ABSTRACT
Background: There is evidence that mental disorders are more frequently reported among emergency services personnel due to the stressful nature of the job in combination with a high exposure to traumatic events. However, most of this research is based on occupational surveys that may lead to a contextual bias in the prevalence estimates or lack an adequate comparison group.
Objectives: To investigate mental health outcomes and associations with individual, job and trauma related characteristics among emergency services personnel compared to other workers.
Method: Participants were identified from the UK Biobank, a large study that collected a variety of genetic, physical and health data on individuals from across the UK. UK Biobank participants were aged between 40–69 years at recruitment. Those employed in the emergency services were identified based on job titles. A comparison sample of other workers was selected and matched to the gender composition of emergency services personnel.
Results: 5052 participants were included, and 842 were currently working in the emergency services. The majority were male (77.4%) and the mean age at Biobank enrolment was 52.5 years. Alcohol misuse was reported in 32.8% of emergency services personnel compared to 29.2% in non-emergency services personnel, followed by PTSD (9.2% vs 6.0%), depression (6.8% vs 5.1%) and anxiety (3.9% vs 3.6%). An increased risk of PTSD was found among emergency services personnel compared to other workers (odds ratio 1.58, 95% confidence interval 1.21–2.06), but this association was no longer significant after adjustment for exposure to traumatic events and job characteristics.
Conclusions: The substantial levels of alcohol misuse and increased risk of PTSD, possibly as a result of traumatic exposures in the line of duty in combination with job stressors such as shift work, call for continued monitoring of the health and wellbeing of emergency services personnel.
Antecedentes: Existe evidencia de que los trastornos mentales son reportados con mayor frecuencia entre el personal de servicios de emergencia debido a la naturaleza estresante del trabajo, en combinación, con una alta exposición a eventos traumáticos. Sin embargo, la mayor parte de esta línea de investigación se basa en encuestas ocupacionales que pueden conducir a un sesgo contextual en las estimaciones de prevalencia o carecer de un adecuado grupo de comparación.
Objetivos: Investigar los resultados de salud mental y las asociaciones con características individuales, laborales y relacionadas con trauma entre el personal de servicios de emergencia en comparación con otros trabajadores.
Método: Los participantes del Biobanco del Reino Unido tenían entre 40 y 69 años al momento del reclutamiento. Los empleados en los servicios de emergencia se identificaron utilizando los códigos de Clasificación Ocupacional Estándar 2000, y la frecuencia se ajustó a una muestra aleatoria de participantes, equivalentes según género, que trabajaban en otras ocupaciones.
Resultados: Se incluyeron 5052 participantes y 842 estaban en ese momento trabajando en los servicios de emergencia. La mayoría eran hombres (77,4%) y la edad media de inscripción en el Biobanco fue de 52,5 años. El abuso de alcohol se reportó en el 32.8% del personal de servicios de emergencia en comparación con el 29.2% en el personal de servicios que no eran de emergencia, seguido de TEPT (9.2% vs 6.0%), depresión (6.8% vs 5.1%) y ansiedad (3.9% vs 3.6%). Se encontró un mayor riesgo de TEPT entre el personal de servicios de emergencia en comparación con otros trabajadores (odds ratio 1.58, intervalo de confianza del 95% 1.21-2.06), pero esta asociación dejó de ser significativa después del ajuste por exposición a eventos traumáticos y características del trabajo. Los factores más fuertemente asociados con los resultados adversos de salud mental en ambos grupos de trabajadores incluyeron la exposición a eventos traumáticos.
Conclusiones: Los niveles sustanciales de abuso de alcohol y el mayor riesgo de TEPT, posiblemente como resultado de exposiciones traumáticas en cumplimiento de sus funciones, requieren un monitoreo continuo de la salud y el bienestar del personal de servicios de emergencia.
背景: 有证据表明, 由于与高度暴露于创伤事件结合的工作的紧张性质, 紧急服务人员报告心理疾病更为频繁。但是, 大多数研究基于职业调查, 这可能会导致对于患病率的估计出现背景偏差或缺乏足够的对照组。
目的: 考查紧急服务人员相较于其他工作者的心理健康结果以及与个人, 工作和创伤相关特征的关联。
方法: 招募了英国生物银行40-69岁之间的参与者。紧急服务人员采用2000年标准职业分类系统进行识别, 其频率与一个性别匹配的其他行业工作者参与者的随机样本相匹配。
结果: 5052名参与者被纳入, 842名目前正在紧急服务部门工作。多数是男性 (77.4%), 入职生物银行的平均年龄为52.5岁。32.8%的紧急服务人员报告了酒精滥用, 而非紧急服务人员则为29.2%, 其次是PTSD (9.2%比6.0%), 抑郁 (6.8%比5.1%) 和焦虑 (3.9%比3.6%) 。 与其他工作者相比, 急救人员中发现了增高的PTSD风险 (优势比为1.58, 95%置信区间为1.21-2.06), 但这一关联在调整了创伤事件暴露和工作特征之后不再显著。两组工作者中与不良心理健康结果最密切相关的因素包括暴露于创伤事件。
结论: 可能因执行任务时创伤暴露所致的大量酒精滥用和PTSD风险增高, 要求对紧急服务人员健康幸福的持续监测。
1. Introduction
Emergency services personnel, here defined as those working in the police force, fire brigade and ambulance services, are likely to be at a heightened risk of developing mental disorders as they are operating in highly stressful environments and are regularly exposed to traumatic situations during work (Benedek, Fullerton, & Ursano, Citation2007; Berger et al., Citation2012; Fraess-Phillips, Wagner, & Harris, Citation2017; Petrie et al., Citation2018; Skogstad et al., Citation2013). Differing prevalence estimates of mental disorders have been reported among emergency services personnel, also named first responders, due to variation in measures used, research setting and occupational group.
In a meta-analysis of 28 international studies, Berger and colleagues (2012) found the highest prevalence of post-traumatic stress disorder (PTSD) among ambulance personnel (16.5%; 95% CI 8.8–20.3), followed by members of the fire brigade (7.3%; 95% CI 3.6–11.0) and police force (4.7%; 95% CI 1.2–8.3) (Berger et al., Citation2012). A recent meta-analysis (2018) solely including ambulance personnel resulted in slightly lower but comparable, pooled PTSD prevalence of 11% (95% CI 7.0–14.0) (Petrie et al., Citation2018). Interestingly, studies conducted after 2000 resulted in a pooled PTSD estimate of 8% (95% CI 4.0–12.0), indicating a downward trend in levels of PTSD found among ambulance personnel (Petrie et al., Citation2018). This may be at least partly explained by changes in survey methodology over time. However, there may have been a genuine reduction in cases as a result of strategies put in place by employers and individuals to promote good mental health and encourage recognition of symptoms and take-up of mental health support. A study exploring PTSD among Australian career fire fighters indicated PTSD rates of 8% in current career fire fighters, with an approximately 2.5-fold increase in PTSD symptomatology among those who had left the fire service (18%) (Harvey et al., Citation2016). A substantially higher prevalence rate of PTSD, namely 21.6%, was found in a study among 1286 police officers from 5 different countries including the UK (Menard, Arter, & Khan, Citation2016).
PTSD has been the primary focus of mental health research among emergency services personnel, and other mental disorders including common mental disorders (e.g. depression and anxiety) and alcohol misuse have received far less attention, despite high levels of co-morbidity (Jones, Citation2017). According to two international studies, 15.0% of ambulance personnel reported symptoms of depression or anxiety and 25.0% of police officers met the criteria for problematic drinking (Menard et al., Citation2016; Petrie et al., Citation2018). High levels of alcohol misuse have also been reported among members of the fire service. For example, Meyer et al., (2012) found that 22.5% of US professional fire fighters reported problematic alcohol use in the past year (Meyer et al., Citation2012). Another US study found that about one in three fire fighters reported binge drinking in the past 30 days and this was positively associated with increased years of service (Piazza-Gardner et al., Citation2014). One of the largest studies to date aimed to determine the prevalence of depression and anxiety among 34,340 US emergency medical technicians and paramedics suggested a depression prevalence estimate of 6.8% followed by anxiety at 6.0% (Bentley, Mac Crawford, Wilkins, Fernandez, & Studnek, Citation2013).
Common risk factors found to be associated with mental disorders among emergency workers include: the exposure to the injury of others; proximity to death; feeling at risk personally; and perceived survivors’ guilt (Benedek et al., Citation2007; Skogstad et al., Citation2013). In addition, job demands such as shift work, long working hours and working a job that carries a high level of visible social responsibility may create an additional burden on one’s ability to cope with traumatic situations (Fraess-Phillips et al., Citation2017; Vargas de Barros, Saitz, Bastos, Ronzani, & Ronzani, Citation2012). Pre-service vulnerabilities such as childhood adversities have shown to be a strong predictor of poor mental health later in life in other high-risk occupations but have received less attention in the first responder population (Iversen et al., Citation2007). However, it is important to note that evidence suggests that not all emergency services personnel are negatively impacted by working under these circumstances. Support from friends, family and colleagues, good leadership, work morale and prior training can foster resilience in personnel (Fraess-Phillips et al., Citation2017; Prati & Pietrantoni, Citation2010; Regehr, Hill, & Clancy, Citation2000; Skogstad et al., Citation2013; Vargas de Barros et al., Citation2012).
Most of the estimated rates of mental disorders in emergency services personnel are derived from occupational surveys and not population studies. A systematic review done by Goodwin and colleagues (2013), suggested that when studies focus on a specific occupational group, higher prevalence estimates are found compared to estimates that select a group of workers from a population study (Goodwin et al., Citation2013). A possible explanation may be that occupational surveys are often framed in a negative way (e.g. stress). This, in combination with workers using the survey to communicate their work frustrations, may result in increased symptom reporting compared with population surveys (Goodwin et al., Citation2013). In addition, most of the research into the mental health of emergency services personnel originated from countries other than the UK and failed to include a comparison group.
To address these two gaps in research, the current study used data from the UK Biobank, a large population study, to examine mental disorders among people employed in the emergency services compared to a gender-matched sample of people working in other occupations. Further, individual, work and trauma related factors associated with mental disorders were explored. Based on the literature, our hypothesis was that emergency services personnel were more likely to meet caseness criteria for probable mental disorders, particularly PTSD, and that this would be at least partly explained by occupation-related exposure to trauma.
2. Methods
2.1. Study design and participants
The current study used readily available data the UK Biobank, a large population-based study. Baseline data for the UK Biobank was collected between 2006 and 2010: a random sample of over 9 million people were invited to take part if they were between the 40–69 years of age, were registered with the National Health Service (NHS) and lived within a 25-mile radius from one of the 23 study assessment centres. 503,325 participated in the study, reflecting a response rate of 5.5% (Allen et al., Citation2012; Sudlow et al., Citation2015).
2.2. Procedures
Eligible people were invited to a nearby assessment centre to provide baseline information, physical measures and biological samples. Information was collected via a touch-screen self-completed questionnaire followed by a computer-assisted personal interview. Further, trained staff collected participants’ anthropometric measurements such as blood pressure, height, weight and blood and urine samples were taken. Consent was requested to access participants primary and national care medical records. At baseline, only limited information was asked about participants mental health. Therefore, an online questionnaire named ‘thoughts and feelings’ was sent out to all UK Biobank participants who agreed to future contact and published in the participant domain of the Biobank website in 2016. As of July 2017, 157,366 fully completed online mental health questionnaires were received from those who agreed to be contacted via email (response rate 46%) (Davis et al., Citation2018).
2.3. Participant selection current study
For the current study, participants who reported to be in employment other than the emergency services at the time of their baseline assessment and had responded to the ‘thoughts and feelings’ questionnaire (n = 99,614) were identified. Subsequently, these other workers were matched to the gender composition of emergency services personnel and a random sample selected for this study. Non-emergency services personnel were oversampled at a ratio of 1:5 to increase the power of the study. The final sample for analyses included 842 emergency services personnel and 4210 non-emergency services personnel (total N = 5052). Based on an anticipated prevalence of PTSD of 10% in emergency services personnel and 4.4% in non-emergency services personnel, we had sufficient power to detect a difference in PTSD rates (Berger et al., Citation2012; McManus, Jenkins, & Brugha, Citation2016).
2.4. Materials
2.4.1. Employment
As part of the baseline assessment, participants were asked about their current employment status. Those who reported to be in a job at the time were asked to provide more details to enable trained interviewers to code their current job using the four-digit Standard Occupational Classification (SOC) V.2000 (ONS 2000) (Statistics OfN, Citation2000). Further, an ad hoc seven-digit SOC code was created, within each four-digit SOC code, to classify more specific job titles (de Matteis, Darnton, Fishwick, Rushton, & Cullinan, Citation2017). For the purpose of this study, the seven-digit code was used to identify emergency responders across services such as police, fire brigade and ambulance workers (including paramedics). A total of 842 participants were identified who, at the time of the baseline assessment, were employed as an emergency services worker.
Additional employment-related information was collected such as the average number of working hours per week, job duration and whether the job involved shift work.
2.4.2. Mental health outcomes
The primary mental health outcomes of interest included PTSD, alcohol, depression and anxiety. Using the 6-item PTSD Checklist (PCL-6), symptoms of PTSD were examined. A score of 14 or more was used as indicative of PTSD symptoms (Lang & Stein, Citation2005). Alcohol misuse was examined using the 10-item World Health Organization Alcohol Use Disorders Identification Test (AUDIT), with a score of 8 or more used as a cut off to indicate alcohol use disorder (Babor, Saunders, & Monteiro, Citation2001; Reinert & Allen, Citation2007). Symptoms of depression were measured with the 9-item Patient Health Questionnaire (PHQ-9) and the 7-item Generalised Anxiety Disorder (GAD-7) was used to measure symptoms of anxiety (Kroenke, Spitzer, & Williams, Citation2001; Kroenke, Spitzer, Williams, & Lowe, Citation2010; Spitzer, Kroenke, Williams, & Lowe, Citation2006). For both the PHQ-9 and GAD-7, a cut-off score of 10 or more was used to identify moderate to severe depression or anxiety (Kroenke et al., Citation2001, Citation2010; Spitzer et al., Citation2006).
2.4.3. Trauma
Three different measures were used to examine exposure to adverse events. The 5-item Childhood Trauma Screen was used to examine childhood adversity whereas exposure to adverse events during adulthood were assessed with the 5-item Adult Trauma Screen (Glaesmer et al., Citation2013; Khalifeh, Gram, Trevillion, Johnson, & Howard, Citation2015). Childhood adverse events included: felt unloved as a child; physically abused by family as a child; felt hated by family members as a child; sexually molested as a child; and nobody being around to take the child to a doctor when needed as a child. Adult adverse events included: not been in a confiding relationship as an adult; physical violence by partner or ex-partner as an adult; sexual interference by partner or ex-partner without consent as an adult; and not able to pay rent/mortgage. For both measures, a score over the threshold on any of the 5 items was identified as a screen positive (Davis et al., Citation2018). Participants were also asked whether they had been exposed to situations that are known to be triggers for trauma-related disorders including: been a victim of sexual assault or physically violent crime; been in a life-threatening accident; have witnessed sudden violent death; been diagnosed with a life-threatening; illness or been involved in combat or exposed to a war-zone (Frissa et al., Citation2016). A positive answer to any of these situations was identified as a screen positive.
2.5. Analyses
All statistical analyses were performed using the statistical package Stata (version SE 15.1). The socio-demographic, employment and trauma characteristics of the sample were described using descriptive statistics and compared between non-emergency services personnel and emergency services personnel using the Pearson’s Chi-squared test to compare proportions. Means and standard deviations were calculated for continuous variables (age in years). Supplementary analysis was conducted using logistic regression analysis to explore individual differences within the socio-demographic and employment characteristics with more than two categories of interest between non-emergency services personnel and emergency services personnel. The main analyses assessed whether there were differences in the prevalence of depression, anxiety, PTSD or alcohol misuse between non-emergency services personnel and emergency services personnel using logistic regression. A logistic regression model was used, whereby we first adjusted for demographic variables which were significantly associated with the outcome (p < 0.05), followed by employment characteristics into the second step of adjustments and finally trauma exposure in the third step. Odds ratios (OR), adjusted odds ratios (AOR) and 95% confidence intervals (95% CI) are reported. Missing data were <1% in the mental health outcomes of interest and were dropped for analyses.
2.6. Ethical approval
Ethical approval for the UK Biobank study was obtained via the North West Multi-Centre Research Ethics Committee and written informed consent was obtained from all participants. The additional ‘thoughts and feelings’ questionnaire was approved as a substantial amendment to UK Biobank by the North West – Haydock Research Ethics Committee, 11/NW/0382 – mental health questionnaire. Approval to use the UK Biobank data for this project was granted as part of application 34553.
3. Results
Most of the study sample included were male (77.4%). Emergency services personnel were significantly younger than non-emergency services personnel (). They lived in significantly less deprived areas, for example 11.9% of emergency services personnel lived in an area in the upper quintile indicating highest deprivation compared to 21.6% of non-emergency services personnel (p < 0.001). Emergency services personnel reported lower educational attainment compared to those not working in the emergency services. No significant difference was found regarding smoking status between the two groups. 79.4% of emergency services personnel had been in their job for over 10 years, as compared with only 48.1% of non-emergency services personnel (p < 0.001 for both 11–20 years and >20 years) (). Emergency services workers reported working significantly longer hours per week than their non-emergency services counterparts (p < 0.001 for each of the individual categories of 21 hours and more). For 49.6% of emergency workers working shifts was the norm; in contrast, only 7.5% of non-emergency workers’ roles involved regular shift work (p < 0.001 for both ‘sometimes’ or ‘usually/always’ shift work). Please refer to the Supplementary Material for further information on differences within the categories of interest.
Table 1. Characteristics of emergency and non-emergency services personnel.
Table 2. Employment characteristics of emergency and non-emergency services personnel.
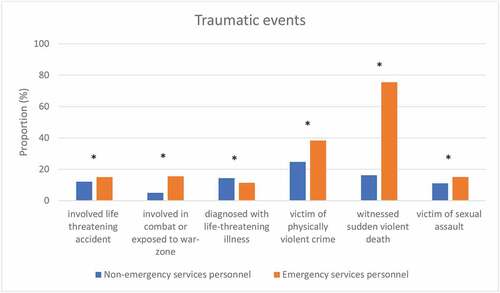
Stark differences were found in the reported rates of exposure to traumatic situations such as witnessed sudden violent death (75.5% vs 16.2%) and been a victim of a physically violent crime (38.3% vs 24.7%) among emergency services personnel compared with non-emergency services personnel (). The only event that was significantly more often reported by non-emergency services personnel was being diagnosed with a life-threatening illness (14.4% vs 11.4%). Slightly more emergency workers reported childhood adverse events such as feeling hated or physically abused by a family member (51.0% vs. 46.8%) (). Adult adverse events such as money problems or having been in an abusive relationship were reported in similar proportions in both groups of workers.
Table 3. Traumatic experiences among emergency and non-emergency services personnel.
Figure 1. Description of type of traumatic events among emergency and non-emergency services personnel.
Thirty-two-point eight percent of emergency services personnel reported symptoms of alcohol misuse and 9.2% reported symptoms indicative of PTSD (). Depression and anxiety were less common, 6.8% and 3.9%, respectively. In comparison with non-emergency services workers, emergency services workers were more likely to report symptoms of PTSD, symptoms of depression, or meet criteria for alcohol misuse. After adjustment for socio-demographic characteristics (age, deprivation, qualifications), these differences only remained significant for PTSD. None of the differences were significant after further adjustment for job characteristics (job duration, average working week hours, shift work) and trauma exposure (childhood adverse events, other traumatic events). Anxiety was reported in similar proportions in both groups of workers.
Table 4. Current mental disorders among non-emergency and emergency services personnel adjusted for socio-demographic, work and trauma characteristics.
A closer examination of the adjusted logistic regressions models suggested that for both groups of workers, the factor most consistently associated with mental disorders included traumatic exposure (data available upon request). Workers in both groups had a 1.2–2.6 greater odds of meeting criteria for mental disorders.
4. Discussion
This paper explored mental health outcomes in UK emergency services personnel and compared these to a sample of people working in other occupations. Alcohol misuse was the most prevalent condition, followed by PTSD, in both groups of workers. We found that more emergency services personnel reported symptoms of PTSD, depression and alcohol misuse compared with other workers. However, after adjustment for socio-demographic, work and trauma characteristics, none of these associations remained significant. Still, the higher rates of PTSD among emergency services personnel appear to be driven by occupational related traumatic exposures and job characteristics. Across both groups of workers, the factor most strongly associated with mental disorders included higher levels of trauma exposure.
4.1. Comparison with the literature
The overall level of PTSD at 9.2% in our sample of UK emergency services workers is comparable to the pooled PTSD estimate of 7.4% (95% CI 4.60–10.20) among first responders found in European studies (Berger et al., Citation2012), but considerably higher than the 4.4% found in the UK general population (McManus et al., Citation2016). Based on our analysis and as highlighted in previous research, we suggest that this is due to a combination of occupational stressors such as traumatic exposures, working long hours and shift work (Bara & Arber, Citation2009; Harvey et al., Citation2016; Vargas de Barros et al., Citation2012). Marked differences were found in the exposure to traumatic events, such as having witnessed a sudden violent death between emergency services workers and non-emergency services workers in our sample. Furthermore, most of our emergency services workers had been in their role for more than 10 years. The accumulation of job stress and traumatic exposure may take its toll on people’s health over time. This tendency has already been shown in a study among Australian fire fighters amongst whom there was a positive trend for increasing numbers of traumatic exposures in the line of duty to increase the risk of symptoms of PTSD, depression and excessive alcohol consumption (Harvey et al., Citation2016).
In the current study, we were unable to explore whether there were any differences in adverse mental health outcomes across the different branches of emergency services personnel. Evidence indicates that PTSD is most common in ambulance personnel, followed by fire fighters and the lowest among police officers (Skogstad et al., Citation2013). Berger and colleagues suggested that ambulance personnel are operating in an even more pressurised and stressful environment than police officers and fire fighters. This is evidenced by the fact that they respond to a far higher number of emergency calls and that during the emergency response, they often have closer contact with the victims. Another reason why police officers may have lower levels of PTSD is because they undergo a stringent selection process before joining whereas in most countries, that is not the case for ambulance services personnel and fire fighters. Future research among UK emergency services personnel should explore this further.
The frequent and prolonged exposure to shift work may add to the burden of mental ill health seen in emergency services personnel as compared with other workers. For example, results from the British Household Panel Survey found a dose-response relationship between the risk of common mental disorders, such as depression, and exposure to shift work over a longer period (Bara & Arber, Citation2009). In the UK general population about one in six adults are affected by common mental disorders (McManus et al., Citation2016). This is slightly higher than if we were to combine the prevalence rates of anxiety and depression among emergency services personnel in the current study (10.7%). A UK study conducted among 617 ambulance workers found a prevalence of depression of 10% and 22% for anxiety, again substantially higher than the current findings (Bennett, Williams, Page, Hood, & Woollard, Citation2004). The reason for differential prevalence estimates between studies is unclear, but methodological differences such as participant selection, study samples, response rates and mental health measures used may partly explain the discrepancies.
The higher rates of alcohol misuse in emergency workers compared with other workers may be partly explained by their increased risk of comorbid mental disorders. This has been commonly reported in other high-risk occupations such as military personnel (Debell et al., Citation2014). Nevertheless, in the current study, this difference was no longer significant after adjustment for socio-demographic variables. As we know that alcohol use declines with age, this may be explained by the slightly younger age composition of the emergency workers compared with other workers (McManus et al., Citation2016). To date, alcohol misuse has received less attention in the emergency responder literature (Jones, Citation2017). However, a study among police officers from five western countries found that alcohol misuse was common, with 25.0% of officers meeting criteria indicative of problematic drinking and 22.0% reporting symptoms of PTSD (Menard et al., Citation2016). We found higher levels of alcohol misuse among both samples in our study which may be at least partly explained by cultural differences in levels of alcohol consumption between the UK and other western countries (Lang & Stein, Citation2005). Most police officers included in this study were from the US and were found to have lower levels of alcohol consumption than their UK counterparts (Lang & Stein, Citation2005).
Considering our results, it is important that at an organisational level a comprehensive health and wellbeing strategy is implemented to promote mental fitness of emergency services personnel over time. Further, for those newly entering the job, adequate training should be provided to foster resilience from the start. Skogstad et al., (2013) identified various protective factors operating at an individual level (e.g. coping mechanisms and training) as well as an institutional level (e.g. support working environment, good morale) that could prevent or ameliorate mental health symptoms (Skogstad et al., Citation2013). It is important that attention is being paid to both risk and protective factors that can be modified when implementing possible mental health initiatives.
4.2. Strengths and limitations
A strength of this study was the comparison of a substantial sample of people working in the emergency services with a random sample of people working in other occupations. We were able to compare outcomes for the combined emergency services as a similar methodology and identical, validated mental health measures were used. As the data were not collected as part of an occupational health survey, it is less likely that the rates of mental ill health found are an overestimation (Goodwin et al., Citation2013). Still, caution is needed to generalise these findings, as the response rate of people participating in the UK Biobank was low and females and those who attained higher levels of education were more likely to take part (Fry et al., Citation2017). Further, people who participated in the mental health questionnaire sent after the baseline assessment also had higher educational attainment, were of higher socioeconomic status and were less likely to report a longstanding illness or disability (Davis et al., Citation2018). These factors would, however, be expected to affect both groups similarly, since both were working at the time of the baseline questionnaire, although the higher proportion of emergency workers doing shift-work may have impacted recruitment differentially. Further, it could be that the demands of emergency works requires an especially fit workforce, and the nature of the sample, comprising people in mid-life, means that we have identified only those emergency personnel who, at the time of the baseline questionnaire, had lasted relatively unscathed. Others with a history of emergency work may have had to take other forms of employment, taken early retirement or were off sick. Nevertheless, approx. 80% of the emergency workers had been in their job for over 10 years, compared to less than 50% of non-emergency workers. Still, whilst our selection of a comparison group who were in employment may have reduced such effects, we cannot rule out such selection bias (Morton, Cahill, & Hartge, Citation2006). Finally, although we used multivariable analyses to control for known confounders and potential mediators, the emergency workers were different to the comparison group in many respects, and there may be other, unmeasured, confounders which account for the differences we have observed.
4.3. Future research
Several areas of future research should be considered. First, most of the research in emergency services personnel to date has focused on PTSD, whereas our findings show that alcohol misuse is considerably more common with likely substantial long-term physical health risks as well as possible safety risks whilst undertaking their roles. Hence, research needs to be directed at alcohol misuse as well as common mental disorders (e.g. anxiety, depression). Second, it is vital to explore levels of help-seeking for mental health problems among emergency services personnel. People in other high-risk, male dominated occupations such as the military, report substantial levels of stigma, a preference for self-reliance and practical barriers to care that may hinder help-seeking for mental health problems (Haugen, McCrillis, Smid, & Nijdam, Citation2017; Jones, Keeling, Thandi, & Greenberg, Citation2015). Third, it is well-established that emergency services personnel are exposed to occupational hazards including chemicals, intense heat and operating under high pressure, and these may negatively impact on their physical health. There is evidence suggesting that fire fighters, police officers and paramedics have an increased prevalence of cardiovascular disease (Bedi & Arora, Citation2007), but UK studies are lacking. Therefore, the size and nature of physical, as well as mental, health problems should be explored in UK emergency services personnel.
4.4. Conclusions
The findings of this paper highlight the importance of considering the mental health of emergency services personnel. Efforts should be directed into the prevention of mental disorders via training, creating a supportive working environment and adequate leadership and the effectiveness of these approaches should be evaluated. Timely access to evidence-based treatment should be provided for those who are affected by mental ill health.
Author contribution
SAMS conceived the idea for this paper, developed the statistical analysis plan, conducted the data analyses and wrote the paper. DP contributed to the data cleaning and data analysis. AD and KD contributed to the data analysis and provided comments on the manuscript. KWB helped to interpret the results and commented on the manuscript. NTF and MH provided advice on the statistical analysis plan, helped to interpret the results and commented on the manuscript.
Supplemental Material
Download MS Word (23.5 KB)Disclosure statement
NTF is a specialist member of the Independent Group Advising on the Release of Data for NHS Digital (IGARD). MH is a National Institute for Health Research Senior Investigator.
Supplementary material
Supplemental data for this article can be accessed here.
Data availability
The data used in this study are from the UK Biobank. Further details on how to access this data can be found here: https://www.ukbiobank.ac.uk/
Additional information
Funding
References
- Allen, N., Sudlow, C., Downey, P., Peakman, T., Danesh, J., Elliott, P., … Collins, R. (2012). UK Biobank: Current status and what it means for epidemiology. Health Policy and Technology, 1(3), 123–11.
- Babor, T. F., Saunders, C. H.-B. J., & Monteiro, M. G. (2001). AUDIT. the alcohol use disorders identification test: Guidelines for use in primary care. Geneva: World Health Organisation.
- Bara, A.-C., & Arber, S. (2009). Working shifts and mental health–findings from the British household panel survey (1995–2005). Scandinavian Journal of Work, Environment & Health, 35(5), 361–367.
- Bedi, U. S., & Arora, R. (2007). Cardiovascular manifestations of posttraumatic stress disorder. Journal of the National Medical Association, 99(6), 642–649.
- Benedek, D. M., Fullerton, C., & Ursano, R. J. (2007). First responders: Mental health consequences of natural and human-made disasters for public health and public safety workers. Annual Review of Public Health, 28(1), 55–68.
- Bennett, P., Williams, Y., Page, N., Hood, K., & Woollard, M. (2004). Levels of mental health problems among UK emergency ambulance workers. Emergency Medicine Journal, 21(2), 235–236.
- Bentley, M. A., Mac Crawford, J., Wilkins, J. R., Fernandez, A. R., & Studnek, J. R. (2013). An assessment of depression, anxiety, and stress among nationally certified Ems professionals. Prehospital Emergency Care, 17(3), 330–338.
- Berger, W., Coutinho, E. S. F., Figueira, I., Marques-Portella, C., Luz, M. P., Neylan, T. C., & Mendlowicz, M. V. (2012). Rescuers at risk: A systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Social Psychiatry and Psychiatric Epidemiology, 47(6), 1001–1011.
- Davis, K. A. S., Coleman, J. R. I., Adams, M., Allen, N., Breen, G., Cullen, B., … Hotopf, M. (2018). Mental health in UK Biobank: Development, implementation and results from an online questionnaire completed by 157 366 participants (vol 4, pg 83, 2018). Bjpsych Open, 4(5), 352–353.
- de Matteis, S. J., Darnton, D., Fishwick, A., Rushton, D., & Cullinan, L. (2017). The occupations at increased risk of COPD in the UK Biobank Cohort. European Respiratory Journal, 50. doi:10.1183/13993003.00711-2017
- Debell, F., Fear, N. T., Head, M., Batt-Rawden, S., Greenberg, N., Wessely, S., & Goodwin, L. (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1401–1425.
- Fraess-Phillips, A., Wagner, S., & Harris, R. L. (2017). Firefighters and traumatic stress: A review. International Journal of Emergency Services, 6(1), 67–80.
- Frissa, S., Hatch, S. L., Fear, N. T., Dorrington, S., Goodwin, L., & Hotopf, M. (2016). Challenges in the retrospective assessment of trauma: Comparing a checklist approach to a single item trauma experience screening questionle. Bmc Psychiatry, 16(1). doi:10.1186/s12888-016-0720-1
- Fry, A., Littlejohns, T. J., Sudlow, C., Doherty, N., Adamska, L., Sprosen, T., & Allen, N. E. (2017). Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. American Journal of Epidemiology, 186(9), 1026–1034.
- Glaesmer, H., Schulz, A., Hauser, W., Freyberger, H. J., Brahler, E., & Grabe, H. J. (2013). The Childhood Trauma Screener (CTS) - Development and validation of cut-off-scores for classificatory diagnostics. Psychiatrische Praxis, 40(4), 220–226.
- Goodwin, L., Ben-Zion, I., Fear, N. T., Hotopf, M., Stansfeld, S. A., Wessely, S., & de Boer, A. (2013). Are reports of psychological stress higher in occupational studies? A systematic review across occupational and population based studies. Plos One, 8(11), e78693.
- Harvey, S. B., Milligan-Saville, J. S., Paterson, H. M., Harkness, E. L., Marsh, A. M., Dobson, M., & Bryant, R. A. (2016). The mental health of fire-fighters: An examination of the impact of repeated trauma exposure. Australian and New Zealand Journal of Psychiatry, 50(7), 649–658.
- Haugen, P. T., McCrillis, A. M., Smid, G. E., & Nijdam, M. J. (2017). Mental health stigma and barriers to mental health care for first responders: A systematic review and meta-analysis. Journal of Psychiatric Research, 94, 218–229.
- Iversen, A. C., Fear, N. T., Simonoff, E., Hull, L., Horn, O., Greenberg, N., … Wessely, S. (2007). Influence of childhood adversity on health among male UK military personnel. British Journal of Psychiatry, 191(6), 506–511.
- Jones, N., Keeling, M., Thandi, G., & Greenberg, N. (2015). Stigmatisation, perceived barriers to care, help seeking and the mental health of British Military personnel. Social Psychiatry and Psychiatric Epidemiology, 50(12), 1873–1883.
- Jones, S. (2017). Describing the mental health profile of first responders: A systematic review. Journal of the American Psychiatric Nurses Association, 23(3), 200–214.
- Khalifeh, H., Gram, S., Trevillion, K., Johnson, S., & Howard, L. M. (2015). Recent intimate partner violence among people with chronic mental illness: Findings from a national cross-sectional survey. British Journal of Psychiatry, 207(3), 207–212.
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
- Kroenke, K., Spitzer, R. L., Williams, J. B. W., & Lowe, B. (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry, 32(4), 345–359.
- Lang, A. J., & Stein, M. B. (2005). An abbreviated PTSD checklist for use as a screening instrument in primary care. Behaviour Research and Therapy, 43(5), 585–594.
- McManus, S. B. P., Jenkins, R., & Brugha, T. (eds). (2016). Mental health and wellbeing in England: Adult psychiatric morbidity survey 2014. Leeds: NHS Digital.
- Menard, K. S., Arter, M. L., & Khan, C. (2016). Critical incidents, alcohol and trauma problems, and service utilization among police officers from five countries. International Journal of Comparative and Applied Criminal Justice, 40(1), 25–42.
- Meyer, E. C., Zimering, R., Daly, E., Knight, J., Kamholz, B. W., & Gulliver, S. B. (2012). Predictors of posttraumatic stress disorder and other psychological symptoms in trauma-exposed firefighters. Psychological Services, 9(1), 1–15.
- Morton, L. M., Cahill, J., & Hartge, P. (2006). Reporting participation in epidemiologic studies: A survey of practice. American Journal of Epidemiology, 163(3), 197–203.
- Petrie, K., Milligan-Saville, J., Gayed, A., Deady, M., Phelps, A., Dell, L., & Harvey, S. B. (2018). Prevalence of PTSD and common mental disorders amongst ambulance personnel: A systematic review and meta-analysis. Social Psychiatry and Psychiatric Epidemiology, 53(9), 897–909.
- Piazza-Gardner, A. K., Barry, A. E., Chaney, E., Dodd, V., Weiler, R., & Delisle, A. (2014). Covariates of alcohol consumption among career firefighters. Occupational Medicine-Oxford, 64(8), 580–582.
- Prati, G., & Pietrantoni, L. (2010). The relation of perceived and received social support to mental health among first responders: A meta-analytic review. Journal of Community Psychology, 38(3), 403–417.
- Regehr, C., Hill, J., & Clancy, G. D. (2000). Individual predictors of traumatic reactions in firefighters. Journal of Nervous and Mental Disease, 188(6), 333–339.
- Reinert, D. F., & Allen, J. P. (2007). The alcohol use disorders identification test: An update of research findings. Alcoholism-Clinical and Experimental Research, 31(2), 185–199.
- Skogstad, M., Skorstad, M., Lie, A., Conradi, H. S., Heir, T., & Weisaeth, L. (2013). Work-related post-traumatic stress disorder. Occupational Medicine-Oxford, 63(3), 175–182.
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
- Statistics OfN. (2000). SOC: Archive. Office for National Statistics. Retrieved from: https://www.ons.gov.uk/methodology/classificationsandstandards/standardoccupationalclassificationsoc/socarchive
- Sudlow, C., Gallacher, J., Allen, N., Beral, V., Burton, P., Danesh, J., … Collins, R. (2015). UK Biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Medicine, 12(3), e1001779.
- Vargas de Barros, V. M., Saitz, L. F., Bastos, R., Ronzani, R. R., & Ronzani, T. M. (2012). Mental health conditions, individual and job characteristics and sleep disturbances among firefighters. Journal of Health Psychology, 18(3), 350–358.
