ABSTRACT
Background
Refugees are at high risk for developing post-traumatic stress disorder (PTSD). Narrative exposure therapy (NET) is an evidence-based treatment of PTSD, designed for patients exposed to (multiple) traumatic events and recommended for patients with culturally diverse backgrounds. In clinical practice, adherence to the NET-protocol has been challenged because of psychosocial complexities and comorbid disorders.
Objective:
The current study investigated the feasibility of NET embedded in an outpatient day treatment programme for refugees and examined reduction in PTSD symptoms and improvement of global functioning as well as correlates of change.
Method
Participants were patients who consecutively entered an outpatient daytreatment programme from 2013-2017. The majority had a history of prior unsuccessful treatment. PTSD was assessed with the Clinically Administered PTSD Scale (CAPS) before and after finishing NET. Global Assessment of Functioning (GAF) was used to examine changes in functioning. Changes in PTSD scores and functioning were analyzed using paired t-tests and reliable change indices. Patients showing significant improvement were compared to those who did not, on patient and treatment characteristics, including sex, age, region of origin, childhood trauma and treatment duration and dosage of NET.
Results:
Of 97 patients, 76 (78.4%) completed NET. Completers had a longer residency and were more likely to have a partner. Significant reductions in PTSD symptoms and improvements in global functioning were observed. Twenty-eight percent showed reliable improvement with large effect sizes. Four patients did no longer meet the criteria for PTSD. No strong moderators for changes were found. Patients who did not improve more often had a history of childhood trauma.
Conclusions
NET embedded in an outpatient day treatment programme appears to be feasible. In those who improved, a substantial decline in symptoms and improvement of functioning were observed. The findings suggest that a socially supportive living environment enhances acceptability of trauma-focused treatment in refugees.
Antecedentes: Los refugiados están en alto riesgo de desarrollar trastorno de estrés postraumático (TEPT). La terapia de exposición narrativa (NET) es un tratamiento basado en evidencia del TEPT, diseñado para pacientes expuestos a eventos traumáticos (múltiples) y recomendado para pacientes con antecedentes culturalmente diversos. En la práctica clínica, la adherencia al protocolo NET ha sido desafiada debido a las complejidades psicosociales y los trastornos comórbidos.
Objetivo: El estudio actual investigó la factibilidad de NET incluido en un programa de tratamiento diurno ambulatorio para refugiados y examinó la reducción de síntomas de TEPT y la mejora del funcionamiento global, así como correlatos de cambio.
Método: Los participantes fueron pacientes que ingresaron consecutivamente a un programa de tratamiento diurno ambulatorio entre 2013–2017. La mayoría tenía antecedentes de tratamiento previo sin éxito. El TEPT se evaluó con la Escala de TEPT administrada clínicamente (CAPS, por sus siglas en ingles) antes y después de finalizar NET. La Evaluación Global del Funcionamiento (GAF) se utilizó para examinar los cambios en el funcionamiento. Los cambios en los puntajes y el funcionamiento del TEPT se analizaron mediante t-test pareados e índices de cambio confiables. Los pacientes que mostraron una mejoría significativa fueron comparados con aquellos que no lo hicieron, en cuanto a las características del paciente y tratamiento, incluidos sexo, edad, región de origen, trauma infantil y duración del tratamiento, y dosificación de NET.
Resultados: De 97 pacientes, 76 (78.4%) completaron NET. Los que completaron tenían un periodo de residencia más largo y tenían más probabilidades de tener una pareja. Se observaron reducciones significativas en los síntomas de TEPT y mejoras en el funcionamiento global. Veintiocho por ciento mostró una mejora confiable con grandes tamaños de efecto. Cuatro pacientes ya no cumplían los criterios para TEPT. No se encontraron fuertes moderadores para los cambios. Los pacientes que no mejoraron con mayor frecuencia tenían antecedentes de trauma infantil.
Conclusiones: NET integrado en un programa de tratamiento ambulatorio diurno se muestra factible. En aquellos que mejoraron, se observó disminución sustancial de los síntomas y una mejoria del funcionamiento. Los hallazgos sugieren que un entorno de vida de apoyo social aumenta la aceptabilidad del tratamiento centrado en el trauma en los refugiados.
背景: 难民患创伤后应激障碍 (PTSD) 的风险很高。叙事暴露疗法 (NET) 是PTSD的循证治疗, 旨在用于暴露于 (多种) 创伤事件的患者, 并建议具有多重文化背景的患者使用。在临床实践中, 由于社会心理的复杂性及并发症, 对NET协议的依从性受到了挑战。
目标: 本研究探究了将NET纳入难民的门诊日间治疗计划中的可行性, 并考查了PTSD症状的减轻, 整体功能的提高以及变化间的相关性。
方法: 参与者为2013至2017年间连续参与门诊日间治疗计划的患者。多数患者有既往治疗失败的病史。在完成NET前后, 使用临床用PTSD量表 (CAPS) 对PTSD进行了评估。使用功能大体评估量表 (GAF) 考查了功能的变化。使用配对t检验和可靠的变化指数分析了PTSD得分和功能的变化。对表现出显著改善的患者与未表现出显著改善的患者进行患者及治疗特征上的比较, 包括性别, 年龄, 籍贯, 童年期创伤以及治疗时间和NET剂量。
结果: 97例患者中, 有76例 (78.4%) 完成了NET。完成者的居住时间更长, 并且更有可能拥有伴侣。观察到了PTSD症状的明显减轻以及整体功能的提高。 28%的患者表现出高效应量的可靠改善。四名患者不再符合PTSD标准。未发现这些变化较强的调节因子。病情无改善的患者常有童年期创伤史。
结论: 将NET纳入门诊日间治疗计划似乎是可行的。在有所改善的患者中, 观察到症状的显著下降和功能的提高。研究结果表明, 社会支持的生活环境提高了难民对聚焦创伤疗法的可接受性。
PALABRAS CLAVE:
HIGHLIGHTS:
- • NET embedded in an outpatient day treatment programme is feasible and facilitates the chance of completion of trauma-focused therapy, even in patients with a history of unsuccessful treatment.
- • A substantial decline in symptoms and better functioning was observed in those improved.
- • A socially supportive living environment enhances the acceptability of trauma-focused treatment in refugees.
At the end of 2019, 70.8 million people were forcibly displaced around the globe as a result of persecution, conflict, war, violence or/and human rights violations. Whereas the majority is internally displaced, 25.9 million people are considered refugees and 3.5 million asylum seekers (United Nations High Commissioners for Refugees [UNHCR], Citation2019). Refugees are often sheltered in a neighbouring country, but some of them seek asylum in Western countries. Nearly all of them have been exposed to war, have witnessed or experienced violence, or the loss of loved ones, and some of them have been victim of torture. After suffering from adversities in their homeland, insecurity, starvation, and poverty during the flight, as well as adjustment stress during resettlement, refugees and war-affected populations are at high risk for post-traumatic stress disorder (PTSD) and major depressive disorder (MDD) (American Psychiatric Association [APA], Citation2013). A high prevalence of PTSD is found in epidemiological studies, with prevalence of 9% PTSD and 5% with MDD (Steel et al., Citation2009; Fazel, Wheeler, & Danesh, Citation2005). Even several years after resettlement mental disorders tend to be highly prevalent (Bogic, Njoku, & Priebe, Citation2015). The need for adequate psychological treatment for refugees is self-evident.
A systematic review revealed that psychosocial interventions in refugees and asylum seekers resettled in high-income countries were effective in decreasing PTSD symptoms relative to control groups, and that narrative exposure therapy (NET) was the best-supported intervention (Nosè et al., Citation2017). NET is an evidence-based short-term intervention for PTSD, designed for patients exposed to complex or multiple traumatic events (Schauer, Neuner, & Elbert, Citation2011). It has been found to be feasible in a wide range of participants with culturally diverse backgrounds and cultural settings (Nosè et al., Citation2017; Robjant & Fazel, Citation2010).
Despite the evidence, clinical experience suggests that psychosocial problems, comorbid mental health problems, and ongoing current stressors of refugees can challenge the feasibility of trauma-focused therapy with severely traumatized refugees. These pressing issues may prevent clinicians from adhering to the treatment protocol and may reduce the chance to complete trauma-focused therapy. Furthermore, ongoing current stressors may also be related to the severity of mental health complaints and prevent patients to complete or benefit from treatment. Several studies describe the debilitating impact of postmigration factors and ongoing stressors on mental health (Chu, Keller, & Rasmussen, Citation2013; LeMaster et al., Citation2018; Schick et al., Citation2018; Steel, Dunlavy, Harding, & Theorell, Citation2017; Tinghög et al., Citation2017). Addressing these ongoing stressors would contribute to better mental health (Miller & Rasmussen, Citation2017).
In clinical practice, these types of problems are often addressed in group treatment or a multimodal setting. In a review on group treatment for PTSD, group treatment was found efficacious compared with no treatment, and combining individual and group interventions was recommended (Sloan, Bovin, & Schnurr, Citation2012). The few studies on multimodal approaches in refugees did not yield compelling evidence for their efficacy (Nickerson, Bryant, Silove, & Steel, Citation2011). However, in a recent naturalistic study based on this approach, a decrease of PTSD complaints and increase of quality of life were found (Stammel et al., Citation2017).
We hypothesized that the feasibility of NET would improve when it would not be offered as a stand-alone treatment modality but embedded in a multidisciplinary multimodal day treatment setting. In such a multidisciplinary setting different types of counselling and services could be offered ranging from group therapy, psychosocial counselling and social work, to pharmacotherapy according to the individual needs, alongside trauma-focused treatment (NET). The clinician providing NET would not have to postpone or interrupt the trauma-focused therapy when psychosocial problems could be discussed in a group or with a social worker of the multidisciplinary team. In such a setting we expected that patients would be supported to complete NET, adherence to the treatment protocol of the NET-therapists would be facilitated and ongoing stressors could be dealt with. Then, it would be more likely that patients actually benefit from NET and the impact of ongoing stressors would be alleviated. Accordingly, we developed an outpatient day treatment programme for refugees using a well-structured three phase-based model (Cloitre et al., Citation2012; Herman, Citation2015; National Institute for Health and Care Excellence [NICE], Citation2005).
In the present naturalistic study, we investigated the feasibility of NET embedded in an outpatient day treatment programme for refugees and examined the changes of PTSD symptoms and global functioning as well as correlates of change. The feasibility of NET was examined by analysing the treatment trajectory of the patients (including NET completion, drop out and adherence to the treatment protocol by the therapists). Furthermore, changes in symptom severity, diagnoses of PTSD and global functioning during the treatment were assessed. Finally, we explored whether improvement in PTSD and functioning was associated with a number of variables, including patient characteristics such as sex, age, region of origin and treatment characteristics, such as treatment duration and dosage of NET to gain insight in what factors may moderate symptom changes.
1. Methods
1.1. Participants
Participants (N = 97) were all refugees who entered the outpatient day treatment programme for PTSD between January 2013 and February 2017 at our treatment facility, ARQ Centrum ’45 (C45). C45 is a Dutch mental health institute specialised in the treatment of psychopathology associated with trauma and (multiple) loss due to war and organised violence. C45 receives national referrals of patients, including refugees who cannot be treated in general mental health care because of the complexity or severity of their complaints or who have shown insufficient response to treatment elsewhere. ‘Refugee’ refers to political arrival status of a person who was exposed to traumatic events in his or her home country and during the flight, often followed by adverse life situations.
Some of the refugees entering treatment are torture survivors. They have been exposed to torture as defined in article 1 of the United Nations Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment: ‘any act by which severe pain or suffering, whether physical or mental, is intentionally inflicted on a person for such purposes as obtaining from him or a third person information or a confession, punishing him for an act he or a third person has committed or is suspected of having committed, or intimidating or coercing him or a third person, or for any reason based on discrimination of any kind, when such pain or suffering is inflicted by or at the instigation of or with the consent or acquiescence of a public official or other person acting in an official capacity. It does not include pain or suffering arising only from, inherent in or incidental to lawful sanctions’ (United Nations General Assembly, Citation1984).
The outpatient day treatment programme was offered as a standard modality to all patients after intake, when they suffered from severe PTSD complaints, multiple trauma, and to those who had unsuccessful treatment elsewhere or/and had limited social support. Unsuccessful treatment refers to treatment that did not bring about any change in PTSD symptoms or functioning or that had not been completed. When they were not willing to participate in the outpatient day treatment programme or had insufficient Dutch language proficiency, they were offered individual trauma-focused treatment or supportive treatment in our outpatient clinic. Furthermore, patients with acute and active suicidality, severe manifest psychotic symptoms and/or severe alcohol or substance dependency were not eligible for the treatment programme. Also, refugees whose symptoms were related primarily to the traumatic loss of loved ones were referred to an outpatient day patient treatment for traumatic grief (De Heus et al., Citation2017).
1.2. The outpatient day treatment programme for refugees
The outpatient day treatment programme for refugees was administered by a multidisciplinary team. The team consisted of a psychiatrist, a medical doctor, two psychiatrists in training, two clinical psychologists, two psychotherapists, three psychologists in training, two psychomotor therapists, an art therapist, and three social workers. The members of the team were predominantly native Dutch women, with an age ranging from approximately 20 to 60 years. The team included a male psychiatrist, a male clinical psychologist and two male social workers. Throughout the years, the team members did not change, except for the psychiatrists and psychologists in training of whom several had a non-Western origin and could speak either Arabic, Farsi/Dari or Servokroatic.
The group-based outpatient day treatment programme comprised of a weekly five-hour programme. The programme lasted one year and consisted of three phases, each phase with a duration of 4 months. Every 4 months a new group of eight participants started the programme in phase 1 (see ).
Figure 1. Outline of the outpatient treatment programme for refugees. The programme consists of three phases having a 4-month duration.
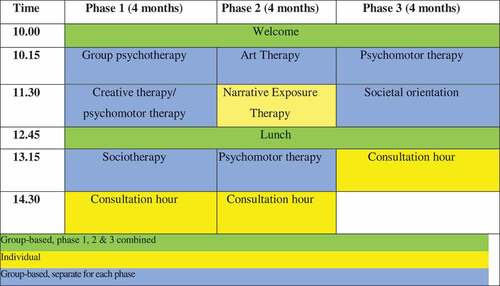
Phase 1. The focus of phase 1 was on building mutual trust and support within the group as well as gaining control over psychiatric symptoms. This was obtained by offering different group therapies. In group psychotherapy, therapists facilitated a holding environment and focused on getting to know and learn to trust each other, and on cohesion within the group. Sociotherapy addressed emotion regulation, sleeping patterns and coping skills. Through art therapy, patients were encouraged in sharing (positive and negative) experiences and expressing emotions. Through psychomotor therapy, patients were assisted to gain control over emotional instability and physical signs of anxiety. When indicated, medication was prescribed in accordance with the guidelines for PTSD (NICE, Citation2005).
Phase 2. The focus of phase 2 was on emotionally and cognitively processing the traumatic experiences, through individual NET. During NET, therapist and patient together develop a narrative of the patient’s life by identifying the most meaningful (positive and negative) life events, symbolized by ‘flowers’ and ‘stones’, respectively. The therapist supports the patient in constructing a chronological narrative of his/her whole life, while encouraging exposure to traumatic experiences. Exposure to each traumatic event in a chronological order aims to reconnect fragmented traumatic memories with the autobiographical memory and in order to diminish trauma-related complaints (Schauer et al., Citation2011). Furthermore, psychomotor group therapy and art therapy were offered, further supporting coping with emotions.
Phase 3. The focus of phase 3 was on further integrating the traumatic experiences in the life history, shifting attention from the past to the present and making future plans. In supportive group therapy patients were encouraged to discuss future plans and strengthen social networks. They were assisted in applying for jobs or voluntary work and expanding their fields of interest. In psychomotor therapy emotion regulation skills were consolidated by exercises.
In each phase, consultations with the psychotherapist, physician or social worker were offered when needed.
1.3. Procedure
When participants entered the programme, an inventory was made regarding patient characteristics, treatment needs and current stressors at the consultation with an individual therapist. Finally, treatment goals were formulated. Assessments pre- and post-treatment were conducted for clinical purposes during the programme, in the first month of the day treatment programme before the start of NET (T1) and after finishing NET (T2), in general during the third phase of the programme, by a team of trained and supervised psychologists/psychologists in training. The person who carried out the assessment was not the same person as the individual therapist. The primary aim of these assessments was providing feedback to the therapist regarding progress in a number of treatment outcomes due to the individual NET. Assessment data were archived for scientific research purposes. Participants were informed about the storage of the assessment data and given the opportunity to have their data removed from the database. Upon consultation, the institutional review board of Leiden University stated that no review of the ethical merits of this study was needed and obtaining informed consent was not requisite, because assessments were conducted primarily for clinical and secondarily for research purposes.
The protocol was applied in phase 2 of the Day Treatment Programme in which the sessions were scheduled every week. In case of no show, the therapist continued NET the following week or scheduled sessions twice a week to compensate for missed appointments (of NET). After an interruption of treatment due to holidays or somatic illness the therapist read the narrative before the continuation of the exposure sessions. NET sessions lasted 75 minutes on average. NET was offered by trained therapists, and treatment progress was discussed every 6 to 8 weeks in intervision with the NET therapists of the programme.
Data on treatment characteristics, such as treatment attendance and missed appointments, adherence to the treatment protocol were recorded every week in the Electronic Patient File (EPF). For NET completers, i.e. those who did not drop out during NET, the duration of the individual treatment (in number of sessions) was registered. Non-completers, i.e. those who did drop out during NET, were asked the reasons for drop out by their clinician during consultations on treatment progress.
Data from the assessments were merged to the data on treatment attendance, missed appointments and adherence to the treatment protocol from the EPF by the data manager of the organization. Data were subsequently anonymized by removing and altering information in the data file such that the data could not directly be traced to an individual patient by the researchers. Finally, the anonymized data file was made available to the researchers.
1.4. Instruments
1.4.1. Clinician-Administered PTSD Scale
The Dutch version of the Clinician-Administered PTSD Scale (CAPS) for the fourth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; Blake et al., Citation1995) as well as the version for DSM-5 (CAPS-5; Boeschoten et al., Citation2018; Weathers et al., Citation2018) were used to assess the current diagnosis of PTSD and the current severity of PTSD complaints. The CAPS is a clinician-rated interview that taps all diagnostic criteria for PTSD of the DSM. In the first period of data collection, the CAPS-IV was used. Excellent psychometric properties across a wide variety of clinical research settings and trauma populations have been reported for the CAPS-IV. It is the ‘gold’ standard criterion measure in the field of psychotrauma because of its convergent and discriminant validity, diagnostic utility, and sensitivity to clinical change (Weathers, Keane, & Davidson, Citation2001). The summed score of frequency and intensity of symptoms represents overall current PTSD severity with scores >80 indicating extreme PTSD (range 0–136). A current PTSD diagnosis was calculated by using the default F1/I2 rule, whereby a symptom is considered present if Frequency is rated 1 or higher and Intensity is rated 2 or higher (Weathers et al., 2017). In the second period of data collection after the introduction of the DSM-5 (American Psychiatric Association [APA], Citation2013), the CAPS-5 was used. Psychometric properties of this version also have been found to be solid (Boeschoten et al., Citation2018; Weathers et al., Citation2018). It assesses all DSM-5 criteria of PTSD. A single symptom severity score is rated based on a combination of frequency and intensity on a 5-point scale ranging from 0 to 4. By summing the scores of the 20 DSM-5 PTSD symptoms, a total of current PTSD symptom severity score was computed (range 0–80). According to the CAPS-5 scoring rule (SEV2 rule), a symptom or impairment was considered present if its severity is rated with 2 or higher (Weathers et al., Citation2018). A current PTSD diagnosis was established using the DSM-5 algorithm with the SEV2 rule.
1.5. Global Assessment of Functioning
Global Assessment of Functioning (GAF) was rated by the patients’ clinician – who was not the NET therapist – at pre- and post-treatment. The GAF score ranges from 0 to 100 in line with DSM-IV and reflects an individual’s occupational, psychological, and social functioning on a continuum of mental health illness. The scores are based on defining characteristics, which include both symptoms and social functioning (Startup, Jackson, & Bendix, Citation2002). A higher score refers to better functioning. Research showed that the GAF score proved to be a reliable measure (Jones, Thornicroft, Coffey, & Dunn, Citation1995). Although the GAF score was originally designed as a continuous measure, in clinical practice it is mostly used as a categorical measure. In addition, the range of the GAF-scores in the present study was limited – i.e. the pre- and post-treatment GAF-scores ranged between 40 and 70. Therefore, the GAF score was treated as an ordinal measure instead of continuous by dividing the original into 20 ordinal categories (category 1: GAF score 1–5, category 2: 6–10 etcetera).
1.6. Statistical analysis
Statistical analyses were run in the statistical package SPSS.
The first step of the evaluation of the feasibility of the outpatient day treatment programme included descriptive analysis of treatment characteristics including completion of NET, duration of NET, drop-out and adherence to the treatment protocol.
Treatment completers and non-completers were compared on several characteristics using chi-square tests and independent sample t-tests. They were compared on the following characteristics: region of origin (Eastern Europe, the Middle East/Maghreb, Iran–Afghanistan region, and Niger/Congo), age, sex, having a partner (yes or no), type of trauma (torture or no torture), age of first trauma, type and number of daily stressors (problems on life domains, including family relationships, financial problems, work-related problems or living conditions).
Change of symptoms and global functioning was examined in those patients who had a complete assessment pre- and posttreatment. A paired-sample t-test was used to test whether there was a change in the mean level of PTSD symptom severity between the pre- and post-treatment measurement. Cohen’s d were calculated (Cohen, Citation1988). In order to obtain a single pre-treatment (T1) and post-treatment (T2) score for PTSD symptom severity, the PTSD symptom severity scores of the CAPS-IV and CAPS-5 were standardized and combined. To make sure that differences between T1 and T2 were conserved, standardization of the total PTSD symptom severity scores at T1 as well as T2 was based on the mean and standard deviation at T1. The same version of the CAPS was used at T1 and T2 for 55 out of a total of 56 patients for whom data on PTSD were available at T1 and T2. Because no valid comparison can be made between scores derived from the CAPS-IV and CAPS-5, the standardized PTSD symptom severity scores, as well as the diagnosis scores at T1 and T2 were recoded to missing for one patient who was assessed with the CAPS-IV at T1 and CAPS-5 at T2. The Wilcoxon signed-rank test for related samples was used to test whether there was a change in the median level of the ordinal GAF score between the pre- and post-treatment measurement.
Because of the relatively small sample size, an alternative method of evaluating change in PTSD symptom severity was also used that does rely on individual differences rather than means. Individual changes in PTSD symptom severity were categorized into recovered, improved, unchanged, and deteriorated from T1 to T2 based on criteria of the Reliable Change Index (RCI) and clinically significant change. The RCI was used to establish whether the difference between two test scores obtained at two measurement occasions reflects statistically reliable change, and was calculated conform the method described by Jacobson and Truax (Citation1991), i.e. the ratio between the difference score between T1 and T2 and the standard error of the difference score. RCI values larger than 1.96 (or smaller than −1.96) indicate that there is a statistically reliable difference between two test scores, i.e. with 95% certainty, the difference between the test scores is due to actual change (improvement or deterioration) rather than measurement error. Clinically significant change was defined as a shift from a clinical to a subclinical level of PTSD symptoms, i.e., respectively, the presence and absence of a diagnosis of PTSD based on the CAPS. Recovery can be defined by both a clinically significant change and a statistically reliable improvement (based on RCI). Improvement and deterioration can be defined by a statistically reliable improvement or deterioration (based on RCI), but no clinically significant change. Unchanged symptom severity can be defined by the absence of a statistically reliable change, based on the RCI. Because the GAF score was an ordinal measure and no clinical cut-off score has been defined for it, we based the significant change for the GAF score on the DSM-IV where the GAF scale is divided into 10 gradations of global functioning with 10-point intervals (e.g. GAF score 1–10: Persistent danger of severely hurting self or others; GAF score 11–20: Some danger of hurting self or others). Based on this categorization, clinically significant change with regard to the GAF score was assumed when there was a difference of at least 10 points (i.e. 2 categories on the constructed ordinal measure) between T1 and T2.
The group of patients who recovered or improved regarding PTSD complaints and on global functioning and the group of patients who did not were compared on patient and treatment characteristics again using chi-square and independent samples t-tests to gain insight in who is able to benefit from this type of treatment and who is not. Patient characteristics were region of origin, age, sex, having a partner, type of trauma (torture survivor or not), age of first trauma, type and number of current stressors (problems on several life domains, including family, relationship, financial, work or living conditions). Treatment characteristics were history of prior treatment (yes/no), length or duration of NET (number of sessions), and number of minutes of NET.
2. Results
2.1. Patient characteristics
Ninety-seven patients started the treatment during the study period. Most participants were men (N = 75; females N = 22) with an average age of 45.5 (SD = 8.5, range 25–62) years. The participants originated mainly from Eastern Europe (N = 38), the Middle East/Maghreb (N = 32), Iran–Afghanistan region (N = 21), and Niger/Congo (N = 5). The educational level varied from no education/primary school (N = 16), secondary education (N = 48) to high education (N = 31). Sixty participants had a partner (61.9%). The average stay in the Netherlands before entering treatment at C45 was 17 years (SD = 6.5, range 3–35 years). The vast majority had obtained a (permanent) residency permit or Dutch citizenship. All patients suffered from cumulative trauma in the past and were affected by war violence experiencing or witnessing, i.e. violence, abuse, or/and loss. Thirty-three (34.4%) experienced trauma before the age of 12. This could encompass domestic violence, sexual abuse or war-related trauma. Twenty-eight (28.9%) patients were torture survivors. The majority of the participants reported ongoing stressors in their current life; 84.5% reported somatic comorbidity, 66% reported family problems, 54.2% reported work problems, i.e. unemployment, conflicts at work, 49% suffered from financial problems, i.e. debts, insufficient income, and 22.7% reported problems with the living conditions, i.e. poor housing; 64.6% reported three or more current stressors. Eighty-three patients (85%) entering treatment in our programme were patients with prior unsuccessful treatment elsewhere. Two thirds of those with an unsuccessful treatment history had been offered another form of trauma-focused therapy, such as EMDR. In , the patient characteristics are summarized.
Table 1. Sociodemographic and trauma characteristics of the participants (N = 97).
2.2. The feasibility of NET
The majority of the 97 patients were able to complete NET (N = 76; 78.4%); 61 patients (80.2%) completed NET within the outpatient day treatment programme, whereas 15 patients continued individual NET in our outpatient clinic after the end of the treatment programme (i.e. after ending phase 3). The average duration of the NET of the completers was 12.5 sessions (SD = 6.6). Sessions were scheduled as planned weekly and occasionally twice a week to compensate for missed appointments. Session duration was 75 minutes. The average dose of NET was 965 minutes (SD = 412). Adherence to the treatment protocol of the NET therapists when applying NET was sufficient. Seventy-eight percent of the therapists were able to focus on the NET protocol and did not spend more than 2 sessions on other issues (90% no more than 3 sessions). In those patients who were not able to complete NET within the outpatient day treatment programme, but continued individual NET in our outpatient clinic, the duration of therapy was extended because the NET was interrupted at several occasions, often related to absence because of somatic illness, holidays and current stressors.
Drop out of patients occurred at several moments during the programme. Three patients left the programme during phase 1, 13 during phase 2 and 4 patients dropped out from outpatient treatment. The reasons for drop-out varied and sometimes patients mentioned more than one reason. Eight patients of all 20 patients who did not complete NET mentioned that they were unable to complete treatment because of the difficulties to deal with the emotions provoked by the confrontation with the traumatic memories during NET or felt the group setting was too demanding. They were offered stabilization interventions as an alternative treatment in an individual trajectory. Other patients who dropped out mentioned reasons related to current stressors, including somatic illness, practical, familial or financial problems (travel expenses to the institution).
Completers and non-completers were compared with chi-square analyses and independent samples t-tests on patient characteristics and treatment characteristics. Only a few significant differences were found between NET completers and non-completers. The average residence in the Netherlands was significantly longer for the completers (M = 18.1, SD = 5.8) in comparison to non-completers (M = 13,5, SD = 7.3, t (85) = −2.9, p < 0.01), and completers were also more likely to have a partner (χ2(1) = 4.9, p < 0.05). Non-completers reported more often problems with their living condition (housing) as a current stressor than non-completers (χ2(1) = 4.2, p < 0.05), but did not report significantly more current stressors than completers.
2.3. Changes in PTSD symptoms during treatment
Only participants with a complete pre- and post-treatment assessment of the CAPS of the outpatient day treatment programme were included in the analysis (N = 55 for the CAPS). No differences were found between patients with a complete assessment and those without on patient characteristics. The mean scores of PTSD symptoms on CAPS-IV and CAPS-5 are summarized in . The mean PTSD scores of the patients’ pre-treatment indicated a high symptom severity, which can be categorized as ‘extreme PTSD’ and ‘severe PTSD’ according to the standards of Weathers et al. (Citation2001); Weathers et al. (Citation2018).
Table 2. PTSD symptoms of CAPS-IV and CAPS-5.
A significant decrease in standardized CAPS scores was found from pre- to post-treatment (t(54) = 5.43, p < 0.001). Paired samples t-test for the CAPS resulted in a large effect size (Cohen’s d was 0.78). shows the results of the analysis on the combined CAPS z-scores. As indicated by the RCIs, 13 (23.7%) patients reported improvement with regard to PTSD symptoms and four patients (7%) showed full remission of PTSD; 38 (69%) reported no change with regard to PTSD symptoms. No patients deteriorated. We demonstrate in that those classified as recovered or improved according to the RCIs substantially declined in PTSD symptom severity by approximately 2 to 3 standard deviations.
Table 3. Changes of symptoms on CAPS combined scores (z-scores) and RCI with regard to PTSD.
Table 4. Median of the GAF scores for the total group of patients with longitudinal GAF data and RCI with regard to the GAF.
Differences between those who improved and those who remained unchanged on PTSD symptom severity were compared by means of chi-square or independent samples t-test analyses with regard to patient characteristics and treatment characteristics. Results showed that those who did not improve on PTSD were more likely to have been exposed to a trauma before the age of 12 (χ2 (1) = 6.42, p < 0.05). Those in remission differed in terms of background, age, sex and region of origin.
2.4. Changes in global functioning during treatment
Only participants with a complete pre- and post-treatment assessment on global functioning were included in the analysis (65 on the GAF). shows the results of the analysis of the GAF scores. A significant increase in GAF scores was found from pre- to post-treatment (standardized test statistic = 5.30, p < 0.001). Regarding global functioning, 20 patients improved (30.7%) and 45 (69.2%) remained unchanged. No patients deteriorated. Wilcoxon test for GAF scores resulted in a large effect size (r was 0.66). In it can be seen that those classified as recovered or improved according to the RCIs substantially improved in functioning by approximately 15 points.
Differences between those who improved and those who remained unchanged on global functioning were compared by means of chi-square or independent samples t-test analyses with regard to patient characteristics and treatment characteristics. Those who did not improve on global functioning had more sessions of NET on average (M = 9.3, SD = 5.9 vs M = 13.4, SD = 5.4), t(63) = −2.79, p < 0.01). This implies that a higher trauma load was associated with less improvement.
3. Discussion
This study provided evidence supporting the feasibility of an outpatient day treatment programme including NET, even in those patients that before failed to benefit from other treatments. Changes in symptoms and global functioning were observed. Specifically, about 30% of patients showed a reduction of PTSD symptoms (including those with full recovery). Enhanced global functioning was observed in 30% of the patients, which was associated with fewer NET sessions than those who had a stable GAF score from T1 to T2. Although, overall, a minority of the participants improved, those who actually reliably and clinically improved showed a considerable alleviation of symptoms or an improvement in global functioning.
The fact that, in this sample, 78.4% of all patients completed NET, attests to the feasibility of NET embedded in an outpatient day treatment programme. In a large study on non-response and dropout rates in PTSD treatment, it was shown that dropout rates varied considerably across studies (Schottenbauer, Glass, Arnkoff, Tendick, & Gray, Citation2008). The average dropout rate in clinical trials on PTSD was found to be 20%, although the aggregated dropout rate of active treatments of PTSD in clinical trials in a meta-analysis was slightly lower, namely 18.3% (Imel, Laska, Jakupcak, & Simpson, Citation2013). Yet, previous studies on NET have reported high treatment completion for NET in comparison to prolonged exposure (PE), with mean dropout rates of 5.1% of NET (ranging from 0 − 20%) vs 27.2% in studies on PE (ranging from 0% to 41%) (Mørkved et al., Citation2014). However, only six studies on NET included samples of refugees resettled in high-income countries, and dropout rates in these samples were on average higher than dropout rates of NET in other samples (Lely, Smid, Jongedijk, Knipscheer, & Kleber, Citation2019). The dropout rate of 20.6% in our naturalistic setting accords with previous studies, considering that the majority of our sample was diagnosed with (chronic) PTSD often classified as ‘extreme’ or ‘severe’ PTSD, and with a history of unsuccessful treatment prior to the start of the outpatient day treatment programme.
Of those who dropped out, 60% mentioned reasons related to current stressors, although no significant differences were found on the number of current stressors between completers and non-completers. As the current stressors could be addressed at consultation hours during the programme, the NET therapist was indeed able to focus on the NET, as evidenced by our finding that most therapists did not spend more than two sessions on other issues than NET. A minority of those who dropped out (40.0%) specifically felt that the confrontation with the traumatic memories was too overwhelming, and were offered non-trauma-focused treatment. Considering that none of the patients after NET showed deterioration in terms of PTSD or global functioning, the use of exposure in the majority of the sample appears to be safe.
Some differences between completers and non-completers were found. Although all participants had already lived in the Netherlands for several years, the length of stay in the Netherlands was found significantly higher in the group of completers. In a systematic review on mental health care utilisation of refugees, it was found that a longer time of resettlement was associated with more mental health care utilisation (Satinsky, Fuhr, Woodward, Sondorp, & Roberts, Citation2019). A longer time of resettlement may be related to more familiarity with mental health care so that patients will better know what to expect, and hence facilitating completion.
Completers were also more likely to have a partner, which suggests that a socially supportive living environment enhances the acceptability of trauma-focused treatment in refugees. Several studies show that perceived lack of social support is a risk factor for PTSD (Brewin, Andrews, & Valentine, Citation2000). Perceived social support is also associated with complex PTSD (Hecker, Huber, Maier, & Maercker, Citation2018; Simon, Roberts, Lewis, van Gelderen, & Bisson, Citation2019). In a sample of Iraqi refugees more social support was associated with better acculturation and less mental health complaints (LeMaster et al., Citation2018). The current programme could be modified to support the most vulnerable group, to further enhance social support which facilitates conditions in which a trauma-focussed therapy can be completed.
Although our findings are encouraging, and effect sizes are comparable to other studies on NET (Lely et al., Citation2019), the number of those reliably improved or recovered based on the RCI of PTSD symptoms and global functioning was modest. This may be explained by several factors. A first point to consider is the severity of the complaints of the patients. That is, 70% of the refugees in the study had an overall severity score in the extreme PTSD range on the CAPS before treatment. Those who did not improve on global functioning had more NET sessions on average, which implies a higher trauma load. Trauma load is also associated with a higher severity of PTSD complaints (Kolassa et al., Citation2010). Hence, expecting full recovery may not always be realistic. Indeed, in a meta-analysis of studies on the efficacy of PTSD treatment in military veterans, a high pre-treatment PTSD severity was associated with lower treatment gains (Haagen, Smid, Knipscheer, & Kleber, Citation2015). Secondly, the overall number of current stressors of the participants was high, despite several years of resettlement. The impact of current stressors on mental health has been documented in several studies (Chu et al., Citation2013; LeMaster et al., Citation2018; Minihan, Liddell, Byrow, Bryant, & Nickerson, Citation2018; Schick et al., Citation2018; Steel et al., Citation2017; Tinghög et al., Citation2017). In the study by Minihan et al. (Citation2018) on patterns and predictors of PTSD in refugees, living condition emerged as an important predictor of PTSD symptoms. In a 3 year follow up study in a clinical sample of refugees, it was found that reduction of post-migration living difficulties predicted changes over time for depression and anxiety, but not for PTSD (Schick et al., Citation2018). In our study, it is unclear in what way current stressors relate to (the severity and course of) the PTSD complaints and global functioning or vice versa. Nevertheless, the number of current stressors in our sample and severity of the complaints suggests support for the ecological model of distress in refugees which postulates that mental health of refugees is affected not only by war exposure, but also by current stressors (Miller & Rasmussen, Citation2017).
A further notable finding is that the patients who remained unchanged on PTSD were more likely to have had a first trauma before the age of 12. A relationship between childhood adversities and psychopathology later in adulthood has been found in refugees in at least one study (Opaas & Varvin, Citation2015). Nevertheless, a meta-analysis of psychological interventions in patients who have experienced childhood adversities showed good results of trauma-focused interventions (Ehring et al., Citation2014). In phase 1 of our treatment programme, we incorporate complicating factors often associated with more complex and often early trauma, such as dissociation, when discussing emotion regulation (Cloitre et al., Citation2012). However, we did not specifically address the debilitating core cognitions regarding the self, others, and the world, commonly found in relation to early traumatization. The moderate effects of NET in those with childhood trauma may be improved by a person-oriented therapeutic stance fostering basic trust and safety or applying interventions that address dysfunctional/maladaptive cognitions about self, others and the world. Notably, long-term interventions may be necessary to achieve symptom remission following childhood trauma (Young, Klosko, & Weishaar, Citation2003).
3.1. Strengths and limitations
A strength of the current study is that it was carried out in a clinical setting. The naturalistic design demonstrates how the NET protocol – and possibly other evidence-based trauma-focused treatments as well – can be successfully implemented in clinical practice and conditions can be met to complete an evidence-based treatment in a group of severely traumatized refugees.
However, there are several limitations to the current study. The naturalistic setting only allows us to draw cautious conclusions on symptom changes and moderators of treatment outcome. The number of NET sessions was based on the number of traumatic events (‘stones’) patients mentioned and was not standardized across patients. We were not able to examine the relative contribution of the different components of the outpatient day treatment programme, such as the group therapies, to changes in symptoms and global functioning. A further notable limitation is that no control group was included.
3.2. Future research
The results of our study are promising and call for further research on the efficacy of NET in severely traumatized refugees in a multimodal programme. In doing so, treatment outcome should preferably be monitored for a longer period of time. Several studies found a further decline in symptoms months after (CBT and/or pharmacotherapeutic) treatment (Böck Buhmann, Nordentoft, Ekstroem, Carlsson, & Mortensen, Citation2018). The efficacy of NET has shown to be gradual and treatment effects have been found to continue after termination of treatment (Palic & Elklit, Citation2011). Therefore, a follow-up assessment of the patients participating in the outpatient day treatment programme is needed.
In a larger sample, it would be important to examine what factors moderate treatment response and how the severity of the complaints interacts with current stressors using multi-composite moderators. The relative contribution of single moderators is found to be limited and diffuse. In several studies, different moderators were found, such as gender, age, or employment status, whereas other studies found legal status, resettlement variables or post-migration stressors related to mental health outcome or treatment response (Li, Liddell, & Nickerson, Citation2016; Sonne et al., Citation2016; Stammel et al., Citation2017; Stenmark, Catani, Neuner, Elbert, & Holen, Citation2013; Stenmark, Guzey, Elbert, & Holen, Citation2014; Whitsett & Sherman, Citation2017). Predicting treatment outcome may require multi-composite moderators (Cloitre, Petkova, Su, & Weiss, Citation2016; Smagula et al., Citation2016; Wallace, Frank, & Kraemer, Citation2013). This may be helpful in gaining insight in who will benefit from what type of intervention.
4. Conclusions
NET embedded in an outpatient day treatment programme is feasible and facilitates the chance of completion of trauma-focused therapy. The current study shows that even in those patients that have a history of unsuccessful treatment offering a trauma-focussed therapy embedded in an outpatient day treatment programme can be worthwhile. In those who improved, a substantial decline in symptoms and better functioning was observed. Our findings suggest that a socially supportive living environment enhances the acceptability of trauma-focused treatment in refugees.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., & Keane, T. M. (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8, 75–13.
- Böck Buhmann, C., Nordentoft, M., Ekstroem, M., Carlsson, J., & Mortensen, E. L. (2018). Long-term treatment effect of trauma-affected refugees with flexible cognitive behavioural therapy and antidepressants. Psychiatry Research, 264, 217–223.
- Boeschoten, M. A., Van der Aa, N., Bakker, A., Ter Heide, F. J. J., Hoofwijk, M. C., Jongedijk, R. A., … Olff, M. (2018). Development and evaluation of the Dutch clinician-administered PTSD scale for DSM-5 (CAPS-5). European Journal of Psychotraumatology, 9, 1546085.
- Bogic, M., Njoku, A., & Priebe, S. (2015). Long-term mental health of war-refugees; a systematic literature review. BMC International Health and Human Rights, 15, 29.
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766.
- Chu, T., Keller, A. S., & Rasmussen, A. (2013). Effects of post-migration factors on PTSD outcomes among immigrant survivors of political violence. Journal of Immigrant and Minority Health, 15, 890–897.
- Cloitre, M., Courtois, C. A., Ford, J. D., Green, B. L., Alexander, P., Briere, J., & Van der Hart, O. (2012). The ISTSS expert consensus treatment guidelines for complex PTSD in adults. Retrieved from https://www.istss.org/ISTSS_Main/media/Documents/ISTSS-Expert-Concesnsus-Guidelines-for-Complex-PTSD-Updated-060315.pdf
- Cloitre, M., Petkova, E., Su, Z., & Weiss, B. J. (2016). Patient characteristics as a moderator of PTSD treatment outcome: Combining symptom burden and strengths. British Journal of Psychiatry, 2, 101–106.
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). New York: Lawrence Erlbaum associates.
- De Heus, A., Hengst, S. M. C., De la Rie, S. M., Djelantik, A. A. A. M. J., Boelen, P. A., & Smid, G. E. (2017). Day patient treatment for traumatic grief: Preliminary evaluation of a one year treatment program for patients with multiple and traumatic losses. European Journal of Psychotraumatology, 8, 1375335.
- Ehring, T., Welboren, R., Morina, N., Wicherts, J. M., Freitag, J., & Emmelkamp, P. M. G. (2014). Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clinical Psychology Review, 34, 645–657.
- Fazel, M., Wheeler, J., & Danesh, J. (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. The Lancet, 365, 1309–1314.
- Haagen, J. F. G., Smid, G. E., Knipscheer, J. W., & Kleber, R. J. (2015). The efficacy of recommended treatments for veterans with PTSD: A metaregression analysis. Clinical Psychology Review, 40, 184–194.
- Hecker, T., Huber, S., Maier, T., & Maercker, A. (2018). Differential associations among PTSD and complex PTSD symptoms and traumatic experiences and postmigration difficulties in a culturally diverse refugee sample. Journal of Traumatic Stress 31, 31(6), 795–804.
- Herman, J. (2015). Trauma and recovery. Jackson, TN: Ingram Publisher Services.
- Imel, Z. E., Laska, K., Jakupcak, M., & Simpson, T. L. (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81, 394–404.
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19.
- Jones, S. H., Thornicroft, G., Coffey, M., & Dunn, G. (1995). A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). The British Journal of Psychiatry, 166, 654–659.
- Kolassa, I. T., Ertl, V., Eckhart, C., Onyut, L., Kolassa, S., & Elbert, T. (2010). Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychological Trauma: Theory,Research, Practice and Policy, 2(3), 169–174.
- Lely, J. C. G., Smid, G. E., Jongedijk, R. A., Knipscheer, W., & Kleber, R. J. (2019). The effectiveness of narrative exposure therapy: A review, meta-analysis and meta-regression analysis. European Journal of Psychotraumatology, 10, 1550344.
- LeMaster, J. W., Broadbridge, C. L., Lumley, M. A., Arnetz, J. E., Arfken, C., Fetters, M. D., … Arnetz, B. B. (2018). Acculturation and post-migration psychological symptoms among Iraqi refugees: A path analysis. American Journal of Orthopsychiatry, 88, 38–47.
- Li, S. S. Y., Liddell, B. J., & Nickerson, A. (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18, 1–9.
- Miller, K. E., & Rasmussen, A. (2017). The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiology and Psychiatric Sciences, 26, 129–138.
- Minihan, S., Liddell, B. J., Byrow, Y., Bryant, R. A., & Nickerson, A. (2018). Patterns and predictors of posttraumatic stress disorder in refugees: A latent class analysis. Journal of Affective Disorders, 232, 252–259.
- Mørkved, N., Hartmann, K., Aarsheim, L. M., Holen, D., Milde, A. M., Bomya, J., & Thorp, S. R. (2014). A comparison of narrative exposure therapy and prolonged exposure therapy for PTSD. Clinical Psychology Review, 34, 453–467.
- National Institute for Clinical Excellence [NICE]. (2005). Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care. London: NICE.
- Nickerson, A., Bryant, R. A., Silove, D., & Steel, Z. (2011). A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31, 399–417.
- Nosè, M., Ballette, F., Bighelli, I., Turrini, G., Purgato, M., Tol, W., … Barbui, C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. PLoS ONE, 12, 1–16.
- Opaas, M., & Varvin, S. (2015). Childhood adverse experiences with mental health and quality of life at treatment start for adult refugees traumatized by pre-flight experiences of war and human rights violations. The Journal of Nervous and Mental Disease, 203, 684–695.
- Palic, S., & Elklit, A. (2011). Psychosocial treatment of posttraumatic stress disorder in adult refugees: A systematic review of prospective treatment outcome studies and a critique. Journal of Affective Disorders, 131, 8–23.
- Robjant, K., & Fazel, M. (2010). The emerging evidence for narrative exposure therapy: A review. Clinical Psychology Review, 30, 1030–1039.
- Satinsky, E., Fuhr, D. C., Woodward, A., Sondorp, A., & Roberts, B. (2019). Mental health care utilisation and access among refugees and asylum seekers in Europe: A systematic review. Health Policy, 123, 851–863.
- Schauer, M., Neuner, F., & Elbert, T. (2011). Narrative Exposure Therapy (NET): A short-term intervention for traumatic stress. Cambridge: Hogrefe Publishing.
- Schick, M., Morina, N., Mistridis, P., Schnyder, U., Bryant, R. A., & Nickerson, A. (2018). Changes in post-migration living difficulties predict treatment outcome in traumatized refugees. Frontiers in Psychiatry, 9, 476–484.
- Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008). Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry: Interpersonal and Biological Processes, 71, 134–168.
- Simon, N., Roberts, N. P., Lewis, C. E., van Gelderen, M., & Bisson, J. (2019). Associations between perceived social support, posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD): Implications for treatment. European Journal of Psychotraumatology, 10, 1573129.
- Sloan, D. M., Bovin, M. J., & Schnurr, P. P. (2012). Review of group treatment for PTSD. Journal of Rehabilitation Research and Development, 49(5), 689–702.
- Smagula, S. F., Wallace, M. L., Anderson, S. J., Karp, J. F., Lenze, E. J., Mulsant, B. H., … Reynolds, C. F. (2016). Combining moderators to identify clinical profiles of patients who will, and will not, benefit from aripiprazole augmentation for treatment resistant late-life major depressive disorder. Psychiatric Research, 81, 112–118.
- Sonne, C., Carlsson, J., Bech, P., Vindbjerg, E., Mortensen, E. L., & Elklit, A. (2016). Psychosocial predictors of treatment outcome for trauma-affected refugees. European Journal of Psychotraumatology, 7, 30907.
- Stammel, N., Knaevelsrud, C., Schock, K., Waltherd, L., Wenk-Ansohn, M., & Böttche, M. (2017). Multidisciplinary treatment for traumatized refugees in a naturalistic setting: Symptom courses and predictors. European Journal of Psychotraumatology, 8(sup2), 1–13.
- Startup, M., Jackson, M. C., & Bendix, S. (2002). The concurrent validity of the Global Assessment of Functioning (GAF). British Journal of Clinical Psychology, 41, 417–422.
- Steel, J. L., Dunlavy, A. C., Harding, C. E., & Theorell, T. (2017). The psychological consequences of pre-emigration trauma and post-migration stress in refugees and immigrants from Africa. Journal of Immigrant and Minority Health, 19, 523–532.
- Steel, Z., Tien Chey, M., Silove, D., Marnane, C., Bryant, R., & Van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement. A systematic review and meta-analysis. JAMA, 5, 537–549.
- Stenmark, H., Catani, C., Neuner, F., Elbert, T., & Holen, A. (2013). Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behaviour Research and Therapy, 51(10), S. 641–647.
- Stenmark, H., Guzey, I. C., Elbert, T., & Holen, A. (2014). Gender and offender status predicting treatment success in refugees and asylum seekers with PTSD. European Journal of Psychotraumatology, 5, 20803.
- Tinghög, P., Malm, A., Arwidson, C., Sigvardsdotter, E., Lundin, A., & Saboonchi, F. (2017). Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: A population-based survey. BMJ Open, 7, e018899.
- United Nations General Assembly. (1984, December 10). Convention against torture and other cruel, inhuman or degrading treatment or punishment (Vol. 1465, pp. 85). Treaty Series. United Nations. Retrieved from https://www.refworld.org/docid/3ae6b3a94.html
- United Nations High Commissioners for Refugees [UNHCR]. (2019). Figures at a glance. Retrieved from https://www.unhcr.org/figures-at-a-glance.html
- Wallace, M. L., Frank, E., & Kraemer, H. C. (2013). A novel approach for developing and interpreting treatment moderator profiles in randomized clinical trials. JAMA Psychiatry, 70, 1241–1247.
- Weathers, F. W., Bovin, M. J., Lee, D. J., Sloan, D. M., Schnurr, P. P., Kaloupek, D. G., Keane, T.M., & Marx, B. P. (2018). The clinician-administered PTSD scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30, 383–395.
- Weathers, F. W., Keane, T. M., & Davidson, J. R. T. (2001). Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety, 13, 132–156.
- Whitsett, D., & Sherman, M. F. (2017). Do resettlement variables predict psychiatric treatment outcomes in a sample of asylum-seeking survivors of torture? International Journal of Social Psychiatry, 63, 674–685.
- Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema therapy: A practitioner’s guide. New York, NY: Guilford Press.