?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background: It is generally recommended to exercise caution in applying trauma-focused treatment to individuals with posttraumatic stress disorder (PTSD) and comorbid borderline personality disorder (BPD).
Objective: To investigate the effects of a brief, intensive, direct trauma-focused treatment programme for individuals with PTSD on BPD symptom severity.
Methods: Individuals (n = 72) with severe PTSD (87.5% had one or more comorbidities; 52.8% fulfilled the criteria for the dissociative subtype of PTSD) due to multiple traumas (e.g. 90.3% sexual abuse) participated in an intensive eight-day trauma-focused treatment programme consisting of eye movement desensitization and reprocessing (EMDR) and prolonged exposure (PE) therapy, physical activity, and psychoeducation. Treatment did not include any form of stabilization (e.g. emotion regulation training) prior to trauma-focused therapy. Assessments took place at pre- and post-treatment (Borderline Symptom List, BSL-23; PTSD symptom severity, Clinician Administered PTSD Scale for DSM-5, CAPS-5), and across the eight treatment days (PTSD Checklist, PCL-5).
Results: Treatment resulted in significant decreases of BPD symptoms (Cohen’s d = 0.70). Of the 35 patients with a positive screen for BPD at pre-treatment, 32.7% lost their positive screen at post-treatment. No adverse events nor dropouts occurred during the study time frame, and none of the patients experienced symptom deterioration in response to treatment.
Conclusion: The results suggest that an intensive trauma-focused treatment is a feasible and safe treatment for PTSD patients with clinically elevated symptoms of BPD, and that BPD symptoms decrease along with the PTSD symptoms.
Antecedentes: generalmente se recomienda tener precaución al aplicar un tratamiento centrado en el trauma a las personas con trastorno de estrés postraumático (TEPT) y trastorno de personalidad límite comórbido (TPL).
Objetivo: Investigar los efectos de un programa de tratamiento breve, intensivo y directo centrado en el trauma para personas con TEPT sobre la gravedad de los síntomas de TPL.
Métodos: los participantes (n = 72) con TEPT grave (87.5% tenían una o más comorbilidades; 52.8% cumplieron los criterios para el subtipo disociativo de TEPT) debido a múltiples traumas (por ejemplo, 90.3% abuso sexual) participaron en un programa intensivo de ocho días de tratamiento centrado en el trauma, consistente en EMDR, terapia de exposición prolongada (PE), actividad física y psicoeducación. El tratamiento no incluyó ninguna forma de estabilización (por ejemplo, entrenamiento de regulación emocional) antes de la terapia centrada en el trauma. Las evaluaciones se realizaron antes y después del tratamiento (Lista de síntomas límite, BSL-23; severidad de los síntomas de TEPT, Escala de TEPT administrada por clínicos para DSM-5, CAPS-5) y durante los ocho días de tratamiento (Lista de verificación de TEPT, PCL-5).
Resultados: el tratamiento resultó en una disminución significativa de los síntomas de TPL (d de Cohen = 0.70). De los 35 pacientes con un tamizaje positivo de TPL en el pretratamiento, el 32,7% perdió su tamizaje positivo en el postratamiento. No ocurrieron eventos adversos ni abandonos durante el período de tiempo del estudio, y ninguno de los pacientes experimentó deterioro de los síntomas en respuesta al tratamiento.
Conclusión: Los resultados sugieren que un tratamiento intensivo centrado en el trauma es un tratamiento factible y seguro para pacientes con TEPT con síntomas clínicamente elevados de TPL, y que los síntomas de TLP disminuyen junto con los síntomas de TEPT.
背景:通常建议对创伤后应激障碍 (PTSD) 并发边缘型人格障碍 (BPD) 的患者进行聚焦创伤治疗时要谨慎。
目标:考查针对PTSD简短, 密集, 直接聚焦创伤的治疗流程对BPD症状严重程度的影响。
方法:由于多重创伤 (例如90.3%的性虐待) 导致的严重PTSD (87.5%患有一种或多种并发症; 52.8%符合PTSD分离亚型的标准) 的72名个体, 参加了一次八天的密集型聚焦创伤治疗流程, 包括EMDR和延长暴露 (PE) 治疗, 体育锻炼和心理教育。在聚焦创伤治疗前, 疗程不包括任何形式的稳定治疗 (例如情绪调节训练) 。在治疗前后使用《边缘型症状列表》 (BSL-23) 和《临床用DSM-Ⅳ PTSD诊断量表》 (CAPS-5的PTSD量表) 进行评估, 在整个治疗的八天中使用《PTSD清单》 (PCL-5) 进行评估。
结果:治疗使BPD症状显著减少 (Cohen’s d= 0.70) 。在治疗前BPD筛查阳性的35例患者中, 32.7%的患者在治疗后不再是阳性。在研究时间范围内无不良事件及流失现象出现, 并且没有患者因治疗而出现症状恶化。
结论:结果表明, 针对BPD临床症状升高的PTSD患者, 密集型聚焦创伤治疗是一种可行且安全的疗法, 并且BPD症状随PTSD症状减轻而减轻。
The presence of posttraumatic stress disorder (PTSD) has been found to increase the risk of developing a range of other mental health conditions (Perkonigg, Kessler, Storz, & Wittchen, Citation2000) and comorbidity is highly prevalent in samples of patients suffering from PTSD (Pietrzak, Goldstein, Southwick, & Grant, Citation2012). For example, it has been estimated that when diagnosed with PTSD, the risk of fulfilling the diagnostic criteria of at least one comorbid personality disorder, such as borderline personality disorder (BPD), is up to 35% (Friborg, Martinussen, Kaiser, Øvergård, & Rosenvinge, Citation2013).
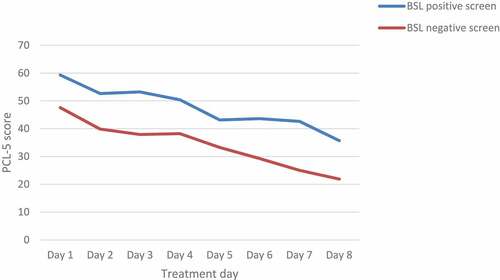
Figure 3. Mean PTSD symptom scores as measured with PCL-5 at each treatment day for individuals with positive and negative screens for BPD
There is a great resemblance in the aetiology and symptomology of PTSD and BPD (Frías & Palma, Citation2015; Kulkarni, Citation2017). For instance, traumatic victimization is seen as a key factor in the development of both mental health conditions (Kulkarni, Citation2017). Regarding the symptoms of (Complex) PTSD, a study using latent class analysis on a dataset of women with histories of childhood abuse detected four BPD symptoms that are distinctive and that distinguish BPD from Complex PTSD, i.e. a strong tendency to avoid abandonment, unstable sense of self, unstable and intense interpersonal relationships, and impulsiveness (Cloitre, Garvert, Weiss, Carlson, & Bryant, Citation2014). Conversely, core features of BPD such as affective instability, cognitive disturbance, interpersonal dysfunction, dissociation, and paranoid experiences have been found in individuals suffering from both complex PTSD and BPD (Cloitre et al., Citation2014).
Despite the significant overlap in symptoms and aetiology between the PTSD and BPD diagnoses, there are entirely different treatment recommendations for PTSD on the one hand, and BPD (with comorbid PTSD) on the other. International guidelines on the treatment of PTSD recommend a trauma-focused treatment approach, such as prolonged exposure (PE) and eye movement desensitization and reprocessing (EMDR) therapy as first-line treatments (ISTSS Guidelines Committee, Citation2018; World Health Organization, Citation2013). However, in the case of BPD with comorbid PTSD, the focus of evidence-based treatment is on increasing an internalized and stable sense of self and reducing destructive behaviours such as self-harm and suicidality before treating comorbid PTSD (Bateman, Gunderson, & Mulder, Citation2015; Linehan, Citation1993; National Collaborating Centre for Mental Health [NCCMH], Citation2009). These psychological and co-occurring social and functional problems that are associated with BPD are the reason that internationally respected experts exercise caution in applying trauma-focused treatment on individuals with PTSD and comorbid BPD (e.g. Harned, Citation2013). Trauma-focused therapy would lead to complications, including those involving reduced treatment compliance, intentional self-injury, and emotion dysregulation (Harned, Korslund, & Linehan, Citation2014), particularly in patients suffering from severe clinical levels of BPD symptoms.
To address potential difficulties related to providing trauma-focused therapy in these comorbid individuals, it is often recommended to apply trauma-focused treatment only after comprehensive skills training (Harned, Citation2013). Most of these treatment programmes include patients with BPD and integrate trauma-focused treatment (prolonged exposure) within Dialectical Behaviour Therapy (DBT; Bohus et al., Citation2013; Harned et al., Citation2014). One recent example is a trauma treatment integrated within a 12-week residential treatment programme (DBT-PTSD; Bohus et al., Citation2019) which includes 19–22 sessions training in mindfulness and compassion skills, distress tolerance skills, and emotion regulation skills followed by one-year outpatient treatment consisting of a minimum of 45 individual therapy sessions (involving skills training, mindfulness training, self-esteem improvement, PTSD-specific psychoeducation, and music and art therapy; Bohus et al., Citation2019). Despite the diversity of treatment interventions and the relatively long duration, such treatment programmes have been found effective, feasible, and safe, thereby confirming the assumption that trauma-focused interventions must be preceded or accompanied by skills training aimed at interrupting dissociation and improving emotion regulation to tolerate the PTSD treatment.
To test the assumption that emotion regulation difficulties indeed have a negative impact on trauma-focused treatment, Jerud, Pruitt, Zoellner, and Feeny (Citation2016) examined the efficacy of direct trauma-focused treatment (prolonged exposure or Sertraline) in a sample of 200 individuals with PTSD with various levels of emotion regulation abilities. They found that individuals’ emotion regulation skills significantly improved following trauma-focused treatment without any prior emotion regulation skill training, especially for those individuals who had poorer emotion regulation at baseline. These results are consistent with the findings that PTSD may intensify symptoms of BPD, resulting in emotion dysregulation (e.g. Cackowski, Neubauer, & Kleindienst, Citation2016), or overlap with BPD symptoms (Cloitre et al., Citation2014). Hence, BPD symptoms may decrease when PTSD symptoms decline, and skill training to address the BPD symptoms beforehand may not be necessary. Only a few studies have evaluated the impact of trauma-focused treatment on symptoms of BPD. For example, in an uncontrolled open pilot study with BPD patients and those with other personality disorders who also suffered from PTSD, the application of trauma-focused (i.e. EMDR) therapy appeared effective in terms of a significant reduction of PTSD symptoms (Slotema, van den Berg, Driessen, Wilhelmus, & Franken, Citation2019). No differences in outcome were found between the group with BPD (n = 16) and the group with other personality disorders (n = 16). However, although the median number of sessions of completers was only four sessions of 60–90 minutes, the total drop out was 32%, and because therapy was applied as an addition to treatment as usual for personality disorders, the effect of trauma-focused treatment on borderline symptoms is unknown. If we consider the reverse relationship, namely the impact of the severity of BPD symptoms on trauma-focused treatment outcome, it appears that none of the studies that investigated this relationship found outcome to be related to the severity of BPD symptoms (Bohus et al., Citation2013; Clarke, Rizvi, & Resick, Citation2008; Hendriks, de Kleine, Broekman, Hendriks & Van Minnen, Citation2018). These findings cast doubts on the need to exclude patients with high levels of BPD symptoms from trauma-focused treatment.
In the last decade, short and highly intensive trauma-focused treatment programmes have been developed (Ehlers et al., Citation2014; Meyers et al., Citation2017). These programmes show that it is possible to intensify trauma-focused treatment for PTSD patients exposed to a wide variety of multiple traumas, including childhood sexual abuse, and suffering from high rates of comorbidity, dissociative symptoms, and suicidal ideation, while symptom worsening and patient dropout appears to be rare (Hendriks et al., Citation2018; Van Woudenberg et al., Citation2018; Wagenmans, Van Minnen, Sleijpen, & De Jongh, Citation2018). The purpose of the current study was to evaluate the effects of a brief intensive trauma-focused treatment programme (Van Woudenberg et al., Citation2018), that does not contain any explicit form of training in emotion regulation skills, for PTSD patients with clinically elevated levels of borderline symptoms. We were primarily interested in the extent to which this treatment affected borderline symptom severity. Given the aforementioned overlap in aetiology and symptoms, it was hypothesized that symptoms of BPD would significantly decrease following treatment. Furthermore, because of the alleged difficulties concerning trauma-focused treatment of individuals with PTSD and comorbid BPD, it was predicted that individuals with clinically elevated symptoms of BPD would profit significantly less from trauma-focused treatment, compared to those with no or few symptoms of BPD. One feature that might negatively influence the outcome of trauma-focused treatment is dissociation (e.g. Lanius, Brand, Vermetten, Frewen &Spiegel, Citation2012). Therefore, we also examined whether individuals who met the criteria for the dissociative subtype of PTSD would show a significantly poorer improvement regarding their borderline symptoms associated with treatment than patients who did not meet these criteria. Finally, to investigate patient safety and potential negative reactions to the intervention, the proportion of patients experiencing PTSD symptom worsening and dropout were determined.
1. Methods
1.1. Participants
Patients were enrolled in a short intensive treatment programme for PTSD at the Psychotrauma Expertise Centre (PSYTREC), a mental health centre in Bilthoven, the Netherlands, and were treated from June to August 2017. Before entering treatment, psychologists assessed whether patients met the inclusion criteria, i.e. (1) being at least 18 years old, (2) having a diagnosis of PTSD according to the DSM-5 (American Psychiatric Association [APA], Citation2013), (3) being able to speak and understand the Dutch language, and (4) no attempts of suicide three months prior to beginning of therapy. Ethical exemption of the study protocol was appointed by the Medical Ethics Review Committee of VU University Medical Centre (registered with the US Office for Human Research Protections (OHRP) as IRB00002991, FWA number FWA00017598).
1.2. Procedure
Patients were referred for treatment by their general practitioner, psychologist, psychiatrist, or other mental health centres. During intake, the Clinician Administered PTSD Scale (CAPS-5; Boeschoten et al., Citation2018) was administered to establish a PTSD diagnosis, and the Mini International Neuropsychiatric Interview (MINI) was used to establish comorbid psychiatric disorders. Patients completed the borderline symptom list (BSL-23; Bohus et al., Citation2009) after the intake session at home. At intake, a treatment plan for eight days was established with at least eight traumatic memories according to, and ordered based upon, the level of disturbance (i.e. memories with the highest subjective units of disturbance first). After the intake procedure, the eight-day intensive treatment started during which patients stayed at the clinic. After the first four treatment days, patients went home for three days, after which they returned for the second series of four days. At the beginning of the first therapy session of each treatment day, patients were asked to complete the PTSD Checklist (PCL-5; Weathers et al., Citation2013) At post-treatment, nine days after the last treatment day, the CAPS-5 and BSL-23 were administered again.
1.3. Treatment programme
Each day of treatment consisted of an individual PE session of 90 minutes in the morning and an individual EMDR therapy session of 90 minutes in the afternoon. Additionally, patients participated in physical activity four times a day with a total of six hours per day provided by professional physical trainers. Patients also attended two hours of psychoeducation per day presented by psychologists. Both physical activity sessions and psychoeducation were provided in groups. No relaxation or emotion regulation skills training was applied prior to the processing of their memories (see De Jongh et al., Citation2016, for the rationale). To avoid confounding of elements of stabilization and trauma-focused therapy, the second phase (i.e. safe place exercise section) was removed from the standard EMDR protocol.
Treatment sessions were employed by clinical psychologists, trained in both EMDR and PE therapy. The PE protocol largely followed the approach of Foa, Hembree, and Rothbaum (Citation2007). According to this approach, patients were asked to imagine the memories of the traumatic events as vividly as possible and had to describe their traumatic memories in the present tense, out loud and in detail. During treatment, in vivo exposure to feared but safe trauma-related stimuli was used.
The EMDR therapy protocol used followed the eight phases approach of Shapiro (2017) and de Jongh and Ten Broeke (Citation2013). During treatment, patients were asked to memorize the most distressing part of the experienced trauma while their working memory capacities are challenged by visually tracking the finger movements of the therapist or other stimuli to maximize the work load of the working memory, such as a light bar, clicking sounds, and/or hand-held buzzers. The flashforward protocol (Logie & De Jongh, Citation2014) was used for treatment of irrational fears and avoidance behaviour in case of anticipatory fear (e.g. of getting overwhelmed by their memories or their emotions).
Between the trauma-focused sessions patients participated in a physical activity programme of six hours per day. The physical activity programme included low and high intensity activities such as mountain biking and hiking. The two hours of psychoeducation per day consisted of PTSD-related topics, such as symptoms of PTSD, and avoidance and safety behaviours.
1.4. Measurements
The primary outcome measure was the severity of BPD symptoms, assessed by the Borderline Symptom List (BSL-23; Bohus et al., Citation2009; Leenarts, Boonman, Diehle, & Rinne, Citation2009). The BSL-23 is a self-report measure and includes 23 items on a Likert scale from 0 (not at all) to 4 (very much) and has a good test-retest reliability over a one-week period, and a high internal consistency (Bohus et al., Citation2009). The internal consistency in the current study was very good (α = .94). A mean item score between 1.5 and 2 indicates the presence of a clinically elevated level of BPD symptoms (Glenn, Weinberg, & Klonsky, Citation2009). Using a stringent cut-off score, we categorized patients into ‘positive screen for BPD’ when they scored a mean item score of ≥ 2, and into ‘negative screen for BPD’ when they scored a mean item score of < 2.
PTSD diagnosis and symptom severity were assessed by using the Dutch version of the Clinician Administered PTSD Scale for DSM-5 (CAPS-5; Boeschoten et al., Citation2018; Weathers et al., Citation2017). The CAPS-5 measures the severity of PTSD. Psychometric evaluation demonstrates a high internal consistency and a good validity (Boeschoten et al., Citation2018; Weathers et al., Citation2017). The CAPS includes two separate items representing the symptoms of the dissociative subtype: depersonalization and derealization. Using the conservative score rule of frequency ≥ 2 and severity ≥ 2 on at least one of these items, patients were classified as meeting or not meeting the criteria of the dissociative subtype.
To be able to monitor the change in PTSD symptoms during treatment, the PTSD Checklist (PCL-5; Weathers et al., Citation2013) was administered at each of the eight treatment days. The PCL-5 is a self-report measure of PTSD and includes 20 items that correspond to the symptoms in the DSM-5 (APA, Citation2013) and are rated from 0 (not at all) to 4 (extremely). Psychometric evaluation demonstrates a high internal consistency and good validity (Bovin et al., Citation2016).
The Dutch version of Mini-International Neuropsychiatric Interview (MINI; Overbeek, Schruers, & Griez, Citation1999; Sheehan et al., Citation1998) is a structured diagnostic interview used to asses psychiatric disorders and suicide risk. The MINI appears to be reliable and well-validated (Overbeek et al., Citation1999; Sheehan et al., Citation1998).
1.5. Statistical analyses
SPSS version 25 was used to perform all statistical analyses. Participants were excluded from analysis if missing data exceeded 10% of the total number of items of the CAPS-5 or the BSL-23. Person mean imputation was performed when missing values did not exceed this percentage. The average item score for each participant was computed and imputed for the missing items for that participant (Hawthorne & Elliott, Citation2005). Independent t-test and chi-square analyses were conducted to compare pre-treatment differences (gender, age, type of trauma, and CAPS-5 score at pre-treatment) between the group of participants excluded for analyses due to missing data and the analysed group.
A mixed-design analysis of variance was used to determine the impact of treatment on BPD symptoms, and of BPD symptoms on PTSD symptoms as measured with either CAPS-5 or PCL-5. The between subjects factor included BPD symptoms (positive or negative screen for BPD) and the within subjects factor included time (BSL-23, CAPS-5, or PCL-5 scores). Preliminary analyses indicated no violations of assumptions of additivity and linearity, normality, homogeneity of variance, and independence. Also, the additional assumption of homogeneity of intercorrelations was not violated. A Greenhouse-Geisser correction was applied when the violation of sphericity was violated. To determine whether individuals experienced clinical reliable worsening of PTSD symptoms a reliable change (RC) index was calculated to determine whether patients’ CAPS scores changed beyond a level that could be attributed to measurement error alone (Evans, Margison & Barkham, Citation1989). Within effect sizes were calculated using Cohen’s d formula, which divides the difference of the means by the weighted pooled standard deviations of these groups (Cohen, Citation2013). A mixed analysis of variance was conducted to determine possible differences between patients who had the dissociative subtype of PTSD at baseline and those who did not. One patient had missing data on the CAPS items representing the symptoms of the dissociative subtype. Therefore, this analysis included 71 patients. Effect sizes were interpreted by the guidelines of Cohen (Citation1988), considering 0.2 or less as a small effect, 0.5 a medium effect, and 0.8 or greater a large effect. The level of significance for all statistical analyses in this study was set at a = .05.
2. Results
2.1. Patient flow and sample characteristics
The patient flow is presented in . A total of 99 participants entered the study and were eligible for research. All participants provided informed consent for participation, nine were excluded because they lacked a baseline BSL measurement, and 18 lacked a post-treatment BSL measurement.
Accordingly, in total 72 participants (81.9% women), with a mean age of 38.9 years (SD = 13.2), were included in this study. Post-treatment CAPS-5 data were missing for one patient. Baseline characteristics of study participants are displayed in . Participants had been exposed to a wide variety of multiple traumatic events, including sexual abuse (90.3%). Individuals with a positive screen for BPD at baseline had experienced physical abuse significantly more often than those with a negative screen (p = .023). The treatment sample represented a severe PTSD patient population in that they showed high comorbidity rates (87.5% had one or more comorbidities), more than half (53.5%) fulfilled the criteria for the dissociative subtype of PTSD, and the majority (47.2%) reported an elevated suicide risk. Thirty-five patients (48.6% of the sample) fulfilled the criterion of a ‘positive screen’ for BPD at baseline, and they showed significantly higher BSL-23, CAPS-5, and PCL-5 scores at baseline than patients with a negative screen for BPD (BSL-23: t(70) = −12.42, p < .001; CAPS-5: t(70) = −2.41, p = .019; PCL-5: t(70) = −5.15, p < .001). There were no significant differences between the two groups with regard to gender, type of trauma, and comorbidity.
Table 1. Baseline characteristics of patients with a negative and a positive screen for borderline personality disorder
2.2. Change in borderline symptom severity
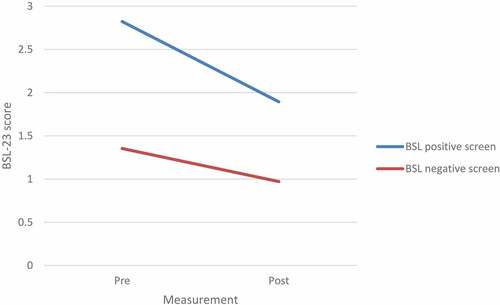
A mixed-design ANOVA showed a significant main effect of time with BSL-23 scores decreasing during treatment (F(1, 70) = 37.55, p < .001, ƞ2 = 0.35; see for mean BSL-23 scores and effect sizes). Furthermore, a significant main effect for BPD screen was found (F(1, 70) = 66.54, p < .001, ƞ2 = 0.49) There was a significant interaction effect between time and BPD screen, indicating that the effect of time significantly differed between those with a negative and a positive BPD screen (F(1, 70) = 6.62, p = .012, ƞ2 = 0.09, see also ). Those with a positive screen for BPD showed a significantly greater decrease in BSL-23 scores compared to patients with a negative screen for BPD. Of the 35 patients who met the criteria of a positive screen for BPD, 32.7% no longer met these criteria after treatment.
Table 2. BSL-23, CAPS-5, and PCL-5 scores at pre- and post-treatment
2.3. Change in PTSD symptom severity (CAPS-5)
Patients in the total group showed a decrease in PTSD symptoms from baseline to post-treatment as measured with the CAPS-5 (Cohen’s d = 1.24). The mixed-design ANOVA showed a significant main effect of time (F(1, 69) = 115.90, p < .001, ƞ2 = 0.63). Also, a main significant effect for BPD screen was found (F(1, 69) = 14.47, p < .001, ƞ2 = 0.17). There was a significant interaction effect between time and BPD screen, indicating that patients with a negative screen for BPD showed a significantly larger decline in PTSD symptoms from pre-treatment to post-treatment than those with a positive BPD screen (F(1, 69) = 4.77, p = .032, ƞ2 = 0.65).
2.4. Course of PTSD symptoms during the eight days of treatment
shows the mean PCL-5 scores at each of the eight treatment days for each group. A mixed-design ANOVA showed a significant main effect of time with PCL-5 scores decreasing during treatment (F(4.397, 294.566) = 40.923, p < .001, ƞ2 = 0.38). Again, a significant main effect for BPD screen was found (F(1, 70) = 20.86, p < .001, ƞ2 = 0.23). There was no significant interaction effect between time and BPD screen, indicating that the effect of time did not significantly differ for those with a negative and positive BPD screen (F(4.397, 294.566) = 0.911, p = .564, ƞ2 = 0.013).
2.5. Borderline symptom change compared between individuals with and without dissociative subtype
A mixed-design ANOVA showed a significant main effect of time [F(1, 69) = 36.45, p < .001, = .346] with both groups showing a change in BSL-23 scores over time. The main effect comparing both dissociation groups was not significant [F(1, 69) = 0.72, p = .398,
= .010] indicating that the BSL-23 scores were not significantly different between the dissociation group and the group without dissociation at pre-treatment (M = 2.17, SD = 0.86 vs M = 1.96, SD = 0.94) and at post-treatment (M = 1.47, SD = 0.99 vs M = 1.33, SD = 1.15). Also, the interaction between time and group was not significant [F(1, 69) = 0.085, p = .772,
= .001] which suggests that the change over time did not differ between the dissociation groups.
2.6. Patient safety and adverse events
Adverse events and attrition were monitored for the duration of the study by therapists and staff. No adverse events occurred during the study time frame and there was no dropout in this study group. None of the patients and, hence, no patients with a positive screen for BPD, experienced clinically reliable worsening of PTSD symptoms.
3. Discussion
To our knowledge, this is the first study that evaluated the effects of an intensive trauma-focused therapy programme for patients with PTSD on comorbid BPD symptoms. The main finding was that the treatment programme was well tolerated with medium to large effect sizes regarding both BPD and PTSD symptoms. After this brief treatment, one-third of the PTSD patients who met a positive screen for BPD before treatment no longer fulfilled this criterion after treatment. Importantly, no dropout nor any adverse events occurred.
Hence, the data were supportive of the hypothesis that symptoms of BPD would decrease significantly associated with intensive trauma-focused treatment aimed at resolving the memories that were driving the PTSD. This finding is in line with those supporting positive treatment effects of trauma-focused treatment in individuals with PTSD and comorbid BPD (e.g. Harned, Ruork, Liu, & Tkachuck, Citation2015; Steuwe et al., Citation2016). However, the difference is that the current treatment programme, which combined two trauma-focused guideline therapies for PTSD, was much shorter and did not contain any explicit form of training in emotion regulation skills, nor any form of intervention aimed at reducing destructive behaviours, such as self-harm and suicidality prior to treatment. The finding that improvement of borderline symptoms did not differ between individuals who fulfilled the diagnostic criteria of the dissociative sub-type of PTSD as indexed by the CAPS-5 and those who did not meet the criteria of this condition is consistent with earlier findings of our treatment programme in another sample of patients (Zoet, Wagenmans, Van Minnen, Sleijpen, & De Jongh, Citation2018). More generally, the results are in line with findings that, overall, comorbid psychopathological symptoms improve as a result of successful trauma-focused therapy (Van Minnen, Zoellner, Harned, & Mills, Citation2015) and with studies, showing that direct trauma-focused treatment is a feasible option for individuals with symptoms of BPD (Hendriks et al., Citation2018; Meyers et al., Citation2017).
One explanation for the finding that the key symptoms of BPD decreased might be related to the fact that all participants in this study had been exposed to childhood adversities or multiple other traumas and suffered from severe symptoms of (complex) PTSD. Given the resemblance in terms of affective instability and interpersonal dysfunction being present in individuals suffering from both (complex) PTSD and BPD (Cloitre et al., Citation2014; Kulkarni, Citation2017), a reduction in PTSD symptoms might also have resulted in a reduction of BPD symptoms. Furthermore, it is likely that the intensive treatment format had a positive effect on some of the clinical complexities of BPD such as treatment non-compliance and co-occurring psychological, social, and functional problems (Harned, Citation2013). In addition, patients might be more focused on treating their PTSD, instead of problems related to relationships or suicidal ideation. Moreover, the short duration of the treatment with a fixed and predictable conclusion of therapy could have contributed to the results and may also explain the lack of dropout in the present study.
Partial support was also found for the hypothesis that PTSD patients with a positive screen for BPD would profit significantly less from trauma-focused treatment in terms of decline of PTSD symptoms, compared to those with a negative screen for BPD. Although regarding our self-report measure PCL-5 no differences were found, the clinician’s rated PTSD Scale showed that PTSD patients with a positive screen for BPD did not perform as well. On the one hand, the BSL-23 items, that are based on criteria of the DSM-IV, the revised version of the Diagnostic Interview for BPD, and opinions of both clinical experts and BPD patients, partly contain items that operationalize factors that are distinctive for BPD (Cloitre et al., Citation2014). This particularly holds true for items that relate to self-organization symptoms that define both the Complex PTSD and BPD diagnoses. However, the BSL-23 contains virtually no items that measure symptoms characteristic of PTSD. Therefore, it was to be expected that those who scored high on the BSL-23 would benefit less from a treatment that was mainly aimed at reducing PTSD symptomatology. Likewise, this finding is consistent with opinions of experts and current treatment guidelines recommending a focus on symptoms characteristic of BPD such as the reduction of self-destructive behaviours and with treatment guidelines in which trauma-focused treatment for patients with BPD is discouraged (Bateman et al., Citation2015; Linehan, Citation1993; NCCMH, Citation2009). On the other hand, also for the patients high on BPD symptoms, the effect sizes were still large. That patients high on BPD symptoms responded to a lesser degree than those low on BPD might mean that these patients, who also started higher on PTSD symptoms, would need more treatment sessions for their PTSD symptoms to decrease. It would be enlightening to test this hypothesis in a future study. Clearly, the processing of traumatic experiences does not automatically lead to the development of new skills sets and patients with more severe BPD symptoms may need additional treatment for their symptoms. However, the present results contradict the DBT philosophy of a staged hierarchy approach where PTSD symptoms are treated only after extensive skill training. One might argue that treatment of PTSD leads to subsequent changes in emotions and cognitions that enable behaviour change to occur more efficiently after PTSD treatment. With this in mind, it would be interesting to study whether, and if so, for whom, which form of skill training would be effective after instead of before trauma-focused treatment.
Some study limitations are worth noting. First and foremost, the current study design lacked the methodological rigour that is associated with a randomized controlled trial such as blinding to condition and a comparison group with minimal bias and confounding factors. Despite these inherent limitations, the current study retains a high degree of rigour by the application of very straight forward treatment package with fixed time schedules and 16 sessions of two well validated evidence based trauma-focused therapies for PTSD. Therapists were instructed to perform the therapies according to written protocols and, to assure that the therapies were delivered according to these protocols, supervisors were present during the daily multidisciplinary meetings. Other important limitations include the lack of follow-up measurements and a control group which makes it difficult to demonstrate durable non-transient ‘halo’ effects, and to determine whether these effects were due to the intensive trauma-focused treatment programme or to other factors. Although it could be argued that it is unlikely that the change in BPD symptom can be explained as ‘placebo effects’ or attributed to spontaneous improvement, symptom fluctuation, or regression to the mean, replication using a RCT design is certainly required. Another reason why we need to be cautious in interpreting the present findings is that patients high on borderline symptoms were not officially diagnosed with BPD. However, the BSL-23 has been found to be strongly associated with the presence of DSM BPD symptoms as assessed by valid semi-structured interviews (i.e. the Structured Interview for Diagnostic and Statistical Manual of Mental Disorders, fourth Edition, Personality Disorders [SIDP-IV]), thereby supporting the BSL-23 as a valid and clinically useful measure of BPD symptomatology (Glenn et al., Citation2009). In addition, we used a stringent cut-off score for the BSL-23. Yet, the use of a structured interview for diagnosing BPD would certainly have contributed to the reliability of the results. A final limitation of current research has to do with the exclusion criterion; that is, not to admit people to the treatment programme who have attempted suicide in the last three months, and this may have resulted in people with severe borderline patients not participating in the study. However, we used very few exclusion criteria, and our patients had a high level of comorbidity, including high levels of suicidality, and our mean item-scores on the BSL-23 were comparable (M = 2.01, SD = 0.89) to those of Bohus et al. (Citation2007; M = 2.05; SD = 0.90) in a sample of 379 psychiatric in- and outpatients who met the DSM criteria for BPD.
In conclusion, to our knowledge this is the first study to investigate the effect of intensive PTSD treatment including EMDR and PE with regard to BPD symptoms in a relatively large sample of patients. Although symptoms of BPD reduced as a result of direct trauma-focused treatment, patients with a positive screen for BPD profit less from intensive treatment for PTSD compared to patients with a negative screen (note however that there were no differences in self-reported PTSD symptoms). Yet, the present findings do not support the notion of detrimental effects of trauma-focused treatment on BPD symptoms and suggest that an intensive trauma-focused treatment programme can lead to PTSD symptom reduction among patients with a high level of BPD symptoms without significant exacerbation of these symptoms. Accordingly, the findings of this study have many implications for clinical practice in that a brief intensive trauma-focused treatment might be a valuable option to consider when PTSD patients are diagnosed with additional BPD. If the present results could be replicated using well-designed studies and implemented in other settings, this could greatly reduce the cost of mental health care for this target group.
Disclosure statement
Ad De Jongh receives income from published books on EMDR therapy and for the training of postdoctoral professionals in this method. Agnes Van Minnen receives income for published book chapters on PTSD and for the training of postdoctoral professionals in prolonged exposure. The other authors do not have competing interests.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, USA: American Psychiatric Association. doi:10.1176/appi.books.9780890425596
- Bateman, A. W., Gunderson, J., & Mulder, R. (2015). Treatment of personality disorder. The Lancet, 385(9969), 735–11.
- Boeschoten, M. A., Van der Aa, N., Bakker, A., Ter Heide, F. J. J., Hoofwijk, M. C., Jongedijk, R. A., … Olff, M. (2018). Development and evaluation of the Dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). European Journal of Psychotraumatology, 9(1), 1546085.
- Bohus, M., Dyer, A. S., Priebe, K., Krüger, A., Kleindienst, N., Schmahl, C., ..., Steil, R. (2013). Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: A randomised controlled trial. Psychotherapy and Psychosomatics, 82(4), 221–233.
- Bohus, M., Kleindienst, N., Limberger, M. F., Stieglitz, R. D., Domsalla, M., Chapman, A. L., … Wolf, M. (2009). The short version of the Borderline Symptom List (BSL-23): Development and initial data on psychometric properties. Psychopathology, 42(1), 32–39.
- Bohus, M., Limberger, M. F., Frank, U., Chapman, A. L., Kühler, T., & Stieglitz, R. D. (2007). Psychometric properties of the borderline symptom list (BSL). Psychopathology, 40(2), 126–132.
- Bohus, M., Schmahl, C., Fydrich, T., Steil, R., Müller-Engelmann, M., Herzog, J., … Priebe, K. (2019). A research programme to evaluate DBTPTSD, a modular treatment approach for Complex PTSD after childhood abuse. Borderline Personality Disorder and Emotion Dysregulation, 6, 7.
- Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28, 1379.
- Cackowski, S., Neubauer, T., & Kleindienst, N. (2016). The impact of posttraumatic stress disorder on the symptomatology of borderline personality disorder. Borderline Personality Disorder and Emotion Dysregulation, 3, 7.
- Clarke, S. B., Rizvi, S. L., & Resick, P. A. (2008). Borderline personality characteristics and treatment outcome in cognitive-behavioral treatments for PTSD in female rape victims. Behavior Therapy, 39, 72–78.
- Cloitre, M., Garvert, D. W., Weiss, B., Carlson, E. B., & Bryant, R. A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5(1), 25097.
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hilsdale, NJ: Lawrence Earlbaum Associates. doi:10.1002/bs.3830330104
- Cohen, J. (2013). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum.
- De Jongh, A., Resick, P. A., Zoellner, L. A., Minnen, A., Lee, C. W., Monson, C. M., … Rauch, S. A. (2016). Critical analysis of the current treatment guidelines for complex PTSD in adults. Depression and Anxiety, 33(5), 359–369.
- de Jongh, A., & Ten Broeke, E. (2013). Handboek EMDR: Een geprotocolleerde behandelmethode voor de gevolgen van psychotrauma [EMDR manual: A protocolised treatment method for the consequenes of psychotrauma]. Amsterdam, The Netherlands: Pearson Assessment and Information BV.
- Ehlers, A., Hackmann, A., Grey, N., Wild, J., Liness, S., Albert, I., … Clark, D. M. (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. The American Journal of Psychiatry, 171, 294–304.
- Evans, C., Margison, F., & Barkham, M. (1989). The contribution of reliable and clinically significant change methods to evidence-based mental health. Evidence Based Mental Health, 1, 70–72.
- Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. New York, NY: Oxford University Press. doi:10.1093/med:psych/9780195308501.001.0001
- Frías, Á., & Palma, C. (2015). Comorbidity between post-traumatic stress disorder and borderline personality disorder: A review. Psychopathology, 48(1), 1–10.
- Friborg, O., Martinussen, M., Kaiser, S., Øvergård, K. T., & Rosenvinge, J. H. (2013). Comorbidity of personality disorders in anxiety disorders: A meta-analysis of 30 years of research. Journal of Affective Disorders, 145(2), 143–155.
- Glenn, C. R., Weinberg, A., & Klonsky, E. D. (2009). Relationship of the Borderline Symptom List to DSM-IV borderline personality disorder criteria assessed by semi-structured interview. Psychopathology, 42(6), 394–398.
- Harned, M. S. (2013). Treatment of posttraumatic stress disorder and comorbid borderline personality disorder. doi:10.1007/978-14614-6458-7_14.
- Harned, M. S., Korslund, K. E., & Linehan, M. M. (2014). A pilot randomized controlled trial of dialectical behavior therapy with and without the dialectical behavior therapy prolonged exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behaviour Research and Therapy, 55, 7–17.
- Harned, M. S., Ruork, A. K., Liu, J., & Tkachuck, M. A. (2015). Emotional activation and habituation during imaginal exposure for PTSD among women with borderline personality disorder. Journal of Traumatic Stress, 28(3), 253–257.
- Hawthorne, G., & Elliott, P. (2005). Imputing cross-sectional missing data: Comparison of common techniques. Australian and New Zealand Journal of Psychiatry, 39, 583–590.
- Hendriks, L., de Kleine, R. A., Broekman, T. G., Hendriks, G.-J., & Minnen, A. (2018). Intensive prolonged exposure therapy for chronic PTSD patients following multiple trauma and multiple treatment attempts. European Journal of Psychotraumatology, 9(1), 1425574.
- ISTSS Guidelines Committee. 2018. Guidelines position paper on complex PTSD in adults. Oakbrook Terrace, IL: Author. Retrieved from http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-Treatment-Guidelines/ISTSS_CPTSD-Position-Paper-(Adults)_FNL.pdf.aspx
- Jerud, A. B., Pruitt, L. D., Zoellner, L. A., & Feeny, N. C. (2016). The effects of prolonged exposure and sertraline on emotion regulation in individuals with posttraumatic stress disorder. Behaviour Research and Therapy, 77, 62–67.
- Kulkarni, J. (2017). Complex PTSD–a better description for borderline personality disorder? Australasian Psychiatry, 1039856217700284. doi:10.1177/1039856217700284
- Lanius, R. A., Brand, B., Vermetten, E., Frewen, P. A., & Spiegel, D. (2012). The dissociative subtype of posttraumatic stress disorder: Rationale, clinical and neurobiological evidence, and implications. Depression and Anxiety, 29(8), 701–708.
- Leenarts, L. E. W., Boonman, C., Diehle, J., & Rinne, T. (2009). Borderline Symptomen Lijst 23 (BSL-23). Retrieved from https://www.zi-mannheim.de/fileadmin/user_upload/downloadsforschung/PSM_downloads/BSL_23_dutch_0912.pdf
- Linehan, M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford press.
- Logie, R. D. J., & De Jongh, A. (2014). The “Flashforward procedure”: Confronting the catastrophe. Journal of EMDR Practice and Research, 8, 25–32.
- Meyers, L., Voller, E. K., McCallum, E. B., Thuras, P., Shallcross, S., Velasquez, T., & Meis, L. (2017). Treating veterans with PTSD and borderline personality symptoms in a 12-week intensive outpatient setting: Findings from a pilot program. Journal of Traumatic Stress, 30(2), 178–181.
- National Collaborating Centre for Mental Health (UK). (2009). Borderline personality disorder: Treatment and management. British Psychological Society. Retrieved from https://www.rcpch.ac.uk/sites/default/files/asset_library/Research/Clinical%20Effectiveness/Endorsed%20guidelines/Borderline%20Personality%20Disorder%20%28NICE%29/CG78NICEGuidance.pdf
- Overbeek, T., Schruers, K., & Griez, E. (1999). MINI: Mini international neuropsychiatric interview, Dutch version 5.0. 0 (DSM-IV). Maastricht: University of Maastricht.
- Perkonigg, A., Kessler, R. C., Storz, S., & Wittchen, H. U. (2000). Traumatic events and posttraumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica, 101(1), 46–59.
- Pietrzak, R. H., Goldstein, R. B., Southwick, S. M., & Grant, B. F. (2012). Psychiatric comorbidity of full and partial posttraumatic stress disorder among older adults in the USA: Results from wave 2 of the national epidemiologic survey on alcohol and related conditions. The American Journal Of Geriatric Psychiatry, 20, 380–390.
- Shapiro, F. (2017). Eye movement desensitization and reprocessing: Basic principles,protocols and procedures (3nd ed.). New York, NY: Guilford Press.
- Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., … Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–33.
- Slotema, C. W., van den Berg, D. P., Driessen, A., Wilhelmus, B., & Franken, I. H. A. (2019). Feasibility of EMDR for posttraumatic stress disorder in patients with personality disorders: A pilot study. European Journal of Psychotraumatology, 10(1), 1614822.
- Steuwe, C., Rullkötter, N., Ertl, V., Berg, M., Neuner, F., Beblo, T., & Driessen, M. (2016). Effectiveness and feasibility of narrative exposure therapy (NET) in patients with borderline personality disorder and posttraumatic stress disorder – a pilot study. BMC Psychiatry, 16, 254. doi: 10.1186/s12888-016-0969-4
- Van Minnen, A., Zoellner, L., Harned, M., & Mills, K. (2015). Changes in co-morbidities after prolonged exposure for PTSD: A literature review. Current Psychiatry Reports, 17. doi:10.1007/s11920-015-0549-1
- Van Woudenberg, C., Voorendonk, E. M., Bongaerts, H., Zoet, H. A., Verhagen, M., Van Minnen, A., … De Jongh, A. (2018). The effectiveness of an intensive treatment program combining prolonged exposure and EMDR for severe posttraumatic stress disorder (PTSD). European Journal of Psychotraumatology, 9(1). doi:10.1080/20008198.2018.1487225
- Wagenmans, A., Van Minnen, A., Sleijpen, M., & De Jongh, A. (2018). The impact of childhood sexual abuse on the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology, 9(1), 1430962.
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., … Marx, B. P. (2017). The clinician-administered PTSD scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Retrieved from https://www.ptsd.va.gov/
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5). Boston, MA: National Center for PTSD.
- World Health Organization. (2013). Guidelines for the management of conditions that are specifically related to stress. World Health Organization. Retrieved from http://apps.who.int/iris/bitstream/10665/85119/1/9789241505406_eng.pdf
- Zoet, H. A., Wagenmans, A., Van Minnen, A., Sleijpen, M., & De Jongh, A. (2018). Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology, 9(1). doi:10.1080/20008198.2018.1468707.