ABSTRACT
Background: Emergency room personnel are indirectly exposed to many traumas. Few studies have examined secondary traumatic stress in emergency room nurses and only a single study examined emergency room physicians. The extent of vicarious post-traumatic growth, i.e., the growth associated with such trauma, has also hitherto not been examined in emergency room personnel.
Objective: Our first goal was to examine secondary traumatization in both emergency room nurses and physicians. Our second goal was to examine vicarious post-traumatic growth in emergency room personnel. Finally, we also address the association (linear and curvilinear) between secondary traumatization and vicarious traumatic growth.
Methods: A questionnaire comprising demographic variables, secondary traumatic stress and vicarious post-traumatic growth was administered electronically to a sample of emergency room personnel from the Wolfson Hospital, Holon, Israel.
Results: There were no differences between nurses and physicians in overall secondary trauma or vicarious post-traumatic growth levels. For physicians, there was both a linear and a curvilinear association between secondary trauma and vicarious post-traumatic growth; for nurses, there was no overall association. Further sub-group analyses revealed that emergency room nurses with low workload, in conjunction with low work experience, did show a linear association.
Conclusion: Results indicate that while vicarious post-traumatic growth is linked to secondary traumatic stress for emergency room physicians, it is not so for nurses. Theoretical implications concerning the role of trauma symptoms in vicarious post-traumatic growth are discussed. Clinical implications are raised regarding the identification of excessive secondary traumatic stress levels and the need for interventions to both decrease stress levels, and to increase vicarious post-traumatic growth levels.
HIGHLIGHTS
• Emergency room physicians and nurses have same level of secondary trauma and vicarious post-traumatic growth. • In physicians these variables were linked; in nurses they were not. • Different sources for growth in physicians and nurses are discussed.
Antecedentes: El personal de las salas de emergencia está indirectamente expuesto a muchos traumas. Pocos estudios han examinado estrés traumático secundario en enfermeros en salas de emergencia y sólo un estudio en médicos de salas de emergencia. La envergadura del crecimiento vicario postraumático, es decir, el crecimiento asociado con tal trauma, hasta ahora tampoco ha sido estudiado en el personal de salas de emergencia.
Objetivo: Nuestro principal objetivo fue examinar la traumatización secundaria tanto en médicos como enfermeros de salas de emergencia. Nuestro segundo objetivo fue estudiar el crecimiento vicario postraumático en el personal de salas de emergencia. Finalmente, abordamos también la asociación (lineal y curvilínea) entre traumatización secundaria y crecimiento vicario postraumático.
Métodos: Se administró electrónicamente un cuestionario a una muestra del personal de salas de emergencia del Hospital Wolfson, Holon, Israel, abarcando variables demográficas, estrés traumático secundario y crecimiento vicario postraumático.
Resultados: No hubo diferencias en general en trauma secundario o crecimiento vicario postraumático entre enfermeros y médicos. Para los médicos, hubo una asociación tanto lineal como curvilínea entre trauma secundario y crecimiento vicario postraumático; para enfermeros, no hubo asociación en general. Análisis adicionales de subgrupos revelaron que los enfermeros de salas de emergencia con baja carga laboral, en combinación con baja experiencia laboral, mostró una asociación lineal.
Conclusiones: Los resultados indican que mientras el crecimiento vicario postraumático está asociado a trauma secundario en médicos de salas de emergencia, no ocurre así para el caso de los enfermeros. Se discuten implicaciones teóricas en relación al rol de los síntomas traumáticos en el crecimiento vicario postraumático. Surgen implicaciones clínicas que involucran la identificación de niveles excesivos de estrés traumático secundario y la necesidad de intervenciones para disminuir los niveles de estrés; y además, aumentar los niveles de crecimiento vicario postraumático.
背景: 急诊室工作人员间接暴露于许多创伤。很少有研究考查急诊室护士的二次创伤应激, 只有一项研究考查了急诊室医生。至今尚无考查急诊室人员中替代性创伤后成长的程度, 即与这种创伤相关的成长。
目的: 我们的第一个目标是考查急诊室护士和医生的二次创伤。我们的第二个目标是考查急诊室人员的创伤后替代成长情况。最后, 我们还讨论了二次创伤与替代性创伤后成长之间的关联 (线性和曲线) 。
方法: 向以色列霍隆沃尔夫森医院急诊室人员样本提供了一份包括人口统计学变量, 二次创伤应激和替代性创伤后成长情况的电子问卷。
结果: 护士和医生在总体二次创伤或替代性创伤后成长水平上没有差异。对于医生而言, 二次创伤与替代性创伤后成长之间存在线性和曲线关系。对于护士而言, 没有整体关联。进一步的亚组分析显示, 低工作量的急诊室护士加上低工作经验的确表现出线性关联。
结论: 结果表明, 尽管对急诊室医生而言, 替代性创伤后成长与二次创伤应激有关, 对护士而言并非如此。讨论了创伤症状在替代性创伤后成长中作用的相关理论意义。识别过度的二次创伤应激水平以及需要采取干预措施以降低应激水平和提高替代性创伤后, 成长水平的临床意义已经有所增长。
1. Introduction
1.1. Secondary traumatic stress
Secondary traumatic stress (STS) is defined as ‘the stress deriving from helping others who are suffering or who have been traumatized’ (Figley, Citation1999, p. 10). STS relates to behaviours and emotions, and manifests as the very same trauma symptoms that are displayed after direct exposure to trauma (Figley, Citation1995). Although STS was only formally recognized in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], Citation2013), it was extensively researched prior to that (e.g. Bride, Robinson, Yegidis, & Figley, Citation2004), and was based on the DSM-IV’s (APA, Citation1994) symptom clusters of recurrent thoughts, avoidance and arousal. STS symptoms develop after repeated indirect exposure or in cases of extreme exposure of an indirect nature (see Greinacher, Derezza-Greeven, Herzog, & Nikendei, Citation2019). As shown below, both types of exposure are common in emergency room medicine and thus, after addressing STS, the effects of such trauma on emergency room personnel are addressed.
Secondary traumatization symptoms can have a broad impact on one’s personal and professional life (see Figley, Citation1995). Such effects may include emotional depletion, insomnia and impaired interpersonal relationships (see Greinacher et al., Citation2019 for a review). Higher STS levels and their negative impact are typically evident in first responders, e.g. police officers, firefighters and ambulance workers (Setti, Lourel, & Argentero, Citation2016). Symptom levels may vary by demographic variables and by professions. For example, some studies show that variables such as sex, age, work experience and marital status are associated with STS levels (see Greinacher et al., Citation2019 for review). In addition, as reviewed by Hoffman and Shrira (Citation2017), one’s level of previous trauma symptoms following direct exposure may also impact one’s STS level, for example, experiencing trauma from directly being in a car accident during a vacation may impact one’s STS level from work related trauma.
1.1.1. STS in healthcare professions
As mentioned, STS has also been found to differ across healthcare professions, e.g. STS prevalence was 15% in social workers (Bride, Citation2007) and 19% in mental health providers treating military patients (Cieslak et al., Citation2013). Nurses from several fields displayed high STS prevalence, e.g. oncology nurses, 38% (Quinal, Harford, & Rutledge, Citation2009), intensive care nurses, 25% (Karanikola et al., Citation2015), and nurse-midwives, 35% (Beck & Gable, Citation2012). STS in physicians is relatively understudied. In a mixed sample of heart/lung transplant teams which included physicians (Carey et al., Citation2019), STS prevalence was 43%. STS prevalence was 16% in Israeli physicians treating terror victims (Weiniger et al., Citation2006) and in a more civilian context, 22% of surgeons displayed STS (Warren et al., Citation2013).
STS levels in physicians and nurses from the same departments were also compared. Taubman-Ben-Ari and Weintroub (Citation2008) sampled personnel from 3 paediatric units (Haematology-oncology, Intensive Care, and Internal Medicine) and found that nurses experienced significantly higher STS levels than paediatricians. These authors argue that nurses are closer to patients, are more intimately involved with their physical, physiological, and mental needs, and spend more time with patients – often devoting an entire shift to treating patients – while physicians meet with them for shorter periods during their daily rounds. However, Shiri, Wexler, Alkalay, Meiner, and Kreitler (Citation2008) found similar STS levels for physicians and nurses in a mixed sample (Intensive Care, Rehabilitation, and Emergency Room).
1.1.2. STS experienced by emergency room staff
Emergency room personnel typically treat patients with extreme trauma (severe injuries, road accidents, assaults, rape, abuse, and gunshots) on a repeated, even daily, basis (Dominguez-Gomez & Rutledge, Citation2009; Morrison & Joy, Citation2016). In addition to such exposure, the daily critical life-and-death decisions made in emergency rooms, often with limited time and resources, render emergency room personnel likely to experience one of the highest levels of STS in healthcare professions (see Roden-Foreman et al., Citation2017).
In most studies addressing STS in emergency room staff, nurses were typically surveyed. An Irish study found 64% of nurses from three emergency rooms (n = 117) reported STS symptoms (Duffy, Avalos, & Dowling, Citation2015). A similar study conducted in the USA (n = 67) found that 33% of the emergency room nurses suffered from STS (Dominguez-Gomez & Rutledge, Citation2009). In Scotland, a study assessing 80 emergency room nurses found that 39% suffered from secondary traumatization (Morrison & Joy, Citation2016). High STS levels are explained by increased indirect exposure to recurrent and intense trauma at work, thus emergency room nurses are likely to develop STS (Dominguez-Gomez & Rutledge, Citation2009; Morrison & Joy, Citation2016). To the best of our knowledge, only one study (Roden-Foreman et al., Citation2017) has examined emergency room physicians (across 10 hospitals in Texas, USA), revealing an STS prevalence of 12.7%. To explain the relatively lower STS rates, Roden-Foreman et al. argue that physicians have limited interaction with patients, thus they have lower levels of indirect exposure to traumatic stress than nurses do. As the studies did not compare nurses and physicians from the same emergency room, conclusions regarding such differences may be premature. Our first goal was thus to measure STS in nurses and physicians from the same emergency room.
1.2. Growth after trauma
A positive outcome of trauma exposure can be post-traumatic growth, which refers to positive psychological changes that may be observed (Tedeschi & Calhoun, Citation1995; Whealin et al., Citation2020). Post-traumatic growth neither refers to one’s pre-trauma ability to withstand a trauma nor is it conceived to stem from mere exposure to trauma; rather, it is born out of one’s struggle with trauma (Tedeschi & Calhoun, Citation1996). Growth is manifest as positive change in interpersonal relationships, greater appreciation of life, increased personal strength, greater awareness of new possibilities and spiritual growth, and has been observed in many studies following post-traumatic stress disorder stemming from direct trauma exposure (e.g. Dekel, Ein-Dor, & Solomon, Citation2012; Kleim & Ehlers, Citation2009). As reviewed below, when the exact same growth occurs in cases of secondary trauma (Arnold, Calhoun, Tedeschi, & Cann, Citation2005), it is typically termed vicarious post-traumatic growth (VPTG). To reiterate, the only difference between post-traumatic growth and VPTG is whether this growth is respectively associated with trauma symptoms stemming from direct, or indirect trauma exposure.
1.2.1. VPTG
To the best of our knowledge, VPTG was not hitherto addressed in emergency rooms. VPTG was, however, examined in other health settings and was, for example, higher in nurses than in social workers (Lev-Wiesel, Goldblatt, Eisikovits, & Admi, Citation2009; however, see Manning-Jones, de Terte, & Stephens, Citation2016). Zerach and Shalev (Citation2015) have shown that psychiatric nurses display higher VPTG levels than community nurses. Nurses in paediatric departments also showed higher VPTG than physicians did (Taubman-Ben-Ari & Weintroub, Citation2008). Similarly, Shiri et al. (Citation2008) found that nurses and psychotherapists experienced higher levels of VPTG than physicians did in a mixed sample from three departments, including the emergency room. As VPTG seems to also vary by departments and professions, and as it was not examined in the emergency room context, our second goal was to examine VPTG level in emergency room physicians and nurses.
1.3. Nature of the trauma-growth association
The associations between trauma symptoms and growth were predominantly addressed in the context of direct trauma exposure, where this was addressed as the link between post-traumatic stress disorder and post-traumatic growth (Hall, Saltzman, Canetti, & Hobfoll, Citation2015; Kleim & Ehlers, Citation2009). Theoretically, the negative impacts of trauma and PTSD can coexist simultaneously with the positive impact of PTG (e.g. Solomon & Dekel, Citation2007; Tedeschi & Calhoun, Citation2004). Yet the relationship between these concurrent (positive and negative) effects are debated. Some studies obtained a negative correlation (higher PTSD levels were linked with less growth), suggesting that trauma symptoms and growth are opposite poles of a continuum (Frazier, Conlon, & Glaser, Citation2001). Other studies claim that growth is unrelated to PTSD symptom levels (Salsman, Segerstrom, Brechting, Carlson, & Andrykowski, Citation2009); rather, as trauma and growth varied independently, growth may be driven by other factors, such as social support (see e.g. Tedeschi & Calhoun, Citation2004). However, most studies report a positive relationship (e.g. Solomon & Dekel, Citation2007; see Shakespeare-Finch & Lurie-Beck, Citation2014, for review) between PTSD and growth (the higher the PTSD level was the greater the growth levels were). Longitudinal cross-lagged studies (Dekel et al., Citation2012; Hall et al., Citation2015; Whealin et al., Citation2020) support a causal association, whereby trauma symptoms drive growth. In line with Tedeschi and Calhoun’s (Citation1996) theory, growth is built by trying to make meaning of the trauma and its aftermath. The precise nature of this causal association has been debated with two distinct options, i.e. a linear (Pargament, Smith, Koenig, & Perez, Citation1998) vs. a curvilinear (e.g. Solomon & Dekel, Citation2007) association. Butler et al. (Citation2005) noted that a linear association indicates that as trauma symptoms increase, so do growth levels, whereas a curvilinear association suggests that, initially, a higher level of traumatic distress leads to an increase in post-traumatic growth, but beyond a certain point, traumatic psychological distress is associated with a decline in post-traumatic growth (for review see Shakespeare-Finch & Lurie-Beck, Citation2014)
1.3.1. VPTG-STS associations
In medical settings, trauma exposure is typically indirect, and thus the association between trauma symptoms and growth typically assumes the form of the STS-VPTG link; yet here too, findings are disparate. Taubman-Ben-Ari and Weintroub (Citation2008), sampling physicians and nurses from three paediatric wards did not find any STS-VPTG association, suggesting that growth may be due to other factors. In a study sampling different hospital departments in Romania, a negative STS-VPTG correlation was observed in nurses, i.e. lower STS was linked with higher VPTG (Măirean, Citation2016). In another study (Kjellenberg, Nilsson, Daukantaite, & Cardena, Citation2014), medical personnel working with war survivors showed the aforementioned typical (positive) linear STS-VPTG association.
Curvilinear STS-VPTG associations were also observed in medical settings. In one study, only hospital psychologists (not physicians/nurses/social workers), displayed a curvilinear STS-VPTG association (Manning-Jones, de Terte, & Stephens, Citation2017). Shiri et al. (Citation2008), surveying a mixed sample including emergency room personnel, found a significant curvilinear STS-VPTG association for physicians and psychotherapists, but not for nurses, while a linear STS-VPTG association existed for all three professions. Shiri et al. (Citation2008) speculate that as opposed to nurses, physicians who showed a curvilinear association may be limited in their ability to grow due to coping mechanisms they developed to regulate their stress levels. Another study examining a mixed sample of nurses from different departments with a very high percentage of emergency room nurses (Shamia, Thabet, & Vostanis, Citation2015) found neither a linear nor a curvilinear association between work related STS and VPTG. Thus, although STS-VPTG associations were not hitherto examined in emergency room personnel, based on these two studies (Shamia et al., Citation2015; Shiri et al., Citation2008) which included a significant proportion of emergency room personnel, we hypothesize that for physicians, there should be both linear and curvilinear STS-VPTG associations (Shiri et al., Citation2008), while for nurses there should either be a linear STS-VPTG association (Shiri et al., Citation2008) or no STS-VPTG association (Shamia et al., Citation2015). Research reviewed by Kjellenberg et al. (Citation2014) may be revealing, as it suggests that low workload and low work experience may impact STS and growth. Accordingly, nurses with low work experience and low workload may indeed show an STS-VPTG association.
1.4. Summary of study aims
In summary, the first two goals of assessing STS and VPTG levels in emergency room nurses and physicians are exploratory in nature. Concerning our third goal, we hypothesized that emergency room physicians will likely show both linear and curvilinear STS-VPTG associations; for nurses, an STS-VPTG association may be evident under the conjoint condition of low workload and low work experience. The potential effects of demographic variables (e.g. sex, age, departmental work experience and marital status) and post-traumatic stress symptoms on the STS-VPTG association were controlled for in the research reported here.
2. Method
2.1. Participants
The study included emergency room physicians (n = 82) and nurses (n = 81) from one of the hospitals in the centre of the country. This study was approved both by the author’s University and by the hospital’s Helsinki Committee. All participants provided informed consent to the procedures approved by these committees. The inclusion criterion was at least six months of emergency room work experience.
2.2. Instruments
In addition to demographic variables (sex, age, education, marital status, work experience and workload) three measures were administered.
2.2.1. STS scale
This scale comprised 17 items (Bride et al., Citation2004; e.g. ‘I had little interest in being around others’). Participants responded on a 5-point Likert scale ranging from 1 (never) to 5 (very often). This scale has very good reliability (e.g. internal) and validity (convergent/discriminant/factorial, Bride et al., Citation2004). Internal reliability in the current study was high (Cronbach’s alpha =.91).
2.2.2. VPTG inventory
This scale comprised 21 items. Participants were asked to rate their change (e.g. ‘I changed my priorities about what is important in life’) by responding on a 6-point Likert scale ranging from 1 (experienced no change) to 6 (experienced a very great degree of change). This scale was developed by Tedeschi and Calhoun (Citation1996) and has excellent reliability (e.g. test-retest) and validity (convergent, discriminant and factorial). Instructions were to rate growth stemming from the challenging work in the emergency room. Cronbach’s alpha for VPTG was 0.94.
2.2.3. International trauma questionnaire
This measure comprised 6 items and is based on the 11th version of the International Classification of Diseases, known as the ICD-11 (World Health Organization, Citation2018). We selected this measure because: 1) Its overlap with the STS scale in items and structure is minimal, 2) These six items cover the same three clusters as the STS scale – recurrent thoughts, avoidance and arousal, 3) The scale’s excellent reliability and validity (see Cloitre et al., Citation2018). Items (e.g. ‘I feel jumpy or easily startled’) are responded to on a 5-point Likert scale ranging from 1 (not at all) to 5 (very much). Cronbach’s alpha for the international trauma questionnaire was 0.78.
2.3. Procedure
This survey was disseminated via a Google Docs link to emergency room personnel. The survey took 13–15 minutes to complete and the study ran for two months. The vast majority of participants (150 participants out of a total of 163) were recruited via a convenience sample, whereby the first author, an emergency room nurse at Wolfson Hospital, directly asked colleagues to participate in this study. To obtain as many emergency room participants as possible, sampling was supplemented by snowballing, whereby these colleagues put the first author in touch with other nurses/physicians working in the same emergency room. Questionnaires were anonymous.
2.4. Data analysis
All analyses were conducted with the SPSS 25 software package (IBM SPSS). The first and second hypotheses were examined by independent sample t-tests. The STS-VPTG association was examined both 1) by curve estimation analysis and 2) via a hierarchal regression, which may reveal if the curvilinear association holds beyond the linear association. Both analyses were conducted for the entire sample, and separately for physicians and nurses. An additional regression analysis was conducted whilst controlling for demographic variables (sex, marital status, post-traumatic stress symptoms and departmental work experience). A final regression analysis was conducted on nurses, to discern if STS-VPTG association exists under a conjoint interactive condition of two moderators, i.e. low work experience and low workload. The appropriate SPSS PROCESS plugin model (Hayes, Citation2018) was applied (Model-3) to probe the source for this interaction. All questionnaire items were obligatory, i.e. the Google Docs form could not be submitted until all items were responded to, thus there were no missing variables.
3. Results
3.1. Descriptive statistics
Descriptive statistics appear in , which shows that physicians and nurses differed in the distribution of sex and work experience. As depicted in , STS levels were identical for both nurses and physicians, t < 1. Likewise, VPTG levels for nurses and physicians were similar (), t = 1.31, df = 161, p > 0.19.
Table 1. Descriptive statistics (frequencies, means, ranges or standard deviations) for the study variables for the entire sample and separately for emergency room physicians and nurses
Table 2. Mean (SD) of sum VPTG and sum STS for emergency room personnel
3.2. Results of the STS-VPTG association
The STS-VPTG association was initially examined via curve estimation analysis, a method used in previous studies (e.g. Nuttman-Shwartz, Dekel, & Tuval-Mashiach, Citation2011). Both linear [F(1,161) = 7.41, p = .007] and curvilinear [F(2,160) = 6.44, p = 0.002] (see ) associations were significant.
Figure 1. Linear and curvilinear STS-VPTG associations for the entire sample (physicians and nurses)
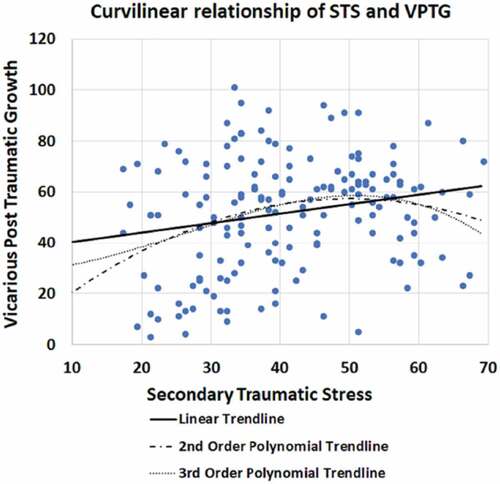
A hierarchal regression was conducted to discern if the curvilinear association held beyond the linear association (e.g. Kleim & Ehlers, Citation2009). STS was regressed on VPTG levels in Step 1, and VPTG squared (VPTG2) in Step 2. Both the linear (Step 1) association, β = 0.21, t = 2.72, p = .007 (), and the curvilinear (STS-VPTG2) association beyond the linear association, β = −0.80, t = 2.711, p = .007, were significant. The results remained significant after controlling for sex, marital status, PTSD levels and departmental work experience, i.e. linear association (β = .23, t = 2.86, p = .005), curvilinear association (β = −.776, t = 2.57, p = .011)
Table 3. Results of hierarchical regression analysis at each step
3.3. Results of STS-VPTG association in nurses and physicians
Both analyses were applied separately to nurses and physicians. For nurses, curve estimation analysis revealed neither a linear STS-VPTG association (F < 1) nor a curvilinear association [F(2,78) = 1.18, p = 0.31]. For physicians, however, both the linear [F(1,80) = 8.36, p = .005] and curvilinear [F(2,79) = 4.78, p = .01] associations were significant.
Similar results were obtained using hierarchical regression analysis, where STS was regressed on VPTG in Step 1, and on VPTG2 in Step 2. Nurses showed neither linear (β = .06, t = .50, p = .4) nor curvilinear (β = −.392, t = .80, p = .42) STS-VPTG associations. Physicians, however, displayed both linear (β = .37, t = 3.65, p = 0.0001) and curvilinear (β = −.85, t = 2.19, p = 0.03) STS-VPTG associations (). Results remained the same when controlling for sex, marital status, PTSD and departmental work experience in Step 1, VPTG in Step 2, and VPTG2 in Step 3.
Table 4. Results of hierarchical regression analysis that tested for an STS-VPTG curvilinear association (Step 2) beyond linear association (Step 1), for nurses and physicians
3.4. Moderation results of nurses’ STS-VPTG association
To assess if the STS-VPTG association in nurses would be moderated by work experience and workload, we conducted a final hierarchical regression analysis. We controlled for sex, marital status and post-traumatic stress disorder (results were the same without controlling for these variables) and found the expected three-way interaction. Namely, the conjoint effect of Night Shifts × Work Experience moderated the STS-VPTG association, B = 0.06, t = 2.04, p = 0.04. The source of this interaction was probed with the PROCESS plugin (Model-3, which is designed for two moderators) to further assess the STS-VPTG association at ±1 SD levels of work-experience and workload. As shown in , results reveal that only nurses with little work experience (≤ 2 years) and low workload (no night shifts) showed an STS-VPTG association, B = 1.6, t = 2.49, p = 0.01. Similar results were obtained for the curvilinear STS-VPTG association, both the interaction (B = 6.7, t = 2.02, p < 0.05) and its source (B = 146.79, t = 2.22, p < 0.05) appeared significant. Yet, this curvilinear relationship was not significant beyond the linear association, B = 0.04, t < 1.
4. Discussion
The current study shows similar STS levels for nurses and physicians. Previous findings indicating that nurses have higher STS levels than physicians were obtained from non-emergency room departments (e.g. Taubman-Ben-Ari & Weintroub, Citation2008) or cross-study comparisons of emergency room studies (see e.g. Roden-Foreman et al., Citation2017). The current results suggest that difficult emergency room work (Dominguez-Gomez & Rutledge, Citation2009) may be equally challenging to both nurses and physicians. The second finding showed similar VPTG levels in emergency room physicians and nurses. Previous data from other departments that revealed higher VPTG levels for nurses were explained by suggesting that nursing tasks comprise greater intimacy and involvement with the patient, versus physicians who see patients mainly on their rounds (Taubman-Ben-Ari & Weintroub, Citation2008). Although this task distinction seemingly characterizes emergency room personnel as well, the lack of quantitative differences in VPTG across professions does not preclude qualitative differences. This idea of a qualitative distinction is supported by the finding that while growth in physicians was linked to their STS, growth for nurses was unrelated to their STS.
4.1. Qualitative VPTG differences between nurses and physicians
For physicians, both the straightforward linear STS-VPTG association, and even more so the curvilinear association, are consistent with the notion of growth stemming from trauma (Tedeschi & Calhoun, Citation1996; Whealin et al., Citation2020). Growth for physicians may occur only for moderate levels of STS, as within this range, individuals retain sufficient resources to cope with both affect and cognition (Benight, Harwell, & Shoji, Citation2018). For emergency room physicians, higher STS levels may arrest growth (Zoellner & Maercker, Citation2006). Thus, maintaining STS at moderate levels may not only be efficacious, but a necessity.
In stark contrast, emergency room nurses’ growth levels were immune to their STS. Further research to discern the source of growth for emergency room nurses is required. Joseph and Linley (Citation2006) suggested that growth from adversity can occur in several manners, e.g. by increasing the value of friends/family, changing self-views or worldviews. Accordingly, growth in emergency room nurses may not directly stem from their STS but, rather, is speculated to stem from other factors, such as the nurses’ level of professional self-esteem (Taubman-Ben-Ari & Weintroub, Citation2008), social support (Măirean, Citation2016), and meaning in work (Gómez-Salgado, Navarro-Abal, López-López, Romero-Martín, & Climent-Rodríguez, Citation2019). In line with these speculations, nurses with low experience levels and thus, likely had lower social support, lower professional esteem and less meaning in work did show an STS-VPTG association, provided their workload was low (see Kjellenberg et al., Citation2014). Future research should address the source of growth in emergency room nurses and whether these factors drive growth independent of STS, or perhaps are driven by STS in an indirect manner (e.g. higher STS→higher social support→higher growth). Likewise, the finding that for physicians, STS levels were linked with VPTG levels does not preclude the impact of these factors – e.g. professional self-esteem and meaning in work – on physicians’ VPTG levels.
Taken together, the findings support the aforementioned notion that positive (VPTG) and negative (STS) outcomes of trauma may co-exist and co-vary (Shakespeare-Finch & Lurie-Beck, Citation2014), as in the case of physicians. At the same time, the current results also show that these positive and negative outcomes can independently co-exist without co-varying (Salsman et al., Citation2009), as displayed by nurses. This differential results pattern for each profession may resolve some of the aforementioned controversy surrounding the trauma-growth association (see review Shakespeare-Finch & Lurie-Beck, Citation2014; Whealin et al., Citation2020). Taken together, the current results suggest that STS may be a sufficient, but not a necessary, condition for growth.Footnote1
The current results also have important practical implications for emergency room personnel, where burnout is high and caregiving may suffer (Potter, Citation2006). Based on research showing that improving caregivers’ mental health may in turn improve caregiving level (Molnar et al., Citation2017), two implications are noted. First, the importance of monitoring and identifying excessive STS levels in emergency room physicians, whose higher STS level does not allow for growth. This may also be important for emergency room nurses, as high STS levels are unhealthy in and of themselves (e.g. Figley, Citation1995; Greinacher et al., Citation2019), even if they do not curb growth. Accordingly, charging a senior, experienced, and trained physician/medical psychologist with monitoring emergency room staff STS levels may be helpful in such identification. Second, introducing suitable interventions for physicians and nurses, to both reduce and prevent STS (e.g. mindfulness, Molnar et al., Citation2017) as well as to promote growth, e.g. via social support (Abu-Sharkia, Taubman–Ben‐Ari, & Mofareh, Citation2020) or via enhancing meaning in work (Gómez-Salgado et al., Citation2019). A final point worth considering is based on a recent study assessing decorated veterans, suggesting that appreciation by the organization may both reduce trauma symptoms and promote growth (Stein, Bachem, Lahav, & Solomon, Citation2020).
This study has several limitations: First, its cross-sectional design precludes determination of causality. Second, although the sampling method was suited to the study’s goal of obtaining the maximum amount of emergency room participants from the Wolfson Hospital as possible (Sadler, Lee, Lim, & Fullerton, Citation2010), it is possible that this narrow focus may have impaired generalizability to different emergency rooms. This topic may be explored in future research. Third, self-report measures as opposed to in-depth interviews were used. Fourth, this study could have benefited from a control group, e.g. nurses and physicians from different departments in the same hospital, as well as additional emergency rooms form other hospitals, as mentioned.
This study also has several strengths. First, STS was not previously measured in nurses and physicians from the same emergency room. Second, VPTG was not previously studied in emergency rooms. Third, the STS-VPTG association was examined here for the first time in the important emergency room context. Finally, the current study controlled for post-traumatic stress symptoms arising from direct exposure unrelated to work.
5. Conclusions
Emergency room nurses and physicians had the same levels of STS and VPTG. Yet while growth for physicians was associated with STS levels in both linear and curvilinear manners, VPTG for nurses was not associated with STS, suggesting that growth for nurses was driven by factors other than STS. Thus, although physicians and nurses may work in the same emergency room, be exposed to similar difficulties, and display similar STS and VPTG levels; the quality of the growth experience seems different and warrants future research. Such research will likely have an impact both on policy and on potential interventions.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability
The data that support the findings of this study are openly available as supplemental materials in https://osf.io/3bktf/
Additional information
Funding
Notes
1. This last point of STS being sufficient but not necessary for VPTG could be specific to STS, and may not apply to the related term of vicarious traumatization and its association with VPTG. Vicarious traumatization is sometimes used interchangeably with secondary traumatization and its status as a distinct term has been debated (see Dar & Iqbal, Citation2020 for review), yet many treat it as an independent construct with its own definition (Bourke & Craun, Citation2014). Namely, as opposed to secondary traumatization where the very same symptoms as in PTSD emerge after indirect trauma exposure, vicarious traumatization relates to a variety of changes in one’s cognitive schema following indirect exposure to trauma (Craig & Sprang, Citation2010). As such, the variety of changes associated with vicarious traumatization is more inclusive than the narrower PTSD symptoms of STS. Growth is driven by these very changes to one’s cognitive schema (e.g., Cohen & Collens, Citation2013). Accordingly, the finding that nurses’ STS is unrelated to VPTG, may not apply to vicarious traumatization, which relates to changes in cognitive schema deemed necessary for vicarious growth.
References
- Abu-Sharkia, S., Taubman–Ben‐Ari, O., & Mofareh, A. (2020). Secondary traumatization and personal growth of healthcare teams in maternity and neonatal wards: The role of differentiation of self and social support. Nursing & Health Sciences, 22(2), 283–11. doi:10.1111/nhs.12710
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4rd ed). American Psychiatric Association, Washington, DC: Author. doi:10.1176/ajp.152.8.1228
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5rd ed). American Psychiatric Association, Washington, DC: Author. doi:10.1176/appi.books.9780890425596
- Arnold, D., Calhoun, L. G., Tedeschi, R., & Cann, A. (2005). Vicarious posttraumatic growth in psychotherapy. Journal of Humanistic Psychology, 45(2), 239–263.
- Beck, C. T., & Gable, R. K. (2012). A mixed methods study of secondary traumatic stress in labor and delivery nurses. Journal of Obstetric, Gynecologic & Neonatal Nursing, 41(6), 747–760.
- Benight, C. C., Harwell, A., & Shoji, K. (2018). Self-regulation shift theory: A dynamic personal agency approach to recovery capital and methodological suggestions. Frontiers in Psychology, 9(1738), 1–8.
- Bourke, M. L., & Craun, S. W. (2014). Coping with secondary traumatic stress: Differences between U.K. and U.S. child exploitation personnel..Traumatology: An International Journal, 20(1), 57–64. doi:10.1037/h0099381
- Bride, B. E. (2007). Prevalence of secondary traumatic stress among social workers. Social Work, 52(1), 63–70.
- Bride, B. E., Robinson, M. R., Yegidis, B., & Figley, C. R. (2004). Development and validation of the Secondary Traumatic Stress Scale. Research on Social Work Practice, 14(1), 27–35.
- Butler, L. D., Blasey, C. M., Garlan, R. W., McCaslin, S. E., Azarow, J., Chen, X.-H., … Spiegel, D. (2005). Posttraumatic growth following the terrorist attacks of September 11, 2001: Cognitive, coping, and trauma symptom predictors in an internet convenience sample. Traumatology, 11(4), 247–267. doi:10.1177/153476560501100405
- Carey, S. A., Roden-Foreman, J. W., Felius, J., Tecson, K. M., Shelley, J., Hall, S. A., & Warren, A. M. (2019). Secondary traumatic stress in multi-disciplinary teams caring for heart and lung transplant patients. Traumatology, 25(4), 275–281.
- Cieslak, R., Anderson, V., Bock, J., Moore, B. A., Peterson, A. L., & Benight, C. C. (2013). Secondary traumatic stress among mental health providers working with the military. The Journal of Nervous and Mental Disease, 201(11), 917–925.
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., … Hyland, P. (2018). The International Trauma Questionnaire: Development of a self‐report measure of ICD‐11 PTSD and complex PTSD. Acta psychiatrica Scandinavica, 138(6), 536–546.
- Cohen, K., & Collens, P. (2013). The impact of trauma work on trauma workers: A metasynthesis on vicarious trauma and vicarious posttraumatic growth.. Psychological Trauma: Theory, Research, Practice, and Policy, 5(6), 570–580 doi:10.1037/a0030388
- Craig, C. D., & Sprang, G. (2010). Compassion satisfaction, compassion fatigue, and burnout in a national sample of trauma treatment therapists. Anxiety, Stress, & Coping, 23(3), 319–339. doi:10.1080/10615800903085818
- Dar, I. A. & Iqbal, N. (2020). Beyond Linear Evidence: the Curvilinear Relationship between Secondary Traumatic Stress and Vicarious Posttraumatic Growth among Healthcare Professionals. Stress and Health, 36(2), 203-–212. doi:10.1002/smi.v36.2
- Dekel, S., Ein-Dor, T., & Solomon, Z. (2012). Posttraumatic growth and posttraumatic distress: A longitudinal study. Psychological Trauma: Theory, Research, Practice, and Policy, 4(1), 94.
- Dominguez-Gomez, E., & Rutledge, D. (2009). Prevalence of secondary traumatic stress among emergency nurses. Journal of Emergency Nursing, 35(3), 199–204.
- Duffy, E., Avalos, G., & Dowling, M. (2015). Secondary traumatic stress among emergency nurses: A cross-sectional study. International Emergency Nursing, 23(2), 53–58.
- Figley, C. (1995). Compassion fatigue: Toward a new understanding of the cost of caring. In B. Stamm (Ed.), Secondary traumatic stress: Self care issues for clinicians, researchers and educators (pp. 3–28). Lutherville: Sidran Press.
- Figley, C. R. (1999). Compassion fatigue: Toward a new understanding of the cost of caring. In B. H. Stamm (Ed.), Secondary traumatic stress (pp. 3–28). Towson, MD: Sidran Institute.
- Frazier, P., Conlon, A., & Glaser, T. (2001). Positive and negative life changes following sexual assault. Journal of Consulting and Clinical Psychology, 69(6), 1048–1055.
- Gómez-Salgado, J., Navarro-Abal, Y., López-López, M., Romero-Martín, M., & Climent-Rodríguez, J. (2019). Engagement, passion and meaning of work as modulating variables in nursing: A theoretical analysis. International Journal of Environmental Research and Public Health, 16(1), 108.
- Greinacher, A., Derezza-Greeven, C., Herzog, W., & Nikendei, C. (2019). Secondary traumatization in first responders: A systematic review. European Journal of Psychotraumatology, 10(1), 1562840.
- Hall, B. J., Saltzman, L. Y., Canetti, D., & Hobfoll, S. E. (2015). A longitudinal investigation of the relationship between posttraumatic stress symptoms and posttraumatic growth in a cohort of Israeli Jews and Palestinians during ongoing violence. PLoS One, 10(4), e0124782.
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford.
- Hoffman, Y., & Shrira, A. (2017). Shadows of the past and threats of the future: ISIS anxiety among grandchildren of Holocaust survivors. Psychiatry Research, 253, 220–225. doi:10.1016/j.psychres.2017.03.053
- Joseph, S., & Linley, P. A. (2006). Growth following adversity: Theoretical perspectives and implications for clinical practice. Clinical Psychology Review, 26(8), 1041–1053.
- Karanikola, M., Giannakopoulou, M., Mpouzika, M., Kaite, C. P., Tsiaousis, G. Z., & Papathanassoglou, E. D. (2015). Dysfunctional psychological responses among Intensive Care Unit nurses: A systematic review of the literature. Revista da Escola de Enfermagem da USP, 49(5), 847–857.
- Kjellenberg, E., Nilsson, F., Daukantaite, D., & Cardena, E. (2014). Transformative narratives: The impact of working with war and torture survivors. Psychological Trauma: Theory, Research, Practice, and Policy, 6, 120–128.
- Kleim, B., & Ehlers, A. (2009). Evidence for a curvilinear relationship between posttraumatic growth and posttraumatic depression and PTSD in assault survivors. Journal of Traumatic Stress, 22(1), 45–52.
- Lev-Wiesel, R., Goldblatt, H., Eisikovits, Z., & Admi, H. (2009). Growth in the shadow of war: The case of social workers and nurses working in a shared war reality. British Journal of Social Work, 39(6), 1154–1174.
- Măirean, C. (2016). Secondary traumatic stress and posttraumatic growth: Social support as a moderator. The Social Science Journal, 53(1), 14–21.
- Manning-Jones, S., de Terte, I., & Stephens, C. (2016). Secondary traumatic stress, vicarious posttraumatic growth, and coping among health professionals: A comparison study. New Zealand Journal of Psychology, 45(1), 20–29.
- Manning-Jones, S., de Terte, I., & Stephens, C. (2017). The relationship between vicarious posttraumatic growth and secondary traumatic stress among health professionals. Journal of Loss & Trauma, 22(3), 256–270.
- Molnar, B. E., Sprang, G., Killian, K. D., Gottfried, R., Emery, V., & Bride, B. E. (2017). Advancing science and practice for vicarious traumatization/secondary traumatic stress: A research agenda. Traumatology, 23(2), 129.
- Morrison, L. E., & Joy, J. P. (2016). Secondary traumatic stress in the emergency department. Journal of Advanced Nursing, 72(11), 2894–2906.
- Nuttman-Shwartz, O., Dekel, R., & Tuval-Mashiach, R. (2011). Post-traumatic stress and growth following forced relocation. British Journal of Social Work, 41(3), 486–501.
- Pargament, K. I., Smith, B. W., Koenig, H. G., & Perez, L. (1998). Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion, 37(4), 710.
- Potter, C. (2006). To what extent do nurses and physicians working within the emergency department experience burnout: A review of the literature. Australasian Emergency Nursing Journal, 9(2), 57–64.
- Quinal, L., Harford, S., & Rutledge, D. N. (2009). Secondary traumatic stress in oncology staff. Cancer Nursing, 32(4), E1–E7.
- Roden-Foreman, J. W., Bennett, M. M., Rainey, E. E., Garrett, J. S., Powers, M. B., & Warren, A. M. (2017). Secondary traumatic stress in emergency medicine clinicians. Cognitive Behaviour Therapy, 46(6), 522–532.
- Sadler, G. R., Lee, H.-C., Lim, R. S.-H., & Fullerton, J. (2010). Recruitment of hard‐to‐reach population subgroups via adaptations of the snowball sampling strategy. Nursing & Health Sciences, 12(3), 369–374.
- Salsman, J. M., Segerstrom, S. C., Brechting, E. H., Carlson, C. R., & Andrykowski, M. A. (2009). Posttraumatic growth and PTSD symptomatology among colorectal cancer survivors: A three-month longitudinal examination of cognitive processing. Psycho-oncology, 18(1), 30–41.
- Setti, I., Lourel, M., & Argentero, P. (2016). The role of affective commitment and perceived social support in protecting emergency workers against burnout and vicarious traumatization. Traumatology, 22(4), 261.
- Shakespeare-Finch, J., & Lurie-Beck, J. (2014). A meta-analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. Journal of Anxiety Disorders, 28(2), 223–229.
- Shamia, N. A., Thabet, A. A. M., & Vostanis, P. (2015). Exposure to war traumatic experiences, post‐traumatic stress disorder and post‐traumatic growth among nurses in Gaza. Journal of Psychiatric and Mental Health Nursing, 22(10), 749–755.
- Shiri, S., Wexler, I. D., Alkalay, Y., Meiner, Z., & Kreitler, S. (2008). Positive psychological impact of treating victims of politically motivated violence among Hospital-Based Health Care Providers. Psychotherapy and Psychosomatics, 77(5), 315–318.
- Solomon, Z., & Dekel, R. (2007). Posttraumatic stress disorder and posttraumatic growth among Israeli ex‐POWs. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 20(3), 303–312.
- Stein, J. Y., Bachem, R., Lahav, Y., & Solomon, Z. (2020). The aging of heroes: Posttraumatic stress, resilience and growth among aging decorated veterans. The Journal of Positive Psychology, 1–8. doi:10.1080/17439760.2020.1725606
- Taubman-Ben-Ari, O., & Weintroub, A. (2008). Meaning in life and personal growth among pediatric physicians and nurses. Death Studies, 32(7), 621–645.
- Tedeschi, R. G., & Calhoun, L. G. (1995). Trauma and transformation: Growing in the aftermath of suffering. Thousand Oaks, CA: Sage. doi:10.4135/9781483326931
- Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471.
- Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18.
- Warren, A. M., Jones, A. L., Shafi, S., Roden-Foreman, K., Bennett, M. M., & Foreman, M. L. (2013). Does caring for trauma patients lead to psychological stress in surgeons? Journal of Trauma and Acute Care Surgery, 75(1), 179–184.
- Weiniger, C. F., Shalev, A. Y., Ofek, H., Freedman, S., Weissman, C., & Einav, S. (2006). Posttraumatic stress disorder among hospital surgical physicians exposed to victims of terror: A prospective, controlled questionnaire survey. Journal of Clinical Psychiatry, 67(6), 890–896.
- Whealin, J. M., Pitts, B., Tsai, J., Rivera, C., Fogle, B. M., Southwick, S. M., & Pietrzak, R. H. (2020). Dynamic interplay between PTSD symptoms and posttraumatic growth in older military veterans. Journal of Affective Disorders, 269, 185–191.
- World Health Organization. (2018). International statistical classification of diseases and related health problems (11th ed). 6B40 Post traumatic stress disorder. Retrieved from https://icd.who.int/browse11/l-m/en#/id.who.int/icd/entity/2070699808
- Zerach, G., & Shalev, T. B. I. (2015). The relations between violence exposure, posttraumatic stress symptoms, secondary traumatization, vicarious post traumatic growth and illness attribution among psychiatric nurses. Archives of Psychiatric Nursing, 29(3), 135–142.
- Zoellner, T., & Maercker, A. (2006). Posttraumatic growth in clinical psychology—A critical review and introduction of a two component model. Clinical Psychology Review, 26(5), 626–653.