2011) found no difference to usual care at 3–6 months but there was a difference at 7–12 months (N = 185; SMD −0.38 CI −0.67 to −0.09; GRADE low). This effect was not judged clinically important.
No differences were found for group counselling (Ryding et al., Citation2004), a three step parenting intervention following premature birth (Borghini et al., Citation2014), brief interpersonal counselling (Holmes et al., Citation2007), communication facilitator in an intensive care setting (Curtis et al., Citation2016), supported psychoeducation (Als et al., Citation2015), a nurse led intensive care recovery program (Jensen et al., Citation2016), or collaborative care (Zatzick et al., Citation2001). Six studies did not provide data that we were able to interrogate because data were not adequately reported in study papers and we were unable to obtain additional data from study authors (Andre et al., Citation1997; Biggs et al., Citation2016; Lindwall et al., Citation2014; Taghizadeh et al., Citation2008; Wang et al., Citation2015; Wijesinghe et al., Citation2015). Of these, one study (Taghizadeh et al., Citation2008) reported a difference in PTSD severity for counselling at 3–6 months over usual care (N = 300) for women who had experienced a traumatic birth. Positive findings were not reported for PTSD outcomes in other studies.
3.1.2. Studies offering intervention to individuals with traumatic stress symptoms within three months of a traumatic event
Thirty-four studies (Ben-Zion et al., Citation2018; Bisson et al., Citation2004; Bryant et al., Citation1998, Citation1999, Citation2003, Citation2005, Citation2008; Bugg et al., Citation2009; Cernvall et al., Citation2015; Echeburua et al., Citation1996; Ehlers et al., Citation2003; Foa et al., Citation2006; Freedman, Citationn.d., Citationin press; Freyth et al., Citation2010; Jarero et al., Citation2011, Citation2015; Nixon, Citation2012; Nixon et al., Citation2016; O’Donnell et al., Citationn.d., Citation2012; Öst et al., Citationn.d.; Shalev et al., Citation2012; Shapiro & Laub, Citation2015; Shapiro et al., Citation2018; Shaw et al., Citation2013; Sijbrandij et al., Citation2007; Skogstad et al., Citation2015; van Emmerik et al., Citation2008; Wagner et al., Citation2007; Wu et al., Citation2014; Zatzick et al., Citation2004, Citation2013, Citation2015) evaluated interventions for individuals with traumatic stress symptoms beginning within three months of a traumatic event. Statistically significant differences were found in favour of CBT-T over wait list and supportive counselling at initial follow-up for PTSD severity (see ). Findings for both comparisons were judged to be clinically important. Follow-up data were incomplete but statistically significant differences were present at several time points. A post hoc sub-group analysis suggested that effects were largest for interventions of 12 or more sessions (K = 3; N = 181; SMD −1.11 CI-1.62, −0.61) when compared against wait list. Statistically significant differences for PTSD severity were also found for cognitive therapy without exposure and EMDR over wait list at initial follow-up. One single study (van Emmerik et al., Citation2008) showed a significant difference for structured writing therapy over wait list (N = 45; SMD −0.97 CI −1.59, −0.35; GRADE very low) but there was no difference when compared against psychoeducation only (Bugg et al., Citation2009) in another single study. Another single study (Cernvall et al., Citation2015) showed a significant difference for internet-based guided self-help over wait list (N = 58; SMD −0.66 CI −1.19, −0.13: GRADE very low). Findings for cognitive therapy and EMDR were judged as clinically important. No significant differences were found between telephone based CBT-T and wait list or, from single studies of behavioural activation (Wagner et al., Citation2007) and internet-based virtual reality therapy over wait list (Freedman, Citationn.d.). No difference was found between computerized neurobehavioral training and a reading-based control condition (Ben-Zion et al., Citation2018). We found a significant effect for collaborative care over wait list at 3–6 months post-trauma but there was no effect at 1 month or 7–12 months. These effects were not judged clinically important. In head to head comparisons we found no difference between CBT-T and self-help or trauma focused CBT and cognitive therapy.
3.1.3. Studies offering intervention to individuals with a diagnosis of acute stress disorder or PTSD
Fourteen studies (Bryant et al., Citation1998, Citation1999, Citation2003, Citation2005, Citation2008; Echeburua et al., Citation1996; Ehlers et al., Citation2003; Nixon, Citation2012; Nixon et al., Citation2016; Öst et al., Citationn.d.; Shalev et al., Citation2012; Sijbrandij et al., Citation2007; van Emmerik et al., Citation2008; Wagner et al., Citation2007) offered interventions to individuals with a diagnosis of acute stress disorder or PTSD, within three months of the traumatic event. Statistically significant differences were found in favour of CBT-T over a wait list control group and supportive counselling post treatment. Follow-up data were incomplete but statistically significant differences were present at some follow-up time points. There was also a significant difference in favour of cognitive therapy over waitlist. There was no difference in head to head comparison between CBT-T and cognitive therapy.
3.2. Methodological quality of included studies
Risk of bias judgements for individual studies are shown in Table S2 (see online supplement). Thirty-six studies adequately described a method of allocation judged to make no bias possible. Five studies were considered to be at high risk of bias. Reporting of adequate concealment procedures was present in 25 studies, with six studies considered to be at high risk of bias. Adequate blinding of the assessor of outcome measures was present in 42 studies, with 4 studies considered to be at high risk. Incomplete outcome data was considered low risk in 26 studies, with a further 22 studies judged to be at high risk of bias. Twelve studies, all published since 2010, were judged low risk for selective reporting. The majority of other studies were of unclear risk, with three studies being judged at high risk. Forty studies were judged at high risk for other bias. Reasons for possible other bias included author affiliation with one of the interventions being tested, small sample size, use of measures with inadequate validation, non-manualized intervention and poor treatment adherence. No risk of bias was indicated in only eight studies. There were insufficient studies in any of the meta-analyses to allow us to investigate for potential publication bias by preparing funnel plots.
To determine the impact of quality on outcome we undertook a sensitivity analysis for allocation concealment. Four studies with low risk of bias for allocation concealment evaluating CBT-T versus waitlist were included in a sensitivity analysis. We compared the effect size and confidence intervals from this analysis with that of the full analysis to identify possible differences. There was little differences to the estimated effect size (N = 367, SMD −0.61 CI −1.05, −0.17) from that of the original analysis (N = 746, SMD −0.63 CI −0.93, −0.32). We were unable to repeat this sensitivity analysis for CBT-T versus supportive counselling as no study was rated low risk of bias for allocation concealment.
4. Discussion
4.1. Main findings
There was little evidence that most multiple session intervention aimed at everyone, irrespective of their symptoms, following a traumatic event were effective. Where there was evidence of significant effects, these effects were judged as not being clinically important on our primary outcome measure.
CBT-T, cognitive therapy without exposure, EMDR, structured writing therapy and internet-based guided self-help all did significantly better than waitlist/usual care at reducing traumatic stress symptoms in individuals who were symptomatic at entry into the study. Findings for CBT-T, EMDR and cognitive therapy without exposure were judged as clinically important. CBT-T was the most frequently evaluated approach but EMDR showed the largest effects with positive findings from four small studies. Findings in relation to structured writing therapy and internet-based guided self-help were from single small studies. CBT-T was the only approach to be thoroughly evaluated against an active control, with evidence of significant and clinically important effects in relation to supportive counselling. Only CBT-T and cognitive therapy were evaluated for individuals who were diagnosed with acute stress disorder or PTSD and the magnitude of effect was larger for these individuals. Evidence of the benefits of CBT-T for symptomatic individuals who did not meet full diagnostic criteria for these conditions was weaker. Although intervention in many of the positive trials included in this review began more than a month after the trauma, there was evidence of the benefit of both CBT-T and EMDR being offered within 2–4 weeks from a number of trials (Bryant et al., Citation1998, Citation1999, Citation2003, Citation2005, Citation2008; Jarero et al., Citation2011, Citation2015), suggesting that it is appropriate to offer early intervention, when indicated within this acute phase. With the exception of one study evaluating cognitive therapy based on the Ehlers & Clarke model (Ehlers et al., Citation2003), the majority of positive trials of CBT-T were based on adapted versions of prolonged exposure. Several well-controlled studies evaluated a collaborative/stepped care approach for individuals with traumatic stress symptoms beginning within three months of a traumatic event. In meta-analysis there was evidence of an effect at 3–6 months; findings were not judged clinically important. The GRADE ratings for most meta-analyses was low to very low suggesting that further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate, for findings rated low and findings should be considered uncertain for findings rated very low. There was considerable variability in the timing and collection of medium and long-term follow-up data which made it difficult to draw firm conclusions about the maintenance of effects over time. Although there was some inconsistent evidence of long-term benefit for CBT-T.
4.2. Heterogeneity
There was evidence of both clinical and statistical heterogeneity in the included studies. There were significant differences in the clinical populations across the included studies, especially with regards to the nature of trauma exposure and the psychiatric and physical severity of symptoms on entry into the studies. Of note, participants in some studies had experienced serious and life threatening medical conditions associated with a chronic illness and it is likely that intervention outcomes in these studies would be influenced by the degree and pace of physical recovery and enduring health problems (e.g. Cox et al., Citation2018; Irvine et al., Citation2011; Jensen et al., Citation2016; Jones et al., Citation2010). Studies also differed in the methodologies that they used, for example with regard to sources of recruitment and inclusion and exclusion criteria.
Although all the trials attempted to reduce traumatic stress symptoms, the nature of the interventions and target populations were diverse. This was partially dealt with by separating interventions into predetermined groups for studies offering intervention to individuals with traumatic stress symptoms within three months of a traumatic event and studies offering intervention to individuals with a diagnosis of acute stress disorder or PTSD, although some interventions did not fit with these pre-planned groups and this resulted in some unplanned categorizations. We attempted to group studies in a clinically meaningful way with regards to the intervention and the clinical populations included but recognize that this is not empirically based and would have contributed to heterogeneity. This should be borne in mind when interpreting our findings (Borenstein, Hedges, Higgins, & Rothstein, Citation2009). Some interventions and populations were so dissimilar that it was meaningless to group them at all, particularly for studies evaluating interventions aimed at any individual, regardless of symptoms.
As in our previous review (Roberts et al., Citation2009), there were more studies evaluating CBT-T than other interventions. Most CBT-T studies were based on a prolonged exposure paradigm, but the specific CBT-T interventions varied in their use of imaginal exposure, in-vivo exposure and cognitive techniques. Two studies were based on a cognitive processing therapy paradigm (Nixon, Citation2012; Nixon et al., Citation2016) and showed no effect when compared against supportive counselling. The total number of hours of intervention provided varied from around two hours to around 16 hours. A post hoc sub-group analysis suggested the effects were larger for studies offering more sessions of CBT-T. However, the largest treatment effect that we observed was for brief EMDR which at 2–4½ hours were amongst the shortest interventions that were included.
4.3. Methodological quality
The overall quality of the studies was varied. Using the Cochrane risk of bias criteria, the proportion of studies describing appropriate randomization, allocation concealment and blinding of assessors was higher than in our previous review. It is possible that other included studies also used appropriate randomization and allocation concealment procedures but reporting of these procedures was sometimes limited. The proportion of studies with low risk for incomplete outcome data was low (43%), suggesting that many studies had difficulties with retention. Pre-registration of trial protocols was an emerging issue at the time of our previous review and none of the studies previously included provided a pre-publication protocol. Only a third of the newly included studies provided pre-registered study protocols and reported outcomes consistent with these protocols. Few studies were free of other biases. These biases included author affiliation with one of the interventions being tested, small sample size, use of measures with inadequate validation, non-manualized intervention and poor treatment adherence.
Many of the included studies had some methodological limitations. However, a sensitivity analysis of higher quality studies based on allocation concealment made little difference to the estimated effect of CBT-T. This suggests that study quality did not have a major effect in elevating apparent efficacy in this key comparison; although we could not undertake similar sensitivity analyses in other smaller comparisons. There is evidence that smaller studies can exaggerate intervention effects as they tend not to be conducted with the same methodological rigour as larger trials (Higgins & Green, Citation2011). Many of the trials in this review were small and this needs to be borne in mind when considering the large effects of some of our findings. For example, the large effect in favour of EMDR over waiting list was a result of 4 trials with a total of 84 participants.
Four studies evaluated a collaborative/stepped care approach (O’Donnell et al., Citation2012; Zatzick et al., Citation2004, Citation2013, Citation2015). The specific collaborative care models differed across these studies, with intervention potentially ongoing to 12 months in some trials. Intervention effects in one smaller study (O’Donnell et al., Citation2012) were noticeably larger than for the other studies. This study differed from the other studies in that participants were screened for elevated symptoms on two occasions which meant that only participants who demonstrated high symptom severity were randomized and then offered a menu of interventions. The other studies allocated patients at an earlier time point and it is likely that some patients would have experienced natural recovery. Whilst effects across these studies was small, it has been argued that collaborative care based approaches can have a larger population impact than early interventions such as CBT-T, when intervention reach is taken into account (Giummarra et al., Citation2018; Zatzick, Koepsell, & Rivara, Citation2009).
There was only very limited reporting of adverse events. Where adverse events were reported, this was mainly in trials where there was a high risk of mortality in included participants, resulting from chronic illnesses (e.g. Irvine et al., Citation2011-Jones et al., Citation2010). We did not see evidence of significant differences in rates of dropout between intervention and control conditions, which continues to suggest that adverse effects were not common. Despite our previous recommendation there was an absence of tolerability assessment, evaluating the acceptability of interventions, in new studies. We were unable to investigate for publication bias. Many of the studies reported in this review did report null results and we enquired about non-published studies that had registered a study protocol. However, we cannot exclude the possibility that some of our findings may have been influenced by some non-reporting of negative findings.
4.4. Implications for practice
Consistent with our previous review, the current findings suggest that psychological intervention offered to all individuals exposed to a traumatic event irrespective of their symptoms cannot be recommended for routine use following traumatic events. Several interventions – CBT-T, cognitive therapy without exposure, EMDR, structured writing therapy, and internet-based guided self-help – provided evidence of efficacy in reducing traumatic stress symptoms, when targeted at symptomatic individuals. Evidence was strongest for CBT-T and for those who fulfilled the diagnostic criteria for acute stress disorder or PTSD. We believe that this evidence is now sufficiently strong to recommend the provision of CBT-T, cognitive therapy or brief EMDR to individuals who are symptomatic following exposure to a traumatic event, as was recommended in the recent ISTSS PTSD Treatment Guidelines (International Society for Traumatic Stress Studies, Citation2018). However, we note that the National Institution for Health and Care Excellence had access to the same evidence base but only felt able to recommend CBT-T (National Institute for Health and Care Excellence, Citation2018). We also note that positive studies were mainly those including victims of accidental physical injury, such as industrial accidents and motor vehicle accidents; physical assault/violent crime; and terrorism. Only one small positive trial was undertaken following a natural disaster (Jarero et al., Citation2011). We did not identify any positive studies that were carried out with military personnel and studies conducted mainly or solely with victims of rape and sexual assault were not positive (Echeburua et al., Citation1996; Foa et al., Citation2006). This needs to be borne in mind when considering the generalizability of these findings.
Whilst no intervention aimed at all individuals exposed to a traumatic event provided clinically important findings for a reduction in traumatic symptoms, small significant differences were observed for brief CBT based dyadic therapy, self-guided internet-based intervention and intensive care diaries at 3–6 months. Given that many individuals experience improvement in traumatic stress symptoms without the need for intervention, it is possible that that these interventions may demonstrate a greater effect if targeted at symptomatic individuals. This should be examined further.
Findings from this review provide a strengthening case for early routine detection and assessment of individuals exposed to traumatic events and the provision of early psychological intervention when needed, although optimal models of care require further exploration. This is consistent with recent work which suggests that early structured clinician based PTSD assessment using the Clinician Administered PTSD Scale can predict the likelihood of developing long-term PTSD with a high degree of accuracy, across a number of different cultures (Shalev et al., Citation2019). Arguably, routine use of detection-based approaches would help to reduce the incidence of chronic disorders and associated secondary problems discussed earlier (McFarlane, Citation2010). Self-guided (Mouthaan et al., Citation2013) and guided self-help (Cernvall et al., Citation2015) potentially offer a flexible and cost-effective means of increasing availability of intervention and should be investigated further.
This review did not focus on the use of pharmacological early interventions. Other work that we have undertaken for the ISTSS Treatment Guidelines suggests that the evidence for such interventions is currently very limited (Astill-Wright et al., Citationin press; International Society for Traumatic Stress Studies, Citation2018). However, we recognize that medication may still have a role in holistic patient care, when indicated, following trauma exposure.
4.5. Implications for research
Several interventions included in this review showed promising outcomes but have not been thoroughly evaluated in well-designed RCTs, with long-term follow-up. EMDR, cognitive therapy and structured writing therapy all require further evaluation and may benefit from head to head comparison with an evaluated CBT-T based intervention. A number of other interventions included in this review, such as behavioural activation (Wagner et al., Citation2007), have also not been adequately investigated and would benefit from further investigation. Optimal length of early intervention should also be explored further, given our finding that effects were larger for 12 or more sessions of CBT-T. Future reviews should consider whether the literature is sufficiently developed to evaluate CBT-T based interventions by treatment model. New technologies have the potential to increase the range of options and modes of delivery of early psychological interventions. We included several studies investigating these approaches in this review (e.g. Ben-Zion et al., Citation2018; Freedman, Citationn.d.). Development and evaluation of these approaches are in their infancy but they potentially offer new ways of preventing and ameliorating early symptoms. A further limitation of this review is that we only focused on the prevention and early treatment of PTSD. Future studies and reviews should also focus on the prevention of other common mental health problems such as depression and anxiety disorders following from trauma.
Supplemental Material
Download MS Word (34.1 KB)Acknowledgements
We wish to express our thanks to authors of studies in the review for providing unpublished data, the Cochrane Common Mental Disorders Group for his help with searches and with translation and the International Society for Traumatic Stress Studies Treatment Guideline Committee for help with the methodological framework. Neil Roberts had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosure statement
Jonathan Bisson has published one RCT that was included in the review. The other authors report no competing interests. Neil Roberts, Neil Kitchiner, Catrin Lewis and Jonathan Bisson have all been involved in the development of an internet based guided self-help intervention for PTSD called SPRING and may receive future profits if the intervention is monetized.
Supplementary Material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Als, L. C. , Nadel, S. , Cooper, M. , Vickers, B. , & Garralda, M. E. (2015). A supported psychoeducational intervention to improve family mental health following discharge from paediatric intensive care: Feasibility and pilot randomised controlled trial. BMJ Open , 5(suppl 12), e009581.
- Andre, C. , Lelord, F. , Legeron, P. , Reignier, A. , & Delattre, A. (1997). Etude controlee sur l’efficacite a 6 mois d’une prise en charge precoce de 132 conducteurs d’autobus victims d’agression [Effectiveness of early intervention on 132 bus drivers victims of aggressions: A controlled trial]. L’Encephale , 23, 65–25.
- Astill-Wright, L. , Sibrandij, M. , Sinnerton, R. , Lewis, C. , Roberts, N. P. , & Bisson, J. I. (in press). Pharmacological prevention and early treatment of post-traumatic stress disorder and acute stress disorder: a systematic review and meta-analysis. Translational Psychiatry
- Atwoli, L. , Stein, D. J. , Koenen, K. C. , & McLaughlin, K. A. (2015). Epidemiology of posttraumatic stress disorder: Prevalence, correlates and consequences. Current Opinion in Psychiatry , 28(4), 307–311.
- Bastos, M. H. , Furuta, M. , Small, R. , McKenzie‐McHarg, K. , & Bick, D. (2015). Debriefing interventions for the prevention of psychological trauma in women following childbirth. Cochrane Database of Systematic Reviews , 10(suppl 4), CD007194.
- Ben-Zion, Z. , Fine, N. B. , Keynan, N. J. , Admon, R. , Green, N. , Halevi, M. , & Shalev, A. Y. (2018). Cognitive flexibility predicts ptsd symptoms: Observational and interventional studies. Frontiers in Psychiatry , 9, 477.
- Berger, W. , Coutinho, E. S. , Figueira, I. , Marques-Portella, C. , Luz, M. P. , Neylan, T. C. , & Mendlowicz, M. V. (2012). Rescuers at risk: A systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology , 47(suppl 6), 1001–1011.
- Biggs, Q. M. , Fullerton, C. S. , McCarroll, J. E. , Liu, X. , Wang, L. , Dacuyan, N. M. , & Ursano, R. J. (2016). Early intervention for post-traumatic stress disorder, depression, and quality of life in mortuary affairs soldiers postdeployment. Military Medicine , 181(suppl 11), e1553–60.
- Bisson, J. I. , Berliner, L. , Cloitre, M. , Forbes, D. , Jensen, T. K. , Lewis, C. , … Shapiro, F. (2019). The international society for traumatic stress studies new guidelines for the prevention and treatment of posttraumatic stress disorder: Methodology and development process. Journal of Traumatic Stress . doi:10.1002/jts.22421
- Bisson, J. I. , Roberts, N. P. , Andrew, M. , Cooper, R. , & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults (review). Cochrane Database of Systematic Reviews , 12, CD003388.
- Bisson, J. I. , Shepherd, J. P. , Joy, D. , Probert, R. , & Newcombe, R. G. (2004). Early cognitive-behavioural therapy for post-traumatic stress symptoms after physical injury. British Journal of Psychiatry , 184, 63–69.
- Borenstein, M. , Hedges, L. V. , Higgins, J. P. T. , & Rothstein, H. R. (2009). Introduction to meta-analysis . New York: John Wiley & Sons.
- Borghini, A. , Habersaat, S. , Forcada-Guex, M. , Nessi, J. , Pierrehumbert, B. , Ansermet, F. , & Müller-Nix, C. (2014). Effects of an early intervention on maternal post-traumatic stress symptoms and the quality of mother-infant interaction: The case of preterm birth. Infant Behavior and Development , 37(suppl 4), 624–631.
- Brom, D. , Kleber, R. J. , & Hofman, M. (1993). Victims of traffic accidents: Incidence and prevention of post-traumatic stress disorder. Journal of Clinical Psychology , 49(suppl 2), 131–140.
- Brunet, A. , Des Groseilliers, I. B. , Cordova, M. J. , & Ruzek, J. I. (2013). Randomized controlled trial of a brief dyadic cognitive-behavioral intervention designed to prevent PTSD. European Journal of Psychotraumatology , 26, 4.
- Brunet, A. , Monson, E. , Liu, A. , & Fikretoglu, D. (2015). Trauma exposure and posttraumatic stress disorder in the Canadian military. The Canadian Journal of Psychiatry , 60(suppl 11), 488–496.
- Bryant, R. A. , Harvey, A. G. , Dang, S. T. , Sackville, S. T. , & Basten, C. (1998). Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology , 66(suppl 5), 862–866.
- Bryant, R. A. , Mastrodomenico, J. , Felmingham, K. L. , Hopwood, S. , Kenny, L. , Kandris, E. , … Creamer, M. (2008). Treatment of acute stress disorder: A randomized controlled trial. Archives Of General Psychiatry , 65, 659–667.
- Bryant, R. A. , Moulds, M. , Guthrie, R. , & Nixon, R. D. V. (2003). Treating acute stress disorder following mild traumatic brain injury. American Journal of Psychiatry , 160, 585–587.
- Bryant, R. A. , Moulds, M. L. , Guthrie, R. M. , & Nixon, R. D. V. (2005). The additive benefit of hypnosis and cognitive-behavioral therapy in treating acute stress disorder. Journal of Consulting and Clinical Psychology , 73, 334–340.
- Bryant, R. A. , Moulds, M. L. , Nixon, R. D. V. , Mastrodomenico, J. , Felmingham, K. , & Hopwood, S. (2006). Hypnotherapy and cognitive behaviour therapy of acute stress disorder: A 3 year follow-up. Behaviour Research and Therapy , 44, 1331–1335.
- Bryant, R. A. , Moulds, M. L. , & Nixon, R. V. D. (2003). Cognitive behaviour therapy of acute stress disorder: A four-year follow-up. Behaviour Research and Therapy , 41, 489–494.
- Bryant, R. A. , Sackville, T. , Dang, S. T. , Moulds, M. , & Guthrie, R. (1999). Treating acute stress disorder: An evaluation of cognitive behavior therapy and supportive counseling techniques. The American Journal of Psychiatry , 156(suppl 11), 1780–1786.
- Bugg, A. , Turpin, G. , Mason, S. , & Scholes, C. (2009). A randomised controlled trial of the effectiveness of writing as a self-help intervention for traumatic injury patients at risk of developing post-traumatic stress disorder. Behaviour Research and Therapy , 47, 6–12.
- Cernvall, M. , Carlbring, P. , Ljungman, L. , Ljungman, G. , & von Essen, L. (2015). Internet-based guided self-help for parents of children on cancer treatment: A randomized controlled trial. Psycho-oncology , 24(suppl 9), 1152–1158.
- Cox, C. E. , Hough, C. L. , Carson, S. S. , White, D. B. , Kahn, J. M. , Olsen, M. K. , & Porter, L. S. (2018). Effects of a telephone- and web-based coping skills training program compared with an education program for survivors of critical illness and their family members a randomized clinical trial. American Journal of Respiratory and Critical Care Medicine , 197(suppl 1), 66–78.
- Curtis, J. R. , Treece, P. D. , Nielsen, E. L. , Gold, J. , Ciechanowski, P. S. , Shannon, S. E. , & Engelberg, R. A. (2016). Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. American Journal of Respiratory and Critical Care Medicine , 193(suppl 2), 154–162.
- Dworkin, E. R. , Menon, S. V. , Bystrynski, J. , & Allen, N. E. (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review , 56, 65–81.
- Echeburua, E. , de Corral, P. , Sarasua, B. , & Zubizarreta, I. (1996). Treatment of acute posttraumatic stress disorder in rape victims: An experimental study. Journal of Anxiety Disorders , 10(suppl 3), 185–199.
- Ehlers, A. , Clark, D. , Hackmann, A. , McManus, F. , Fennell, M. , Herbert, C. , & Mayou, R. (2003). A randomized controlled trial of cognitive therapy, a self-help booklet and repeated assessments as early interventions for posttraumatic stress disorder. Archives Of General Psychiatry , 60(suppl 10), 1024–1032.
- Ferry, F. R. , Brady, S. E. , Bunting, B. P. , Murphy, S. D. , Bolton, D. , & O’Neill, S. M. (2015). The economic burden of PTSD in Northern Ireland. Journal of Traumatic Stress , 28(suppl 3), 191–197.
- Fletcher, J. (2007). What is heterogeneity and is it important? BMJ , 334, 94–96.
- Foa, E. B. , Zoellner, L. A. , & Feeny, N. C. (2006). An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress , 19(suppl 1), 29–43.
- Forneris, C. A. , Gartlehner, G. , Brownley, K. A. , Gaynes, B. N. , Sonis, J. , Coker-Schwimmer, E. , … Lohr, K. N. (2013). Interventions to prevent post-traumatic stress disorder: A systematic review. American Journal of Preventive Medicine , 44(6), 635–650.
- Freedman, S. (in press). Early telephone cognitive behavioral therapy (ET-CBT) for the prevention of PTSD. European Journal of Psychotraumatology.
- Freedman, S. (n.d.). Early intervention for preventing posttraumatic stress disorder: An internet based treatment . Manuscript in preparation.
- Freedman, S. A. , Dayan, E. , Kimelman, Y. B. , Weissman, H. , & Eitan, R. (2015). Early intervention for preventing posttraumatic stress disorder: An internet-based virtual reality treatment. European Journal of Psychotraumatology , 6 (1). doi:10.3402/ejpt.v6.25608
- Freyth, C. , Elsesser, K. , Lohrmann, T. , & Sartory, G. (2010). Effects of additional prolonged exposure to psychoeducation and relaxation in acute stress disorder. Journal of Anxiety Disorders , 24(suppl 8), 909–917.
- Gamble, J. (2010). Do women who have experienced a traumatic birth and are provided with a midwife led counselling intervention compared with parenting support experience lower levels of postnatal distress? Australian New Zealand Trials Registry . Retrieved from https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=320476
- Gamble, J. , Creedy, D. , Moyle, W. , Webster, J. , McAllister, M. , & Dickson, P. (2005). Effectiveness of a counseling intervention after a traumatic childbirth: A randomized controlled trial. Birth , 32(suppl 1), 11–19.
- Gidron, Y. , Gal, R. , Freedman, S. , Twiser, I. , Lauden, A. , Snir, Y. , & Benjamin, J. (2001). Translating research findings to PTSD prevention: Results of a randomized-controlled pilot study. Journal of Traumatic Stress , 14(suppl 4), 773–780.
- Gidron, Y. , Gal, R. , Givati, G. , Lauden, A. , Snir, Y. , & Benjamin, J. (2007). Interactive effects of memory structuring and gender in preventing posttraumatic stress symptoms. The Journal of Nervous and Mental Disease , 195(suppl 2), 1–4.
- Giummarra, M. J. , Lennox, A. , Dali, G. , Costa, B. , & Gabbe, B. J. (2018). Early psychological interventions for posttraumatic stress, depression and anxiety after traumatic injury: A systematic review and meta-analysis. Clinical Psychology Review , 62, 11–36.
- Greenberg, P. E. , Sisitsky, T. , Kessler, R. C. , Finkelstein, S. N. , Berndt, E. R. , Davidson, J. R. T. , & Fyer, A. J. (1999). The economic burden of anxiety disorders in the 1990s. The Journal of Clinical Psychiatry , 60, 427–435.
- Guyatt, G. H. , Oxman, A. D. , Schünemann, H. J. , Tugwell, P. , & Knottnerus, A. (2011). GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology , 64(suppl 4), 380–382.
- Guyatt, G. H. , Oxman, A. D. , Sultan, S. , Brozek, J. , Glasziou, P. , Alonso-Coello, P. , & Schünemann, H. J. (2013). GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. Journal of Clinical Epidemiology , 66(suppl2), 151–157.
- Hewitt, C. , Hahn, S. , Torgerson, D. J. , Watson, J. , & Bland, J. M. (2005). Adequacy and reporting of allocation concealment: Review of recent trials published in four general medical journals. BMJ , 330(7499), 1057–1058.
- Higgins, J. P. , Altman, D. G. , Gøtzsche, P. C. , Jüni, P. , Moher, D. , Oxman, A. D. , … Sterne, J. A. (2011). The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ , 343, d5928.
- Higgins, J. P. T. , & Green, S. (editors.). (2011). Cochrane handbook for systematic reviews of interventions version 5.1.0 . The Cochrane Collaboration. Retrieved from www.cochrane-handbook.org
- Holmes, A. , Hodgins, G. , Adey, S. , Menzel, S. , Danne, P. , Kossmann, T. , & Judd, F. (2007). Trial of interpersonal counselling after major physical trauma. Australian and New Zealand Journal of Psychiatry , 41(suppl 11), 926–933.
- International Society for Traumatic Stress Studies . (2018). Posttraumatic stress disorder prevention and treatment guidelines . Author. Retrieved from http://www.istss.org/treating-trauma/new-istss-guidelines.aspx
- Irvine, J. , Firestone, J. , Ong, L. , Cribbie, R. , Dorian, P. , Harris, L. , … Sears, S. (2011). A randomized controlled trial of cognitive behavior therapy tailored to psychological adaptation to an implantable cardioverter defibrillator. Psychosomatic Medicine , 73, 226–233.
- Jarero, I. , Artigas, L. , & Luber, M. (2011). The EMDR protocol for recent critical incidents: Application in a disaster mental health continuum of care context. Journal of EMDR Practice and Research , 5, 82–94.
- Jarero, I. , Uribe, S. , Artigas, L. , & Givaudan, M. (2015). EMDR protocol for recent critical incidents: A randomized controlled trial in a technological disaster context. Journal of EMDR Practice and Research , 9, 166–173.
- Jensen, J. F. , Egerod, I. , Bestle, M. H. , Christensen, D. F. , Elklit, A. , Hansen, R. L. , … Overgaard, D. (2016). A recovery program to improve quality of life, sense of coherence and psychological health in ICU survivors: A multicenter randomized controlled trial, the RAPIT study. Intensive Care Medicine , 42(suppl 11), 1733–1743.
- Jones, C. , Bäckman, C. , Capuzzo, M. , Egerod, I. , Flaatten, H. , Granja, C. , … RACHEL Group, T. (2010). Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: A randomised, controlled trial. Critical Care , 14(suppl 5), R168.
- Kazak, A. E. , Simms, S. , Alderfer, M. A. , Rourke, M. T. , Crump, T. , McClure, K. , … Reilly, A. (2005). Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. Journal of Pediatric Psychology , 30(suppl 8), 644–655.
- Kearns, M. C. , Ressler, K. J. , Zatzick, D. , & Rothbaum, B. O. (2012). Early interventions for PTSD: A review. Depression and Anxiety , 29(suppl 10), 833–842.
- Kessler, R. , Sonnega, A. , Bromet, E. , Hughes, M. , & Nelson, C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives Of General Psychiatry , 52, 1048–1060.
- Kessler, R. C. , Aguilar-Gaxiola, S. , Alonso, J. , Benjet, C. , Bromet, E. J. , Cardoso, G. , … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology , 8(sup5), 1353383.
- Langendam, M. W. , Akl, E. A. , Dahm, P. , Glasziou, P. , Guyatt, G. , & Schünemann, H. J. (2013). Assessing and presenting summaries of evidence in Cochrane reviews. Systematic Reviews , 23(2), 81.
- Lindwall, J. J. , Russell, K. , Huang, Q. , Zhang, H. , Vannatta, K. , Barrera, M. , … Phipps, S. (2014). Adjustment in parents of children undergoing stem cell transplantation. Biology of Blood and Marrow Transplantation , 20(suppl 4), 543–548.
- Lowe, S. R. , & Galea, S. (2017). The mental health consequences of mass shootings. Trauma, Violence, & Abuse , 18(suppl 1), 62–82.
- Marchand, A. , Guay, S. , Boyer, R. , Iucci, S. , Martin, A. , & St-Hilaire, M.-H. (2006). A randomized controlled trial of an adapted form of individual critical incident stress debriefing for victims of an armed robbery. Brief Treatment and Crisis Intervention , 6(suppl 2), 122–129.
- McFarlane, A. C. (2010). The long-term costs of traumatic stress: Intertwined physical and psychological consequences. World Psychiatry : Official Journal of the World Psychiatric Association (WPA) , 9(suppl 1), 3–10.
- McNally, R. J. , Bryant, R. A. , & Ehlers, A. (2003). Does early psychological intervention promote recovery from posttraumatic stress disorder? Psychological Science in the Public Interest , 4(suppl 2), 45–79.
- Mouthaan, J. , Sijbrandij, M. , de Vries, G. J. , Reitsma, J. B. , van de Schoot, R. , Goslings, J. C. , … Olff, M. (2013). Internet-based early intervention to prevent posttraumatic stress disorder in injury patients: Randomized controlled trial. Journal of Medical Internet Research , 15(suppl 8), e165.
- National Collaborating Centre for Mental Health . (2005). Post-traumatic stress disorder: The management of PTSD in adults and children in primary and secondary care . London: Gaskell.
- National Institute for Health and Care Excellence . (2018). Evidence reviews for psychological, psychosocial and other non-pharmacological interventions for the prevention of PTSD in adults: NICE guideline NG116. Retrieved from https://www.nice.org.uk/guidance/ng116
- Neria, Y. , Nandi, A. , & Galea, S. (2008). Post-traumatic stress disorder following disasters: A systematic review. Psychological Medicine , 38(suppl 4), 467–480.
- Nixon, R. D. V. (2012). Cognitive processing therapy versus supportive counseling for acute stress disorder following assault: A randomized pilot trial. Behavior Therapy , 43(suppl 4), 825–836.
- Nixon, R. D. V. , Best, T. , Wilksch, S. R. , Angelakis, S. , Beatty, L. J. , & Weber, N. (2016). Cognitive processing therapy for the treatment of acute stress disorder following sexual assault: A randomised effectiveness study. Behaviour Change , 33(suppl 4), 232–250.
- O’Donnell, M. , Lau, W. , Howard, A. , Alkemade, N. , Fletcher, S, Holmes, A., … Forbes, D. (n.d.). The efficacy of telephone delivered cognitive behavioural therapy as an early intervention for high anxiety and affective symptoms after injury . Draft manuscript.
- O’Donnell, M. L. , Lau, W. , Tipping, S. , Holmes, A. C. , Ellen, S. , Judson, R. , … Forbes, D. (2012). Stepped early psychological intervention for posttraumatic stress disorder, other anxiety disorders, and depression following serious injury. Journal of Traumatic Stress , 25(suppl 2), 125–133.
- Öst, L. , Paunovic, N. , & Gillow, A. (n.d.). Cognitive-behavior therapy in the prevention of chronic PTSD in crime victims . Unpublished.
- Review Manager (RevMan) [ Computer program]. (2014). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration.
- Roberts, N. P. , Kitchiner, N. J. , Kenardy, J. , & Bisson, J. I. (2009). Systematic review and meta-analysis of multiple session early interventions following traumatic events. American Journal of Psychiatry , 166(suppl 3), 293–301.
- Rose, S. C. , Bisson, J. , Churchill, R. , & Wessely, S. (2002). Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews , (2), CD000560.
- Rothbaum, B. O. , Kearns, M. C. , Price, M. , Malcoun, E. , Davis, M. , Ressler, K. J. , … Houry, D. (2012). Early intervention may prevent the development of posttraumatic stress disorder: A randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry , 72(suppl 11), 957–963.
- Ryding, E. , Wijma, K. , & Wijma, B. (1998). Postpartum counselling after an emergency cesarean. Clinical Psychology & Psychotherapy , 5, 231–237.
- Ryding, E. , Wiren, E. , Johansson, G. , Ceder, B. , & Dahlstrom, A.-M. (2004). Group counseling for mothers after emergency cesarean section: A randomized controlled trial of intervention. Birth , 31(suppl 4), 247–253.
- Santiago, P. N. , Ursano, R. J. , Gray, C. L. , Pynoos, R. S. , Spiegel, D. , Lewis-Fernandez, R. , … Coyne, J. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS One , 8(4), e59236.
- Shalev, A. Y. , Ankri, Y. , Gilad, M. , Israeli-Shalev, Y. , Adessky, R. , Qian, M. , & Freedman, S. (2016). Long-term outcome of early interventions to prevent posttraumatic stress disorder. Journal of Clinical Psychiatry , 77(suppl 5), e580–587.
- Shalev, A. Y. , Ankri, Y. , Israeli-Shalev, Y. , Peleg, T. , Adessky, R. , & Freedman, S. (2012). Prevention of posttraumatic stress disorder by early treatment: Results from the Jerusalem trauma outreach and prevention study. Archives Of General Psychiatry , 69(suppl 2), 166–176.
- Shalev, A. Y. , Gevonden, M. , Ratanatharathorn, A. , Laska, E. , van der Mei, W. F. , Qi, W. , & Koenen, K. C. (2019). Estimating the risk of PTSD in recent trauma survivors: Results of the international consortium to predict PTSD (ICPP). World Psychiatry : Official Journal of the World Psychiatric Association (WPA) , 18(1), 77–87.
- Shapiro, E. , & Laub, B. (2015). Early EMDR intervention following a community critical incident: A randomized controlled trial. Journal of EMDR Practice and Research , 9, 17–27.
- Shapiro, E. , Laub, B. , & Rosenblat, O. (2018). Early EMDR intervention following intense rocket attacks on a town: A randomised clinical trial. Clinical Neuropsychiatry , 15(suppl 3), 194–205.
- Shaw, R. J. , St John, N. , Lilo, E. A. , Jo, B. , Benitz, W. , Stevenson, D. K. , & Horwitz, S. M. (2013). Prevention of traumatic stress in mothers with preterm infants: A randomized controlled trial. Pediatrics , 132(suppl 4), e886–894.
- Sijbrandij, M. , Olff, M. , Reitsma, J. , Carlier, I. V. E. , de Vries, M. H. , & Gersons, B. P. R. (2007). Treatment of acute posttraumatic stress disorder with brief cognitive behavioral therapy: A randomized controlled trial. American Journal of Psychiatry , 164, 82–90.
- Skogstad, L. , Hem, E. , Sandvik, L. , & Ekeberg, O. (2015). Nurse-led psychological intervention after physical traumas: A randomized controlled trial. Clinical Medicine & Research , 7(suppl 5), 339–347.
- Taghizadeh, Z. , Jafarbegloo, M. , Arbabi, M. , & Faghihzadeh, S. (2008). The effect of counseling on post traumatic stress disorder after a traumatic childbirth. Hayat: Faculty of Nursing & Midwifery Quarterly , 13(suppl 4), 23–31.
- van Emmerik, A. A. P. , Kamphuis, J. H. , & Emmelkamp, P. M. G. (2008). Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: A randomized controlled trial. Psychotherapy and Psychosomatics , 77(suppl 2), 93–100.
- Wagner, A. W. , Zatzick, D. F. , Ghesquiere, A. , & Jurkovich, G. J. (2007). Behavioral activation as an early intervention for posttraumatic stress disorder and depression among physically injured trauma survivors. Cognitive and Behavioral Practice , 14, 341–349.
- Wang, X. , Lan, C. , Chen, J. , Wang, W. , Zhang, H. , & Li, L. (2015). Creative arts program as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. International Journal of Clinical and Experimental Medicine , 8(suppl 8), 13585–13591.
- Wijesinghe, C. A. , Williams, S. S. , Kasturiratne, A. , Dolawaththa, N. , Wimalaratne, P. , Wijewickrema, B. , … Franco-Paredes, C. (2015). A randomized controlled trial of a brief intervention for delayed psychological effects in snakebite victims. PLOS Neglected Tropical Diseases , 9(suppl 8), e0003989.
- Wu, K. K. , Li, F. W. , & Cho, V. W. (2014). A randomized controlled trial of the effectiveness of brief-CBT for patients with symptoms of posttraumatic stress following a motor vehicle crash. Behavioural and Cognitive Psychotherapy , 42(suppl 1), 31–47.
- Zatzick, D. , Jurkovich, G. , Rivara, F. P. , Russo, J. , Wagner, A. , Wang, J. , … Katon, W. (2013). A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery , 257(suppl 3), 390–399.
- Zatzick, D. , O’Connor, S. S. , Russo, J. , Wang, J. , Bush, N. , Love, J. , … Van Eaton, E. (2015). Technology-enhanced stepped collaborative care targeting posttraumatic stress disorder and comorbidity after injury: A randomized controlled trial. Journal of Traumatic Stress , 28(suppl 5), 391–400.
- Zatzick, D. , Roy-Byrne, P. , Russo, J. , Rivara, F. , Droesch, R. , Wagner, A. , … Katon, W. (2004). A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives Of General Psychiatry , 61(suppl 5), 498–506.
- Zatzick, D. , Roy-Byrne, P. , Russo, J. E. , Rivara, F. P. , Koike, A. , Jurkovich, G. J. , & Katon, W. (2001). Collaborative interventions for physically injured trauma survivors: A pilot randomized effectiveness trial. General Hospital Psychiatry , 23(suppl 3), 114–123.
- Zatzick, D. F. , Koepsell, T. , & Rivara, F. P. (2009). Using target population specification, effect size, and reach to estimate and compare the population impact of two PTSD preventive interventions. Psychiatry: Interpersonal and Biological Processes , 72(4), 346–359.