 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background: Physical health concerns (e.g. chronic pain, fatigue) are common among clients with posttraumatic stress disorder (PTSD). Prior research has indicated that clients report improved physical functioning and fewer physical health symptoms after receiving Cognitive Processing Therapy (CPT) for PTSD. However, less is known about the impact of physical functioning on the clients’ PTSD symptom improvement in CPT.
Objective: The current study examined the patterns of change of and between physical functioning and PTSD symptoms over the course of CPT among a diverse military, veteran, and community sample.
Method: We collected clients’ (N = 188) physical functioning and PTSD symptom severity prior to and during CPT using the 12-Item Short Form Health Survey and the PTSD Checklist. We used multilevel modelling to 1) evaluate the impact of baseline physical functioning on the PTSD symptom trajectory, 2) examine the trajectory of physical functioning, and 3) assess the dynamics between physical functioning and PTSD symptoms over the course of CPT.
Results: Our multilevel analyses indicated that 1) physical functioning significantly improved for those with low levels of functioning prior to treatment, 2) poorer baseline physical functioning predicted slower improvements in PTSD symptoms, and 3) poorer physical functioning in one session predicted less PTSD symptom improvement by the next session.
Conclusions: Our findings demonstrate that while physical functioning can interfere with PTSD symptom improvement, physical functioning can also improve over the course of CPT. In light of the interconnected nature of physical health and PTSD symptoms, clinicians may need to attend to lower levels of physical functioning when providing CPT or other trauma-focused therapies. Future research to determine whether specific treatment adaptations may benefit such clients is needed.
Antecedentes: Los problemas de salud física (ej. dolor crónico, fatiga) son comunes entre los clientes con trastorno de estrés postraumático (TEPT). La investigación previa ha indicado que los clientes reportan una mejoría en el funcionamiento físico y menos síntomas de salud física después de recibir Terapia de Procesamiento Cognitivo (CPT, por su sigla en inglés) para TEPT. Sin embargo, se sabe menos sobre el impacto del funcionamiento físico sobre la mejoría de los síntomas de TEPT de los clientes en la CPT.
Objetivo: El presente estudio examinó los patrones de cambio del funcionamiento físico y los síntomas de TEPT, por separado y entre sí, en el curso de la CPT en una muestra diversa de militares, veteranos y personas de la comunidad.
Método: Recolectamos el funcionamiento físico y la severidad de los síntomas de TEPT de los clientes (N=188) antes y durante la CPT, utilizando el Cuestionario Corto de Salud de 12 items y la Lista de chequeo de TEPT. Utilizamos un modelo multinivel para 1) evaluar el impacto del funcionamiento físico basal sobre la trayectoria de los síntomas de TEPT, 2) examinar la trayectoria del funcionamiento físico, y 3) evaluar la dinámica entre el funcionamiento físico y los síntomas de TEPT en el curso de la CPT.
Resultados: Nuestros análisis multinivel indicaron que 1) el funcionamiento físico mejoró en forma significativa en quienes tenían bajos niveles de funcionamiento antes del tratamiento, 2) un peor funcionamiento físico basal predijo una mejoría más lenta de los síntomas de TEPT, y 3) un peor funcionamiento físico en una sesión predijo una menor mejoría sintomática en la siguiente sesión.
Conclusiones: Nuestros hallazgos demuestran que mientras que el funcionamiento físico puede interferir con la mejoría de los síntomas de TEPT, el mismo también puede mejorar en el curso de la CPT. A la luz de la naturaleza interconectada de la salud física y los
síntomas de TEPT, los clínicos pueden necesitar poner atención a niveles más bajos de funcionamiento físico cuando proveen CPT u otras terapias centradas en el trauma. Se requiere futura investigación para determinar si estos clientes se pueden beneficiar de adaptaciones de tratamiento específicas.
背景: 躯体健康问题 (如慢性疼痛, 疲劳) 在创伤后应激障碍 (PTSD) 患者中很常见。先前研究表明, 在接受 PTSD 认知加工疗法 (CPT) 后, 患者报告了身体功能提高和躯体健康症状减少。但是, 对于 CPT 中生理机能对患者 PTSD 症状改善的影响知之甚少。
目的: 当前研究在不同军人, 退伍老兵和社区样本中考查了 CPT 过程中生理机能和PTSD症状之间的变化模式。
方法: 在进行 CPT 之前和期间, 我们使用12条目健康调查简表和 PTSD 检查表收集了118名患者的生理机能和 PTSD 症状严重程度。我们使用多水平模型来:1) 评估基线生理机能对 PTSD 症状轨迹的影响,2) 考查生理机能的轨迹, 以及3) 评估 CPT 过程中生理机能与 PTSD 症状之间的动态过程。
结果: 我们的多水平分析表明,1) 治疗前功能水平较低者的生理机能显著提高; 2) 较差的基线生理机能预测PTSD症状更缓慢的改善; 3) 一个疗程中较差的生理机能预测下一个疗程中 PTSD 症状更少的改善。
结论: 我们的发现表明, 尽管生理机能会干扰 PTSD 症状的改善, 生理机能也可以随 CPT 进程得到改善。考虑到躯体健康和 PTSD 症状的相互联系, 临床医生在提供 CPT 或其他聚焦创伤疗法时可能需要注意较低水平的生理机能。需要未来研究去确定特定治疗方案是否可以使此类患者受益。
Individuals with a history of trauma often experience physical health concerns alongside the psychological effects of trauma. Although posttraumatic stress disorder (PTSD) is a widely studied psychological sequelae of trauma, research indicates that exposure to trauma is also related to poor physical health (e.g. Afari et al., Citation2014; López-Martínez et al., Citation2018; Pacella, Hruska, & Delahanty, Citation2013; Schnurr, Citation2017). Types of physical health concerns often associated with trauma exposure include: chronic pain (Ang, Peloso, Woolson, Kroenke, & Doebbeling, Citation2006), fibromyalgia (Ciccone, Elliott, Chandler, Nayak, & Raphael, Citation2005), chronic fatigue syndrome (Clark, Goodwin, Stansfeld, Hotopf, & White, Citation2011), irritable bowel syndrome (Heitkemper, Cain, Burr, Jun, & Jarrett, Citation2011), and psoriasis (Boscarino, Citation2004), among others. Research indicates that PTSD may mediate the relationship between trauma exposure and physical health symptoms often experienced by trauma survivors (Campbell, Greeson, Bybee, & Raja, Citation2008; Green & Kimerling, Citation2004; Lilly & Lim, Citation2013; Schnurr & Green, Citation2004). Researchers have therefore sought to understand whether and how individuals with comorbid physical health concerns and PTSD can benefit from evidence-based psychotherapies (EBPs) for PTSD.
0.1. Evidence-based psychotherapies for PTSD
Based on the existing literature connecting physical health concerns and PTSD, few studies have examined whether clients with various health problems can experience improvements in both PTSD symptoms and physical health concerns over the course of EBPs for PTSD. Galovski, Monson, Bruce, and Resick (Citation2009) found that clients who received Cognitive Processing Therapy (CPT; Resick, Monson, & Chard, Citation2016) and Prolonged Exposure (PE; Foa, Hembree, & Rothbaum, Citation2007) reported lower health-related concerns and improvement in sleep quality, with better health outcomes for CPT. Shipherd, Clum, Suvak, and Resick (Citation2014) conducted a latent curve analysis to examine the relationship between physical health and PTSD symptoms among female participants receiving CPT. Their results indicated that the clients’ PTSD symptom improvements were associated with decreases in their concerns with physical health symptoms. Both Galovski et al. (Citation2009) and Shipherd et al. (Citation2014) measured clients’ physical health with the Pennebaker Inventory of Limbic Languidness (PILL; Pennebaker, Citation1982), which assesses the frequency of common physical symptoms and sensations such as coughing, runny nose, and headaches.
Although the PILL has been linked to physical health related-work absences (Pennebaker, Citation1982) and other measures of health complaints (e.g. The Hopkins Symptom Checklist; Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, Citation1974; Watson & Pennebaker, Citation1989), few studies have directly evaluated whether CPT can improve clients’ perceived physical functioning (i.e. belief in their ability to perform physical activities). Holliday, Williams, Bird, Mullen, and Surís (Citation2015) found a significant improvement in physical functioning with CPT using the 36-Item Short Form Survey (SF-36; Ware, Citation1993), but their sample was limited to veterans with military sexual trauma (MST)-related PTSD. Given that different index traumas can have a varying impact on clients’ physical health outcomes (Flood, McDevitt-Murphy, Weathers, Eakin, & Benson, Citation2009), it is important to examine physical functioning in other, more diverse, samples.
Although research has examined how EBPs may impact physical health, the inverse relationship (i.e. how physical functioning affects EBP outcomes) also warrants further investigation. Previous literature demonstrates that health problems may impact treatment dropout rates (Issakidis & Andrews, Citation2004; Reece, Citation2003), treatment effectiveness (Brown, Schulberg, & Prigerson, Citation2000), and clinician perception of client readiness (Cook, Dinnen, Simiola, Thompson, & Schnurr, Citation2014; Nutting et al., Citation2002). However, no research to date has explored whether physical functioning may alter the trajectory of PTSD symptomatology during the course of receiving an EBP for PTSD.
0.2. Current study
The current study aims to add to the growing literature on physical health and PTSD by moving beyond individual physical health symptoms and examining the dynamics between physical functioning and PTSD in CPT. The first aim of this study was to examine changes in physical functioning over the course of CPT in a diverse community sample. We hypothesized that clients’ physical functioning would significantly improve over the course of CPT (hypothesis 1). We also examined the association between baseline physical functioning and PTSD symptom change over the course of treatment. We hypothesized that individuals with poorer physical functioning would experience a decreased rate of PTSD symptom change during treatment (hypothesis 2). Finally, we sought to examine a potential reciprocal relationship between physical functioning and PTSD symptom change over the course of treatment. We hypothesized that poorer physical functioning would interfere with session-to-session PTSD symptom change, and that PTSD symptoms in a given session would be associated with physical functioning in the next session (hypothesis 3).
1. Method
The parent study (see Monson et al., Citation2018) was a randomized controlled trial of different CPT training and consultation strategies that enrolled individuals with PTSD who received CPT from participating clinicians in routine care treatment settings. The study procedures were approved by the university Research Ethics Board (REB) and 11 other REBs from participating sites across Canada.
1.1. Participants
Clients eligible for the study were diagnosed with PTSD by their clinicians according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association [APA], Citation2000) criteria, and scored 50 or higher on the Posttraumatic Stress Disorder Checklist – Fourth Edition (PCL-IV; Weathers, Litz, Herman, Huska, & Keane, Citation1993). Clients (N = 188) consented to participate in CPT and have their therapy sessions audio recorded and their outcome measures collected throughout the protocol. Clients with any of the following characteristics were ineligible to participate: uncontrolled psychosis or bipolar disorder, substance dependence, cognitive impairment, and imminent suicidality or homicidality. The average age of client participants was 39.39 years (SD = 11.27). Forty-eight percent of clients were male, 88% white, and 42% active duty military or veterans, and 58% civilians. Please see Monson et al., Citation2018 for more detailed information about the sample.
1.2. Procedures
One hundred thirty-four clinicians from Veterans Affairs Canada Operational Stress Injury clinics, Canadian Forces mental health services, and the broader Canadian community provided CPT to a total of 188 clients. Before providing CPT, clinicians attended a 2-day standardized CPT workshop. Clinicians were then randomized into one of three post-workshop support strategies: 1) standard expert-led group consultation without review of session audio (Standard Consultation); 2) expert-led group consultation including review of session audio (Consultation Including Audio Review); or 3) No Consultation. As part of the study, clinicians collected session recordings and self-reported outcome measures to examine symptoms from consenting clients at each session.
1.3. Measures
1.3.1. Posttraumatic stress disorder checklist (PCL-IV; Weathers et al., Citation1993)
At baseline and the beginning of each therapy session, clients completed the PCL-IV, a well-validated 17-item self-report questionnaire with strong psychometric properties (Wilkins, Lang, & Norman, Citation2011). Each item assesses severity of the DSM-IV criteria for PTSD on a 5-point Likert scale from not at all to extremely. The PCL-IV exhibited high internal consistency in the current study (α =.94).
1.3.2. 12-Item Short Form Health Survey (SF-12; Ware, Kosinski, & Keller, Citation1996)
At baseline and every other session, clients completed the SF-12. The SF-12 is the abbreviated version of the SF-36 (Ware, Citation1993), which has demonstrated strong psychometric and clinical validity in measuring physical and mental health constructs (McHorney, Ware, & Raczek, Citation1993). To measure client’s functioning, we followed the recommended scoring procedures (Ware, Keller, & Kosinski, Citation1998) for the SF-12 Physical Component Summary (SF-12 PCS).
1.4. Analytic plan
We conducted our statistical analyses in R (R Core Team, Citation2018) to test the relationship between clients’ physical functioning and PTSD symptoms in CPT. For multilevel modelling, we used the lme4 (Bates, Maechler, Bolker, & Walker, Citation2015) and lmerTest (Kuznetsova, Brockhoff, & Christensen, Citation2017) packages.
1.4.1. Aim 1: physical functioning improvement in CPT
We examined changes in physical functioning in a multilevel model with SF-12 PCS measures from every other session. Given that not every client joined the study with poor physical functioning (i.e. not much room for improvement), we accounted for the interaction between the clients’ baseline levels of physical functioning and their rates of change (Kenny, Citation1975; Kraemer, Wilson, Fairburn, & Agras, Citation2002). We first calculated SF-12 PCS change scores from the clients’ baseline and examined the distribution of variance of the change scores in an unconditional model. Our only fixed effect in the unconditional model was the intercept, and our three levels of nesting were within-clients (Level-1), between-clients (Level-2), and between-clinicians (Level-3). We compared the fit indices of the linear and linear plus quadratic time variables to determine the more appropriate way to model the trajectory. We created the linear time variable for each session by counting the number of days past each client’s baseline assessment date. For the quadratic time variable, we squared the linear time variable. In our final model, our dependent variable was the SF-12 PCS change score, and our fixed effects were the baseline SF-12 PCS score, the better fitting time variable, and their interaction.
1.4.2. Aim 2: baseline physical functioning on overall PTSD symptom reduction
To examine whether baseline physical functioning affects the trajectory of PTSD symptom change in CPT, we conducted a multilevel moderator analysis. We first evaluated an unconditional model where we only included the intercept as a fixed effect and examined the distribution of variance of PCL-IV scores across the three levels of nesting: within-clients (Level-1), between-clients (Level-2), and between-clinicians (Level-3). Next, in our unconditional growth model, we confirmed the trajectory of PTSD symptoms reported in the parent study (linear plus quadratic; Monson et al., Citation2018). We added the clients’ baseline SF-12 PCS score as a moderator of the PTSD symptom trajectory to evaluate the impact of clients’ baseline levels of physical functioning on their PTSD symptom improvement with CPT.
1.4.3. Aim 3: session-to-session change in physical functioning and PTSD symptoms
To test our hypothesis on the effects of a client’s physical functioning in one session on PTSD symptom change by next session, we conducted multilevel cross-lagged analyses using the same significant nesting levels and symptom trajectory found in Aim 2. Our dependent variable was the PCL-IV score in a particular session, and our predictor of interest was the previous session’s SF-12 PCS score (cross-lagged). We controlled for the previous session’s PCL-IV score (auto-correlated), and to account for the trajectory of PTSD symptoms during CPT, we also included the time covariates.
In addition to our hypothesized effects of physical functioning on PTSD, we tested for the reverse relationship. We first examined the distribution of the variance of SF-12 PCS scores in an unconditional model and determined the better fitting trajectory in an unconditional growth model. In our cross-lagged analysis, the dependent variable was the SF-12 PCS score from a particular CPT session, and our predictor of interest was the cross-lagged PCL-IV score. We controlled for the auto-correlated SF-12 PCS score and the time covariates.
We also estimated the effect sizes of our fixed effects with partial regression coefficients (small = .10, medium = .24, large = .37; Kirk, Citation1996).
2. Results
Clients’ PCL-IV and SF-12 PCS scores from baseline to Session 12 are presented in . Self-reported levels of physical functioning in the sample were moderately low with high variability at baseline and throughout the course of CPT.
Table 1. Descriptive statistics for number of days since baseline, PCL-IV, and SF-12 PCS.
2.1. Physical functioning improvement in CPT
According to our unconditional model for the repeated SF-12 PCS change scores, 54% of the variance was explained by the repeated assessments within clients (Level-1), and 44% was explained by between-clients (Level-2; p < .001). Only 2% of the variance was attributed to between-clinicians (Level-3; p = 1.00). Our unconditional growth models for SF-12 PCS change scores indicated that there was no significant difference in the model fit indices between the linear and linear plus quadratic time variables (ΔDEV = 1.40, ΔParms = 1, p = .24). Thus, we conducted analyses with the linear only time variable.
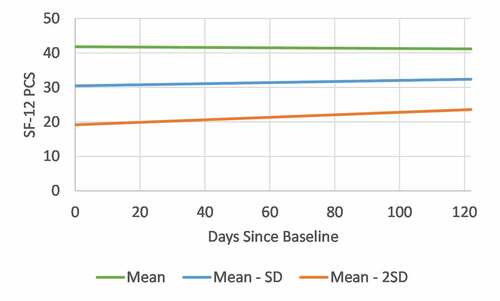
The fixed effect of the linear time variable indicated that SF-12 PCS improved over time in CPT, b = .07, t(667) = 5.56, p < .001, pr = .21, but individuals with high baseline levels experienced a lower rate of change, b = −.002, t(669) = −6.35, p < .001, pr = −.23 (see and ). The effect size of the time variable was small to medium.
Table 2. Fixed effect estimates of the multilevel physical functioning change score analysis.
Figure 1. Predicted trajectory of clients’ physical functioning over the course of CPT. Clients who entered the treatment with low levels of physical functioning reported a significant improvement in their perceived physical functioning. SF-12 PCS = Short Form Physical Health Survey Physical Component Summary, SD = standard deviation, CPT = cognitive processing therapy.
2.2. Baseline physical functioning on overall PTSD symptom reduction
In our unconditional model, 37% of the variance for the PCL-IV scores was attributed to the repeated assessments, within-clients (Level-1), and 62% to between-clients (Level-2; p < .001). However, between-clinicians (Level-3; p = .89) only represented 1% of the variance and was not a significant nesting level. Our unconditional growth model confirmed the combination of linear and quadratic patterns of change over time to be the better fitting trajectory of PTSD symptoms (ΔDEV = 44.15, ΔParms = 1, p < .001). Thus, in our hypothesized multilevel cross-lagged analyses, we included the two nesting levels (within-clients and between-clients) as random effects and both the linear and quadratic time variables as covariates.
Our multilevel moderator analysis indicated that baseline SF-12 PCS was a significant moderator of PCL-IV trajectories, with poorer baseline physical functioning predicting smaller PTSD symptom improvements, b = −0.002, t(1217) = −2.25, p = .02, pr = −.06 (see ). The effect size of the interaction term was small.
Table 3. Fixed effect estimates of the multilevel moderator analysis on the interaction between clients’ baseline physical health and PTSD symptom trajectory.
2.3. Session-to-session change
2.3.1. PTSD symptoms on physical functioning
When controlling for the auto-correlated PCL-IV scores and the symptom trajectory of PTSD, the cross-lagged SF-12 PCS scores predicted the next PCL-IV score, b = −0.10, t(140) = −3.46, p < .001, pr = −.28 (see ), such that poorer physical functioning in a session predicted a decreased PTSD symptom change. The effect size of the cross-lagged SF-12 PCS score was medium.
Table 4. Fixed-effect estimates for the hypothesized and exploratory multilevel lagged analyses.
2.3.2. Physical functioning on PTSD symptoms
According to our unconditional model for the repeated SF-12 PCS scores, 21% of the variance was explained by the repeated assessments, within-clients (Level-1), and the remaining 79% by between-clients (Level-2; p < .001). No variance was attributed to between-clinicians (Level-3; p = 1.00). There was no significant difference in the model fit indices between the linear and linear plus quadratic time variables (ΔDEV = .08, ΔParms = 1, p = .78), and thus we included only the linear time variable.
When controlling for the auto-correlated SF-12 PCS score and the trajectory of physical functioning, the cross-lagged PCL-IV score did not predict the next SF-12 PCS score, b = −0.04, t(125) = −1.02, p = .31, pr = −.09. The effect size of the PCL-IV score was small.
3. Discussion
The current study examined the relationship between clients’ physical functioning and PTSD symptoms over the course of CPT, an EBP for PTSD. Previous studies have established the impact of PTSD treatment on clients’ physical health symptoms. However, very few studies have thoroughly evaluated how physical functioning might change over the course of CPT, and how physical functioning might affect PTSD symptom change in psychotherapy. The current study sought to expand on prior research by examining 1) whether clients’ physical functioning improves with CPT in a sample of individuals who received treatment in military, veteran, and community settings, 2) whether clients’ baseline levels of physical functioning affect their PTSD treatment outcomes, and 3) how physical functioning and PTSD symptoms influence one another on a session-to-session basis.
Results from the first aim of the study supported previous findings on clients’ physical health improvement with CPT. We found that clients’ levels of physical functioning significantly increased over the course of CPT if they entered the treatment with low levels of physical health functioning. Those with average or high baseline levels of physical functioning showed less improvement but also did not have much room to improve from the beginning. Consistent with previous findings (Galovski et al., Citation2009; Holliday et al., Citation2015), the current study demonstrates that clients with PTSD can experience benefits beyond PTSD symptom change over the course of treatment, as CPT can also result in improved physical functioning.
However, results from our multilevel moderator analysis indicated that clients who reported poorer physical functioning at the beginning of treatment experienced a slower rate of PTSD symptom improvement. Similarly, in our cross-lagged analyses, clients who reported poorer physical functioning in a given session experienced a decreased PTSD symptom change by next session, whereas in the reverse direction, clients’ PTSD symptom severity in one session did not predict physical functioning improvement by next session. Clients who are in a good state of physical functioning might feel more ready to engage in psychotherapy than those with low levels of physical functioning. Pain and other physical concerns can impede the cognitive functioning necessary for engaging in trauma-focused treatment and challenging maladaptive beliefs (Moriarty & Finn, Citation2014). Poor physical functioning may also interfere with homework compliance (Branch, Citation2012), which has been linked to improved treatment outcome in CPT (Stirman et al., Citation2018).
Although clients’ physical functioning improved over the course of CPT, our null finding on the impact of PTSD symptoms on session-to-session change in physical functioning suggests that this improvement was not driven by changes in PTSD symptoms. One possible explanation is that CPT helps a client develop a more positive perception of their physical functioning, especially if a client learns to challenge their maladaptive beliefs related to limitations in physical functioning. Additionally, CPT specifically targets avoidance of activities and situations that remind individuals of the trauma, which may lead to improved functioning. Another explanation is that changes in depressive symptoms, rather than PTSD symptoms, mediate the clients’ improvement in physical functioning, given that CPT has shown to treat comorbid depressive and PTSD symptoms (Liverant, Suvak, Pineles, & Resick, Citation2012).
The interaction between physical functioning and PTSD symptoms in CPT has important implications. First, clients’ perception of pain and their physical functioning may improve after participation in CPT. Decreased levels of physical functioning are common among individuals with PTSD, and this added benefit to treatment is important and may further motivate clients to engage in trauma-focused therapy. As clients challenge their maladaptive beliefs about themselves and the world and reduce their level of avoidance, they may also change some of their perceptions of their physical functioning, or they may learn to not avoid certain activities. Second, clients who exhibit poor physical functioning prior to CPT may need to stay in treatment longer to experience optimal benefits from the treatment due to the slower trajectory of change. Additional sessions could compensate for decreased rates of PTSD symptom change associated with low baseline levels of physical functioning. Third, when clients disclose issues related to physical functioning between sessions, clinicians need to attend to the impact those issues may have on clients’ PTSD symptom improvement. Clinicians may find it beneficial to problem solve any physical functioning related barriers to treatment engagement in and between sessions and work with clients to examine maladaptive beliefs and patterns of behaviour that may be associated with their physical functioning. PTSD interventions that integrate attention to physical concerns such as pain may also be appropriate in some cases (Otis, Keane, Kerns, Monson, & Scioli, Citation2009).
The current study presents novel findings on the dynamic relationship between physical functioning and PTSD symptoms over the course of CPT. However, there are important limitations to acknowledge. First, SF-12 measures an individual’s perception of their physical functioning. The conclusions drawn in this study are limited to the effect of perceived, thus subjective, physical functioning on PTSD symptoms. This limitation warrants further investigation and exploration of whether objective measures of physical health or functioning are associated with PTSD symptom change over the course of treatment. Second, we only assessed SF-12 every other session, limiting the amount of session-level data available. Although multilevel lagged analysis was still appropriate due to the weekly assessment of PCL-IV, it might be important to replicate the current study with a sample that reports physical functioning weekly. Finally, while the sample was diverse in terms of gender and military or veteran status, the lack of ethnic and racial diversity limits our study’s generalizability to a wider range of individuals. Future research should explore the effects of physical functioning on PTSD among a more diverse sample, as race and culture play a role in health-related perceptions, behaviours, and pain (Cykert, Joines, Kissling, & Hansen, Citation1999). Future research should investigate how these sample characteristics affect the relationship between physical functioning and PTSD symptoms over the course of an EBP.
Throughout the course of CPT, individuals with poorer physical functioning experienced decreased overall and session-to-session change in PTSD symptoms. However, it is important to note that clients with lower levels of physical functioning prior to treatment still experienced improvements in their perceived physical functioning and PTSD over the course of CPT. These findings indicate that clinicians should be cognizant of their client’s physical functioning at the beginning of treatment and at each session, but that they should not necessarily allow physical functioning concerns to delay treatment. Future research might explore how clinicians should address physical health concerns in EBPs for PTSD to better improve PTSD symptoms, particularly when they are providing the treatment in medical centres such as those in the VA Healthcare System. Nevertheless, the findings from the current study provide a strong foundation for clinicians and researchers to further understand the interconnectedness of physical health and PTSD.
Disclosure statement
Dr. Monson receives royalties for a published book describing Cognitive Processing Therapy. The other authors claim no possible financial or other conflicts of interests.
Additional information
Funding
References
- Afari, N., Ahumada, S. M., Wright, L. J., Mostoufi, S., Golnari, G., Reis, V., & Cuneo, J. G. (2014). Psychological trauma and functional somatic syndromes: A systematic review and meta-analysis. Psychosomatic Medicine, 76, 2–9.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
- Ang, D. C., Peloso, P. M., Woolson, R. F., Kroenke, K., & Doebbeling, B. N. (2006). Predictors of incident chronic widespread pain among veterans following the first Gulf War. The Clinical Journal of Pain, 22(6), 554–563.
- Bates, D., Maechler, M., Bolker, B., & Walker, S. (2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48.
- Boscarino, J. A. (2004). Posttraumatic stress disorder and physical illness: Results from clinical and epidemiologic studies. Annals of the New York Academy of Sciences, 1032(1), 141–153.
- Branch, R. (2012). Challenges with homework in CBT. In W. Dryden & R. Branch (Eds.), The CBT handbook (pp. 251–269). London, UK: Sage.
- Brown, C., Schulberg, H. C., & Prigerson, H. G. (2000). Factors associated with symptomatic improvement and recovery from major depression in primary care patients. General Hospital Psychiatry, 22, 242–250.
- Campbell, R., Greeson, M. R., Bybee, D., & Raja, S. (2008). The co-occurrence of childhood sexual abuse, adult sexual assault, intimate partner violence, and sexual harassment: A mediational model of posttraumatic stress disorder and physical health outcomes. Journal of Consulting and Clinical Psychology, 76(2), 194–207.
- Ciccone, D. S., Elliott, D. K., Chandler, H. K., Nayak, S., & Raphael, K. G. (2005). Sexual and physical abuse in women with fibromyalgia syndrome: A test of the trauma hypothesis. The Clinical Journal of Pain, 21(5), 378–386.
- Clark, C., Goodwin, L., Stansfeld, S. A., Hotopf, M., & White, P. D. (2011). Premorbid risk markers for chronic fatigue syndrome in the 1958 British birth cohort. The British Journal of Psychiatry, 199(4), 323–329.
- Cook, J. M., Dinnen, S., Simiola, V., Thompson, R., & Schnurr, P. P. (2014). VA residential provider perceptions of dissuading factors to the use of two evidence-based PTSD treatments. Professional Psychology, Research and Practice, 45(2), 136–142.
- Cykert, S., Joines, J. D., Kissling, G., & Hansen, C. J. (1999). Racial differences in patients’ perceptions of debilitated health states. Journal of General Internal Medicine, 14(4), 217–222.
- Derogatis, L. R., Lipman, R. S., Rickels, K., Uhlenhuth, E. H., & Covi, L. (1974). The Hopkins Symptom Checklist (HSCL): A self‐report symptom inventory. Behavioral Science, 19(1), 1–15.
- Flood, A. M., McDevitt-Murphy, M. E., Weathers, F. W., Eakin, D. E., & Benson, T. A. (2009). Substance use behaviors as a mediator between posttraumatic stress disorder and physical health in trauma-exposed college students. Journal of Behavioral Medicine, 32, 234–243.
- Foa, E., Hembree, E., & Rothbaum, B. O. (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide. New York: Oxford University Press.
- Galovski, T. E., Monson, C., Bruce, S. E., & Resick, P. A. (2009). Does cognitive–behavioral therapy for PTSD improve perceived health and sleep impairment? Journal of Traumatic Stress, 22(3), 197–204.
- Green, B. L., & Kimerling, R. (2004). Trauma, posttraumatic stress disorder, and health status. In P. P. Schnurr & B. L. Green (Eds.), Trauma and health: Physical health consequences of exposure to extreme stress (pp. 13–42). Washington, DC: American Psychological Association. doi:10.1037/10723-002
- Heitkemper, M. M., Cain, K. C., Burr, R. L., Jun, S. E., & Jarrett, M. E. (2011). Is childhood abuse or neglect associated with symptom reports and physiological measures in women with irritable bowel syndrome? Biological Research for Nursing, 13, 399–408.
- Holliday, R., Williams, R., Bird, J., Mullen, K., & Surís, A. (2015). The role of cognitive processing therapy in improving psychosocial functioning, health, and quality of life in veterans with military sexual trauma-related posttraumatic stress disorder. Psychological Services, 12(4), 428–434.
- Issakidis, C., & Andrews, G. (2004). Pretreatment attrition and dropout in an outpatient clinic for anxiety disorders. Acta psychiatrica Scandinavica, 109(6), 426–433.
- Kenny, D. A. (1975). A quasi-experimental approach to assessing treatment effects in the nonequivalent control group design. Psychological Bulletin, 82, 345–362.
- Kirk, R. E. (1996). Practical significance: A concept whose time has come. Educational and Psychological Measurement, 56(5), 746–759.
- Kraemer, H. C., Wilson, G. T., Fairburn, C. G., & Agras, W. S. (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59(10), 877–883.
- Kuznetsova, A., Brockhoff, P., & Christensen, R. (2017). lmerTest package: Tests in linear mixed effects models. Journal of Statistical Software, 82(13), 1–26.
- Lilly, M. M., & Lim, B. H. (2013). Shared pathogeneses of posttrauma pathologies: Attachment, emotion regulation, and cognitions. Journal of Clinical Psychology, 69(7), 737–748.
- Liverant, G. I., Suvak, M. K., Pineles, S. L., & Resick, P. A. (2012). Changes in posttraumatic stress disorder and depressive symptoms during cognitive processing therapy: Evidence for concurrent change. Journal of Consulting and Clinical Psychology, 80(6), 957–967.
- López-Martínez, A. E., Serrano-Ibáñez, E. R., Ruiz-Párraga, G. T., Gómez-Pérez, L., Ramírez-Maestre, C., & Esteve, R. (2018). Physical health consequences of interpersonal trauma: A systematic review of the role of psychological variables. Trauma, Violence & Abuse, 19(3), 305–322.
- McHorney, C. A., Ware, J. E., & Raczek, A. E. (1993). The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31(3), 247–263.
- Monson, C. M., Shields, N., Suvak, M. K., Lane, J. E. M., Shnaider, P., Landy, M. S. H., … Stirman, S. W. (2018). A randomized controlled effectiveness trial of training strategies in cognitive processing therapy for posttraumatic stress disorder: Impact on patient outcomes. Behaviour Research and Therapy, 110, 31–40.
- Moriarty, O., & Finn, D. P. (2014). Cognition and pain. Current Opinion in Supportive and Palliative Care, 8(2), 130–136.
- Nutting, P. A., Rost, K., Dickinson, M., Werner, J. J., Dickinson, P., Smith, J. L., & Gallovic, B. (2002). Barriers to initiating depression treatment in primary care practice. Journal of General Internal Medicine, 17(2), 103–111.
- Otis, J. D., Keane, T. M., Kerns, R. D., Monson, C., & Scioli, E. (2009). The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Medicine, 10(7), 1300–1311.
- Pacella, M. L., Hruska, B., & Delahanty, D. L. (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders, 27(1), 33–46.
- Pennebaker, J. W. (1982). The psychology of physical symptoms. New York, NY: Springer.
- R Core Team. (2018). R: A language and environment for statistical computing [Computer software]. Vienna, Austria: R Foundation for Statistical Computing. Retrieved from https://www.R-project.org/
- Reece, M. (2003). HIV-related mental health care: Factors influencing dropout among low-income, HIV-positive individuals. AIDS Care, 15(5), 707–716.
- Resick, P. A., Monson, C. M., & Chard, K. M. (2016). Cognitive processing therapy for PTSD: A comprehensive manual. New York, NY: The Guilford Press.
- Schnurr, P. P. (2017). Physical health and health services utilization. In S. N. Gold (Ed.), APA handbooks in psychology. APA handbook of trauma psychology: Foundations in knowledge (pp. 349–370). Washington, DC: American Psychological Association.
- Schnurr, P. P., & Green, B. L. (2004). Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association.
- Shipherd, J. C., Clum, G., Suvak, M., & Resick, P. A. (2014). Treatment-related reductions in PTSD and changes in physical health symptoms in women. Journal of Behavioral Medicine, 37(3), 423–433.
- Stirman, S. W., Gutner, C. A., Suvak, M. K., Adler, A., Calloway, A., & Resick, P. (2018). Homework completion, patient characteristics, and symptom change in cognitive processing therapy for PTSD. Behavior Therapy, 49(5), 741–755.
- Ware, J. E. (1993). Measuring patients’ views: The optimum outcome measure. British Medical Journal, 306(6890), 1429–1430.
- Ware, J. E., Keller, S. D., & Kosinski, M. (1998). SF-12: How to score the SF-12 physical and mental health summary scales. Boston, MA: Health Institute, New England Medical Center.
- Ware, J. E., Kosinski, M., & Keller, S. D. (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
- Watson, D., & Pennebaker, J. W. (1989). Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychological Review, 96(2), 234–254.
- Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993, October). The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the meeting of the International Society for Traumatic Stress Studies, San Antonio, TX.
- Wilkins, K. C., Lang, A. J., & Norman, S. B. (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety, 28(7), 596–606.
