ABSTRACT
Objective
Posttraumatic stress disorder (PTSD) and depression substantially impair health-related quality of life (HRQOL) for many Canadian Armed Forces (CAF) veterans. Although PTSD and depression are highly comorbid, little is known about whether the disorders may interact in their association with HRQOL. We sought to investigate whether depressive symptoms modify the relation between PTSD and HRQOL in treatment-seeking veterans.
Method
We accessed the clinical data of 545 CAF veterans aged 18 to 65 years who were seeking treatment at a specialized clinic in London, Ontario. We used hierarchical linear regression to assess the additive and multiplicative relations between depression and PTSD symptoms on HRQOL, controlling for age and alcohol/substance abuse. Simple slopes were examined to probe significant interactions.
Results
Probable PTSD and major depression were present in 77.4% and 85.3% of the sample, respectively, and 73.0% of the sample presented with probable PTSD-depression comorbidity. Depression symptoms significantly modified the relation between PTSD symptoms and overall mental HRQOL (β = 0.12, p <0.001, ∆R2 = 0.014), and role impairment due to emotional difficulties (β = 0.20, p <0.001, ∆R2 = 0.035). Simple slope analyses revealed the impact of PTSD was greater among those with lower depression symptoms and became weaker with greater depression symptom severity. In adjusted models, only depression was significantly associated with all mental and physical HRQOL domains; PTSD was not associated with physical HRQOL, role emotional impairment, or vitality.
Conclusions
For those with severe comorbid depression, PTSD symptoms were no longer associated with mental HRQOL, particularly in areas related to emotional functioning. Findings suggest the importance of targeting depression in patients presenting with PTSD-depression comorbidity.
Objetivo: El trastorno de estrés postraumático (TEPT) y la depresión afectan sustancialmente la calidad de vida relacionada con la salud (CVRS) para muchos veteranos de las Fuerzas Armadas de Canadá (CAF). Aunque TEPT y depresión son altamente comórbidos, poco se sabe acerca de si los trastornos pueden interactuar en su asociación con la CVRS. Quisimos investigar si los síntomas depresivos modifican la relación entre el TEPT y la CVRS en los veteranos que buscan tratamiento.
Método: Accedimos a los datos clínicos de 545 veteranos de CAF de 18 a 65 años que buscaban tratamiento en una clínica especializada en London, Ontario. Utilizamos regresión lineal jerárquica para evaluar las relaciones aditivas y multiplicativas entre depresión y síntomas de TEPT en la CVRS, controlando por edad y abuso de alcohol/sustancias. Las pendientes simples se examinaron para investigar interacciones significativas.
Resultados: TEPT probable y depresión mayor estaban presentes en el 77.4% y el 85.3% de la muestra, respectivamente, y el 73.0% de la muestra presentaba comorbilidad probable TEPT-depresión. Los síntomas de depresión modificaron significativamente la relación entre los síntomas de TEPT y la CVRS mental general (β = 0.12, p <0.001, ∆R2 = 0.014), y el deterioro de rol debido a dificultades emocionales (β = 0.20, p <0.001, ∆R2 = 0.035). Los análisis de pendiente simple revelaron que el impacto del TEPT fue mayor entre aquellos con síntomas de depresión más bajos y se debilitaron con una mayor gravedad de los síntomas de depresión. En los modelos ajustados, solo la depresión se asoció significativamente con todos los dominios de CVRS mental y física; El TEPT no se asoció con la CVRS física, deterioro emocional de rol o la vitalidad.
Conclusiones: Para aquellos con depresión comórbida severa, los síntomas de TEPT ya no se asociaban con la CVRS mental, particularmente en áreas relacionadas con el funcionamiento emocional. Los hallazgos sugieren la importancia de enfocarse en la depresión en pacientes que presentan comorbilidad de TEPT-depresión.
目标: 创伤后应激障碍 (PTSD) 和抑郁症严重损害了许多加拿大武装部队 (CAF) 退伍军人的健康相关生活质量 (HRQOL) 。尽管PTSD和抑郁症高度共发, 但对于这些疾病与HRQOL的关联中是否可能存在交互作用知之甚少。我们试图考查寻求治疗的退伍军人中, 抑郁症状是否会影响PTSD与HRQOL之间的关系。
方法: 我们获得了在安大略省伦敦市一家专科门诊接受治疗的545名18至65岁的CAF退伍军人的临床数据。我们控制了年龄和酒精/药物滥用, 使用分层线性回归来评估抑郁与PTSD症状之间加性和乘性关系对HRQOL的作用。考查了简单斜率以探查显著的交互作用。
结果: 样本人群中分别有77.4%和85.3%患有可能的PTSD和重性抑郁症, 73.0%有可能的PTSD-抑郁共病。抑郁症状显著影响PTSD症状与总体心理HRQOL之间的关系 (β= 0.12, p<0.001, ΔR2 = 0.014), 以及由情绪困扰导致的角色障碍 (β= 0.20, p <0.001, ΔR2 = 0.035) 。简单斜率分析显示, PTSD的影响在抑郁症状较轻者中更强, 在抑郁症状较严重者中更弱。在校正模型中, 只有抑郁与所有心理和躯体HRQOL域均显著相关PTSD与躯体HRQOL, 角色情感障碍或生命力无关。
结论: 对于有严重抑郁症并发的患者, PTSD症状不再与心理HRQOL相关, 尤其是在情绪功能相关领域。研究结果表明了在患有PTSD-抑郁共病的患者中以抑郁症为靶点的重要性。
1. Introduction
Major Depressive Disorder and posttraumatic stress disorder (PTSD) affect many military members and veterans, with recent epidemiological data suggesting that approximately 21% and 14% of Canadian Armed Forces (CAF) veterans endorse the presence of depression and PTSD, respectively (Van Til, Sweet, & Poirier et al., Citation2017). Previous work has shown that individuals with depression or PTSD frequently report diminished life satisfaction and difficulties within social and vocational domains (Rapaport, Clary, Fayyad, & Endicott, Citation2005), consequences that may persist even in the remission of psychiatric symptoms (Angermeyer, Holzinger, Matschinger, & Stengler-Wenzke, Citation2002). As such, comprehensive screening and treatment strategies should not only consider patients’ symptomatology, but also their subjective functioning across psychological, physical, and social domains, broadly termed quality of life (QOL), or health-related quality of life (HRQOL) for functioning specifically related to health status (Mendlowicz & Stein, Citation2000). Although depression and PTSD have independently been linked with reductions in HRQOL (Hansson, Citation2002; Olatunji, Cisler, & Tolin, Citation2007), there is scarce research on whether the disorders interactively influence HRQOL. Considering that depression and PTSD often co-occur (comorbidity ranging between 36-70% within military samples) (Campbell et al., Citation2007; Kehle et al., Citation2010; Zamorski et al., Citation2016), it is imperative to develop a nuanced understanding of the ways in which the two disorders may interact to impact HRQOL.
Diminished QOL appears to be significantly associated with depression (Goldney, Fisher, Wilson, & Cheok, Citation2000; Hansson, Citation2002; Pyne et al., Citation1997) and PTSD (Hansson, Citation2002; Kehle et al., Citation2010; Mendlowicz & Stein, Citation2000; Mogotsi, Kaminer, & Stein, Citation2000), with reductions that are similar to or greater than for chronic physical conditions (Alonso, Angermeyer, & Bernert et al., Citation2004; Hays, Wells, & Sherbourne et al., Citation1995; Spitzer et al., Citation1995; Wells, Stewart, & Hays et al., Citation1989). Using a well-validated measure of HRQOL, the SF-36 (Ware, Snow, & Kosinsk et al., Citation1993), both depression and PTSD symptoms were uniquely associated with all mental components (e.g. vitality, social functioning) in samples of US and Canadian veterans (Pittman, Goldsmith, Lemmer, Kilmer, & Baker, Citation2012; Richardson, Long, Pedlar, & Elhai, Citation2010, Citation2008). Of note, neither disorder predicted physical HRQOL in US veterans (Pittman et al., Citation2012), and only depression predicted physical HRQOL declines in Canadian veterans (Richardson et al., Citation2010, Citation2008). Importantly, in both civilian (Olatunji et al., Citation2007; Pagotto et al., Citation2015; Rapaport et al., Citation2005; Schonfeld et al., Citation1997) and military (Kehle et al., Citation2010; Olatunji et al., Citation2007) samples, depression and PTSD symptoms have not only been shown to uniquely predict QOL but have emerged as the strongest predictors of QOL declines compared with other psychiatric symptoms and diagnoses. Although evidence suggests that depression and PTSD contribute independently to HRQOL reductions, it is unknown whether there are any interaction effects in this relation.
The co-occurrence of depression and PTSD among Canadian military members and veterans is high (ranging from 41-62%) (Richardson et al., Citation2017; Zamorski et al., Citation2016), the implications of which may extend beyond the independent impact of either disorder. Indeed, relative to those with depression or PTSD alone, the presence of both disorders has been linked with more severe psychiatric symptoms, greater suicidal ideation, and increased likelihood of undesirable treatment outcomes (Blanchard, Buckley, Hickling, & Taylor, Citation1998; Campbell et al., Citation2007; Kramer, Booth, Han, & Williams, Citation2003, Steiner, Boulos, & Mirocha et al., Citation2017). Further, compared to those with only depression, those with comorbid PTSD have exhibited significantly worse QOL (Campbell et al., Citation2007; Steiner et al., Citation2017). However, the impact of depression-PTSD comorbidity on QOL is not entirely consistent within the literature. In a study of US veterans, HRQOL impairments were similar between those with depression only, and those with comorbid depression and PTSD. However, both depression groups tended to report significantly more impairment on the SF-36 than those with PTSD only (Kramer et al., Citation2003). In another study with currently serving US military members, overall QOL and social functioning did not differ between those with PTSD alone and those with PTSD and comorbid conditions (including depression) (Kehle et al., Citation2010). Variable findings suggest there may be nuanced relations between PTSD and depression with HRQOL that are masked by generalized analyses; more precise analyses that account for the interactions between depression and PTSD symptoms may clarify such relations.
Classically, PTSD has been associated with military populations, who may have had frequent exposure to potentially traumatic events. As such, we intend to examine the effect of PTSD on HRQOL, while considering the role of depression as an effect modifier. To our knowledge, no study has examined whether depression and PTSD symptoms interact to impact HRQOL. Accordingly, the current study extends research by assessing whether PTSD is differentially associated with HRQOL across levels of depression symptom severity. Using a treatment-seeking sample of CAF members and veterans, we assessed the independent and interactive contributions of PTSD and depression on HRQOL after controlling for age, substance use disorder, and alcohol use disorder, each of which has shown associations with QOL in prior research (Richardson et al., Citation2008; Rudolf & Watts, Citation2002).
2. Methods
2.1. Participants and procedure
Participants included 545 treatment-seeking veterans and currently serving CAF members, aged between 18 and 65 years old (see for sample characteristics). All participants were referred to a specialized clinic (St. Joseph’s Health Care London, Operational Stress Injury Clinic in London, Ontario, Canada) for outpatient treatment of a service-related mental health condition between January 2016 and April 2019. As part of standard intake procedure, all participants completed self-report questionnaires assessing demographic variables, psychological and physical symptoms, substance and alcohol abuse, and HRQOL. All study participants consented for their clinical data to be used for future research, including the current study. This study was approved by all relevant research boards and offices.
Table 1. Sociodemographic characteristics of the study sample (sample size = 545).
2.2. Clinical measures
2.2.1. Posttraumatic stress disorder
PTSD symptom severity was assessed using the PTSD Checklist for the DSM-5 (PCL-5) (Blevins, Weathers, Davis, Witte, & Domino, Citation2015). Participants reported their past-month symptom severity, where higher scores indicate greater PTSD symptom severity (total score ranging from 0 to 80). Scores of 33 or higher were considered indicative of probable PTSD. (Bovin et al., Citation2016) The reliability and validity of the PCL-5 have been well-established within treatment-seeking military populations (current sample α = 0.94) (Bovin et al., Citation2016; Wortmann et al., Citation2016).
2.2.2. Depression
Depression symptom severity was assessed using the Patient Health Questionnaire-9 (PHQ-9) (Spitzer, Kroenke, & Williams, Citation1999). Participants reported their symptom severity within the past 14 days, where higher scores indicated greater depressive symptom severity (total score ranging from 0 to 27). A score of 10 or higher was indicative of probable major depression (Kroenke, Spitzer, & Williams, Citation2001). The PHQ-9 has exhibited reliability and validity across large clinical samples (current sample α = 0.87) (Kroenke et al., Citation2001).
2.2.3. Alcohol misuse
Problematic drinking behaviours were assessed using the Alcohol Use Disorders Identification Test (AUDIT) (Saunders, Aasland, & Babor et al., Citation1993). Participants reported their past-year drinking behaviours, where higher scores indicated more problematic alcohol use behaviour (total score ranging from 0 to 41). Scores of 8 or greater signified probable alcohol use disorder (Saunders, Aasland, & Babor et al., Citation1993). Researchers have shown that the AUDIT has adequate validity within clinical settings (current sample α = 0.89) (Bohn, Babor, & Kranzler, Citation1995).
2.2.4. Substance abuse
Potentially problematic substance use was assessed using the 10-item Drug Abuse Screening Test (DAST-10) (Skinner, Citation1982). Participants reported their past-year substance use, where higher scores indicated more problematic substance use (total score ranging from 0 to 10). Scores of three or higher suggested probable substance use disorder (Yudko, Lozhkina, & Fouts, Citation2007). Researchers have validated the DAST-10 in inpatient populations (current sample α = 0.78) (Bohn, Babor, & Kranzler, Citation1991).
2.2.5. Health-related quality of life
HRQOL was measured using the 36-item Short-Form Health Survey (SF-36) (Ware et al., Citation1993). The SF-36 assessed mental and physical functional impairment across eight domains which are used to generate two summary scores, the Mental Component Score (MCS) and the Physical Component Score (PCS). Vitality (VT), Role Emotional (RE; role limitations due to emotional concerns), Social Functioning (SF), and Mental Health (MH) subscales were used to inform MCS, and Physical Functioning (PF), Role Physical (RP; role limitations due to physical concerns), Bodily Pain (BP), and General Health (GH) were used to inform PCS. The mental health aggregate score and subscales are of primary interest in light of reliable support that PTSD and depression negatively impact mental wellbeing and functioning. PTSD has generally not influenced the physical component and subscale scores of HRQOL after controlling for depression (Pagotto et al., Citation2015; Pittman et al., Citation2012; Richardson et al., Citation2010, Citation2008), but we have chosen to include all scales in analyses for comprehensiveness. Scores were calculated by summing responses, transforming them to a 0–100 scale (where higher scores indicated better functioning), and standardizing them according to Canadian age- and sex-based norms (Hopman, Towheed, & Anastassiades et al., Citation2000). Component scores of below 50 indicated below-average health (Ware et al., Citation1993). The reliability and validity of the SF-36 have been established within large samples across several countries and clinical populations (current sample α’s = 0.76-0.92 for subscales) (Gandek et al., Citation1998; McHorney, Ware, Lu, & Sherbourne, Citation1994).
2.3. Data analysis
Hierarchical multiple linear regression was used to assess whether PTSD and depression individually and interactively predicted HRQOL. Separate analyses were run to predict (1) MCS, and (2) PCS. In the case of a significant interaction on either component score, separate regressions were run to predict the component subscale scores. Each regression model was adjusted for age, substance use disorder, and alcohol use disorder. Predictors were entered in five steps to assess their incremental associations with HRQOL, Step 1: age, Step 2: alcohol use disorder severity and substance use disorder severity, Step 3: PTSD symptom severity, Step 4: depression symptom severity, and Step 5: a cross-product term between PTSD symptom severity and depressive symptom severity to assess the interaction between depression and PTSD. To probe significant interactions, simple slopes were examined to assess the relation between PTSD and HRQOL across three levels of depression symptom severity (−1 SD, 0 SD, +1 SD). PTSD and depression were each mean-centred prior to inclusion in regression models. To protect against inflated rates of Type I error, we are applying a Bonferroni correction based on the number of separate regression models. Thus an alpha level of 0.05/6 = 0.008 was used for statistical significance in all tests. Regression and correlations were conducted using IBM SPSS Statistics, Version 25 and simple slopes were examined using an SPSS Macro (PROCESS) (Hayes, Citation2018).
2.4. Missing data
Consistent with SF-36 manual instructions (Ware et al., Citation1993), missing data on the SF-36 were imputed using participants’ personal means for the relevant subscales, as long as participants had at least 50% of the scores for that subscale. For all other measures, missing data was handled using multiple imputation, but was restricted to participants that had 20% or less missing data on any of the relevant scales. We inspected the pattern of missing data from the DAST-10, AUDIT, PCL-5, and PHQ-9, and determined that the data appeared to be missing at random. We then used multiple imputation by chained equations (MICE) in R (Buuren & Groothuis-Oudshoorn, Citation2010) to impute the data missing from these fields. Predictive mean matching was used for all values, and a max iteration value of 50 was set for the equation with the random seed set to 42. Auxiliary variables used for MICE included demographic variables (e.g. marital status, age, education) and psychiatric symptoms assessed at clinic intake (e.g. general anxiety disorder symptoms, somatization); SF-36 scores were also included as auxiliary variables, but these values were not imputed.
3. Results
3.1. Participant characteristics
Of 719 eligible participants, 29 were excluded for missing demographic information, and 145 were excluded for either missing more than 20% of item scores on the AUDIT, DAST-10, PCL-5, or PHQ-9, or more than 50% of scores on any one of the SF-36 mental health subscales (final N = 545). Excluded participants were compared to those with complete data using t-tests for continuous variables (age, alcohol use disorder, substance use disorder, PTSD, depression, and SF-36 scores), and using chi-square tests for categorical demographic variables (marital status, education, and military status). The samples were comparable on all variables, except for marital status; participants with complete data were more likely to be married (χ 2 = 5.11, p = 0.02). Demographic characteristics are presented in .
More than a third of participants met the probable alcohol use disorder cut-off (n = 203; 37.2%), and relatively fewer participants met the cut-off criteria for probable substance use disorder (n = 77; 14.1%). Most participants had probable PTSD (n = 422; 77.4%), and probable major depression (n = 465; 85.3%). Most of the participants with probable depression also had probable PTSD (n = 398; 85.6%). Considering that scores under 50 indicate below-average health, participants had considerably compromised HRQOL according to the MCS and PCS (see ).
Table 2. Clinical and health-related quality of life characteristics of the study sample.
3.2. Hierarchical regression models
3.2.1. MCS and MCS subscales
depicts each of the hierarchical models predicting MCS. More severe substance abuse was associated with lower MCS, indicating worse mental HRQOL. However, once PTSD symptom severity was added to the model in Step 3, only PTSD significantly predicted of MCS (∆R 2 = 0.26). In Step 4, depression and PTSD symptom severity were the only significant predictors of MCS (∆R 2 = 0.13). For both disorders, as symptom severity increased, MCS decreased. In the final model, depression and PTSD symptom severity remained significant independent predictors of MCS, and the interaction between depression and PTSD was also significant (Adj. R 2 = 0.43, ∆R 2 = 0.01).
Table 3. Hierarchical regression: Depression x PTSD symptomatology predicting Mental Component Score (MCS).
To probe the interaction on MCS, the simple slopes of PTSD symptom severity on MCS were analysed at −1 SD, 0 SD, and +1 SD of depression symptoms (see )). At −1 SD and 0 SD, elevated PTSD symptom severity was significantly associated with reduced MCS (b = −0.19, t(538) = −5.08, p < 0.001 and b = −0.11, t(538) = −3.42, p < 0.001, respectively). At +1 SD, greater PTSD symptom severity no longer predicted declines in MCS (b = −0.04, t(538) = −0.86, p = 0.39). Thus, the impact of PTSD symptom severity on MCS decreased as depression symptoms increased, with no significant impact of PTSD on MCS for those with more severe depression.
Figure 1. Predicted Mental Component Score (MCS), and Role Emotional (RE) according to posttraumatic stress disorder (PTSD) symptom severity, across three levels of depression symptom severity. Higher scores on PTSD and depression indicate more severe symptomatology. Higher scores on MCS and RE indicate better health-related quality of life.
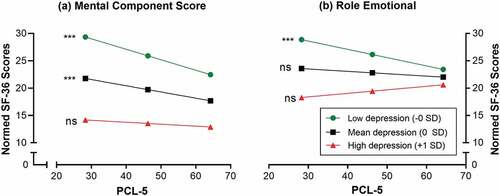
The same 5-step hierarchical regression analyses were applied to each MCS subscale. In Step 4, with all individual predictors entered, depression symptom severity was the only significant predictor for VT (b = −1.08, p < 0.001), and RE (b = −0.61, p < 0.001). For each outcome, as depression symptoms increased, the HRQOL domain scores decreased. For SF and MH, both PTSD symptom severity (b = −0.19, p < 0.001; b = −0.18, p < 0.001), and depression symptom severity (b = −0.88, p < 0.001; b = −1.23, p < 0.001) were significant predictors. For each outcome, as PTSD and depression symptoms increased, subscale scores decreased. In the final models, the interaction terms were significant for RE (b = 0.02, p < 0.001, Adj. R 2 = 0.22, ∆R 2 = 0.04) but not for SF, MH, and VT.
The relation between PTSD and RE was analysed at three levels of depression symptoms (see )). Greater PTSD symptom severity predicted decreased RE scores at −1 SD (b = −0.15, t(538) = −3.98, p < 0.001), but not at 0 SD (b = −0.04, t(538) = −1.30, p = 0.19), or at +1 SD (b = 0.07, t(538) = 1.54, p = 0.12). Thus, PTSD symptom severity was only negatively associated with RE for those with relatively low levels of depression. As depression symptoms increased, PTSD symptom severity no longer impacted RE.
3.2.2. PCS
Following the same hierarchical steps to predict PCS, no covariates showed significant associations. When PTSD was added to the model in Step 3, elevated symptoms were associated with lower PCS, indicating worse HRQOL (∆R 2 = 0.05). However, depression symptomatology was the only significant predictor when added in Step 4 (∆R 2 = 0.02). PCS decreased as depression symptoms increased. Depression remained the only significant predictor in the final model, where neither PTSD nor the interaction were significant (∆R 2 < 0.001; See ).
Table 4. Hierarchical regression: Depression x PTSD symptomatology predicting Physical Component Score (PCS).
4. Discussion
Our research presents novel findings regarding the interactive impact of depression and PTSD symptoms on HRQOL. After adjusting for age, and alcohol and substance disorder symptoms, depression severity significantly moderated the association between PTSD symptoms and the mental component of HRQOL; this moderation effect was not present for physical HRQOL. Depression and PTSD symptoms were each uniquely associated with reduced mental HRQOL. In contrast, only symptoms of depression were associated with reduced physical HRQOL. Consistent with prior research (Richardson et al., Citation2017; Seal et al., Citation2009; Zamorski et al., Citation2016), a large portion of our sample reported comorbid PTSD and depression, attesting to the importance of examining their interactive and relative relations with HRQOL.
Current findings add to the mounting evidence that depression and PTSD are uniquely associated with mental HRQOL (Rapaport et al., Citation2005; Schonfeld et al., Citation1997). Of note, however, whereas PTSD symptom severity was an independent predictor for MCS, MH, and SF, depression symptoms were independently associated with reduced functioning on all mental subscales. The consistent negative impact of depression across all mental HRQOL domains has been reliably reported (Goldney et al., Citation2000; Hays et al., Citation1995; Richardson et al., Citation2010, Citation2008; Schonfeld et al., Citation1997), and our findings reinforce the claim that depression may exert the most wide-spread and strongest negative impact on HRQOL compared to anxiety or trauma-related disorders (Ikin, Creamer, Sim, & McKenzie, Citation2010; Olfson et al., Citation1997; Pittman et al., Citation2012). Although PTSD has been linked with reductions across all mental components of HRQOL in prior research (Pittman et al., Citation2012; Richardson et al., Citation2010, Citation2008), this finding has been inconsistent as others have reported that PTSD predicted only a subset of mental HRQOL domains after adjusting for comorbidities (e.g. depression and alcohol use) (Kehle et al., Citation2010; Pagotto et al., Citation2015). Notably, out of the subsample with probable depression, 86% also had probable PTSD; the proportion of those with probable PTSD who also had depression was even greater (94%). The direct and moderated impact of depression on HRQOL further highlights the need to assess, monitor, and target depressive symptoms in treatment-seeking veterans with PTSD.
In our sample, we found that higher PTSD symptoms were associated with reductions in mental HRQOL and role emotional functioning across low levels of depression, but not for those with moderate (for role emotional) or high depressive symptoms. In individuals with high depressive symptoms, HRQOL remained steadily low regardless of PTSD symptom severity. This interaction may explain the inconsistent findings in previous research. After controlling for depressive and other psychiatric symptoms, there is evidence that PTSD is associated HRQOL (Richardson et al., Citation2008), and evidence that it does not affect functional impairment (Olfson et al., Citation1997). Similarly, compared to those with depression only, research has found both that PTSD comorbidity predicts further declines in quality of life (Steiner et al., Citation2017), and that it does not (Kramer et al., Citation2003). Among a number of possible explanations, the lack of an association between PTSD symptom severity and HRQOL in the most severely depressed participants could represent a floor effect. That is, the HRQOL scores within the high depression severity participants may be so low, and thus exhibit such little variation, that meaningful differences due to PTSD symptoms are undetectable. This could be due to a real inability to experience further declines in HRQOL, or it could represent a lack of sensitivity of the HRQOL measure among those with considerably compromised wellbeing. Though, it is worth noting that the interaction explains only a small amount of HRQOL variance, with the main effects of depression and PTSD symptoms representing moderate to large effect sizes (Cohen, Citation1992). Thus the importance of each disorder in reducing HRQOL should not be overlooked. Notably, due to the treatment-seeking nature of our sample, many study participants had substantial illness burden and severity; even at 1 SD below the mean depression symptom severity score, participants were above the cut-off for probable depression. Importantly, the interaction evidenced that depression was the most consistently and critically related to mental and emotional aspects of HRQOL (Ikin et al., Citation2010; Olfson et al., Citation1997; Pittman et al., Citation2012; Schonfeld et al., Citation1997).
Only depression was significantly associated with physical HRQOL in the fully adjusted regression model. Our findings thus emphasize the wide-ranging negative impact of depression on HRQOL domains, whether mental or physical. Similarly, researchers have revealed that depression, but not PTSD, has been independently associated with physical HRQOL domains (Pagotto et al., Citation2015; Pittman et al., Citation2012; Richardson et al., Citation2010, Citation2008). Depression has been reliably associated with negative physical health outcomes, including stroke (Pan, Sun, Okereke, Rexrode, & Hu, Citation2011), diabetes (Vancampfort et al., Citation2016), hypertension (Patten et al., Citation2009), obesity (Strine et al., Citation2008), and cardiovascular disease (Musselman, Evans, & Nemeroff, Citation1998). Although an extensive review of the reasons underlying such associations is beyond the scope of this paper, correlates of depression including neuroendocrine alterations (e.g. hyperactive sympathetic nervous system) (Musselman et al., Citation1998), inflammation and immune system dysfunction (Leonard, Citation2010; Shimbo, Chaplin, Crossman, Haas, & Davidson, Citation2005), and increased unhealthy behaviours (e.g. smoking, physical inactivity, heavy drinking) (Strine et al., Citation2008) may mediate changes in physical health and functioning. It is possible that PTSD does not account for changes in physical HRQOL beyond these correlates, and indeed PTSD is less consistently associated with physical HRQOL in the literature. A recent meta-analysis noted considerable heterogeneity in PTSD and physical functioning relations, but did find a small and significant effect of PTSD on physical HRQOL (Pacella, Hruska, & Delahanty, Citation2013). The nonsignificant relation in the current study may be influenced by our measure, as larger effect sizes have been found for general health symptoms and health conditions, relative to HRQOL (Pacella et al., Citation2013). Additionally, larger effect sizes between PTSD and physical health outcomes have been found in female samples, and so our mostly male sample may have influenced our results (Pacella et al., Citation2013). Generally, both depression and PTSD evidenced smaller slopes for physical changes than for changes in mental HRQOL, which may explain the lack of interaction. We hypothesized that a floor effect on mental functioning occurred due to such severely impacted scores in those with high depressive symptoms. Such a floor effect is less likely if the influence of depression is smaller. The complex relations between mental illnesses and physical health are worth further exploration in future research.
Our study had limitations worth noting. Data was collected at clinical intake and the analysis was limited to a cross-sectional assessment; accordingly, causality cannot be determined. Because all participants were treatment-seeking, the majority of the study sample had severe, chronic mental illnesses, with particularly high rates of depression and PTSD comorbidity. As such, our findings may not generalize to those without comorbidities, those with subclinical levels of depressive or PTSD symptoms, or non-military populations. Treatment-seeking in itself may also be uniquely related to quality of life. For instance, those seeking treatment may have improved quality of life compared to those with similar symptom severity of either PTSD or depression by way of their access to devoted clinicians with means to provide therapeutic support. Of notable significance, although we explored the impact of PTSD symptoms at three levels of depression severity, the subsample with high levels of depression severity and low levels of PTSD severity (i.e. −1 SD) was small; thus, analyses may have been underpowered to identify the association of those with relatively ‘low’ PTSD symptomatology among severely depressed individuals. Future research should address these limitations to confirm and further validate our findings across different populations and symptom profiles. Nonetheless, our study had several strengths, including systematic and standardized assessments, optimal missing data handling, and access to a large treatment-seeking military sample, which can be challenging to acquire for research purposes, particularly within Canada.
5. Conclusion
The present study demonstrated that depression severity moderates the relation between PTSD and HRQOL. Although extant research has highlighted the significant and unique impact of both PTSD and depression on HRQOL, due to their high levels of comorbidity, it was imperative to explore whether PTSD and HRQOL were differentially associated across varying severity of depression symptoms. We found that depression and PTSD each explained unique variation in the aggregate mental HRQOL, as well as social functioning, mental health, and bodily pain. However, only depression significantly predicted both the component scores and all mental HRQOL domains. Importantly, we showed that PTSD was associated with HRQOL among the moderately and mildly depressed, but not among the severely depressed participants. This trend held for general mental HRQOL, as well as emotion-related role limitations. The detrimental impact of depression on HRQOL is thus at the forefront of our findings and speaks to the importance of targeting depression symptomatology among treatment-seeking veterans with comorbidities.
Data access
Data is maintained within relevant hospital firewalls and cannot be released to unauthorized researchers. Data contains sensitive personal health information that may increase the risk of re-identification of participants enrolled in this research study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Alonso, J. , Angermeyer, M. C. , Bernert, S. , Bruffaerts, R., Brugha, T., Bryson, H., …, & Vollebergh, W. (2004). Disability and quality of life impact of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica , 109(s420), 38–10.
- Angermeyer, M. C. , Holzinger, A. , Matschinger, H. , & Stengler-Wenzke, K. (2002). Depression and quality of life: Results of a follow-up study. International Journal of Social Psychiatry , 48(3), 189–199.
- Blanchard, E. B. , Buckley, T. C. , Hickling, E. J. , & Taylor, A. E. (1998). Posttraumatic stress disorder and comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders , 12(1), 21–37.
- Blevins, C. A. , Weathers, F. W. , Davis, M. T. , Witte, T. K. , & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress , 28(6), 489–498.
- Bohn, M. , Babor, T. , & Kranzler, H. (1991). Validity of the Drug Abuse Screening Test (DAST-10) in inpatient substance abusers. Problems of Drug Dependence , 119, 233–235.
- Bohn, M. J. , Babor, T. F. , & Kranzler, H. R. (1995). The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol , 56(4), 423–432.
- Bovin, M. J. , Marx, B. P. , Weathers, F. W. , Gallagher, M. W. , Rodriguez, P. , Schnurr, P. P. , & Keane, T. M. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychological Assessment , 28(11), 1379–1391.
- Buuren, S. , & Groothuis-Oudshoorn, K. (2010). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software , 45(3), 1–68.
- Campbell, D. G. , Felker, B. L. , Liu, C.-F. , Yano, E. M. , Kirchner, J. E. , Chan, D. , & Chaney, E. F. (2007). Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine , 22(6), 711–718.
- Cohen, J. (1992). A power primer. Psychological Bulletin , 112(1), 155.
- Gandek, B. , Ware, J. E. , Aaronson, N. K. , Alonso, J. , Apolone, G. , Bjorner, J. , …, & Sullivan, M. (1998). Tests of data quality, scaling assumptions, and reliability of the SF-36 in eleven countries: Results from the IQOLA project. Journal of Clinical Epidemiology , 51(11), 1149–1158.
- Goldney, R. D. , Fisher, L. J. , Wilson, D. H. , & Cheok, F. (2000). Major depression and its associated morbidity and quality of life in a random, representative Australian community sample. Australian & New Zealand Journal of Psychiatry , 34(6), 1022–1029.
- Hansson, L. (2002). Quality of life in depression and anxiety. International Review of Psychiatry , 14(3), 185–189.
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach . New York: Guilford Press.
- Hays, R. D. , Wells, K. B. , Sherbourne, C. D. , Rogers, W., & Spritzer, K. (1995). Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Archives of General Psychiatry , 52(1), 11–19.
- Hopman, W. , Towheed, T. , Anastassiades, T. , Tenenhouse, A., Poliquin, S., Berger, C., ..., & Papadimitropoulos, E. (2000). Canadian normative data for the SF-36 health survey. CMAJ , 163(3), 265–271.
- Ikin, J. F. , Creamer, M. C. , Sim, M. R. , & McKenzie, D. P. (2010). Comorbidity of PTSD and depression in Korean War veterans: Prevalence, predictors, and impairment. Journal of Affective Disorders , 125(1), 279–286.
- Kehle, S. M. , Reddy, M. K. , Ferrier-Auerbach, A. G. , Erbes, C. R. , Arbisi, P. A. , & Polusny, M. A. (2010). Psychiatric diagnoses, comorbidity, and functioning in national guard troops deployed to Iraq. Journal of Psychiatric Research , 45(1), 126–132.
- Kramer, T. L. , Booth, B. M. , Han, X. , & Williams, D. K. (2003). Service utilization and outcomes in medically ill veterans with posttraumatic stress and depressive disorders. Journal of Traumatic Stress , 16(3), 211–219.
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine , 16(9), 606–613.
- Leonard, B. E. (2010). The concept of depression as a dysfunction of the immune system. Curr Immunol Rev, 6(3), 205–212.
- McHorney, C. A. , Ware, J. E. , Lu, R. , & Sherbourne, C. D. (1994). The MOS 36-item short-form health survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care , 32, 40–66.
- Mendlowicz, M. V. , & Stein, M. B. (2000). Quality of life in individuals with anxiety disorders. American Journal of Psychiatry , 157, 669–682.
- Mogotsi, M. , Kaminer, D. , & Stein, D. J. (2000). Quality of life in the anxiety disorders. Harvard Review of Psychiatry , 8(6), 273–282.
- Musselman, D. L. , Evans, D. L. , & Nemeroff, C. B. (1998). The relationship of depression to cardiovascular disease: Epidemiology, biology, and treatment. Archives of General Psychiatry , 55(7), 580–592.
- Olatunji, B. O. , Cisler, J. M. , & Tolin, D. F. (2007). Quality of life in the anxiety disorders: A meta-analytic review. Journal of Clinical Psychology Review , 27(5), 572–581.
- Olfson, M. , Fireman, B. , Weissman, M. M. , Leon, A. C. , Sheehan, D. V. , Kathol, R. G. , …, & Farber, L. (1997). Mental disorders and disability among patients in a primary care group practice. American Journal of Psychiatry , 154(12), 1734–1740.
- Pacella, M. L. , Hruska, B. , & Delahanty, D. L. (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders , 27(1), 33–46.
- Pagotto, L. F. , Mendlowicz, M. V. , Coutinho, E. S. , Figueira, I. , Luz, M. P. , Araujo, A. X. , & Berger, W. (2015). The impact of posttraumatic symptoms and comorbid mental disorders on the health-related quality of life in treatment-seeking PTSD patients. Comprehensive Psychiatry , 58, 68–73.
- Pan, A. , Sun, Q. , Okereke, O. I. , Rexrode, K. M. , & Hu, F. B. (2011). Depression and risk of stroke morbidity and mortality: A meta-analysis and systematic review. JAMA , 306(11), 1241–1249.
- Patten, B. S. , Williams, V. A. J. , Lavorato, H. D. , Campbell, N. R. C. , Eliasziw, M. , & Campbell, T. S. (2009). Major depression as a risk factor for high blood pressure: Epidemiologic evidence from a national longitudinal study. Psychosomatic Medicine , 71(3), 273–279.
- Pittman, J. O. E. , Goldsmith, A. A. , Lemmer, J. A. , Kilmer, M. T. , & Baker, D. G. (2012). Post-traumatic stress disorder, depression, and health-related quality of life in OEF/OIF veterans. Quality of Life Research , 21(1), 99–103.
- Pyne, J. M. , Patterson, T. L. , Kaplan, R. M. , Ho, S. , Gillin, J. C. , Golshan, S. , & Grant, I. (1997). Preliminary longitudinal assessment of quality of life in patients with major depression. Psychopharmacology Bulletin , 33(1), 23–29.
- Rapaport, M. H. , Clary, C. , Fayyad, R. , & Endicott, J. (2005). Quality-of-life impairment in depressive and anxiety disorders. American Journal of Psychiatry , 162(6), 1171–1178.
- Richardson, J. , Long, M. E. , Pedlar, D. , & Elhai, J. D. (2010). Posttraumatic stress disorder and Health Related Quality of Life (HRQol) in pension-seeking Canadian WW II and Korean veterans. Journal of Clinical Psychiatry , 71, 1099–1101.
- Richardson, J. D. , Ketcheson, F. , King, L. , Shnaider, P. , Marlborough, M. , Thompson, A. , & Elhai, J. D. (2017). Psychiatric comorbidity pattern in treatment-seeking veterans. Psychiatry Research , 258, 488–493.
- Richardson, J. D. , Long, M. E. , Pedlar, D. , & Elhai, J. D. (2008). Posttraumatic stress disorder and Health Related Quality Of Life (HRQol) among a sample of treatment- and pension-seeking deployed Canadian forces peacekeeping veterans. Canadian Journal of Psychiatry , 53(9), 594–600.
- Rudolf, H. , & Watts, J. (2002). Quality of life in substance abuse and dependency. International Review of Psychiatry , 14(3), 190–197.
- Saunders, J. , Aasland, O. , Babor, T. , Fuente, J. R., & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption‐II. Addiction , 88(6), 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
- Schonfeld, W. H. , Verboncoeur, C. J. , Fifer, S. K. , Lipschutz, R. C. , Lubeck, D. P. , & Buesching, D. P. (1997). The functioning and well-being of patients with unrecognized anxiety disorders and major depressive disorder. Journal of Affective Disorders , 43(2), 105–119.
- Seal, K. H. , Metzler, T. J. , Gima, K. S. , Bertenthal, D. , Maguen, S. , & Marmar, C. R. (2009). Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using department of veterans affairs health care, 2002-2008. American Journal of Public Health , 99(9), 1651–1658.
- Shimbo, D. , Chaplin, W. , Crossman, D. , Haas, D. , & Davidson, K. W. (2005). Role of depression and inflammation in incident coronary heart disease events. The American Journal of Cardiology , 96(7), 1016–1021.
- Skinner, H. A. (1982). The drug abuse screening test. Addictive Behaviors , 7, 363–371.
- Spitzer, R. , Kroenke, K. , & Williams, J. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA , 282(18), 1737–1744.
- Spitzer, R. L. , Kroenke, K. , Linzer, M. , Hahn, S. R. , Williams, J. B. W. , deGruy, F. V. , …, & Davies, M. (1995). Health-related quality of life in primary care patients with mental disorders: Results from the PRIME-MD 1000 study. JAMA , 274(19), 1511–1517.
- Steiner, A. J. , Boulos, N. , Mirocha, J. , Wright, S. M., Collison, K. L., & IsHak, W. W. (2017). Quality of life and functioning in comorbid posttraumatic stress disorder and major depressive disorder after treatment with citalopram monotherapy. Clinical Neuropharmacology , 40(1), 16.
- Strine, T. W. , Mokdad, A. H. , Dube, S. R. , Balluz, L. S. , Gonzalez, O. , Berry, J. T. , …, & Kroenke, K. (2008). The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. General Hospital Psychiatry , 30(2), 127–137.
- Van Til, L. , Sweet, J. , Poirier, A. , McKinnon, K., Sudom, K., Dursun, S., & Pedlar, D. (2017). Well-being of Canadian regular force veterans, findings from LASS 2016 survey (Research Directorate Technical Report, 23 June 2017. Executive Summary). Charlottetown PE: Veterans Affairs Canada.
- Vancampfort, D. , Correll, C. U. , Galling, B. , Probst, M. , De Hert, M. , Ward, P. B. , …, & Stubbs, B. (2016). Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: A systematic review and large scale meta‐analysis. World Psychiatry : Official Journal of the World Psychiatric Association (WPA) , 15(2), 166–174.
- Ware, J. , Snow, K. , Kosinsk, M. , & Gandek, B. (1993). SF-36 health survey: Manual and lnterpretation guide . Boston, MA: New England Medical Center.
- Wells, K. , Stewart, A. , Hays, R. , Burnam, M. , Rogers, W. , Daniels, M. , & Ware, J . (1989). The Functioning and Well-being of Depressed Patients: Results From the Medical Outcomes Study. JAMA , 262(7), 914–919.
- Wortmann, J. H. , Jordan, A. H. , Weathers, F. W. , Resick, P. A. , Dondanville, K. A. , Hall-Clark, B. , & Litz, B. T. (2016). Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment , 28(11), 1392–1403.
- Yudko, E. , Lozhkina, O. , & Fouts, A. (2007). A comprehensive review of the psychometric properties of the drug abuse screening test. Journal of Substance Abuse Treatment , 32(2), 189–198.
- Zamorski, M. A. , Bennett, R. E. , Rusu, C. , Weeks, M. , Boulos, D. , & Garber, B. G. (2016). Prevalence of past-year mental disorders in the Canadian armed forces, 2002-2013. The Canadian Journal of Psychiatry , 61(1suppl), 26S–35S.
