ABSTRACT
Background
Both the latent variable model and the network model have been widely used to conceptualize mental disorders. However, it has been pointed out that there is no clear dichotomy between the two models, and a combination of these two model could enable a better understanding of psychopathology. The recently proposed latent network model (LNM) has provided a statistical framework to enable this combination. Evidence has shown that posttraumatic stress disorder (PTSD) could be a suitable candidate disorder to study the combined model. In the current study, we initiated the first investigation of the latent network of PTSD symptoms.
Methods
The latent network of DSM-5 PTSD symptoms was estimated in 1196 adult survivors of China’s 2008 Wenchuan earthquake. Validation testing of the latent network was conducted in a replication sample of children and adolescent who experienced various trauma types. PTSD symptoms were measured by the PTSD Checklist for DSM-5 (PCL-5). The latent network was estimated using the seven-factor hybrid model of DSM-5 PTSD symptoms, analysed using the R package lvnet.
Results
The latent network model demonstrated good fit in both samples. A strong weighted edge between the intrusion and avoidance dimensions was identified (regularized partial correlation = 0.75). The externalizing behaviour dimension demonstrated the highest centrality in the latent network.
Conclusions
This study is the first to investigate the latent network of DSM-5 PTSD symptoms. Results suggest that both latent symptom dimension and associations between the dimensions should be considered in future PTSD studies and clinical practices.
Antecedentes: tanto el modelo de variable latente como el modelo de red se han utilizado ampliamente para conceptualizar los trastornos mentales. Sin embargo, se ha señalado que no existe una dicotomía clara entre los dos modelos, y una combinación de estos dos modelos podría permitir una mejor comprensión de la psicopatología. El modelo de red latente (LNM) recientemente propuesto ha proporcionado un marco estadístico para permitir esta combinación. La evidencia ha demostrado que el trastorno de estrés postraumático (TEPT) podría ser un trastorno candidato adecuado para estudiar el modelo combinado. En el presente estudio, iniciamos la primera investigación de la red latente de síntomas de TEPT.
Métodos: La red latente de síntomas del TEPT DSM-5 se estimó en 1196 adultos sobrevivientes del terremoto de Wenchuan en China en 2008. Las pruebas de validación de la red latente se realizaron en una muestra de replicación de niños y adolescentes que experimentaron varios tipos de trauma. Los síntomas de TEPT se midieron mediante la Lista de verificación de TEPT para DSM-5 (PCL-5). La red latente se estimó utilizando el modelo híbrido de siete factores de síntomas del TEPT DSM-5, analizados utilizando el paquete R lvnet.
Resultados: El modelo de red latente demostró un buen ajuste en ambas muestras. Se identificó un margen ponderado fuerte entre las dimensiones de intrusión y evitación (correlación parcial regularizada = 0,75). La dimensión del comportamiento de externalización demostró la centralidad más alta en la red latente.
Conclusiones: este estudio es el primero en investigar la red latente de síntomas de TEPT DSM-5. Los resultados sugieren que tanto la dimensión de los síntomas latentes como las asociaciones entre las dimensiones deben considerarse en futuros estudios de TEPT y prácticas clínicas.
背景: 潜变量模型和网络模型已被广泛用于精神障碍的概念化。然而已有文献指出,这两种模型之间没有明确的二分,且这两种模型的合并可以更好地理解心理病理学。最近提出的潜网络模型(LNM)提供了一个可以实现这种合并的统计框架。有证据表明,创伤后应激障碍(PTSD)可能是研究这种合并模型的合适候选疾病。本研究中,我们首次对PTSD症状潜网络进行了考查。
方法: 在2008年汶川地震的1196名成年幸存者中估计了DSM-5 PTSD症状潜网络。在一个经历多种创伤类型的儿童和青少年的重复样本中进行了潜网络的验证。 PTSD症状由DSM-5 PTSD检查表(PCL-5)测量。潜网络由DSM-5 PTSD症状的七因素混合模型估计,并使用R的lvnet程序包进行分析。
结果: 潜网络模型在两个样本中均有良好拟合。识别出了闯入和回避维度之间较强的加权边(正则化偏相关= 0.75)。潜网络中外化行为维度具有最高的中心性。
结论: 本研究是第一个考查DSM-5 PTSD症状潜网络的研究。结果表明,在未来的PTSD研究和临床实践中应同时考虑潜在症状维度和维度之间的关联。
PALABRAS CLAVE:
1. Introduction
There has been abundant discussion and inquiry into the conceptualizations of mental disorders (Kendler, Zachar, & Craver, Citation2011). One classic framework for mental disorders was based on latent variable modelling. An underlying latent variable, which represents the disorder, was introduced into the model to account for the co-occurrence of symptoms (Bollen & Lennox, Citation1991). A causal interpretation of the latent variable modelling conceptualized latent variable as the common cause of corresponding symptoms (e.g. Borsboom & Cramer, Citation2013). An underlying disorder occurs first and consequently causes corresponding symptoms, such as medical diseases. All the observed symptoms are simply reflections of the presence of the non-observable disorder, in this common cause conceptualization. The most widely used approach to conducting psychiatric and psychological research under the latent variable framework is factor analysis. Symptoms are organized into different latent symptom dimensions to explain the covariance patterns between them. Each dimension represents a distinct psychological construct closely related to corresponding symptoms.
However, the recently proposed network model provided some new perspectives on mental disorders (Borsboom, Citation2017; Borsboom & Cramer, Citation2013; Cramer, Waldorp, Van Der Maas, & Borsboom, Citation2010; Fried et al., Citation2017). The model conceptualizes a mental disorder as a network formed by casual relationships between symptoms. The construct of a mental disorder is no longer considered as a common cause of the symptoms, but instead an ‘emergence’ resulting from the network constructed by associations and feedback loops between the symptoms. Symptoms with higher centrality in the network are believed to play more important roles in the onset and maintenance of mental disorders. This new theory challenges the classic common cause perspective by focusing on specific symptoms instead of an underlying latent disorder. Network theory has raised a great deal of attention, and enlightened more recent studies on pathology of mental disorders. As previously reviewed (Birkeland, Greene, & Spiller, Citation2020; Contreras, Nieto, Valiente, Espinosa, & Vazquez, Citation2019; Robinaugh, Hoekstra, Toner, & Borsboom, Citation2020), network theory has been widely applied to psychopathology studies on most of the mental disorders including affective/mood disorders, psychosis and personality disorders in the recent 10 years.
The debate on whether latent variable or network modelling approaches reflect a better model of mental disorders has not yet been resolved, as both models have gained support from empirical studies. The key difference in the two models involves their assumptions on the manner in which symptoms of mental disorder are organized together (Schmittmann et al., Citation2013). However, these two models can potentially complement, rather than exclude one other (Epskamp & Fried, Citation2018). Some researchers have noted that a mental disorder is a complex construct, and may not be best understood by choosing only latent variable or symptom network modelling; instead, both models might contribute to explain the psychopathology of mental disorders (Fried & Cramer, Citation2017). Also, it has been demonstrated that latent variable models and network models are mathematically equivalent. The two models can be transformed to each other with equal number of free parameters and goodness of fit (Bringmann & Eronen, Citation2018). Therefore, there is no clear statistical boundary between these two models. Both factor analysis and network analysis deal with the covariance matrix of variables. By using network analysis to model the latent variance–covariance matrix produced by factor analysis, it is possible to combine these two models within a single statistical framework (Epskamp, Rhemtulla, & Borsboom, Citation2017).
More recently, the combination of network and latent variable models was described in more detail (Epskamp et al., Citation2017). A new framework called ‘latent network modeling’ (LNM) was proposed to model conditional independence relationships between latent variables. Within this framework, symptom dimensions still exist as latent factors, with the symptoms loading onto corresponding dimensions. Simultaneously, the model estimates the covariance structure of latent variables as a network. Estimation of the latent network is based on the Gaussian graphical model (GGM), which has been widely used in the estimation of mental disorder symptom networks (Epskamp, Borsboom, et al., Citation2018). In the network, nodes are latent variables and represent symptom dimensions, while edges are partial correlation coefficients and represent conditional independence relationships between latent symptom dimensions. Therefore, LNM offers a useful tool for exploratory estimation of relationships between symptom dimensions without making any assumptions of directionality.
The latent network model combines the characteristics of latent variable and network models, and thus has several methodological advantages over each of the two models alone. First, LNM extends traditional factor analysis. Although correlations between the latent variables are estimated in factor analysis, the conditional independence relationships between them were still unknown. Estimation of the GGM network address this problem. In addition, by applying graph theory methods, it is possible to identify latent variables with higher centrality in the latent network. Also, the model addresses some limitations of a symptom-based network. It has often been pointed out that measurement error could adversely affect the estimation of partial correlation coefficients in networking modelling, and further threatens the stability of symptom networks (Forbes, Wright, Markon, & Krueger, Citation2017, Citation2019; Fried & Cramer, Citation2017). Yet, the latent variable model approach constructs a network while taking measurement error into account, and accordingly can improve measurement of the true score of a continuous variable, and solve the stability issue (Epskamp et al., Citation2017).
Considering the theoretical and methodological advantages, applying latent network modelling to studying disorders leads to a more complete conceptualization of mental disorders. There have been no such studies on mental disorders using LNM until now, but PTSD has been recommended as a suitable candidate disorder to study the combined model of latent variable and network modelling (Fried & Cramer, Citation2017; Young, Citation2015). There is also increasing empirical evidence implying (but not directly examining) the presence of a latent structure within the symptom network of PTSD. According to a review of (non-latent) PTSD symptom network studies (Birkeland et al., Citation2020), the most often identified edges were usually those between symptoms within the same DSM cluster (e.g. edges between ‘hyperarousal’ and ‘startle’; and between the two avoidance items, ‘diminished interest in activities’ and ‘restricted range of affect’). It was also reported that both the re-experiencing avoidance symptom cluster networks became more strongly inter-correlated after trauma exposure (Segal et al., Citation2019). Additionally, in a network cluster analysis of PTSD symptoms (Moshier et al., Citation2018), several clusters of nodes in the PTSD symptom network were identified, including clusters of (1) five intrusion symptoms (B1-B5) and sleep disturbance (E6); (2) two avoidance symptoms (C1-C2) and trauma-related amnesia (D1); (3) anhedonia, detachment, inability to experience positive feelings (D5-D7), and concentration difficulties (E5); (4) irritable and reckless behaviour (E1-E2); (5) hypervigilance and exaggerated startle response (E3-E4); and (6) distorted blame, distorted negative beliefs, and persistent negative emotions (D2-D4). The result of clustering largely overlapped with the well-recognized seven-factor latent structure model of PTSD (Armour et al., Citation2015).
Investigating the latent network structure of PTSD has both important theoretical and clinical implications. A large bodywork has studied the latent dimensional structure of PTSD, and some symptom clusters of the disorder were stably identified (Armour, Műllerová & Elhai, Citation2016). However, few theories have been proposed to discuss the causal relationships between these symptom clusters. By shedding light on the conditional independent relationship between latent factors, the LNM allows researchers to generate further hypotheses about such causal relations. Also, nodes with higher centrality and edges with higher weight in the latent network may usually have more important clinical meanings (Borsboom, Citation2017). Treatments focusing on these elements could change the structure of the symptom network, and therefore lead to recovery from the disorder. In clinical practice, these related symptom dimensions should be given more attention during assessment and treatment of PTSD patients.
Current evidence supports the seven-factor hybrid model as best describing the latent structure of DSM-5 PTSD, proposed by Armour et al. (Citation2015). The model has demonstrated best model fit across different age groups, cultures and trauma types, as previously reviewed (e.g. Armour et al., 2016; Contractor, Caldas, Dolan, Natesan, & Weiss, Citation2019). Also, the hybrid model demonstrated longitudinal invariance across time (Wang et al., Citation2017). In addition to good model fit, the hybrid model has gain some support for its external validity. Recently the symptom clusters in the 7-factor hybrid model demonstrated differential associations with external variables from different perspectives, such as behaviour (e.g. psychiatric comorbidities, suicidal ideation, hostility, functioning and quality of life, Pietrzak et al., Citation2015), neuroimaging (e.g. the integrity of the uncinate fasciculus, Fani et al., Citation2019), and genetic variables (e.g. 5-HTTLPR genotype, Li et al., Citation2018). Therefore, we built the latent network model based on the 7-factor hybrid model in this study. First, we investigated the latent network structure of DSM-5 PTSD symptoms in a sample of Chinese adult survivors of the 2008 Wenchuan earthquake. Subsequently, we replicated this model in a sample of children and adolescents who experienced various trauma types, in order to validate the model in an independent dataset. Based on aforementioned evidence, we hypothesized that the LNM model would show a good fit to the data, and probably better fit than confirmatory factor analysis (CFA) models. Considering the exploratory nature of LNM, we did not pose any a priori hypotheses of the network structure.
2. Methods
2.1. Participants and procedures
The current study was a reanalysis to two previously reported datasets. The first dataset was from an adult sample recruited from a community in Hanwang Town, one of the most affected areas of the 2008 Wenchuan earthquake. Five and a half years after the earthquake, we conducted an epidemiological survey in one of the largest rebuilt communities located in the town (for detail see Cao et al., Citation2015; Liu et al., Citation2014). The final adult sample included 1196 people (response rate = 95%), with 67.7% females and 32.3% males. Most participants were adults from 18 to 65 years old (mean age = 47.9 years, SD = 10.0). Self-reported ethnicity was mainly Han (99.7%) Chinese. In this sample, 86.8% of participants were married, and 13.0% were unmarried (single/divorced/separated/widowed). In terms of education level, 31.6% completed high school or above, and 67.1% did not complete high school. All participants completed a self-reported questionnaire with assistance from well-trained psychology undergraduate students. Participants were introduced to the aim of the study and signed an informed consent form before the survey. The study protocol was approved by the Institutional Review Board of the Institute of Psychology, Chinese Academy of Sciences, Beijing, China.
Both development period and trauma types have been supported as influencing PTSD phenotypes. Testing the latent network model in a replication sample with different ages and trauma types is thus important for validation of the model. The second dataset was composed of adolescents who experienced various kinds of traumatic events. The participants were recruited from two secondary schools in Beijing and one secondary school in Changsha, China (for complete details see Liu, Wang, Cao, Qing, & Armour, Citation2016). The survey was conducted by class groups, monitored by trained research assistants and school teachers. Written informed consent was obtained from all participants. The final sample included 559 trauma-exposed adolescents and 43.5% were girls. Mean age of the replication sample was 15.8 years (range: 12–19, SD = 1.4). The study protocol was approved by the Institutional Review Board of the Institute of Psychology, Chinese Academy of Sciences, Beijing, China.
2.2. Measurement
DSM-5 PTSD symptoms were evaluated with the Chinese version of the PTSD Checklist for DSM-5 (PCL-5) in both samples. The PCL-5 is a self-report checklist of 20 DSM-5 PTSD symptoms. Each item is rated on a 5-point Likert scale reflecting severity from 0 (not at all) to 4 (extremely) during the past month. For the adult earthquake survivor sample, participants were instructed to rate their PTSD symptoms specifically based on the earthquake. In the adolescent sample, PTSD symptoms were rated in terms of the traumatic event most adversely affecting the participant. The PCL-5 scale has demonstrated good psychometric properties (Bovin et al., Citation2016). The Chinese PCL-5 was adapted by translation and back translation and has been widely used in trauma-exposed Chinese adult and adolescent samples (e.g. Li et al., Citation2018; Wang et al., Citation2017). Cronbach’s α was 0.94 in the adult earthquake survivor sample and 0.94 in the replication adolescent sample.
2.3. Statistical analysis
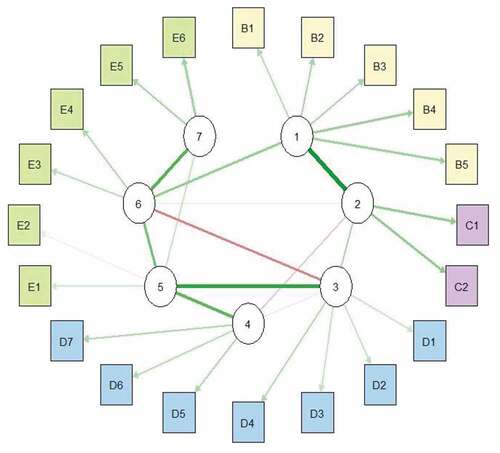
In the first step, a CFA model and a latent network model were separately estimated in the earthquake survivor sample. Both models were estimated the 7-factor hybrid model of DSM-5 PTSD (Armour et al., Citation2015): Intrusion was measured by symptoms B1 to B5, avoidance by symptoms C1 and C2, negative affect by symptoms D1 to D4, anhedonia by symptoms D5 to D7, externalizing behaviours by symptoms E1 and E2, anxious arousal by symptoms E3 and E4, dysphoric arousal by symptoms E5 and E6. Fit indices including RMSEA, CFI, TLI and SRMR were used to determine model fit. According to Hu and Bentler (Citation1999), RMSEA ≤ 0.08, SRMR ≤ 0.08, CFI ≥ 0.90, and TLI ≥ 0.90 indicate good fit, and RMSEA ≤ 0.05, SRMR ≤ 0.08, CFI ≥ 0.95, and TLI ≥ 0.95 indicate excellent fit. Differences in Bayesian Information Criterion (BIC) values were calculated as a reference for model comparison.
The CFA model was estimated by maximum likelihood (ML) estimation. The latent network was estimated via Graphical Gaussian Models (GGMs). The latent network contained seven nodes, and each represented one latent factor in the 7-factor hybrid model of PTSD, consisting of intrusion symptoms, avoidance, negative affect, anhedonia, externalizing behaviours, anxious arousal, and dysphoric arousal. Edge weight between two nodes refers to the regularized partial correlation between those symptom dimensions after controlling for other nodes. As suggested previously (Epskamp, Waldorp, Mõttus, & Borsboom, Citation2018), the graphic least absolute shrinkage and selection operator (gLASSO) (Friedman, Hastie, & Tibshirani, Citation2008) in combination with extended BIC (EBIC, Chen & Chen, Citation2008) were used for estimation of the GGMs by the R package lvnet (Epskamp et al., Citation2017). The function lvnetLasso was utilized for the EBIC-based gLASSO estimation for an exploratory network search. This algorithm tests a sequence of 20 tuning parameters, and automatically chooses the model with the lowest EBIC. Then, the best model was again fit to the data without gLASSO to obtain fit indices. Centrality indices of nodes in the latent network were calculated with the R package networktools. We used bridge expected influence as the centrality index in a network with negative edges (Robinaugh, Millner, & McNally, Citation2016). One-step expected influence is defined as the sum of the value (positive or negative) of all edges that exist between a node and all other nodes. The two-step expected influence is similar, but also considers the indirect effect of the node through other nodes. Indirect effects are weighted by the first edge weight and then added to the 1-step expected influence. Closeness and betweenness were not used because they delete negative edges in calculations. Strength was not used as it uses the absolute value of edge weights (Jones, 2018).
The second step was to examine stability of the latent network. Because the bootstrap-based test of network stability (Epskamp, Borsboom, & Fried, Citation2018) is not available for latent networks at present, we used a confirmatory approach in the replication sample. We used the latent network model found in the adult sample and tested the same model in the replication sample (i.e. trauma-exposed adolescent sample) to assess how well that original model fit in replication. If the model also demonstrated good fit in the replication sample, this would provide evidence of network stability (Fried & Cramer, Citation2017).
3. Results
All participants in the earthquake survivor sample reported experiencing at least one PTSD symptom of mild (1 or higher) severity. The mean PCL-5 score in this sample was 18.8 (range: 1–77, SD = 13.5). According to the DSM-5 diagnostic algorithm of at least one re-experiencing, one avoidance, two negative alterations in cognitions and mood, and two alterations in arousal and reactivity symptoms of at least moderate (2 or higher) severity, prevalence of probable PTSD was 13.8% (165 of 1196). In the replication sample, the mean PCL-5 score was 16.1 (range: 0–77, SD = 14.3), and prevalence of probable PTSD cases was 12.3% (69 of 559).
3.1. Factor analysis results
The seven-factor hybrid model of PTSD demonstrated good fit both in the earthquake survivor sample (χ2 (149) = 525.334, CFI = 0.970, TLI = 0.962, RMESA = 0.046 (90% CI: 0.042–0.050), SRMR = 0.027, BIC = 54991.63) and in the replication adolescent sample (χ2 (149) = 430.449, CFI = 0.952, TLI = 0.938, RMESA = 0.058 (90% CI: 0.052–0.065), SRMR = 0.038, BIC = 27758.15). As shown in , the seven latent variables were well measured by corresponding items.
Table 1. Standardized factor loadings of the 7-factor PTSD model.
3.2. Latent network results
The latent network model demonstrated excellent fit in the earthquake survivor sample (χ2 (158) = 558.427, CFI = 0.968, TLI = 0.962, RMESA = 0.046 (90% CI: 0.042–0.050), SRMR = 0.027, BIC = 54960.94). BIC for the latent network model was lower than the CFA model (ΔBIC = 30.69).
The latent network of PTSD is illustrated in . The strongest edges were between intrusion symptoms and avoidance (edge weight = 0.75), between externalizing behaviours and negative affect (edge weight = 0.63), and between anxious and dysphoric arousal (edge weight = 0.52). There were also medium associations between externalizing behaviours and anhedonia (edge weight = 0.50), between anxious arousal and externalizing behaviours (edge weight = 0.43), and between intrusion symptoms and anxious arousal (edge weight = 0.33). Moreover, a negative edge with medium weight was identified between anxious arousal and negative affect (edge weight = −0.37). Centrality indices of the symptom dimensions are shown in . Overall, externalizing behaviours showed the highest centrality and negative affect showed the lowest centrality in the network.
In the sensitivity analysis, latent network modelling was conducted in a subsample (n = 469) including participants with moderate to severe PTSD symptom severity (i.e. PCL total score ≧ 20). Results were consistent with those found in the original sample. The model demonstrated good fit in the subsample (χ2 (156) = 326.838, CFI = 0.932, TLI = 0.917, RMESA = 0.048 (90% CI: 0.041–0.056), SRMR = 0.042, BIC = 25991.09).
The latent network revealed above in the earthquake survivor sample also demonstrated good fit in the adolescent replication sample (χ2 (170) = 531.051, CFI = 0.938, TLI = 0.931, RMESA = 0.062 (90% CI: 0.056–0.068), SRMR = 0.045, BIC = 27725.91). BIC for the latent network model was 32.24 points lower than for the CFA model. According to fit indices, the latent network generated from the earthquake survivor sample showed good cross-sample stability.
4. Discussion
The current study is the first to investigate the latent network structure of PTSD symptoms. The latent network model fit the sample very well and demonstrated good cross-sample stability, which provides preliminary support for using a combination of latent modelling and network modelling to conceptualize PTSD. BIC values were lower for LNM than CFA in both datasets, which represent better model fit for LNM. Other fit indices were comparable between the two models. It is still too early to claim that the latent network model is superior to the factor analysis model before we obtain more evidence from further studies, however. More studies are needed to test the internal fit of LNM in additional populations. Also, it is necessary for future studies to evaluate external validity of the model.
The externalizing behaviour dimension was identified as the most central symptom dimension in the latent network of DSM-5 PTSD symptoms. This result was not consistent with some previous studies using non-latent network analyses. According to a systematic review (Birkeland et al., Citation2020), intrusion symptoms such as ‘recurrent thoughts of trauma’ and negative affect symptoms of ‘persistent negative emotional state’ were usually reported as symptoms with high centrality in PTSD symptom networks, while externalizing behaviour symptoms (i.e. irritability/anger and self-destructive/reckless behaviour) usually show relatively low centrality. While another study found externalizing behaviour symptoms to demonstrate highest closeness in a DSM-5 PTSD symptom network (Armour, Fried, Deserno, Tsai, & Pietrzak, Citation2017). Our finding’s discrepancy from prior studies could be explained by the long time interval between the trauma exposure and our survey – five and a half years after the disaster, which reflects chronic PTSD symptoms. Previous studies have reported elevated residual externalizing symptoms such as anger/irritability in patients who had meaningful reductions in overall PTSD symptom severity over time (Schnurr & Lunney, Citation2019). Therefore, it is possible that externalizing symptoms might demonstrate high centrality in a network of chronic PTSD symptoms. Considering relatively few studies on chronic PTSD symptom networks, more evidence from empirical studies on chronic PTSD is needed to test this hypothesis.
A strong connection between intrusion symptoms and avoidance was identified in our network, suggesting strong association between them. Intrusion, also known as re-experiencing, and avoidance have always been believed to be the core symptoms unique to PTSD (Yehuda et al., Citation2015). A large amount of theoretical and empirical work has been conducted to reveal relationships between intrusion and avoidance symptoms of PTSD. According to cognitive theories of PTSD, behavioural and cognitive avoidance of reminders of trauma are believed to be defensive strategies to contain distress generated by intrusive memories of traumatic events (Ehlers & Clark, Citation2000). Another cognitive processing model of PTSD also conceptualizes avoidance (including escape behaviours and cognitive reattributions) as coping strategies in response to discomfort caused by the intrusion stage (Creamer, Burgess, & Pattison, Citation1992). Longitudinal studies have found that changes in intrusion were highly correlated with changes in avoidance over 18-month post-trauma (Suvak, Walling, Iverson, Taft, & Resick, Citation2009). Furthermore, many cross-lagged studies of PTSD also found the level of intrusion symptoms could predict levels of avoidance at the next time point, which strongly supports the possible causal relationship between intrusion and avoidance (Maples-Keller, Price, Rauch, Gerardi, & Rothbaum, Citation2017; Schell, Marshall, & Jaycox, Citation2004; Solberg, Birkeland, Blix, Hansen, & Heir, Citation2016). Besides, the association between avoidance and intrusion was also highlighted by avoidance theory proposed by Horowitz (Citation2001). It was hypothesized that avoidance emerges upon initial realization of traumatic events and intrusion symptoms follow as defensive coping processes. This hypothesis was supported by cross-lagged studies finding avoidance symptom severity could predict later intrusion symptom severity (e.g. Pietrzak et al., Citation2014). Most recent non-latent symptom network studies of PTSD also reported medium to strong weighed edges between intrusion and avoidance symptoms, usually between emotional/physiological cue reactivity and both cognitive/behavioural avoidance (Armour et al., Citation2017; Cao et al., Citation2018; von Stockert, Fried, Armour, & Pietrzak, Citation2018), which is in accordance with the cognitive model of PTSD (Ehlers & Clark, Citation2000). It has been demonstrated that intrusion and avoidance mediate exposure to trauma and PTSD symptom development (Creamer et al., Citation1992). Therefore, this strong association between intrusion and avoidance may also play an important role in the onset and maintenance of PTSD’s symptom network, and could probably be an ideal intervention target (Fried et al., Citation2017).
Furthermore, we identified a moderate negative edge between anxious arousal and negative affect. We hypothesize this may reflect a common effect structure between anxious arousal and negative affect. As previously introduced, if both two nodes can cause a third node, a negative edge will generate between these two nodes in a GGM network (Epskamp & Fried, Citation2018). In the current latent network model, both anxious arousal and negative affect were positively related to externalizing behaviours, and the negative edge between the symptom dimensions suggests that externalizing behaviours might result from both anxious arousal and negative affect symptoms. Results from previous studies provide additional support that both anxious arousal and negative affect could cause externalizing behaviours. As described in cognitive action theory of PTSD (Chemtob, Roitblat, Hamada, Carlson, & Twentyman, Citation1988), hypervigilance, which belongs to the anxious arousal dimension, would lead to anger. In a network study of PTSD, moderate edges between hypervigilance and both externalizing behaviours (irritable and reckless behaviours) were also identified (Moshier et al., Citation2018). Regarding the relationship between negative affect and externalizing behaviour, regulation of negative affect has been conceptualized as a potential causal factor in the aetiology of externalizing problems (Halligan et al., Citation2013; Kochanska & Knaack, Citation2003). Moderate to strong edges between negative affect and externalizing behaviour symptoms have also been repeatedly reported in PTSD symptom networks (e.g. Armour et al., Citation2017). According to the current results, it could be inferred that although externalizing behaviour is the most central dimension in the network, it might not be the cause of other symptoms, rather but the outcome instead. As the current study used a cross-sectional design, studies using longitudinal datasets or experiment studies are needed in order to clarify the role of externalizing behaviour in the symptom network of PTSD.
Our current exploration of the latent network of PTSD symptoms provides important implications for future research and clinical practice. The latent network model fits both datasets, which indicates that the model explaining covariation between PTSD symptoms across different development periods and trauma types. Previous PTSD studies used either a latent variable or network model. Some researchers have argued that there is no clear dichotomy between latent variable and network models, and solely relying on one of them will lose sight of the larger clinical picture of mental disorders (Bringmann & Eronen, Citation2018). The current study takes the first empirical step to test this opinion. Results inform that both dimensional and dynamic perspectives are necessary for future PTSD studies. It is still important to explore the underlying cause of different symptom dimensions (e.g. genetic underpinnings, abnormities in brain structure and function), but this approach alone may not be enough, as associations between the dimensions should not be ignored. Uncovering the biological mechanism of symptom dimensions with more connections to other dimensions would efficiently improve our understanding of PTSD pathology. Also, the latent network model highlighted the connections between symptom clusters in intervention. For example, existing structured treatment protocols for PTSD such as prolonged exposure therapy focus on the avoidance–intrusion association (Foa, Hembree, & Rothbaum, Citation2007). Our finding of strong connection between intrusion and avoidance in the latent network provides support for this treatment.
Several limitations of the current study should be noted. First, statistical tools to test the reliability of the latent network have not yet been developed. Reliability has been a major issue in symptom network studies (Forbes et al., Citation2017; Fried & Cramer, Citation2017; Fried et al., Citation2018). Additional studies are needed to verify the reliability and stability of the network. Recent reliability tests based on a bootstrap method might be a future direction once they are developed (Epskamp et al., Citation2018). Second, our study was only conducted in Chinese samples, which restricts generalizability of the results. According to a cross-cultural multisite study of PTSD symptom networks, networks varied between samples with different cultural backgrounds (Fried et al., Citation2018). Therefore, it is important to investigate the latent network structure of PTSD in trauma-exposed samples from different cultural backgrounds. Last, the current study used cross-sectional datasets, which limit our ability to capture the dynamic interplay between different symptom dimensions (Bos et al., Citation2017). Although edges in the cross-sectional network imply possible causal relations, the existence of causal relationships still needs to be verified in future studies. By using Experience Sampling Methodology (ESM) to collect longitudinal data, future research can generate a dynamic latent network of PTSD, which might help explain how symptom dimensions affect each other over time.
This study is the first to investigate the latent network of DSM-5 PTSD symptoms. By uncovering the latent network of PTSD in a Chinese earthquake survivor sample and testing its cross-sample stability, our study shows that PTSD could be well described by utilizing a latent network modelling approach. Results suggest that both latent symptom dimensions and associations between the dimensions should be considered in future PTSD studies and clinical practice.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Armour, C., Fried, E. I., Deserno, M. K., Tsai, J., & Pietrzak, R. H. (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in U.S. military veterans. Journal of Anxiety Disorders, 45, 49–11.
- Armour, C., Műllerová, J., & Elhai, J. D. (2016). A systematic literature review of PTSD’s latent structure in the diagnostic and statistical manual of mental disorders: DSM-IV to DSM-5. Clinical Psychology Review, 44, 60–74. doi:10.1016/j.cpr.2015.12.003
- Armour, C., Tsai, J., Durham, T. A., Charak, R., Biehn, T. L., Elhai, J. D., & Pietrzak, R. H. (2015). Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid anhedonia and externalizing behaviors model. Journal of Psychiatric Research, 61, 106–113.
- Birkeland, M. S., Greene, T., & Spiller, T. R. (2020). The network approach to posttraumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 11(1), 1700614.
- Bollen, K., & Lennox, R. (1991). Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin, 110(2), 305–314.
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13.
- Borsboom, D., & Cramer, A. O. J. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121.
- Bos, F. M., Snippe, E., De Vos, S., Hartmann, J. A., Simons, C. J. P., Van Der Krieke, L., … Wichers, M. (2017). Can we jump from cross-sectional to dynamic interpretations of networks? Implications for the network perspective in psychiatry. Psychotherapy and Psychosomatics, 86(3), 175–177.
- Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., & Keane, M. B. (2016). Psychometric properties of the Turkish version of the PTSD checklist for diagnostic and statistical manual of mental disorders, Fifth Edition (PCL-5). Psychological Assessment, 28(11), 1379–1391.
- Bringmann, L. F., & Eronen, M. I. (2018). Don’t blame the model: Reconsidering the network approach to psychopathology. Psychological Review, 125(4), 606–615.
- Cao, X., Wang, L., Cao, C., Fang, R., Chen, C., Hall, B. J., & Elhai, J. D. (2018). Sex differences in global and local connectivity of adolescent posttraumatic stress disorder symptoms. Journal of Child Psychology and Psychiatry, and Allied Disciplines. doi:10.1111/jcpp.12963
- Cao, X., Wang, L., Cao, C., Zhang, J., Liu, P., Zhang, B., … Elhai, J. D. (2015). Patterns of DSM-5 posttraumatic stress disorder and depression symptoms in an epidemiological sample of Chinese earthquake survivors: A latent profile analysis. Journal of Affective Disorders, 186, 58–65.
- Chemtob, C. M., Roitblat, H. L., Hamada, R. S., Carlson, J. G., & Twentyman, C. T. (1988). A cognitive action theory of post-traumatic stress disorder. Journal of Anxiety Disorders, 2(3), 253–275.
- Chen, J., & Chen, Z. (2008). Extended Bayesian information criteria for model selection with large model spaces. Biometrika, 95(3), 759–771.
- Contractor, A. A., Caldas, S. V., Dolan, M., Natesan, P., & Weiss, N. H. (2019). Invariance of the construct of posttraumatic stress disorder: A systematic review. Journal of Traumatic Stress, 32, 287–298.
- Contreras, A., Nieto, I., Valiente, C., Espinosa, R., & Vazquez, C. (2019). The study of psychopathology from the network analysis perspective: A systematic review. Psychotherapy and Psychosomatics, 88(2), 71–83.
- Cramer, A. O. J., Waldorp, L. J., Van Der Maas, H. L. J., & Borsboom, D. (2010). Comorbidity: A network perspective. Behavioral and Brain Sciences, 33(2–3), 137–150.
- Creamer, M., Burgess, P., & Pattison, P. (1992). Reactions to trauma: A cognitive processing model. Journal of Abnormal Psychology, 101(3), 452–459.
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behavior Research and Therapy, 38, 319–345.
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212.
- Epskamp, S., & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23(4), 617–634.
- Epskamp, S., Rhemtulla, M., & Borsboom, D. (2017). Generalized network psychometrics: Combining network and latent variable models. Psychometrika, 82(4), 904–927.
- Epskamp, S., Waldorp, L. J., Mõttus, R., & Borsboom, D. (2018). The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behavioral Research, 1–28. doi:10.1080/00273171.2018.1454823
- Fani, N., Michopoulos, V., van Rooij, S. J. H., Clendinen, C., Hardy, R., Jovanovic, T., … Stevens, J. S. (2019). Structural connectivity and risk for anhedonia after trauma: A prospective study and replication. Journal of Psychiatric Research, 116, 34–41.
- Foa, E. B., Hembree, E. A., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences. New York, NY: Oxford University Press.
- Forbes, M. K., Wright, A. G. C., Markon, K. E., & Krueger, R. F. (2017). Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology, 126(7), 969–988.
- Forbes, M. K., Wright, A. G. C., Markon, K. E., & Krueger, R. F. (2019). The network approach to psychopathology: Promise versus reality. World Psychiatry, 18(3), 272–273.
- Fried, E. I., & Cramer, A. O. J. (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12(6), 999–1020.
- Fried, E. I., Eidhof, M. B., Palic, S., Costantini, G., Huisman-van Dijk, H. M., Bockting, C. L. H., … Karstoft, K. I. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351.
- Fried, E. I., van Borkulo, C. D., Cramer, A. O. J., Boschloo, L., Schoevers, R. A., & Borsboom, D. (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52(1), 1–10.
- Friedman, J., Hastie, T., & Tibshirani, R. (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics, 9(3), 432–441.
- Halligan, S. L., Cooper, P. J., Fearon, P., Wheeler, S. L., Crosby, M., & Murray, L. (2013). The longitudinal development of emotion regulation capacities in children at risk for externalizing disorders. Development and Psychopathology, 25(2), 391–406.
- Horowitz, M. J. (2001). Stress response syndromes (3rd ed.). New York: Jason Aronson.
- Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi:10.1080/10705519909540118
- Kendler, K. S., Zachar, P., & Craver, C. (2011). What kinds of things are psychiatric disorders? Psychological Medicine, 41(6), 1143–1150.
- Kochanska, G., & Knaack, A. (2003). Effortful control as a personality characteristic of young children: Antecedents, correlates, and consequences. Journal of Personality, 71(6), 1087–1112.
- Li, G., Wang, L., Cao, C., Fang, R., Liu, P., Luo, S., … Elhai, J. D. (2018). DSM-5 posttraumatic stress symptom dimensions and health-related quality of life among Chinese earthquake survivors. European Journal of Psychotraumatology, 1–7. doi:10.1080/20008198.2018.1468710
- Liu, L., Wang, L., Cao, C., Qing, Y., & Armour, C. (2016). Testing the dimensional structure of DSM-5 posttraumatic stress disorder symptoms in a nonclinical trauma-exposed adolescent sample. Journal of Child Psychology and Psychiatry, 57(2), 204–212.
- Liu, P., Wang, L., Cao, C., Wang, R., Zhang, J., Liu, P., … Elhai, J. D. (2014). The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. Journal of Anxiety Disorders, 28, 345–351.
- Maples-Keller, J. L., Price, M., Rauch, S., Gerardi, M., & Rothbaum, B. O. (2017). Investigating relationships between PTSD symptom clusters within virtual reality exposure therapy for OEF/OIF Veterans. Behavior Therapy, 48(2), 147–155.
- Moshier, S. J., Bovin, M. J., Gay, N. G., Wisco, B. E., Mitchell, K. S., Lee, D. J., … Marx, B. P. (2018). Examination of posttraumatic stress disorder symptom networks using clinician-rated and patient-rated data. Journal of Abnormal Psychology, 127(6), 541–547.
- Pietrzak, R. H., Feder, A., Schechter, C. B., Singh, R., Cancelmo, L., Bromet, E. J., & Southwick, S. M. (2014). Dimensional structure and course of post-traumatic stress symptomatology in world trade center responders. Psychological Medicine, 44(10), 2085–2098.
- Pietrzak, R. H., Tsai, J., Armour, C., Mota, N., Harpaz-Rotem, I., & Southwick, S. M. (2015). Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: Results from the national health and resilience in veterans study. Journal of Affective Disorders, 174, 522–526. doi:10.1016/j.jad.2014.12.007
- Robinaugh, D. J., Hoekstra, R. H. A., Toner, E. R., & Borsboom, D. (2020). The network approach to psychopathology: A review of the literature 2008–2018 and an agenda for future research. Psychological Medicine, 50(3), 353–366.
- Robinaugh, D. J., Millner, A. J., & McNally, R. J. (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125(6), 747–757.
- Schell, T. L., Marshall, G. N., & Jaycox, L. H. (2004). All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology, 113(2), 189–197.
- Schmittmann, V. D., Cramer, A. O. J., Waldorp, L. J., Epskamp, S., Kievit, R. A., & Borsboom, D. (2013). Deconstructing the construct: A network perspective on psychological phenomena. New Ideas in Psychology, 31(1), 43–53.
- Schnurr, P. P., & Lunney, C. A. (2019). Residual symptoms following prolonged exposure and present-centered therapy for PTSD in female veterans and soldiers. Depression and Anxiety, 36(2), 162–169.
- Segal, A., Wald, I., Lubin, G., Fruchter, E., Ginat, K., Ben Yehuda, A., … Bar-Haim, Y. (2019). Changes in the dynamic network structure of PTSD symptoms pre-to-post combat. Psychological Medicine, 1–8. doi:10.1017/S0033291719000539
- Solberg, O., Birkeland, M. S., Blix, I., Hansen, M. B., & Heir, T. (2016). Towards an exposure-dependent model of post-traumatic stress: Longitudinal course of post-traumatic stress symptomatology and functional impairment after the 2011 Oslo bombing. Psychological Medicine, 46(15), 3241–3254.
- Suvak, M., Walling, S. M., Iverson, K. M., Taft, C. T., & Resick, P. A. (2009). Multilevel regression analyses to investigate the relationship between two variables over time: Examining the longitudinal association between intrusion and avoidance. Journal of Traumatic Stress, 22(6), 622–631.
- von Stockert, S. H. H., Fried, E. I., Armour, C., & Pietrzak, R. H. (2018). Evaluating the stability of DSM-5 PTSD symptom network structure in a national sample of U.S. military veterans. Journal of Affective Disorders, 229(December2017), 63–68.
- Wang, L., Cao, X., Cao, C., Fang, R., Yang, H., & Elhai, J. D. (2017). Factor structure of DSM-5 PTSD symptoms in trauma-exposed adolescents: Examining stability across time. Journal of Anxiety Disorders, 52(February), 88–94.
- Yehuda, R., Hoge, C. W., McFarlane, A. C., Vermetten, E., Lanius, R. A., Nievergelt, C. M., … Hyman, S. E. (2015). Post-traumatic stress disorder. Nature Reviews Disease Primers, 1(10), 1–22.
- Young, G. (2015). Causality in psychiatry: A hybrid symptom network construct model. Frontiers in Psychiatry, 6(November). doi:10.3389/fpsyt.2015.00164